#Motility Disorders
Explore tagged Tumblr posts
Text
If nothing improves in the next 4 weeks, I will be getting referred to the feeding tube team at my hospital. There will probably be an additional wait before I can get in with them. What's the best way to advocate for a feeding tube that bypasses my stomach when ive been vomiting 1-2 times a day; subsisting on 1 small, solid meal most days and the rest oral intake of feeding tube formula and still vomiting up my meds at least once to twice a week; and having acute flares where i vomit repeatedly and can't keep down any food, fluids, or meds for days and days and destabilize in my other medical conditions as a result. And I'm nauseous and having abdominal pain daily, too. My diagnosis is gastroparesis and global dysmotility. I'm autistic and have to plan ahead what I'm going to say at appointments to program my Lingraphica AAC device, and id like advice on what to share and how to advocate because these are new doctors ro me and a new thing to advocate for, and I think it could really improve my quality of life.
#gastroparesis#feeding tube#medical advocacy#advice#scripting#aac user#actually autistic#actually audhd#gi issues#actually autism#global dysmotility#motility#communication disorder
0 notes
Text
Gastric Motility Disorder Drug: New Treatments Emerging for Difficult Gastric Disorders

Understanding Gastric Motility Disorder Drug GMD are a group of conditions that affect the normal movement of contents through the stomach. The stomach acts as a holding chamber, churning and partially breaking down food before advancing it into the small intestine. In GMD, this process is disrupted leading to a variety of symptoms. Some common types of GMD include gastroparesis, dysfunctional dyspepsia, and nausea and vomiting of unknown cause. Gastroparesis, or delayed gastric emptying, occurs when the stomach takes too long to empty its contents. This allows food to linger and ferment in the stomach, causing discomfort. Symptoms of gastroparesis include vomiting, heartburn, bloating, and abdominal pain after eating. Dysfunctional dyspepsia is characterized by these same symptoms but normal gastric emptying. The exact cause is unknown. Nausea and vomiting of unknown cause involves episodes of nausea and vomiting without an identifiable trigger. All of these conditions can greatly impact quality of life. Current Treatment Limitations The current treatment paradigm for Gastric Motility Disorder Drug focuses on symptom management rather than addressing the underlying dysfunction. For gastroparesis, dietary changes such as smaller, more frequent low-fat meals are recommended, along with prokinetic drugs to stimulate gastric emptying. However, available prokinetics have important tolerability issues and limited efficacy. Metoclopramide is often used but can cause Parkinsonism-like side effects with long-term use. Domperidone is not approved in the U.S. due to cardiac concerns. For symptoms like nausea and vomiting, antiemetics are utilized, but they do not work for all patients and their effects are temporary. Other approaches used include antacids and proton pump inhibitors for reflux relief. While these measures provide some benefit, they do not correct the gastric dysmotility driving the ongoing symptoms. A large unmet need exists for new options that can more predictably and sustainably improve gastric function and resolution of symptoms for those suffering from these difficult disorders. Emerging Treatments Targeting Underlying Pathophysiology Researchers are pursuing novel mechanisms that could restore normal coordinated gastric contractions in order to enhance emptying. One approach involves enhancing vagal nerve stimulation, important for controlling gastric motility. Implantable neurostimulation devices are being studied to electrically activate the vagus nerve in a coordinated manner. Early data suggests increased antral contractions and symptom improvement compared to sham stimulation in gastroparesis patients. Further development is ongoing. Aside from neurostimulation, pharmacological agents targeting specific receptors involved in gastric motility are being investigated. One drug enhances the activity of motilin, a hormone critical for digestive muscle contractions. It is currently in Phase III testing for gastroparesis. By mimicking the natural process motilin triggers, this medication may have the potential to safely and effectively promote gastric emptying in a sustained manner. Another compound under study targets a bile acid receptor called TGR5. TGR5 activation leads to GLP-1 release which drives gastric emptying. Preliminary results show more rapid gastric emptying compared to placebo in healthy individuals. If successful in motility disorders, these novel mechanisms could change the fundamental treatment paradigm. Get More Insights On This Topic: Gastric Motility Disorder Drug
#Gastric Motility Disorder Drug#Digestive Health#Gastrointestinal Disorders#Pharmacotherapy#Digestive System#Gastroenterology#Medication#Treatment Options
0 notes
Text
tysm!!! i'm also writing for this instagram account called Sanitas Vitae (focusing on biology and medicine) for their Specialty Sundays!!
guyssss my writing got accepted by this magazine called wonton's letter!! it was a poem <3
#hap��s happenings#mutuals#my first piece was on gastroenterology (colonic motility disorders - ibs)
4 notes
·
View notes
Text
Because my most popular post is about weight loss and how it's a crock, I get a lot of questions about various things, including bariatric surgery--just posted the link to the post I did about that--but also Ozempic/Wegovy, the once-weekly injectable semaglutide medication that was developed for diabetes but was found to have independent benefits on weight loss.
I always said that weight loss was like Viagra: when a medication came along that actually worked, it would explode. We'd all hear about it. Fen-phen in the 90s worked, but it was bad for your heart. Stimulants, like meth, may cause weight loss, but they do it at the cost of heart health, and raise your likelihood of dying young. Over the counter weight loss supplements often contain illegal and unlisted thyroid hormone, which is also dangerous for the heart if taken in the absence of a real deficiency. Orlistat, or "Alli," works the same way as the Olestra chips Lays made in the 1990s--it shuts off your ability to digest fats, and the problem with that is that fats irritate the gut, so then you end up with fatty diarrhea and probably sharts. Plus Alli only leads to 8-10lbs of weight loss in the best case scenario, and most people are not willing to endure sharts for the sake of 8lbs.
And then came the GLP-1 agonists. GLP stands for glucagon-like peptide. Your body uses insulin to make cells uptake sugar. You can't just have free-floating sugar and use it, it has to go into the cells to be used. So if your body sucks at moving sugar into the cells, you end up with a bunch of glucose hanging out in places where it shouldn't be, depositing on small vessels, damaging nerves and your retinas and kidneys and everywhere else that has a whole lot of sensitive small blood vessels, like your brain.
Glucagon makes your liver break down stored sugars and release them. You can think of it as part of insulin's supporting cast. If your body needs sugar and you aren't eating it, you aren't going to die of hypoglycemia, unless you've got some rare genetic conditions--your liver is going to go, whoops, here you go! and cough it up.
But glucagon-like peptide doesn't act quite the same way. What glucagon-like peptide does is actually stimulating your body to release insulin. It inhibits glucagon secretion. It says, we're okay, we're full, we just ate, we don't need more glucagon right now.
This has been enough for many people to both improve blood sugar and cause weight loss. Some patients find they think about food less, which can be a blessing if you have an abnormally active hunger drive, or if you have or had an eating disorder.
However, every patient I've started on semaglutide in any form (Ozempic, Wegovy, or Rybelsus) has had nausea to start with, probably because it slows the rate of stomach emptying. And that nausea sometimes improves, and sometimes it doesn't. There's some reports out now of possible gastroparesis associated with it, which is where the stomach just stops contracting in a way that lets it empty normally into the small intestine. That may not sound like a big deal, but it's a lifelong ticket to abdominal pain and nausea and vomiting, and we are not good at treating it. We're talking Reglan, a sedating anti-nausea but pro-motility agent, which makes many of my patients too sleepy to function, or a gastric pacemaker, which is a relatively new surgery. You can also try a macrolide antibiotic, like erythromycin, but I have had almost no success in getting insurance to cover those and also they have their own significant side effects.
Rapid weight loss from any cause, whether illness, medication, or surgery, comes with problems. Your skin is not able to contract quickly. It probably will, over long periods of time, but "Ozempic face" and "Ozempic butt" are not what people who want to lose weight are looking for. Your vision of your ideal body does not include loose, excess skin.
The data are also pretty clear that you can't "kick start" weight loss with Ozempic and then maintain it with behavioral mechanisms. If you want to maintain the weight loss, you need to stay on the medication. A dose that is high enough to cause weight loss is significantly higher than the minimum dose where we see improvements in blood sugar, and with a higher dose comes higher risk of side effects.
I would wait on semaglutide. I would wait because it's been out for a couple of years now but with the current explosion in popularity we're going to see more nuanced data on side effects emerging. When you go from Phase III human trials to actual use in the world, you get thousands or millions more data points, and rare side effects that weren't seen in the small human trials become apparent. It's why I always say my favorite things for a drug to be are old, safe, and cheap.
I also suspect the oral form, Rybelsus, is going to get more popular and be refined in some way. It's currently prohibitively expensive--all of these are; we're talking 1200 or so bucks a month before insurance, and insurance coverage varies widely. I have patients who pay anything from zero to thirty to three hundred bucks a month for injectable semaglutide. I don't think I currently have anyone whose insurance covers Rybelsus who could also tolerate the nausea. My panel right now is about a thousand patients.
There are also other GLP-1 agonists. Victoza, a twice-daily injection, and Trulicity, and anything else that ends in "-aglutide". But those aren't as popular, despite being cheaper, and they aren't specifically approved for weight loss.
Mounjaro is a newer one, tirzepatide, that acts on two receptors rather than one. In addition to stimulating GLP-1 receptors, it also stimulates glucose-dependent insulinotropic polypeptide (GIP) receptors. It may work better; I'm not sure whether that's going to come with a concomitantly increased risk of side effects. It's still only approved for diabetes treatment, but I suspect that will change soon and I suspect we'll see a lot of cross-over in terms of using it to treat obesity.
I don't think these medications are going away. I also don't think they're right for everyone. They can reactivate medullary thyroid carcinoma; they can fuck up digestion; they may lead to decreased quality of life. So while there may be people who do well with them, it is okay if those people are not you. You do not owe being thin to anyone. You most certainly do not owe being thin to the extent that you should risk your health for it. Being thin makes navigating a deeply fat-hating world easier, in many ways, so I never blame anyone for wanting to be thin; I just want to emphasize that it is okay if you stay fat forever.
783 notes
·
View notes
Note
Hi! This might be an odd question but do you know where a layperson could read/learn about paraplegia and other neurological disorders in cats and dogs? I don't have any pets with that issue, but I was recently diagnosed with BLE spasticity, and as someone who draws and writes about animals frequently, it made me wonder if the same thing can happen to them. Of course I've seen photos and videos of paraplegic cats and dogs, but I have no idea if they're actually experiencing something similar to me (spastic or flaccid? sensory loss or paresthesia or just motor loss? does it affect their GI motility or other spinal cord functions as well? etc). I hope that makes sense, thank you for any pointers!
Hi, Sueanoi here.
My favorite resource is Merck Manual. They have pet owner version and professional version that you can read.
Unfortunately "Paraplegia" is not a disease name. It is a symptom that can be caused by many nuanced etiology. The page I recommend you start is this one.
26 notes
·
View notes
Text
It's Gastroparesis Awareness Month
Hi! I have gastroparesis and I'm an insufferable know-it-all so let's talk about it!
Gastroparesis, or a paralyzed stomach, is a condition that causes delayed gastric emptying.
This can cause a range of symptoms and complications:
nausea
vomiting
early satiety/fullness
upper gastric pain
heartburn
malabsorption
dehydration
malnutrition
Gastroparesis can be treated by a gastroenterologist, but often needs to be managed by a motility specialist due to a lot of misconceptions about the condition. Providers, especially in the emergency department, will commonly misdiagnose gastroparesis as cannabis-hyperemesis syndome, cyclic vomiting syndrome, gastritis, food poisoning, etc.
There are several commonly known causes of gastroparesis like vagus nerve damage from diabetes, injury to the stomach, and stomach surgery like hernia repair or bariatric surgery. There are also idiopathic cases with no known cause. Other causes of gastroparesis are:
Connective tissue disorders like HSD and EDS (commonly hEDS and cEDS)
Post-viral (like COVID, viral gastritis, mononucleosis/Epstein-Barr)
Restrictive eating disorders
Autoimmune diseases like Systemic sclerosis (scleroderma), Lupus, Hashimoto's
Central nervous system disorders
Gastroparesis also has common comorbidities with conditions like:
POTS and other forms of dysautonomia (POTS, EDS, and gastroparesis are a common triad of diagnoses)
MCAS
SMAS (which can also present with similar symptoms to GP)
Intestinal dysmotility and esophageal dysmotility disorders (known as global dysmotility)
PCOS with insulin resistance
Endometriosis
SIBO/SIFO
Chronic intestinal pseudo-obstruction
Migraines
Certain medications like Ozempic and other drugs in that class act on the digestive system to delay gastric emptying, which has caused people to be diagnosed with gastroparesis. Some people report that their cases have not gone away since stopping the medication, others report feeling better after stopping. Other drugs like opiates and narcotics can cause delayed gastric and intestinal motility as well, but these are commonly known side effects of those painkiller classes.
Gastroparesis is classed based on severity and graded based on how you respond to treatment.
Severity of delay ranges from mild to very severe, and this is based on your actual stomach retention calculated at 4 hours into a gastric emptying study.
The grading scale ranges from one to three, one being mild and three being gastric failure.
There is no consistent single treatment that is proven to work for gastroparesis, and there is no cure. Treatments can consist of:
Diet changes (3 Step Gastroparesis Diet, liquid diet, oral sole source nutrition)
Prokinetic (motility stimulating) drugs
Anti-nausea medications
Proton-pump inhibitors
Gastric stimulator/gastric pacemaker
Pyloric botox and dilation
G-POEM/pyloroplasty
Post-pyloric tube feeding
Gastric venting/draining
Parenteral nutrition
IV fluids
Other surgical interventions like gastrectomy or rarely, transplant
Gastroparesis is a terrible disease and I hope that if any of these symptoms resonate with you that you can get checked out. I was misdiagnosed for a long time before getting a proper gastroparesis diagnosis, and all it took was a gastric emptying study. This is ESPECIALLY true if you're having post-COVID gastrointestinal problems that are not improving. I almost died from starvation ketoacidosis because of how serious my GP got in a short period of time post-COVID (I had GP before COVID), and now I'm tube reliant for all my nutrition and hydration.
Stay safe friends!
673 notes
·
View notes
Text
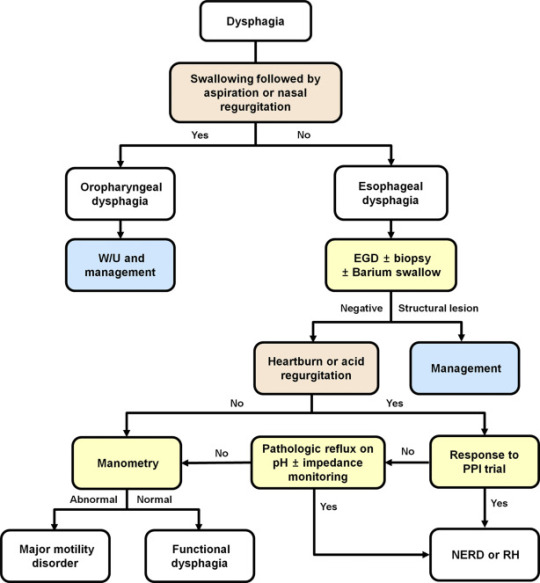
Explaining dysphagia
Dysphagia is simultaneously a symptom and a diagnosable condition. Most people think of it (if they think of it at all) as the choking on food disease but in reality it's much more complicated than that.
There are four categories of dysphagia: oropharyngeal, esophageal, esophagogastric, and paraesophageal
only two of those categories (oropharyngeal and esophageal) are commonly used and diagnosed so those are the main two I'll be talking about.
The diagnosis of dysphagia is a fairly complicated process involving a lot of radiological testing and things stuck up your nose and down your throat.
lost the source :(
source
the ICD 10 further divides dysphagia into unspecified, oral phase, oropharyngeal phase, pharyngeal phase, pharyngoesophageal phase, and other dysphagia which includes cervical dysphagia and neurogenic dysphagia
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when someone has difficulty initiating a swallow. It's often accompanied by coughing, choking, feeling food stick in the throat, and nasal regurgitation. Other symptoms include frequent repetitive swallows, frequent throat clearing, a gargly voice after meals, hoarse voice, nasal speech and dysarthria, drooling, and recurrent pneumonia.
Oropharyngeal dysphagia is diagnosed with a modified barium swallow and/or a transnasal video endoscopy.
Some of the consequences of oropharyngeal dysphagia include aspiration pneumonia, upper respiratory infections, and weight loss. Common treatment includes rehabilitative swallowing exercises, botox, surgery, and/or a feeding tube.
Esophageal Dysphagia
Esophageal dysphagia is dysphagia where there is a problem with the passage of food or liquids through the esophagus between the upper and lower esophageal sphincter. Esophageal dysphagia is usually a result of abnormal motility in the esophagus or a physical obstruction to the esophagus. Symptoms of esophageal dysphagia vary depending on cause.
Motility: People with esophageal motility disorders will experience problems with swallowing both liquids and solids. Motility disorders consist of abnormal numbers of contractions in the esophagus, abnormal velocity of contractions, abnormal force of contractions, abnormal coordinated timing of contractions, or several of these simultaneously. People with esophageal motility disorders may also experience spasms or chest pain.
Obstruction: People with an esophageal obstruction will have more difficulty swallowing solids than liquids.
Some symptoms of both include pain when swallowing, the inability to swallow, sensation of food being stuck in your throat or chest, drooling, and regurgitation.
Esophageal dysphagia can be diagnosed with a barium swallow, upper endoscopy, esophageal manometry, and an endoFLIP.
Some common treatments for esophageal dysphagia include medication, esophageal dilation, surgery, stent placement, and/or a feeding tube.
Esophagogastric Dysphagia
Esophagogastric dysphagia occurs when there is a problem with material passing from the lower esophageal sphincter into the gastric fundus.
Paraesophageal Dysphagia
Paraesophageal dysphagia occurs when the esophagus is narrowed due to extrinsic compression.
The ICD 10 Classifications
Oral phase - difficulty moving food or liquid to the back of the throat
Oropharyngeal phase - difficulty initiating swallowing
Pharyngeal phase - difficulty swallowing when food or liquid is at the top of the throat
Pharyngoesophageal phase - unable to find information
Other dysphagia- cervical dysphagia (caused by problems with the cervical spine) or neurogenic dysphagia (caused by problems with the central or peripheral nervous system)
Sources
x x x
+ some others I definitely (/sarcasm) didn't lose the link to
98 notes
·
View notes
Text
at a christian high school graduation and not to sound dramatic but im having a trauma response so im in the bathroom thankfully i can claim a motility disorder
11 notes
·
View notes
Text
symptoms of dysautonomia ✿
these are all of the symptoms of dysautonomia I could find. two disclaimers: 1) please don't use this to diagnose yourself, lots of these symptoms overlap with other disorders, and 2) some of these symptoms may only apply to certain dysautonomias and not to others, in which case I will attempt to specify.
also these categories are very nonspecific and kinda weirdly ordered. I just needed to have the symptoms vaguely organized, lol.
neurological
headaches
migraines
dizziness
tinnitus
tremors
vertigo
brain fog
syncope
presyncope
motor / body
weakness/loss of muscle strength
muscle tension
lack of coordination
unsteady gait
stiffness (in MSA)
hypermobility
absence of tendon reflexes
spasms
low tone (in FD)
body/joint pain
sensation / neuropathic
abnormal sensation
neuropathy (numbness/tingling)
insensitivity to pain
diminished sense of temperature
diminished sense of touch
skin
extreme itching
skin reactions/rashes
dry skin
flushing
pale pallor
eyes
dry eye
eye pain
excessive tearing
blurred vision
tunnel vision
vision loss
impaired pupillary response
light sensitivity
ears / mouth
sound sensitivity
dry mouth
tooth decay
difficulty swallowing
abnormal saliva production
circulatory / heart
tachycardia
bradycardia
heart palpitations
irregular heart rate
poor circulation
cold extremities
discolored skin
blood pooling
low blood pressure
high blood pressure
low blood volume
pulmonary / chest
chest pain
shortness of breath
pain while breathing
air hunger
stomach / digestion
general nausea
postprandial nausea
vomiting
indigestion
bloating
abdominal pain
loss of appetite
weight loss
impaired motility/gastric emptying
food intolerances
constipation
diarrhea
frequent urination
painful urination
painful bowel movements
irregular bowel movements
reproductive
irregular periods
painful periods
sexual dysfunction
psychological
anxiety
depression
sense of impending doom
mood swings
poor memory
irritability
sleep
insomnia
night sweats
circadian rhythm disorders
unrestful sleep
general / miscellaneous (aka idk where to put this)
adrenaline dumps
"coat hanger" neck/shoulder pain
temperature intolerance/dysregulation
low body temperature
exercise intolerance
caffeine intolerance
excessive sweating (hyperhidrosis)
lack of sweating (hypohidrosis)
inflammation
galbladder inflammation
galbladder pain
low blood sugar
excessive thirst
#autonomic dysfunction#autonomic nervous system#ans#dysautonomia#pots#pots syndrome#postural orthostatic tachycardia syndrome#ist#inappropriate sinus tachycardia#vasovagal syncope#nervous system#disability#disabled#actually disabled#disability awareness#dysautonomia awareness
13 notes
·
View notes
Text
📌PINNED POST📌
ₓ˚. ୭ ˚○◦˚ℍ𝕖𝕝𝕝𝕠 𝕖𝕧𝕖𝕣𝕪𝕠𝕟𝕖!!˚◦○˚ ୧ .˚ₓ
╰┈➤ Welcome to my page! Here I will be posting disability and chronic illness awareness content. I live with multiple disabilities and chronic illnesses, some of which include (Yes, I'm diagnosed!):
❁ Tourette's Syndrome (TS)
❁ Gastroparesis
❁ Postural Orthostatic Tachycardia Syndrome (POTS)
❁ Guillain-Barré Syndrome (GBS)
❁ Non Epileptic Seizures (NES/PNES/NEAD)
❁ Ineffective Esophageal Motility (IEM)
❁ Essential Tremor Disorder
❁ Autism Spectrum Disorder (ASD)
**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**

**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**
╰┈➤ I also struggle with quite a few mental illnesses, some of wish are:
❁ Borderline Personality Disorder (BPD)
❁ Obsessive Compulsive Disorder (OCD)
❁ Post Traumatic Stress Disorder (PTSD)
❁ Generalized Anxiety Disorder (GAD)
❁ Major Depressive Disorder (MDD)
**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**

**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**
╰┈➤ Due to living with these conditions, I have a medical device called a G Tube, which is a surgically placed feeding tube that goes directly into the stomach. I also use different mobility aids for GBS including a wheelchair, walker, crutches, cane, and AFO braces. These all give me the ability to be independent and survive. I'll be sharing my experiences with these conditions and devices on this account! I also have other socials as well! I'll link them below!
https://www.instagram.com/chronically_strawberry?igsh=dGpucTkxbThvbnA4
╰┈➤ Now that I've got all that out of the way, I want to talk a little more about who I am! Starting with the fact that I'm an artist! I love everything creative. I like to draw (traditional and digital), paint, crochet, sculpt, and really anything I can get my hands on. I also like to write! Stories and poetry! Singing is another thing I like to do, along with gaming. Being out in nature is one of my favorite things though. I like to hike, skateboard, ride my bike, and anything active. (When my body will allow it.) When I'm not feeling up to doing more active things, I'll usually end up doing something creative, working on my socials, or playing things like Cult of the Lamb, Dress to Impress, Far Cry 5, Overwatch, Minecraft, and many more games.
╰┈➤Next I want to get into my interests. I really like anime. Some of my favorite animes are Blue Lock, The Disastrous Life of Saiki K, and Sk8 the Infinity, though I'll be making a whole section of this post listing the animes I like XD! I also like music. My favorite artist is My Chemical Romance, though I have so many runner-ups. I like science, space, nature, plants, bugs, mushrooms, moths, cosplay, and plushies!
**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**

**✿❀○❀✿*✿❀○❀✿*✿❀○❀✿**
╰┈➤ My Favorite Animes: Blue Lock, The Disastrous Life of Saiki K, Blue Period, Bungo Stray Dogs, Mob Psycho 100, Yuri!!! On Ice, Sk8 the Infinity, Made In Abyss, Higurashi No Naku Koro Ni, Another, Given, Seraph of the End, Last Hope, Voltron (Not an anime but I love it!), Pokémon, Parasyte, Fairy Tail, Run with the Wind, Black Butler, Mobile Suit Gundam Unicorn, Haikyuu, Deadman Wonderland, Tokyo Ghoul, Alice in Borderland (Also not an anime but 100% reccomend!), Love Stage, Persona 5, Black Lagoon, Sailor Moon, Terror in Resonance, more cuz I'm probably forgetting some.
╰┈➤ That's all! I can't wait to start posting here!
#feeding tube#physically disabled#wheelchair user#wheelchair#accessibility#pots syndrome#disabled community#actually chronically ill#chronic disability#disability#disabled#actually disabled#invisible disability#invisible illness#guillainbarresyndrome#gbs#gastroparesis#g tube#autism#autistic adult#actually autistic#asd#potsie#potsawareness#pots#spoonie#tourettes#actually tourettic#tics#tics and tourettes
11 notes
·
View notes
Text
Breakthroughs in Treatment: Gastric Motility Disorder Drug Unveiled

Gastric motility disorders can significantly impact an individual's quality of life, leading to symptoms such as bloating, nausea, and delayed gastric emptying. Fortunately, recent advancements in medical research have led to the development of promising treatments, including the introduction of novel Gastric Motility Disorder Drug therapies.
Exploring the Potential of Gastric Motility Disorder Drug:
Targeted Therapeutic Approach: Gastric Motility Disorder Drug therapies aim to address the underlying causes of gastric dysmotility, targeting specific receptors or pathways involved in gastrointestinal motility regulation. These drugs offer a more targeted and effective approach to symptom management compared to traditional treatments.
Improved Symptom Management: Clinical trials of Gastric Motility Disorder Drug therapies have shown promising results in improving symptoms associated with gastric motility disorders. From reducing bloating and abdominal discomfort to enhancing gastric emptying, these drugs offer hope for individuals struggling with gastrointestinal symptoms.
Benefits of Gastric Motility Disorder Drug Therapy:
Enhanced Treatment Efficacy: Gastric Motility Disorder Drug therapies offer enhanced treatment efficacy compared to conventional approaches. By targeting specific mechanisms involved in gastric dysmotility, these drugs can effectively alleviate symptoms and improve overall gastrointestinal function.
Increased Patient Compliance: The introduction of Gastric Motility Disorder Drug therapies may improve patient compliance with treatment regimens. With the potential for fewer side effects and improved symptom relief, patients are more likely to adhere to their prescribed medication, leading to better long-term outcomes.
Potential for Personalized Medicine: As research in Gastric Motility Disorder Drug therapies continues to advance, there is potential for personalized medicine approaches tailored to individual patient needs. By identifying specific genetic or molecular markers associated with gastric motility disorders, clinicians can prescribe targeted therapies for optimal treatment outcomes.
Get More Insights On This Topic: Gastric Motility Disorder Drug
#Gastric Motility Disorder Drug#Gastrointestinal Health#Digestive Disorders#Pharmacotherapy#Medical Innovation#Symptom Management#Healthcare Advances#Therapeutic Breakthroughs
0 notes
Note
Hello! I've read a few of your fics and loved them and followed your account! Here's something I think you might find interesting for a fic or senerios (warning kinda long? I'm not sure what the normal length for these messages are)
I'm a ill person myself so I enjoy reading sickfics and looking into conditions and whatnot one thing I've looked into is the illnesses irl Akutagawa one thing he was diagnosed with was Gastric Atony that one caught my eye because it is delayed gastric emptying (something I very likely have due to another illnesses) it's heavily implied Akutagawa might have this based on his behavior. Now delayed gastric emptying might not seem like a serious diagnosis at first, but it can cause a plethora of problems ranging from chronic pain and constipation to forming a bezoar or rupturing the stomach
Some information if you want to use this in a fic or senerio
Delayed gastric emptying has a very strict diet to follow which is no insoluble fiber (soluble is fine for most in moderation), no fruit or vegetable skins, low fat or no fat foods (this means avoiding things like redmeat and dairy), no raw fruits or vegetables and following a specific routine like eating smaller more frequent meals and chewing thoroughly
This condition can also make it hard to eat large meals but also messes with hunger/fullness cues so you may overeat and vomit or get severe acid reflux because you couldn't feel the sensation of fullness this also goes for hunger where you have no idea you're hungry
It also causes blood suger fluctuations because If the stomach empties too slowly, nutrients might not be absorbed quickly enough and insulin may start to rise or drop before glucose enters the bloodstream and causes hypoglycemia. Or food when that has been sitting in the stomach finally enters the small intestine, a rapid rise in blood glucose can happen, leading to hyperglycemia.
In severe cases people have to live off of a feeding tube or a full liquid diet because their bodies can no longer process food for some it's short term for others it's long term or permanent
Some people with delayed gastric emptying may alternate between it and something called dumping-symdrome which is...exactly what it sounds like the stomach rapidly dumps food into the intestines which can cause hypoglycemia, palpitations, tremors and can lead to fainting
Treatments include: diet, antiemetics, and gut motility stimulators, strong laxatives (such as enemas and magnesium citrate), antacids, digestive aids (such a probiotics and digestive pills), and staying very hydrated
Causations include: An0rexia, Malnutrition, Connective tissue disorders, Idiopathic, nerve damage, intestinal obstruction, and much more but I'd be here awhile listing causes lol
Anyway i hope you find this helpful or interesting! I have so many more things i want to write about Akutagawas illnesses/potential illnesses and senerios, but I'll save that stuff for a proper post on my acc. Tbh i love your accs sm they make me feel less guilty about my projection on Akutagawa. Cause of that currently, I'm working on a breakdown of potential symptoms he might have because of his canonical childhood and current malnutrition and lung disease. :)
THIS IS AMAZING THANK YOU!! I've actually never heard of this by that name, I'm familiar with it as gastroparesis because it's something I see in the field I work im but this was a very interesting read because I don't know the details of it, and I appreciate you taking the time to talk about it here!!!
I could totally see this for Akutagawa...I love the idea of him having a condition like this but having no clue about it so the symptoms just seem out of nowhere to himself but also people around him, and especially being something uncommon and not something most people would assume based on the various symptoms...he is just Suffering 💔💔
Please tag me in anything you may post regarding his illnesses I'd be very interested to see !!!! 💖💖
#i love getting long asks this is so beautiful#thank you !!!!!!#akutagawa#bungo stray dogs#bungou stray dogs#bsd#illness#ask box#sick#bsd headcanons#emeto#vomiting#medical whump
10 notes
·
View notes
Text
I finally have a diagnosis!
After three long and painful years I finally have a diagnosis as to why my GI tract and abdomen hurt so badly. Why I am unable to eat or drink. Why I have chronic constipation.
For years doctors have been saying it’s all in my head and to see a therapist. (Jokes on them I’ve been seeing one since childhood! Hasn’t changed anything.) They’d give me medication that didn’t help.
Tests kept coming back normal which made me feel more and more crazy.
My mental health fell a part as doctors and medical staff would gaslight me insisting there was nothing wrong with me. Making me constantly question my sanity. Breaking me down little by little.
I finally was refered to one of our state’s research hospitals. They have a clinic that focuses on motility disorders.
My results came back and they say I have Global Slow Transit. Also known as Global Gut Dysmotility.
This means my entire digestive tract is affected. It moves much much slower than it should. This causes food and liquid to get backed up. This is what causes the early satiety, pain, nausea, bloating, and constipation.
They are putting me on Motegrity and Mirtazzapine. I get to get off linzess which I am grateful for since they were a pain to put in a syringe (or more accurately, what I have heard. My caregiver does that). I hear the side affects can be a lot though so I will brace myself and hope for the best!
I am also having appointments with a neuropsychologist and neuro nutritionist. I never even knew the former existed so it will be interesting learning what they have to say.
I desperately needed to talk with a more advanced nutritionist so I am grateful this opportunity arose. I have one provided by my DME, but they were at the end of their knowledge.
I am not tolerating tube feeds well. I only am at 30ml per hour only consuming around 2 cartons of Kate Farms Peptide 1.5 formula per 24 hours. Let’s just say I am malnourished and under weight (again).
Whenever I would try to increase it (or sometimes even it being where it was) I would complain of my intestines feeling engorged and my pain and nausea being off the charts miserable.
(This is where they say the neuropsychologist can help)
So talking about how to best get nutrients and hydration would really help right now. Every doctor has scoffed when I have brought up TPN but I fire back with well if I can’t eat and drink orally, not tolerating tube feeds well, and am underweight and malnourished then….whats the alternative? I hope we can discuss such alternatives at our first appointment. Does anyone have any good alternatives or arguments for or against TPN? I would love advice.
In the end I would love to try a community now that I have a confirmed condition. Is anyone else affected by this condition? How similar and different is this to gastroparesis and intestinal dysmotility? I would love to have other tubie friends. I am lonely. 
#chronically ill#chonic illness#feeding tube#feedingtube#gi pain#gi disorder#diagnosis#finally after all these years#global slow transit#global gut dysmotility#dysmotility#gastroparesis#chronic intestinal dysmotility#I have them all#does anyone else have this problem#looking for friends#tubie friends
18 notes
·
View notes
Text
09.03 placebo effect
Science and Magick

“…the efficacy of magick will depend on the extent to which the act has meaning for the practitioner…”
Placebo Effect
Sourced at https://skygardentarot.com/2020/02/22/magick-and-the-placebo/ and https://www.cbc.ca/natureofthings/episodes/brain-magic-the-power-of-the-placebo
Placebos can have powerful — and real — effects on our mind and body. (A patient experienced relief from the symptoms of a painful medical condition, even though she knew she was taking sugar pills.)
Placebos cause changes in neurobiological signaling pathways and have measurable physiological effects on heart rate, blood pressure (including affecting coronary blood flow and fainting), gastrointestinal tract (including contractions, nausea, motion sickness, bowel motility, functional gastrointestinal disorders, the pulmonary system, especially asthma), immune responses (such as psoriasis, allergic rhinitis, lupus erythematosus).
If we operate from the paradigm that magick is a placebo then by definition the efficacy of magick will depend on the extent to which the act has meaning for the practitioner.
Like what you see? Consider supporting me! ko-fi.com/thatdruidgal
#science and magick#witchy things#grimoire#witchblr#witch stuff#witchcraft#neurodivergent witches#green witch#druidcraft#druidry
7 notes
·
View notes
Note
whats weird about you?
a lot of things lol
i mean mental illness aside, I managed to get put into a body that has really random issues
for example my throat is literally just. Fucked up. I have a esophageal motility disorder only its idiopathic so doctors literally just have no idea what caused it
and then the back of my head is flat
4 notes
·
View notes
Text
Male Infertility in 2025: Causes, Treatments, and Hope for Parenthood

Male infertility is a growing concern worldwide, affecting approximately 40-50% of couples experiencing difficulty in conceiving. In 2025, advancements in medical technology and a better understanding of male reproductive health are providing more solutions for men facing fertility challenges. Understanding the causes, treatments, and the steps you can take to address male infertility can make a huge difference in achieving the dream of parenthood.
In this article, we’ll explore the main causes of male infertility, the most effective treatments available, and lifestyle changes that can improve sperm health. Whether you are starting your fertility journey or considering assisted reproductive treatments, this comprehensive guide will provide you with the essential information you need.
What is Male Infertility?
Male infertility refers to the inability of a man to contribute to conception after at least one year of regular, unprotected intercourse. It is often linked to problems with sperm production, function, or delivery. While male infertility is relatively common, advancements in fertility science have made diagnosing and treating it more accessible.
Causes of Male Infertility
There are several potential causes of male infertility. These causes can be divided into medical, environmental, and lifestyle-related factors.
1. Medical Causes
Several medical conditions can interfere with sperm production, quality, or delivery. Some of the most common causes include:
Varicocele: Enlarged veins within the scrotum can lead to reduced sperm production and poor sperm quality.
Hormonal Imbalances: Imbalances in hormones such as testosterone, follicle-stimulating hormone (FSH), or luteinizing hormone (LH) can affect sperm production.
Infections: Certain infections, including sexually transmitted diseases (STDs), can lead to scarring or blockages that hinder sperm transport.
Ejaculation Disorders: Retrograde ejaculation, where semen enters the bladder instead of being expelled through the penis, can also lead to infertility.
2. Environmental Causes
Exposure to environmental factors can negatively impact sperm health. These factors include:
Radiation or Toxins: Frequent exposure to harmful chemicals or radiation can decrease sperm production and quality.
Overheating the Testicles: Consistent exposure to heat, such as using hot tubs or saunas, may temporarily lower sperm count.
3. Lifestyle-Related Causes
Certain lifestyle habits and behaviors can also influence male fertility. Common contributors include:
Smoking and Alcohol: Both smoking and excessive alcohol consumption are linked to reduced sperm production and poor sperm quality.
Obesity: Being overweight or obese can lead to hormonal imbalances that affect sperm production.
Stress: Chronic stress can interfere with the hormones that regulate sperm production and decrease sexual function.
Signs and Symptoms of Male Infertility
Often, male infertility does not present noticeable symptoms. However, there are some signs that may indicate fertility issues, including:
Difficulty conceiving after a year of trying.
Decreased sexual function, including difficulty with ejaculation or erections.
Pain or swelling in the testicle area.
A lower-than-average sperm count found during testing.
If you experience any of these symptoms or suspect infertility, it's crucial to consult a healthcare provider for a thorough evaluation.
How is Male Infertility Diagnosed?
The diagnosis of male infertility typically involves several steps, including a physical examination, medical history review, and semen analysis. Common diagnostic tests include:
Semen Analysis: A sample of your semen will be evaluated to determine sperm count, motility, and shape.
Blood Tests: Hormone levels, including testosterone, FSH, and LH, are checked to identify hormonal imbalances.
Ultrasound: A scrotal ultrasound may be performed to detect varicocele or other abnormalities.
Genetic Testing: In some cases, genetic tests may be performed to identify hereditary conditions that impact fertility.
Treatment Options for Male Infertility
The treatment for male infertility depends on its underlying cause. Thanks to advancements in reproductive medicine, several treatment options are available.
1. Medication
For men with hormonal imbalances or infections, medications can be prescribed to address these issues. Hormonal therapies can help regulate sperm production, while antibiotics can treat infections affecting fertility.
2. Surgical Procedures
Certain conditions, such as varicocele or blockages in the reproductive tract, can be treated through surgery. Surgical intervention can improve sperm production and allow for natural conception in some cases.
3. Assisted Reproductive Technology (ART)
When other treatments fail, assisted reproductive technology offers several options for couples trying to conceive:
Intrauterine Insemination (IUI): Sperm is collected and inserted directly into the uterus during ovulation, increasing the chances of fertilization.
In Vitro Fertilization (IVF): Sperm is combined with eggs outside the body, and embryos are then transferred to the uterus.
Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected directly into an egg during IVF, which is particularly useful for men with low sperm counts or poor sperm quality.
4. Sperm Donation
If a man is unable to produce viable sperm, sperm donation is another option. This involves using donor sperm to achieve pregnancy via IUI or IVF.
Improving Male Fertility: Lifestyle Changes for 2025
In addition to medical treatments, certain lifestyle changes can improve sperm quality and increase fertility potential.
1. Eat a Balanced Diet
A diet rich in antioxidants, vitamins (especially Vitamin C and E), zinc, and folic acid can boost sperm health. Foods such as nuts, seeds, leafy greens, and lean proteins are excellent choices.
2. Exercise Regularly
Maintaining a healthy weight through regular physical activity can help improve hormone levels and sperm production. However, avoid excessive exercise, as it can have the opposite effect.
3. Avoid Heat and Toxins
Minimize exposure to excessive heat (e.g., hot tubs, tight clothing) and harmful chemicals. Avoid smoking and excessive alcohol consumption, as these can significantly impair sperm health.
4. Manage Stress
Chronic stress negatively impacts hormonal balance and sexual function. Practicing stress-reducing techniques like meditation, yoga, or mindfulness can benefit your overall well-being and fertility.
Male Infertility and Mental Health
Dealing with infertility can take an emotional toll on men. Feelings of inadequacy, anxiety, or depression are common. It’s essential to recognize these emotions and seek support from mental health professionals, fertility counselors, or support groups.
At Yellow Fertility & IVF Center, we not only focus on physical health but also offer resources to support emotional well-being. Navigating fertility challenges can be overwhelming, but you don’t have to go through it alone.
Conclusion
In 2025, male infertility continues to be a significant aspect of fertility challenges faced by couples. However, advancements in medical treatments and lifestyle interventions offer hope. At Yellow Fertility & IVF Center, we are committed to providing the best solutions for men facing infertility, empowering you to take control of your reproductive health and start your journey toward parenthood.
If you or your partner are concerned about male infertility, don’t hesitate to reach out to our experienced team for consultation and guidance. We are here to support you every step of the way.
#yellowivfgurgaon#fertility#ivf#writers on tumblr#ivf success rate#male infertility#male fertility treatments#fertility clinic 2025#male reproductive health#male fertility solutions#fertility awareness#male fertility lifestyle changes#yellow fertility & ivf center
2 notes
·
View notes