#Minimally invasive
Explore tagged Tumblr posts
Text
Sapphire FUE Hair Transplant: A High-Tech and Minimally Invasive Solution to Hair Loss
What is Sapphire FUE Hair Transplantation?
The Sapphire FUE (Follicular Unit Extraction) hair transplant technique is a minimally invasive procedure that involves extracting individual hair follicles from the donor area and implanting them into the recipient area using a specialized tool made of sapphire.
The sapphire FUE method uses a sapphire blade to create small incisions in the scalp, which allows for more precise and controlled implantation of hair follicles. The blade is made of sapphire, which is a high-quality material that is known for its durability and sharpness. This allows for a more efficient and accurate implantation of hair follicles, resulting in a higher success rate.

Advantages of Sapphire FUE Hair Transplantation
Minimal Scarring: The Sapphire FUE method is a minimally invasive procedure that does not require any incisions or stitches. This means that there is minimal scarring, and the recovery time is much faster compared to other hair transplant techniques.
High Success Rate: The sapphire FUE method has a high success rate, with most patients experiencing natural-looking results. The use of a sapphire blade allows for more precise and controlled placement of hair follicles, resulting in a seamless blend between the transplanted hair and the existing hair.
Faster Recovery: The Sapphire FUE method has a faster recovery time compared to other hair transplant techniques. Patients can usually return to their normal activities within a few days of the procedure.
Versatile: The Sapphire FUE method can be used on all hair types, including curly or wavy hair. It is also suitable for individuals with a limited donor area, as the sapphire blade can extract hair follicles from areas that may be difficult to access with other techniques.
Conclusion
The Sapphire FUE method is a high-tech and minimally invasive hair transplant technique that offers many benefits over other hair transplant procedures. It has a high success rate, minimal scarring, and faster recovery time. The use of a sapphire blade allows for more precise and controlled placement of hair follicles, resulting in natural-looking results. If you are considering a hair transplant, the Sapphire FUE method is definitely worth considering.
#Sapphire FUE#Hair transplantation#Hair loss#Hair restoration#Minimally invasive#Natural-looking results#Precise placement#Scalp incisions#Recovery time#Donor area#Curly or wavy hair#Cosmetic surgery
2 notes
·
View notes
Text
Why Choose Laparoscopic Surgery?
Laparoscopic surgery, commonly referred to as minimally invasive surgery, has emerged as a revolutionary approach to treating various medical conditions. Unlike traditional open surgery, laparoscopic procedures are performed through small incisions using specialized instruments and a high-definition camera for precision. This modern surgical technique offers multiple benefits, making it a preferred choice for patients and surgeons alike.

1. High Success Rate Laparoscopic surgeries are known for their high success rates across a variety of medical conditions, including gallbladder removal, hernia repair, appendectomy, and more. The advanced techniques and technologies used ensure that the surgery is precise, with minimal complications.
This high success rate can be attributed to better visualization of internal organs, reduced trauma to surrounding tissues, and the use of state-of-the-art surgical tools. Patients undergoing laparoscopic surgery often report better outcomes and faster recovery times compared to traditional surgeries.
2. Less Discomfort One of the most significant advantages of laparoscopic surgery is the reduced discomfort experienced by patients. Since the procedure involves smaller incisions, there is less tissue damage, resulting in minimal pain during and after surgery.
Patients often experience faster pain relief and require fewer pain medications during their recovery. This reduced discomfort allows patients to return to their normal routines sooner, improving their overall surgical experience.
3. Minimal Blood Loss The precision of laparoscopic techniques ensures minimal damage to surrounding tissues and blood vessels, leading to significantly reduced blood loss during the procedure.
For patients with pre-existing medical conditions, such as anemia or heart disease, this is particularly beneficial. Minimal blood loss not only reduces the need for transfusions but also accelerates recovery and reduces surgical risks.
4. Less Risk of Wound Infection Traditional open surgeries involve larger incisions, which can increase the risk of wound infections. Laparoscopic surgery, on the other hand, uses small incisions, reducing the chances of bacterial contamination and infection.
This minimized risk of infection leads to quicker healing, fewer complications, and improved patient satisfaction. Post-surgical care is also simplified, as patients don’t have to manage large wounds.
5. Faster Recovery and Shorter Hospital Stay Laparoscopic surgery typically results in shorter hospital stays and quicker recovery times. Patients often return home within 24-48 hours of the procedure, as opposed to several days with traditional surgery.
This shorter recovery period not only reduces hospital costs but also allows patients to resume their normal activities and work sooner, making it a more convenient option for modern lifestyles.
Why Choose Dr. Puneet Tyagi? When it comes to laparoscopic surgery, expertise and experience matter. Dr. Puneet Tyagi, a highly skilled general and laparoscopic surgeon with over 10 years of experience, is renowned for his precision and dedication to patient care.
Dr. Puneet Tyagi specializes in a wide range of laparoscopic procedures, ensuring that patients receive the most advanced and effective treatment tailored to their needs. Located at Svasti Care Medical Center, Dehradun, Dr. Tyagi provides compassionate care, state-of-the-art facilities, and successful outcomes.
Benefits of Choosing Svasti Care Medical Center - Advanced Technology: Equipped with modern laparoscopic instruments. - Personalized Care: Focused on patient well-being and comfort. - Experienced Team: Led by a surgeon with over a decade of experience. - Convenient Location: Easily accessible in Dehradun.
Contact Us Phone: 8800884026 | 9997138391 | 9997138392 | 9997138393 Location: Svasti Care Medical Center, 7A, S S Tower, Haridwar Road, Dehradun Website: (http://svasticaremedicalcentre.com)
Take the first step towards better health with laparoscopic surgery. Contact us today to book your appointment or learn more about our services.
1 note
·
View note
Text
Neuralink Rival Sets Brain-Chip Record With 4,096 Electrodes On Human Brain! Precision Expects Its Minimally Invasive Brain Implant To Hit The Market Next Year.
Brain-computer interface company Precision Neuroscience says that it has set a new world record for the number of neuron-tapping electrodes placed on a living human's brain—4,096, surpassing the previous record of 2,048 set last year, according to an announcement from the company on Tuesday.
— Beth Mole | May 28th, 2024

Each of Precision's microelectrode arrays comprises 1,024 electrodes ranging in diameter from 50 to 380 microns, connected to a customized hardware interface.
The high density of electrodes allows neuroscientists to map the activity of neurons at unprecedented resolution, which will ultimately help them to better decode thoughts into intended actions.
Precision, like many of its rivals, has the preliminary goal of using its brain-computer interface (BCI) to restore speech and movement in patients, particularly those who have suffered a stroke or spinal cord injury. But Precision stands out from its competitors due to a notable split from one of the most high-profile BCI companies, Neuralink, owned by controversial billionaire Elon Musk.
Precision was co-founded by neurosurgeon and engineer Ben Rapoport, who was also a co-founder of Neuralink back in 2016. Rapoport later left the company and, in 2021, started rival Precision with three colleagues, two of whom had also been involved with Neuralink.
In a May 3 episode of The Wall Street Journal podcast "The Future of Everything," Rapoport suggested he left Neuralink over safety concerns for the company's more invasive BCI implants.
To move neural interfaces from the world of science to the world of medicine, "safety is paramount," Rapoport said. "For a medical device, safety often implies minimal invasiveness," he added. Rapoport noted that in the early days of BCI development—including the use of the Utah Array—"there was this notion that in order to extract information-rich data from the brain, one needed to penetrate the brain with tiny little needlelike electrodes," he said. "And those have the drawback of doing some amount of brain damage when they're inserted into the brain. I felt that it was possible to extract information-rich data from the brain without damaging the brain." Precision was formed with that philosophy in mind—minimal invasiveness, scalability, and safety, he said.
Neuralink's current BCI device contains 1,024 electrodes across 64 thinner-than-hair wires that are implanted into the brain by a surgical robot. In the first patient to receive an implant, the wires were inserted 3 millimeters to 5 mm into the brain tissue. But, 85 percent of those wires retracted from the patient's brain in the weeks after the surgery, and some of the electrodes were shut off due to the displacement. Neuralink is reportedly planning to implant the wires deeper—8 mm—in its second patient. The Food and Drug Administration has reportedly given the green light for that surgery. The Utah Array, meanwhile, can penetrate up to 1.5 mm into the brain.
Precision's device does not penetrate the brain at all, but sits on top of the brain. The device contains at least one yellow film, said to be a fifth the thickness of a human hair, that contains 1,024 electrodes embedded in a lattice pattern. The device is modular, allowing for multiple films to be added to each device. The films can be slipped onto the brain in a minimally invasive surgery that requires cutting only a thin slit in the skull, which the yellow ribbon-like device can slide through, according to Precision. The film then conforms to the surface of the brain. The processing unit that collects data from the electrodes is designed to sit between the skull and the scalp. If the implant needs to be removed, the film is designed to slide off the brain without causing damage.
In April, a neurosurgery team from the Mount Sinai Health System placed one of Precision's devices containing four electrode-containing films—totaling 4,096 electrodes—onto the brain of a patient who was having surgery to remove a benign brain tumor. While the patient was asleep with their skull opened, Precision researchers used their four electrode arrays to successfully record detailed neuronal activity from an area of approximately 8 square centimeters of the brain.
"This record is a significant step towards a new era," Rapoport said in a press release Tuesday. "The ability to capture cortical information of this magnitude and scale could allow us to understand the brain in a much deeper way."
The test of the implant marks the 14th time Precision has placed its device on a human brain, according to CNBC, which was present for the surgery in New York. Precision says that it expects to have its first device on the commercial market in 2025.
#ARS Technica#Step Forward#Neuralink#Brain 🧠-Chip#Electrodes | Human Brain 🧠#Minimally Invasive#Brain 🧠 | Implant#Brain-Computer | Interface Company | Precision Neuroscience
0 notes
Text
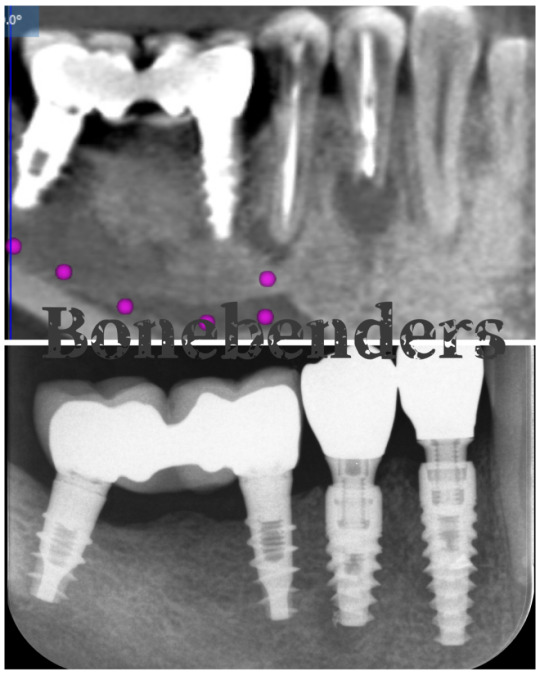
When a tooth is lost, an immediate implant is always the best solution regardless of the bone defect.
Oral surgeons and periodontists doing implants must be careful, but they must be also competent. Ultimately, you must be yourself. I am myself when I give my patients the best possible treatment, in safety. I am myself when I don’t follow the mainstream. I am myself if my treatment is in line with my patient’s expectations and it is also as fast and minimally invasive as possible. It is my…
View On WordPress
#Bonebenders#bonebending#dental implants#flapless surgery#grafts#immediate dental implant#minimally invasive#teeth in a day
0 notes
Text
Navigating the Depths: Understanding Deep Venous Disease
Introduction:
In the intricate network of blood vessels that course through our bodies, the veins play a crucial role in returning blood to the heart. However, not all veins are created equal, and some individuals may find themselves grappling with a condition known as Deep Venous Disease (DVD). This complex medical issue can have profound implications for one's health and well-being, making it imperative to unravel the intricacies of this condition.

Understanding Deep Venous Disease:
Deep Venous Disease, often referred to as deep vein thrombosis (DVT), encompasses a range of conditions that affect the deeper veins within the body. The deep veins, found in the muscles of the legs and pelvis, play a vital role in carrying oxygen-depleted blood back to the heart. When these veins become compromised, it can lead to a host of complications.
Causes and Risk Factors:
Several factors contribute to the development of Deep Venous Disease, and understanding these triggers is paramount for prevention and early intervention. Sedentary lifestyles, prolonged immobility (such as long flights or bed rest), obesity, smoking, and certain medical conditions like cancer or inflammatory disorders can increase the risk of DVD. Additionally, genetic factors and a history of blood clotting disorders may elevate susceptibility.
Symptoms and Detection:
Identifying the symptoms of Deep Venous Disease is crucial for timely intervention. Common signs include swelling in the affected leg, pain or tenderness, warmth, and discoloration of the skin. However, it's important to note that some cases may be asymptomatic, making routine screenings and awareness crucial for early detection.
Diagnostic tools such as ultrasound imaging and venography allow healthcare professionals to visualize blood flow and identify potential clots. Early diagnosis significantly improves the chances of successful treatment and reduces the risk of complications.
Complications of Deep Venous Disease:
Left untreated, Deep Venous Disease can lead to severe complications, the most alarming being the risk of pulmonary embolism. When a blood clot breaks loose and travels to the lungs, it can cause a life-threatening situation. Chronic venous insufficiency, characterized by long-term damage to the veins and impaired blood flow, is another potential consequence. This condition may manifest as leg ulcers, skin changes, and persistent swelling.
Treatment and Management:
The approach to managing Deep Venous Disease is multifaceted, often combining lifestyle modifications, medications, and, in some cases, invasive procedures. Anticoagulant medications, commonly known as blood thinners, are prescribed to prevent the growth of blood clots and reduce the risk of further complications. Compression stockings, designed to improve blood flow in the legs, are a non-invasive option that aids in symptom relief.
For more severe cases, procedures like thrombolysis or thrombectomy may be considered to remove or dissolve clots. In cases where chronic venous insufficiency has developed, interventions such as vein ablation or venous stenting may be recommended to restore normal blood flow.
Prevention:
Preventing Deep Venous Disease involves adopting a proactive approach to mitigate risk factors. Regular exercise, maintaining a healthy weight, avoiding prolonged periods of immobility, and refraining from smoking are key lifestyle choices that can significantly reduce the likelihood of developing DVD. For individuals with a family history of blood clotting disorders, genetic testing and consultation with healthcare professionals can provide valuable insights and guidance.
Conclusion:
Deep Venous Disease is a formidable health challenge that demands our attention and understanding. By recognizing the risk factors, symptoms, and available treatments, individuals can take proactive steps to safeguard their vascular health. Early detection and intervention are crucial, emphasizing the importance of routine screenings for those at higher risk. As we delve deeper into the complexities of Deep Venous Disease, we empower ourselves and our communities to navigate the currents of health with knowledge and resilience.
0 notes
Text
When it comes to addressing varicose veins, there are several types of treatment available. Some people opt for surgery, while others use home remedies. However, there is another option that is becoming increasingly popular: laser treatment. As experts in body treatments in Texas, we will discuss the positive effects of laser spider vein removal:
0 notes
Text
Minimally Invasive Varicose Vein Treatments: Regaining Beautiful, Healthy Legs with Less Disruption
Varicose veins are enlarged, twisted veins that appear just beneath the skin's surface, often on the legs. While they are primarily a cosmetic concern for some, they can also cause pain, swelling, and discomfort. If you're seeking relief from varicose veins, minimally invasive treatments offer a highly effective and less disruptive alternative to traditional surgery.

Unlike traditional vein stripping, which involves larger incisions and longer recovery times, minimally invasive procedures utilize advanced technologies to target and close off malfunctioning veins with minimal tissue disruption.
Common Minimally Invasive Varicose Vein Treatments:
Laser Ablation: A laser fiber inserted into the vein delivers heat energy, sealing the vein shut.
Radiofrequency Ablation(RFA): Radiofrequency waves heat and close the vein from within.
Foam Sclerotherapy: A medicated foam injected into the vein irritates and closes the vessel wall.
Mechanochemical Ablation: A special solution combined with a catheter closes the vein through a chemical reaction.
Benefits of Choosing Minimally Invasive Varicose Vein Treatments:
Less pain and discomfort.
Faster recovery.
Reduced risk of complications.
Minimal or no visible scarring.
Dr. Mohamed Ismail, a renowned laparoscopic and general surgeon in Kerala, India, is also a specialist in minimally invasive varicose vein treatments. With over 35 years of experience and extensive expertise in laparoscopic surgery, Dr. Ismail offers his patients advanced Laser, Radiofrequency, and Sclerotherapy procedures for effective and long-lasting varicose vein removal.
Remember, seeking timely treatment for varicose veins can prevent complications and improve your overall quality of life.
Kindly visit our website to learn more.
0 notes
Text

If you suffer from chronic back pain, look no further than effective kyphoplasty Chicago treatments to alleviate your discomfort. Experience enhanced mobility and improved quality of life with this minimally invasive spinal procedure. Don't endure the pain any longer; book your consultation now!
0 notes
Text
Revolutionizing Knee Health with Robo3DResurfacing.

In the world of medical innovation, few advancements have been as transformative as Robot3D Resurfacing. This cutting-edge knee health machine, employed by the renowned knee surgeon Dr. Bhanu Shaluja, has emerged as a beacon of hope for those seeking relief from knee-related issues. In this blog, we will delve into the remarkable features of Robot3D Resurfacing, including its design, 3D modeling capabilities, and the significant benefits it offers to patients.
The Evolution of Knee Surgery
Knee surgeries have come a long way from their earlier iterations, which often involved extensive incisions, drilling into thigh bones, and lengthy recovery periods. The introduction of minimally invasive techniques was a significant step forward, but Robo3D Resurfacing takes knee health to an entirely new level.
The Power of Design, Size, and Position through 3D Models
At the heart of Robo3D Resurfacing lies the use of advanced 3D modeling technology. The journey begins with a precise 3D scan of the patient’s knee joint. This comprehensive scan allows surgeons to create a highly detailed digital model, enabling them to plan the procedure with unprecedented accuracy.
With this 3D model, surgeons can:
Customize the Procedure: Each patient is unique, and their knees have individual characteristics. Robo3D Resurfacing tailors the surgery to fit the patient’s specific anatomy, ensuring a perfect match for implants.
Visualize the Surgery: The interactive 3D visual interface provides surgeons with a dynamic, real-time view of the entire surgical process. It’s akin to having a GPS guiding them through uncharted terrain, ensuring precision every step of the way.
Faster, Safer, and More Efficient
Robo3D Resurfacing redefines the knee surgery experience in several critical ways:
Swift Surgery: The entire surgical process typically takes only 10–15 minutes, significantly reducing the time spent in the operating room. This minimizes the patient’s exposure to potential risks and complications.
Preservation of Thigh Bone: Unlike traditional knee surgeries, Robo3D Resurfacing eliminates the need to drill into the thigh bone. This preservation of the patient’s natural bone structure can lead to a more comfortable and less invasive procedure.
Rapid Recovery: Patients who undergo Robo3D Resurfacing can often walk within three hours of their surgery. This swift recovery allows for a quicker return to everyday activities, including climbing stairs from the very next day.
Enhanced Comfort: Another notable benefit is the elimination of urinary and drainage pipes post-surgery, contributing to an improved patient experience.
Reduced Risk of Infection
With shorter surgical times and minimized invasiveness, Robo3D Resurfacing significantly reduces the risk of post-operative infections. The streamlined process and precision-guided surgery provide a level of safety that’s unparalleled in traditional knee surgeries.
For more information visit → https://robot3dresurfacing.com/
#revolutionizing knee health#Robot3D Resurfacing#surgical precision#knee surgery#3D modeling#minimally invasive#Dr. Bhanu Shaluja#rapidrecovery#infectioncontro
0 notes
Text
DHI Technique: The High-Tech Solution to Hair Transplantation
Hair loss is a common problem among both men and women, and it can have a significant impact on one's confidence and self-esteem. Over the years, various hair transplant techniques have been developed to address this issue, with the Direct Hair Implantation (DHI) technique being one of the most advanced and high-tech methods available today.

What is DHI Hair Transplantation?
The DHI technique is a minimally invasive hair transplantation procedure involving the direct implantation of individual hair follicles from the donor area to the recipient area. Unlike other hair transplant techniques that involve creating incisions or slits in the scalp, DHI uses a specialized tool called a Choi Implanter Pen to extract and implant hair follicles.
The Choi Implanter Pen has a hollow needle that extracts individual hair follicles from the donor area. These hair follicles are loaded into the pen and implanted directly into the recipient area using a gentle push. This process allows for precise and controlled placement of hair follicles, resulting in a natural-looking hairline.
Advantages of DHI Hair Transplantation
Minimally Invasive: One of the main advantages of the DHI technique is that it is a minimally invasive procedure that does not require any incisions or stitches. This means that there is minimal scarring, and the recovery time is much faster compared to other hair transplant methods.
High Graft Survival Rate: The DHI technique involves the direct implantation of hair follicles, which results in a high graft survival rate. The hair follicles are not exposed to external factors, such as air, which can damage them, leading to a higher success rate.
Natural-looking Results: The DHI technique allows for a precise and controlled placement of hair follicles, resulting in a natural-looking hairline. The implantation of hair follicles in a specific direction and angle helps create a seamless blend between the transplanted hair and the existing hair, giving the appearance of a fuller head of hair.
Fewer Grafts Required: Since the DHI technique allows for precise placement of hair follicles, fewer grafts are required compared to other hair transplant methods. This means that the procedure is quicker, and the recovery time is shorter.
Conclusion
The DHI technique is a high-tech hair transplantation method that offers many benefits over other hair transplant techniques. It is minimally invasive, has a high graft survival rate, and produces natural-looking results. Using the Choi Implanter Pen allows for precise and controlled placement of hair follicles, resulting in a seamless blend between the transplanted hair and the existing hair. If you are considering a hair transplant, the DHI technique is definitely worth considering.
#DHI technique#Hair transplantation#Hair loss#Hair restoration#Choi Implanter Pen#Minimally invasive#Graft survival rate#Natural-looking results#Hairline restoration#Cosmetic surgery
3 notes
·
View notes
Text
Disc Replacement Treatment in Lucknow - Dr Abhinav Srivastava
When it comes to searching for the expertise of a spine health care provider, Dr. Abhinav Srivastava stands out as the best spine surgeon in Lucknow. With a stellar reputation and a music file of excellence, Dr. Srivastava has earned the accept as true with of limitless sufferers looking for remedy from spinal problems.
As the top spine surgeon in Lucknow, Dr. Abhinav Srivastava specializes in a extensive types of spinal treatments, which includes Disc Replacement and spinal twine tumor remedy. His technique is characterized through a commitment to minimally invasive strategies, making processes much less painful and ensuring quicker recuperation instances for his patients.

One of Dr. Srivastava's extremely good strengths is his talent as an endoscopic backbone medical professional. This superior technique permits for precision and accuracy in diagnosing and treating spinal conditions, minimizing the risk related to traditional surgical treatment. Dr. Abhinav Srivastava's determination to affected person care, blended with his significant experience and contemporary competencies, make him the pinnacle choice for those in want of backbone-associated treatment in Lucknow. With Dr. Srivastava, you can rest confident that you're inside the fingers of the best spine surgeon in Lucknow, presenting personalized care and powerful solutions to repair your spinal health.
📆 For more information contact us:
📞 087651 86092
📍 D, 1, Block D, Rajajipuram, Lucknow, Uttar Pradesh 226017
#spine surgeon#spine specialist#endoscopic spine surgeon#Minimally Invasive#Disc Replacement#treatment#lucknow#Spine Surgery#doctor#spine doctor
1 note
·
View note
Text
Lipo on Chin: Sculpting Your Jawline with Confidence
Are you yearning for a jawline that exudes confidence and charisma? The allure of a well-defined jawline is undeniable, and the answer to achieving it might lie in the transformative world of chin liposuction. In this all-encompassing guide, we will embark on a journey into the realm of chin liposuction, unveiling its myriad benefits, delving into the intricate procedure details, and seeking…

View On WordPress
#Aesthetics#Board-certified surgeon#Chin liposuction#Confidence Boost#Cosmetic procedure#expert insights#Facial contouring#Facial rejuvenation#Healthy Lifestyle#Jawline sculpting#Local anesthesia#Minimally invasive#Permanent results#Psychological Impact#recovery process#Self-esteem#Submental liposuction#Surgical alternatives
0 notes
Text
#Aesthetic Enhancements#Anti-Aging#Beauty Treatments#Collagen stimulation#Cosmetic Procedures#Facial contouring#Facial rejuvenation#Minimally Invasive#Non-Surgical Face Lift#Non-surgical facelift#Rejuvenation Techniques#Skin Lifting#Skin tightening#Thread Lifts#Youthful Appearance
0 notes
Text









Memories in Ruins
<previous - next>
#Final Fantasy XIV#FFXIV#Erenville#X'vahl Tia#Erenvahl#WoL x Erenville#wolship#Dawntrail spoilers#7.0 spoilers#I have certain sets that I consider to be sort of... not ''filler'' but like...#mostly just rehashing actual MSQ with minimal changes#but that I consider necessary for pacing#this is one of those#(the next one will also be one of those)#I have the next two already drafted though#so hopefully I can get them both out fairly soonish#I guess this one *does* have some minor character stuff in it by way of X'vahl's trust issues.#after Asahi he's had issues trusting people in certain situations#and since he's already seen her during the whole invasion on Tuliyollal#he's immediately wary of her.
52 notes
·
View notes