#Mild Dengue Symptoms
Explore tagged Tumblr posts
Text
Immediate Treatment For Dengue - Emergency Care in Patna

Is Dengue Contagious? Dengue fever, a viral infection transmitted by mosquitoes, impacts thousands and thousands international, particularly in tropical and subtropical regions.
The onset of dengue can be unexpected and, if no longer dealt with immediately, can motive excessive headaches.
In Patna, wherein Dengue Fever Temperature Pattern may be commonplace, nicely timed medical intervention is crucial. Big Apollo Spectra Hospital, with its modern-day-day emergency services, is fully organized to cope with such times.
This weblog will manual you at the without delay What Is The Fastest Cure For Dengue actions and why travelling an emergency clinic like Big Apollo Spectra can be lifestyles-saving.
Recognizing Dengue Symptoms Early
Early detection plays a critical role in Prevention Of Dengue. Warning Signs Of Dengue Fever embody:
High fever
Severe headache
Pain in the back of the eyes
Joint and muscle ache
Nausea and vomiting
Skin rashes
Mild bleeding (nose or gums)
If you or a loved one display any of those signs and Mild Dengue Symptoms, it is essential to act speedy, as not on time remedy can expand to excessive dengue, causing inner bleeding, organ failure, or perhaps death.
What Is The Immediate Action For Dengue?
While medical remedy is the most crucial step, there are fantastic subjects you may do at home to manage the Dengue Fever Recovery Phase:
Hydration: What Is The First Line Of Treatment For Dengue? One of the number one risks of dengue is dehydration because of fever and vomiting. Drink loads of fluids like water, coconut water, or oral rehydration solutions (ORS). Hydration allows preserve fluid balance and reduces the chance of marvel.
Rest: Dengue can purpose immoderate fatigue, so rest is vital for recovery. Avoid strenuous sports activities to maintain strength.
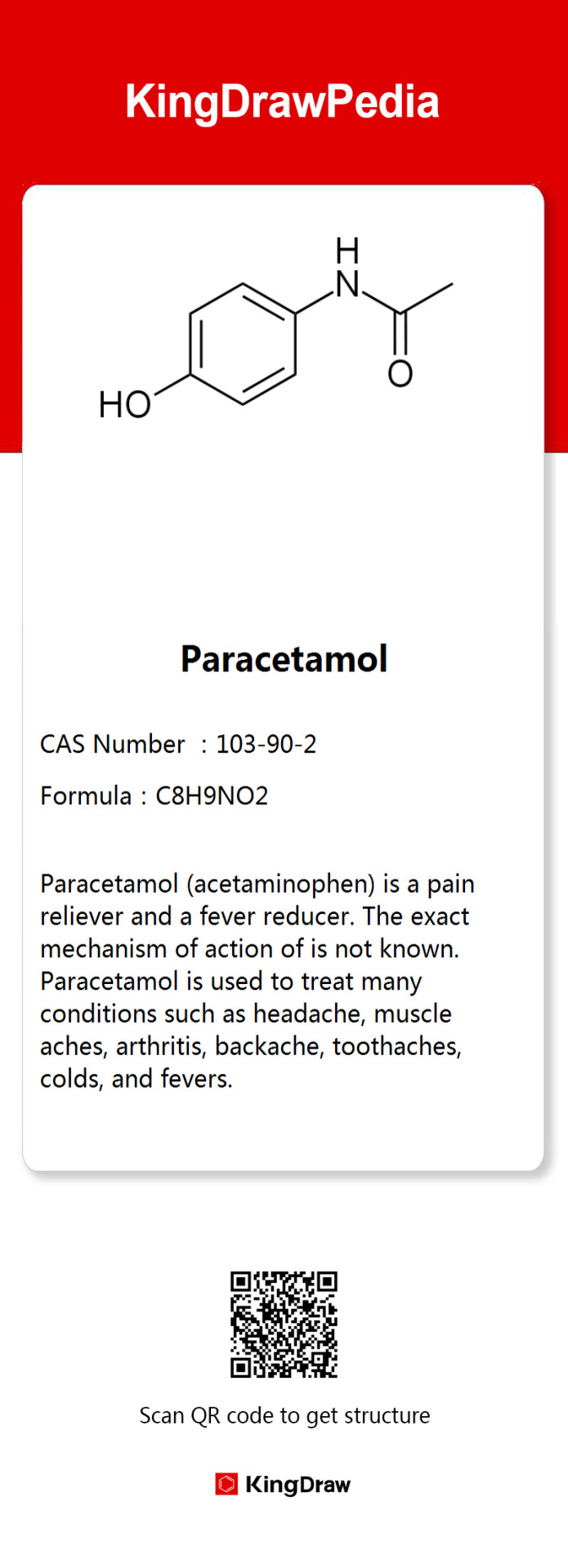
Manage Fever: What Is The First Aid Of Dengue? Nonprescription capsules which includes paracetamol (acetaminophen) can lessen Dengue Fever Medication and alleviate ache. Steer clean of NSAIDs which includes ibuprofen and aspirin, as they could increase the risk of bleeding.
Monitor Symptoms: Keep a near eye at the improvement of signs and symptoms and signs and symptoms. If the fever persists for additional than more than one days or worsens, it's time to looking for Best Emergency Services in Patna for help.
When to Seek Emergency Care in Patna?
Dengue has the potential to progress into a more extreme circumstance referred to as dengue hemorrhagic fever or dengue shock syndrome, each of which may be lethal. Signs that propose a need for emergency hospital treatment include:
Severe stomach ache
Persistent vomiting
Rapid breathing
Fatigue and restlessness
Bleeding gums or nose
Blood in vomit or stool
Cold or clammy pores and skin
Decreased urine output
If any of those signs and symptoms get up, immediate hospitalization is critical.
Big Apollo Spectra Hospital in Patna offers 24/7 emergency care, and its institution of particularly expert doctors and medical personnel can offer the immediate intervention required in intense dengue cases.
Emergency Hospital Treatment for Dengue
Once at the health facility, the remedy for dengue normally specializes in dealing with signs and symptoms, as there's no specific antiviral treatment for the dengue virus. Some of the crucial element medical interventions include:
Intravenous (IV) Fluids: If dehydration is extreme, IV fluids may be administered to repair fluid stability and save you wonder.
Pain Management: Paracetamol may be given to manipulate fever and alleviate pain under strict clinical supervision to keep away from headaches from other medicinal capsules.
Blood Transfusions: In instances of extreme bleeding, blood platelets can be required to replace out of place blood and reduce the threat of hemorrhage.
Close Monitoring: Severe dengue can result in a drop in platelet depend, low blood stress, or fluid accumulation within the lungs. Continuous monitoring of critical signs and symptoms and lab consequences will ensure that complications are speedy addressed.
Preventing Dengue: What You Can Do?
Although a dengue vaccine does not exist, there are numerous preventive movements which can assist lessen the risk of mosquito bites and the transmission of the disease.
Use Mosquito Repellents: Put on repellents with DEET or picaridin on uncovered skin, specifically at some point of peak mosquito pastime instances (early morning and late afternoon).
Wear Protective Clothing: Protective garb inclusive of long-sleeved shirts and pants can help in keeping off mosquito bites.
Use Mosquito Nets: When sound asleep, make certain to use bed nets to defend your self from mosquitoes, especially in areas with a excessive range of mosquitoes.
Remove Standing Water: Mosquitoes reproduce in status water. Frequently inspect and clean out boxes consisting of flower pots, buckets, and birdbaths.
Why Big Apollo Spectra Hospital is best Emergency Care in Patna?
In a dengue emergency, time is of the essence. Big Apollo Spectra Hospital in Patna is renowned for its rapid reaction and expert care in dealing with lifestyles-threatening conditions.
Equipped with superior scientific generation and a team of exceptionally professional specialists, the health center offers round-the-clock emergency services, ensuring that dengue patients get hold of properly timed and suitable remedy. From the moment you arrive, you’ll be within the amazing feasible palms.
Dengue fever can expand fast, making immediate medical interest important. While home care can assist control slight symptoms, it's far critical to are searching for for professional remedy at the earliest signs and symptoms of excessive headaches.
Big Apollo Spectra Hospital in Patna best emergency care hospital near me, imparting expert remedy and take care of dengue and exceptional clinical emergencies. Don't look ahead to the state of affairs to get worse—choose out Big Apollo Spectra for set off and powerful medical interest.
#What Is The Immediate Action For Dengue#What Is The First Line Of Treatment For Dengue#What Is The First Aid Of Dengue#Warning Signs Of Dengue Fever#Dengue Fever Medication#Dengue Fever Temperature Pattern#Mild Dengue Symptoms#Is Dengue Contagious#Dengue Fever Recovery Phase#Prevention Of Dengue
0 notes
Text
Dengue Symptoms
डेंगू सिम्पटम्स: कारण, लक्षण और उपचार (Dengue Symptoms: Causes, Symptoms and Treatment) Dengue Symptoms परिचय डेंगू एक बेहद खतरनाक बीमारी है जो एडीजी संक्रमण मच्छर के काटने से होती है। यह एक वायरल रोग है जिसमें डेंगू वायरस (DENV) संक्रमित व्यक्ति के रक्त में प्रवेश करता है। यह वायरस एक विशेष प्रकार के मच्छर के द्वारा फैलता है, जिन्हें एडीजी मच्छर कहा जाता है। यह मच्छर आमतौर पर दिन में काटते हैं…
View On WordPress
#Dengue#dengue fever rash#dengue fever symptoms#dengue fever treatment#dengue rashes pictures#dengue symptoms#mild dengue symptoms#signs and symptoms of dengue#signs of dengue#signs of dengue fever
0 notes
Text
So disappointed that I misunderstood the doctor. I guess not still officially having Dengue is NOT the same as being over it, so they gave me extra-mega-strength antihistamines (laced with a mild steroid anti-inflammatory) and a cough suppressant for about another week. :(
Now for the whining: Aight, y'all know I have joint injuries, spine injuries, AND both osteo- and rheumatoid arthritis, right? And extra joint pain is a side effect of Dengue AND my heart medication. I'll get over dengue soon, but I'm gonna have to work my ass off to get off the heart meds (thanks, long covid).
And hey, guess what the best way to do the latter is? Yep, exercise. And guess what joint pain and long covid symptoms make harder? You got it! (This is especially galling for a former fitness/martial arts nut who used to run 2 miles in a little over ten minutes and bench pressed 260 lbs despite being only 160 myself. )
Oh, I'll do it, but, y'know...

50 notes
·
View notes
Text
Chemistry behind Dengue

Dengue is a mosquito-borne disease caused by the dengue virus, mainly spread by "Aedes aegypti." Mild cases have a 1% death rate; 80% show no symptoms, while 15% have mild fever, headache, and muscle/joint pain. Avoid NSAIDs like ibuprofen and aspirin, as they can worsen bleeding risks. Seek medical help if bitten by a tiger mosquito and show symptoms like high fever, severe pain, and redness on the skin.


8 notes
·
View notes
Text
//OOC//:
Hello! So uhm, this is gonna be my final post for now because I’m gonna have to take a break from using gadgets.
So in at least 2 of my posts, I mentioned having a fever, well I found out what type of fever I have! I have a type of Dengue fever, but luckily I have a mild dengue fever. I’ve been drinking a LOT of water recently, I went to the hospital last night for a check up, and they injected me so they can get my blood to do tests smth like that.
And yes, I am positive with the fever but I haven’t really had abdominal pain, nosebleeds, and all those other symptoms. I’ve been trying to get a lot of rest but I’ve been having trouble sleeping, so uhm yeah
Anyways I’ll come back once Ive fully recovered, bye !!!
4 notes
·
View notes
Text
Dengue fever infections have skyrocketed as many nations have reported increasingly hot temperatures, which create ideal conditions for the mosquitoes that spread dengue to hatch en masse and carry higher amounts of the virus.
The most common symptom among those who contract the mosquito-borne disease is fever. Other symptoms include serious headaches, nausea, vomiting, rash and body pain.
Symptoms can be mild or severe. Most dengue fever patients recover in a week, but in severe cases the disease can be life-threatening and require hospitalization since it can result in shock, internal bleeding and even death.
4 notes
·
View notes
Text
A record surge in dengue cases throughout Latin America and the Caribbean prompted the head of the Pan American Health Organization to warn of the need for proactive measures to curb the virus that is transmitted by mosquitoes.
PAHO Director Dr. Jarbas Barbosa said in a press briefing Thursday that as of March 26, the region had seen more than 3.5 million cases of dengue and more than 1,000 deaths.
"This is cause for concern, as it represents three times more cases than those reported for the same period in 2023, a record year with more than 4.5 million cases reported in the region,” he said.
As of March, the hardest-hit countries in Latin America are Brazil, Paraguay and Argentina — which have accounted for 92% of the dengue cases and 87% of the deaths — where mosquitoes have thrived because of the warm and rainy weather this time of year.
Barbosa said, however, that they're seeing an uptick in Barbados, Costa Rica, Guadeloupe, Guatemala, Martinique and Mexico, "where transmission is usually higher in the second half of the year.”
U.S. embassies have been issuing health alerts in countries throughout the region, urging people to cover their arms and legs, use mosquito repellent and avoid stagnant water and other mosquito-breeding places.
The U.S. territory of Puerto Rico declared a dengue public health emergency this week, with a surge in cases mostly in the island's capital, San Juan.
According to the Centers for Disease Control and Prevention, “dengue viruses are spread to people through the bite of an infected Aedes species” mosquito, with symptoms that can range from mild to life-threatening for those who get sick from the infection. About 1 in 20 people can get severe dengue, which can lead to death.
The most common symptom is fever, according to the CDC; other symptoms include serious headaches, nausea, vomiting, rash and body pain.
“Facing the dengue problem is a task for all sectors of society,” Barbosa said, urging community engagement.
This includes “efforts to eliminate mosquito breeding sites and protect against mosquito bites, increase preparedness in health services for early diagnosis and timely clinical management, and continuous work to educate the population about dengue symptoms and when to seek prompt medical attention,” according to a PAHO news release.
3 notes
·
View notes
Text
Similarly, for as much flak as the Humor theory gets it is surprisingly sound and when applied correctly rather effective -
Because Humoral theory is based on food.
Yes, it's based on blood. The four humors are, in fact, the components of blood. Phlegm is white blood cells. Cholera or yellow bile is Plasma. Bile, black bile or Melancholera is dead red blood cells and platelets. Blood or Blud is the living red cells.
By filling a clear flask with a person's blood one could see whether they had an excess or deficit of any one, since blood settles in layers. and a specialised diet would be prescribed to help aid them. Conditions of Humor were often indicated by whatever a person's blood had in excess, and so if, for instance, you were particularly Choleric, too much plasma, or your blood is too thin, you would be fed/prescribed a very carb and iron/meat heavy diet, which would restore your apparent anemia. Chronic Anemia, by the way, has a reputation for making people very cranky and unpredictable, hence descriptions of Choleric people being easily flustered and snappy.
Similarly if one had too much Phlegm, white blood cells, it was well understood that you were very sick - phlegmatic people needed a simple, digestible diet so they could get better.
Black bile, also called Melancholera, was associated with depression and sadness, but also delusions, mood swings, and insanity. There are a lot of conditions which cause your red blood cells to die and sink in excess (something now called a sedimentation rate) though there was one extremely common ailment of the European continent for most of its history: Malaria. The four species of malaria in Europe in particular can cause weird mood issues in some people, narcoleptic symptoms in others, and overall makes you feel listless and generically unwell, though the symptoms can be hard to pin down.
Other causes of this increased sedimentation rate can hearken to genetic blood and tissue disorders, Lyme disease in later centuries, tuberculosis (which was and is fairly common) early signs of Plague, now-extinct species of the Dengue virus, and critically rabies.
Various nutritional deficiencies, including scurvy as it would happen, along with vitamin D deficiency, could also cause Melancholera. Because the causes could be so abstract and hard to pin down, Melancholy as it became known was very hard to treat, and became the bane of many a physicians existence. However, it also lead to a very "throw everything at it and hope it works" approach that the Humor method is so infamous for. In spite of that, the usual means of treating melancholy were to prescribe anti malaria medicine (in the form of slippery elm bark if im not mistaken) if it was the right season, and encouraging those afflicted to spend time outside, socialise, and eat a whole lot of rich and spicy food. Fruits preserved in honey, wine, fat or mead don't lose their vitamin C too much, and cider was so popular in the middle ages it wasn't even funny. Cider keeps most it's vitamin C, though admittedly there's not much to begin with. Fish, onion, garlic, and licorice or anise, along with mint and sage and coriander were all strongly pushed. Fish has vitamin D in it, onions and garlic have quite a bit of vitamin C, licorice has mood stabilising effects and aids digestion, as does anise (part of why it was so common to add to wines) mint and sage have a decent amount of Zinc, without which you can not absorb iron or process vitamin D, E, or C, and Coriander (cilantro seeds) has a mild stimulant effect if you chew the raw, whole seeds, which can have a mood boosting effect.
Of course no one using Humoral theory really understood the complexities, but they did understand that the food we eat becomes part of our blood, (which I will get to) which in turn sustains us. So much of humoral theory was centered on the use of food as medicine.
One exceedingly infamous exception, kind of, is an excess of red blood. Too much red blood meant something was going wrong, very wrong, and that it needed to be gotten out of you NOW.
So while dietary prescriptions were definitely implemented, especially in the earlier medieval period, before 1500, it became increasingly common after that point to simply bleed a person. This was sometimes done with Melancholy too, increasingly toward the end of the Renaissance when politics and plague destroyed a good chunk of generational knowledge about how these things worked.
Excess red blood was associated with being excitable, manic, and famously hysteric. Insanity and delusions of its own sort was associated with too much blood, which was otherwise considered a very good thing to have a decent amount of.
However the kinds of conditions which actually cause an excess of red blood cells basically boils down to rare forms of skeletal tuberculosis, bone cancers, and oddly enough poisoning. Poisoning by what, specifically, is not fully understood, though mercury, lead and especially copper poisoning can cause the blood to carry a bit of a different hue. Some plants can cause this effect as well, most tellingly being Evening primrose - a plant that produces nasty anticoagulants and has been used as an aborteficent since Roman times. Little wonder young women up to "trouble" would sometimes go nuts for seemingly no reason - evening primrose is also slightly hallucinogenic. Another plant guilty of similar effects on the blood and mind is a kind of fern known only as "blackroot" - most likely a type of bracken, but no one's entirely sure what species since braken is usually edible. It's been suggested it's not the fern, but a fungus growing around the rhizome of the fern, which bears the name. But we do know it was used as both medicine and to induce abortion, and that it could have troubling side effects like mania and hallucinations. (Sure sounds like a shroom to me).
Point being that ancient people were no less smart or observant than you or I today, they just didnt have access to the kinds of information we do now. Nonetheless they knew what they were doing well enough to say it was no mere accident our species still survives.
And speaking of scurvy, I am eternally amused by the thing where some ancient form of healing that was born in a time where people didn't know exactly how the human body works, or what causes it to stop working sometimes, that still somehow worked. Like how so many old folk medicinal plants were listed as a cure for various ailments that - from a modern view - are clearly just symptoms of scurvy, and the plant itself is rich in vitamin C.
I recall reading some story, no recollection of the exact time or place, where the king of a large empire suffered from constant horrible headaches and was incapable of falling asleep unless drugged or blackout drunk. Sick of taking temporary fixes to dull the pain and having to be sedated every night, he called up some old sage healer who was said to know how to fix things nobody else could explain, and the healer heard his symptoms and went
"Hmm. You spend too much time being a king. Your skull is packed so full of kingly thoughts that they don't all fit in there and that's why your head is in pain. You need to spend time not being a king." And prescribed him to schedule three days every month where he must go to a peasant village where nobody knows he's the king, live with a family there under a fake name and identity, work in the rice fields with them, eating the same food and sleeping on the same mats. Absolutely nobody is allowed to address him as the king, speak to him of any royal or political matters, and he himself is not allowed to think any kingly thoughts or think of himself as the king.
And naturally, this worked. Taking a regular scheduled break from a highly stressful office desk job to completely decompress, paired with physical exercise in the form of hard but simple physical labour, plain and simple food and Just Not Thinking About Your Fucking Job All The Time does help chronic stress, which here was worded as "spending too much time being a king clogs your brain."
Sometimes you do have ghosts in your blood, though I'm not entirely sure whether you should do cocaine about it.
48K notes
·
View notes
Text
Dengue fever, caused by the Dengue virus (DENV), is a mosquito-borne disease affecting millions worldwide. It is transmitted primarily by the Aedes aegypti mosquito and leads to severe complications such as dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS) if not diagnosed and treated promptly. Early detection is critical for effective management and reducing mortality rates, and this is where dengue test kits become invaluable.
In this blog, we will delve into how dengue test kits work, their types, benefits, and their role in managing this potentially life-threatening disease.
Understanding Dengue Fever
Dengue fever manifests with symptoms such as:
High fever
Severe headache
Joint and muscle pain
Skin rash
Nausea and vomiting
In severe cases, it can lead to internal bleeding, low platelet counts, and plasma leakage, making timely diagnosis essential.
What is a Dengue Test Kit?
A dengue test kit is a diagnostic tool used to detect the presence of the Dengue virus or its components in a patient’s blood sample. These kits enable early diagnosis, helping healthcare professionals decide the right course of treatment to prevent complications.
How Does a Dengue Test Kit Work?
Dengue test kits rely on various methods to detect:
Viral Antigens: Proteins from the Dengue virus, such as the NS1 antigen, which appears in the bloodstream early in the infection.
Antibodies: The immune system’s response to the virus, specifically IgM and IgG antibodies.
Common Testing Methods
NS1 Antigen Test
Detects the Dengue virus NS1 antigen in the early stages (1–7 days post-infection).
It provides rapid results, making it ideal for early diagnosis.
2. IgM/IgG Antibody Test
Identifies antibodies produced by the immune system:
IgM: Indicates recent infection (appears 4–5 days after symptoms begin).
IgG: Suggests a past or secondary infection.
3. RT-PCR (Reverse Transcription Polymerase Chain Reaction)
Detects viral RNA with high accuracy.
Usually performed in specialized laboratories.
4. Rapid Dengue Test Kits
Combines NS1 antigen and IgM/IgG antibody detection for a quick and convenient diagnosis.
Steps to Use a Dengue Test Kit
Sample Collection: A small blood sample is collected through a finger prick or venipuncture.
Apply Sample to the Test Device: Add the blood sample to the designated test strip or cartridge area.
Add Reagents (if required): Specific reagents may be included in the kit to trigger the test reaction.
Wait for Results: Most rapid test kits provide results within 15–20 minutes.
Interpret the Results
Positive: Indicates the presence of the virus or antibodies.
Negative: No detectable virus or antibodies, though further testing may be needed if symptoms persist.
Benefits of Using Dengue Test Kits
Early Detection: Rapid kits help diagnose dengue in its early stages, enabling timely treatment.
Convenience: Portable and easy to use, suitable for clinics, hospitals, and remote areas.
Cost-Effective: Affordable options make dengue screening accessible, especially in low-resource settings.
Quick Results: Rapid test kits provide results within minutes, saving valuable time in emergencies.
Accurate Diagnosis: High sensitivity and specificity help differentiate dengue from other febrile illnesses.
Applications of Dengue Test Kits
Hospitals and Clinics: Aid in the immediate diagnosis of suspected dengue cases.
Public Health Campaigns: Used for mass screening in dengue-endemic areas to control outbreaks.
At-Home Testing: Some kits are designed for home use, providing convenience for individuals with mild symptoms.
Epidemiological Studies: Help monitor and track dengue prevalence in a population.
Limitations of Dengue Test Kits
False Negatives: Testing too early or late in the infection cycle may result in undetectable levels of antigens or antibodies.
Cross-Reactivity: Antibodies may cross-react with other flaviviruses like Zika or Yellow Fever, affecting accuracy.
Confirmation Needed: Positive rapid test results often require confirmation through laboratory tests like RT-PCR.
Tips for Accurate Testing
Test Early: Use the NS1 antigen test during the first week of symptoms for accurate detection.
Follow Instructions: Carefully follow the kit’s guidelines to avoid errors.
Seek Professional Advice: Always consult a healthcare provider for interpretation of results and next steps.
Store Kits Properly: Ensure the kit is stored at the recommended temperature to maintain effectiveness.
Why Timely Diagnosis Matters
Early diagnosis of dengue fever:
Prevents severe complications like hemorrhagic fever and shock syndrome.
Enables appropriate medical interventions such as hydration therapy and platelet monitoring.
Reduces the risk of spreading the virus through effective patient isolation.
Conclusion
Dengue test kits are an indispensable tool in the global fight against dengue fever. By providing rapid and reliable results, they empower healthcare professionals and individuals to take prompt action, reducing the disease’s impact.
Whether for clinical use, public health campaigns, or personal monitoring, these kits play a vital role in improving outcomes and saving lives. If you suspect dengue or live in an endemic area, having access to a dengue test kit could make all the difference.
1 note
·
View note
Text
What Should You Know About Dengue Fever? - Schwabe India
Learn everything you need to know about dengue fever, including its symptoms, prevention, and how homeopathy can support recovery and boost immunity during dengue outbreaks.
0 notes
Text
Platelets, also known as thrombocytes, play a vital role in our blood clotting system. A decrease in platelet count, medically termed thrombocytopenia, can lead to various health concerns, including excessive bleeding, slower wound healing, and fatigue. Conditions like dengue and chikungunya are notorious for drastically lowering platelet counts, making effective management crucial. While there are medical interventions, many people are turning to natural remedies like Papgoat Syrup for a safe, effective, and natural way to boost platelet levels.
In this article, we’ll explore the causes of low platelet count, the importance of natural solutions, and how Papgoat Syrup can support platelet recovery, especially during dengue and chikungunya.
Understanding Platelets and Their Importance
Platelets are small, colorless cell fragments in our blood that help form clots and stop bleeding. They are produced in the bone marrow and have an average lifespan of 7–10 days. A healthy platelet count ranges between 150,000 and 450,000 platelets per microliter of blood.
When the count falls below this range, the risk of internal bleeding, bruising, and delayed healing increases. This can occur due to several reasons, such as:
Viral infections like dengue, chikungunya, or Zika virus.
Bone marrow disorders.
Autoimmune diseases like lupus or idiopathic thrombocytopenic purpura (ITP).
Side effects of certain medications or chemotherapy.
For those affected by diseases like dengue and chikungunya, managing platelet count is essential to prevent severe complications.
Symptoms of Low Platelet Count
Some common symptoms of thrombocytopenia include:
Easy bruising or petechiae (small red dots on the skin).
Prolonged bleeding from cuts or injuries.
Frequent nosebleeds or gum bleeding.
Fatigue or generalized weakness.
Blood in urine or stool in severe cases.
Recognizing these symptoms early is crucial for timely intervention.
Why Opt for Natural Solutions?
Conventional medical treatments like platelet transfusions or steroids are effective but may not always be necessary or sustainable for mild to moderate cases. Natural solutions offer an alternative that supports the body’s ability to recover without adverse side effects.
The benefits of natural remedies include:
Fewer side effects.
Supporting overall immune function.
Compatibility with ongoing treatments.
This is where Papgoat Syrup comes into play.
What is Papgoat Syrup?
Papgoat Syrup is a herbal formulation specifically designed to naturally enhance platelet production and support immune health. Its unique combination of ingredients is particularly effective in combating the platelet-depleting effects of illnesses like dengue and chikungunya.
Key Ingredients of Papgoat Syrup
Papaya Leaf Extract: Rich in enzymes like papain and chymopapain, papaya leaves are renowned for their ability to boost platelet count. Studies have shown that they increase the production of thrombocytes and reduce oxidative stress.
Goat Milk Extract: A natural source of bioactive compounds that help improve bone marrow function and platelet production. Goat milk also enhances overall immunity.
Giloy (Tinospora cordifolia): Known as the "Root of Immortality," giloy boosts immunity and combats viral infections. It also has anti-inflammatory and antioxidant properties.
Amla (Indian Gooseberry): A potent source of Vitamin C, amla strengthens the immune system and supports healthy blood production.
How Does Papgoat Syrup Work?
Papgoat Syrup targets multiple aspects of platelet health:
Enhances Bone Marrow Function: Ingredients like goat milk extract support bone marrow, the production site of platelets.
Strengthens Immunity: Its antioxidant-rich components improve overall immune defense, aiding recovery from infections like dengue and chikungunya.
Reduces Inflammation: Inflammatory markers caused by viral infections can hinder platelet production. Giloy and papaya leaf extracts help mitigate these effects.
Boosts Natural Healing: The syrup accelerates recovery by supporting the body’s natural healing mechanisms.
Scientific Evidence Supporting Papgoat Ingredients
Numerous studies validate the efficacy of Papgoat’s key components:
Papaya Leaf Extract: Research published in the Asian Pacific Journal of Tropical Biomedicine found that papaya leaf juice significantly increased platelet count in patients with dengue fever.
Goat Milk Extract: A study in the International Journal of Biological Sciences highlighted goat milk’s role in enhancing immune and bone marrow health.
Giloy: A clinical trial reported in the Journal of Ethnopharmacology demonstrated giloy’s effectiveness in managing viral infections and improving platelet recovery.
These findings underscore the scientific foundation of Papgoat Syrup’s formulation.
How to Use Papgoat Syrup
For optimal results, follow the recommended dosage as prescribed on the packaging or by a healthcare provider. Generally:
Adults: 2 teaspoons twice daily after meals.
Children: 1 teaspoon twice daily after meals.
Always consult a healthcare professional before starting any new supplement, especially if you have underlying medical conditions or are pregnant.
Complementary Lifestyle Changes
While Papgoat Syrup is effective, combining it with healthy lifestyle habits can further enhance platelet recovery:
Stay Hydrated: Drink plenty of fluids to prevent dehydration and improve blood circulation.
Consume Iron-Rich Foods: Include spinach, lentils, and red meat in your diet to support blood production.
Add Vitamin B12 and Folate: Eggs, dairy, and fortified cereals can help improve platelet count.
Avoid Processed Foods: Reduce intake of sugary and processed foods, which can weaken immunity.
Rest and Recovery: Adequate sleep is crucial for the body’s repair processes.
Why Choose Papgoat Syrup?
Papgoat Syrup stands out for its:
Scientifically backed ingredients.
Natural formulation with no known side effects.
Proven effectiveness in managing platelet loss during dengue and chikungunya.
Incorporating it into your recovery plan offers a holistic approach to managing platelet health.
BOTTOM LINE
A healthy platelet count is vital for overall well-being, particularly during illnesses like dengue and chikungunya. Natural remedies like Papgoat Syrup offer a safe, effective, and scientifically backed solution for supporting platelet recovery. Combined with a balanced diet and lifestyle changes, this herbal formulation can play a key role in managing your health naturally.
SarabHerbs® is proud to bring you high-quality, research-driven natural products like Papgoat Syrup, designed to empower your wellness journey. Choose SarabHerbs® for trusted, effective solutions that prioritize your health.
0 notes
Text
Symptoms, Prevention & Treatment of Dengue Fever Explained
Dengue fever, a viral mosquito-borne illness, triggers symptoms like high fever, headache, joint pain, skin rash, and mild bleeding. Learn more here.
0 notes
Text
Dengue Prevention and Treatment: Expert Advice from an MD in Medicine Doctor
Dengue fever, caused by the dengue virus and transmitted by Aedes mosquitoes, poses a significant health threat in tropical and subtropical regions, particularly during the monsoon season. An MD in Medicine doctor emphasizes that awareness and preventive measures are crucial for safeguarding health. Here’s a comprehensive guide:
Understanding Dengue Fever
Dengue fever can range from mild to severe and is characterized by high fever, severe headache, pain behind the eyes, joint and muscle pain, and rash. Severe cases can lead to dengue hemorrhagic fever or dengue shock syndrome, which are life-threatening.
Prevention Strategies
Mosquito Control:
Eliminate Breeding Sites: Aedes mosquitoes breed in stagnant water. Regularly check and remove water from flower pots, old tires, buckets, and any other containers.
Use Insecticides: Apply larvicides to water storage containers and use adulticides as needed to reduce mosquito populations.
Community Awareness: Engage with local health authorities to promote community cleanup drives to remove potential mosquito breeding grounds.
Personal Protection:
Clothing: Wear long-sleeved shirts, long pants, socks, and shoes to reduce skin exposure.
Insect Repellent: Use EPA-registered insect repellents that contain DEET, picaridin, oil of lemon eucalyptus, or IR3535. Reapply as directed, especially after sweating or swimming.
Mosquito Nets: Sleep under a mosquito net, especially if you are in an area with high mosquito activity.
Home Protection:
Screens: Install screens on windows and doors to prevent mosquitoes from entering your home.
Air Conditioning: Use air conditioning when possible, as it helps reduce indoor mosquito populations.
Recognizing Symptoms
Dengue symptoms usually appear 4-10 days after being bitten by an infected mosquito. Key symptoms to monitor include:
High fever (up to 104°F or 40°C)
Severe headache
Pain behind the eyes
Joint and muscle pain
Nausea and vomiting
Skin rash
Early detection and intervention are critical for effective management.
Treatment Options
Currently, there is no specific antiviral treatment for dengue fever. However, the MD Medicine doctor can recommend supportive care, which includes:
Hydration: Staying hydrated is crucial. Drink plenty of fluids such as water, electrolyte solutions, and clear soups to prevent dehydration.
Medications:
Pain Relief: Use acetaminophen (Tylenol) for pain and fever relief. Avoid non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen, as they can increase bleeding risks.
Monitoring: In severe cases, hospitalization may be necessary for monitoring vital signs, platelet counts, and providing intravenous fluids if dehydration occurs.
Avoiding Complications:
Be alert for warning signs of severe dengue, such as persistent vomiting, severe abdominal pain, rapid breathing, bleeding gums, fatigue, and irritability. Seek medical attention immediately if these symptoms appear.
By following preventive measures and recognizing symptoms early, individuals can minimize the risk of dengue fever and ensure timely treatment.
0 notes
Text
Understanding Dengue Fever: Symptoms, Causes, and Prevention

Dengue fever, a virus that mosquitoes spread, has become a big health problem in hot and humid areas. This blog will tell you about the signs, reasons, and ways to avoid dengue fever, so you can know more and stay safe.
What is Dengue Fever?
The dengue virus causes dengue fever. Infected female Aedes mosquitoes Aedes aegypti and Aedes albopictus, spread this virus to humans through bites. The virus has four strains. A person who gets infected with one strain might become immune to it. However, the other strains can still infect them. This raises the chances of severe symptoms.
Symptoms of Dengue Fever
Dengue fever symptoms change based on how severe the infection is. People start to show symptoms 4-10 days after an infected mosquito bites them.
Mild Dengue Fever Symptoms:
high temperature (up to 104°F/40°C)
Bad headaches
Pain behind the eyes
Hurting joints, muscles, and bones
Feeling sick and throwing up
Skin rash showing up 2-5 days after the fever starts
A bit of bleeding (like nosebleeds or gums bleeding)
These signs go away within a week, but for some people, the sickness can get worse.
Severe Dengue Symptoms: Severe dengue also called dengue hemorrhagic fever or dengue shock syndrome, can result in life-threatening issues like plasma leakage fluid buildup, breathing problems heavy bleeding, and organ damage. Severe dengue has these signs:
Intense stomach pain
Non-stop throwing up
Bleeding from the gums or nose
Blood in pee, poop, or vomit
Trouble breathing
Tiredness, unease, or crankiness
Severe dengue might show up after the fever goes away, so it's vital to watch infected people.
Causes of Dengue Fever
The dengue virus infects humans when Aedes mosquitoes with the virus bite them. A mosquito gets the virus when it bites someone who has dengue in their blood. Once a mosquito has the virus, it can pass it to others. Remember, dengue can't spread between people.
You're more likely to get dengue if:
You live in or visit tropical or subtropical areas where dengue is common (like Southeast Asia, Pacific islands, Latin America, and Africa)
You're around infected mosquitoes when they're most active (early morning and late afternoon)
Complications of Dengue Fever
Severe dengue can lead to problems like shock bleeding inside the body, and harm to organs such as the liver and heart. Without treatment severe dengue can kill. You need to get medical help right away if you notice any serious symptoms.
How to Prevent Dengue Fever
No specific cure or shot exists for dengue fever so stopping it from spreading is crucial. Here are some key ways to prevent it:
Don't Let Mosquitoes Bite You:
Put on bug spray with DEET, picaridin, or lemon eucalyptus oil.
Cover up with long sleeves, pants, and socks to shield your skin.
Set up bug nets or screens to keep mosquitoes out of your house.
Get Rid of Mosquito Breeding Grounds:
Dump out and clean any containers that collect water, like flower pots, buckets, and tires where mosquitoes lay eggs.
Switch out the water in outdoor pet bowls and bird baths often.
Keep Up with the News:
Watch out for dengue outbreaks if you travel to or live in areas with high risk. Stay away from places full of mosquitoes when these pests are most active.
Shots in High-Risk Places:
Some countries offer the dengue shot Dengvaxia, but doctors suggest it for people who've already had dengue. If you've never had dengue, this shot isn't for you because it might make dengue worse if you catch it later.
When to See a Doctor
If you have symptoms of dengue fever after a trip to an area where dengue spreads, get medical help right away. Quick diagnosis and proper care can lower the chance of problems.
When to Get Tested for Dengue
If you have symptoms such as high fever, body aches, or bleeding after visiting an area with dengue outbreaks, you should see a doctor. At RML Pathology, our complete testing services will help confirm the diagnosis allowing for quick care and lowering the risk of serious complications.
Dengue fever can be deadly. Quick diagnosis, prevention, and treatment are key to fighting this disease. Keep yourself informed, take steps to prevent it, and get tested at RML Pathology to have the best chance of recovery.
Keep yourself protected and take action in the battle against dengue with cutting-edge diagnostic help from RML Pathology!
Conclusion
Dengue fever is a serious illness that can turn into life-threatening conditions. Knowing its symptoms, causes, and ways to prevent it helps you take steps to protect yourself and your family. Stay alert in places where dengue often occurs, and control mosquitoes to cut down the risk of getting sick.
For people in areas with lots of mosquito’s steady work on prevention and staying informed can help control the spread of dengue fever.
This blog offers a complete guide to dengue fever. It stresses how crucial it is to spot, prevent, and treat this disease. To protect your health from this mosquito-spread illness, it's key to stay in the know and take the right steps.
#Dengue fever symptoms#Causes of dengue#Dengue prevention tips#Dengue testing#Dengue NS1 antigen test#Dengue IgG and IgM tests#Mosquito-borne diseases#Severe dengue complications#Dengue diagnosis#Dengue treatment#Aedes mosquito#RML Pathology dengue test#Dengue outbreak prevention#Early detection dengue#Dengue fever in Lucknow#Best pathology lab Lucknow#Dengue care Lucknow#Health checkup for dengue
1 note
·
View note
Text
Dengue in the UAE

Dengue is a viral infection caused by four variants of the Dengue virus (Dengue-1, Dengue-2, Dengue-3, and Dengue-4). It is transmitted through mosquito bites, primarily by the Aedes Aegypti mosquito and, to a lesser extent, by the Aedes Albopictus species. This disease is common in tropical and subtropical regions and affects between 100 to 400 million people annually, according to the World Health Organization. Symptoms often start with mild fever but can escalate to severe flu-like conditions if left untreated.
Read more : https://www.alshouroukajman.com/dengue-in-the-uae.aspx
0 notes
Text
Monsoon Diseases in Children: Common Diseases & Practical Tips for Prevention and Treatment

The monsoon season brings much-needed relief from the scorching summer heat, but it also ushers in a host of health issues, particularly for children. The combination of increased humidity, stagnant water, and the proliferation of insects creates an environment ripe for various diseases. Understanding the common monsoon diseases and knowing how to prevent and treat them can help keep your children healthy during this time.
COMMON MONSOON DISEASES IN CHILDREN
1. Dengue Fever
Dengue fever is a viral infection transmitted by Aedes mosquitoes, which breed in stagnant water. Children are particularly vulnerable to this disease, which can cause high fever, severe headache, joint and muscle pain, skin rash, and mild bleeding.
Prevention and Treatment:
Prevention: Ensure that there are no stagnant water sources around your home. Use mosquito repellents, sleep under mosquito nets, and wear long-sleeved clothing. Windows and doors should be closed.
Treatment: Dengue has no specific treatment, but supportive care can help. Ensure the child is well-hydrated, and use fever reducers like paracetamol (not aspirin or ibuprofen). Seek immediate medical attention if severe symptoms, like bleeding or persistent vomiting, occur.
2. MALARIA
Malaria, caused by Plasmodium parasites and spread through Anopheles mosquito bites, may present with symptoms such as high fever, chills, sweating, headache, nausea, and vomiting.
Prevention and Treatment:
Prevention: Use mosquito nets, repellents, and insecticide-treated bed nets. Eliminate standing water and ensure proper drainage around the home.
Treatment: Antimalarial medications are prescribed according to the specific type of malaria parasite.
3. TYPHOID FEVER
Typhoid fever is caused by the Salmonella typhi bacteria and is usually spread through food and water that has been contaminated. Symptoms may include a prolonged high fever, weakness, stomach pain, headache, and loss of appetite.
Prevention and Treatment:
Prevention: Ensure clean drinking water, practice good hand hygiene, and avoid street food. Vaccination is also available and effective.
Treatment: The primary treatment for typhoid fever is Antibiotic. Hydration and a nutritious diet aid in recovery. Hospitalization may be needed.
4. CHOLERA
Cholera is a bacterial infection caused by Vibrio cholerae, that spreads through contaminated water and food, often in areas with poor sanitation, and can be life-threatening if not promptly treated.
Prevention and Treatment:
Prevention: Ensure access to clean drinking water, practice good sanitation and hygiene, and avoid raw or undercooked foods.
Treatment: Oral rehydration salts (ORS) and intravenous fluids are crucial to prevent dehydration. In severe cases may be Antibiotics prescribed.
5. LEPTOSPIROSIS
Leptospirosis is an infection caused by Leptospira bacteria that can be caught through exposure to contaminated water or soil. Symptoms include high fever, severe headache, muscle pain, red eyes, and vomiting.
Prevention and Treatment:
Prevention: Avoid wading through or swimming in floodwaters. Ensure proper sanitation and hygiene.
Treatment: Antibiotics are effective in treating leptospirosis. Prompt diagnosis and treatment are essential to prevent complications.
6. GASTROENTERITIS
Gastroenteritis, also known as stomach flu, is an inflammation of the stomach and intestines resulting from viral, bacterial, or parasitic infections. Common symptoms are diarrhea, vomiting, stomach cramps, and fever.
Prevention and Treatment:
Prevention: Maintain good hand hygiene, ensure clean drinking water, and avoid contaminated food. Promote regular handwashing among children.
Treatment: Ensure the child stays hydrated by giving oral rehydration solutions.
PRACTICAL TIPS FOR PREVENTION
Maintain Cleanliness:
Keep your home and surroundings clean and free of stagnant water to prevent mosquito breeding.
Ensure proper waste disposal and drainage.
Promote Good Hygiene:
Teach children to wash their hands regularly with soap and water, especially before eating and after using the toilet.
Ensure they maintain personal hygiene by bathing regularly and wearing clean clothes.
Safe Drinking Water:
Ensure clean and safe drinking water.
Avoid consuming street food and ensure food is cooked and stored properly.
Use Mosquito Protection:
Use mosquito nets, repellents, and insecticide-treated bed nets.
Dress children in long-sleeved clothing and full-length pants to minimize skin exposure.
Vaccination:
Ensure children are up-to-date with their vaccinations, including those for typhoid and other preventable diseases.
Awareness and Education:
Educate children about the importance of hygiene and avoiding contaminated water or food.
Inform them about the dangers of playing in floodwaters or stagnant water.
PRACTICAL TIPS FOR TREATMENT
Hydration:
Ensure children stay hydrated, especially if they are experiencing symptoms like diarrhea or vomiting. Use ORS solutions to prevent dehydration.
Rest and Nutrition:
Encourage rest and provide a nutritious diet to help with recovery.
Steer clear of heavy, greasy, or spicy foods that could worsen symptoms.
Seek Medical Attention:
Do not hesitate to consult a doctor if your child shows symptoms of any monsoon-related illness.
Follow Prescribed Treatment:
Adhere to the treatment regimen prescribed by the doctor, including completing the full course of any antibiotics.
CONCLUSION
The monsoon season, while refreshing, can pose significant health risks for children. By being aware of common monsoon diseases and taking practical steps for prevention and treatment, you can help ensure your child stays healthy during this time. Maintain cleanliness, promote good hygiene, ensure safe drinking water, and use mosquito protection to minimize risks. Always seek medical advice from thebest doctors in Kerala if your child exhibits symptoms of illness, and follow the prescribed treatment plan diligently. With these measures, you can navigate the monsoon season safely and keep your children healthy and happy.
To ensure your child’s well-being during the monsoon season, our paediatric department in are ready to assist. We prioritize your children’s health because they are our future. If your child shows any symptoms of monsoon-related illnesses, don’t hesitate to schedule an appointment with us. We are dedicated to providing the best care and treatment to ensure a swift recovery.
0 notes