#Methadone without prescription
Text
Shout-out to a patient yesterday who must have gotten arrested for something, but is on the safe supply and methadone program and had a cop go pick up his drugs. Real power move to have a cop be your drug gofer 😂😂😂
#winters ramblings#obviously the cop had the patients consent to get his prescription but LMAO one of the other patients saw the cop#and did a double take and was like YOURE on methadone?!? and the cop was like no im picking up for someone who is#which HILARIOUS that patient is now a fav because of how hilarious that is#the opposite of a shoutout to the cops who called today asking if certian patients came here for meds#because they KNOW they cant ask for that info without a warrant#so nice to know if you inforce the law you dont need to worry about FOLLOWING it
0 notes
Text
febuwhump day 28: "you're safe now"
sequel to days 7 & 19 | tw: aftermath of torture, overdose, graphic injury | general audiences
It takes 24 hours to get a full list of possible suspects: anyone in the nearby area who matches Mulder’s rough description, who’s been in prison recently for violence against women or girls. The list is only 13 names long, but that’s still more than the local police can track down and interview in one day, and they’re running out of time.
Scully hasn’t had a vision since the one during the briefing, and she tries not to think about what that means.
It’s 8pm. The police force aren’t willing to send out officers until the morning, even though they have a list of addresses, even though Mulder might be dying, or dead – don’t think about that – and she’s rereading the names again, unable to do much else, when she realises she recognises one of them. It takes her ten minutes of scouring through the casefile before she finds it: one of the first witness interviews, for the first abducted man, before he was found dead, before the FBI got involved.
The man – Marshall Dunn, aged 35, released from prison 5 months ago after serving 2 years for aggravated assault - wasn’t a suspect, hadn’t even been called down to the station. But he’d worked in the same auto repair shop as the first victim. That’s a link.
It’s a hunch. A Mulder-sized one. But it sure beats waiting for another ten hours.
xXx
Less than an hour later, and Skinner’s pulled some strings to get her backup. Ten minutes later, they’re on the road, a ragtag convoy of her sedan and two FBI SUVs, and that’s when she gets another vision.
Mulder isn’t in it.
Instead she watches as the man washes his hands in the sink – his hands, stained red with blood – and pointedly looks up, into the mirror. She looks right into the eyes of Marshall Dunn, and feels her blood run cold as he speaks.
“Come find me. My work’s all done now, anyway.”
The vision fades away, and she pulls off the road, heart pounding so hard that for a moment she worries she’s going to pass out. It takes a minute to even her breathing, and when she raises her head she sees Skinner leaning out the back of one of the SUVs, looking over at her with concern painted across his face. She nods to him, once. Jaw clenched, she forces back tears.
Okay, you bastard. I’m on my way.
xXx
Marshall Dunn is upstairs, in the back bedroom, with an empty bottle of vodka and a pill container that once held prescription methadone. He’s still breathing, shallowly – by the time Scully gets to him, he’s already been put in the recovery position and an ambulance is on its way.
Even though she’s the doctor, and probably has some legal obligation to stay and help, she leaves the room without a word. The house isn’t very big, and it doesn’t take her long to sweep through the few rooms. There’s a bathroom – the bathroom, she recognises the mirror, and the sink is still stained with blood – a kitchen, a front room, but there’s nothing, no sign of Mulder’s presence. She checks the garage last, but even that reveals nothing – there’s no blood, no sign of a struggle, no weapon. It’s not the same room she saw in the visions.
The thought she’s not dared to think creeps into her mind: What if Mulder was never in the house at all?
Then she hears it; a human grunt of pain.
Her heart stops for a moment, relief and shock stopping all higher brain function, before she runs over the corner of the room. There, half-hidden under a tarp, is a trapdoor. It’s locked with a brand new heavy-duty padlock, the implications of which aren’t lost on her.
“Mulder?”
His voice – pained, shaky, but definitely Mulder – replies. “Scully.”
“I’m going to get you out of there.”
No time to find a key. She’ll have to shoot the lock off. It’ll destroy evidence – really, she should wait until someone can photograph it – but right now she doesn’t want to waste any more time. She fumbles with her gun, heart pounding in an echo of the two-beat in her head: Mul-der, Mul-der, Mul-der.
“Mulder, keep talking to me.”
There’s a sound from the other side of the door, one she can’t make out.
“Mulder?”
“Cold,” he whispers.
“I’m coming down there.” She forces her hands steady and takes aim at the lock. “Cover your head.”
The sound of the gun echoes through the garage, and she distantly hears shouts of surprise from upstairs. She should have warned them. Never mind. The trapdoor, now without the padlock, is easy enough to lift. She shines her flashlight into the hole and sees nothing but the floor.
“Mulder?”
No reply. She holsters her gun and drops down.
There’s a crunch as she hits the ground at an angle, her foot twisting awkwardly under her weight, but she grits her teeth through the pain. Raising her flashlight again, she realises that this is it, the place in the visions – the same cold dirt floor, the same breezeblock walls. She turns, orientating herself, and there’s Mulder, hunched in one of the corners, trembling. God.
She limps over to him and crouches by his side, assessing the situation. His shirt is in tatters, torn and cut away from his body, and his chest is covered in bruises and wounds. There are three long, deep cuts across his chest, one of which she recognises as the one she watched him receive. Scully knows they’re infected, too; one in particular is inflamed and still weeping fluid.
Mulder’s hands are pressed into the left side of his stomach, shaking worse than the rest of him; she wraps her fingers around one wrist, and eases it away from his body. Underneath is a mess of blood and torn fabric – he’s tried to stop the bleeding, probably too far gone to realise it wouldn’t help – but she can tell it’s bad. A penetrating abdominal wound, probably with a dirty blade.
Lying her coat on the ground, she eases him down until he’s on his back. He whimpers, eyes opening, and she leans over into his line of sight.
“Hey, it’s me. You’re going to be okay.”
There are tears in his eyes. She’s not sure if they’re from pain or fear or both; either way, she swipes them away with her thumb, trying to soothe.
“It’s okay. It’s okay. I’ve got you.”
Under her hands, she feels his pulse start to calm as his body stops shaking. There’s movement above; she hears Skinner’s voice, shouting for someone to bring the paramedics, but she doesn’t take her eyes off Mulder’s. There’s an emotion in his gaze that she can’t quite label, but it brings a lump to her throat that she swallows down.
“I’ve got you,” she murmurs again, as his eyes start to close. “You’re safe now.”
@today-in-fic
28 notes
·
View notes
Text
against against prescription drug diversion
From browsing PhilPapers, it looks like VERY few medical ethicists or other philosophers have written on the ethics of prescription drug diversion and anti-diversion methods. This is a HUGE gap in the literature.
Even when the topic has come up, it seems to have mainly been to make modest criticisms of excessively burdensome methods of preventing diversion. It does not challenge the assumption that diversion is always bad, and it does not challenge the assumption that preventing diversion should be one of the medical system's major goals when prescribing drugs. I would challenge both of these assumptions. The first is false, and the second is questionable.
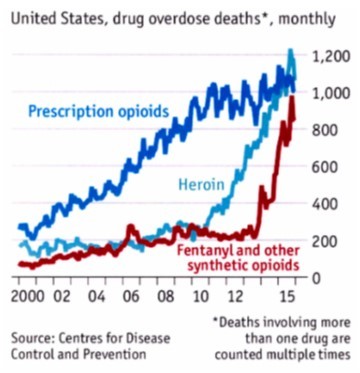
Contrary to mainstream perceptions, I'd argue that prescription drug diversion is sometimes good-- these days, it might even be *usually* good (at least in the US and Canada), although plausibly it was usually bad back in the 2000s. It depends in part on the counterfactuals.
In the 2000s, diversion of pharmaceutical opioids to non-medical drug users was a major part of opioid addiction and overdose (largely through mixing opioids and non-opioids). among people who'd plausibly *otherwise* not be using as many "hard" drugs.
But today, diversion of pharmaceutical grade drugs is a major way that many people (who'd definitely *otherwise* use low-quality street fentanyl) can use something else much less likely to kill them. In fact, some movements now push for policies that can increase how much *good* drug diversion is taking place, as a way to save lives.
Moreover, I'd argue that drug diversion may also sometimes be ethical on other grounds. People may have a property right in the drugs they've been prescribed, and they may have often a right to share these drugs with other people for their own preferred ends, including non-medical use. Poor people may have a moral permission to sell prescribed drugs for money for themselves and their families. People in general may often have a moral permission to share drugs to help their friends.
If diverting drugs is often good or at least morally permissible, then this may weaken the case for anti-diversion priorities, or make it unjust to use some anti-diversion methods.
Anti-diversion methods are often unjust, *even* when aimed at bad forms of diversion. This is because of how they e.g. (1) burden patients, (2) hinder the quality of medical care, (3) damage the doctor-patient relationship e.g. by expressing and creating distrust and resentment, and (4) perpetuate racial and class discrimination (e.g. more scrutiny against black patients, who are seen as more likely to "misuse" or sell their drugs, and who are already subjected to medical discrimination in other overt and subtle ways).
In addition, I also think it is plausible that it is illegitimate for the medical system to value anti-diversion *at all* at least when it puts *any* burden whatsoever on the patient. To value anti-diversion *at all*, when it clashes with patient care (which it obviously does, a lot), might violate the role of medical professionals and undermine the integrity of the medical system.
When anti-diversion is put on the agenda, this constitutes a strange sort of interference by the criminal justice system into the medical system's drug prescription practices. In effect, this gives criminal justice actors such as the DEA the ability to practice medicine without a license. Somewhat similarly, it non-consensually deputizes doctors and their patients into being agents of the drug war, compromising their ability to function as doctor and patient.
The topic of diversion has been indirectly touched on a bit in papers about the ethics of opioid contracts (which include anti-diversion goals), and in a few papers that criticize how coercive the US methadone clinic system is (which is partly driven by anti-diversion concerns), and in a few other places. But, at least on PhilPapers, there seems to be little to nothing challenging the presumed badness of diversion or the presumed legitimacy of anti-diversion goals.
The most in-depth discussion on the ethics of diversion and anti-diversion, by far, is in the drug reform activist literature. The drug user rights podcast Crackdown will soon be doing an episode on diversion and its important relation to safe supply arguments.
These are ethically serious and philosophically interesting issues which seem to have barely, if at all, been discussed in the medical ethics or related literatures by philosophers.
7 notes
·
View notes
Text
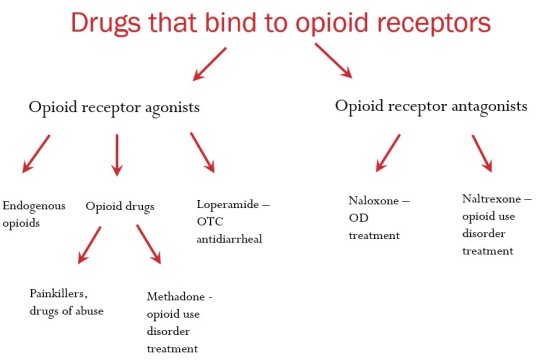
All About: Opioids
- Opioids are substances that act on opioid receptors to produce morphine-like effects.
- Opioids include opiates, an older term that refers to the drugs derived from opium, including morphine.
Opioids = Narcotic Analgesics
- The opioid drugs are narcotic analgesics:
sleep-inducing (narcotic)
pain-relieving (analgesic)
- They are the best painkillers known to humankind, and they also produce a sense of euphoria.
- They create a sense of relaxation, but at high doses, they can lead to coma and death.
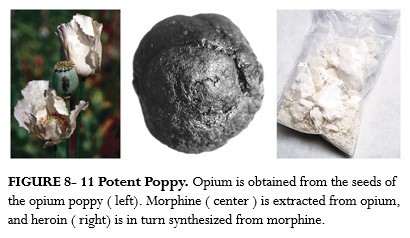
Opium
- Opium has been used recreationally and in medicine for thousands of years (since 5000 BC in China).
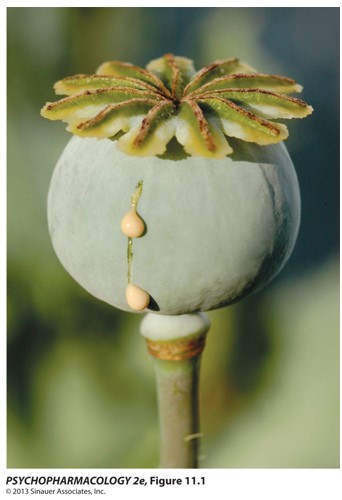
- Opium is an extract of the poppy plant (Papaver somniferum).
- Opium is prepared by drying and powdering the milky juice taken from the seed capsules of the opium poppy just before ripening.
- Opium contains morphine, codeine, thebaine, narcotine, and other ingredients.
- Recreational users often smoke opium for its rapid absorption from the lungs.
Opium-Based Products
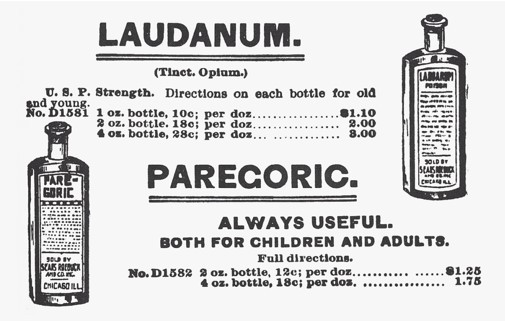
- Laudanum, an opium-based medicinal drink, was introduced to England in 1680.
- Drinking laudanum-laced wine was the accepted form of opium use in Victorian England & USA.
- Up to the 20th century, laudanum was common in popular remedies.
Morphine
- extracted from the poppy plant in 1805 by a German chemist named Friedrich Serturner
- It was the first time an active ingredient of any medicinal plant was isolated.
- Extraction of morphine allowed doctors to prescribe it in known dosages.
- very powerful analgesic and euphoric drug
- named after Morpheus, the Greek god of dreams
Codeine
- isolated in 1832
- less analgesic effect and fewer side effects than morphine
- A potent cough suppressant, it is often included in cough medicine and in pain relievers.
Heroin
- was developed by the Bayer Company in 1874 to be more effective in relieving pain and cough without the danger of addiction.
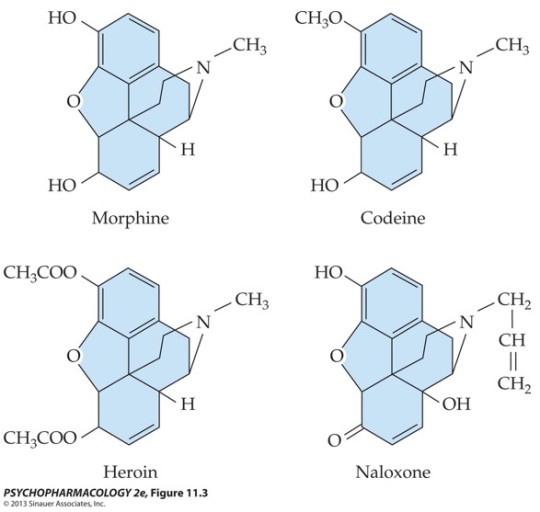
- Heroin was made by adding two acetyl groups to morphine, making it more lipid soluble. The very rapid action of heroin is responsible for the dramatic euphoric effects achieved with that drug.
- as a street drug, preferred over morphine
- pharmacological effects of morphine and heroin are essentially identical because heroin is converted to morphine in the brain.
Oxycodone
- semisynthetic opioid derived from thebaine
- In 1916, German scientists at the University of Frankfurt developed oxycodone as an analgesic less addictive than morphine.
- Oxycodone was approved by the FDA in 1950 as Percodan (mix of oxycodone & aspirin).
- Since the early 1960s, abuse of prescription opioids containing oxycodone has been a major concern in the USA.
- In 1996, Purdue Pharma introduced (and aggressively marketed) OxyContin, a controlled release formulation of oxycodone.
- Purdue advertised Oxycontin as non-addictive because the drug was designed to be released within the body over a 12-hour period.
- Recreational drug users quickly learned to get high by crushing or dissolving these time-release pills.
- Spread of Oxycontin abuse has resulted in increased deaths from overdose.
Molecular structure of morphine, codeine, heroin, and naloxone
Selected natural and synthetic opioid drugs
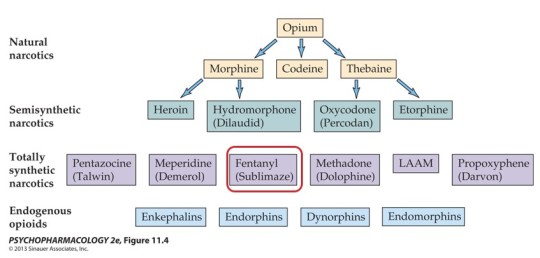
Heroin = Schedule I
Morphine, oxycodone, fentanyl, opium, methadone = Schedule II
Opioids: Routes of Administration
- Recreational users often smoke opium for its rapid absorption from the lungs.
- Morphine:
in hospitals: intravenous, intramuscular, or subcutaneous injection; or given orally
in the streets: inhalation
- Oxycodone, vicodine: taken orally as pills
- “Snorting” heroin leads to rapid absorption through the nasal mucosa. Subcutaneous administration (”skin popping”) may precede the more dangerous “mainlining” (IV injection).
Opioids: Distribution
- Morphine and oxycodone have similar fat-solubility and only a small fraction of the drugs can cross the blood-brain barrier.
- Heroin and fentanyl are much more fat soluble and can reach the brain faster. They are much more potent when injected.
- Opioids easily cross the placenta. Newborns can suffer withdrawal symptoms but can be stabilized with low doses of opioids.
Opioids: Metabolism
- Morphine reaches peak levels with oral administration within 60 minutes; with IV injection, within 15 minutes. The drug has a half-life of about 90 minutes to 3 hours.
- Fentanyl: with IV injection, peaks in 1 minute; half-life of 1.5 hours.
- Oxycodone: oral administration peaks in 30-60 minutes (controlled release 3 hours); half-life is 3-5 hours.
- Oral administration: first-pass metabolism in the liver reduces the bio-availability of opioids.
- Most opioids are metabolized via CYP-mediated oxidation (codeine, oxycodone, methadone) and have substantial drug interaction potential (with the exception of morphine).
Opioids: Excretion
- After metabolism in the liver, most opioid metabolites are excreted in the urine within 24 hours.
- Typically, morphine can be detected in urine for 1-2 days. In cases of heavy or chronic use, morphine might be detectable for slightly longer, but it usually can��t be detected after about 4-5 days.
Pharmacodynamics: Effects of Opioids
- Effects of opioids on the CNS are related to dose and rate of absorption.
- Low to moderate doses result in:
pain relief (analgesia)
relaxation
dreamy sleep
- Some researchers suggest morphine relieves anxiety, aggression, and feelings of inadequacy. This may lead to more drug use.
- At higher doses, there is an abnormal state of elation or euphoria, described as a “kick,” “bang,” or “rush.” This acts as a powerful reinforcer that encourages repeated drug use.
Pharmacodynamics: Side Effects
(A) Behavioral
- drowsiness, inability to concentrate
- (rarely) adverse effects, such as dysphoria, restlessness and anxiety
- At highest doses, the sedative effects may lead to unconsciousness.
(B) Physiological
- constricted pupils
- nausea and vomiting. Opioids affect the area postrema in the brain stem that elicits vomiting.
- constipation: Opium and morphine have been used to treat diarrhea and can be life-saving to stop fluid loss in severe bacterial and parasitic diseases.
Opioid Overdose
- at highest doses = respiratory depression. In recreational users, tolerance to euphoria develops faster than to respiratory depression.
- Opioids act on the brain stem’s respiratory center; respiratory failure is the ultimate cause of death in overdose.
- sedative effects may lead to loss of consciousness.
- body temperature and blood pressure fall
- pupils become very constricted
- antidote = naloxone (Narcan)
Opioid agonists = morphine, oxycodone, fentanyl, etc.
Opioid antagonists = naloxone, naltrexone
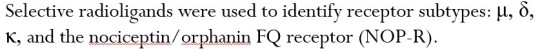
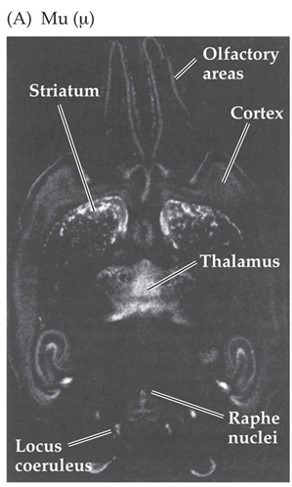
Neurochemical Effects: Receptors and Endogenous Opioids
- Our bodies synthesize our own analgesic substances: endogenous opioids (endorphin, enkephalin, dynorphin)
- Endogenous = produced in our body
- discovered in 1974
- produced in response to pain, but also to exercise, laughter, etc.
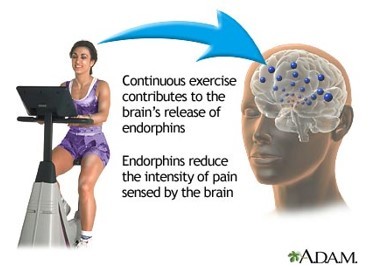
- Both opioid drugs and endogenous opioids produce their effects via endogenous opioid receptors in the CNS.
Analgesia - medial thalamus, periaqueductal gray (PAG), median raphe, spinal cord
Positive reinforcement - nucleus accumbens, VTA
Cardiovascular and respiratory depression, cough control, nausea and vomiting - brainstem
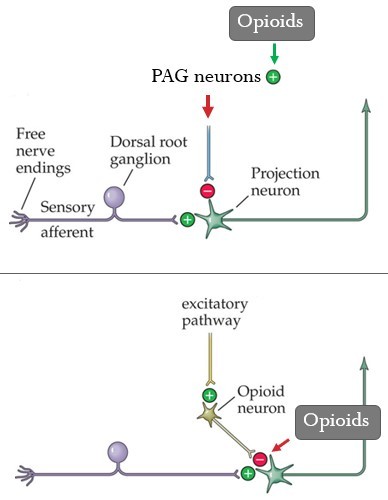
Opioids: Mechanism of Action
- Opioid receptors are metabotropic.
- Opioids inhibit nerve activity in multiple ways:
Postsynaptic inhibition - receptors activate a G protein that opens K+ channels to hyperpolarize the post-synaptic cells, reducing firing rate.
Axoaxonic inhibition - receptors activate G proteins that close Ca2+ channels, reducing the release of neurotransmitter.

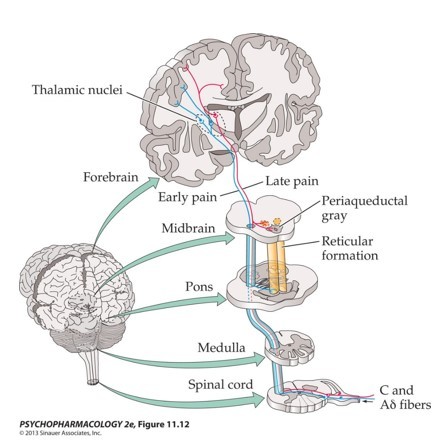
Pain Pathways to the Brain
- How do we feel pain?
- Painful stimuli can be detected by special receptors (nociceptors) located all over our body (including in our skin).
- Sensory information is sent through the spinal cord to the brain, where painful sensation is formed.
- Nociceptors --> Spinal cord --> Thalamus --> Cortex
Pain Management
- Multiple regions in the brain can suppress activity of the pain sensory neurons in the spinal cord.
- PAG (periaqueductal gray) is the key structure.
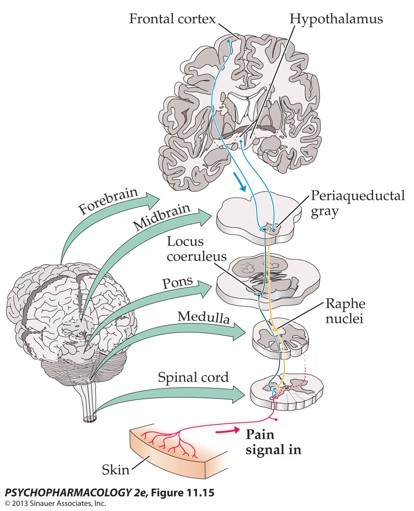
(I) Opioids stimulate neurons in the PAG that are responsible for inhibition of the pain sensory neurons in the spinal cord.
(II) Opioids directly inhibit the pain sensory neurons in the spinal cord.
(III) Opioids also affect higher sensory areas, hypothalamus and limbic structures in the brain.
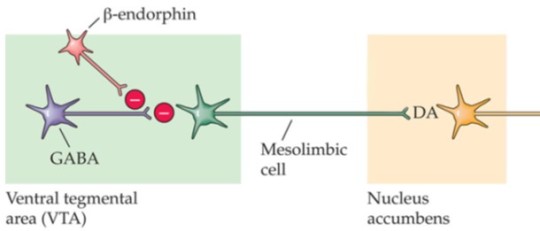
Opioids: Reward Pathway
Reward pathway: mesolimbic: VTA ---> Nacc
- Opioids suppress GABA synapses on VTA dopaminergic neurons
--> Disinhibition --> Increase in firing --> Increase in dopamine release in Nacc
- Experiment: opioids micro-injected into the VTA increase dopaminergic cell firing
- Continued activation of the dopaminergic reward pathway leads to the feelings of euphoria and the ‘high’ associated with opiate use
Chronic Use of Opioids
- Chronic use of opioids leads to neuro-adaptive changes, which are responsible for tolerance, sensitization, and dependence.
- Opioids have significant reinforcing properties.
- Opioids effectively produce tolerance.
- Cross-tolerance among the opioids also exists.
- Example: after chronic heroin use, codeine will elicit a milder-than-normal response even if the individual has never used codeine before.
- Physical dependence: neuro-adaptive state in response to long-term occupation of opioid receptors.
- Physical dependence does not necessarily lead to abuse or addiction.
- When the drug is no longer present, cell function returns to normal and overshoots basal levels. Effects are seen in withdrawal symptoms (abstinence syndrome).
- Opioids in general depress CNS function; opioid withdrawal is rebound hyperactivity.
- Abstinence signs reflect a loss of inhibitory opioid action at all receptors in the CNS and elsewhere, as blood levels of the drug gradually decline.
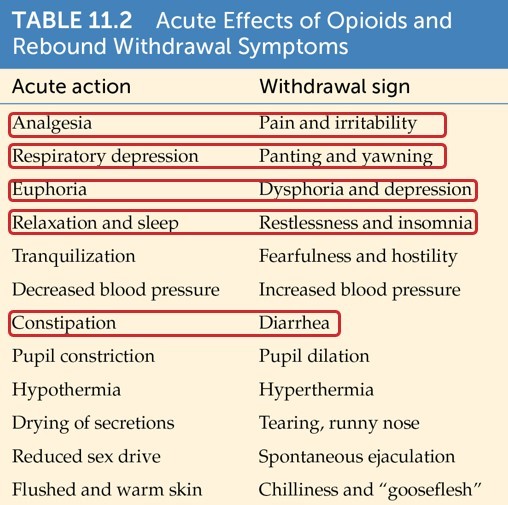
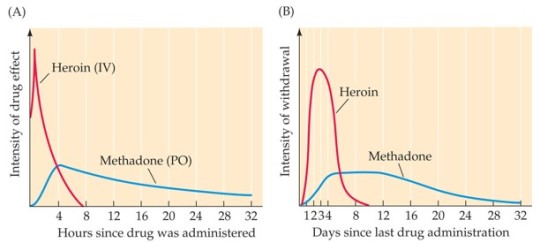
- Severity and time course of withdrawal symptoms can vary with many factors, including the particular drug used:
Heroin: peak within few minutes; withdrawal may begin within 6-24 hours of discontinuation of the drug
Methadone: gradual increase over several days and a gradual decrease over several weeks
- Drug’s time frame can fluctuate with the degree of tolerance as well as the amount of the last consumed dose.
- Withdrawal symptoms can also be classically conditioned.
- The high rate of relapse may be due to the conditioned abstinence syndrome in the old environment.
- Some addicts describe withdrawal symptoms when they visit areas of prior drug use, even years later.
Opioid Addiction
DSM-5: Opioid Use Disorder
- A problematic pattern of opioid use leading to clinically significant impairment or distress, as manifested by at least two of the 11 criteria, occurring within a 12-month period.
Treatment
- A multidimensional approach includes detoxification, pharmacological support, and group or individual counseling.
- Counseling helps addicts identify the environmental cues that trigger relapse and design a behavioral response to those cues.
- Narcotics Anonymous is another option, based on the program for alcohol abuse.
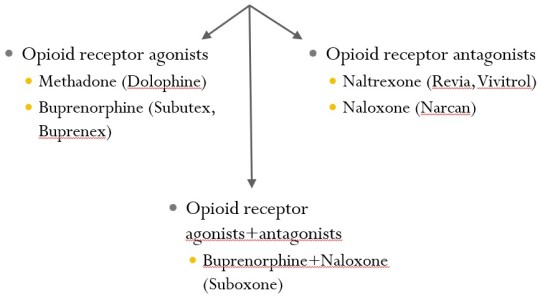
Detoxification is the first step, which can be assisted by opioids such as methadone and buprenorphine (opioid receptor agonists):
substitutes for heroin
reduce symptoms to a comfortable level
Methadone maintenance program:
The most common and effective treatment for heroin addiction. Relieves craving for heroin.
Methadone is long-acting, producing a constant level of drug in the blood.
Methadone has cross-dependence with heroin, which prevents severe withdrawal symptoms.
Methadone can produce a “high” if injected, which could lead to illegal diversion of the drug.
Thus, programs require daily supervised oral administration. Little or no euphoria occurs with oral administration.
Oral administration reduces use of the needle by the addict and the ritual surrounding its use.
- Some treatment programs use narcotic antagonists (= opioid receptor antagonists).
Naltrexone (Trexan) is most commonly used because it has a longer duration of action than naloxone, is effective when taken orally, and has few side effects.
This method is effective for highly motivated individuals. Craving for the drug is not eliminated, so most less-motivated addicts stop antagonist treatment and return to drug use.
Experimental Treatment:
A vaccine is being developed to produce antibodies that would bind to the drug molecules in the blood circulation and prevent entry into the brain.
A vaccine that recognizes heroin and its active metabolites has been tested in rats.
13 notes
·
View notes
Text
Opinion | What Comes Next for the War on Drugs? The Beginning of the End. - The New York Times
There are three bills floating through Congress right now that could not only save lives and money but also help to finally dismantle the nation’s failed war on drugs. The Medicaid Re-entry Act, EQUAL (Eliminating a Quantifiably Unjust Application of the Law) Act and the MAT (Mainstreaming Addiction Treatment) Act all have bipartisan support and could be passed during the lame duck session of Congress. Lawmakers should act on them without delay.
The MAT Act would eliminate the special Drug Enforcement Administration waiver that doctors must apply for in order to prescribe buprenorphine (a medication that helps reduce the craving for opioids). It would enable community health aides to dispense this medication as long as it’s prescribed by a doctor through telemedicine. And it would give the Substance Abuse and Mental Health Services Administration responsibility to start a national campaign to educate health care practitioners about medications for opioid use disorder. Reams of data have shown and addiction specialists agree that these medications offer some of the best options for preventing overdoses and helping people into recovery. But a 2019 report from the National Academies of Sciences, Engineering and Medicine found that fewer than 20 percent of people who could benefit have access to them.
There are several reasons for that, including stigma and a lack of understanding about how medications for opioid use disorder work. The biggest problem is that so few doctors are willing to treat addiction in the first place. Dropping the D.E.A. waiver will not be enough to alleviate that shortage; lawmakers will also have to find ways to ensure that addiction treatment enjoys the same robust reimbursement rates as other chronic conditions. But eliminating the waiver would still be a crucial step in the right direction. The prescription drugs that caused the current epidemic should not be easier to access than the medications that could help alleviate it.
The MAT Act, which was written by Representative Paul Tonko of New York, boasts some 248 co-sponsors and has already passed the House as part of a broader mental health package.
The Medicaid Re-entry Act would allow states to reactivate Medicaid for inmates up to one month before their scheduled release from prison. Those benefits are normally suspended (or in some states terminated) during incarceration because current law prohibits jail and prison inmates from receiving federal health insurance. Reinstating them after incarceration takes time and resources that people who have just been released from jail or prison don’t necessarily have. The resulting disruptions in medical care can be dire: America’s prison population suffers disproportionately from a range of serious ailments, including mental illness, heart disease and opioid use disorder. Among other risks, they are 50 to 150 times as likely to die of an overdose in the first two weeks after their release.
Closing the post-incarceration treatment gap would go a long way toward reducing such deaths. The Rhode Island Department of Corrections reduced its post-incarceration overdose fatalities by 60 percent by ensuring that inmates could access methadone and buprenorphine both during incarceration and after release, without disruption. “It was basically a slam dunk,” says Keith Humphreys, an addiction expert at Stanford University and a former senior adviser to President Barack Obama on drug policy. “Instead of sending them off with a brochure, you connect them to treatment.”
Reinstating Medicaid before release would be another, even more robust way to accomplish the same goal. Several states have already applied for federal waivers that would allow them to do so on a trial basis. The Biden administration should approve those waivers without delay. But Congress should also pass the Medicaid Re-entry Act so that the benefit of seamless care isn’t determined by where an inmate is incarcerated.
The bill, which was also written by Mr. Tonko, has bipartisan backing in both chambers and support from a wide range of groups, including the National Alliance on Mental Illness and the National Sheriffs Association. Experts on addiction believe it could save both lives and money. “It would open up a world of possibilities for taking care of people who are newly released,” Mr. Humphreys says. “There is really no reason not to do it.”
The EQUAL Act would eliminate the federal sentencing disparity between drug offenses involving crack cocaine and powder cocaine. That disparity was created by a 1986 law that equated 50 grams of crack with 5,000 grams of powder cocaine and subjected possession of either to a minimum sentence of 10 years in prison.
The law was based on the now disproved idea that crack cocaine is far more addictive than powder cocaine. It resulted in disproportionately harsher penalties and far more prison time for drug offenders in communities of color: While two-thirds of people who smoke crack are white, 80 percent of people who have been convicted of crack offenses are Black.
In 2010, Congress reduced the crack-to-powder ratio from 100:1 to 18:1. The EQUAL Act would finally eliminate it altogether. If passed, approximately 7,600 people who are serving excessive crack-related sentences could be released an average of six years earlier, according to an estimate from the U.S. Sentencing Commission. That comes out to some 46,500 fewer prison years.
EQUAL, which was written by Representative Hakeem Jeffries of New York, who was recently elected leader of the House Democrats, passed the House last year with overwhelming bipartisan support. We urge the Senate to pass it. Lawmakers should get this long overdue bill across the finish line now, before House investigations and other political battles take priority in the next session.
The nation’s five-decade war on drugs has been a dismal failure. Overdose deaths have reached — and then surpassed — extreme levels in recent years, and the number of people who are still in prison for drug offenses remains stubbornly and egregiously high. Still, it is hard to agree on what comes next. What has been shown to work is not always politically feasible, and what’s politically popular often doesn’t make for sound public health. MAT, EQUAL and the Medicaid Re-entry Acts meet both requirements. Congress should pass all three now.
2 notes
·
View notes
Text
Addressing the Challenges of Opioid Addiction in Lexington, KY
Opioid addiction is a growing concern in many parts of the United States, including Lexington, KY. The widespread availability of prescription opioids, combined with the highly addictive nature of these drugs, has led to a significant increase in opioid dependency. However, there is hope for those struggling with this condition. Opioid addiction in Lexington, KY can be effectively managed with the right treatment and support.
Understanding Opioid Addiction in Lexington, KY
Opioid addiction is a complex condition that affects the brain and behavior, leading to an inability to control the use of opioid drugs. These drugs include prescription medications like oxycodone, hydrocodone, and fentanyl, as well as illegal substances like heroin. The addiction often starts with prescribed painkillers, but over time, it can spiral into a dependency that is difficult to break without professional help.
In Lexington, KY, opioid addiction has become a significant public health issue. Many individuals begin using opioids to manage pain after surgery or injury, but the addictive properties of these drugs can quickly lead to misuse. As the dependency grows, individuals may find themselves engaging in risky behaviors to obtain more drugs, which can lead to serious legal and health consequences.
The Importance of Opioid Addiction Treatment in Lexington, KY
For those struggling with opioid addiction, seeking opioid addiction treatment in Lexington, KY is crucial. Treatment options in the area are designed to address both the physical and psychological aspects of addiction. This comprehensive approach is essential because opioid addiction impacts multiple facets of an individual's life.
Medication-assisted treatment (MAT) is one of the most effective methods for treating opioid addiction. MAT combines FDA-approved medications, such as methadone, buprenorphine, or naltrexone, with counseling and behavioral therapies. These medications help to reduce withdrawal symptoms and cravings, making it easier for individuals to focus on their recovery. When used in conjunction with counseling, MAT can significantly improve the chances of long-term recovery.
In Lexington, KY, opioid addiction treatment centers offer personalized care plans tailored to each individual's needs. This ensures that patients receive the specific treatment required to address their unique circumstances. Whether it's through inpatient rehabilitation, outpatient services, or a combination of both, treatment is designed to provide the tools necessary for lasting recovery.
Overcoming the Stigma of Opioid Addiction
One of the biggest challenges in treating opioid addiction in Lexington, KY is overcoming the stigma associated with the condition. Many individuals struggling with addiction are reluctant to seek help because they fear judgment or discrimination. This stigma can prevent people from accessing the treatment they need, leading to worsening health and increased risk of overdose.
Education and awareness are key to reducing this stigma. By understanding that opioid addiction is a medical condition, not a moral failing, communities can create a more supportive environment for those in need of treatment. In Lexington, KY, there are numerous resources available to educate the public about the realities of addiction and the importance of treatment.
The Role of Family and Community Support
Recovery from opioid addiction is not a journey that individuals should take alone. Family and community support play a vital role in the success of treatment. Loved ones can offer encouragement, help individuals stay accountable, and provide a network of care that extends beyond the treatment center.
In Lexington, KY, various support groups and community programs are available to assist those affected by opioid addiction. These groups offer a safe space to share experiences, learn from others, and gain strength from collective support. Participation in these programs can make a significant difference in the recovery process, helping individuals to maintain their sobriety and rebuild their lives.
Conclusion: Hope for Opioid Addiction Recovery
Opioid addiction treatment in Lexington, KY offers hope to those struggling with this challenging condition. With the right combination of medication, therapy, and support, recovery is possible. It’s essential for individuals facing opioid addiction to seek help as soon as possible to prevent further harm and begin the journey toward a healthier, drug-free life.
By addressing the issue head-on and providing compassionate, evidence-based care, Lexington, KY, is making strides in the fight against opioid addiction. For those battling addiction, reaching out for help is the first and most important step towards recovery.
0 notes
Text
Find Affordable and Reliable Pharmacy Services in Brampton
Looking for a reliable pharmacy in Brampton that offers affordable prescription medications and healthcare supplies? Flowercity Pharmacy is your trusted local pharmacy, providing a wide range of essential services, from prescription refills to home healthcare products. Whether you need to buy prescription medication or order home healthcare supplies, Flowercity Pharmacy makes it easy and convenient.

Convenient Prescription Refills and Medication Purchases
At Flowercity Pharmacy, we simplify the process of managing your health. You can buy prescription medication or quickly get a prescription refill at our pharmacy. We prioritize accuracy, ensuring that all medications are delivered on time and at competitive prices.
Our services also extend to medication for addiction treatment, including options like methadone and buprenorphine, tailored to support recovery. Whether you need these medications or others, our pharmacy guarantees safe and effective service.
Home Healthcare Supplies
If you're searching for home healthcare supplies in Brampton, Flowercity Pharmacy has you covered. From mobility aids to respiratory equipment, we offer a broad selection of products that meet your healthcare needs at home. Our experienced team will assist you in finding the right products to improve your health and comfort.
Affordable and Accessible Healthcare
Flowercity Pharmacy is committed to being a low-cost pharmacy option in Brampton. We ensure that our customers get the best value for essential healthcare services without compromising on quality. Our staff is always available to provide assistance and answer questions regarding medications, making sure you receive personalized and attentive care.
Why Choose Flowercity Pharmacy?
With affordable prices, comprehensive healthcare services, and easy access to prescription medications and home supplies, Flowercity Pharmacy stands out as a top pharmacy in Brampton. We pride ourselves on offering exceptional customer service and meeting the healthcare needs of our local community.
Call to Action
Visit Flowercity Pharmacy today to order your prescriptions or home healthcare supplies. Our knowledgeable staff is here to assist you with all your healthcare needs. Schedule your prescription refill or call us now to get started on your path to better health!
0 notes
Text
Buy Methadone Online from the best online pharmacy in United States of America.
Methadone is an opioid that binds to and activates the opioid receptors in the brain, causing feelings of well-being and euphoria. Methadone should be used as a last resort for treating opioid addiction, and it should only be used in patients under close medical supervision due to its strong potential for abuse and potential for life-threatening respiratory depression.
Use of Methadone
Methadone has been used for many years as a pain medication. Methadone is a synthetic opiate primarily used in the detoxification and maintenance of patients who are dependent on opiates, particularly heroin. It is also used for treatment of patients with chronic, severe pain.
Get Methadone Pills Online on Reasonable Price, Hurry Up

How to Buy Methadone Online
We offer Methadone at a discounted price. Methadone is used to treat addiction to opioids as part of an approved treatment program. It helps prevent withdrawal symptoms caused by stopping other opioids."
Instructions while taking Methadone
Adults—Take this medication at the same time each day, with or without food. Take it as often as your doctor recommends. The dose can be increased each week if needed while you are using methadone consistently and not using any other medications that might make the dose higher. Children—Use and dose must be determined by your doctor.
Before taking Methadone, it is vital to understand its benefits and risks. You should also know about the common side effects associated with this drug. There are certain things that you should do after you consume Methadone as well. You must also be aware of how quickly Methadone wears off and how long it takes for your body to start feeling better after it has been consumed. Some other things related to Methadone are also important to know so that you have a good understanding of how it works in the human body and what happens when it treats a patient suffering from addiction problems
Heart problems
Long QT syndrome
Breathing disorders
Sleep apnea (breathing that stops while sleeping)
Head injuries
Brain tumor
Seizures
Liver disease
Side Effect of Using Methadone
Methadone is a legally prescribed drug that can help reduce cravings and withdrawal symptoms when you take it along with an opioid (narcotic) like heroin or morphine. If you have a prescription, you can get methadone at a pharmacy without a prescription. If you buy methadone online, get it from a trusted seller. Just read reviews to see how the seller does business before agreeing to purchase from them.
What Does Methadone Do?
Methadone is an opioid medicine that you can use to lessen pain caused by an injury, surgery, or other condition. It also may reduce the symptoms of narcotic withdrawal (such as pain and cravings). Methadone changes the way your brain and nervous system respond to pain, so you feel less.
The most common side effects of methadone pills can include:
constipation
nausea
sleepiness
vomiting
tiredness
headache
dizziness
stomach pain
How can you get this Medicine
Go through this Web Link :
Conclusion :
Methadone for sales and Acetaminophen are two of the most-used analgesics worldwide. Methadone and Acetaminophen both possess bioavailability, low cost and short half-life. This combination is effective in the treatment of pain caused by various chronic diseases.
buy methadone online
buy methadone
order methadone online
buy methadone online without prescription
buy methadone online no prescription
buy methadone online without a prescription
buy methadone 10mg online
buy methadone without prescription
methadone for sale online
buy methadone 40mg online
buy methadone pills online
buy methadone no prescription
buy methadone without a prescription
purchase methadone online
buy liquid methadone online
buy methadone overnight
buy dolophine online
methadone online no prescription
order methadone online without prescription
methadone online without prescription
methadone for sale no prescription
buy methadone on the internet
order methadone pills online
buy cheap methadone online
methadone online for sale
#methadone online for sale#order methadone pills online#buy methadone on the internet#methadone for sale no prescription#buy methadone overnight#buy methadone 10mg online#order methadone online#purchase methadone online#ecommerce#economy#commercial#entrepreneur#finance#branding#accounting#business#founder#investing
0 notes
Text
Navigating the Road to Recovery: Comprehensive Approaches to Opiate Addiction Treatment
Opiate addiction, a crisis that has plagued societies worldwide, demands multifaceted and compassionate approaches to treatment. As the opioid epidemic continues to impact millions of lives, the medical community and support networks strive to develop and implement effective strategies to aid those struggling with addiction. Understanding the complexity of opiate addiction and the various treatment options available is crucial for individuals seeking recovery and their loved ones.
Understanding Opiate Addiction
Opiate addiction often begins with the legitimate use of prescription painkillers, such as oxycodone, hydrocodone, or morphine, which can quickly escalate into dependency and misuse. The euphoric effects of these drugs can lead individuals to seek them out illicitly, turning to substances like heroin or fentanyl when prescriptions become inaccessible. The grip of opiate addiction is both physical and psychological, making it a formidable adversary in the battle for sobriety.
Comprehensive Treatment Approaches
Medication-Assisted Treatment (MAT)Medication-Assisted Treatment (MAT) has emerged as a cornerstone in the fight against opiate addiction. MAT combines FDA-approved medications like methadone, buprenorphine, and naltrexone with counseling and behavioral therapies. Methadone and buprenorphine help alleviate withdrawal symptoms and cravings by targeting the same brain receptors as opiates without producing a high. Naltrexone, on the other hand, blocks the effects of opioids altogether. The integration of these medications with therapy addresses both the physical and mental aspects of addiction, improving the chances of long-term recovery.
Behavioral TherapiesBehavioral therapies are essential in addressing the underlying psychological factors contributing to addiction. Cognitive Behavioral Therapy (CBT) helps individuals identify and change destructive thought patterns and behaviors related to substance use. Motivational Interviewing (MI) enhances an individual's motivation to change, fostering a sense of empowerment and commitment to recovery. Additionally, Contingency Management (CM) uses positive reinforcement to encourage sobriety, providing tangible rewards for meeting treatment goals.
Holistic and Complementary TherapiesRecognizing the need for a well-rounded approach, many treatment programs incorporate holistic and complementary therapies. These may include mindfulness meditation, yoga, acupuncture, and art therapy. Such practices help individuals develop healthy coping mechanisms, reduce stress, and promote overall well-being. Holistic therapies are often used in conjunction with traditional treatments to address the physical, emotional, and spiritual aspects of recovery.
Support Groups and Community ResourcesSupport groups play a vital role in the recovery journey. Groups like Narcotics Anonymous (NA) and SMART Recovery offer peer support, providing a sense of community and understanding. Sharing experiences and challenges with others who have faced similar struggles can be immensely therapeutic. Additionally, community resources, including sober living homes and vocational training programs, support individuals as they reintegrate into society, offering stability and purpose.
Challenges and Barriers to Treatment
Despite the availability of effective treatments, many individuals face significant barriers to accessing care. Stigma surrounding addiction can prevent people from seeking help, fearing judgment or discrimination. Moreover, limited access to healthcare, especially in rural or underserved areas, poses a significant challenge. Addressing these barriers requires a concerted effort from policymakers, healthcare providers, and communities to create an environment where seeking help is encouraged and supported.
The Importance of Personalized Treatment Plans
Each individual's journey through addiction and recovery is unique, necessitating personalized treatment plans. A comprehensive assessment by healthcare professionals can determine the most appropriate combination of therapies and interventions. Ongoing evaluation and adjustment of the treatment plan ensure that it continues to meet the individual's evolving needs.
Conclusion
Opiate addiction treatment is a dynamic and evolving field, constantly striving to better meet the needs of those affected by this devastating condition. Through a combination of medication-assisted treatment, behavioral therapies, holistic approaches, and robust support systems, individuals can find a path to recovery. Overcoming opiate addiction is a challenging journey, but with the right support and resources, lasting sobriety is attainable. As society continues to advance in its understanding and treatment of addiction, hope remains the guiding light for all those seeking a new beginning.
0 notes
Text
Comprehensive Guide to Opioid Addiction Treatment in Lexington, KY
Opioid addiction is a significant issue affecting many individuals in Lexington, KY. Effective treatment options are available to help those struggling with addiction. This article provides an in-depth look at opioid addiction treatment in Lexington, KY, highlighting the resources and programs available to support recovery.
Understanding Opioid Addiction
Opioid addiction is characterized by the compulsive use of opioids despite harmful consequences. This addiction can stem from prescription painkillers or illicit drugs like heroin. The physical and psychological dependence on opioids makes quitting challenging without professional help.
Signs of Opioid Addiction
Recognizing the signs of opioid addiction is crucial for early intervention. Common signs include:
Cravings for opioids
Inability to control use
Withdrawal symptoms when not using
Neglect of responsibilities
Social isolation
If you notice these signs in yourself or a loved one, it is essential to seek help immediately.
Treatment Options for Opioid Addiction in Lexington, KY
Lexington, KY offers various opioid addiction treatment options designed to meet the unique needs of individuals. These treatments include:
Medication-Assisted Treatment (MAT)
MAT combines medications like methadone, buprenorphine, or naltrexone with counseling and behavioral therapies. This approach helps reduce withdrawal symptoms and cravings, making it easier to focus on recovery.
Inpatient Rehabilitation
Inpatient rehab provides a structured environment where individuals can receive 24/7 care. This setting is ideal for severe addiction cases requiring intensive support.
Outpatient Programs
Outpatient programs offer flexibility, allowing individuals to receive treatment while maintaining their daily responsibilities. These programs include regular counseling sessions and support group meetings.
Counseling and Therapy
Individual and group counseling sessions are essential components of addiction treatment. Therapy helps individuals address the underlying causes of addiction and develop coping strategies.
Substance Abuse Treatment in Lexington, KY
Substance abuse encompasses the harmful use of various substances, including alcohol and drugs. Lexington, KY, provides comprehensive substance abuse treatment programs designed to help individuals achieve and maintain sobriety.
Types of Substance Abuse Treatment Programs
Residential Treatment: Residential treatment programs offer a home-like environment where individuals receive long-term care and support.
Intensive Outpatient Programs (IOP): IOPs provide a higher level of care than standard outpatient programs, with more frequent counseling and therapy sessions.
Partial Hospitalization Programs (PHP): PHPs offer a structured treatment environment during the day while allowing individuals to return home at night.
Detoxification: Detox programs help individuals safely withdraw from substances under medical supervision.
Benefits of Seeking Professional Treatment
Seeking professional treatment for substance abuse and opioid addiction offers numerous benefits, including:
Medical Support: Access to medical care helps manage withdrawal symptoms and ensures safety.
Psychological Support: Therapy addresses mental health issues and helps develop coping strategies.
Structured Environment: A structured environment reduces the risk of relapse.
Peer Support: Support groups provide encouragement and accountability.
The Role of Family and Community in Recovery
Family and community support play a vital role in the recovery process. Families should be involved in treatment programs and educated about addiction. Community resources and support groups also provide essential support.
Preventing Relapse
Preventing relapse is a critical component of addiction recovery. Strategies to prevent relapse include:
Continuing therapy and counseling
Avoiding triggers
Developing healthy habits
Building a strong support network
Conclusion
Addressing opioid addiction and substance abuse in Lexington, KY, requires a comprehensive approach. Recognizing the signs of addiction and seeking help from reputable treatment centers is essential for recovery. Opioid addiction treatment in Lexington, KY offers various programs to support individuals on their recovery journey. Substance abuse treatment programs in Lexington, KY, provide the necessary resources to help individuals achieve and maintain sobriety. If you or a loved one is struggling with addiction, don't hesitate to seek help. Recovery is possible with the right support, treatment, and commitment.
0 notes
Text
Discover the Difference with 12 Panel Now's Drug Test Cups
At 12 Panel Now, we are committed to providing high-quality, reliable drug testing solutions tailored to meet the needs of both professional and forensic environments. Our range of drug test cups is designed to offer rapid results with accuracy and ease of use. In this blog post, we’ll delve into the features and benefits of our drug test cups, explaining why they are the choice of professionals across the country.
13 Panel Cup – Comprehensive Screening Made Easy
One of our most popular products is the 13 Panel Drug Test Cup. This robust tool is designed to detect a broad spectrum of substances, ensuring comprehensive screening in one simple step. Wondering what a 13 panel drug test checks for? This cup tests for substances including Amphetamines, Opiates, Methamphetamine, Benzodiazepines, Cocaine, Methadone, Oxycodone, Buprenorphine, MDMA, THC, Barbiturates, Tricyclic Antidepressants, and crucially, Fentanyl, which is increasingly important in today’s testing landscape.
Whether you're conducting screenings near or far, the ease of use of our 13 panel urine drug screen makes it a dependable choice. The cup itself is a closed system that reduces the mess and complexity often associated with drug testing. With clear instructions, reading the results is straightforward, enhancing the efficiency of the testing process without the need for extensive training.
Our cups are competitively priced at just $1.99 each, making the 13 Panel Drug Test Cup a cost-effective choice for bulk purchasing. It's perfect for hospitals, rehabilitation centers, and law enforcement agencies looking to buy dependable drug tests in wholesale.
16 Panel Cup – Extended Detection for a Safer Environment
Expanding on our 13 panel model, the 16 Panel Drug Test Cup includes additional tests for Phencyclidine, Ethyl Glucuronide, and Kratom, along with the standard panel. This cup is essential for institutions that require a more extensive screening to maintain a safe and productive environment. The addition of Ethyl Glucuronide allows the cup to detect alcohol consumption, a crucial factor in many testing protocols.
The 16 Panel Cup, priced at $2.69, includes all the features of our other cups, such as easy-to-read results and a no-leak seal, making it ideal for use in high-volume testing scenarios.
16 Panel TRA Cup – Tailored for Comprehensive Insights
Our 16 Panel TRA Cup includes all the substances our standard 16 panel tests for, with the addition of Tramadol, a commonly prescribed pain medication that is not typically included in standard tests. This makes the TRA Cup particularly valuable in environments where a comprehensive analysis of prescription medication usage is necessary.
Like our other products, the 16 Panel TRA Cup is designed for simplicity and accuracy. Priced at $2.39, it offers excellent value for those needing to screen for a wide array of substances, including Fentanyl and alcohol.
18 Panel KET Cup – The Ultimate in Substance Detection
The most comprehensive option in our lineup is the 18 Panel KET Cup. This cup tests for all substances included in our 16 panel cups, plus Ketamine—a drug that is not commonly screened for but can be crucial in certain forensic and clinical settings.
Priced at $2.69, this cup provides unparalleled breadth in drug testing, ensuring that facilities can have the most thorough screening tools at their disposal, complete with fentanyl, alcohol, and now ketamine detection capabilities.
10 Panel Cup FYL – Focused Testing with Critical Insights
For those who need a more focused range of testing while still including critical substances such as Fentanyl, our 10 Panel Cup FYL is an ideal choice. This cup tests for the most commonly abused substances, ensuring that it covers the essentials of drug screening.
The 10 Panel Cup FYL, priced at an affordable $1.59, is particularly suited for quick screenings in settings where the most common drugs of abuse are the primary concern.
Choose 12 Panel Now for Reliable, Efficient Drug Screening
Each of our drug test cups is designed with the user in mind, from the simplicity of obtaining a sample to the clarity of interpreting results. At 12 Panel Now, we are dedicated to providing you with tools that not only meet but exceed the requirements of modern drug testing. Our products are all certified for forensic use, ensuring that they meet the rigorous standards required in professional settings.
Whether you are in the healthcare, law enforcement, or any sector requiring accurate drug screening, our drug test cups provide a reliable, cost-effective solution. Choose 12 Panel Now for your drug testing needs and join countless professionals who trust us to help maintain safety and compliance in their organizations.
0 notes
Text
Methadone Program: The way to treat methadone addiction: Part I
While heroin is its more common opioid cousin, methadone is no less serious of a drug. It’s commonly referred to as “heroin without the high”. And methadone is just as serious as that description makes it sound. Which is why so many people turn to a methadone program when they struggle with methadone addiction. It’s the best way to enter recovery and change a life ravaged by addiction for the better. Here are the facts about methadone and how Florida rehab can help recovery.
What is Methadone?
Methadone is a synthetic opioid medication primarily used to help manage and alleviate withdrawal symptoms in individuals dependent on other opioids, such as heroin or prescription painkillers like oxycodone or morphine. It belongs to the wide family of drugs known as opioids or narcotics.
It works by binding to the same receptors in the brain and body as other opioids, mitigating withdrawal symptoms and reducing cravings without causing the same intense “high” associated with drugs like heroin. Methadone maintenance treatment (MMT) is a common approach in managing opioid addiction, as it helps individuals stabilize their lives and reduces the risks associated with opioid misuse.
When taken as prescribed and under medical supervision, methadone can be effective in reducing opioid cravings and withdrawal symptoms. However, it is a controlled substance with the potential for abuse and addiction if used improperly or in higher doses than prescribed. Regular medical monitoring and adherence to the prescribed dosage are crucial elements of methadone addiction treatment to ensure its safe and effective use. If not, methadone is extremely easy to abuse and become addicted to.
Why is a methadone program necessary: The addictive potential of methadone
Yes, methadone has the potential for addiction and dependence, especially if it is misused or taken in higher doses than prescribed. As an opioid medication, methadone acts on the same brain receptors as other opioids, creating a sense of euphoria and relief from pain. This action can lead to physical dependence and addiction if the drug is used improperly.
Individuals taking methadone for pain management or as part of a treatment program for opioid addiction should strictly follow their prescribed dosage under medical supervision. Abruptly stopping methadone or using it in ways other than directed can lead to withdrawal symptoms and an increased risk of addiction. However, if you begin to develop methadone use disorder, you may need to end your use of methadone.
Medical professionals closely monitor patients on methadone treatment programs to minimize the potential for misuse, manage withdrawal symptoms, and gradually taper off the medication when appropriate. Access to methadone is usually regulated through specialized clinics or healthcare providers to ensure its proper use and reduce the risk of diversion or misuse.
Why is a methadone program with Florida rehab essential: The health consequences of an untreated methadone addiction
A methadone program is essential because methadone addiction can be deadly if left untreated. Methadone addiction can lead to various negative consequences, impacting an individual’s physical health, mental well-being, relationships, and overall quality of life. Some of the negative consequences associated with methadone addiction include:
Physical health effects: Prolonged use or misuse of methadone can lead to numerous health issues, including respiratory problems, constipation, decreased heart rate, lowered blood pressure, increased risk of infections, hormonal imbalances, and potential damage to organs such as the liver.
Tolerance and dependence: Over time, the body can develop tolerance to methadone, requiring higher doses to achieve the same effects. This can lead to dependence, where the individual needs the drug to avoid withdrawal symptoms.
Withdrawal symptoms: Abruptly stopping methadone can cause withdrawal symptoms, which may include anxiety, restlessness, insomnia, muscle aches, nausea, vomiting, diarrhea, sweating, and intense drug cravings.
Impaired cognitive function: Methadone addiction can impact cognitive abilities, leading to problems with attention, memory, decision-making, and overall mental clarity.
Risk of overdose: Misuse or taking high doses of methadone can result in an overdose, characterized by slowed breathing, unconsciousness, and in severe cases, death.
https://ik.imagekit.io/4xricwa81/wp-content/uploads/2023/12/girl-in-vaccination-clinic-2023-11-27-04-50-05-utc.jpg
Other risks of methadone addiction include:
Social and interpersonal consequences: Addiction can strain relationships with family, friends, and colleagues. It may lead to social isolation, financial problems, loss of employment, and legal issues.
Mental health effects: Methadone addiction can exacerbate or lead to mental health disorders such as depression, anxiety, and mood swings.
Decreased quality of life: Overall, methadone addiction can significantly diminish an individual’s quality of life, impairing their ability to function effectively in various aspects of daily life.
Seeking professional help and support from healthcare providers, counselors, or addiction treatment specialists in Florida rehab is crucial for individuals struggling with methadone addiction to address these negative consequences and work toward recovery and rehabilitation.
Next week’s blog on the power of a Methadone program and Florida rehab:
While we’ve already discussed the problems with methadone in this blog, in next week’s blog, we’ll discuss how a methadone program and Florida rehab can change a life for the better.
If you need help from a Methadone program and Florida rehab, contact us and Get Help Now!
In a society where stigma still shrouds neuropsychiatric disorders and addiction, the Neuro-Psychiatric Addiction Clinic is a safe haven. Here, our patients find a wealth of scientific knowledge, cutting-edge treatments, and a compassionate environment where their struggles are met with empathy and understanding. By choosing this clinic, people in need and their loved ones take a decisive step towards embracing a brighter future, one where the rays of hope and healing replace the shadows of addiction and neurological imbalance with a renewed sense of purpose.
Start your journey to wellness today at one of the nation’s leading addiction and mental health treatment facilities. Benefit from recovery in style with great people in a pleasant South Florida location in Port St. Lucie. Call us at (888) 574 3506 or complete the form here. We are available 24/7 to answer any questions regarding our treatment programs.
0 notes
Text
What are the different kinds of pain which can be managed by opioid therapy?
Everyone around us experiences some pain every day. All these patients should receive effective care to eliminate the pain. The main goal of the pain care strategy is to minimize the pain and gain the ability to do daily activities. In this blog, we will learn how different types of pain are managed with opioids.

The kinds of pain managed by opioid therapy
It is important to discuss with your doctor the kind of pain improvement you can expect and continue to follow up with your doctor on your progress. Opioid Agonist Therapy Ontario helps in managing and treating the pain caused in your body with care. Some of the kinds of pains which can be treated pharmacologically are as follows:
Acute pain management: These acute pain include back pain, neck pain, episodic migraines, pain after surgery, muscle strains, etc. Opioid medications are one of the ways to eliminate severe acute pain. It is advisable to talk to your physician about the treatment plan and the benefits and risks of different types of treatment for acute pains.
Chronic pain management: Chronic pain is usually caused by a disease or condition, injury, inflammation, etc. Experiencing this pain for a long period can cause impaired physical functioning, poor mental health, and reduced quality of life which contributes to disability and death every year. It can be managed with both opioids or without opioids. Many non-opioid options have proved to be better with fewer side effects.
What to do if prescribed with opioids for pain management
Some of the tips to follow when prescribed with opioids are as follows:
It is advisable to follow up with the physician regularly within the first few days of starting the prescription ensuring that opioids are helping.
Discuss with them in different intervals about the pain management plan with the Methadone Suboxone Pharmacy Clinic physician.
#Wrappingup
It is important to take control of how to manage your pain and ask the doctor for other alternatives as well.Please listen to your doctor in finding safe and effective care which can help in reach your health goals.
0 notes
Text
0 notes
Text
Types of treatment for addiction disorder and how to choose?

In the realm of addiction disorder, it is essential to understand the nature of the condition and its impact on individuals’ lives. By comprehending addiction and its associated challenges, individuals can better appreciate the significance of seeking professional help and embarking on the journey to recovery.
Addiction disorder is a complex condition that affects millions of people worldwide. When dealing with addiction, seeking proper treatment becomes crucial for achieving long-term recovery and improved quality of life. However, with numerous treatment options available, it can be overwhelming to determine the most suitable approach.
In this article, we will explore the different types of addiction treatment and provide insights on how to make an informed decision.
What is Addiction Disorder?
Addiction disorder, also known as substance use disorder, is a chronic and relapsing condition characterized by compulsive drug or alcohol use despite adverse consequences. It affects the brain’s reward system, leading to intense cravings and a loss of control over substance consumption. Addiction can manifest in various forms, such as substance abuse, gambling addiction, or even behavioral addictions like compulsive gaming or internet usage.
Common Types of Addiction:
Addiction can encompass a wide range of substances and behaviors. Some common types of addiction include:
Alcohol addiction
Opioid addiction
Stimulant addiction (e.g., cocaine, amphetamines)
Marijuana addiction
Prescription drug addiction
Gambling addiction
Internet addiction
Importance of Seeking Treatment:
Seeking treatment for addiction disorder is of utmost importance for several reasons.
Firstly, addiction is a chronic condition that tends to worsen over time without intervention. Delaying treatment can lead to severe health consequences, strained relationships, and financial hardships.
Secondly, professional treatment provides individuals with the necessary tools and support to overcome addiction and establish a healthier, more fulfilling life. Finally, treatment offers a path to recovery and a chance to regain control over one’s life, improving overall well-being.
Types of Treatment Options:
Inpatient Rehabilitation: Inpatient rehabilitation involves a residential treatment program where individuals live at a facility for a specific duration. This intensive form of treatment provides 24/7 medical care, counseling, and structured therapeutic activities. Inpatient rehab is suitable for individuals with severe addiction, co-occurring mental health disorders, or those requiring a controlled and supportive environment.
Outpatient Rehabilitation: Outpatient rehabilitation offers flexibility for individuals to receive treatment while living at home. It involves scheduled therapy sessions, counseling, and support group meetings. Outpatient rehab is ideal for individuals with less severe addictions, strong support systems, and the ability to maintain their daily responsibilities.
Medication-Assisted Treatment: Medication-assisted treatment (MAT) combines medication with therapy to address addiction effectively. Medications like methadone, buprenorphine, or naltrexone help manage withdrawal symptoms and cravings, while therapy focuses on behavioral changes and addressing the root causes of addiction. MAT is commonly used for opioid and alcohol addictions.
Support Groups: Support groups, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), provide a platform for individuals to connect with others who have experienced similar struggles. These groups offer emotional support, accountability, and a sense of community, which can be integral to the recovery process.
Factors to Consider in Choosing Treatment
When selecting the most appropriate treatment option, several factors should be taken into account to ensure the best possible outcome. These factors include:
Individual Needs and Preferences: Each individual has unique needs and preferences when it comes to addiction treatment. Factors such as privacy, treatment philosophy, location, and amenities can influence the decision-making process.
The severity of Addiction: The severity of addiction plays a significant role in determining the level of care required. Severe addictions may necessitate more intensive treatment, such as inpatient rehab, while mild to moderate addictions may be manageable through outpatient programs.
Treatment Effectiveness: It is essential to consider the effectiveness of a particular treatment approach. Researching success rates, testimonials, and evidence-based practices can provide insights into the likelihood of achieving positive outcomes.
Cost and Insurance Coverage: The cost of treatment and insurance coverage are practical considerations. Understanding the financial aspects and exploring available insurance benefits can help individuals plan for treatment without undue financial burden.
Making an Informed Decision:
To make an informed decision about addiction treatment, it is advisable to follow a systematic approach:
Researching Treatment Facilities: Conduct thorough research on various treatment facilities, their treatment approaches, success rates, and reputation. Read reviews, visit their websites, and gather as much information as possible to assess their suitability.
Consulting with Professionals: Seek advice from addiction treatment professionals or healthcare providers who can offer personalized guidance based on an individual’s unique circumstances. They can provide insights into suitable treatment options and help navigate the complexities of the healthcare system.
What is a Faith-Based Program?
A faith-based program, also known as a religious or spiritual program, is a type of addiction treatment program that incorporates religious or spiritual principles and practices as a central part of the recovery process. These programs integrate religious beliefs, values, and teachings into the treatment approach.
Key features of faith-based programs include:
Spiritual Guidance: Faith-based programs often provide spiritual guidance through religious leaders or counselors who incorporate religious teachings, prayer, meditation, and scripture study into the recovery process. These programs emphasize the importance of connecting with a higher power or engaging in spiritual practices to find strength and support during the journey of recovery.
Religious Teachings and Values: Faith-based programs draw on the principles, teachings, and values of a particular religion or faith tradition. They may include regular religious services, religious education classes, or discussions centered around religious texts to help individuals deepen their understanding of their faith and its application to overcoming addiction.
Community Support: Faith-based programs often foster a sense of community and support among individuals who share the same religious or spiritual beliefs. They may encourage involvement in religious congregations, support groups, or fellowship activities where individuals can find encouragement, accountability, and peer support.
Integration of Faith and Recovery: Faith-based programs emphasize the integration of religious or spiritual beliefs and practices with the recovery process. They view addiction as a spiritual problem and approach recovery as a holistic journey that addresses the physical, emotional, and spiritual aspects of an individual’s life.
Moral and Ethical Guidance: Faith-based programs often provide moral and ethical guidance based on the religious teachings of the particular faith tradition. They may focus on principles such as forgiveness, compassion, honesty, and personal responsibility to guide individuals toward healthier behaviors and meaningful life free from addiction.
If your loved one is abusing dangerous drugs, consulting with a family therapist can help the family system heal. Contact a drug and addiction treatment facilities without risk and discuss your recovery alternatives
Continue reading: Types of treatment for addiction
0 notes
