#Jan Urbas
Explore tagged Tumblr posts
Text
2023 IIHF Worlds Slovenia Roster
Wingers
#8 Žiga Jeglič (Fischtown Pinguins/Kranj)
#12 Nik Simšič (H.K. Olimpija/Ljubljana)
#19 Žiga Pance (H.K. Olimpija/Ljubljana)
#21 Jan Drozg (K.K. Amur/Maribor)
#45 Luka Maver (Pioneers Vorarlberg/Ljubljana)
#55 Robert Sabolič (E.C. I.D.M. Wärmepumpen V.S.V./Jesenice)
#81 Tadej Čimžar (H.K. Olimpija/Kranj)
#88 Miha Zajc (H.K. Olimpija/Ljubljana)
#92 Anže Kuralt (Hydro Fehérvár A.V.19/Kranj)
#98 Blaž Tomaževič (E.C. I.D.M. Wärmepumpen V.S.V./Jesenice)
Centers
#18 Ken Ograjenšek (Graz 99ers/Celje)
#24 Rok Tičar (Klagenfurt S.S./Jesenice)
#26 Jan Urbas (Fischtown Pinguins/Jesenice)
#91 Miha Verlič (Fischtown Pinguins/Maribor)
Defensemen
#4 Aleksandar Magovac (H.K. Olimpija/Jesenice)
#6 Miha Štebih (Nice Hockey Côte d'Azur/Maribor)
#14 Matic Podlipnik (Fischtown Pinguins/Jesenice)
#15 Blaž Gregorc (Augsburger Panther/Jesenice)
#17 Žiga Pavlin (C.D.H. Pustertal Wölfe/Kranj)
#44 Aljoša Crnovič (H.K. Olimpija/Jesenice)
#76 Kristjan Čepon (H.K. Olimpija/Ljubljana)
#96 Bine Mašič (Urheilu/Kranj)
Goalies
#32 Gašper Krošelj (B.K. Mladá Boleslav/Ljubljana)
#33 Žan Us (H.K. Olimpija/Ljubljana)
#35 Luka Gračnar (E.V. Landshut/Jesenice)
#Sports#Hockey#Hockey Goalies#National Teams#Slovenia#Celebrities#France#Germany#Italy#Austria#Russia#Czech Republic#Hungary#Finland
0 notes
Text

Long-term injured Captain or equipment manager?
Jan Urbas can do both!
5 notes
·
View notes
Note
This is probably a very stupid question, but how did the Ancient Greeks measure time (in terms of years and months) ? What was their calendar like? What year would Alexander have viewed himself to be living in?
I love these sorts of daily-life details, so I may have got a little carried away…. Before I get into the weeds, however, I want to make everyone aware of a reference resource:
E. J. Bickerman, Chronology of the Ancient World. Thames & Hudson, 1968.
Yeah, it’s old now, but Bickerman spent most of his career on dating puzzles, and I don’t think there’s anything recent to match it. When I first was told about it years ago in my historiography class, I practically bounced off the walls. (My fellow grad students thought I’d lost my mind.)
I’m not sure of the best way to address this query—topically or geographically—but I’ll go with topically. I’ll also say upfront that I’m unfamiliar with Egypt, so they’re not much mentioned. Also, if you want more details on any particular system (Roman, Athenian, Babylonian, Jewish), there are plenty of online resources.

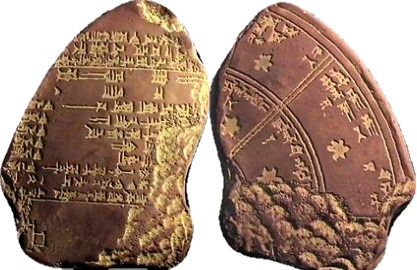
Long-count Calendar
How to number years across a span? Regnal years was most common in antiquity: year 1, year 2, year 3 of ___ king. Also, king lists detailed how long ___ ruled. The Ancient Near East (ANE) excelled at chronologies; we have some that go back to Sumer. That’s pre-Bronze Age. The span of some reigns can be deeply problematic (e.g., mythical), but we have the lists. Fun note, Neo-Assyrians named years by its major military campaign. Tells us a lot about them, no?
What about places without kings? Greece, Rome, Carthage?
The Greeks had several systems, internal and panhellenic. Internal systems often dated by the name of a prominent city magistrate. In Athens, that was the eponymous archon, in Sparta, the eponymous ephor, etc. The panhellenic system used Olympic years. In Dancing with the Lion, if you look at date plates before sections, that’s what I used. It’s a 4-year system, so, “In the year of the 97th Olympiad,” “In the first year of the 97th Olympiad,” “In the second year…,” and “In the third year…,” then we’re to “In the year of the 98th Olympiad…” In modern annotation it’s Ol. 97.1, Ol. 97.2, Ol. 97.3, Ol. 97.4. From (our year) 776 BCE down into the Roman Imperial era, the Olympics made useful anchor dating for the eastern Mediterranean (Magna Graecia).
Rome had its own system: two in fact. It counted years by both consuls, but also AUC = ab urba condita … “from the founding of the city.” Carthage used a similar system involving their two senior Judges for their senate.
When it came to “world histories,” authors such as Diodoros Siculus used several systems: Olympiad, Athenian archon, and Roman consuls. It gets a bit unwieldy, but is about as universal as we have for the Med until Christianity took over everything.
Yearly Calendars
Much of the ancient world used lunar (354 days), not solar (356 days) calendars. Yes, they knew a lunar year didn’t line up with the solar, and they used “intercalation” to fix it, avoiding summer festivals being celebrated in winter. Either a 13th month was needed every 3 years, or they added a few days to months here and there, making a “lunisolar” calendar. We have an intercalated day in our own calendar: Feb. 29th in Leap Year. To fix a calendar, however, an “anchor” is needed. This anchor is usually a solstice or equinox, which may (or may not) correspond to their New Year.
Our modern (Western) world places New Year’s in the dead of winter. But many pre-modern calendars put it in spring. Makes sense: life renews, it’s a new year. The Babylonian New Year was decided by the spring equinox—first new moon after—which pattern affected most of the ANE.
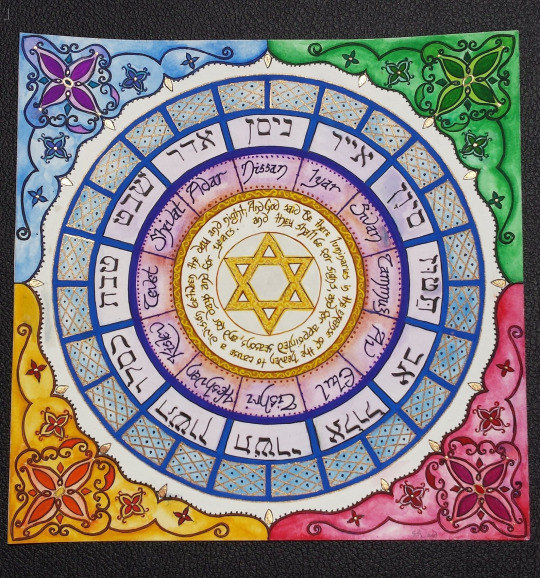
The Hebrew New Year (Rosh Hashana) is in autumn, but their first month (Nisan) is in spring. (They also have a New Year for Trees! Tú bish'vat. How cool is that?) Wanna know when your Jewish friends are having a holiday? Use Hebcal, the gold standard.
MANY ancient cultures have more than one calendar running at a time. So do we. Working in the uni, I have the “normal” year, but also the “academic” year to keep up with.
Despite the dominance of certain early systems like Babylon, counting the new year was specific to a region and people, and their religious traditions. No single Greek new year tradition existed. Both Delos and Athens used the first new moon after the summer equinox: early July. The Macedonian calendar seems to as well, so Alexander was born in the first month of the year. Other city states were different. I’ve forgotten most but do remember Sparta’s is in autumn because their new year almost falls on my birthday.
Remember, although we today talk about “ancient Greece” as if it were a country—it wasn’t. There was a landmass called Hellas, but each city-state was independent, and had its own laws, gov’t, coinage, and religious cult. Too often “Greek” winds up being conflated with “Athenian,” because we happen to have the most evidence from ancient Athens. But both Athens and Sparta were weirdos. Corinth, Thebes, Argos, Mytilene, Cos, Eretria, Miletus…all were a lot more typically Greek in their gov’t systems, etc. There were also 3 (or 4) different branches of Greek: Ionic-Attic, Doric, and Aeolic. When we talk about reading the “ancient Greek” language today, most people mean Attic Greek, or even Koine Greek (Hellenistic era common Greek).
That means every city-state had its own calendar, connected to its own festivals.
In fact, most city-states had several: sacred, civic, etc. Athens had a 12-month lunar calendar for festivals, but a 10-month civic calendar corresponding to the 10 tribes for Assembly business. Originally, they had only 4 tribes, not 10, so political changes meant calendar changes.
In each city-state, month names were derived from the major festival for that month. We have the complete month names for only a few: Athens is one and (fortunately for me) Macedon is another (specifically Ptolemaic, but it’s likely the same as the Argead). Below “Ancient Greek Month” REALLY means “Athenian month,” which annoys the hell out of those of us who don’t consider Athens the be-all and end-all of Greek history!
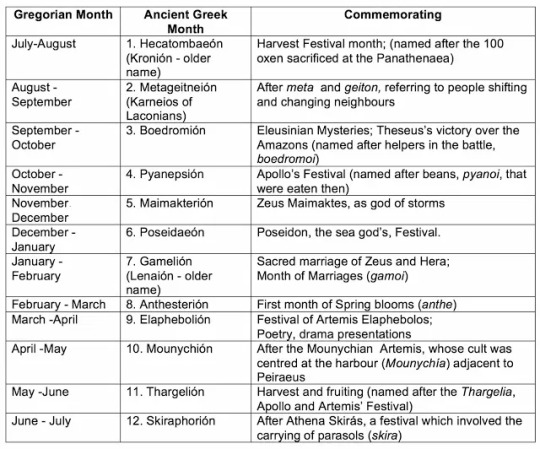
Because their months were lunar, they bisect our months, e.g., July/Aug = Athenian Hekatombian or Macedonian Loos [Alexander’s birthmonth], Jan/Feb = Athenian Gamelion or Macedonian Peritios [probably the month that gave Alexander’s favorite hound his name: Peritos]. Likewise, as the Athenian new year began in midsummer, dating ancient events also bisects. You’ll see 342/1 to designate the year from July of 342 BCE to June of 341.
As mentioned, most places used lunar months as the most basic time-keeping, but the moon isn’t the only way to make a “month.” Rome originally had 10 months of 30/31 days, adding 2 later, which is why our 12 months have Romanesque names.
Just remember: NO UNIVERSAL SYSTEM for months.
What About Weeks?
A seven-day week is borrowed from the Jews via Christianity. Both Jews and Egyptians had a dedicated day of rest. (For Egypt, the 10th day.) In most places, however, days off were festival related. Every month had festivals, which might last from half a day to several days in a row. You worked…took off for a festival…then you worked. No regular day of rest. (For the modern weekend? Thank unions and the Labor Movement!)
How did others subdivide a month? Athenian months were c. 30 days, divided into 10s: 1-10, 11-20, 10-1. Yup, the last is backwards. But dating also counted waxing and waning moons. So the new moon began a month, the 7th of the month would be the 7th waxing moon, the 24th the 6th waning moon. This is the Athenian system. Other city-states are less clear, but probably similar.
Romans had kalens (1st), nones (7th), and ides (15th). Nundinae (market days) means 9th, but were really the 8th day. The 7-day week is late Imperial and, again, owes to Christian take-over of Jewish weeks.
Most systems had “auspicious” and “inauspicious” days for religious activities, civic activities, and business activities. Don’t start anything on an inauspicious day! (These were manipulated, especially in Rome, but that’s a whole different discussion.) The closest modern equivalent I can think of is Mercury Retrograde. 😊 Although in modern Greece, signing a contract on a Tuesday morning is bad juju, or May 29th. Constantinople fell on a Tuesday morning May 29th, 1453. We might, in America, consider 9/11. Who wants to open a business on 9/11?
The Horai (The Hours)
When did the day begin? Again, the ANE and Med are different. In the ANE, day typically began at sunset. So yes, that’s why the Jewish shabbat starts at sunset on Friday and lasts till sunset on Saturday. (If you didn’t know, the Jewish “day of rest” isn’t Sunday, but Saturday.)
For Greece and Rome, et al., day began at dawn. Each day was then evenly divided between day and night, so there was no standard length of an hour. It depended on the time of year. Each half had twelve hours, subdivided into 4 groups of triads. Originally in Greece it seems there were only 9, not twelve, but they increased to match the lunar months. The division of 4 groups of triads also yielded the 4 seasons of 3 months each. Hora was initially a season, not an hour.
In any case, dawn was always the first hour, noon the 6th, sunset the 12th. Same deal for night (twilight, midnight, pre-dawn).
This is great for military and civic purposes, but most people tended to refer to daytime divisions more generally: dawn, midday, etc. And there was nothing like minutes or seconds. That’s totally modern. Closest, they might come would be to count “breaths.”
The gnomon (sundial) was the chief way to measure hours, as it matched longer or shorter days. But it’s kinda hard to use a sundial at night, or on a cloudy day, or inside. Night hours were approximate.

The water clock (klepsudra) was first popularized in Greece in courts and the Assembly (to time speeches), but spread to other use, for inside or on shady days. Yet water clocks are unwieldy to carry around.
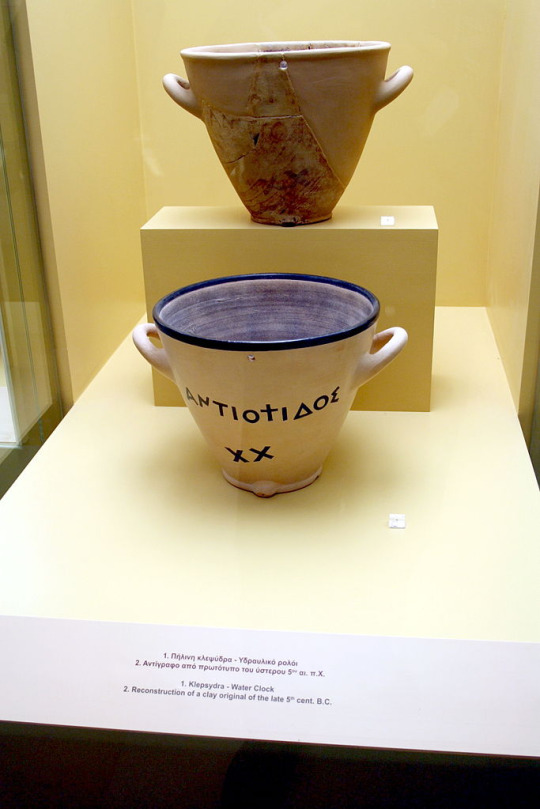
The Romans did have portable sundials (below), but again…needs the SUN. Btw, I should add that sundials aren’t only a Greco-Roman thing. The Chinese had them too. By contrast, the sand-clock or hourglass is a medieval invention. Won’t find them in the ancient world.

#time-keeping#calendars#time in the ancient world#months in the ancient world#ancient Greece#ancient Rome#ancient near east#Jewish calendars#sundials#the Horae#The Hours#Classics#ancient history#ancient Mediterranean history#asks
95 notes
·
View notes
Text
Four Houses in One, Brno
Four Houses in One, Brno Apartments Project, Czech Residential Architecture, Housing Buildings, Images
Four Houses in One in Brno
11 May 2021
Four Houses in One
Design: Kuba & Pilař architekti
Location: Neumannova Street 578/17, Brno, Czech Republic
The Four Houses in One building is located in a quiet residential Masaryk district, full of quality pre-war functionalist architecture. The volume and spatial solution is based on the character and proportions of the nearest buildings.
Residential complex consists of four blocks of different sizes – apartment buildings – which protrude above the terrain from a common underground base. The set of buildings thus naturally fits into its surroundings. The site with a south-west orientation and an attractive view over the Brno Exhibition Centre to the Kohoutovice forest was the reason for the maximum orientation and the opening of the residential complex into this direction.
The apartment buildings descend along the slope, their height decreases towards the southern tip of the plot. The pair of buildings along Neumannova Street has four floors above the ground and one underground floor, which are connected by a staircase hall with elevators.
Two lower apartment buildings have three and two floors above the ground, and with their smaller volume they follow the size of villas along the lower part of the plot. Between the sidewalk of Neumannova Street and the upper apartment buildings, a semi-private living space with a seating area has been designed.
On the roof of the parking base between the individual buildings is a private courtyard with gardens connected to the apartments. They are separated by low hedges – gabion baskets planted with hornbeams. The set of buildings is built as a combined brick and reinforced concrete structure.
The facades are clad with clinker brick slips. The smooth surfaces of the fixed and sliding panels made of aluminium sheets provide contrast to the structured surface of the brick slips. The floors of common areas inside buildings, stairs and tiling of entrance vestibule are made of cast terrazzo. Ceilings, stairs and elevator shafts were made as structural elements from exposed concrete. The unifying element of the whole building is the concept of greenery, which will stand out more and more over the time.
Materials combined brick and reinforced concrete structure sand lime blocks – walls, partitions composite aluminum sheet – facade panels clinker brick slips – facade wood – window frames aluminum – skylight and entrance door frames steel – railings, entrance gates terrazzo – floors of common areas inside buildings, stairs cladding, vestibule wall cladding exposed concrete – ceilings of common corridors, stairs and some walls gypsum plaster – walls, ceilings
Products and Brands walls, partitions — Kalksandstein\www.kalksandstein.cz composite facade sheet — Albond\www.albond.cz clinker brick slips Kontur 472 — Ströher\www.stroeher.com wooden window frames Europrofile 88 — PKS\www.pksokna.cz skylights and entrance doors — Schüco\www.schueco.com garage door — Hormann\www.hormann.cz elevators — ThyssenKrupp\https://ift.tt/2RO39HC outdoor bench Woody — mmcité\www.mmcite.com door entry system Linea 300 — Bticino\www.bticino.com wooden floor Monopark — Bauwerk\www.bauwerk-parkett.com bathroom tiles Stonework — Marazzi\www.marazzigroup.com switches and wall plugs Asfora — Schneider\www.se.com all sanitary facilities — Laufen Pro\www.laufen.cz all bathroom faucets — Hansa\www.hansa.com radiators Radik Line Vertikal — Korado\www.korado.cz interior downlights Takeo 100, 200 — Neko lighting\www.nekolighting.com lights on loggias and balconies RAY 1.0 — WEVER & DUCRÉ Lighting\www.weverducre.com outdoor light Kube 240 — Simes\www.simes.it outdoor step lights Alfia — Ares\www.aresill.net street lamps Urba S — Thorn Lighting\www.thornlighting.cz
Design: Kuba & Pilař architekti
Studio Kuba & Pilař architekti Author Tomáš Pilař Ladislav Kuba Wojciech Wilczek Jan Kopecký
Project location Neumannova Street 578/17, Brno, Czech Republic GPS: 49.195090N, 16.578045E
Project year 2015-2018 Completion year 2020 Built-up Area 3322 sqm Usable Floor Area 3316 m² apartments Plot size 4036 m² Dimensions volume 23 066 m3 47 apartments
Client Neumann bytový dům Client’s website www.trikaya.cz Project website www.neumanka.cz
About studio Kuba & Pilař architekti is an architectural studio founded by Ladislav Kuba and Tomáš Pilař in 1996. The studio ranks among the most recognised ones in Czech Republic. Their buildings have been awarded several times in Grand Prix of Architects – the most prestigious national award for architects. In 2002, they won the main prize for the Library of the Faculty of Arts, Masaryk University in Brno. Other recognised buildings by the studio include the St. Mary’s Chapel in Jestřebí, Residental Estate Na Krutci in Prague and the Omega Department Store in Brno.
Designed by the studio, the building of the Faculty of Chemistry and Technology, University of Pardubice received the main prize in Grand Prix 2009. The Apartment House at Kostelní Square in Ostrava won the first place of Grand Prix 2011 in the New Building Category. In 2015, the Grand Prix certificate of merit went to the studio for the Iron Curtain Memorial. In 2020, they won the Grand Prix for the design of a family house in the Dyje Valley in Znojmo.
Their latest work include the building of the Faculty of Humanities, Charles University in Prague completed in 2020 and extension of the South Bohemian Scientific Library, which was put in use in April 2021.
The work of Kuba & Pilař architekti has been nominated for the European Union Prize for Contemporary Architecture – Mies van der Rohe Award several times and published in both national
Photographer: BoysPlayNice
Signature Restaurant in Brno images / information received 280417
Location: Brno, Czech Republic, central eastern Europe
Brno Architecture
Contemporary Architecture in Brno
Brno Architecture Designs – chronological list
Brno Architect
Brno Architecture photo from architects
Vila Tugendhat photo © Colin Eaton
Future Cities Forum Conference Brno
Czech Architecture
Contemporary Architecture in the Czech Republic
Prague Architecture
Czech Architect – architectural firm listings on e-architect
Zlin Congress Centre Design: Eva Jiricna Architects image from EJAL Zlin Building
Brno Bridge
Tugendhat Villa Brno photo from architects
Prague Buildings
Czech Architect – key architectural firms
Comments / photos for Signature Restaurant in Brno Architecture page welcome
The post Four Houses in One, Brno appeared first on e-architect.
2 notes
·
View notes
Text
Ice Hockey: Wild Wings: Tidy is not enough - DEL
Ice Hockey: Wild Wings: Tidy is not enough – DEL
[ad_1]
In the second section, the Neckarstadter increased. Andreas Thuresson (25th) drew after great preparation by Christopher Fischer centrally before the penguin goal to 1: 1. The match was now balanced, but after a mistake by Kyle Sonnenburg led the North Germans by the goal from Jan Urbas 2-1 (35.). Cedric Schiemenz (39) gave a good chance of the Wild Wings. Andreas Thuresson called before…
View On WordPress
0 notes
Text
Team USA falls unexpectedly to Slovenia in OT to start their 2018 Olympic tournament

A 2-0 lead in the third turned into a shocking 3-2 overtime loss for the men.
Despite leading 2-0 coming into the third period, Team USA was not able to hold onto the lead in their first 2018 Winter Olympics tournament game as Slovenia was able to mount a comeback to win 3-2 in overtime. Jan Mursak got the tying goal for Slovenia with 1:37 left to play in the third period.
The game started well for the United States as veteran Brian O’Neill got the Americans up 1-0 late in the first period with 2:16 to go in the frame. With the Slovenia defense scrambled in their own zone, O’Neill got between the opposing defenders to pot Team USA’s first goal of the tournament. The Americans outshot Slovenia 11-3 in the first period, and that number would only grow throughout the game.
In the second period, 20-year-old Jordan Greenway doubled the Americans’ lead over Slovenia with a goal midway through the period. Greenway was able to pick up a rebound in close before goaltender Gasper Kroselj could slide over to stop the puck. O’Neill got his second point of the day with an assist on Greenway’s even strength tally, but that was the last time the United States would get on the scoreboard.
Even though the Americans came into the third period with the 2-0 lead, the team was sloppy, as they allowed Slovenia to put 11 shots on goal. Their opponents took advantage of the American’s sloppiness as Jan Urbas got Slovenia on the board with 15 minutes left to play in the frame.
Everything eventually collapsed on Team USA when Mursak scored the tying tally with less than two minutes to play with the goaltender pulled for Slovenia.
In the five minute 3-on-3 overtime, Team USA put up no shots on goal before Mursak again tallied the game winner just 38 seconds into the frame for the 3-2 victory.
Mursak had two points for Slovenia in the stunning victory over the United States.
Thanks to the 3-2 Russian loss in regulation, however, Team USA is now third in Group B with one point due to advancing to overtime. The Americans will have a chance at redemption Thursday evening against Slovakia as round robin play continues.
0 notes
Text
Arplis - News: Coronavirus and Kids: Doctors Answer Parents’ COVID-19 Questions
The coronavirus is here and parents have questions about the threat COVID-19 poses to the health of their children. As of now, answers have not been satisfactory, consistent, or satisfactorily consistent. Early studies out of China suggest that though mortality rates are low — though still highly worrisome at a population level — novel coronavirus does pose a serious risk to children as well as the elderly, specifically some children with pre-existing conditions. That said, all children can be vectors for the disease and scientist have not yet uncovered any patterns in infection that might justify complacency. Outcomes among infants, in particular, have been varied and have many front-line medical workers we’ve spoken to are worried.
This story, which will be updated frequently until scientific consensus is reached on the questions posed, is intended to be an up-to-date accounting of what epidemiologists, doctors, and public health workers know so far. All quotes are timestamped because available information is becoming outdated rapidly. Answers should be understood in light of that fact. Just because we believe we know something now does not mean that thing is true. A lot of hypotheses have yet to be tested. In the meantime, the best approach is to maintain social distance and to stay informed.
Will coronavirus kill or hurt my kids?
Dr. John Williams, Chief of the Division of Pediatric Infectious Diseases at the University of Pittsburgh Medical Center Children’s Hospital of Pittsburgh. April 7, 2020 (12:30PM): Currently, there is not much data on kids and coronavirus. Some respiratory illnesses, such as the seasonal flu (influenza), put children at risk of serious health complications. Each year, the flu causes millions of illnesses, thousands of hospitalizations, and some deaths in children. COVID-19, however, appears to be affecting children at a much lower rate. Less than 1% of all COVID-19 hospitalizations in the US are of children. The biggest concern for kids in our country are those with underlying conditions. All of our children’s hospitals, including mine, are doing what we can to protect these vulnerable kids while we learn whether they truly have increased risk.
Dr. Logan Spector, Division Director and Professor, Pediatric Epidemiology and Clinical Research at University of Minnesota, March 24, 2020 (5PM): When it comes to young children, my biggest takeaway is that most severe cases [of COVID-19 in young children] were suffered by children with very serious conditions. In the New England Journal study, three severe cases had leukemia, hydronephrosis, and intussusception. So my takeaway from that is that even among children, the worst cases require comorbidities to have the worse outcome. My day job is studying pediatric cancer and I can tell you it’s not especially common.
Dr. Neel Shah, Director of the Delivery Decisions Initiative at Ariadne Labs and assistant professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School March 20 (1:30PM): There are some neonatal transmissions, but it doesn’t seem like infants and neonates are severely affected. We think of people who are pregnant and infants as vulnerable. But we mean that in a lot of different ways. Simply because they’re not likely to be severely infected does not mean they aren’t affected.
Strains on the healthcare system mean ambulatory services are shutting down, prenatal and postpartum support is being shut down. Social distancing impacts pregnancies too. It’s simply harder to get labor support — from doulas or even family members. And there’s always been concern about social isolation after having a baby. Even more so now.
Barun Mathema, Assistant Professor Epidemiology Columbia University; March 22 (11AM): The most recent evidence from China that shows that children are vulnerable, or at least more so than previously thought. Younger children being a higher risk for more serious clinical symptoms than older children. It appears that mortality is still somewhat rare among children.
Barun Mathema, March 18 (11AM): I’ll preface this by saying we’re all confused. Initially, it was confusing that kids weren’t hit because we were wondering if the disease would follow the patterning of pandemic influenza where the curve is a beautiful bell with age on the bottom. Seasonal flu is the opposite, a u-shape. And initially, this didn’t fit either scenario. COVID-19 seemed like a geometric curve from low to high in terms of severity, but now that picture is getting muddled. We’re seeing folks under 50 with morbidity. We’re seeing teenagers and younger kids with fairly severe symptoms.
There was a sliver of pediatric cases and a sliver of pediatric deaths in China. Kids get colds a lot so there was a theory that some are caused by coronaviruses and so there’s partial immunity. There was also the thought that the ACE2 receptor might not be well expressed in children so there could be inefficient entry. Arguably we should be seeing a huge surge in cases, but questions remain unresolved. One can simply say that given a large sample size and a small morbidity, we’re still talking about a big number.
Dr. Jan Dumois, Pediatric Infectious Diseases physician at Johns Hopkins All Children’s Hospital. March 16, 2020 (4:30PM): “There’s a new article where they review 2100 kids who were suspected to have COVID-19. There was one child who died — teen. Only one. Otherwise, all the other kids survived, but they did have different degrees of severity of illness. Sicker kids tended to be younger and needed more aggressive medical care before they were sent home. … not just showing up to the emergency room and being sent home. Patients who ended up in hospital because they needed oxygen. Or they were found to have pneumonia. Then there were some uncommon cases that needed to be on a respirator. Younger children are more likely to be sicker and require hospitalization. Or to be on a ventilator. Sometimes heart. Or the dysfunction of the kidney. It was more common in children less than one. ��
Ryan Demmer, PhD, University of Minnesota Division of Epidemiology and Community Health. March 16, 2020 (11AM): Kids who had preexisting conditions, particularly chronic or complex medical conditions, were more likely to have adverse medical outcomes and more likely to have severe ones at that. The co-morbidities that seemed to be the most troubling are with asthma and cystic fibrosis. Children with upper respiratory disease seem to be at risk.
While the absolute numbers are low in terms of mortality among young people, there’s a .01 percent mortality rate for flu in youth and early numbers in kids with COVID-19 put the figure around .2. That’s not high, but it’s a 20 fold-increase. If I told you a plane was twenty times more likely that other planes to crash, you would not get on that plane.
How can I avoid getting the virus?
Dyan Hes, MD, Medical Director of Gramercy Pediatrics in New York City and Clinical Assistant Professor of Pediatrics at Weill Medical College of Cornell University. April 9, 2020 (12:00PM): Stay at home. If you have to go to work, you should wear a mask or bandana. You have to wash your hands when you come in from outside. Wash your hands repeatedly throughout the day as you have contact with other people. Some people say that washing your hands every 20 minutes is the best way to decrease the spread of the virus. Don’t touch your face. A lot of people choose to wear gloves whenever they’re out in public, but then they don’t take the gloves off immediately. If you use your gloves outside, when you’re commuting to work let’s say, then touch your phone, your phone is now contaminated. But people don’t think about that. Wearing gloves might be useless because you have this false sense of protection. You really have to understand the use of protective wear.
John Williams, April 7, 2020 (12:30PM): Preventing the spread of COVID-19 from one person in the family to others can be challenging but can be accomplished. For families with older adults or people in their households with chronic illnesses, consideration should be given to see if there is a way to have that person stay with another relative while your child with COVID-19 recovers. If that is not possible, you should work to separate your child from as many of the other household members as possible. This could be accomplished by having the child with COVID-19 stay in one part of the home while those with chronic conditions could stay in another part. In addition, keeping your child with COVID-19 more than 6 feet away from the other people in your home combined with frequent handwashing and cleaning of places like door handles and hard surfaces with bleach containing products can be successful. You should also teach your child with COVID-19 to cover their cough with their elbow and to wash their hands frequently, especially if they are going to be in common areas used by others in the home. People who are sick can wear a cloth mask to reduce transmission to others.
Ashlesha Kaushik, MD, FAAP, Pediatric Infectious Disease Physician and Director of the Antimicrobial Stewardship Program at UnityPoint Health St. Luke’s. April 6, 2020 (3:00PM): The CDC has advised people all across the country that everybody out in public places like a mall or a clinic needs to cover their faces now. They don’t need to use medical or surgical masks for that. Those will be reserved for patients that are sick with symptoms or are being seen actively in a healthcare facility. But for the general public, they’re saying that keeping the nose and mouth area covered will halt the spread of the virus from asymptomatic people.
Barun Mathema; March 22 (11AM) I think the basic rule of thumb is keeping the kids in situations where there is very little density — and certainly keeping the hands clean. So this may be easier in peri-urban or rural locales. Personally, having kids run around outside is really important for general physical and mental health (also for the parents) but not having much or any physical contact would be the goal – this includes surfaces that may be contaminated. It’s hard not to be preachy about things but I will try to politely keep my distance and also explain that even if we do not personally feel at risk, our behavior can (without malintent) put members of our community at risk….we may not even know who is at risk.
Barun Mathema; March 18 (11AM): Just because the elderly and folks with preexisting conditions are vulnerable doesn’t leave everyone else off the hook. This is a serious infection. We read about asymptomatic carriers and minor disease and, yes, many people have had it and will without even noticing. That’s true. It’s also true that three to five percent of otherwise healthy individuals will end up with a serious disease that could require ventilation. Many will recover but it will be an uphill battle. Social distancing and flattening the curve are the answer to this, especially given that a middle-age group will wind up responsible for taking care of most people.
Juan Dumois, March 16, 2020 (4:30PM): The biggest study was able to detect some patients that had no symptoms but were infected. Found quite a few of those. Almost 100. The study wasn’t really designed to look for asymptomatic kids. That study hasn’t yet been published.
When should I get my kid tested?
Dyan Hes, April 9, 2020 (12:00PM): Right now, we’re not testing children in New York City. Your child will only be tested at this point, at least in New York City where we’re having more cases than any country around the world, if they’re in severe respiratory distress and need to be hospitalized. We have to assume that 80% of the colds that are going around now are COVID. We’re not testing because the kids’ cases have been very mild. The only children in my practice that have been tested have been newborns whose parents have been positive. So you don’t have to run to get your child tested if you are sick.
Lindsay Thompson, April 7, 2020 (3:00PM): We unfortunately across the country do not yet have enough screening tests to be able to test children who are fairly well-appearing. It’s not usually until they’re so sick that they might have to go to the emergency room that we do the testing. So I think parents sometimes get frustrated that they can’t know for sure but are told they could have COVID-19. If they’re doing okay, you just need to go home and stay there for two weeks in quarantine. That doesn’t feel as rewarding as getting a test, but in some situations, we’re not able to test everybody. The parents may have to trust their pediatrician to assess that their child at that moment is doing okay.
John Williams, April 7, 2020 (12:30PM): The major concern and the reason for a child to be tested, is only if the child had severe symptoms, which would primarily be difficulty breathing. Children may have fever, which makes them feel bad, but fever isn’t dangerous. If a child has a runny nose or cough, but isn’t having trouble breathing and is drinking ok, they don’t need to be tested and are probably best kept at home.
Barun Mathema; March 18 (11AM): Public health is a very socialist approach. It means health for all trumps health for the individual. This is the antithesis of precision medicine. At this point, as a parent and a public health person, I feel that if a kid is exhibiting alarming symptoms — not a runny nose, but maybe a fever or something that looks unlike a regular cold — parents should consider taking the kid in. But, on some level, it’s important to recognize there’s nothing you’d do differently if your kid tested positive. If children are heavily symptomatic, take them in and get them admitted. Otherwise, you’re going home and observing. Still, there’s some virtue in knowing that you likely have it and that other people in your network likely have it as well.
Georges Benjamin, March 18, 2020: That’s up to every doctor right now. They’re not testing very many kids. I think most kids are only being tested when there’s an emergency. Call the number in the community you’re given, usually the local health department, because these guidelines are changing literally every day.
Sophia Thomas, March 18, 2020: If they have a fever, if they have a cough, they should contact their medical provider to see how they want to handle this. A requirement for testing is patients have to have a negative flu test. With children, oftentimes you would want to do a Strep test as well. If those tests are negative, then they may be eligible to have a COVID-19 test. However, because of the relative shortage of tests right now, different medical practices are doing different things. Some are having to prioritize using the test for the most vulnerable or the ones that have most potential for complications.
Dr. Juan Dumois, Pediatric Infectious Diseases physician at Johns Hopkins All Children’s Hospital, March 16, 2020 (4:30PM): One of the main things that’s going to be changing the way we deal with the pandemic is the availability of testing. It will become more available as the weeks go on. We have more availability this week than last. And tons more this week… some are doing it in their hospitals. We hope to be able to do that test sometime in the next month. As the ability to rapidly and readily do a test where you get results in a few hours and a few days will change the dynamic of people we aren’t currently testing.
Something that might happen int he next six months would be a doctor in the clinic to swab a patient’s nose and get results the next day. Right now we can’t offer the test to everybody and it’s taking 5 days to get results back.
My child has the virus. Now what?
Lindsay Thompson, April 7, 2020 (3:00PM): Hopefully most parents have identified a primary care provider that they can call. I do recommend calling first. Almost all practices have instituted their own version of social distancing, and a lot of practices now offer telemedicine visits. As a pediatrician, you can learn a lot from what’s going on with the child by talking to the parents and seeing the child through telemedicine, so that can be very helpful. I do not recommend going straight to an emergency room unless you can tell that your child is having severe breathing problems or anything like that because we worry that places like emergency rooms inadvertently are spreading the virus or other illnesses that we wouldn’t want your child to get.
There’s some really good resources on the CDC website about taking care of anybody who lives in your house with COVID-19. But children need their parents. If there are other children, I would recommend that if you live in a two-parent household only one parent takes care of that child and the other parent takes care of the other children to try to minimize exposure. If you have the luxury of being able to put that child in their own room with their own bathroom, that would be what I recommend. Really try to isolate them even within the home. Don’t share any plates, cups, knives and forks. Make sure everything is separate. I might even recommend a different meal time for that child compared to the other children. I know it sounds pretty grim. But you really need to separate these children from the rest of the family if possible.
Ashlesha Kaushik, April 6, 2020 (3:00PM): At this point, when we are in the mode of social distancing, pediatricians don’t want to leave the families alone, so parents should call the pediatrician if they are worried about anything — be it symptoms that they might think are related to COVID-19 or to any other stress they’re feeling. The pediatrician can offer emotional support as well as offer valuable medical advice. If the symptoms are really mild, they can advise parents how to keep the children hydrated by making them drink enough water or using Tylenol for fever control.
Georges Benjamin, MD, Executive Director of the American Public Health Association. March 18, 2020 (2PM): When kids get really sick, they often don’t eat enough and they often don’t drink enough. Usually, you can coax them to take small sips of water throughout the day. The most important thing is making sure the kid isn’t very, very sick and doesn’t need medical care right now. Most kids do just fine with this.
Sophia Thomas, March 18, 2020 (11AM): Certainly children right now are catching COVID-19, but they are less likely to have complications. Those are children who just need to be isolated for 14 days. If you suspect your child has the virus, you can simply just keep them at home and care for them unless they start having serious problems such as breathing difficulties.
Barun Mathema; March 18 (11AM): I have kids. If they got it, as a public health person, I would be more concerned about them giving it to someone else. Let your healthcare provider know and then basically take care of your child and enhance social distancing. If you have a nanny, give them a call. The health department doesn’t have the capacity to do that.
I have coronavirus, now what?
Juan Dumois, March 23, 2020 (3:30PM): I think a lot of physicians in infectious diseases are hopeful about some of the treatments being investigated for the sickest patients with COVID-19. And while the official stance is there are no proven drugs (and this is correct) there are promising drugs that are being tested on patients with COVID-19. Unfortunately, we’ll start seeing shortages of all these drugs if we do find drugs that kill the virus.
Elisa Choi, MD, Internal Medicine & Infectious Disease Specialist at Atrius Health. March 23, 2020 (8:30AM):`If someone is having significant difficulty breathing, they may need to get further assessed, and home treatment may not be appropriate. Likewise, if someone is having very high fevers, it may be important to get them evaluated. But if someone can be safely managed at home, at this point in time the management strategy for someone who is either suspected of COVID-19 or has confirmed COVID-19 is supportive care and symptom management. So, for example, if someone has a mild cough, you can try over-the-counter remedies to manage that cough. If someone is having muscle aches, again it would be over-the-counter remedies to manage all of those symptoms.
Barun Mathema; March 18 (11AM): This is a tough question. If you have coronavirus and kids you get tested and you find out that you’re positive. At that point, you can assume that a fraction if not all household members are positive. It’s different if you’ve flown in or been screened prior to symptoms. So you may want to self-isolate. But those lines are blurring. All the quarantining will be a moot point because we’ll all be there. The question is just how extreme or expansive. It’s a guessing game, but you want to isolate you and probably your family.
How scared should I be for my parents?
Elisa Choi, March 23, 2020 (8:30 AM): COVID-19 might have increased the risk of significant complications in older individuals, including the worst complication, which is death related to COVID-19. It is understandable that many adults may worry about their elderly parents with COVID-19, particularly since we don’t have a vaccine for this illness, and there is, as of today, nothing that has been concretely proven as a successful therapeutic. It’s very reasonable to be worried. That being said, the majority of people who contract COVID-19 do tend to have relatively milder symptoms. However, if an adult has specific concerns about their parent because they may have multiple other chronic illnesses or might be immunocompromised, which are some other risk factors for more severe COVID-19 disease, it’s certainly worth being particularly mindful of the current recommendations for minimizing spread of COVID-19. If an adult has concerns about themselves having COVID-19, they should reach out and seek clinical evaluation sooner rather than later, particularly if they are a caretaker of their older parent or are living in the same household as their older parent.
Dr. Alicia Ines Arbaje M.P.H., Ph.D. Director of Transitional Care Research, Johns Hopkins Medicine, March 19 (5 PM): Generally we should be concerned about how health systems can respond to the surge of people coming in. People who are coming to the hospital should be the sickest. If it so happens that they should be older, that is what it is. People who are having milder symptoms should be managed at home. It’s more level of need and not so much level of aid. ERs are set up to triage people appropriately. My biggest concern is that we don’t have the supplies or staffing to help care for people when they come. We haven’t gotten to that point yet, but it’s a real concern. How are we going to mobilize our resources?
Dr. Mary Tinetti, Professor of Medicine and Public Health and is Chief of Geriatrics at Yale School of Medicine March 19, 2020 (11AM): We should be very worried. Most of the data we are able to look at are coming out of Italy and some modeling epidemiologists are doing in the rest of the world is showing positive testing in all age groups. But who is getting seriously ill? The vast majority are people 60 and older. The key in focusing on 60 and older is for their own good and the good of everyone else. They’re more likely to use healthcare resources. More likely to die. All the care consumed by them may limit care for younger people.
For this population especially, the more social isolation the better. This means if you’re over 60 especially don’t go out in public, don’t be within 6 feet of anyone, get deliveries or get someone else to drop off your groceries and medications, and get tested if you can. If we start looking at the asymptomatic 60 year old we’ll see how serious it is. Once it’s available. All localities are prioritizing. The more we know the better. So get tested.
Sophia Thomas, March 18, 2020 (2PM: This is a virus that knows no social barriers, and we do know that older people and people with comorbid conditions including hypertension, heart disease, COPD and asthma tend to have worse outcomes. So all grandparents — anybody over the age of 60 — should take this very seriously and practice social isolation. My mother was going to come and visit me and I just told her stay where you are. We’ll FaceTime and I’ll see you next month.
Dr. Logan Spector, March 18, 2020 (11AM): Look to Italy. One of the reasons it is hit so hard is that it had one of the oldest populations in Europe. I really doubt that’s going to change at all. There have been nearly 200,000 reports and we can say with pretty good statistical certainty who are impacted and it’s very clear the elderly are hardest hit. It’s still not clear to me how much of that is just reduced immune function versus co-morbidities. The older you are, the more likely you are to have a pulmonary disease that compounds the effect of a respiratory virus. But there is still a risk in older people who don’t have co-morbidities. That points to lower immune function as we age.
Ryan Demmer, March 16, 2020: I think we should move forward with caution because mortality rates aren’t just linked to the properties of the disease. They are often a product of the environment or context of the disease. China is not America. In America, we have varied healthcare access and high rates of asthma. That could portend worse outcomes in this country. I should state clearly that there’s no evidence of that yet, but we should be cautious.
When will things go back to normal?
Dyan Hes, April 9, 2020 (12:00PM): I’m not that optimistic right now because we do not have a federal law in place to stay at home. Big cities that have been hit like Detroit, New York City, Chicago, Miami, those cities have good stay-at-home rules in place, and I think they’re working. Staying at home works. But what’s going to happen is once we conquer this epidemic in New York, it’s going to spread to other states and cities that have not been implementing stay-at-home. I fear that it’s going to spread across the country and it will get to places like Arizona where up until a week ago you could go get a mani-pedi. Those states will have outbreaks, and I fear it’s going to come back because you can travel from state to state. Not all people are that ethical. Not all people are keeping quarantine. I almost had to report a family yesterday to Child Services because they’re not keeping their quarantine. We hope people stay at home, but not everybody is that altruistic. I feel like what’s going to happen is they’re going to find a treatment before we’re able to stop it based on human behavior.
Lindsay Thompson, April 7, 2020 (3:00PM): I wish I knew. There’s no magic formula, and certainly, I think we’ll never be the same. So I’m not quite sure what normal will be. But most importantly, it’s not going to be a one-day event where everything turns back to normal. It’s going to be a little bit of loosening different recommendations in different places. If we suddenly all went back to what we were doing before, there would be another round of severe illness for lots of people. Just take a deep breath. Get ready because this may take a while. But the longer we take, the less people will be hurt. So patience is really really important. And selfless.
Ashlesha Kaushik, April 6, 2020 (3:00PM): What the CDC has been projecting is that it will take at least a few weeks to a few months, but nobody is exactly sure about the timeline. They are waiting for the curve to flatten out. The curve is yet to peak, which is the scary part. We haven’t yet reached the peak in the United States. They were projecting the peak to be sometime this week or the next coming week. The few upcoming weeks will be really tough. The more we practice the social distancing measures, the more we can expect to flatten out the curve. That is still a long way to go.
Dr. Logan Spector March 24, 2020 (5PM):“Once you let your foot off the brake of social distancing, will you have resurgent cases? Almost certainly. If we all stayed in our houses we would squelch this thing. The virus would die with that. If there are still people out and about who are infected, it will be reintroduced. That’s always been acknowledged. The idea is to spread it out enough to make sure we have healthcare capacity and give the medical community some time to manufacture PPE and develop a vaccine. Let’s just say that any politician — really anyone — who thinks he knows better than virologists and epidemiologists at this point doesn’t have his head on straight.”
Juan Dumois, March 23, 2020 (3:30 PM): Over the last several day I’ve been looking at some of our local COVID-19 patients (in the Tampa Bay Area) who tested positive The numbers are still relatively small, and I suspect that may be a benefit of the social distancing we’re doing. That makes me optimistic. We may already be having a positive effect. However, i don’t think anyone should be lulled into complacency or thinking that this will be over soon. We need to bear it out for several more months.
Elisa Choi, March 23, 2020 (8:30 AM): Where we are now is the infection and the illness is spreading. I’ll speak to Massachusetts because that’s the state I’m in. The number of cases is increasing daily. So we’re in the phase of the illness where there’s still exponential rise in new cases. Now definitely is not a time where we can scale back on measures to mitigate the spread of infection. It’s really hard to give a firm number or a firm timeline of when all of these kinds of measures can be retracted. My sense of how this would play out, though, is once there’s a plateau reached in terms of how many new infections are being detected every day, there may need to be some gradual reduction in some of the current mitigation measures. And it may not be able to be done all at once. It will need to be determined as we get to that plateau point. How long that will be is uncertain. If we reflect on what’s happening in some of the countries in Asia where they have reached that point — China would probably be the best example — it was about two or so months before they got to that point. Things may be different in the U.S. and things may be different moving from state to state in the U.S.
Georges Benjamin, March 18, 2020 (2PM): We don’t know. There are estimates out there that this could go anywhere through a month or two. Those are probably reasonable assumptions. A month or two does not necessarily mean that all of us will be sequestered for a month or two. We just don’t know. We’ve never done this before.
Sophia Thomas, DNP, President of the American Association of Nurse Practitioners. March 18, 2020 (2:30PM): I think this is our new normal for a while. I heard something yesterday that the CDC anticipates that the peak of this might be in May. I think for the next six to eight weeks we’re going to be dealing with this. I don’t anticipate a resolution anytime soon. If people really stick to the social distancing and listen to the advice of the CDC, we could actually see this resolved much sooner by limiting people’s exposure.
Logan Spector, March 18, 2020 (11:10AM EST): Obviously this is unprecedented in modern memory. Everyone is talking about the 1918 flu pandemic and there a lot of the same characteristics as most flu, but the problem with COVID-19 is that there seems to be asymptomatic transmission. Isolating people with symptoms is a first response — and it’s a logical one. When SARS and MERS came out, this was done as well. But those did not seem to have asymptomatic transmission. I think everyone is trying to do their part including those working from home, but it will take time.
Ryan Demmer, March 16, 2020:From a population health perspective the main issue remains not infecting others. There’s no evidence kids don’t get infected or transmit, just that they’re less effected by the disease. Our key goal has to be social distancing. The growth curve is still coming.
The question is where the peak will be. Probably May-ish. And I’m not saying it’s going to go away…. After the peak, we’ll start coming down. What I’m interested in from an ecological point of view is what’s happening in South Korea and Wuhan. They’re saying there’s one case in the province which I find dumbfounding. And there was an impressive decline in South Korea. So if that’s true —and there’s no second peak — that would be fantastic news…. If there’s a second peak that could be as bad if not worse. COVID-19 could come back in the Fall only to finish off in the spring of 2021 when we have a vaccine. That’s a harsh but not unrealistic scenario.
Parenting during a pandemic is hard. Sign up for our daily newsletter full of tricks, tips, and relevant medical information.
↓ Get the best of Fatherly in your inbox
Oops! Please try again.
Thanks for subscribing!
Related Articles:
A New 'Simpsons' Short Is Coming to Disney+ Tomorrow
Coronavirus Could Tank Your Credit Score. He's How to Protect It
'Modern Family' Aired Its Finale Last Night, But That May Not Be the End
'Toy Story' Songwriter Drops New Quarantine Song
The post Coronavirus and Kids: Doctors Answer Parents’ COVID-19 Questions appeared first on Fatherly.
Arplis - News source http://feedproxy.google.com/~r/Arplis-News/~3/sHw7n0nDWFQ/coronavirus-and-kids-doctors-answer-parents-covid-19-questions
0 notes
Text
Olympics Hockey 2018: Norway Beat Slovenia 2-1 in Overtime Comeback Win
Olympics Hockey 2018: Norway Beat Slovenia 2-1 in Overtime Comeback Win
Norway advanced to the men’s ice hockey quarter-finals at the 2018 Winter Olympics on Tuesday after they came from behind to beat Slovenia 2-1 in overtime in Pyeongchang, South Korea. Jan Urbas opened the scoring for Slovenia in the first period, but Tommy Kristiansen equalised in the third at the Gangneung Hockey Centre before Alexander Bonsaken grabbed the winner in overtime. Norway will take…
View On WordPress
0 notes
Text
VS en Rusland verliezen zonder NHL-spelers hun openingsduel
VS en Rusland verliezen zonder NHL-spelers hun openingsduel
(adsbygoogle = window.adsbygoogle || []).push();
Het olympisch ijshockeytoernooi is begonnen met twee grote verrassingen. De Amerikanen verloren na verlenging met 3-2 van Slovenië en de Russen bogen met dezelfde cijfers voor Slowakije.
Amerika, dat evenals alle andere toplanden in Pyeongchang zonder zijn NHL-sterren aantreedt, verloor voor het eerst sinds 1998 zijn openingsduel op de Spelen.
De ploeg leidde na de tweede periode met 2-0, maar via treffers van Jan Urbas en Jan Mursak (twee goals) zette de nummer vijftien van het afgelopen WK alsnog het duel op z’n kop.
Ook Russen verspelen voorsprong
De Russische ploeg, die het niet alleen zonder de NHL-sterren moet doen, maar ook enkele spelers mist als gevolg van de Russische dopingschorsing, leidde na vier minuten al met 2-0, maar ging toch onderuit tegen de nummer veertien van het WK.
The post VS en Rusland verliezen zonder NHL-spelers hun openingsduel appeared first on FHE | Gratis eredivisie voetbal streams, en buitenlands voetbal streams.
VS en Rusland verliezen zonder NHL-spelers hun openingsduel published first on https://footballhighlightseurope.tumblr.com/
0 notes
Text
VS en Rusland verliezen zonder NHL-spelers hun openingsduel
VS en Rusland verliezen zonder NHL-spelers hun openingsduel
(adsbygoogle = window.adsbygoogle || []).push();
Het olympisch ijshockeytoernooi is begonnen met twee grote verrassingen. De Amerikanen verloren na verlenging met 3-2 van Slovenië en de Russen bogen met dezelfde cijfers voor Slowakije.
Amerika, dat evenals alle andere toplanden in Pyeongchang zonder zijn NHL-sterren aantreedt, verloor voor het eerst sinds 1998 zijn openingsduel op de Spelen.
De ploeg leidde na de tweede periode met 2-0, maar via treffers van Jan Urbas en Jan Mursak (twee goals) zette de nummer vijftien van het afgelopen WK alsnog het duel op z’n kop.
Ook Russen verspelen voorsprong
De Russische ploeg, die het niet alleen zonder de NHL-sterren moet doen, maar ook enkele spelers mist als gevolg van de Russische dopingschorsing, leidde na vier minuten al met 2-0, maar ging toch onderuit tegen de nummer veertien van het WK.
The post VS en Rusland verliezen zonder NHL-spelers hun openingsduel appeared first on FHE | Gratis eredivisie voetbal streams, en buitenlands voetbal streams.
0 notes
Text
Every Goal Of The 2023 IIHF Worlds: Day 7
Hungary Vs. Sweden
#24 Oscar Lindberg (3) Tömmernes (2), A. Lindholm (1) 1:33 1st (Hungary 0-1 Sweden)
#95 Jacob De La Rose (1)(SH) Grundström (2) 5:13 1st (Hungary 0-2 Sweden)
#17 Kiss Roland (1) István (3), Zsombor (1) 7:36 1st (Hungary 1-2 Sweden)
#18 Dennis Everberg (2) Liljegren (1), Sandin (1) 17:50 1st (Hungary 1-3 Sweden)
#20 André Petersson (1)(PP) Tömmernes (3), Raymond (1) 4:17 2nd (Hungary 1-4 Sweden)
#48 Jonatan Berggren (1) Raymond (2), Liljegren (2) 17:37 2nd (Hungary 1-5 Sweden)
#95 Jacob De La Rose (2) Sörensen (2), Tömmernes (4) 18:20 2nd (Hungary 1-6 Sweden)
#23 Lucas Raymond (2) Carlsson (3), Tömmernes (5) 8:48 3rd (Hungary 1-7 Sweden)
Denmark Vs. Germany
#15 Matias Lassen (2) M. Holton-Lauridsen (5), Ehlers (3) 5:39 1st (Denmark 1-0 Germany)
#33 John-Jason Peterka (2) Wissmann (2) 9:12 2nd (Denmark 1-1 Germany)
#40 Alexander Ehl (1) M. Müller (2), Seider (2) 11:08 2nd (Denmark 1-2 Germany)
#91 Moritz Müller (1) Noebels (2), Peterka (1) 17:51 2nd (Denmark 1-3 Germany)
#50 Mathias Bau-Hansen (1) Krogsgaard (1), Wejse (1) 19:37 2nd (Denmark 2-3 Germany)
#65 Christian Wejse (1) Olesen (2), Andersen (3) 15:01 3rd (Denmark 3-3 Germany)
#41 Jonas Müller (1) Wissmann (3), Stachowiak (1) 15:21 3rd (Denmark 3-4 Germany)
#92 Marcel Noebels (2)(EN) Sturm (1) 18:56 3rd (Denmark 3-5 Germany)
#65 Christian Wejse (2) M. Holton-Lauridsen (6), Koch (1) 19:28 3rd (Denmark 4-5 Germany)
#78 Nico Sturm (1)(EN) unassisted 19:35 3rd (Denmark 4-6 Germany)
Czech Republic Vs. Slovenia
#91 Miha Verlič (1) Urbas (1), Gregorc (2) 7:23 1st (Czech Republic 0-1 Slovenia)
#26 Jan Urbas (1)(PP) Gregorc (3), Jeglič (2) 11:49 1st (Czech Republic 0-2 Slovenia)
#18 Dominik Kubalík (4)(PP) Kempný (1), Tomášek (3) 18:19 2nd (Czech Republic 1-2 Slovenia)
#18 Dominik Kubalík (5) Tomášek (4), Smejkal (1) 3:47 3rd (Czech Republic 2-2 Slovenia)
#10 Roman Červenka (2) Voženílek (1), Košťálek (2) 5:00 3rd (Czech Republic 3-2 Slovenia)
#6 Michal Kempný (2) Sobotka (2), Kubalík (3) 11:12 3rd (Czech Republic 4-2 Slovenia)
#18 Dominik Kubalík (6)(EN)(HT) Zbořil (1) 17:49 3rd (Czech Republic 5-2 Slovenia)
#19 Jakub Flek (1) Kempný (2), Dvořák (3) 18:56 3rd (Czech Republic 6-2 Slovenia)
Switzerland Vs. Slovakia
#97 Jonas Siegenthaler (1) Malgin (3), Hischier (1) 5:07 1st (Switzerland 1-0 Slovakia)
#22 Nino Niederreiter (4) Ambühl (1) 4:47 2nd (Switzerland 2-0 Slovakia)
#17 Andrej Kudrna (1) Kelemen (2), Pánik (1) 5:08 2nd (Switzerland 2-1 Slovakia)
#87 Pavol Regenda (1)(PP) Okuliar (1), Kňažko (1) 19:29 2nd (Switzerland 2-2 Slovakia)
#54 Christian Marti (1) Richard (4) 6:51 3rd (Switzerland 3-2 Slovakia)
#92 Gaëtan Haas (1)(EN) Miranda (4), Simion (2) 19:25 3rd (Switzerland 4-2 Slovakia)
#Sports#Hockey#Goals#National Teams#Hungary#Sweden#Denmark#Czech Republic#Slovenia#Switzerland#Slovakia
0 notes
Link
Here's what happened on Day 3 of the World Hockey Championship in Paris, France and Cologne, Germany.
Canada 7 - Slovenia 2
The Canadians flexed their offensive muscles with their most dominant performance of the tournament so far, improving to 2-0-0-0.
Nathan MacKinnon picked up the hat trick and an assist - earning player of the game honors - while his Colorado Avalanche teammate Tyson Barrie also picked up four points of his own (1G, 3A).
KHL forward Jan Mursak scored Slovenia's first tally late in the second period, while Jan Urbas picked up the team's second on a delayed penalty with just over two minutes remaining in the third period.
Canada outshot Slovenia 51-14.
The Canadians' next game comes Monday against Belarus, while Slovenia will enjoy a day off before taking on Norway on Tuesday.
For full scores and coverage, visit the IIHF's World Championship website.
Copyright © 2017 Score Media Ventures Inc. All rights reserved. Certain content reproduced under license.
from New Sports Updates http://ift.tt/2qPPltH
0 notes
Text
Arplis - News: Coronavirus and Kids: Doctors Answer Parents’ COVID-19 Questions
The coronavirus is here and parents have questions about the threat COVID-19 poses to the health of their children. As of now, answers have not been satisfactory, consistent, or satisfactorily consistent. Early studies out of China suggest that though mortality rates are low — though still highly worrisome at a population level — novel coronavirus does pose a serious risk to children as well as the elderly, specifically some children with pre-existing conditions. That said, all children can be vectors for the disease and scientist have not yet uncovered any patterns in infection that might justify complacency. Outcomes among infants, in particular, have been varied and have many front-line medical workers we’ve spoken to are worried.
This story, which will be updated frequently until scientific consensus is reached on the questions posed, is intended to be an up-to-date accounting of what epidemiologists, doctors, and public health workers know so far. All quotes are timestamped because available information is becoming outdated rapidly. Answers should be understood in light of that fact. Just because we believe we know something now does not mean that thing is true. A lot of hypotheses have yet to be tested. In the meantime, the best approach is to maintain social distance and to stay informed.
Will coronavirus kill or hurt my kids?
Dr. John Williams, Chief of the Division of Pediatric Infectious Diseases at the University of Pittsburgh Medical Center Children’s Hospital of Pittsburgh. April 7, 2020 (12:30PM): Currently, there is not much data on kids and coronavirus. Some respiratory illnesses, such as the seasonal flu (influenza), put children at risk of serious health complications. Each year, the flu causes millions of illnesses, thousands of hospitalizations, and some deaths in children. COVID-19, however, appears to be affecting children at a much lower rate. Less than 1% of all COVID-19 hospitalizations in the US are of children. The biggest concern for kids in our country are those with underlying conditions. All of our children’s hospitals, including mine, are doing what we can to protect these vulnerable kids while we learn whether they truly have increased risk.
Dr. Logan Spector, Division Director and Professor, Pediatric Epidemiology and Clinical Research at University of Minnesota, March 24, 2020 (5PM): When it comes to young children, my biggest takeaway is that most severe cases [of COVID-19 in young children] were suffered by children with very serious conditions. In the New England Journal study, three severe cases had leukemia, hydronephrosis, and intussusception. So my takeaway from that is that even among children, the worst cases require comorbidities to have the worse outcome. My day job is studying pediatric cancer and I can tell you it’s not especially common.
Dr. Neel Shah, Director of the Delivery Decisions Initiative at Ariadne Labs and assistant professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School March 20 (1:30PM): There are some neonatal transmissions, but it doesn’t seem like infants and neonates are severely affected. We think of people who are pregnant and infants as vulnerable. But we mean that in a lot of different ways. Simply because they’re not likely to be severely infected does not mean they aren’t affected.
Strains on the healthcare system mean ambulatory services are shutting down, prenatal and postpartum support is being shut down. Social distancing impacts pregnancies too. It’s simply harder to get labor support — from doulas or even family members. And there’s always been concern about social isolation after having a baby. Even more so now.
Barun Mathema, Assistant Professor Epidemiology Columbia University; March 22 (11AM): The most recent evidence from China that shows that children are vulnerable, or at least more so than previously thought. Younger children being a higher risk for more serious clinical symptoms than older children. It appears that mortality is still somewhat rare among children.
Barun Mathema, March 18 (11AM): I’ll preface this by saying we’re all confused. Initially, it was confusing that kids weren’t hit because we were wondering if the disease would follow the patterning of pandemic influenza where the curve is a beautiful bell with age on the bottom. Seasonal flu is the opposite, a u-shape. And initially, this didn’t fit either scenario. COVID-19 seemed like a geometric curve from low to high in terms of severity, but now that picture is getting muddled. We’re seeing folks under 50 with morbidity. We’re seeing teenagers and younger kids with fairly severe symptoms.
There was a sliver of pediatric cases and a sliver of pediatric deaths in China. Kids get colds a lot so there was a theory that some are caused by coronaviruses and so there’s partial immunity. There was also the thought that the ACE2 receptor might not be well expressed in children so there could be inefficient entry. Arguably we should be seeing a huge surge in cases, but questions remain unresolved. One can simply say that given a large sample size and a small morbidity, we’re still talking about a big number.
Dr. Jan Dumois, Pediatric Infectious Diseases physician at Johns Hopkins All Children’s Hospital. March 16, 2020 (4:30PM): “There’s a new article where they review 2100 kids who were suspected to have COVID-19. There was one child who died — teen. Only one. Otherwise, all the other kids survived, but they did have different degrees of severity of illness. Sicker kids tended to be younger and needed more aggressive medical care before they were sent home. … not just showing up to the emergency room and being sent home. Patients who ended up in hospital because they needed oxygen. Or they were found to have pneumonia. Then there were some uncommon cases that needed to be on a respirator. Younger children are more likely to be sicker and require hospitalization. Or to be on a ventilator. Sometimes heart. Or the dysfunction of the kidney. It was more common in children less than one. “
Ryan Demmer, PhD, University of Minnesota Division of Epidemiology and Community Health. March 16, 2020 (11AM): Kids who had preexisting conditions, particularly chronic or complex medical conditions, were more likely to have adverse medical outcomes and more likely to have severe ones at that. The co-morbidities that seemed to be the most troubling are with asthma and cystic fibrosis. Children with upper respiratory disease seem to be at risk.
While the absolute numbers are low in terms of mortality among young people, there’s a .01 percent mortality rate for flu in youth and early numbers in kids with COVID-19 put the figure around .2. That’s not high, but it’s a 20 fold-increase. If I told you a plane was twenty times more likely that other planes to crash, you would not get on that plane.
How can I avoid getting the virus?
Dyan Hes, MD, Medical Director of Gramercy Pediatrics in New York City and Clinical Assistant Professor of Pediatrics at Weill Medical College of Cornell University. April 9, 2020 (12:00PM): Stay at home. If you have to go to work, you should wear a mask or bandana. You have to wash your hands when you come in from outside. Wash your hands repeatedly throughout the day as you have contact with other people. Some people say that washing your hands every 20 minutes is the best way to decrease the spread of the virus. Don’t touch your face. A lot of people choose to wear gloves whenever they’re out in public, but then they don’t take the gloves off immediately. If you use your gloves outside, when you’re commuting to work let’s say, then touch your phone, your phone is now contaminated. But people don’t think about that. Wearing gloves might be useless because you have this false sense of protection. You really have to understand the use of protective wear.
John Williams, April 7, 2020 (12:30PM): Preventing the spread of COVID-19 from one person in the family to others can be challenging but can be accomplished. For families with older adults or people in their households with chronic illnesses, consideration should be given to see if there is a way to have that person stay with another relative while your child with COVID-19 recovers. If that is not possible, you should work to separate your child from as many of the other household members as possible. This could be accomplished by having the child with COVID-19 stay in one part of the home while those with chronic conditions could stay in another part. In addition, keeping your child with COVID-19 more than 6 feet away from the other people in your home combined with frequent handwashing and cleaning of places like door handles and hard surfaces with bleach containing products can be successful. You should also teach your child with COVID-19 to cover their cough with their elbow and to wash their hands frequently, especially if they are going to be in common areas used by others in the home. People who are sick can wear a cloth mask to reduce transmission to others.
Ashlesha Kaushik, MD, FAAP, Pediatric Infectious Disease Physician and Director of the Antimicrobial Stewardship Program at UnityPoint Health St. Luke’s. April 6, 2020 (3:00PM): The CDC has advised people all across the country that everybody out in public places like a mall or a clinic needs to cover their faces now. They don’t need to use medical or surgical masks for that. Those will be reserved for patients that are sick with symptoms or are being seen actively in a healthcare facility. But for the general public, they’re saying that keeping the nose and mouth area covered will halt the spread of the virus from asymptomatic people.
Barun Mathema; March 22 (11AM) I think the basic rule of thumb is keeping the kids in situations where there is very little density — and certainly keeping the hands clean. So this may be easier in peri-urban or rural locales. Personally, having kids run around outside is really important for general physical and mental health (also for the parents) but not having much or any physical contact would be the goal – this includes surfaces that may be contaminated. It’s hard not to be preachy about things but I will try to politely keep my distance and also explain that even if we do not personally feel at risk, our behavior can (without malintent) put members of our community at risk….we may not even know who is at risk.
Barun Mathema; March 18 (11AM): Just because the elderly and folks with preexisting conditions are vulnerable doesn’t leave everyone else off the hook. This is a serious infection. We read about asymptomatic carriers and minor disease and, yes, many people have had it and will without even noticing. That’s true. It’s also true that three to five percent of otherwise healthy individuals will end up with a serious disease that could require ventilation. Many will recover but it will be an uphill battle. Social distancing and flattening the curve are the answer to this, especially given that a middle-age group will wind up responsible for taking care of most people.
Juan Dumois, March 16, 2020 (4:30PM): The biggest study was able to detect some patients that had no symptoms but were infected. Found quite a few of those. Almost 100. The study wasn’t really designed to look for asymptomatic kids. That study hasn’t yet been published.
When should I get my kid tested?
Dyan Hes, April 9, 2020 (12:00PM): Right now, we’re not testing children in New York City. Your child will only be tested at this point, at least in New York City where we’re having more cases than any country around the world, if they’re in severe respiratory distress and need to be hospitalized. We have to assume that 80% of the colds that are going around now are COVID. We’re not testing because the kids’ cases have been very mild. The only children in my practice that have been tested have been newborns whose parents have been positive. So you don’t have to run to get your child tested if you are sick.
Lindsay Thompson, April 7, 2020 (3:00PM): We unfortunately across the country do not yet have enough screening tests to be able to test children who are fairly well-appearing. It’s not usually until they’re so sick that they might have to go to the emergency room that we do the testing. So I think parents sometimes get frustrated that they can’t know for sure but are told they could have COVID-19. If they’re doing okay, you just need to go home and stay there for two weeks in quarantine. That doesn’t feel as rewarding as getting a test, but in some situations, we’re not able to test everybody. The parents may have to trust their pediatrician to assess that their child at that moment is doing okay.
John Williams, April 7, 2020 (12:30PM): The major concern and the reason for a child to be tested, is only if the child had severe symptoms, which would primarily be difficulty breathing. Children may have fever, which makes them feel bad, but fever isn’t dangerous. If a child has a runny nose or cough, but isn’t having trouble breathing and is drinking ok, they don’t need to be tested and are probably best kept at home.
Barun Mathema; March 18 (11AM): Public health is a very socialist approach. It means health for all trumps health for the individual. This is the antithesis of precision medicine. At this point, as a parent and a public health person, I feel that if a kid is exhibiting alarming symptoms — not a runny nose, but maybe a fever or something that looks unlike a regular cold — parents should consider taking the kid in. But, on some level, it’s important to recognize there’s nothing you’d do differently if your kid tested positive. If children are heavily symptomatic, take them in and get them admitted. Otherwise, you’re going home and observing. Still, there’s some virtue in knowing that you likely have it and that other people in your network likely have it as well.
Georges Benjamin, March 18, 2020: That’s up to every doctor right now. They’re not testing very many kids. I think most kids are only being tested when there’s an emergency. Call the number in the community you’re given, usually the local health department, because these guidelines are changing literally every day.
Sophia Thomas, March 18, 2020: If they have a fever, if they have a cough, they should contact their medical provider to see how they want to handle this. A requirement for testing is patients have to have a negative flu test. With children, oftentimes you would want to do a Strep test as well. If those tests are negative, then they may be eligible to have a COVID-19 test. However, because of the relative shortage of tests right now, different medical practices are doing different things. Some are having to prioritize using the test for the most vulnerable or the ones that have most potential for complications.
Dr. Juan Dumois, Pediatric Infectious Diseases physician at Johns Hopkins All Children’s Hospital, March 16, 2020 (4:30PM): One of the main things that’s going to be changing the way we deal with the pandemic is the availability of testing. It will become more available as the weeks go on. We have more availability this week than last. And tons more this week… some are doing it in their hospitals. We hope to be able to do that test sometime in the next month. As the ability to rapidly and readily do a test where you get results in a few hours and a few days will change the dynamic of people we aren’t currently testing.
Something that might happen int he next six months would be a doctor in the clinic to swab a patient’s nose and get results the next day. Right now we can’t offer the test to everybody and it’s taking 5 days to get results back.
My child has the virus. Now what?
Lindsay Thompson, April 7, 2020 (3:00PM): Hopefully most parents have identified a primary care provider that they can call. I do recommend calling first. Almost all practices have instituted their own version of social distancing, and a lot of practices now offer telemedicine visits. As a pediatrician, you can learn a lot from what’s going on with the child by talking to the parents and seeing the child through telemedicine, so that can be very helpful. I do not recommend going straight to an emergency room unless you can tell that your child is having severe breathing problems or anything like that because we worry that places like emergency rooms inadvertently are spreading the virus or other illnesses that we wouldn’t want your child to get.
There’s some really good resources on the CDC website about taking care of anybody who lives in your house with COVID-19. But children need their parents. If there are other children, I would recommend that if you live in a two-parent household only one parent takes care of that child and the other parent takes care of the other children to try to minimize exposure. If you have the luxury of being able to put that child in their own room with their own bathroom, that would be what I recommend. Really try to isolate them even within the home. Don’t share any plates, cups, knives and forks. Make sure everything is separate. I might even recommend a different meal time for that child compared to the other children. I know it sounds pretty grim. But you really need to separate these children from the rest of the family if possible.
Ashlesha Kaushik, April 6, 2020 (3:00PM): At this point, when we are in the mode of social distancing, pediatricians don’t want to leave the families alone, so parents should call the pediatrician if they are worried about anything — be it symptoms that they might think are related to COVID-19 or to any other stress they’re feeling. The pediatrician can offer emotional support as well as offer valuable medical advice. If the symptoms are really mild, they can advise parents how to keep the children hydrated by making them drink enough water or using Tylenol for fever control.
Georges Benjamin, MD, Executive Director of the American Public Health Association. March 18, 2020 (2PM): When kids get really sick, they often don’t eat enough and they often don’t drink enough. Usually, you can coax them to take small sips of water throughout the day. The most important thing is making sure the kid isn’t very, very sick and doesn’t need medical care right now. Most kids do just fine with this.
Sophia Thomas, March 18, 2020 (11AM): Certainly children right now are catching COVID-19, but they are less likely to have complications. Those are children who just need to be isolated for 14 days. If you suspect your child has the virus, you can simply just keep them at home and care for them unless they start having serious problems such as breathing difficulties.
Barun Mathema; March 18 (11AM): I have kids. If they got it, as a public health person, I would be more concerned about them giving it to someone else. Let your healthcare provider know and then basically take care of your child and enhance social distancing. If you have a nanny, give them a call. The health department doesn’t have the capacity to do that.
I have coronavirus, now what?
Juan Dumois, March 23, 2020 (3:30PM): I think a lot of physicians in infectious diseases are hopeful about some of the treatments being investigated for the sickest patients with COVID-19. And while the official stance is there are no proven drugs (and this is correct) there are promising drugs that are being tested on patients with COVID-19. Unfortunately, we’ll start seeing shortages of all these drugs if we do find drugs that kill the virus.
Elisa Choi, MD, Internal Medicine & Infectious Disease Specialist at Atrius Health. March 23, 2020 (8:30AM):`If someone is having significant difficulty breathing, they may need to get further assessed, and home treatment may not be appropriate. Likewise, if someone is having very high fevers, it may be important to get them evaluated. But if someone can be safely managed at home, at this point in time the management strategy for someone who is either suspected of COVID-19 or has confirmed COVID-19 is supportive care and symptom management. So, for example, if someone has a mild cough, you can try over-the-counter remedies to manage that cough. If someone is having muscle aches, again it would be over-the-counter remedies to manage all of those symptoms.
Barun Mathema; March 18 (11AM): This is a tough question. If you have coronavirus and kids you get tested and you find out that you’re positive. At that point, you can assume that a fraction if not all household members are positive. It’s different if you’ve flown in or been screened prior to symptoms. So you may want to self-isolate. But those lines are blurring. All the quarantining will be a moot point because we’ll all be there. The question is just how extreme or expansive. It’s a guessing game, but you want to isolate you and probably your family.
How scared should I be for my parents?
Elisa Choi, March 23, 2020 (8:30 AM): COVID-19 might have increased the risk of significant complications in older individuals, including the worst complication, which is death related to COVID-19. It is understandable that many adults may worry about their elderly parents with COVID-19, particularly since we don’t have a vaccine for this illness, and there is, as of today, nothing that has been concretely proven as a successful therapeutic. It’s very reasonable to be worried. That being said, the majority of people who contract COVID-19 do tend to have relatively milder symptoms. However, if an adult has specific concerns about their parent because they may have multiple other chronic illnesses or might be immunocompromised, which are some other risk factors for more severe COVID-19 disease, it’s certainly worth being particularly mindful of the current recommendations for minimizing spread of COVID-19. If an adult has concerns about themselves having COVID-19, they should reach out and seek clinical evaluation sooner rather than later, particularly if they are a caretaker of their older parent or are living in the same household as their older parent.
Dr. Alicia Ines Arbaje M.P.H., Ph.D. Director of Transitional Care Research, Johns Hopkins Medicine, March 19 (5 PM): Generally we should be concerned about how health systems can respond to the surge of people coming in. People who are coming to the hospital should be the sickest. If it so happens that they should be older, that is what it is. People who are having milder symptoms should be managed at home. It’s more level of need and not so much level of aid. ERs are set up to triage people appropriately. My biggest concern is that we don’t have the supplies or staffing to help care for people when they come. We haven’t gotten to that point yet, but it’s a real concern. How are we going to mobilize our resources?
Dr. Mary Tinetti, Professor of Medicine and Public Health and is Chief of Geriatrics at Yale School of Medicine March 19, 2020 (11AM): We should be very worried. Most of the data we are able to look at are coming out of Italy and some modeling epidemiologists are doing in the rest of the world is showing positive testing in all age groups. But who is getting seriously ill? The vast majority are people 60 and older. The key in focusing on 60 and older is for their own good and the good of everyone else. They’re more likely to use healthcare resources. More likely to die. All the care consumed by them may limit care for younger people.
For this population especially, the more social isolation the better. This means if you’re over 60 especially don’t go out in public, don’t be within 6 feet of anyone, get deliveries or get someone else to drop off your groceries and medications, and get tested if you can. If we start looking at the asymptomatic 60 year old we’ll see how serious it is. Once it’s available. All localities are prioritizing. The more we know the better. So get tested.
Sophia Thomas, March 18, 2020 (2PM: This is a virus that knows no social barriers, and we do know that older people and people with comorbid conditions including hypertension, heart disease, COPD and asthma tend to have worse outcomes. So all grandparents — anybody over the age of 60 — should take this very seriously and practice social isolation. My mother was going to come and visit me and I just told her stay where you are. We’ll FaceTime and I’ll see you next month.
Dr. Logan Spector, March 18, 2020 (11AM): Look to Italy. One of the reasons it is hit so hard is that it had one of the oldest populations in Europe. I really doubt that’s going to change at all. There have been nearly 200,000 reports and we can say with pretty good statistical certainty who are impacted and it’s very clear the elderly are hardest hit. It’s still not clear to me how much of that is just reduced immune function versus co-morbidities. The older you are, the more likely you are to have a pulmonary disease that compounds the effect of a respiratory virus. But there is still a risk in older people who don’t have co-morbidities. That points to lower immune function as we age.
Ryan Demmer, March 16, 2020: I think we should move forward with caution because mortality rates aren’t just linked to the properties of the disease. They are often a product of the environment or context of the disease. China is not America. In America, we have varied healthcare access and high rates of asthma. That could portend worse outcomes in this country. I should state clearly that there’s no evidence of that yet, but we should be cautious.
When will things go back to normal?
Dyan Hes, April 9, 2020 (12:00PM): I’m not that optimistic right now because we do not have a federal law in place to stay at home. Big cities that have been hit like Detroit, New York City, Chicago, Miami, those cities have good stay-at-home rules in place, and I think they’re working. Staying at home works. But what’s going to happen is once we conquer this epidemic in New York, it’s going to spread to other states and cities that have not been implementing stay-at-home. I fear that it’s going to spread across the country and it will get to places like Arizona where up until a week ago you could go get a mani-pedi. Those states will have outbreaks, and I fear it’s going to come back because you can travel from state to state. Not all people are that ethical. Not all people are keeping quarantine. I almost had to report a family yesterday to Child Services because they’re not keeping their quarantine. We hope people stay at home, but not everybody is that altruistic. I feel like what’s going to happen is they’re going to find a treatment before we’re able to stop it based on human behavior.
Lindsay Thompson, April 7, 2020 (3:00PM): I wish I knew. There’s no magic formula, and certainly, I think we’ll never be the same. So I’m not quite sure what normal will be. But most importantly, it’s not going to be a one-day event where everything turns back to normal. It’s going to be a little bit of loosening different recommendations in different places. If we suddenly all went back to what we were doing before, there would be another round of severe illness for lots of people. Just take a deep breath. Get ready because this may take a while. But the longer we take, the less people will be hurt. So patience is really really important. And selfless.
Ashlesha Kaushik, April 6, 2020 (3:00PM): What the CDC has been projecting is that it will take at least a few weeks to a few months, but nobody is exactly sure about the timeline. They are waiting for the curve to flatten out. The curve is yet to peak, which is the scary part. We haven’t yet reached the peak in the United States. They were projecting the peak to be sometime this week or the next coming week. The few upcoming weeks will be really tough. The more we practice the social distancing measures, the more we can expect to flatten out the curve. That is still a long way to go.
Dr. Logan Spector March 24, 2020 (5PM):“Once you let your foot off the brake of social distancing, will you have resurgent cases? Almost certainly. If we all stayed in our houses we would squelch this thing. The virus would die with that. If there are still people out and about who are infected, it will be reintroduced. That’s always been acknowledged. The idea is to spread it out enough to make sure we have healthcare capacity and give the medical community some time to manufacture PPE and develop a vaccine. Let’s just say that any politician — really anyone — who thinks he knows better than virologists and epidemiologists at this point doesn’t have his head on straight.”
Juan Dumois, March 23, 2020 (3:30 PM): Over the last several day I’ve been looking at some of our local COVID-19 patients (in the Tampa Bay Area) who tested positive The numbers are still relatively small, and I suspect that may be a benefit of the social distancing we’re doing. That makes me optimistic. We may already be having a positive effect. However, i don’t think anyone should be lulled into complacency or thinking that this will be over soon. We need to bear it out for several more months.
Elisa Choi, March 23, 2020 (8:30 AM): Where we are now is the infection and the illness is spreading. I’ll speak to Massachusetts because that’s the state I’m in. The number of cases is increasing daily. So we’re in the phase of the illness where there’s still exponential rise in new cases. Now definitely is not a time where we can scale back on measures to mitigate the spread of infection. It’s really hard to give a firm number or a firm timeline of when all of these kinds of measures can be retracted. My sense of how this would play out, though, is once there’s a plateau reached in terms of how many new infections are being detected every day, there may need to be some gradual reduction in some of the current mitigation measures. And it may not be able to be done all at once. It will need to be determined as we get to that plateau point. How long that will be is uncertain. If we reflect on what’s happening in some of the countries in Asia where they have reached that point — China would probably be the best example — it was about two or so months before they got to that point. Things may be different in the U.S. and things may be different moving from state to state in the U.S.
Georges Benjamin, March 18, 2020 (2PM): We don’t know. There are estimates out there that this could go anywhere through a month or two. Those are probably reasonable assumptions. A month or two does not necessarily mean that all of us will be sequestered for a month or two. We just don’t know. We’ve never done this before.
Sophia Thomas, DNP, President of the American Association of Nurse Practitioners. March 18, 2020 (2:30PM): I think this is our new normal for a while. I heard something yesterday that the CDC anticipates that the peak of this might be in May. I think for the next six to eight weeks we’re going to be dealing with this. I don’t anticipate a resolution anytime soon. If people really stick to the social distancing and listen to the advice of the CDC, we could actually see this resolved much sooner by limiting people’s exposure.
Logan Spector, March 18, 2020 (11:10AM EST): Obviously this is unprecedented in modern memory. Everyone is talking about the 1918 flu pandemic and there a lot of the same characteristics as most flu, but the problem with COVID-19 is that there seems to be asymptomatic transmission. Isolating people with symptoms is a first response — and it’s a logical one. When SARS and MERS came out, this was done as well. But those did not seem to have asymptomatic transmission. I think everyone is trying to do their part including those working from home, but it will take time.
Ryan Demmer, March 16, 2020:From a population health perspective the main issue remains not infecting others. There’s no evidence kids don’t get infected or transmit, just that they’re less effected by the disease. Our key goal has to be social distancing. The growth curve is still coming.
The question is where the peak will be. Probably May-ish. And I’m not saying it’s going to go away…. After the peak, we’ll start coming down. What I’m interested in from an ecological point of view is what’s happening in South Korea and Wuhan. They’re saying there’s one case in the province which I find dumbfounding. And there was an impressive decline in South Korea. So if that’s true —and there’s no second peak — that would be fantastic news…. If there’s a second peak that could be as bad if not worse. COVID-19 could come back in the Fall only to finish off in the spring of 2021 when we have a vaccine. That’s a harsh but not unrealistic scenario.
Parenting during a pandemic is hard. Sign up for our daily newsletter full of tricks, tips, and relevant medical information.
↓ Get the best of Fatherly in your inbox
Oops! Please try again.
Thanks for subscribing!
Related Articles:
A New 'Simpsons' Short Is Coming to Disney+ Tomorrow
Coronavirus Could Tank Your Credit Score. He's How to Protect It
'Modern Family' Aired Its Finale Last Night, But That May Not Be the End
'Toy Story' Songwriter Drops New Quarantine Song
The post Coronavirus and Kids: Doctors Answer Parents’ COVID-19 Questions appeared first on Fatherly.
Arplis - News source https://arplis.com/blogs/news/coronavirus-and-kids-doctors-answer-parents-covid-19-questions
0 notes
Text
2020-21 Fischtown Pinguins Bremerhaven S.B. G.M.B.H. Roster
Wingers
#9 Jan Urbas (Ljubljana, Slovenia)
#10 Filip Reisnecker (Prague, Czech Republic)
#13 Žiga Jeglič (Kranj, Slovenia)
#19 Christian Hilbrich (Toronto, Ontario)
#27 Carson McMillan (Brandon, Manitoba)
#48 Niklas Andersen (Esbjerg, Denmark)
#74 Tomas Sykora (Banska Bystrica, Slovakia)
#79 Mitch Wahl (Seal Beach, California)
#91 Miha Verlič (Maribor, Slovenia)
#98 Luca Gläser (Schlema, Germany)
Centers
#11 Cory Quirk (Brockton, Massachusetts)
#14 Ross Mauermann (Janesville, Wisconsin)
#26 Dominik Uher (Frydek-Mistek, Czech Republic)
#57 Alex Friesen (St. Catharines, Ontario)
Defensemen
#18 Maxime Fortunas (La Prairie, Quebec)
#22 Vladimír Eminger (Litvinov, Czech Republic)
#32 Anders Krogsgaard (Esbjerg, Denmark)
#50 Patch Alber (Clifton Park, New York)
#55 Mike Moore (Calgary, Alberta) C
#67 Stanislav Dietz (Pisek, Czech Republic)
Goalies
#31 Brandon Maxwell (Winter Park, Florida)
#42 Tomáš Pöpperle (Broumov, Czech Republic)
#Sports#Hockey#Hockey Goalies#Germany#Celebrities#Florida#Czech Republic#New York#Canada#Quebec#Denmark#Alberta#Ontario#Slovenia#Wisconsin#Manitoba#Massachusetts#Slovakia
0 notes
Text
2017 IIHF World Championships Slovenia Roster
Wingers
#8 Ziga Jeglic (H.C. Slovan Bratislava/Kranj)
#12 David Rodman (Bruleurs De Loups/Jesenice)
#16 Ales Music (H.D.D. Olimpija Ljubljana/Ljubljana)
#19 Ziga Pance (E.C. K.A.C./Ljubljana)
#39 Jan Mursak (H.C. C.S.K.A. Moscow/Maribor)
#55 Robert Sabolic (H.C. Admiral/Jesenice)
#71 Bostjan Golicic (A.D.S. De Gresse d’Agers/Kranj)
#76 Nik Pem (Heilbronner Falken/Jesenice)
#92 Anze Kuralt (Bruleurs De Loups/Kranj)
#93 Gregor Koblar (Lyon H.C./Ljubljana)
Centers
#18 Ken Ograjensek (Graz 99ers/Celje)
#24 Rok Ticar (Avtomobilist Yekaterinburg/Jesenice)
#26 Jan Urbas (E.C. V.S.V./Ljubljana)
#84 Andrej Hebar (Ujpesti T.E./Ljubljana)
#91 Miha Verlic (E.C. V.S.V./Maribor)
Defensemen
#4 Andrej Tavzelj (A.D.S. De Glisse d’Angers/Kovor)
#6 Miha Stebih (H.C. Frydek-Mistek/Maribor)
#7 Klemen Pretnar (H.C. Yunost-Minsk/Bled)
#14 Matic Podlipnik (Lyon H.C./Jesenice)
#15 Braz Gregorc (Mountfield H.K./Jesenice)
#23 Luka Vidmar (Frederikshavn White Hawks/Ljubljana)
#28 Ales Kranjc (Rote Teufel Bad Nauheim/Jesenice)
#51 Mitja Robar (E.C. K.A.C./Maribor)
#61 Jurij Repe (H.C. Kladno/Ljubljana)
#86 Sabahudin Kovacevic (H.C. Yunost-Minsk/Jesenice)
Goalies
#32 Gasper Kroselj (A.I.K. Idrottsforening/Ljubljana)
#40 Luka Gracnar (E.C. Red Bull Salzburg/Jesenice)
#69 Matija Pintaric (Lyon H.C./Maribor)
#Sports#Hockey#Hockey Goalies#Celebrities#National Teams#Slovenia#France#Czech Republic#Belarus#Slovakia#Austria#Denmark#Russia#Germany#Sweden#Hungary
2 notes
·
View notes
Text
Every Goal Of The 2017 IIHF Worlds Day 3
Russia Vs. Italy
#11 Sergei Andronov (2) Barabanov, Gavrikov 9:35 1st (Russia 1-0 Italy)
#63 Yevgeny Dadonov (1)(PP) Panarin 18:59 1st (Russia 2-0 Italy)
#90 Tommaso Traversa (1) Anton Bernard 3:40 2nd (Russia 2-1 Italy)
#86 Nikita Kucherov (1)(PP) Namestnikov 4:50 2nd (Russia 3-1 Italy)
#90 Vladislav Namestnikov (1) Kucherov 15:03 2nd (Russia 4-1 Italy)
#72 Artemi Panarin (2)(PP) Mozyakhin, Shipachyov 16:21 2nd(Russia 5-1 Italy)
#16 Sergei Plotnikov (1)(PP) Namestnikov 3:39 3rd (Russia 6-1 Italy)
#10 Sergei Mozyakhin (1)(PP) Shipachyov 5:29 3rd (Russia 7-1 Italy)
#90 Vladislav Namestnikov (2) Mironov 5:47 3rd (Russia 8-1 Italy)
#72 Artemi Panarin (3)(PP) Mozyakhin 10:20 3rd (Russia 9-1 Italy)
#21 Alexander Barabanov (1) Provorov 18:53 3rd (Russia 10-1 Italy)
U.S.A. Vs. Denmark
#27 Anders Lee (1)(PP) Gaudreau, Larkin 5:35 1st (U.S.A. 1-0 Denmark)
#19 Clayton Keller (1) McAvoy 14:06 1st (U.S.A. 2-0 Denmark)
#29 Morten Madsen (1)(PP) Ehlers, J. Jensen 16:10 1st (U.S.A. 2-1 Denmark)
#13 Johnny Gaudreau (1)(PP) Larkin 18:59 1st (U.S.A. 3-1 Denmark)
#43 Nichlas Hardt (1) Jakobsen 1:08 2nd (U.S.A. 3-2 Denmark)
#19 Clayton Keller (2) Bjugstad 14:31 2nd (U.S.A. 4-2 Denmark)
#27 Anders Lee (2)(PP) Hanifin, McAvoy 17:09 2nd (U.S.A. 5-2 Denmark)
#29 Brock Nelson (1) Schmaltz 17:37 2nd (U.S.A. 6-2 Denmark)
#19 Clayton Keller (3)(hat trick) Murphy 13:00 3rd (U.S.A. 7-2 Denmark)
Slovakia Vs. Latvia
#5 Janis Sprukts (1)(PP) Rihards Bukarts, Girgensons 10:24 1st (Slovakia 0-1 Latvia)
#28 Zemgus Girgensons (1)(PP) Rihards Bukarts, Sprukts 7:26 2nd (Slovakia 0-2 Latvia)
#19 Michel Miklik (2)(PP) Dravecky, Hascak 9:08 3rd (Slovakia 1-2 Latvia)
#25 Andris Dzerins (1)(PP) Cibulskis, Daugavins 10:35 3rd(Slovakia 1-3 Latvia)
Canada Vs. Slovenia
#4 Tyson Barrie (1) De Haan 4:30 1st (Canada 1-0 Slovenia)
#29 Nathan MacKinnon (1) Skinner 14:35 1st (Canada 2-0 Slovenia)
#16 Mitch Marner (1) Konecny, Point 16:13 1st (Canada 3-0 Slovenia)
#29 Nathan MacKinnon (2) Giroux 4:43 2nd (Canada 4-0 Slovenia)
#29 Nathan MacKinnon (3)(PP) (hat trick) Marner, Barrie 5:43 2nd (Canada 5-0 Slovenia)
#39 Jan Mursak (1) Sabolic 15:44 2nd (Canada 5-1 Slovenia)
#16 Mitch Marner (2) Konecny, Point 17:11 2nd (Canada 6-1 Slovenia)
#53 Jeff Skinner (1) unassisted 7:07 3rd (Canada 7-1 Slovenia)
#26 Jan Urbas (1) Music 17:52 3rd (Canada 7-2 Slovenia)
Finland Vs. France
#41 Pierre-Eduard Bellemare (1) Rech, S. Da Costa 14:16 1st (Finland 0-1 France)
#4 Mikko Lehtonen (1) Pihlstrom 1:32 2nd (Finland 1-1 France)
#21 Antoine Roussel (1) Bellemare, Claireaux 13:58 2nd (Finland 1-2 France)
#12 Valentin Claireaux (1)(PP) Janil 18:49 2nd (Finland 1-3 France)
#21 Antoine Roussel (2) unassisted 8:27 3rd (Finland 1-4 France)
#9 Damien Fleury (1)(EN) unassisted 17:49 3rd (Finland 1-5 France)
Switzerland Vs. Norway
#19 Reto Schappi (1) Loeffel 12:04 2nd (Switzerland 1-0 Norway)
#89 Cody Almond (1) Rufenacht 13:59 2nd (Switzerland 2-0 Norway)
#44 Pius Suter (1)(PP) Almond, Ambuhl 9:25 3rd (Switzerland 3-0 Norway)
#Sports#Hockey#Goals#National Teams#Russia#Italy#U.S.A.#U.S.#Denmark#Slovakia#Latvia#Canada#Slovenia#Finland#France#Switzerland#Norway
0 notes