#Intraperitoneal bleeding
Explore tagged Tumblr posts
Text
Why Choose Dr. Aditi Bhatt for Ovarian Cancer Treatment Doctor In Ahmedabad?

Just as timely treatment and a proper diet are crucial for managing ovarian cancer, having the right oncology specialist by your side is equally essential. Among the many skilled and experienced ovarian cancer doctors, Dr. Aditi Bhatt stands out.
Based in Ahmedabad, Dr. Aditi Bhatt is a highly respected and reputable oncologist with around 15 years of experience. One of her renowned treatments for ovarian cancer is HIPEC surgery or Hyperthermic Intraperitoneal Chemotherapy. Through this innovative treatment, she has saved the lives of numerous ovarian cancer patients. Her holistic, patient-centred approach addresses each individual’s unique needs, making her a preferred choice for ovarian cancer care.
Ovarian cancer is often diagnosed at an advanced stage, which makes effective treatment all the more important. In this article, we will explore why Dr. Aditi Bhatt is an excellent choice for ovarian cancer doctor in Ahmedabad.
What is Ovarian Cancer?
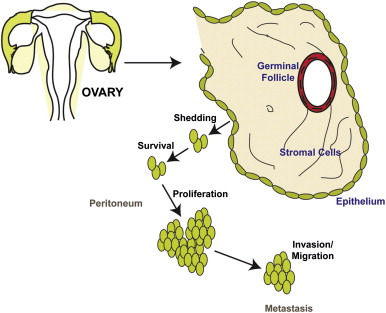
Ovarian cancer is a type of cancer that is mostly detected in the last stage. It is one of the most common cancers that Indian women suffer from. They generally begin in women's reproductive organ ovaries and later, with time, start spreading to other parts of the body. Ovarian cancer is often caused by cells that start growing abnormally. This abnormality leads to tumours. Identifying ovarian cancer in the early stages is quite a difficult task as most of the symptoms of ovarian cancer are so subtle and low-key that they are often confused and misjudged as minor health issues.
Ovarian cancer is segregated into many subtypes like epithelial, germ cells, and stromal ovarian cancer. Depending on the sub-types, symptoms may vary.
Multiple factors are at high risk of causing ovarian cancer. Like age, family history, genetic issues, lifestyle, obesity, menopause, infertility, etc.
How to Check For Ovarian Cancer At Home?
Though it is hard to identify or detect ovarian cancer at an early stage, it is even more difficult to try to detect ovarian cancer at home without prior reports or tests. Though it may seem a difficult task to achieve, there are certain ways in which you can try to identify whether you have ovarian cancer or not.
Firstly, try to see or identify if you have any similar early-stage ovarian cancer symptoms. If you notice a pattern or see consistency in any of the ovarian cancer signs, it is recommended to visit a doctor immediately. Some of the symptoms you may go through:
Feeling persistent pain in the lower abdomen, bloating, loss of appetite, feeling full just after small meals, tiredness, increase in urination, sudden weight loss or weight gain, etc.
Even irregular periods and heavy bleeding can help in early diagnosis. It is suggested to have a pelvic exam, ultrasound, or CA-125 blood test to check for ovarian cancer, as all of these reports are effective in diagnosing ovarian cancer.
Why Choosing the Right Doctor is Crucial?
When you deal with severe health problems like ovarian cancer, it is vital to have someone by your side. The right doctor will help in accurately identifying and diagnosing the type of ovarian cancer you are going through. Moreover, ovarian cancer specialists with years of experience offer advanced treatment facilities that make it easier for fast and effective recovery.
Dr Aditi’s Experience in Treating Ovarian Cancer
Over the 15 years of working, Dr Aditi has treated numerous ovarian patients from early stage to late stage. She is widely regarded for her complex surgeries, including cytoreductive surgery and HIPEC (Hyperthermic Intraperitoneal Chemotherapy). Dr. Aditi also believes in a holistic approach; she thinks a patient’s mental and emotional well-being is above everything else. She takes time to explain every aspect and options patients have in front of them. Moreover, she is also an active member and active participant in learning new cutting-edge technologies.
1: Who is Dr. Aditi Bhatt?
Dr. Aditi Bhatt is a renowned ovarian cancer specialist in ahmedabad with 15 years of experience and is well-known for her complex treatment and surgeries like HIPEC and cytoreductive to treat ovarian cancer. All of this makes her the leading ovarian cancer surgeon in diagnosing and treating ovarian cancer.
2: What makes Dr. Aditi Bhatt an expert in ovarian cancer treatment?
Because of Dr Aditi Bhatt’s specialization and expert knowledge in complex ovarian cancer treatment, she is considered one of the best ovarian cancer surgeons. She is also actively involved in new innovative measures and research to improve ovarian cancer treatment. Her compassionate and patient-centered approach further adds to her reputation, making her a trusted name in ovarian cancer treatment.
3: What are the chances of survival after ovarian cancer surgery?
The survival rate of ovarian cancer is entirely based on several factors like condition, age, treatment effectiveness, and lastly, stage of ovarian cancer. According to data available, about 95% of women can survive more than 5 years if ovarian cancer is detected early, while if ovarian cancer is detected at the last stage (4th), then this survival rate drops to 15%.
0 notes
Text
Ameliorative Effect of Methanolic Extract of Broccoli (BMX) on Diclofenac Sodium (DIC)-Induced Oxidative Damage in Rat Kidney
Introduction: The objective of this study was to investigate the potential protective effect of the methanolic extract of broccoli against oxidative stress induced by diclofenac in rats. Non-steroidal anti-inflammatory drugs (NSAIDs) are known to cause nephrotoxicity, hence the need to explore the therapeutic potential of medicinal plants.
Materials and methods: A total of 48 adult male Wister rats with a maximum age of 2-3 months with an average weight of 220 g were randomly divided into four equal groups (12 in each group The first group was control (C) and fed physiological saline without treatment, the second group was BC which treated with broccoli methanolic extract (BMX) at a dose of 500 mg/kg/Intraperitoneal injection, the third group was DC which treated with diclofenac sodium (DIC, 100 mg/kg, Intra-muscular injection), and the fourth group was BC plus DC which treated diclofenac sodium (100 mg/kg, Intra-muscular injection) and broccoli (500 mg/kg/ Intraperitoneal injection). After blood collection, serum was isolated, and urea, creatinine, interleukin-1, and TNF-α were measured in blood serum. In kidney tissue, malondialdehyde (MDA), superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) were measured. At the end of the study, the samples were taken for histopathological investigation.
Results: The results of the present study indicated that diclofenac sodium causes severe kidney damage. The levels of creatinine and urea showed a significant increase in the DC group compared with the control and other treatment groups. The pro-inflammatory biomarkers in blood serum increased in the DC group and significantly decreased in the BC+DC group compared with control and other treatment groups. These changes were in line with the significant decrease of GPx and CAT enzyme levels in the DC group and its increase in the BC group. Malondialdehyde increased in the DC group and reached its lowest level in the BC group. Hyperemic changes, accumulation of inflammatory cells, and bleeding were indicators of diclofenac tissue poisoning reported in the kidney.
Conclusion: The results of biochemical and histopathological showed that broccoli extract at the dosage of 500 mg/kg with strong antioxidant potential can drama a protective role against diclofenac damage in the kidney.
0 notes
Text
“Roe Lia” (China 1993)
The Department of Forensic Pathology at Tongji Medical University published a report documenting three maternal deaths after legal abortion in Wuhan, China. In all of the cases, maternal death was absolutely preventable. A pseudonym is used here because no real names were given.
Lia was one of the three dead clients killed by her “safe and legal” abortion. She was not given an adequate examination before the abortion. Nobody told Lia that she was in danger, even when the signs were all there. She died of massive intraperitoneal bleeding a few weeks later.
Lia had not been told that she had an ectopic pregnancy, a condition that should have been easily identified by a pre-op examination and ultrasound and by the lack of fetal body parts removed during the abortion. An investigation of cases like this one blamed deaths like hers on a lack of standardized procedures for the adequate monitoring of fetal body parts removed during an abortion and a lack of basic examination.
Studies have shown that the death-to-case rate for ectopic pregnancies concurrent with induced abortion is actually higher than for pregnant people not undergoing abortion. These mothers are typically not given basic examinations before and are sent home to bleed to death.
Archives of Pathology and Laboratory Medicine 117(7): 698-700
https://pubmed.ncbi.nlm.nih.gov/8323431/
#tw abortion#tw murder#abortion debate#abortion#pro life#unsafe yet legal#tw ab*rtion#pro choice#death from legal abortion#unidentified victim
3 notes
·
View notes
Text
Ovarian Cancer
Malignant lesions of the ovaries include primary lesions arising from normal structures within the ovary and secondary lesions from cancers arising elsewhere in the body.
Signs and symptoms
Bloating; abdominal distention or mass
Pressure effects on the bladder and rectum
Constipation, indigestion, reflux
Vaginal bleeding
Shortness of breath, tiredness, weight loss
Diagnosis
Physical findings are uncommon in early stages. Advanced disease may present with ovarian or pelvic mass, ascites, pleural effusion, or abdominal mass or bowel obstruction.
Pathophysiology
Typically spreads to the peritoneal surfaces and omentum.
Occurs via local extension, lymphatic invasion, intraperitoneal implantation, hematogenous dissemination, or transdiaphragmatic passage.
Malignant cells can implant anywhere in the peritoneal cavity but are more likely to implant in sites of stasis along the peritoneal fluid circulation.
Epithelial tumours make up 90% of ovarian tumours. Other histologies include:
Sex-cord stromal tumors
Germ cell tumors
Primary peritoneal carcinoma
Metastatic tumors of the ovary
Epithelial ovarian cancer
Arises from epithelium covering the fimbria of the fallopian tubes, or the ovaries, both of which are derived from the coelomic epithelium.
Found primarily as cystic lesions with solid components.
Surface may be smooth or covered in papillary projections.
Cysts contain fluid from yellow to brown and haemorrhagic.
Four main histologic subtypes:
Serous (from fallopian tube)
Endometrioid (endometrium)
Mucinous (cervix)
Clear cell (mesonephros)
Tumours of low malignant potential
Tumours of low malignant potential (LMP) are a variety of much less aggressive epithelial ovarian cancer, with good prognosis.
LMP tumors can cause a range of symptoms similar to epithelial ovarian cancer, including increasing abdominal girth, an abdominal mass, abdominal pain, abnormal uterine bleeding, urinary symptoms, and gastrointestinal symptoms. They may be asymptomatic and found on routine physical examination or ultrasound scan.
#cancer#oncology#gynecology#ovarian cancer#ovaries#pathology#science#medblr#studyblr#sciblr#medschool#premed#nursing#medicine#biology#human biology#notes#2
162 notes
·
View notes
Text
oncologist surgeon in Hyderabad – umacancercenter
The Oncologist who are dedicated to save lives
The branch of medicine that deals with researching, identifying, and treating cancer is referred to as oncology. A physician who is associated with the field of oncology is called an Oncologist. Dr. Madhu Devarasetty is one of the most renowned oncologist surgeon in Hyderabad, who is associated with Uma cancer center.
In the first step of treatment, the oncologist diagnoses a person with cancer; they do it by performing a biopsy, endoscopy, X-ray, C T scanning, PET scanning, MRI, ultrasound, and other radiology methods.
There is an increasing concern for cancer; very few cancer hospitals provide affordable treatment to patients with great care.
There are three main divisions of oncology, and depending upon the stage of cancer, the nature, and the location of cancer, there are many oncologists.
Medical Oncologist
A medical oncologist is a doctor who treats patients who have cancer. They administer chemotherapy and other medications such as immunotherapy.
The medical oncologist treats all kinds of cancer that originate in different parts of the body.
While administering chemotherapy, the doctors use drugs that kill the cancer cells and leave the patient’s cell unharmed.
Despite the recent advancements in the field, chemotherapy has side effects that are visible on the body of the patients. The significant side effects include nausea, hair loss, weakness, fatigue, loss of appetite, fever, diarrhoea, mouth sores, and prone to bruise and bleed.
Surgical oncologist
This particular oncologist focuses on using surgery to diagnose, staging, and then surgically remove the cancer cell from the affected part of the body.
The possibility of going under surgery depends on the stage, size and location of cancer. The patient’s age and physical fitness is also a factor.
A few of the surgical procedures in oncology include appendectomy; in this procedure, the appendix is removed as it swells due to infection and causes irritation and inflammation.
In bowel resection, doctors surgically remove the colorectal tumours, surrounding tissues and lymph nodes.
Hyperthermic intraperitoneal chemotherapy is administered directly to the abdomen to kill the cancer cells. Before the patients receive the treatment, the doctors perform cytoreductive surgery to remove the tumours.
Pneumonectomy
A surgery that consists of removing an entire lung to treat non-small cell lung cancer, tuberculosis and chronic obtrusive pulmonary disease. Pneumonectomy is invasive and complex surgery.
It takes experienced and accomplished doctors to perform this surgery, and the medical team of Uma hospital prides itself to have a few brilliant oncologist surgeon in Hyderabad.
Radiation Oncologist
Radiation oncologists are those doctors who administer radiation therapy to treat cancer. In radiation therapy, the doctors use high-energy x-rays to eliminate the cancerous cells.
When it becomes difficult to destroy the cells, the doctors use radiation therapy as a procedure to slow down the growth of the tumour. This particular method is also called palliative therapy; its primary goal is to control tumour growth and its lingering effects.
Radiation oncologists also use another procedure called brachytherapy. The radioactive agents are directly placed next to the tumour; they can be removed after the treatment session or not, but it depends on the type of cancer that the patient has.
Gynecologic oncologist
Gynecologic oncologists are specialized doctors who treat the cancers that occur in the female reproductive system.
This category treats ovarian cancer, cervical cancer, uterine cancer, vaginal cancer, and vulvar cancer.
Different surgeries are performed pertaining to other parts of the female reproductive system.
For instance, optimal debulking surgery is employed to treat ovarian cancer, including peritoneal biopsies, abdominal hysterectomy, omentectomy, oophorectomy, lymph node sampling, etc.
Pediatric oncologist
Certain cancers affect children significantly, and pediatric oncologists specialize in this field to rid young children of the disease. Leukaemia, brain tumours, osteosarcoma are some of the cancers that affect children from a young age to adolescence.
A highly efficient team of accomplished doctors happens to be headed by an excellent oncologist surgeon in Hyderabad at Uma cancer centre.
#oncologist surgeon in hyderabad#Surgical Oncologist in Hyderabad#Best Surgical Oncologist in Hyderabad#Best Cancer Hospital in Hyderabad#Best Cancer Doctor in Hyderabad
1 note
·
View note
Text
What is the difference between a tubal pregnancy and an ectopic pregnancy?
In ectopic pregnancy, implantation occurs in a site other than the endometrial lining of the uterine cavity, i.e., in the fallopian tube, horn of the uterus, cervix, ovary, or abdominal or pelvic cavity. Ectopic pregnancies cannot be carried to term and eventually rupture or involute.
Early symptomatology includes pelvic pain, metrorrhagia, and tenderness to the vaginal touch, especially when the cervix is displaced.
Syncope or hemorrhagic shock may occur upon rupture. Diagnosis is based on beta-hCG measurement and pelvic ultrasound. Treatment consists of laparoscopic or open surgical resection or IM methotrexate injection.
The incidence of ectopic pregnancy is approximately 2/100 diagnosed pregnancies.
Etiology of ectopic pregnancy
Factors that particularly increase the risk of ectopic pregnancy include
Tubal lesions
A history of ectopic pregnancy (risk of recurrence 10-25%)
History of pelvic inflammatory disease (especially Chlamydia trachomatis)
Previous abdominal surgery especially on the fallopian tubes, including tubal ligation
Other specific risk factors for ectopic pregnancy include
Intrauterine device (IUD) contraception
Infertility due to tubal damage
Smoking
History of induced abortion
Pregnancy is less likely to occur when an intrauterine device (IUD) is in place; however, about 5% of these pregnancies are ectopic.
Pathophysiology of ectopic pregnancy
The most common location of ectopic pregnancies is the fallopian tube, followed by the uterine horn. Cervical pregnancies, in a caesarean scar, the ovary, the abdomen or the interstitium of the fallopian tube are rare.
( You can follow your Pregnancy & Baby Tracker Pro week by week )
Heterotopic pregnancies (both ectopic and intrauterine) occur in only 1/10,000 to 30,000 pregnancies, but may be more common among women who have used ovulation induction or assisted reproductive technologies such as in vitro fertilization and gamete intrafallopian tube transfer (GIFT); in such cases, the reported rate of ectopic pregnancies is ≤ 1%.
The structure containing the fetus usually ruptures after 6 to 16 weeks. Rupture results in hemorrhage that may be progressive or rapid enough to cause hemorrhagic shock. Intraperitoneal blood irritates the peritoneum. The later the rupture, the more rapid the bleeding and the higher the mortality.
Symptomatology of ectopic pregnancy
Symptoms of ectopic pregnancy vary and are often absent until rupture occurs. Most patients present with pelvic pain (sometimes in the form of cramping) and/or vaginal bleeding. There may or may not be a delay or absence of menstrual bleeding, and the patient may not know that she is pregnant.
Rupture may be heralded by sudden severe pain, followed by syncope or symptoms of hemorrhagic shock or peritonitis. Rapid hemorrhage is more likely in ruptured ectopic pregnancies.
Pain on mobilization of the cervix, unilateral or bilateral adnexal tenderness on vaginal touch, or an adnexal mass may be present. The uterus may be slightly enlarged (but less than expected from delayed menstruation).
Diagnosis of ectopic pregnancy
Quantitative serum human chorionic gonadotropin beta subunit (beta-hCG)
Pelvic ultrasound
Sometimes laparoscopy
An ectopic pregnancy is suspected in any woman of childbearing age with pelvic pain, metrorrhagia, or unexplained syncope or hemorrhagic shock, regardless of contraceptive use, sexual intercourse, or delayed menses. The results of physical examinations (including pelvic touch) are neither sensitive nor specific.
A ruptured ectopic pregnancy is a surgical emergency because it causes maternal hemorrhage with a risk of death; prompt diagnosis is essential.
The first step is a urine pregnancy test, which is nearly 99% sensitive in diagnosing pregnancies (ectopic and others). When the urine beta-hCG test is negative and the clinical signs are not strongly suggestive of ectopic pregnancy, further testing is unnecessary unless the symptoms recur or worsen.
If the urine beta-hCG is positive or the clinical signs are strongly suggestive of ectopic pregnancy, a quantitative serum beta-hCG measurement and pelvic ultrasound are not indicated.
When the quantitative serum beta-hCG is < 5 mIU/mL, ectopic pregnancy is excluded. When ultrasound detects an intrauterine gestational sac, an ectopic pregnancy is highly unlikely except in the woman who has used assisted reproductive techniques (which increases the risk of heterotopic pregnancy); however, a cornual or intra-abdominal pregnancy may initially present as an intrauterine pregnancy.
Ultrasound images suggestive of an ectopic pregnancy (seen in 16 to 32%) of cases include complex masses (mixed solid and cystic masses), particularly in the adnexa, and fluid effusion from the cul-de-sac of Douglas.
If the serum beta-hCG is above a certain level (called the discriminatory zone), the ultrasound should detect a gestational sac in case of intrauterine pregnancy. This level is usually about 2000 mIU/mL. If the beta-hCG level is above the discriminatory zone and no intrauterine gestational sac is detected, an ectopic pregnancy is likely. The use of the transvaginal route or color Doppler can improve detection rates.
If the beta-hCG level is below the discriminatory zone and the ultrasound is negative, it may be an early intrauterine pregnancy or an ectopic pregnancy. If the initial clinical workup suggests an ectopic pregnancy (e.g., significant peritoneal irritation or hemorrhage), diagnostic laparoscopy may be necessary for confirmation.
When an ectopic pregnancy appears unlikely and the patient is stable, plasma beta-hCG levels can be monitored on an outpatient basis (typically every 2 days). Normally, the level doubles every 1.4 to 2.1 days until day 41; in an ectopic pregnancy (as in non-progressive pregnancies), levels may be lower than expected and do not double as rapidly.
If the beta-hCG level does not rise as expected or falls, the diagnosis of spontaneous miscarriage or ectopic pregnancy should be considered.
#pregnant kink#pregnancy#make me huge#huge pregnant belly#belly movement#squirming#preggolife#pregnant#pregnant women#pregnantbeauty#pregnantbelly#big belies#mother#sexy belly#long post#multiples#vintage preg#progress#shes so round#twins
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Fournier Gangrene, Empyema and Retroperitoneal Abscess as a Rare Complication of Perforated Appendicitis: A Case Report
Authored by Emad Aljohani
Abstract
Background: Perforated appendicitis which may be associated with the formation of localized abscess in the right iliac fossa or in the pelvic cavity, can be managed depending on their symptoms. Retroperitoneal abscess is a life-threatening condition because of its clinical manifestations and diagnostic difficulty. The retroperitoneal abscess has the potential to spread rapidly to the perinephric space, the psoas muscle, the lateral abdominal wall, and the lower extremities.
Case presentation: We present a 39 years old patient who presented to the emergency room with empyema and retroperitoneal abscess which managed conservatively with percutaneous drainage and Intravenous antibiotics. After couple of days of observation, he developed Fournier gangrene which managed by surgical debridement. CT scan on the follow up showed intraabdominal collection, emergency exploratory laparotomy along with appendectomy and washout performed. Postoperatively the patient developed perineal wound bleeding which controlled surgically. Afterwards he became severely septic, requiring maximum ionotropic support. Eventually he died due to irreversible septic shock and multiorgan failure.
Conclusion Perforated appendicitis can present with variety of complications. To the best of our knowledge from the literature review, this is the first case to be reported as Fournier gangrene, empyema and retroperitoneal abscess as unusual complication of perforated appendicitis.
Keywords: Perforated appendicitis; Fournier gangrene; Empyema; Retroperitoneal abscess
Introduction
Acute appendicitis is a disease commonly encountered in daily practice, and a very low morbidity and mortality rate can be achieved with proper diagnosis and management at present. Generally, a non-perforated acute appendicitis can be managed by urgent appendectomy, while perforated appendicitis which may be associated with the formation of localized abscess in the right iliac fossa or in the pelvic cavity, can be managed depending on their symptoms either by early appendectomy or by interval appendectomy following percutaneous drainage [1]. Retroperitoneal abscess is still recognized as a life-threatening condition even today because of its insidious clinical manifestations and diagnostic difficulty. Via congenital anatomical communications, the retroperitoneal abscess has the potential to spread rapidly to the perinephric space, the psoas muscle, the lateral abdominal wall, and the lower extremities [2]. An empyema is the result of the accumulation of infected fluid in the pleural space. Most frequently, it occurs due to infection spread by contiguity of intrathoracic disease (pneumonia, mediastinitis, etc.). The secondary infection due to intra-abdominal pathology is less common. In the absence of lung disease or other intrathoracic focus, intra-abdominal origin should be considered [3]. To date, there are no case reports documenting Fournier gangrene, empyema and retroperitoneal abscess as unusual complication of perforated appendicitis.
Presentation of Case
39 years old Eritrean male presented to the emergency department complaining of severe abdominal pain and vomiting for ten days. The patient looked sick, dehydrated, with tachycardia, tachypnea, and febrile on examination. His abdomen was soft with tenderness over the right iliac fossa. He had scrotal swelling, but wasn’t tender nor erythematous. However, DRE was unremarkable. His WBC was 15.9 (109/L). Other labs were within an acceptable range. A chest x-ray showed the presence of an air-filled cavity within the pleural cavity of the right lung (Figure 1). His abdominal x-ray showed the presence of extra-peritoneal air on the right side of the abdomen (Figure 2). After proper resuscitation, chest, abdomen, and pelvis Computed Tomography (CT) scan done. It showed a large right flank collection with multiple peritoneal fat fluid pockets and gas bubbles with a right chest empyema (Figure 3). The patient admitted and started on IV broad-spectrum antibiotics. Chest and flank percutaneous drainage performed by intervention radiology. Upon insertion of the chest and flank pigtails, a total of 60 and 700 milliliters of frank pus drained, respectively. He was shifted to the ward under observation.
The patient improved gradually, both clinically and biochemically. However, on the fourth day of his admission, his WBC increased from 9 to 30 (109/L). A thorough examination was carried out, which showed the presence of scrotal swelling, which was erythematous, warm, and tender to touch. Urgent Pelvis CT was done, and it showed the presence of gas within the soft tissues with fat stranding in the scrotum. Therefore, extensive debridement of the scrotal Fournier Gangrene was done. The patient was then shifted to the ward with daily dressing and IV antibiotics plan. Cultures showed growths of Escherichia Coli and Proteus Mirabilis, and blood culture was positive for Escherichia Coli. Infectious Diseases consulted to guide the course of antibiotics, and they opted to start Meropenem, Vancomycin, and Caspofungin. Also, HIV, Hepatitis B, and Hepatitis C screening tests were all negative.
A couple of days later, CT scan were repeated to follow the chest and retroperitoneal abscesses. It showed an interval decrease in the size of the chest abscess and increase in the size of the retroperitoneal abscess with the finding of an intraabdominal collection, which is communicating with the retroperitoneal abscess. The decision was made to take the patient to the operating room on the 12th day after admission for exploratory laparotomy. Intra-operatively, there were more than two liters of yellowish free fluid found intraperitoneally. The appendix found to be perforated with fecal matter expelled into the abdominal cavity. Thorough irrigation was done after conducting an appendectomy. The patient shifted back to the ward, where he was followed daily for dressing changes over the perineal wound.
On the second day postoperatively, the patient suddenly became septic and hemodynamically unstable. He was shifted to the ICU, which he required ionotropic support. During ICU stay developed bleeding through the perineal wound. Angiography was done to control the bleeder, which failed in localizing a bleeder. For this reason, shifted to Operating Room for bleeding control, and multiple sutures taken over the multiple small bleeders with an application of hemostatic agents. The patient was taken back to the ICU for further supportive care. Unfortunately, the patient started deteriorating the following day with increasing lactic acid levels, and the diagnosis of bowel ischemia was suspected. An abdominal CT scan was done, which showed findings suggestive of non-occlusive ischemic colitis. In the next days, the patient started deteriorating rapidly and has eventually died due to irreversible septic shock and multiorgan failure.
Discussion
Acute appendicitis is the most common abdominal emergency worldwide, and its surgical treatment is simple and effective, resulting in full recovery without adverse consequences in most cases. One of the most serious complications of acute appendicitis is retroperitoneal abscess, which can be difficult to diagnose and manage because of its insidious onset and cause [2].
The CT-diagnosed accuracy rate of retroperitoneal abscess approached 100%. This feature is consistent with the current series in which CT scan was used as the diagnostic tool of choice. However, it should be noted that even though CT can show a retroperitoneal abscess clearly, it is still problematic to identify a perforated appendix, as a correct diagnosis of perforated appendicitis was made in only 5 of 12 patients who underwent CT. This is probably because the severe inflammatory process made the appendix become necrotic and indistinguishable from abscess on the CT scan [4].
Our patient had retroperitoneal perforated appendicitis with significant dissemination of the infection to the chest, perineum and retroperitoneum. He was treated initially with conservative management with drainage of the chest empyema, and retroperitoneum collection. On the follow up CT scan found to have scrotal Fournier Gangrene which required emergency extensive debridement. On follow up CT scan an abdominal collection along with increasing retroperitoneal collection. Exploratory laparotomy, appendectomy and washout performed and shifted to the floor. Post operatively the patient shifted to the ICU as he became septic and during the ICU stay, he developed perineal wound bleeding which can’t be controlled by angiography but surgical bleeding control succeeded. He deteriorated postoperatively, CT done and showed non-occlusive bowel ischemia due to the high requirement of the ionotropic support. Eventually he developed multiorgan failure and died.
In summary, we report rare presentation retroperitoneal perforated appendicitis extending to the chest and perineum. Up to our knowledge from the literature review this is the first case report to be reported as retroperitoneal perforated appendicitis with empyema and Fournier Gangrene.
Conclusion
An empyema or lung abscess caused by an abdominal infection is a rare entity, especially as consequence of acute appendicitis. However, when a retroperitoneal infection is established, it may eventually compromise the thoracic cavity by contiguous spread. The formation of complicated retroperitoneal abscess involving the thigh, psoas muscle, perinephric space, and even the lateral abdominal wall is well recognized as a serious complication of perforated acute appendicitis. In conclusion, perforated acute appendicitis can occasionally manifest as complicated retroperitoneal abscess without remarkable abdominal symptoms; thus, it is necessary to maintain a high index of suspicion in a patient with symptoms of retroperitoneal infection. CT scan should be obtained to evaluate the possible origin and extent of the infection.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#Juniper Publishers#juniper publishers contact info#Biochemistry#Cytology#Emergency Medicine#Infectious Diseases#Obstetrics and Gynaecology
0 notes
Text
12 Things To Know Before Starting Chemotherapy

Cancer can cause a number of unexpected medical complications for patients, making it deadly. Many people have heard of chemotherapy and know it's a set of treatment cycles that uses drugs to treat and can help eventually beat cancer. However, most people still don't have any medical understanding or information about cancer and its adverse effects. In addition, there are a number of types of chemotherapy treatment cycles and other types of cancer therapy. The type of chemo for a patient used by their oncology doctors and their team depends on what might work best for the particular cancer diagnosis, its side effects, and its medical information. Read on for twelve things you should learn about chemotherapy treatment cycles for better understanding before you or your loved ones begin cancer treatment.
1. How is Cancer formed?
The body is composed of trillions of healthy human cells. Cancer begins when something triggers changes in a normal cell. This cancer cell then grows out of control and creates more cancer cells. Each kind of cancer can affect the body in adverse ways. If cancer is not treated in time, it can spread to the rest of your body and cause life-threatening complications. Your oncology doctor and the team may give chemo drugs to help treat your cancer. Often chemotherapy is used to slow down the spread of cancer. Sometimes the treatment goal is given to alleviate symptoms or problems caused by growing cancer tumors. It can be used to improve health.
2. What is Chemotherapy?
Chemotherapy is the use of a number of potent drugs for cancer diagnosis and treatment including ovarian and breast cancer. Chemotherapy is sometimes called "chemo" because of the same combination of cancer medication used. During the 1950s Chemo was first used to help treat cancer. Chemo has made it possible for many people to live a healthy life. An oncology doctor's given chemo drugs have been tested several times to see if they work before they are used for patients. Chemotherapy treatment cycles and radiation therapy is used to help treat cancer cells. It has made it possible for many people to live cancer-free.
3. How are Chemo drugs chosen?
Today more than 100 chemo drugs are given in treatment and they work to help treat cancer. Using the drug information, oncology doctors and specialty teams choose the best medications or chemo substance depending on the type of cancer that you have and its stage (how much cancer is in your body). This can be used by combining chemo drugs for different purposes. Before you begin cancer treatments and a radiation therapy cycle your doctor will give this treatment information to you.
4. How does Chemo help with my Treatment Goals?
Oncology doctors and professionals make use of the best Chemo drug combinations and radiation therapy to help treat cancers including ovarian and breast cancer that have metastasized. Metastasized means cancer that has spread to other parts of the body. Be sure to talk to your oncology doctors about the goal of your treatment and get all the information regarding side effects. The drug combinations given can also have a possible effect on normal cells too. But most normal cells are used to repairing themselves so the good outweighs the bad.
5. How is Type of Chemotherapy Determined for Treatment?
Your complete cancer treatment procedure options to be used will be determined by a few factors. The type of cancer you have, the stage at which you have been diagnosed, whether or not you have received chemotherapy treatment or radiation therapy before, and your personal health history. If the cancer is metastatic, you may not get the type of chemo commonly given through an IV. This treatment is called infusion chemo. For metastatic cancer, Chemotherapy pills that have a particular drug combination are given and must be taken every day, and you only have to visit the hospital once a month to receive an injection. This drug combination injection given is used to enhance healthy bone growth since the metastasized cancer might be attacking your bones.
6. How is Chemotherapy Used?
The oncology team will give Chemotherapy treatments for cancer in many ways including orally, topically, intravenously using IV drips, through injections, intra-arterial administrations, and intraperitoneal administrations. The final treatment and drug combination will be decided by your oncology team.
7. How Often Will I Get Chemotherapy?
How often you undergo chemotherapy treatment varies widely, factors depending on the cancer diagnosis, the form of chemotherapy, the cancer treatment objectives, and other factors. This may be constant or it may alternate with rest periods in between depending on the cancer treatment plan and drug combination as determined by the oncology doctor.
8. What Will Chemotherapy Feel Like?
What you feel when you get chemotherapy treatment depends on a variety of factors including the form of chemotherapy the oncology team gives you, the cancer diagnostic level, the history of personal health, and the capacity of the patient to cope with the symptoms. Symptoms can be noticeable for certain people and other symptoms can take days or even weeks to develop. Typical chemotherapy treatment side effects include fatigue and nausea. In others, these are short bouts from which they can easily recover and for others, the symptoms may last longer. Managing your symptoms and health at your own pace is crucial, and ensure that you take care of yourself during cancer treatment. There is no reason to worry as your oncology team will help you.
9. Not all Chemo Drugs cause Hair Loss
If your oncology team gives you an infusion chemo cycle, you will have to go to the hospital for just a few hours of chemo treatment. Following this, you may have a few days of side effects. Side effects depend on factors like drug or combination of drugs you get, some may not cause hair loss. Side effects regarding your health vary and include aches and pains, nausea and vomiting, diarrhea, hair loss, and other factors. You may have mouth sores for certain medications and loss of appetite, taste, smell, or all three. It's pretty rough to endure, but believe that chemo will do its job and will help you become healthy. This mindset will make you face cancer treatments bravely.
10. Feeling Uneasy is Normal
You'll most likely wake up in the morning on the first day of chemo with anxiety in the heart because you're not sure what's to come. Take a book, a newspaper, your knitting, or any favourite hobby to help you pass the time and keep your mind off it. Having chemo via an IV normally takes a long time. Remind yourself that it is for the sake of your health and undergo your treatment.
11. Always Ask the “What if” Questions
An underlying or secondary disorder may cause severe harm. So don’t hesitate to inform your doctor about your health history. Ask professionals and learn about how particular types of cancer treatment might work to affect you. Ask for the reason when something is done. You can help avoid some unnecessary pain and unwanted treatments if you question your doctor about each step of the treatment given. For example, if you suffer from an underlying bleeding condition. It can cause the hand-foot syndrome, a rare side effect. This can lead to slow leakage of blood from the hands and feet from the tiny capillaries which will soon develop into severe bleeding. As a result, you may have to stay in the hospital longer.
12. Can Chemotherapy make me Cancer free?
If surgery was done to remove a cancerous tumor, such as a lumpectomy for breast cancer, or hysterectomy for ovarian cancer, your oncology specialist may give chemotherapy drugs in cycles, and radiation therapy is given to make sure that any leftover cancer cells are eliminated too. Chemotherapy is also given for making you ready for other types of cancer treatments. It is sometimes given to treat a cancer tumor so it can be surgically removed. Different types of chemo drugs are also given for making you prepared for radiation therapy. During late-stage cancer treatment, chemotherapy drugs are used to alleviate pain.
Conclusion
Chemo may be an inevitable part of your cancer treatments so stock up on healthy and whole foods. Keep yourself hydrated. It can help ease some side effects. So have plenty of low-sugar drinks or juice on hand. Be prepared with frozen meals or book a meal delivery service because you may not feel up to cooking after chemo treatment. Snack on fruits, vegetables, and healthy high-protein food like yogurt. Give yourself time to recuperate and learn your limits. Reach out to an understanding family member or friend to help when your side effects become difficult to manage. There is no reason to undergo it alone.
0 notes
Text
300+ TOP LARGE INTESTINE Objective Questions and Answers
LARGE INTESTINE Multiple Choice Questions :-
1. Which answers are true? In contrast to ulcerative colitis, Crohn's disease of the colon: A. Is not associated with increased risk of colon cancer. B. Seldom presents with daily hematochezia. C. Is usually segmental rather than continuous. D. Has a lower incidence of perianal fistulas. E. Never develops toxic megacolon. Answer: BC 2. Which answers are true? Options to consider when operating for Crohn's disease of the large intestine include: A. Colectomy and ileorectostomy. B. Colectomy, closure of the rectal stump, and ileostomy. C. Colectomy and continent ileostomy (Kock pouch). D. Proctocolectomy and ileostomy. E. Proctocolectomy and ileal pouch–anal canal anastomosis. Answer: ABD 3. Crohn's disease: A. Is caused by Mycobacterium paratuberculosis. B. Is more common in Asians than in Jews. C. Tends to occur in families. D. Is less frequent in temperate climates than in tropical ones. E. Is improved by smoking. Answer: C 4. Recurrence after operation for Crohn's disease: A. Occurs after operations for ileal Crohn's but not colonic Crohn's. B. Is usually found just proximal to an enteric anastomosis. C. Rarely requires reoperation. D. Occurs in 1% of patients at risk per year during the first 10 years after the operation. E. Is prevented by maintenance therapy with corticosteroids. Answer: B 5. Excision rather than bypass is preferred for surgical treatment of small intestinal Crohn's because: A. Excision is safer. B. Bypass does not relieve symptoms. C. Excision cures the patient of Crohn's disease but bypass does not. D. Fewer early complications appear with excision. E. The risk of small intestine cancer is reduced. Answer: E 6. Which statements about anorectal Crohn's disease are true? A. It may be the only overt manifestation of Crohn's disease. B. It accompanies large intestine Crohn's more often than small-intestine Crohn's. C. It subsides when associated small intestinal Crohn's is excised. D. It should not be treated operatively. E. It may subside in response to metronidazole, 250 mg. q.i.d. Answer: ABE 7. The most common indication for operation in Crohn's disease of the colon is: A. Obstruction. B. Chronic debility. C. Bleeding. D. Perforation. E. Carcinoma. Answer: B 8. Which of the following statements about surgical anatomy of the colon and rectum is/are correct? A. The cecum has the largest inner diameter of all segments of the colon (13 to 15 cm.). B. The rectosigmoid junction is situated at approximately 15 to 18 cm. from the anus. C. The rectum is entirely an intraperitoneal organ. D. The ileocolic, right colic, and middle colic arteries are branches from the inferior mesenteric artery. E. The arterial arcade created by communicating vessels at 1 to 2 cm. from the mesenteric is called the artery of Drummond. Answer: BE 9. Which of the following statements about surgical procedures on the colon and rectum is/are correct? A. Successful healing of colonic anastomoses depends on the adequacy of the blood supply. B. In excising part of the colon containing cancer, the lymphatics should be avoided by dividing the mesentery close to the wall of the colon. C. Despite complete removal of the colon and rectum, transanal fecal flow can be preserved by means of an ileal pouch–anal anastomosis. D. When a colostomy is created it cannot be reversed. E. Colostomy can be life saving in patients with colonic perforation or obstruction. Answer: ACE 10. Which of the following statements about colon physiology is/are correct? A. Colonic recycling of urea is accomplished by the splitting of urea by bacterial ureases. B. Fermentation by colonic bacteria may rescue malabsorbed carbohydrates. C. The preferred fuel of the colonic epithelium is glucose. D. Absorption by the colonic mucosa is a passive process. E. Insoluble fibers create bulk in the stool. Answer: ABE

LARGE INTESTINE Objective Questions 11. Which of the following statements about colonic motility is/are true? A. Mass contractions involve only the rectum. B. “Antiperistaltic” contractions occur in the descending colon. C. The rectum can accommodate stool by receptive relaxation. D. Stool in the colon is propelled by tonic contractions. E. Defecation involves both sensory and motor pathways. Answer: ADE 12. Which of the following statements about diagnostic studies for the colon and rectum is/are true? A. Acetylcholinesterase staining of rectal biopsies is unreliable for the diagnosis of Hirschsprung's disease. B. Cinedefecography is useful for detecting “hidden” prolapse or rectal intussusception. C. A negative osmotic gap in stool is indicative of secretory diarrhea. D. A colonic transit time study involves serial abdominal x-rays after ingestion of radiopaque markers. E. Carcinoembryonic antigen (CEA) is useful for monitoring patients after resection for colon cancer. Answer: BCDE 13. Which of the following statements about anorectal functional testing is/are true? A. Anorectal manometry is often performed through open-tipped multilumen catheters perfused with fluid. B. Anorectal manometry can differentiate between segmental and global defects of the anal sphincter in patients with incontinence. C. Electromyography can demonstrate persistent contraction of the pubis rectalis muscle during defecation, which is diagnostic of paradoxical pelvic floor contraction. D. Measurement of sensory thresholds may reveal insensitivity in patients with chronic constipation. Answer: ABCD 14. Which of the following statements about the microbiology of the colon is/are true? A. The colon contains no more bacteria than the stomach. B. The predominant bacteria in the colon are aerobic. C. Nearly one third of the dry weight of feces is bacteria. D. Common bacteria in the colon are Bacteroides, Bifidobacterium, and Enterobacterium species. E. The colonic microflora is relatively stable. Answer: CDE 15. Which of the following statements about bowel preparation for colon surgery is/are true? A. Bowel preparation is accomplished by a combination of mechanical cleansing and nonabsorbable antibiotics. B. Three days of clear liquids provides sufficient mechanical cleansing. C. Commercial electrolyte-polyethylene glycol solutions provide mechanical cleansing without inducing electrolyte imbalance. D. Nonabsorbable antibiotics such as neomycin and erythromycin base are administered the day before the operation in three doses. E. Intravenous antibiotics are also administered the day before surgery. Answer: ACD 16. Which of the following patients generally does not require surgical intervention as a consequence of acute diverticulitis? A. A 35-year-old man with no history of diverticulitis. B. A 68-year-old man status 2 weeks post–renal transplantation. C. A 55-year-old woman with hypertension and diabetes mellitus. D. A 50-year-old man with pneumaturia. E. A 46-year-old man with right-sided diverticulitis. Answer: C 17. The test with the highest diagnostic yield for detecting a colovesical fistula is: A. Barium enema. B. Colonoscopy. C. Computed tomography (CT). D. Cystography. E. Cystoscopy. Answer: E 18. Which of the following is not true of diverticular disease: A. It is more common in the United States and Western Europe than in Asia and Africa. B. A low-fiber diet may predispose to development of diverticulosis. C. It involves sigmoid colon in more than 90% of patients. D. Sixty per cent develop diverticulitis sometime during their lifetime. E. It is the most common cause of massive lower gastrointestinal hemorrhage. Answer: D 19. The most common indication for surgery secondary to acute diverticulitis is: A. Abscess. B. Colonic obstruction. C. Colovesical fistula. D. Free perforation. E. Hemorrhage. Answer:A 20. Which of the following is/are true about colorectal polyps? A. Familial juvenile polyposis is associated with an increased incidence of colon cancer. B. Although the propensity for development of malignancy is related to the size of a neoplastic polyp, those with mixed tubulovillous histologic appearance are most likely to develop malignant changes. C. The loss of a single tumor suppressor gene such as p53 is sufficient to lead to the development of malignancy in colorectal neoplastic polyps. D. Endoscopic polypectomy results in a decreased incidence of carcinomas of the colon and rectum. Answer: AD 21. Which of the following statements about familial adenomatous polyposis (FAP) is/are true? A. Inherited in an autosomal-dominant manner, this genetic defect is of variable penetrance, some patients having only a few polyps whereas others develop thousands. B. The phenotypic expression of the disease depends mostly on the genotype. C. Appropriate surgical therapy includes total abdominal colectomy with ileorectal anastomosis and ileoanal pull-through with rectal mucosectomy. D. Panproctocolectomy with ileostomy is not appropriate therapy for this disease. E. Pharmacologic management of this disease may be appropriate in some instances. Answer: C 22. Which of the following statements about the etiology of chronic ulcerative colitis are true? A. Ulcerative colitis is 50% less frequent in nonwhite than in white populations. B. Psychosomatic factors play a major causative role in the development of ulcerative colitis. C. Cytokines are integrally involved in the pathogenesis of ulcerative colitis. D. Ulcerative colitis has been identified with a greater frequency in family members of patients with confirmed inflammatory bowel disease. E. Ulcerative colitis is two to four times more common in Jewish than in non-Jewish populations. Answer: ACDE 23. Surgical alternatives for the treatment of ulcerative colitis include all of the following except: A. Colectomy with ileal pouch–anal anastomosis. B. Left colectomy with colorectal anastomosis. C. Proctocolectomy with Brooke ileostomy or continent ileostomy. D. Subtotal colectomy with ileostomy and Hartmann closure of the rectum. Answer: B 24. The initial management of toxic ulcerative colitis should include: A. Broad-spectrum antibiotics. B. 6-Mercaptopurine. C. Intravenous fluid and electrolyte resuscitation. D. Opioid antidiarrheals. E. Colonoscopic decompression. Answer: AC 25. Which finding(s) suggest(s) the diagnosis of chronic ulcerative colitis as opposed to Crohn's colitis? A. Endoscopic evidence of backwash ileitis. B. Granulomas on biopsy. C. Anal fistula. D. Rectal sparing. E. Cobblestone appearance on barium enema. Answer: A 26. An 80-year-old man who has been bedridden for many years following a stroke presents with acute onset of abdominal distention, obstipation, and colicky abdominal pain. Abdominal x-rays reveal dilated loops of small bowel and a dilated sigmoid colon resembling a bent inner tube. Examination reveals distention with mild direct tenderness but no rigidity or rebound tenderness. Initial management should consist of: A. Barium enema examination. B. Laparotomy with resection of descending colon and descending colostomy. C. Multiple cleansing enemas to remove impacted feces. D. Rigid sigmoidoscopy and decompression of the sigmoid colon. Answer: D 27. Axial twisting of the right colon or cecal volvulus has been shown to be associated with each of the following except: A. A history of abdominal operation. B. A mobile cecum. C. An obstructing lesion in the transverse or left colon. D. Inflammatory bowel disease. Answer: D 28. Sigmoid volvulus has been associated with each of the following except: A. Chronic constipation and laxative abuse. B. Chronic rectal proplapse. C. Chronic traumatic paralysis. D. Medical management of Parkinson's disease. Answer: B 29. Which of the following statements is not true about inhereted susceptibility to colon cancer? A. There is no known genetic susceptibility to colon cancer. B. There are known genetic susceptibilities to colon cancer, but they are always associated with multiple adenomatous polyps. C. There are known genetic susceptibilities to colon cancer, but they are always associated with specific ethnic or racial groups. D. None of the above. Answer: D 30. Which of the following recommendations for adjuvant chemotherapy of colorectal carcinoma are true? A. Patients with Stage I or Dukes A and B1 disease should receive adjuvant treatment for 1 year with levamisole combined with 5-FU. B. Patients with Stage III or Dukes C disease should receive adjuvant treatment for 1 year with levamisole combined with 5-FU. C. There is no role for adjuvant therapy for colon cancer at any stage. D. Adjuvant chemotherapy is active in colon cancer only when combined with radiotherapy. Answer: B 31. Optimal front-line treatment of squamous cell carcinoma of the rectum includes: A. Abdominal perineal resection. B. Low anterior resection when technically feasible. C. Radiation therapy. D. Chemotherapy. E. Combined radiation and chemotherapy. Answer: E 32. Which of the following statement(s) is/are true about the maintenance of continence? A. It depends on both the internal and external sphincters as well as the puborectalis. B. Resting pressure offers a high-pressure zone that increases resistance to the passage of stools. C. Maximal squeeze pressure can last no more than 1 minute. Answer: ABC 33. Which of the following statement(s) about complete rectal prolapse, or procidentia is/are true? A. Rectal prolapse results from intussusception of the rectum and rectosigmoid. B. The disorder is more common in men than in women. C. Continence nearly always is recovered after correction of the prolapse. D. All of the above are true. Answer: A 34. Which of the following statements about hemorrhoids is/are not true? A. Hemorrhoids are specialized “cushions” present in everyone that aid continence. B. External hemorrhoids are covered by skin whereas internal hemorrhoids are covered by mucosa. C. Pain is often associated with uncomplicated hemorrhoids. D. Hemorrhoidectomy is reserved for third- and fourth-degree hemorrhoids. Answer: C 35. The widely accepted treatment of most localized epidermoid, cloacogenic, or transitional cell carcinoma of the anal canal is: A. Surgical resection. B. Chemotherapy alone. C. Radiotherapy alone. D. Combined chemoradiation. Answer: D 36. Which statement(s) is/are true about hidradenitis suppurativa? A. It is a disease of the apocrine sweat glands. B. It causes multiple perianal and perineal sinuses that drain watery pus. C. The sinuses do not communicate with the dentate line. D. The treatment is surgical. E. All of the above. Answer: E 37. Which of the following statements regarding the vasculature of the colon and rectum is/are correct? a. The middle colic artery is a branch of the superior mesenteric artery b. The inferior mesenteric artery supplies the descending and sigmoid segments of the colon c. An complete anastomotic arcade paralleling the colon wall is present in only 15 to 205 of individuals d. The middle colic artery is a branch of the inferior mesenteric artery Answer: a, b, c 38. Which of the following agents have been proposed as sensory neurotransmitters for the colon? a. Acetylcholine b. Substance P c. Calcitonin gene-related peptide d. Bradykinin e. Somatostatin Answer: b, c 39. How much of the daily insensible water loss is due to loss in stool? a. 200 ml b. 400 ml c. 600 ml d. 800 ml e. 1000 ml Answer: a 40. A 52-year-old woman is involved in an automobile accident and sustains an open fracture of the fight femur, compression fractures of the 10th and 11th thoracic vertebrae and right pulmonary contusion. On the fourth day after injury, her abdomen is noted to be distended, tympanitic and diffusely tender. Abdominal radiographs reveal gaseous distension of the ascending and transverse segments of the colon. The cecum is 13 cm in greatest diameter. Appropriate management includes which of the following as the next step? a. Right hemicolectomy b. Operative cecostomy c. Colonoscopy d. Contrast enema e. Observation Answer: c LARGE INTESTINE Interview Objective type Questions with Answers 41. Which of the following features is/are consistent with a diagnosis of colonic inertia? a. Alternating episodes of severe constipation and normal bowel activity b. Total bowel transit time of 24 hours c. Total bowel transit time of 48 hours d. Total bowel transit time of 96 hours e. Marfinoid habitus Answer: d 42. Which of the following statements regarding the myenteric plexus of the colon is/are correct? a. The myenteric plexus is located between the longitudinal and circular layers of the bowel wall b. The myenteric plexus contains only sensory neurons c. The density of neurons with the colonic plexuses decreases along the length of the bowel d. Neurons of the myenteric plexus control the motor function of the colon Answer: a, c, d 43. Which of the following ocular manifestations of ulcerative colitis respond to therapy with steroids or immunosuppressive agents? a. Iridis b. Uveitis c. Retrobulbar neuritis d. Ulcerative panophthalmitis Answer: a, b, c 44. Which of the following statements regarding the risk of cancer in the context of ulcerative colitis is/are correct? a. After 10 years of active disease, the risk of cancer approximates 20% to 30% b. After 10 years of active disease, the risk of cancer approximates 2% to 3% c. The risk of colon cancer in ulcerative colitis is identical to controls d. After 20 years of disease activity, the risk of colon cancer approximates 80% Answer: b 45. Which of the following features would be more consistent with Crohn’s disease than with ulcerative colitis? a. Transmural inflammation b. Microscopic evidence of granulomas within mucosal biopsies c. Microscopic evidence of submucosal thickening and fibrosis d. Microscopic evidence of submucosal inflammation Answer: a, b, c, d 46. A 19-year-old male is seen in consultation with complaints of bloody diarrhea (10 bowel movements per day), and weight loss (10 pounds). Physical examination reveals the presence of two circular, 4 cm erythematous lesions on the trunk. Each lesion has an area of necrosis in the center. The abdominal examination reveals mild hypogastric tenderness. The stool is guaiac positive. The most appropriate next diagnostic step includes which of the following? a. Barium enema b. Flexible sigmoidoscopy c. Liver biopsy d. Chest x-ray Answer: b 47. Which of the following statement(s) regarding ulcerative colitis is/are correct? a. The most common age of onset for ulcerative colitis is in early adulthood b. Approximately 25% of cases of ulcerative colitis occur after the age of 60 c. Males are affected approximately twice as frequently as females d. Approximately 10% to 25% of patients with ulcerative colitis have first degree relatives with the disease Answer: a, d 48. Many patients with ulcerative colitis are operated upon electively with total abdominal colectomy, rectal mucosectomy, formation of a small intestinal reservoir, and ileoanal anastomosis. The most common postoperative complication after this operation is which of the following? a. Enterocutaneous fistula b. Small bowel obstruction c. Pulmonary embolism d. Urinary retention Answer: b 49. A 25-year-old woman with known ulcerative colitis presents to the emergency room with a 24-hour history of abdominal pain, distention, and obstipation. Physical examination reveals a temperature of 38.6° C, abdominal distention, and diffuse abdominal tenderness. Abdominal x-rays show marked colonic dilatation, most pronounced in the transverse colon. Laboratory examination reveals a white blood count of 19,000/mm3. Over the first 24 hours of hospitalization, symptoms are progressive in spite of intravenous fluid resuscitation, nasogastric suctioning, and intravenous antibiotics. The most appropriate management for this patient would include which of the following? a. Decompressive colonoscopy b. Proctocolectomy with formation of end ileostomy c. Total abdominal colectomy with formation of Hartmann pouch and end ileostomy d. Cecostomy Answer: c 50. The most common postoperative complication after formation of a continent ileostomy (Kock pouch) is which of the following? a. Nipple valve failure b. Small bowel obstruction c. Pancreatitis d. Ischemic necrosis of the pouch Answer: a 51. One year following ileal pouch-anal anastomosis, the mean 24-hour stool frequency is which of the following? a. Two to three b. Five to six c. Eight to nine d. Eleven to twelve Answer: b 52. A 30-year-old male two years postoperative after total abdominal colectomy with ileoanal anastomosis reports a sudden increase in stool frequency, nocturnal leakage, and low-grade fevers. Physical examination is unremarkable. Flexible endoscopic examination of the small intestinal pouch reveals a friable erythematous mucosa. Biopsies of the mucosa are obtained. While awaiting biopsy results, which of the following is the most appropriate empiric therapy? a. Oral corticosteroids b. Oral vancomycin c. Oral metronidazole d. Corticosteroid enema Answer: c 53. A 72-year-old man returns to the hospital 2 weeks following right hip arthroplasty with complaints of 48 hours of mucoid diarrhea, fever, and crampy abdominal pain. Physical examination reveals dehydration, diffuse abdominal tenderness, and a temperature of 102°F. Outpatient medications have included digoxin, propranolol, and cephalothin. If antibiotic-associated colitis is suspected, which of the following is/are appropriate diagnostic tests? a. Fecal leukocyte smear b. Stool culture for C difficile c. Measurement of C difficile toxin in stool d. Barium enema e. Computed topography of abdomen Answer: a, b, c 54. For the patient in the preceding question, after obtaining diagnostic samples, the most appropriate management would include which of the following? a. Oral metronidazole b. Intravenous metronidazole c. Oral vancomycin d. Intravenous vancomycin e. Oral bacitracin Answer: c 55. A 72-year-old woman undergoes anterior resection for a rectal cancer located 7 cm proximal to the anal verge. Pathologic examination of the resected specimen reveals invasion of the tumor into the muscularis propria. Five of 8 lymph nodes contain microscopic tumor. There is no evidence of disseminated disease. Appropriate subsequent management includes which of the following? a. Postoperative radiation plus intravenous 5FU b. Postoperative radiation alone c. Observation d. Postoperative radiation plus intravenous adriamycin Answer: a 56. Which of the following are tumor suppressor genes that have been associated with the development of colorectal cancer? a. The DCC gene b. The APC gene c. The P53 gene d. The Rb gene Answer: a, b, c 57. Which of the following statement(s) is/are correct with regard to the use of carcinoembryonic antigen (CEA) determinations in management of colorectal cancer? a. CEA determination has 95% specificity when used for screening for colon cancer development in patients with ulcerative colitis b. CEA levels are increased in 20% of patients with local recurrence after resectional therapy c. CEA measurements are increased in 90% of patients with disseminated disease d. CEA levels are increased in 90% of patients with local recurrence after resectional therapy Answer: b, c 58. The most common oncogene abnormality observed in association with colorectal cancer is which of the following? a. Overexpression of the N-myc oncogene b. Amplification of the K-ras oncogene c. Suppression of the erbB oncogene d. Amplification of the L-myc oncogene Answer: b 59. Which of the following types of colonic polyps is associated with the highest incidence of malignant degeneration? a. Tubular adenoma b. Tubulovillous adenoma c. Villous adenoma d. Hamartomatous polyp Answer: c 60. A 52-year-old man undergoes a right hemicolectomy for a carcinoma of the ascending colon. Pathological examination of the resected specimen reveals invasion of the tumor to the level of the muscularis propria. Three of 17 lymph nodes contain microscopic tumor. What is the correct Dukes classification (Aster-Coller modification) and associated 5-year survival for this lesion? a. Dukes C2, 45% 5-year survival b. Dukes B1, 75% 5-year survival c. Dukes C1, 45% 5-year survival d. Dukes B3, 65% 5-year survival Answer: c 61. An pedunculated polyp, discovered incidentally at colonoscopy, is removed by snare polypectomy from the ascending colon. Invasive cancer to the level of the submucosa is identified histologically within the polyp. The lesion is well-differentiated. No lymphatic or vascular invasion is noted. The cauterized margin is negative for neoplasm. Appropriate subsequent management includes which of the following? a. Repeat endoscopy at 6 months b. Right hemicolectomy c. Subtotal colectomy d. Repeat endoscopy with fulguration of the polypectomy site Answer: a 62. Dietary risk factors thought to play a causative role in development of colorectal cancer include which of the following? a. High fat intake b. Low fiber intake c. High smoked food intake d. High vegetable intake Answer: a, b 63. Which of the following statements with regard to resection of rectal cancers is/are true? a. A distal margin of 5 cm should be obtained because 42% of patients have microscopic evidence of intramural spread beyond 3 cm from the palpable tumor b. A distal margin of 3 cm should be obtained because only 3% of patients have microscopic evidence of intramural spread beyond 2 cm from the palpable tumor c. Local recurrence rates correlate strongly with distal margins less than 4 cm d. There is no correlation between local recurrence and distal margins beyond 2 cm Answer: b, d 64. A 58-year-old male undergoes resection of a Dukes C2 colon cancer via right hemicolectomy. Three years postoperatively, rising CEA levels prompt evaluation including abdominal computed tomography. Two lesions, each measuring 2 cm, are noted in the right hepatic lobe. No other abnormalities are noted. A right hepatic lobectomy is performed without complication. Which of the following most closely approximates anticipated 5-year survival? a. 85–90% b. 65–70% c. 45–50% d. 25–30% Answer: d 65. An asymptomatic 52-year-old man is undergoing screening sigmoidoscopy. In the rectum, at 6 cm from the anal verge, a 2 cm yellow, submucosal nodule is noted. Deep endoscopic biopsies are consistent with carcinoid. Appropriate management includes which of the following? a. Observation b. Transanal excision c. Low anterior resection d. Abdominoperineal resection Answer: b 66. A 72-year-old woman complains of anal itching and burning. Physical examination reveals an erythematous, scaly lesion, 3 cm in circumference, within the anal canal. The intersphincteric groove can not be appreciated in the area of the lesion. The remainder of the physical examination is normal. Appropriate initial management includes which of the following? a. Acyclovir 200 mg QID for 10 days b. Hydrocortisone cream 0.1% topically for 14 days c. Incisional biopsy d. Metronidazole 250 mg PO QID for 14 days Answer: c 67. For the patient in the preceding question, biopsy revealed an invasive apocrine gland neoplasm. The deep margins included striated muscle infiltrated by neoplastic cells. Appropriate management includes which of the following? a. Primary radiation b. Abdominoperineal resection with bilateral inguinal lymph node dissection c. Abdominoperineal resection only d. Carbon dioxide laser fulguration Answer: c 68. A 43-year-old woman presents with complaints of anal pain and spotting of blood with defecation. Physical examination reveals a 2 3 cm area of ulceration within the anal canal. The remainder of the physical examination is normal. Incisional biopsy is positive for squamous cell carcinoma. Appropriate management includes which of the following? a. Abdominoperineal resection b. Wide local excision, skin grafting, proximal diverting colostomy c. Primary radiation therapy d. Local excision and primary closure Answer: c 69. Recurrent episodes of sigmoid colonic diverticulitis prompt operative therapy. Which of the following describe the appropriate margins for resection? a. Proximal margin, splenic flexure; distal margin, rectosigmoid junction b. Proximal margin, descending colon; distal margin, rectosigmoid junction c. Proximal margin, descending colon; distal margin, mid-rectum d. Proximal margin, transverse colon; distal margin, mid-rectum Answer: b 70. An elderly man presents with complaints that he is passing gas with urination. The past medical history is positive for one episode of diverticulitis, treated medically, transurethral resection of the prostate for benign prostatic hypertrophy, and diabetes. Which of the following diagnostic tests is most appropriate initially? a. Computed tomography of the abdomen and pelvis b. Cystoscopy c. Barium enema d. Intravenous pyelography Answer: a 71. For the patient in the preceding question, a colovesical fistula originating from the sigmoid colon is demonstrated. Colonoscopy reveals diverticula and excludes carcinoma. During laparotomy, a thickened sigmoid colon is found to be adherent to the dome of the bladder. A definite fistula is not observed. Appropriate operative management includes which of the following? a. Sigmoid resection, primary colonic anastomosis, catheter drainage of bladder b. En-bloc resection of sigmoid colon and adjacent bladder wall, primary colonic anastomosis, suprapubic cystostomy c. En-bloc resection of sigmoid colon and adjacent bladder wall, formation of descending colostomy and Hartmann’s pouch, suprapubic cystostomy d. Sigmoid resection, primary colonic anastomosis, bilateral percutaneous nephrostomies Answer: a 72. A 65-year-old woman develops obstipation, lower abdominal pain, and fever. Physical examination reveals a temperature of 38.5°C, left lower quadrant tenderness, and an ill-defined lower abdominal mass. White blood count is 17,500 per mm3. Intravenous hydration, broad spectrum antibiotics, and analgesics are ordered. After 48 hours, symptoms have not improved. Appropriate management includes which of the following? a. Barium enema b. Computed tomography of the abdomen c. Immediate laparotomy d. Intravenous pyelogram Answer: b 73. Which of the following statement(s) relating to anal sphincteric function is/are correct? a. When the rectum is distended, the internal anal sphincter relaxes and the external anal sphincter contracts b. When the rectum is distended, the internal anal sphincter contracts and the external anal sphincter relaxes c. The external anal sphincter is responsible for resting anal pressure d. The internal anal sphincter is responsible for resting anal pressure Answer: a, d 74. The most common complication after hemorrhoidectomy is which of the following? a. Urinary retention b. Rectal bleeding c. Incontinence d. Wound infection Answer: a 75. Appropriate treatment of chlamydial proctitis includes which of the following? a. Tetracycline 500 mg QID b. Metronidazole 250 mg QID c. Acyclovir 200 mg QID d. Erythromycin 500 mg QID Answer: a, d 76. A 65-year-old man presents with complaints of mucous discharge and perianal discomfort. Physical examination reveals a fistulous opening lateral to the anus. Anoscopic examination permits passage of a probe through the fistula tract. The fistula traverses the internal anal sphincter, the intersphincteric plane, and a portion of the external anal sphincter. The fistula is categorized as which type? a. Intersphincteric b. Transsphincteric c. Suprasphincteric d. Extrasphincteric Answer: b 77. For the patient in the preceding question, appropriate management includes which of the following? a. Division of the tissues over the probe with electrocautery, leaving the wound open to heal by secondary intention b. Division of the tissues over the probe with electrocautery, closing the wound using a pedicled skin flap c. Division of the internal anal sphincter using electrocautery, encircling the external sphincter with a seton d. Proximal diverting colostomy and antibiotics Answer: c LARGE INTESTINE Questions and Answers pdf Download Read the full article
0 notes
Text
“Hannah Roe,” 29 (USA 1978)
A medical journal published two cases of death by uterine rupture after legal saline-oxytocin abortion. The authors noted that although the association between oxytocin administration and uterine rupture in pregnancy was well-established, it was common for abortionists to administer oxytocin in combination with saline for abortions.
One of the women killed is “Hannah Roe”. She was 29 and pregnant for the 4th time. She was approximately 20 weeks pregnant when she underwent a saline-oxytocin abortion in a hospital. She had never had any uterine surgery in her life. Hannah was obese, which made abortion in general riskier for her.
The abortion was started by removing 40 ccs of amniotic fluid and injecting 200 ccs of saline. The following events show a timeline of Hannah’s decline and death. All timeframes are counting from the start of the abortion. Please note that amounts of time are approximate.
4 hours: Hannah was given IV oxytocin, which was intended to speed up the abortion.
24 hours: Even though she had already had 60u of oxytocin, Hannah was given another 40u through IV.
27 hours: Hannah was very pale and her blood pressure was registered at 70/30. A pelvic exam showed mild bleeding. An additional 60u of oxytocin was administered.
27 hours and >10 minutes: Hannah suffers from profuse vaginal bleeding.
After her bleeding became severe, Hannah was rushed to the operating room. Her dead child and the placenta were manually removed and the uterus was examined, but no defect was found at the time. Hannah was given 2 units of whole blood and fibrinogen to treat the bleeding. Then she was transferred to another hospital that had a better blood bank.
At the second hospital, Hannah’s blood pressure was only 40/0 and her hematocrit level was 20%. Her abdomen was full of blood. Doctors administered more blood transfusions, but Hannah’s condition was too critical for surgery. 5 hours and multiple cardiopulmonary arrests later, Hannah was declared dead.
The autopsy revealed a transverse rupture of Hannah’s right lower uterine segment. The rupture was half as long as the entire wall. In addition to the intraperitoneal hemorrhage, an estimated 1,500 ccs of blood was found retroperitoneally.
The case report also noted that similar uterine ruptures had been caused by prostaglandin abortions augmented with oxytocin.
(Hannah Roe is Patient 2)
#pro life#tw abortion#abortion#pro choice#tw murder#abortion debate#tw ab*rtion#unidentified victim#unsafe yet legal
3 notes
·
View notes
Text
Opinion: Maternal Morbidity Associated with Splenic Artery Rupture and Retroperitoneal Haematomas (RPH) in Pregnancy
Letter to EditorRecently a case report was published in Global Journal of reproductive medicine by Mulla AA et al. [1] on Spontaneous Rupture of splenic artery aneurysm. There need to be increased awareness about such cases in obstetric population because the incidence of splenic artery rupture in pregnancy is low and also may be not many cases are reported in literature. The finding of inquest [2] in the death of pregnant women revealed that eight deaths occurred in Australia from year 2000-2012 due to splenic artery rupture in pregnant women and main reason was that it was late and misdiagnosed. A review on 21 cases of retroperitoneal haematoma in obstetrics highlighted the fact that splenic artery rupture is one of the important causes of retroperitoneal haematoma and presentation can be confusing posing a diagnostic dilemma for clinicians .Upper Abdominal pain in splenic artery rupture and inferior epigastric artery rupture is confused with placental abruption and stretching pain of the hepatic capsule especially with history of pre-eclampsia [3,4]. I would also highlight the case of malaria in obstetric patient causing splenic accident and retroperitoneal haematoma in pregnant woman. Probable mechanism of spontaneous rupture of spleen can be due to hyperplasia and stretching of splenic parenchyma, infarcts, haemorrhage and hematomas, tears or fibrosis can be the contributory factors [5].The issue of retroperitoneal haematoma is very important in maternal morbidity and mortality but it's very rare and there is not enough awareness among obstetricians. Although there was more intraperitoneal bleeding in this case, however it can pose major morbidity and mortality issue where bleeding is only confined to retroperitoneal space and picked up quite late unless incidentally found on ultrasound abdopelvis or CT- scan. The Advanced Life Support (ALS) Manuals and Obstetric drills include chest pain as the most important cause of collapse. But In obstetric patient chest pain due to splenic artery rupture is misdiagnosed or confused with Amniotic fluid embolism, pulmonary embolism, Myocardial infarction and Pneumomediastinum [4,5]. And further on since splenic artery rupture may not always present with obvious peritoneal symptoms so can be easily missed or diagnosed late when it only cause retroperitoneal bleed. We need to strengthen this opinion that National Guidelines must address and emphasise on the rare causes of maternal morbidity, mortality and collapse during puerperium. Only then it would be possible to increase awareness among obstetricians.Authored By: Rafi J*

#peer review journals#high impact journals in juniper publishers#Juniper Publishers#global journal of reprodutive medicine
0 notes
Text
Best oncologist surgeon in Hyderabad – umacancercenter
The Oncologist who are dedicated to save lives
The branch of medicine that deals with researching, identifying and treating cancer is referred to as oncology. A physician who is associated with the field of oncology is called an Oncologist. Dr Madhu Devarasetty is one of the most renowned oncologist surgeon in Hyderabad, who is associated with Uma cancer centre.
In the first step of treatment, the oncologist diagnoses a person with cancer; they do it by performing a biopsy, endoscopy, X-ray, C T scanning, PET scanning, MRI, ultrasound, and other radiology methods.
There is an increasing concern for cancer; very few cancer hospitals provide affordable treatment to patients with great care.
There are three main divisions of oncology, and depending upon the stage of cancer, the nature and the location of cancer, there are many oncologists.
Medical Oncologist
A medical oncologist is a doctor who treats patients who have cancer. They administer chemotherapy and other medications such as immunotherapy.
The medical oncologist treats all kinds of cancer that originate in different parts of the body.
While administering chemotherapy, the doctors use drugs that kill the cancer cells and leave the patient’s cell unharmed.
Despite the recent advancements in the field, chemotherapy has side effects that are visible on the body of the patients. The significant side effects include nausea, hair loss, weakness, fatigue, loss of appetite, fever, diarrhoea, mouth sores, and prone to bruise and bleed.
Surgical oncologist
This particular oncologist focuses on using surgery to diagnose, staging, and then surgically remove the cancer cell from the affected part of the body.
The possibility of going under surgery depends on the stage, size and location of cancer. The patient’s age and physical fitness is also a factor.
A few of the surgical procedures in oncology include appendectomy; in this procedure, the appendix is removed as it swells due to infection and causes irritation and inflammation.
In bowel resection, doctors surgically remove the colorectal tumours, surrounding tissues and lymph nodes.
Hyperthermic intraperitoneal chemotherapy is administered directly to the abdomen to kill the cancer cells. Before the patients receive the treatment, the doctors perform cytoreductive surgery to remove the tumours.
Pneumonectomy
A surgery that consists of removing an entire lung to treat non-small cell lung cancer, tuberculosis and chronic obtrusive pulmonary disease. Pneumonectomy is invasive and complex surgery.
It takes experienced and accomplished doctors to perform this surgery, and the medical team of Uma hospital prides itself to have a few brilliant oncologist surgeon in Hyderabad.
Radiation Oncologist
Radiation oncologists are those doctors who administer radiation therapy to treat cancer. In radiation therapy, the doctors use high energy x-rays to eliminate the cancerous cells.
When it becomes difficult to destroy the cells, the doctors use radiation therapy as a procedure to slow down the growth of the tumour. This particular method is also called palliative therapy; its primary goal is to control tumour growth and its lingering effects.
Radiation oncologists also use another procedure called brachytherapy. The radioactive agents are directly placed next to the tumour; they can be removed after the treatment session or not, but it depends on the type of cancer that the patient has.
Gynecologic oncologist
Gynecologic oncologists are specialized doctors who treat the cancers that occur in the female reproductive system.
This category treats ovarian cancer, cervical cancer, uterine cancer, vaginal cancer, and vulvar cancer.
Different surgeries are performed pertaining to other parts of the female reproductive system.
For instance, optimal debulking surgery is employed to treat ovarian cancer, including peritoneal biopsies, abdominal hysterectomy, omentectomy, oophorectomy, lymph node sampling, etc.
Pediatric oncologist
Certain cancers affect children significantly, and pediatric oncologists specialize in this field to rid young children of the disease. Leukaemia, brain tumours, osteosarcoma are some of the cancers that affect children from a young age to adolescence.
A highly efficient team of accomplished doctors happens to be headed by an excellent oncologist surgeon in Hyderabad at Uma cancer centre.
#oncologist surgeon in hyderabad#surgical oncologist in hyderabad#best cancer doctor in Hyderabad#best cancer hospital in hyderabad
0 notes
Text
Ovarian Cancer: More Deadly Than Breast Cancer
A few years ago I was asked if I knew what the most deadly gynecologic cancer was and I answered “Well, breast cancer of course.” Oh, how I was wrong. The American Cancer Society estimates that the average five year survival rate of breast cancer at any stage to actually be 89 percent. While no cancer is good that’s a pretty good rate. The correct answer to the question is ovarian cancer, and its five year survival rate (estimated by the American cancer society) is only 46 percent. We need to find out why this cancer is so deadly.
Cancer is a dangerous and mysterious thing to people that don’t know much about it. Well, everyone is made up of cells, cells are what make up tissue and tissue is what makes up our organs. Normally when a cell gets old and tired it dies just like we do and a new cell takes its place. Our body produces these new cells by growing and dividing healthy cells. Sometimes our body overproduces cells and this is when tumors (mass of tissue) are formed. These tumors aren’t always cancer; when they are not they are called benign tumors. When they are cancer they are call malignant; these are the ones that can be life-threatening. Both types of tumors can be removed but the cancerous ones are more likely to grow back and only they also can spread to different parts of your body. When this happens the cancer cells are breaking away from the original tumor and entering the blood stream to use it like a highway to travel around your body. When the cancer cells spread like this it’s called metastasis and the cancer can start to go new tumors. If these cells reach any of your organs and start to go new tumors and this is when damage can be done.
They call it ovarian cancer because the tumor first starts at the ovaries and is made up of over productive ovarian cells. The ovaries are part of the women’s reproductive system and are attached to the uterus by the fallopian tubes. When a malignant tumor starts to grow these areas can also be affected because of their close proximity to the ovaries. When this tumor starts to shed cancer cells the cells typically go to the abdomen first because it’s closest to where the reproductive system is located. Then as I said before the cancerous cells can start to affect your lymph nodes and enter your blood stream to travel to different organs.
Ovarian cancer is so deadly because it’s very hard to detect. Every year more than 14,600 women die from ovarian cancer in the United States. This may not seem like a lot when you think of all the billion people that live here but when about 20,000 women are diagnosed with ovarian cancer each year that number seems like a lot. So this means that on average 7 out of 10 women will die from this disease and this is all because it is so hard to detect. In order to detect it you have to know what the symptoms are. The most common symptoms are pain in the abdomen, pelvis, back or legs because of where the cancer is located in your body. You can also have a swollen or bloated abdomen because it can fill up with fluids. You will also feel very tired all the time and would have some nausea, indigestion, gas, constipation, or even diarrhea. Some less common symptoms would be shortness of breath, the urge to urinate often, and unusual vaginal bleeding. Now these are pretty general symptoms and many other disease or illnesses can cause them and that’s why it’s so hard to detect because ovarian cancer is not typical the very first thing we think of when we have one or more of these symptoms.
Most women would think if there was a problem that it would show up on their Pap test which is a once yearly screening that women get from their doctor. However, a Pap test is only screening for cervical cancer and it cannot be used to diagnose ovarian cancer. When women do go in to your doctor for the Pap test he or she should be doing a pelvic exam as well, during this they will feel your ovaries and organs in close proximity for any lumps or changes in shape and/or size. More often than not the doctors will not be able to feel a tumor until they are a substantial size. This is why we look to other testing as well as the pelvic exam to diagnose this cancer. If women who have abdominal bloating or pain and would go to the doctor, they may check your abdomen for fluid buildup. If they some find some a sample can be taken to test for ovarian cancer cells as part of the diagnoses. There is also blood testing where your doctor would check your CA-125 level to see if it is high. The CA-125 is a substance that is found on the surface of the ovarian cancer cells but also on some normal tissue, this is why a high level might indicate cancer. Unfortunately this test cannot be used as the only test for diagnosing ovarian cancer. It is mainly used for monitoring a woman that has already been diagnosed and is going through treatment or as an early detection for the return of cancer after treatment has been completed. The next way to get diagnosed is by having an ultrasound done. There are two different types of ultrasounds that can be done; the first is the less invasive of the two. This is where they take the ultrasound device and press it up against your abdomen and the sound waves that it produces bounce off the organs to produce a picture for us to see. By using this they would be able to get a picture of the ovaries to see if there was a tumor or any abnormalities. The second type of ultrasound they can do is a transvaginal ultrasound and it does the same things as the regular one however this device is inserted into the vagina for a much better view of the ovaries. The last test to help diagnose this cancer is a biopsy. They will only do a biopsy if blood test and one of the ultrasounds have indicated that there may be a tumor. A biopsy is when they take a sample of tissue or fluid to look for cancer cells. Once they biopsy has been done a pathologist will look as the sample under a microscope for any cancer cells. If there are some found then they will be described as either grade 1, 2, or 3 and this is based off of how abnormal the cells look.
Once the doctors have determined that there are cancer cells present they have to determine what stage the disease is in before they can start any treatment. In order to find out what stage the cancer is in the doctor must know grade the tumor is which we discussed earlier and they also may need to run a series of more test such as a CT scan or a chest x-ray. The CT scan is where they would give you some contrast material and the machine would then take several pictures to get a clearer picture of your pelvis and abdomen to see any tumors or abdominal fluid. The chest x-ray is used to see if the cancer has spread to your lungs and if there is any fluid buildup there as well.
There are four stages of ovarian cancer; the first stage is called stage 1. Stage 1 is where cancer cells can be found on one or both ovaries or in abdominal fluid. Only 15 percent of the total women diagnosed have stage 1 and they have a 5 year survival rate of 93.8 percent (statistics). Stage 2 is where the cancer has spread to other reproductive organs such as the fallopian tubes and the uterus. It can also be found in abdominal fluid as well as other tissue in the pelvis area. The 5 year survival rate for stage 2 is 72.8 percent and only 17 percent of women diagnosed have this stage. Stage 3 is where the cancer has spread to the lymph nodes and can be also found on the outside of the liver. This is the most common stage that women are diagnosed (62 percent) with only a 28.2 percent survival rate or 5 years (statistics). The last stage is stage 4 and this is when the cancer can be found in the lungs or in any other organs. So, at this point it has traveled out of both the pelvic and abdominal areas. This has the lowest survival rate of 27.3 percent and the lowest percent of women diagnosed at 7 percent (statistics).
Once the doctor has determined what stage you are in you can start treatment accordingly. Most women will have surgery to remove cancer cells and also both ovaries and fallopian tubes, your uterus, any nearby lymph nodes, as well as the omentum which is a thin fat pad that covers the intestines. If you only have stage 1 sometimes the doctors will leave the uterus intact and only take one ovary and fallopian tube but this depends on your age and whether or not you would like to become pregnant and have children. If the cancer is one of the other stages (2, 3 or 4) then they might have to go in further and remove as much cancer as they possibly can. They can also do chemotherapy as a form of treatment. This is when “anticancer” drugs are given to kill the cancerous cell. The drugs can be given by either inserting them into the vein (IV), intraperitoneal (IP) which is given directly into the abdomen through a very thin tube, or by mouth via pill form (ovarian cancer 13). The side effects to the chemotherapy can be hair loss, vomiting, and diarrhea. This is because the drugs also harm normal cells, so it can damage your hair cells (hair loss) and the cells that line your digestive tract (vomiting and diarrhea) but it can also damage your blood cells and make your body bruise easier and you would be more susceptible to get infections because your blood cells are what help fight infections off.
As of right now we cannot explain why one women may develop this cancer and another will not but there are some women that are at higher risk. If you have any women in your family that has had ovarian cancer, specifically your mother, daughter, or sister you or a family member are at a higher risk. But, also if you or any other family members have had uterus, colon, rectum, or breast cancer you or a family member will be at a higher risk. Most women that are diagnosed with this disease are over the age of 55 and have never been pregnant. If you or a family member is at an increase risk you want to talk to your family member to make sure they are aware of these risks. Then I would encourage those at risk people to consult your doctor and see if anything can be done to make sure if you would so some signs of cancer, it could be detected early.
They may recommend genetic testing to see if you have a certain mutation of the BRCA 1 or BRCA 2 gene which has been linked to ovarian cancer and breast cancer. If you go and have this testing done you will have to provide a detailed family history and also give a blood sample. They will test they blood for mutations in your DNA, specifically looking at your BRCA 1 and 2 genes. When you get the results back they will let you know if they found a mutation and if they did you know that you for sure are at an increase risk. If they don’t find a mutation they will still put you into an at risk category based on your family history. This testing has been very important in determining the links between certain mutations and ovarian cancer. The more data we can collect the better off we are on finding a connection.
The most important thing to remember is that this is the most deadly gynecologic cancer with very nonspecific symptoms, 15,000 women die from this cancer every year. If you or anyone you know are having any of these symptoms you should talk to them and encourage them to contact their doctor in hopes of early detection. The earlier the detection the better chances you or a family member has of not becoming one of the 15,000.
Source by Kimberly Jean
from Home Solutions Forev https://homesolutionsforev.com/ovarian-cancer-more-deadly-than-breast-cancer/ via Home Solutions on WordPress from Home Solutions FOREV https://homesolutionsforev.tumblr.com/post/186988592785 via Tim Clymer on Wordpress
0 notes
Text
Types of Gynecological cancers
Gynecological cancers are cancers that start in a woman's reproductive system or organs. It begins in different places within the women's pelvis (area below the stomach and between the hip bones).
The five most common gynecological cancers are-
Cervical cancer
Ovarian cancer
Vaginal cancer
Vulvar cancer
Womb cancer
Cervical Cancer- Cervix is the lower part of the uterus that connects to the vagina, and cervical cancer is a type of cancer that occurs in the cervix cells.
HPV is a sexually transmitted infection. I will play a significant role in causing the most cervical cancers. The human body, when exposed to HPV, the immune system typically prevents the virus from going home. Still, in a small percentage of people, the virus survives for years, contributing to some cervical cells becoming cancer cells.
There are symptoms like Vaginal bleeding after intercourse or between periods or after menopause. Bloody discharge from the vagina that may be heavy or have a foul odor. Pelvic pain
Ovarian Cancer- There are two ovaries and a female reproductive system. One on each side of the uterus. They are there to produce eggs and hormones estrogen and progesterone. Ovarian cancer begins in the ovaries and opens undetected until it gets spread within the pelvis and abdomen, and that's why when a female enters the late stage of ovarian cancer, it becomes tough to treat.
Symptoms include- Abdominal bloating or swelling Feeling for me, even after eating low Discomfort in the pelvis area Constipation Frequent need to urinate
Vaginal Cancer- The vagina is the muscular tube that connects your uterus with your outer genitals. Vagina cancer most commonly occurs in the cell that lined the surface of your vagina. It is a rare condition that occurs in the female reproductive system.
Symptoms- The unusual vagina is bleeding Frequent urination Constipation Pelvic pain Lump or mass in your vagina
Vulvar Cancer- we will cancel that occurs in the outer surface of female genitalia. The world is the skin area that contains the urethra and vagina, including the clitoris and labia. Vulvar cancer commonly causes lumps or sores, which usually gives itching. It can occur at any stage, and it is the most frequently diagnosed cancer in older adults.
Symptoms include- Continuous itching Pain around area Unusual bleeding Skin changes ( color change) Lump
Womb Cancer- It is also known as typical uterus cancer that affects the reproductive system. It affects those women who have been through menopause.
Symptoms- The most common sign of womb cancer is abnormal vagina bleeding, and especially if you have been through menopause, then the bleeding is considered not good for you.
Treatment for gynecological cancers
As mentioned above, when a woman is facing any cancer, it becomes essential to visit a gynecologist. There are very experienced Gynecologists in sector 14 Gurgaon. Medically it is proven that women dealing with gynecological cancers get more than one kind of treatment. Treatment includes surgery, chemotherapy, or radiation.
Cancer detected at an early stage becomes easy to cure. Gynecologists in Sector 14 Gurgaon help you with treatments like chemotherapy, immunotherapy, hormone therapy.
Types of surgeries- Debulking surgery- it removes as much of the humor as possible Total hysterectomy- Removes uterus and cervix Radical hysterectomy- removes the uterus, cervix, or part of a vagina. Omentectomy- Removes a fat pad within the abdominal cavity Lymph node removal- Removal of lymph nodes affected by cancer.
A unique treatment directly delivers chemotherapy drugs into the abdominal cavity through a catheter known as intraperitoneal chemotherapy. Only experience gynecological or specialized people or proven to do this treatment. Dr. Ritu at cloudnine Gurgaon is considered best for such issues.
0 notes
Text
Ovarian Cancer: More Deadly Than Breast Cancer
A few years ago I was asked if I knew what the most deadly gynecologic cancer was and I answered “Well, breast cancer of course.” Oh, how I was wrong. The American Cancer Society estimates that the average five year survival rate of breast cancer at any stage to actually be 89 percent. While no cancer is good that’s a pretty good rate. The correct answer to the question is ovarian cancer, and its five year survival rate (estimated by the American cancer society) is only 46 percent. We need to find out why this cancer is so deadly.
Cancer is a dangerous and mysterious thing to people that don’t know much about it. Well, everyone is made up of cells, cells are what make up tissue and tissue is what makes up our organs. Normally when a cell gets old and tired it dies just like we do and a new cell takes its place. Our body produces these new cells by growing and dividing healthy cells. Sometimes our body overproduces cells and this is when tumors (mass of tissue) are formed. These tumors aren’t always cancer; when they are not they are called benign tumors. When they are cancer they are call malignant; these are the ones that can be life-threatening. Both types of tumors can be removed but the cancerous ones are more likely to grow back and only they also can spread to different parts of your body. When this happens the cancer cells are breaking away from the original tumor and entering the blood stream to use it like a highway to travel around your body. When the cancer cells spread like this it’s called metastasis and the cancer can start to go new tumors. If these cells reach any of your organs and start to go new tumors and this is when damage can be done.
They call it ovarian cancer because the tumor first starts at the ovaries and is made up of over productive ovarian cells. The ovaries are part of the women’s reproductive system and are attached to the uterus by the fallopian tubes. When a malignant tumor starts to grow these areas can also be affected because of their close proximity to the ovaries. When this tumor starts to shed cancer cells the cells typically go to the abdomen first because it’s closest to where the reproductive system is located. Then as I said before the cancerous cells can start to affect your lymph nodes and enter your blood stream to travel to different organs.
Ovarian cancer is so deadly because it’s very hard to detect. Every year more than 14,600 women die from ovarian cancer in the United States. This may not seem like a lot when you think of all the billion people that live here but when about 20,000 women are diagnosed with ovarian cancer each year that number seems like a lot. So this means that on average 7 out of 10 women will die from this disease and this is all because it is so hard to detect. In order to detect it you have to know what the symptoms are. The most common symptoms are pain in the abdomen, pelvis, back or legs because of where the cancer is located in your body. You can also have a swollen or bloated abdomen because it can fill up with fluids. You will also feel very tired all the time and would have some nausea, indigestion, gas, constipation, or even diarrhea. Some less common symptoms would be shortness of breath, the urge to urinate often, and unusual vaginal bleeding. Now these are pretty general symptoms and many other disease or illnesses can cause them and that’s why it’s so hard to detect because ovarian cancer is not typical the very first thing we think of when we have one or more of these symptoms.
Most women would think if there was a problem that it would show up on their Pap test which is a once yearly screening that women get from their doctor. However, a Pap test is only screening for cervical cancer and it cannot be used to diagnose ovarian cancer. When women do go in to your doctor for the Pap test he or she should be doing a pelvic exam as well, during this they will feel your ovaries and organs in close proximity for any lumps or changes in shape and/or size. More often than not the doctors will not be able to feel a tumor until they are a substantial size. This is why we look to other testing as well as the pelvic exam to diagnose this cancer. If women who have abdominal bloating or pain and would go to the doctor, they may check your abdomen for fluid buildup. If they some find some a sample can be taken to test for ovarian cancer cells as part of the diagnoses. There is also blood testing where your doctor would check your CA-125 level to see if it is high. The CA-125 is a substance that is found on the surface of the ovarian cancer cells but also on some normal tissue, this is why a high level might indicate cancer. Unfortunately this test cannot be used as the only test for diagnosing ovarian cancer. It is mainly used for monitoring a woman that has already been diagnosed and is going through treatment or as an early detection for the return of cancer after treatment has been completed. The next way to get diagnosed is by having an ultrasound done. There are two different types of ultrasounds that can be done; the first is the less invasive of the two. This is where they take the ultrasound device and press it up against your abdomen and the sound waves that it produces bounce off the organs to produce a picture for us to see. By using this they would be able to get a picture of the ovaries to see if there was a tumor or any abnormalities. The second type of ultrasound they can do is a transvaginal ultrasound and it does the same things as the regular one however this device is inserted into the vagina for a much better view of the ovaries. The last test to help diagnose this cancer is a biopsy. They will only do a biopsy if blood test and one of the ultrasounds have indicated that there may be a tumor. A biopsy is when they take a sample of tissue or fluid to look for cancer cells. Once they biopsy has been done a pathologist will look as the sample under a microscope for any cancer cells. If there are some found then they will be described as either grade 1, 2, or 3 and this is based off of how abnormal the cells look.
Once the doctors have determined that there are cancer cells present they have to determine what stage the disease is in before they can start any treatment. In order to find out what stage the cancer is in the doctor must know grade the tumor is which we discussed earlier and they also may need to run a series of more test such as a CT scan or a chest x-ray. The CT scan is where they would give you some contrast material and the machine would then take several pictures to get a clearer picture of your pelvis and abdomen to see any tumors or abdominal fluid. The chest x-ray is used to see if the cancer has spread to your lungs and if there is any fluid buildup there as well.
There are four stages of ovarian cancer; the first stage is called stage 1. Stage 1 is where cancer cells can be found on one or both ovaries or in abdominal fluid. Only 15 percent of the total women diagnosed have stage 1 and they have a 5 year survival rate of 93.8 percent (statistics). Stage 2 is where the cancer has spread to other reproductive organs such as the fallopian tubes and the uterus. It can also be found in abdominal fluid as well as other tissue in the pelvis area. The 5 year survival rate for stage 2 is 72.8 percent and only 17 percent of women diagnosed have this stage. Stage 3 is where the cancer has spread to the lymph nodes and can be also found on the outside of the liver. This is the most common stage that women are diagnosed (62 percent) with only a 28.2 percent survival rate or 5 years (statistics). The last stage is stage 4 and this is when the cancer can be found in the lungs or in any other organs. So, at this point it has traveled out of both the pelvic and abdominal areas. This has the lowest survival rate of 27.3 percent and the lowest percent of women diagnosed at 7 percent (statistics).
Once the doctor has determined what stage you are in you can start treatment accordingly. Most women will have surgery to remove cancer cells and also both ovaries and fallopian tubes, your uterus, any nearby lymph nodes, as well as the omentum which is a thin fat pad that covers the intestines. If you only have stage 1 sometimes the doctors will leave the uterus intact and only take one ovary and fallopian tube but this depends on your age and whether or not you would like to become pregnant and have children. If the cancer is one of the other stages (2, 3 or 4) then they might have to go in further and remove as much cancer as they possibly can. They can also do chemotherapy as a form of treatment. This is when “anticancer” drugs are given to kill the cancerous cell. The drugs can be given by either inserting them into the vein (IV), intraperitoneal (IP) which is given directly into the abdomen through a very thin tube, or by mouth via pill form (ovarian cancer 13). The side effects to the chemotherapy can be hair loss, vomiting, and diarrhea. This is because the drugs also harm normal cells, so it can damage your hair cells (hair loss) and the cells that line your digestive tract (vomiting and diarrhea) but it can also damage your blood cells and make your body bruise easier and you would be more susceptible to get infections because your blood cells are what help fight infections off.
As of right now we cannot explain why one women may develop this cancer and another will not but there are some women that are at higher risk. If you have any women in your family that has had ovarian cancer, specifically your mother, daughter, or sister you or a family member are at a higher risk. But, also if you or any other family members have had uterus, colon, rectum, or breast cancer you or a family member will be at a higher risk. Most women that are diagnosed with this disease are over the age of 55 and have never been pregnant. If you or a family member is at an increase risk you want to talk to your family member to make sure they are aware of these risks. Then I would encourage those at risk people to consult your doctor and see if anything can be done to make sure if you would so some signs of cancer, it could be detected early.
They may recommend genetic testing to see if you have a certain mutation of the BRCA 1 or BRCA 2 gene which has been linked to ovarian cancer and breast cancer. If you go and have this testing done you will have to provide a detailed family history and also give a blood sample. They will test they blood for mutations in your DNA, specifically looking at your BRCA 1 and 2 genes. When you get the results back they will let you know if they found a mutation and if they did you know that you for sure are at an increase risk. If they don’t find a mutation they will still put you into an at risk category based on your family history. This testing has been very important in determining the links between certain mutations and ovarian cancer. The more data we can collect the better off we are on finding a connection.
The most important thing to remember is that this is the most deadly gynecologic cancer with very nonspecific symptoms, 15,000 women die from this cancer every year. If you or anyone you know are having any of these symptoms you should talk to them and encourage them to contact their doctor in hopes of early detection. The earlier the detection the better chances you or a family member has of not becoming one of the 15,000.
Source by Kimberly Jean
from Home Solutions Forev https://homesolutionsforev.com/ovarian-cancer-more-deadly-than-breast-cancer/ via Home Solutions on WordPress
0 notes
Text
Diagnosis and Treatment of Epithelial Ovarian Cancer
Ovarian tumor speaks to around 25% of all female genital tract malignancies. In any case, there are more passings from this type of growth every year in the United States than from endometrial disease and cervical tumor consolidated. The lifetime danger of creating unconstrained ovarian tumor is around 1.7%. Epithelial ovarian malignancy was normal reason 15,520 passings in 2008. Mean age at determination is 60. There has been a huge change in the multi year survival rate for patients with ovarian growth. This is likely a blend of better tumor debulking medical procedures and better chemotherapeutic choices.
Most patients with this sort of ovarian malignancy don't have signs or manifestations until the point when ailment spreads to the upper mid-region. 70% of patients give propelled sickness. Manifestations for beginning time ovarian tumor can incorporate nonspecific pelvic inconvenience, urinary recurrence and blockage which are caused by a broadening pelvic mass. With cutting edge malady, patients encounter stomach torment, swelling, anorexia, sickness and stoppage.
The best tumor marker for ovarian malignancy is CA 125. Minor rises in CA 125 can likewise be found in endometriosis, amiable tumors, fibroids and in pregnant and baby blues ladies. Furthermore, direct rise of CA 125 can be seen in other adnocarcinoma, for example, bosom and endometrial disease. The affectability of CA 125 is 70% to 80% and the specificity is 98.6% to 99.4%. Nonetheless, in the normal hazard populace with low commonness of ovarian malignancy, the false positive can be unsatisfactorily high.
The National Cancer Institute suggests screening for ovarian female malignancy with known hereditary disorders related with this illness and for ladies with solid family history. Routine screening of ladies without family history of ovarian growth isn't suggested. The known hereditary disorders incorporate genetic bosom and ovarian malignancy disorder related with BRCA 1, BRCA 2 and Hereditary Nonpolyposis Colorectal Cancer Syndrome (HNPCC). The total danger of ovarian growth within the sight of either BRCA 1 or BRCA 2 transformation ranges from 16% to 60%. For patients with HNPCC disorder, the lifetime danger of ovarian malignancy is 9% to 12%.
Epithelial growth represents around 90% of ovarian malignancies. Normal histologies incorporate serous, mucinous, endometroid, transitiona and clear cell composes. Germ cell tumors incorporate dysgerminoma, endodermal sinus tumor, dangerous teratoma embryonal carcinoma or essential choriocarcinoma. Stromal tumors incorporate granulose tumor or Sertoli-Leydig tumor.
Upon beginning introduction, medical procedure is utilized for affirmation and arranging the tumor. Stage I ailment is limited to one or the two ovaries. Stage II includes one or the two ovaries with expansion to the pelvic viscera. Stage III is related with inserts on the abdominopelvic divider or the serosal surface of the liver or includes little entrail or omentum. Stage IV sickness includes inaccessible metastasis. The multi year survival for arrange IA infection and grade 1 or 2 histology is more prominent than 90%. For high hazard organize I malady and stage II ailment, multi year survival is 80%. For patients with organize III sickness after ideal debulking, multi year survival is 20% to 30%. This diminishes to be under 10% for arrange III patients with problematic debulking and stage IV sickness.
Stage I ovarian malignancy with good prognostic highlights can be treated with medical procedure alone. For ladies with high hazard, beginning period malignancy (Stage I review 3 or stage II infection), adjuvant chemotherapy with platinum based specialists demonstrate a 11% change in movement free survival and 8% change in general survival. For organize III and IV infection, the present standard of care incorporate maximal endeavor at careful cytoreduction taken after by chemotherapy with platinum based operators.
Ideal debulking is a critical part in the treatment of malignancy in the ovaries. Review information have demonstrated that survival is better for ladies who get chemotherapy within the sight of low volume illness. In the setting where ideal careful cytoreduction can't be accomplished, an elective approach is for the patient to get chemotherapy in advance. For patients who have a fractional reaction to neoadjuvant chemotherapy, it might be suitable to endeavor careful evacuation of naturally visible illness around then.
With respect to the standard of tend to cutting edge ovarian-type growth, contemplates have demonstrated that paclitaxel/cisplatin blend is better than cyclophosphamide/cisplatin mix. Later investigations demonstrated that carboplatin/paclitaxel is at any rate as successful as cisplatin/paclitaxel.
Intraperitoneal chemotherapy is an engaging methodology for treating a malady that is to a great extent limited in the peritoneal space. GOG 172 which was a stage III clinical preliminaries exhibited that this territorial approach brought about prevalent movement free survival and in general survival when contrasted and the intravenous approach alone. The drawback of this approach incorporates neighborhood danger, and necessity for intraperitoneal catheter arrangement.
On account of the high repeat rate in patients with cutting edge ovarian disease, the issue of whether solidification chemotherapy may enhance time to movement and generally speaking survival was inspected in a stage III preliminary looking at 3 and 12 cycles of taxol. Movement free survival supported the 12 cycle arm. Be that as it may, generally speaking survival was not diverse between the two arms. In this manner, the oncologist needs to talk about with the patient and enable them to choose whether the enhanced movement free survival legitimizes toxicities including fringe neuropathy and alopecia.
For some patients with cutting edge ovarian tumor who have an underlying treatment reaction, malady backslides at a later time. The treatment of patients with intermittent ailment or safe ailment should be individualized. For individuals with long treatment free interim, comparable medications many be reused. There are likewise various single specialist drugs with movement in ovarian tumor. These incorporate altretamine, bevacizumab, docetaxel, etoposide, gemcitabine, liposomal doxorubicin, paclitaxel, tamoxifen, topotecan and vinorelbine.
Radiation can likewise assume a part in the concealment of a few patients with repetitive ovarian tumor. Indications, for example, torment from becoming pelvic mass or bone metastasis can be vindicated. Rarely cerebral metastasis can create which can likewise be treated with radiation.
The best treatment of ovarian malignancy needs a group approach between the essential care doctor, gynecological oncology specialist, therapeutic oncologists and radiation oncologists. As more chemotherapeutic operators wind up accessible and as we additionally comprehend the science of epithelial ovarian malignancy, we plan to additionally enhance the general survival and personal satisfaction of our patients.
Gigi Q. Chen, MD, got her restorative oncology and hematology preparing at University of California at Davis. She currently rehearses at Diablo Valley Oncology and Hematology at the California Cancer Research and Treatment Center at Pleasant Hill, California. Her office represents considerable authority in exhaustive, bleeding edge treatment of all types of malignancy through clinical preliminaries, chemotherapy, organic medications, analytic imaging, and radiation. She is on the therapeutic staff of John Muir Medical Center in both Walnut Creek and Concord and the San Ramon Regional Medical Center.
Article Source: https://EzineArticles.com/master/Gigi_Chen,_M.D./492993
Article Source: http://EzineArticles.com/3339129
0 notes