#Hyperglycemia vs diabetes
Explore tagged Tumblr posts
Text


#Is type 2 diabetes hyperglycemia or hypoglycemia#Hyperglycemia vs hypoglycemia symptoms#Which is more dangerous hypoglycemia or hyperglycemia#Hypoglycemia vs hyperglycemia treatment#Difference between hyperglycemia and hypoglycemia ppt#Hyperglycemia symptoms#Hypoglycemia vs diabetes#Hyperglycemia vs diabetes
0 notes
Text
Cool water, or a cool can from the fridge (not the freezer) on your wrists can help cool you down, basically something cool on your pulse points can help cool your body down gradually
"Cold Blankets" exist and are awesome, search them online. They literally make you feel like you are wrapped in ice without needing to be wet or requiring any electricity
UV blocking SPF hats clothing can be very handy if you must cover for religious/cultural reasons. Buy a size up and go for as much ease between you and the fabric as you can for max air flow.
Tiny desktop sized swamp coolers exist and can make a really good cone of cold, but if you have pets and small children do not use the scent diffuser option on them.
Remember, this is the coolest summer of the rest of your life, and wait until Winter to buy an A/C if you can, it'll be cheaper, meaning you can get more A/C for less money than if you buy one while it's hot.
They make cooling mats that are pressure activated for pets AND people! They aren't very expensive and literally you or your pet just needs to lay on it and it becomes cool.
Water your potted plants at night, the water will have more time to soak in vs. evaporate, same with watering your garden. If you have a lawn... first of all, why? But if you must water it, do it in the evening after the sun goes down, (But please consider replacing it with locally native pollinator attracting flowers, or trees)

This is a comprehensive list, not a complete one. You can check your specific meds (and you should) by searching the medication's generic name and "heat sensitivity" If you are Diabetic, and especially if you are more prone to Hypoglycemia (not Hyperglycemia, which requires insulin use and should avoid sugars) You are more prone to blood glucose drops, be ready to test and treat more often.
And yes You can have Gatorade. (also they do make sugar-free Gatorade now, so if your Endo/Nutritionist allows you to have that particular artificial sweetener, you can have it too)

For all of the northerners that stood up for Texas during our freeze and said, "Don't make fun of them, they've never dealt with this before. Their infrastructure isn't made for snow and freezing."
This one is for you.
Where I live 108°F with 80% humidity with no wind is normal.
Pacific North West is dealing historic best waves 35-40°C or 95-105°F.
First of all. Don't make fun of them for bitching about the heat. Just like Texas isn't built for a freeze and our pipes burst, Pacific North West isn't built for heat and a lot of their homes don't have AC.
If you live somewhere with a high humidity like 80+ HUMIDITY IS NOT YOUR FRIEND. The "humidity makes it feel cooler" is a lie once it gets beyond a point.
If you live somewhere with a lower humidity, misters are nice to cool off outside.
Once you get over 90°F (32°C) a fan will not help you. It's just pushing around hot air. (I mean if you can't afford a small AC unit because they're expensive as hell, by all means a fan is better than nothing).
If you have pets, those portable AC units aren't safe. If your pets destroy the outtake thing, it'll leak CO2. Window units are safer.
Window AC units will let mosquitoes or other small bugs in. Sucks, but that's life.
Now is not the time to me modest. If you have to cover for religious reasons, by all means. If you don't, I've seen people wear short shorts and a swim top. It's not trashy if it keeps you from getting heat stroke.
If you do have to cover up for religious reasons, look for elephant pants or something similar. They're made with a breathable material.
Shade is better than no shade, but that shit it just diet sun after some point. Don't think shade will save you from heat stroke.
I know the "drink your water" is a fun meme now, but if you're sweating excessively you need electrolytes. Drink Gatorade, Powerade, or Pedialite PLEASE. I don't care if you're fucking sitting in one spot all day. That shit WILL save you from heat stroke.
Most importantly. RESEARCH THE DIFFERENCE BETWEEN HEAT STROKE AND HEAT EXHAUSTION PLEASE!
If you're diabetic and can't drink Gatorade, mix water, fruit juice, and either lite salt or pink salt
If you can afford it, cover windows with thick curtains to insulate the house
If you have tile floors, lay on them with skin to tile contact. If you don't, laying your head on cool counters works too.
If the temperature where you're at is hotter than your body temperature, don't wear heat wicking clothing. Moisture wicking is safe though.
Check your medication labels. Many make you more susceptible to sun and heat
-Room temperature water will get into your body faster. This is something I learned doing marching band in high summer in Georgia, and it saved all of our asses. Sip it, don't gulp it, especially if you're getting into the red; same goes for whatever fluid you're drinking. And just in general drink during the day.
-If you are moving from an air conditioned space to an un-air conditioned space, if at all possible try to make the shift gradual. When my dad and I were working outside and in un-ac houses a few years ago, he'd turn the air down to low in the truck about ten-fifteen minutes before we got where we were going. This way your body doesn't go from low low temps to high temps. S'bad for you.
-If you can, keep your lights off during the day. Light bulbs may not generate a lot of heat, but the difference is noticeable when it gets hot enough. I literally only turn my bedroom light on in the evening when it gets too dark.
Don't be afraid to just like... pour water on yourself if you need to. The evaporation will cool you off.
Put your hand to the cement for 15 seconds. If you can't handle the heat, it'll burn your dog's paws. Don't let them walk on it.
Dogs with flat faces are more prone to heat stroke. Don't leave them out unsupervised.
Frozen fruit is delicious in water.
Wet/Cold hat/handkerchief on your head/neck will help you stay cool.
Pickle juice is great for electrolytes! You can even make pickle juice Popsicles!
Heat exhaustion is more, "drink water and get you cooled off." Heat stroke is more "Oh my god call 911."
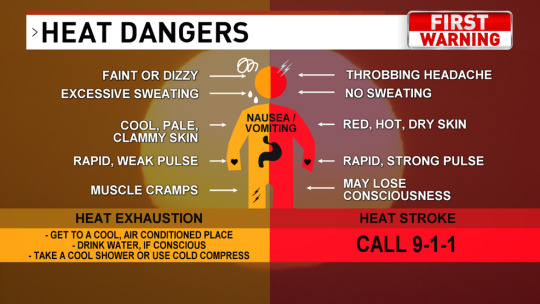
Image Description provided by @loveize
[Image description: an infographic showing the difference between heat exhaustion and heat stroke. The graphic is labeled "Heat Dangers: First Warning." Signs of heat exhaustion: faint or dizzy, excessive sweating, cool, pale, clammy skin, rapid, weak pulse, muscle cramps. If you think you or someone else may be experiencing heat exhaustion, get to a cool, air-conditioned place, drink water if conscious, and take a cool shower or use cold compress. Signs of heat stroke: throbbing headache, no sweating, red, hot, dry skin, rapid, strong pulse, may lose consciousness. If you think you or someone else may be experiencing heat stroke, call 911. End description]
Be safe.
-fae
122K notes
·
View notes
Text
CelluCare Blood Sugar
Introduction
Blood sugar management is a crucial aspect of maintaining overall health and preventing chronic diseases such as diabetes. With the rise in lifestyle-related health issues, finding effective and reliable solutions to manage blood sugar levels has become a priority for many. One such solution is Cellucare a dietary supplement designed to help regulate blood sugar levels and promote overall well-being. This article will delve into the importance of blood sugar management, explore the features and benefits of CelluCare Blood Sugar, and provide insights into its efficacy based on scientific research and user testimonials.
Understanding Blood Sugar Levels
What is Blood Sugar?
Blood sugar, or blood glucose, is the main sugar found in the blood and the primary source of energy for the body's cells. It comes from the food we eat and is carried to the cells via the bloodstream. Maintaining a balance in blood sugar levels is vital for the body's proper functioning.
How is Blood Sugar Regulated in the Body?
The regulation of blood sugar levels is a complex process involving the hormone insulin, produced by the pancreas. Insulin facilitates the uptake of glucose by cells, where it is either used for energy or stored for future use. When blood sugar levels rise after eating, the pancreas releases insulin to help lower the glucose levels in the blood.
The Role of Insulin
Insulin acts as a key that allows glucose to enter cells from the bloodstream. Without sufficient insulin, or if the body's cells become resistant to insulin's effects, blood sugar levels can become elevated, leading to various health issues.
Normal vs. Abnormal Blood Sugar Levels
Normal blood sugar levels typically range between 70 and 130 mg/dL before meals and less than 180 mg/dL after meals. Abnormal blood sugar levels, whether too high (hyperglycemia) or too low (hypoglycemia), can cause a range of symptoms and complications. Hyperglycemia, in particular, is a major concern as it can lead to serious health problems if left unmanaged.
Causes and Risks of High Blood Sugar
Causes of High Blood Sugar (Hyperglycemia)
High blood sugar levels can be caused by several factors, including:
Poor dietary choices (high intake of sugary and refined foods)
Lack of physical activity
Stress and illness
Certain medications
Insufficient insulin production or insulin resistance
Risk Factors for Developing High Blood Sugar
Several risk factors can increase the likelihood of developing high blood sugar, including:
Family history of diabetes
Obesity or being overweight
Sedentary lifestyle
Age (risk increases with age)
High blood pressure and cholesterol levels
Short-term and Long-term Effects of High Blood Sugar on Health
Short-term effects of high blood sugar can include fatigue, frequent urination, increased thirst, and blurred vision. Long-term effects are more severe and can lead to complications such as:
Cardiovascular diseases
Nerve damage (neuropathy)
Kidney damage (nephropathy)
Eye damage (retinopathy)
Increased risk of infections
Introduction to CelluCare Blood Sugar
What is CelluCare Blood Sugar?
CelluCare Blood Sugar is a dietary supplement formulated to help regulate blood sugar levels naturally. It combines a blend of ingredients known for their beneficial effects on blood sugar management, offering a convenient and effective solution for individuals looking to maintain healthy glucose levels.
Key Ingredients and Their Functions
CelluCare Blood Sugar contains a mix of scientifically backed ingredients, including:
Berberine: Known for its ability to improve insulin sensitivity and lower blood sugar levels.
Chromium: Helps in the metabolism of carbohydrates and fats, enhancing insulin action.
Cinnamon Extract: Contains compounds that mimic insulin and increase glucose uptake by cells.
Alpha Lipoic Acid: A powerful antioxidant that helps reduce oxidative stress and improve insulin sensitivity.
How It Works in the Body to Manage Blood Sugar Levels
CelluCare Blood Sugar works by enhancing the body's natural ability to regulate blood sugar. Its ingredients help improve insulin sensitivity, reduce glucose absorption in the intestines, and promote the uptake of glucose by cells. This multi-faceted approach ensures a comprehensive solution to maintaining healthy blood sugar levels.
Visit Here To Official Website>
#Cellucare
#CellucareReviews
#CelluCareBloodSugar
0 notes
Text
Blood Sugar Maintaining Methods

Introduction to Blood Sugar
What is blood sugar?
Importance of maintaining balanced blood sugar levels
Factors Affecting Blood Sugar Levels
Role of insulin and glucagon
Impact of diet and nutrition
Influence of physical activity
Stress and its effect on blood sugar
Understanding Blood Sugar Regulation
How the body regulates blood sugar levels
Hormonal control (insulin and glucagon)
Liver's role in glycogen storage and release
Signs and Symptoms of Imbalanced Blood Sugar
Hypoglycemia (low blood sugar)
Hyperglycemia (high blood sugar)
Long-term implications of uncontrolled blood sugar levels
Monitoring Blood Sugar Levels
Importance of regular monitoring
Devices for blood sugar measurement (glucometers, continuous glucose monitors)
Target blood sugar ranges for different individuals
Dietary Strategies for Blood Sugar Management
Importance of balanced meals
Impact of carbohydrates on blood sugar
Glycemic index and glycemic load
Role of fiber and protein in blood sugar stability
Nutritional Supplements for Blood Sugar Support
Vitamins and minerals (e.g., chromium, magnesium)
Herbal supplements (e.g., cinnamon, bitter melon)
Omega-3 fatty acids and their role
Physical Activity and Blood Sugar Control
Benefits of exercise for blood sugar regulation
Types of exercises (aerobic vs. resistance training)
Timing of exercise in relation to meals
Stress Management Techniques
Impact of stress on blood sugar levels
Relaxation techniques (meditation, deep breathing)
Importance of adequate sleep for stress management
Medication and Insulin Therapy
Types of diabetes medications (oral vs. injectable)
Insulin therapy for type 1 and type 2 diabetes
Side effects and considerations
Lifestyle Modifications for Blood Sugar Health
Smoking cessation and its impact
Alcohol consumption moderation
Weight management strategies
Alternative Therapies and Their Efficacy
Acupuncture and acupressure
Yoga and tai chi for stress reduction
Biofeedback techniques
Educational Resources and Support Groups
Role of diabetes educators
Online resources and apps for tracking blood sugar
Support groups and community resources
Tips for Dining Out and Managing Social Situations
Making healthy choices when eating out
Alcohol consumption tips
How to handle peer pressure
Long-Term Strategies for Blood Sugar Maintenance
Setting realistic goals
Tracking progress and making adjustments
Celebrating successes and staying motivated
Challenges and Common Pitfalls in Blood Sugar Management
Factors that can derail progress
Dealing with setbacks and staying resilient
Importance of self-care and mental health
Research and Developments in Blood Sugar Management
Latest advancements in diabetes treatment
Promising research studies and clinical trials
Future trends in blood sugar monitoring and treatment
Personal Stories and Inspirational Journeys
Success stories of individuals managing blood sugar effectively
Overcoming obstacles and achieving health goals
Encouragement for readers on their own journey
Conclusion: Empowering Readers for Blood Sugar Control
Recap of key points in blood sugar management
Encouragement to take proactive steps
Inspiring readers to prioritize their health
Call to Action: Start Your Journey to Better Blood Sugar Control Today
Link to recommended products or services
Encouragement to seek medical advice if needed
Invitation to engage with the community and share experiences
Complete reading with details visit Here...
Continue Reading in details....
#public health#healthyhabits#health insurance#good health#healthy relationships#healthy weight loss#healthy diet#blood#blood sugar#diabetes#healthyfood#healthy eating#health wealth happiness#diabetic
0 notes
Text
The Game-Changer: Real-Time CGM vs. Traditional Glucometers for Type 1 Diabetes Management
Introduction:
Living with Type 1 Diabetes (T1D) requires vigilant blood sugar monitoring, and advancements in technology have introduced a revolutionary tool - Continuous Glucose Monitoring (CGM) systems. In this blog, we'll delve into the benefits of real-time CGM over traditional glucometers for individuals navigating the complexities of Type 1 Diabetes.
Understanding the Basics:
Before exploring the advantages of real-time CGM, let's briefly distinguish between traditional glucometers and CGM systems. Glucometers provide point-in-time blood glucose readings, requiring a fingerstick to obtain results. On the other hand, CGM systems continuously monitor glucose levels throughout the day and night, offering real-time data and trends.
Continuous Insight:
Traditional glucometers provide a single data point, offering a snapshot of blood sugar levels at a specific moment. In contrast, CGM systems provide a continuous stream of data, allowing users to observe trends, patterns, and fluctuations in glucose levels over time.
Real-time information empowers individuals to make informed decisions about insulin dosages, meal planning, and physical activity, leading to more precise diabetes management.
Early Detection of Trends:
CGM systems alert users to impending highs and lows before they become critical. This proactive approach helps prevent severe hypoglycemia or hyperglycemia, allowing for timely intervention and adjustments to insulin therapy.
Reduced Fingerstick Dependence:
Traditional glucometers necessitate frequent fingersticks, which can be uncomfortable, especially for children. CGM systems minimize the need for constant fingersticks, offering a more convenient and less invasive method of glucose monitoring.
Enhanced Quality of Life:
Real-time CGM systems contribute to a better quality of life for individuals with Type 1 Diabetes. The continuous data stream reduces the stress associated with constant monitoring, allowing for increased peace of mind for both users and their caregivers.
Integration with Smart Devices:
Many CGM systems seamlessly integrate with smartphones and smartwatches, providing real-time glucose data at the users' fingertips. This connectivity facilitates quick access to crucial information, fostering a sense of control and empowerment.
Customized Alerts and Insights:
CGM systems can be customized to provide alerts for specific glucose thresholds. This feature ensures that users receive timely notifications about potential highs or lows, enabling them to take prompt action.
Conclusion:
The shift from traditional glucometers to real-time CGM systems represents a significant leap forward in Type 1 Diabetes management. The continuous, real-time insights offered by CGM technology empower individuals to proactively manage their condition, leading to improved overall health and a more flexible, fulfilling lifestyle. As technology continues to advance, the landscape of diabetes management is evolving, providing hope and enhanced tools for those living with Type 1 Diabetes.
0 notes
Text
Spotting the Warning Signs: Hypoglycemia vs. Hyperglycemia
What are the signs and symptoms of hypoglycemia and hyperglycemia? What is Diabetes Mellitus? What is the role of insulin? What are the different types of diabetes mellitus? What are the first common signs of diabetes mellitus? What causes hypoglycemia (low blood sugar level)? How do you manage hypoglycemia? How can you prevent hypoglycemia? What causes hyperglycemia? How can you maintain a…

View On WordPress
0 notes
Text
Evaluation of Glycemic Control Obtained from NPH Insulin in Patients Experiencing Corticosteroid-Induced Hyperglycemia

Authored by Megan N Hodges
Abstract
Objective:To compare the safety and efficacy of neutral protamine Hagedorn (NPH) insulin to other antidiabetic regimens in the treatment of corticosteroid-induced hyperglycemia in non-critically ill; hospitalized patients.
Methods:This retrospective cohort included patients treated with methylprednisolone or prednisone concomitantly with NPH or other antidiabetic medications for at least two days. Patients were screened for inclusion in reverse chronological order and matched based on gender; age; body mass index; steroid dose; and history of diabetes. The primary objective was mean daily blood glucose (BG). Secondary outcomes included percentage of readings between 70mg/dL-180mg/dL; median daily BG; number of hypoglycemic events; daily steroid to NPH ratios; and mean weight-based dose of NPH for each 10mg increment of prednisone when BG readings were within goal.
Results:A total of 72 patients were included in each arm. The primary efficacy endpoint of mean daily BG ranged from 111-217mg/dL in the control group and 163-228mg/dL in the NPH arm; however; there were no statistically significant differences (p>0.05). Overall rates of hypoglycemia were slightly lower in the NPH group but with no statistically significant differences (0.61% vs. 1.12%; p = 0.51).
Conclusions:NPH; compared to other regimens; may not have an impact on achieving glycemic controlin corticosteroid-induced hyperglycemia.
Keywords: Diabetes mellitus; Corticosteroid; Hyperglycemia; Neutral protamine hagedorn
Go to
Introduction
Systemic corticosteroids are commonly used for a wide variety of medical conditions on both an inpatient and outpatient basis for the treatment of inflammation and immune suppression. Acute asthma and chronic obstructive pulmonary disease (COPD) exacerbations, rheumatoid arthritis, and organ transplant comprise just a few of the many indications. Although corticosteroids are highly efficacious, its use is limited by many serious adverse effects during acute and chronic treatment [1-6]. During short-course therapy, patients commonly develop hyperglycemia. Several studies have reported odds ratios from 1.5 to 2.5 for the development of new-onset diabetes relating specifically to steroid utilization [2-5]. Corticosteroids also have the potential to significantly worsen hyperglycemia in patients with a history of diabetes mellitus [1,7] . This represents a substantial health risk to patients since studies have found a correlation between hyperglycemia and decreased wound healing, increased length of stay (LOS) and mortality in hospitalized patients [8].
Several studies have been undertaken to better understand the exact mechanism of steroid-induced hyperglycemia. In patients receiving short-term therapy, skeletal muscle and hepatic cells develop reduced insulin sensitivity leading to decreased glucose uptake. During the post-prandial phase in particular, blood glucose (BG) levels are further elevated by impaired suppression of glucose production secondary to hepatic insulin resistance [6].
Insulin acts on liver, adipose tissue, and skeletal muscle to regulate metabolism of carbohydrates, fat, and protein. A cross- sectional review of 66 patients suggested that patients receiving ≥10mg per day of prednisolone compared to those not receiving corticosteroids experience afternoon and evening hyperglycemia despite receiving basal-bolus insulin regimens [9]. Neutral protamine Hagedorn (NPH) is a crystalline suspension of human insulin with protamine and zinc, which makes it intermediate acting insulin. Neutral protamine Hagedorn insulin produces a peak effect four to eight hours after administration with a total duration of sixteen to eighteen hours. These kinetic properties closely mirror the action of prednisone. Methylprednisolone also has a similar duration of action with a shorter onset of one to two hours [10-12]. In theory, the pharmacokinetic principles of subcutaneous NPH make it a prime candidate for the treatment of glucocorticoid induced hyperglycemia. The objective of this study is to compare NPH to other antidiabetic agents in the treatment of steroid-induced hyperglycemia.
Go to
Materials and Methods
Study design
This single-center retrospective cohort study evaluated patients at a 450-bed community hospital. The trial was approved by the hospital Institutional Review Board before data collection began. Due to the retrospective nature of the study, informed consent was not necessary. All data was obtained through electronic medical records.
Eligibility requirements included age ≥18 years, concurrent treatment with methylprednisolone or prednisone with NPH insulin or other antidiabetic medications for at least two days, and steroid doses ≥10mg prednisone equivalent on day one. Patients receiving NPH for the treatment of steroid-induced hyperglycemia were included in the treatment arm and patients being treated with any other combination of antidiabetic medications were evaluated in the control arm. Patients in the NPH arm with glargine insulin as a home medication were included in the study if the glargine titration was limited to± 20% during the hospitalization since a 20% reduction is recommended at admission to decrease risk of hypoglycemia and to limit confounding adjustments to the glargine during steroid titration [13]. Patients were not eligible for inclusion in the NPH treatment arm if they received any other antidiabetic medications in addition to NPH, rapid acting insulin, or glargine as described above. Oral antidiabetic agents were allowed in the control arm; however, per institutional protocols and American Diabetes Association (ADA) recommendations these agents are routinely discontinued upon admission to the hospital [14]. Patients admitted with a BG>400mg/dL, those in the intensive care unit, patients on insulin pumps, and pregnant patients were excluded. Patients were also excluded if they had less than two BG readings per day or no recorded weight.
Patient characteristics were identified through queries of the hospital electronic medical record. Starting October 2014 through October 2012, all patients receiving ≥10mg of prednisone equivalent of methylprednisolone or prednisone for at least one day were consecutively screened for inclusion in reverse chronological order. After patients were identified for analysis in the NPH arm, controls were then matched by manual chart review to the NPH patients based on age, gender, body mass index (BMI) classification, steroid dose on day one, and history of diabetes.
Study outcomes and definitions
The primary outcome was the mean daily BG. Secondary outcomes included the percent of BG readings within a preset goal of 70mg/dL to 180mg/dL. All BG readings were incorporated in the analysis regardless of the patients’ fasting state, thus a higher goal of <80mg/dL was established based on the ADA random BG recommendations for non-critically ill, hospitalized patients. The low end of this range was based on the ADA definition of hypoglycemia, which is BG<70mg/dL [14]. Other secondary objectives included median daily BG, number of hypoglycemic and severe hypoglycemic events with and without intervention. Intervention was defined as intake of juice, oral glucose tablets or administration of glucagon or dextrose 50% water. As defined by the ADA, BG<40mg/dL is considered severe hypoglycemia. [14] Daily steroid to NPH ratios and steroid to NPH ratios on the index day were also collected. The index day was defined as the last day of steroid therapy or the day of discharge if the patient continued steroids as an outpatient. Mean weight-based dose of NPH for each 10mg increment of prednisone equivalent (8mg methylprednisolone) was collected for days on which all BG readings were within the goal range with the intention of formulating a standardized NPH protocol. Two subgroup analyses were performed on mean blood glucose to compare NPH to sliding scale insulin alone and to compare NPH to other antidiabetic regimens in patients admitted with a documented history of diabetes.
Statistical analysis
The outcomes data was analyzed to determine the glycemic control achieved with each regimen by looking at all available BG readings throughout the patients’ hospitalizations excluding repeat readings within 10 minutes. Baseline characteristics and outcomes were reported using means, medians, and standard deviations for interval level data and percentages for nominal and ordinal level data. Baseline demographics and study outcomes were compared between groups using Student’s t-test for continuous data and Fisher’s exact or chi-square test for categorical data. A p value of <0.05 indicated statistical significance. All analyses were performed with IBM SPSS Statistics for Windows.
To the authors’ knowledge, the only other published trials addressing this treatment regimen included a maximum of 66 patients in each arm and did not find a statistically significant difference; therefore, power was not calculated [15-17]. Based on available information, 72 patients were included in each arm.
Go to
Results
A total of 241 patients were identified through the pharmacy informatics system for potential inclusion in the NPH arm. Of these patients, 72 were eligible based on the inclusion and exclusion criteria. Patients were well matched in regards to baseline demographics (Table 1). The only significant difference between groups was total LOS, which was significantly higher in the NPH group (6.98days vs. 4.88days, p =0.003). However, no differences existed among indication for steroid utilization. Baseline glycemic control was similar between groups: mean BG of 186mg/dL in the NPH group and 177mg/dL in the control group at admission (p=0.492).
*There were no significant differences between the two groups except for LOS (p=0.003)
The primary efficacy endpoint of mean daily BG ranged from 111-217mg/dL in the control group and 164-228mg/dL in the NPH arm; however, no statistically significant differences were detected for any day (Figure 1) & (Table 2). The results on the index day (Table 3) showed numerically though not statistically improved glycemic control for the control group compared with the NPH arm with a mean BG of 195mg/dL for the NPH group and 179mg/dL for the control group (p =0.135).
In regards to efficacy, the only statistically significant difference found was in the percent of BG readings between 70- 180mg/dL for day 1 in favor of the control arm (41.9%vs.28.1%, p=0.01) (Table 4). No trends were observed for the steroid: NPH ratios or weight-based NPH doses. Consistent glycemic control was achieved faster in the control arm; mean daily BG readings were <180mg/dL starting on day 5 compared to day 10 in the NPH arm (Figure 1). In contrast to a previous study, the NPH arm received a significantly higher total daily insulin dose on the index day compared to the control arm (0.37unit/kg vs. 0.21unit/kg, p=0.002). However, these differing results are likely accounted for by the inclusion of glargine insulin in the NPH arm [15].
aData presented as mean ± standard deviation.
Glycemic control was similar in both subgroup analyses (patients with a history of diabetes and those receiving only slide scale insulin compared to NPH) (data not shown). In patients with a documented history of diabetes, the mean BG on the index day was 197mg/dL in the NPH arm compared to 185mg/dL in the control arm (p=0.313). When comparing NPH and sliding scale insulin versus sliding scale insulin alone, BG on the index day was 187mg/dL in the NPH group and 174mg/dL in the sliding scale insulin group (p=0.246).
Overall, the incidence of hypoglycemia was low in both arms, with more events occurring in the control arm (Figure 2). A total of 9(0.61%) hypoglycemic episodes occurred in the NPH arm and 15(1.12%) in the control arm (p=0.51). Only one episode of severe hypoglycemia was noted in the control arm.
Go to
Discussion
When interpreting these results, it is important to note that the number of patients evaluated dropped considerably each consecutive day. By day eleven, only two patients remained in the NPH arm compared to one patient in the control arm. Although daily trends are important to consider, the results on the index day may provide the most insight on glycemic control.
Several limitations exist within this study. Due to the retrospective design, there is also potential for data extraction errors and chart documentation errors. Another limitation is the lack of standardized NPH dosing at this institution. The doses prescribed varied greatly between patients, and the majority of weight-based NPH doses were much lower than other institution protocol recommendations [1,8-15]. Overall glycemic control was also relatively poor in both groups compared to previous studies. This could be partly due to higher daily steroid doses and lack of Diabetes Management Services [15]. Lastly, patients in the NPH group had a significantly longer LOS compared to the control group, which could have resulted in worse overall BG control with increased time of steroid exposure. However, there were no measurements to determine severity of illness to help explain the extended LOS. Although this study was conducted at a single community hospital with a limited sample size, it is the largest study to evaluate this topic.
Despite a lack of evidence, several institutions have implemented protocols for the use of weight-based NPH dosing for hyperglycemic patients treated with steroids. The doses usually range from 0.1units/kg to 0.5units/kg depending on steroid doses [1,8-15]. One retrospective cohort of 120 patients found no difference between NPH versus glargine to control steroid-induced hyperglycemia in patients with type 2 diabetes [15]. A randomized control trial of 50 patients evaluated whether an NPH-based insulin regimen is safer and more effective than a glargine-based regimen in hospitalized adults with prednisolone-induced hyperglycemia. The initial daily insulin dose was 0.5units/kg or 130% of the current daily insulin dose. No differences in either outcome was observed [16]. Another randomized control trial of 53 patients examining glargine versus NPH in type II diabetics with respiratory disease and glucocorticoid induced hyperglycemia yielded similar results [17]. This current trial included patients regardless of their diabetes history or steroid indication. Despite the similarity in pharmacokinetic profiles between corticosteroids and NPH, this approach may not offer better glycemic coverage in steroidinduced hyperglycemia over other regimens as shown in this trial and in the studies by Dhital et al. [15], Ruiz de Adana et al. [17], & Radhakutty et al. [16]. Additional large, randomized-controlled trials are warranted to further help direct future evidence-based treatment strategies for steroid-induced hyperglycemia.
Go to
Conclusion
Based on the results of this study, no conclusions can be determined about the efficacy of NPH insulin for corticosteroidinduced hyperglycemia. Patients receiving standard care (control group) appeared to have better glycemic control over patients in the NPH arm; however, the resulting differences were not statistically significant and hampered by small sample size.
To Know More About Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
#Juniper Publishers#open access journals#peer review journals#high impact journals in juniper publishers#Diabetes#obesity
0 notes
Text
Can Your Character Survive... Altered Mental Status
Character E is confused. She thinks she's talking to someone besides Character F and accidentally admits that she has a crush on F while F is treating her injury. Oops.
Or, F is trying to get E out of the enemy base and E keeps laughing when F shushes her, attracting the attention of the guards
Whether for comedy or tension, altered mental status can add a fun wrinkle to your plot. But, what causes altered mental status and how do you make sure E survives?
STOPEATS
The big kahuna of the altered mental status world is the acronym STOPEATS. If it makes your brain go a bit wonky, it's probably included in STOPEATS.
Sugar
If E is a diabetic and lost track of her sugar intake, she could suffer from altered mental status as a part of hyperglycemia. If F knows E has diabetes, he can hopefully guess at the cause of her confusion and help her take her medication, or get her to a hospital.
Temperature
When the body gets really cold or really hot, the brain can stop working right. In fact, altered mental status is a key sign of being hypothermic vs. just cold. Ditto with heat stroke. Hopefully, the environment makes if obvious to F what is causing E's weird behavior. He can treat her by bringing her out of the cold or heat.
Oxygen
youtube
Hypoxia occurs when the brain is starved of oxygen, such as at a high altitude. It is most common in mountain climbers and pilots, such as the one in this video who reports having "no control" of his aircraft but otherwise, is not concerned at all about the situation. Astronomers may also suffer from hypoxia on occasion.
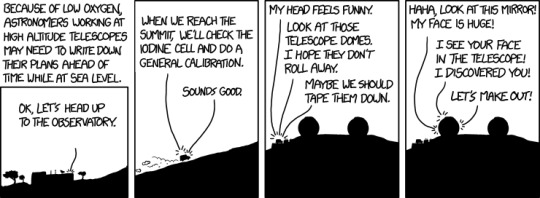
XKCD 1463: Altitude
Hypoxic people behave as if drunk. They are often euphoric, may speak slowly, and will act confused. The key treatment for high-altitude hypoxia is reducing altitude ASAP. In the video, you can hear the air traffic controller trying to coax the pilot lower. He knows he doesn't need the pilot to land—as soon as he can breathe a little better, he'll remember how to fly be able to land himself.
Pressure
If a brain injury causes bleeding in the skull, that blood has nowhere to go and can build up pressure. This causes the brain to lose functioning and is called intracranial pressure (ICP). It's the worst type of traumatic brain injury (TBI) besides one that just kills E outright.
If E is suffering from ICP, she'll probably be confused and behaving erratically. She may have gaps in her memory as well. Most likely, she'll also report "the worst headache of my life"—literally. In training, we were told to look out for that exact phrase when diagnosing head taumas. In later stages of ICP, E may also vomit, a lot.
Treatment involves getting to surgery ASAP so a doctor can cut open her skull and relieve some of the pressure. For obvious reasons, that is not something we attempt in the field.
Electricity
I'll be honest: I think they just wanted the acronym to work when they made this one E. What they actually mean in most cases is seizures. The classic seizure is a grand mal seizure, which involves the muscles tensing, twitching, etc. But seizures come in all shapes and sizes. For some, a seizure might mean smelling something that isn't there, or hearing music, or a single twitching muscle. Because seizures are unauthorized electrical activity in the brain, they can cause disorientation and erratic behavior.
Often, coming out of a seizure can be quite disorienting too. If F is helping E through a seizure, he should first try to prevent her from harming herself. If she's banging her head against the wall, that means putting a hand or pillow there. If she's near a table, that means moving the table. (NO sitting on / restraining people with seizures and NO putting stuff in their mouth! No! Why? You want them to choke? No!). As she recovers, F can remain calm, help her understand what happened if she needs it, and get her further care if requested.
Altitude
As with temperature, both very high and very low altitudes can cause brain problems (if you are beginning to suspect the brain is just a picky organ, you'd be correct). Scuba divers who ascend too quickly can suffer from nitrogen narcosis, which can lead to euphoria, confusion, memory loss, difficulty concentration, etc. (all classic signs of altered mental status).
If E goes too high, say, on a mountain, she could suffer from High-Altitude Cerebral Edema (HACE—controversial opinion but high-altitude stuff has all the good acronyms and names, HACE being but one example). It occurs when the brain swells at a high altitude and leads to confusion, lethargy, and a headache.
Luckily, as with most high-altitude problems, it can be solved quickly by going lower. When in doubt, on a mountain, taking the patient to a lower altitude is probably a good idea.
Toxins
Alcohol, LSD, marijuana, morphine—drugs cause altered mental status, as can bites or stings from venemous animals.
There are as many ways to treat toxins as there are toxins, maybe more, so I leave you with a fun fact the majority of snake bites in the US are people who tried to pick up the snakes.
In the words of Mod N's WFR instructor: "Red near black? Who cares. It's a snake. Why are you messing with snakes?"
Salt
Salt concentrations across cell membranes is one way nutrients travel into and out of cells. If E's blood suddenly has way less salt (electrolytes) than normal, this causes all the nutrients to flow out of her cells and into her blood, starving her organs. Brains run on salt and not having enough salt makes... neurons fire different? Stop firing? Something scientific and complicated. For our purposes: not enough salt = brain go weird.
This is called hyponatremia and is my favorite of all the STOPEATS ailments. Hyponatremic people behave as if drunk. The treatment is to 1) stop chugging water, 2) stop competing in your high-endurance sport (and therefore stop sweating), and 3) drink / eat something salty.
Conclusion
Give your characters altered mental statuses. It will be fun. I promise.
The most easily treatable problems that make brain go weird are: hypoxia and high-altitude cerebral edema.
Please write more characters with hyponatremia.
#ict#cycs#altered mental status#stopeats#writing advice#writing tips#hyponatremia#hypoxia#wilderness medicine
8 notes
·
View notes
Text
Anion gap, alk/acidosis, lipase, A1C, UUN, labs, specialized labs, clinical presentation, BUN, Creatinine
Anion gap (will cover this in more depth with diabetes) is calculated from sodium level – (chloride + bicarbonate). You could do (sodium + potassium) – (chloride + bicarbonate). Potassium contributes so little that it’s often omitted, however. Anion gap means something else is contributing to the acid-base balance, not just the exchange of chloride for bicarbonate, for example.
Metabolic acidosis: Low pH, a low HCO3- concentration. Compensatory hyperventilation that contributes to a decreased pCO2. Most common causes: Inability of kidneys to excrete dietary hydrogen ion load, increase in hydrogen ion generation due to an addition of hydrogen ions or a loss of bicarbonate
Metabolic alkalosis: High pH, a high bicarbonate- concentration, and compensatory hypoventilation that contributes to an increased pCO2. Most common causes: loss of gastric acid from vomiting or nasogastric suction, loss of intravascular volume and chloride from diuretic use. Overtreatment of metabolic acidosis with bicarbonate. Excess of acetate in PN (parenteral nutrition), which becomes metabolized to bicarbonate
A1C distinguishes between diabetes and hyperglycemia associated with metabolic stress
Protein: Again:
First start by converting the protein intake of the patient (94g in this example) to grams of nitrogen. Second, calculate their nitrogen balance. We find that the patient is in negative nitrogen balance. Nitrogen balance should be the same amount of nitrogen coming into the body as is coming out in the urine. Third: Correct the deficit to get into nitrogen balance. Take that -2g of deficit that they are at (take the minus sign away), and multiply that by 6.25g of protein (1g of nitrogen = 6.25g of protein). Correcting the deficit of nitrogen finds that the patient will require 12.5 more grams of protein just to get into nitrogen balance. Fourth, we still need the patient to be in positive nitrogen balance, so, we increase protein and shoot for 2g more protein to promote anabolism (goal for anabolism is +2-4g of nitrogen a day more). So, that low end we are aiming for is 2g of nitrogen: 2N (6.25g of protein/1g of nitrogen) = 12.5g of protein needed to put the patient in positive nitrogen balance. Fifth, we want to try to promote anabolism, so we have to add the amount of protein that puts the patient at nitrogen balance to the amount of protein that puts the patient in positive nitrogen balance, and add the sum of those two to the amount of protein the patient is taking in (the 94g). Hence the new protein goal is 94g + 12.5g + 12.5g = 119g of protein/day or approximately 120g of protein per day.
Remember: even though you prescribed 100g of protein a day, the patient only actually got 94g. So, that’s why you use 94g in these calculations.
A valid 24-hour urine collection can be difficult to collect
Conversion factor of UUN to total nitrogen excretion may not be accurate in certain conditions: burns, major wounds, diarrhea, vomiting
Factor of 0.85 converts UUN to TUN
Assumes that 85% of urinary nitrogen is from urea
Other nitrogen sources in urine= ammonia, proteins
Conditions that alter or increase ammonia excretion will lead to underestimation
Ex if Adam had liver disease and ammonia excretion was higher/ UUN only 75%
◦ UUN = 13 (13/0.75) = 17 (vs 15)
Diminished renal function alters results
For the most part you are addressing whether the patient is renal insufficient or dehydrated. BUN:Cre ratio, if high BUN and Cre is normal, then it's usually dehydration. If the BUN and Cre are high, it's often renal failure.
LABS:
K+, Cr, and Phosphate are often looked at when assessing kidney function. K+, Mg2+, phosphate are often looked at together as well
Refeeding syndrome (hemodilution, hemodynamics) is indicated by labs. Lab error (e.g. blood that has been sitting out too long, things degrade), stress impacts labs, components of the blood (e.g. serum iron) need to be looked at with other portions of bloodwork. Disease states affect labs. High blood glucose can begin to displace sodium, causing sodium to appear low (false low result), like in diabetic ketoacidosis.
• Think about which labs are affected by which organ system
• Lungs: chloride, acetate
• Kidneys: BUN, creatinine, potassium, phosphorus, albumin, calcium
• Heart: Sodium, BUN (volume status)
• Pancreas: Blood glucose, serum lipase
• Liver: Liver function tests
• Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
• Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution efffect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution effect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Serum sodium doesn't really relate to dietary sodium. Serum sodium is a marker of fluid status, because salt is like a sponge and pulls in a lot of fluid. So, if sodium is really low, often times there’s a fluid issue going on. High sodium indicates a fluid deficit.
• Potassium: 3.4– 5.1 mmol/L
• Magnesium: 1.7 – 2.6 mg/dL
• Low magnesium can make it difficult to successfully replete potassium and phosphorus (SO YOU WANT TO MAKE SURE MAGNESIUM IS NORMAL)
• Phosphorus: 2.4 – 4.3 mg/dL
Story: Patient with a phosphorus of 7 starting nutrition at a slow rate, but then his team gave him a bunch of dextrose-containing fluids to correct a sodium issue, and his phosphorus then dipped to a 2! This results from massive refeeding. The trends in your potassium, magnesium, phosphorus are important. What essentially happened was that the glucose (dextrose) activated insulin, and insulin activation caused a massive shift intracellularly of phosphorus, leading to lower levels of phosphorus in the blood. When not eating much, your cells aren’t taking in magnesium and phosphorus, etc. So, again, sugar stimulates intracellular shift because insulin will activate when sugar is reintroduced, leading to even lower blood levels of minerals. Your heart won’t have enough potassium to beat properly, your lungs won’t have enough phosphorus to breathe well. Certain diuretics can lead to potassium deficiency, E.g. thiamin follows potassium (Wernicke's Encephalopathy), certain diuretics that are potassium wasting come with a risk of thiamin deficiency. Can fix this by prophylactically give thiamin in anticipation of potassium drop.
CONSEQUENCES OF REPLETING TOO QUICKLY
• Low potassium: cardiac arrhythmia, cardiac arrest
• Low magnesium: seizure, coma
• Low phosphorus: respiratory distress, difficulty breathing/getting off mechanical ventilation
Patients who are at risk for refeeding syndrome can have a number of different conditions to begin with:
• Anorexia nervosa
• Chronic alcoholism
• Cancer
• Post-surgery (NPO for many days pre- and post-op)
• Elderly (poor dentition, reduced thirst/taste sensation)
• Uncontrolled diabetes mellitus (electrolyte abnormalities, polyuria)
• Critically ill and unfed for >7 days
• Inflammatory bowel disease, chronic pancreatitis, short bowel syndrome
• Cystic fibrosis
• Long-term antacid use (phosphorus levels are often low 2/2 magnesium and aluminum salts in the medications)
• Long term diuretic use (potassium-wasting) such as with CHF
• Patients who are vomiting frequently
Patients with poor blood levels at baseline (K/Mg/P) will be at risk of intracellular shifts and thus lower blood lab values. Patients with SBD have reduced absorptive capacity, for example, and are at risk for refeeding syndrome.
• When a patient is experiencing hyperkalemia (K+ > 5.1 mmol/L), there are a number of treatments a Team may utilize
• 50% Dextrose ampule + Insulin
• Calcium Gluconate
• Kayexalate or Lokelma
• Why would we use these medications? (insulin will stimulate intracellular K+ shift, Lokelma and Kayexalate bind potassium)
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells.
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells. With renal patients who are often in a hyperkalemic state, kayexalate and lokelma will stop potassium absorption in GI tract. When someone’s potassium hits the ceiling, arrhythmia can occur. Calcium is given to offset that. If a pt is hyperkalemic and EKG changes are seen, patient is given 2g of calcium. Calcium gluconate is the preferred IV administration for hypocalcemia (Severe symptomatic hypocalcemia should be corrected promptly with IV administration of calcium gluconate over 10 minutes to control symptoms. Calcium gluconate is the preferred salt for peripheral venous administration to avoid extravasation—leakage of liquid into surrounding tissue.)
Specialized labs: Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
When T. bili is >5 mg/dL, give PO multivitamin without minerals, or remove copper and manganese from your TPN (total parenteral nutrition) solution
If patient is eating, give them a multivitamin without minerals. If patient is on TPN, remove copper and manganese, as toxicity of these can risk brain damage.
Blood and iron studies: Hemoglobin is the last thing to change. Look at ferritin as an earlier sign. Hematocrit can respond to anemia, but also to an overflow of other blood cells. Professor Trussler works with blood in the heme oncology setting. White blood cells in certain type of malignancies (e.g. leukemia) are elevated. Blood smear can count white blood cells and immature white blood cells (blasts). High blasts signals that something is wrong in bone marrow and they’re pumping a lot of immature white blood cells out. Also, immature blasts are a measure of whether someone’s chemotherapy has been effective. Treatment decisions can be made on this.
Absolute number of neutrophils can be used to determine treatment decisions. Low neutrophil count can be used as a guideline for a neutropenic (low bacteria) diet.
A1C: 3-month average blood glucose. When someone is acutely ill, you can see high glucose in the blood, but this is not diabetes, it’s “stress hyperglycemia” (due to injury). But if this is prolonged, an A1C can help you see if they have undiagnosed prediabetes. A1C is useful for newly diagnosed diabetic patients.
Lipase: You shouldn't be seeing a lot of lipase in the bloodstream, as this indicates pancreatic damage (e.g. pancreatitis)
Vitamin and mineral labs get expensive, so you don't want to be checking EVERYTHING for every situation. There are some vitamins and minerals where a serum lab isn't going to be helpful. E.g. pyridoxine (B6), Per the American Society of Parenteral and Enteral Nutrition (A.S.P.E.N.), you need serum B6, 24-urinary B6, erythrocyte AST, and erythrocyte ALT to assess sufficiency of B6.
Common vitamin labs:
· Someone who is having trouble absorbing fat will be at risk for vitamin A deficiency. Vitamin A is key to skin integrity and building (a pressure injury/injuries not healing well may indicate vitamin A deficiency), with substance use disorder deficiency comes up because you’re generating a lot of free radical damage from substance use disorders and the vitamin A is getting used up for that. Vitamin A is protein bound (RBP), so you can look at C-reactive protein in combination with this, because vitamin A may look low when it's not (falsely low result).
· B12 is worth looking at, esp. for vegans, vegetarians, elderly, heavy alcohol or substance users, and patients with IBD.
· Vitamin C builds collagen matrix for skin, thus wounds could cause a vitamin C deficiency in wound patients. Dialysis causes water loss, so you can lose vitamin C. COVID-19 may cause a vitamin C deficiency (the antioxidant vitamin is getting used up).
· Check vitamin D, after it's activated by the kidneys a second time, that active form doesn't last very long, so it may not give you a good result. Vitamin D labs are good to check for elderly patients who don’t synthesize enough vitamin D, and for kidney injury patients because their kidneys aren’t activating as much vitamin D. Checking vitamin D for oncology patients is also great, because they may have some complications in certain cancer treatments. COVID-19 appears to be affecting vitamin D levels.
· Vitamin E is good to check in a patient who is malabsorbing fat. If you think someone is malabsorbing, the team can do more work up.
Less common vitamin labs:
If the vitamin is water soluble, there’s less risk of toxicity, so you can give it prophylactically. For example, folate costs about $1, so it can be given for 3 days prophylactically.
B1 (thiamin) is given prophylactically if you think the patient is deficient. At Brigham and Women’s, if you anticipate that someone might refeed, you give them thiamin for the first few days that they’re getting nutrition support to anticipate that shift with potassium.
Professor T doesn’t usually check vitamin K often, because gut microbiota make vitamin K. Prothrombin (PT-INR, a marker of blood clotting) is a better indicator of vitamin K sufficiency because the clotting factors in your blood need vitamin K to work. If you were truly functionally deficient, you would have trouble clotting.
Common mineral labs
Both copper and ceruloplasmin must be low in order to diagnose a true copper deficiency. Bariatric patients tend to be low, esp. in Roux-en-Y gastric bypass patients, as the surgery is bypassing some of the areas where copper is absorbed. Wouldn't normally suspect a copper deficiency unless there's some sort of malabsorptive process occurring.
Zinc deficiency is caused by (and can also cause) diarrhea. If you have someone with diarrhea that isn’t resolving, it could be due to zinc deficiency, and also zinc could be causing the diarrhea. Zinc is lower in stressed state. If a patient is borderline deficient and their CRP is very high, you may want to hold off on repleting zinc, and then check zinc levels again.
Selenium, like zinc, decreases when someone has diarrhea, but can also cause diarrhea as a side effect of deficiency. Selenium will be low in substance use disorder patients, as it participates in antioxidant functioning (where antioxidants get used up).
Less common mineral labs:
Manganese: No good lab test to measure for this. If worried patient is getting too much, try to just remove it. E.g. taking manganese out of total parenteral nutrition, or giving a supplement that doesn’t have manganese. Manganese toxicity can cause brain damage
Chromium: No real lab measure for chromium, either, but people on long term TPN might develop this deficiency. Sometimes chromium is given prophylactically. People who are diabetic can be low in chromium, but it is difficult to figure out because you can’t check this mineral.
Specialty Lab
• Fecal Calprotectin
• Marker of inflammatory bowel disease
• Protein released by immune cells (neutrophils) at sites of inflammation in the GI tract, which is then excreted in the stool
• Low level (10-50 mcg/mg): likely IBS or viral infection
• Moderate level (>50 mcg/mg): potential IBD flare or worsening inflammatory condition such as parasitic infection
#anion gap#alkalosis#acidosis#lipase#A1C#UUN#labs#specialized labs#clinical#BUN#creatinine#dietetics#Medical Nutrition Therapy
2 notes
·
View notes
Text
November is Diabetes Awareness Month!
Alright, it is coming up on that time of year folk... November! That means more posts about diabetes, more reblogs to raise awareness, maybe a selfie with my pump and CGM. In honor of that, I am going to come up with my own topics for each month (and try to keep them every day, fingers crossed)
Diagnosis story
3 gifs to describe my diabetes
how I tell people about my diabetes
Type 1 vs Type 2
PWD or diabetic
hypoglycemia story
hyperglycemia story
“diabeetus”
Tips for newly diagnosed people
Famous people with diabetes
Insulin pump or shots?
Advocacy
Songs and diabetes
World Diabetes day! (free day)
Holidays and diabetes
Traveling with diabetes
Coping with humor
Activism
Diabetes and pick-up lines
Stereotyping
Media and diabetes
Management in school
Adulting is fun
Perks of diabetes
Burnout
A day in my life
State of my psyche
Support systems
Hope for the future
Invisible disability
Self-review
As always, my ask box is open to talk and answer questions about this.
#actually diabetic#diabetes awareness month#type 1 diabetes#t1d#woohoo#another year#another month about diabetes
4 notes
·
View notes
Text
You expect to see ketonuria in someone who has been vomiting and not eating for days, but not glucosuria. So a urinalysis alone can clue you into DKA.
You have to have a diagnosis of diabetes, high blood sugar, and bicarbonate less than 15 (acidosis) to diagnose DKA.
If bicarbonate is below 15, start insulin gtt. Give lots of IV fluids. You will need insulin for the rest of your life whether it's type 1 or 2 diabetes. DKA is a risk factor for brain edema, electrolyte imbalance (hypokalemia), lactic acidosis.
VBG is as good as ABG if VBG oxygenation is greater than 75%.
Triggers for DKA: infection, menstruation increases risk
Fluids, insulin, electrolytes. Isotonic NS or 0.45 NS with other added electrolytes like K+. Start with LR or NS. Then can decrease to 0.45 NS as you add K+. Give fluids as if pt is 10% dehydrated over 48 hours. Start by giving fluids before insulin. Bolus fluids will help decrease glucose. Insulin gtt: 0.1 units per Kg per hour.
You give insulin until the anion gap closes. Can stop insulin gtt when bicarbonate is above 15. At that point, you need to start subQ insulin. You can give basal insulin at time of presentation. Lantus for example; 0.2 per kilogram. Can give SubQ insulin 1 hour before stopping the gtt.
If glucose drops more than 100 mg/dL/hour, you may need to add dextrose to the fluids. If blood glucose is 250 to 300 mg/dL, you can add glucose to fluids. This is to prevent dropping osmolarity too fast and prevent brain edema. Capillary leak can cause brain edema.
Bicarbonate can be given if you're worried about other organs shutting down due to the acidosis. pH below 6.9, can give Bicarbonate. Check bmp at least q4 hours. Insulin moves K+ into cells. Could check BMP q2 hours if you didn't give K+. Don't give K+ if there is EKG abnormality or no urine output.
Type 2 DM can also have DKA. Their phosphorus can be low, which can cause rhabdomyolysis. Check for evidence of rhabdomyolysis.
SGLT2 inhibitor can cause euglycemic DKA. They lower blood glucose by making you eliminate it. People with DM1 took SGLT2 inhibitor, which lowered their blood glucose. Then since they had lower blood glucose levels, they lowered the amount of insulin they took. So basically, they lowered their blood glucose, but then also were not getting glucose into cells. This then lead to DKA where the blood glucose level was normal, but they had ketone production. So these pts need treatment with insulin gtt and dextrose-containing fluid.
To get CME credit, go to:
This is from the post-test for this episode:
While both DKA itself and treatment of DKA have been associated with the development of cerebral edema, many RCTs have shown no difference in neuro outcomes when comparing 0.9% NaCl, 0.45% NaCl, and LR. Key Point: The sodium chloride content (0.9% vs 0.45% vs LR) of intravenous fluids does not significantly influence the neurologic outcomes in children with diabetic ketoacidosis.
Citation: Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, Sperling MA, Codner E. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018 Oct;19 Suppl 27:155-177. doi: 10.1111/pedi.12701. PMID: 29900641.
Resolution of DKA: pH is greater than 7.3, bicarbonate is greater than 15, blood ketone level less than 0.6 mmol/L.
Blood glucose level does not play a role in determining whether a patient is in DKA or not. A patient is considered no longer in DKA when their pH is >7.3, bicarbonate is >15, and blood ketone level is <0.6 mmol/L.
Key Point: While patients in DKA often present with hyperglycemia, it is not required for a diagnosis of DKA. Additionally, glucose levels play no role in determining the resolution of DKA.
Citation: Evans K. Diabetic ketoacidosis: update on management. Clin Med (Lond). 2019;19(5):396-398. doi:10.7861/clinmed.2019-0284
Insulin has a short half-life (7-10 minutes), so when stopping an insulin drip, subcutaneous basal insulin should be given before the insulin drip is stopped or at the time of stopping the drip. This is due to the high likelihood of ketosis returning promptly without insulin on board. Additionally, there is a movement starting of giving basal insulin at the time of presentation along with the insulin drip. This gives a safety level of insulin, so there is less worry when stopping the insulin drip.
Key Point: Due to the risk of opening the anion gap back up without any insulin on board, basal insulin should either be administered at the time of presentation along with the insulin drip or immediately after stopping the insulin drip.
Citation: Barski L, Brandstaetter E, Sagy I, Jotkowitz A. Basal insulin for the management of diabetic ketoacidosis. Eur J Intern Med. 2018 Jan;47:14-16. doi: 10.1016/j.ejim.2017.08.025. Epub 2017 Aug 31. PMID: 28864157.
1 note
·
View note
Text
Gluco Freeze Review Type Two Diabetes Diet Consider
One of the companies that makes nutrients for women and specializes in supplements for women health is nutraOrigin. According to several studies there appears to be a correlation between magnesium and Type 2 diabetes. How to lower blood sugar without medications is the beginning of a new way of living. No products must be given priority when you go for grocery.

Lose weight: Your blood glucose will be much easier to manage if you get your mass down to standard levels. If you workout regularly on rolling terrain or ascending and descending roads, you'd have a good chance of working on your concentric and eccentric muscle groups. After you eat (what's called 'post-prandial'), it's normal that your blood glucose will go up.
glucofreeze complaints gluco freeze review gluco freeze amazon gluco freeze phone number glucofreeze dr taylor glucofreeze label glucofreeze capsules glucofort vs glucofreeze
It won't help you if you feel a need to eat everything in sight. The simplest way of beating hyperglycemia is the rule of "Take 15 to 20 gms" of fast absorbing carbohydrates either in the form of tablets or through proper diet choice. One of the widely used and most trusted herbal supplements for diabetic patients is Diabkil capsule.
If a person makes the habit of checking the habit of blood sugar level consistently with a blood glucose meter. There are many products and supplements available in the market promising to lower blood glucose level. It's typically either 130 or 140 mg/dl (7.2 or 7.8 mm/l). Many people who have been diagnosed with Type 2 diabetes prefer to go the natural route when trying to manage their condition.
This makes this herb an ideal thing to be included in one's daily diet. Burning more calories will make it possible for your body to require less insulin, and can also increase insulin sensitivity. The reason this kind of cinnamon may help with weight loss is that it slows down the passage of food from your stomach to your colon. One may treat diabetes naturally with the help of natural herbal supplements like diabkil capsules etc making use of herbs like neem, fenugreek, bitter melon, cinnamon, ginger, garlic, ginkgo biloba, Asian ginseng, bilberry etc.
Most of us will never need to have an ultra sound taken of our kidneys and will, therefore, never know how many kidneys we actually have. Avoid foods like sweets, candies, pastries, ice-creams and cakes as they contain very high amount of sugar. The numbers that determine if you are a pre-diabetic will range from 100-125 mg/dL. Instead, taking a 2 tablespoon (30 ml) dose of vinegar before two meals a day for four weeks helped Type 2 diabetics with weight loss and a drop in blood sugar levels.
In a modern state, like USA, there are many common health problems; obesity comes top in the list. One can have a jog around the neighborhood or work blood sugar supplements out on a treadmill and then followed by a few minutes of walking. Walking uses your whole body, especially if you swing your arms when you walk. Stevia: Who would believe the medicinal herb called Stevia lowers your blood sugar levels even though its leaves are 300 times sweeter than sugar?
If you have problems with your lipid or glucose tolerance, you better start walking. After close consultation with your doctor, embark on a concentric-eccentric walking workout regularly. These active ingredients help by reducing and inhibiting the excess glucose production.
https://gethealth24.com/gluco-freeze/ https://www.facebook.com/Gluco-Freeze-New-Zealand-105694645589450 https://www.facebook.com/Gluco-Freeze-Canada-104792035680527 https://www.facebook.com/Gluco-Freeze-Australia-106871442135714 https://www.facebook.com/Gluco-Freeze-Reviews-USA-102724902557928 https://gluco-freeze.blogspot.com/2022/08/glucofreeze-reviews-2022-does-it-work.html https://groups.google.com/g/gethealth24/c/7lRRVPrMcpY https://sites.google.com/view/glucofreeze-complaints https://glucofreezeusa.wordpress.com/2022/08/18/glucofreeze-complaints/ https://gluco-freeze.weebly.com
0 notes
Text
Implementation of a Standardized Admission Hyperglycemia Insulin Order Set in a Veterans Hospital
Abstract
Purpose: The efficacy of an implemented hyperglycemia admission insulin order set containing basal-bolus-correction regimens to facilitate protocol-adherent prescribing in non-critically ill patients was evaluated.
Method: In this retrospective, single-center, observational study, patients age 18 years or older with a history of type 2 diabetes or admission blood glucose >180mg/dL were identified through electronic medical record review of patients admitted to medicine wards. Patients were excluded if admitted to intensive care or surgical units during hospitalization, identified to have a history of type I diabetes, treated for diabetic ketoacidosis, pregnant, or allergic to insulin. Patients were evaluated pre- and post-protocol implementation. The primary endpoint was mean hospitalization glucose levels. Secondary endpoints included: percentage of patients with average hospitalization glucose < 180mg/dL, percentage of basal insulin utilization, and hypoglycemia incidence.
Results: A total of 200 patients were included in this study, with 100 patients in each group. Average hospitalization glucose was not significantly lower in the post-implementation group compared to the pre-implementation group (169 vs. 177mg/dL, p=0.33). More patients in the post-implementation group had mean hospitalization glucose < 180mg/dL, though this was not significant (66 vs. 55%, p=0.15). However, percentage of patients with basal insulin use did not change (43% vs 44%, p=1.00). There was no difference in hypoglycemic episodes (27 vs 24 events, p=0.75).
Conclusion: The new basal-bolus-correction insulin order set at STVHCS is not associated with any difference in inpatient hyperglycemia control. Education at multiple interdisciplinary levels is required for effective hyperglycemia protocol implementation.
Read More about this Article: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555701.php
Read More Juniper Publishers Google Scholar: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=rp_7-igAAAAJ&citation_for_view=rp_7-igAAAAJ:BrmTIyaxlBUC
#Juniper Publishers Google Scholar#juniper publishers publons#Journal of Case Studies#ophthalmology#barotrauma#case reports
0 notes
Text
Omnipod 5 'Artificial Pancreas' Shows Benefit in Type 1 Diabetes
New Post has been published on https://tattlepress.com/health/diabetes/omnipod-5-artificial-pancreas-shows-benefit-in-type-1-diabetes/
Omnipod 5 'Artificial Pancreas' Shows Benefit in Type 1 Diabetes

Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes as young as 2 years of age, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the US Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2 to 5.9 years with type 1 diabetes were presented during the virtual American Diabetes Association (ADA) 81st Scientific Sessions.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7 in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the US Food and Drug Administration, the Omnipod 5 would be the third commercially available automated insulin delivery system — also called hybrid closed-loop or artificial pancreas systems — in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
“No Tubing“ Feature Will Be a Draw for Parents of Young Children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, told Medscape Medical News: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the US.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t…the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal Data Show Benefit in “Difficult to Manage“ Preschool Children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale School of Medicine, New Haven, Connecticut.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, she noted, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing Benefit Seen in Older Children and Adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, Minnesota, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Carlson and colleagues concluded.
Reduced Diabetes Distress, Don‘t Forget Parents‘ Quality of Life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford University, California, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization-5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Hood said.
Jacobsen has reported no relevant financial relationships. Sherr has reported being an advisor for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
ADA 2021. Presented June 26, 2021. Abstracts 70-OR, 71-OR.
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
!function(f,b,e,v,n,t,s)if(f.fbq)return;n=f.fbq=function()n.callMethod? n.callMethod.apply(n,arguments):n.queue.push(arguments);if(!f._fbq)f._fbq=n; n.push=n;n.loaded=!0;n.version='2.0';n.queue=[];t=b.createElement(e);t.async=!0; t.src=v;s=b.getElementsByTagName(e)[0];s.parentNode.insertBefore(t,s)(window, document,'script','//connect.facebook.net/en_US/fbevents.js'); fbq('init', '490389451150319'); fbq('track', "PageView"); Source link
0 notes