#euglycemic DKA
Explore tagged Tumblr posts
Text
Causas comunes de cetoacidosis diabética (CAD)
#can you die from diabetic ketoacidosis#diabetic ketoacidosis#diabetic ketoacidosis (dka)#diabetic ketoacidosis icd 10#diabetic ketoacidosis in dogs#diabetic ketoacidosis medication#diabetic ketoacidosis occurs when#diabetic ketoacidosis specialists#diabetic ketoacidosis supportive therapy#diabetic ketoacidosis symptoms#diabetic ketoacidosis treatment#diabetic ketoacidosis treatments#euglycemic diabetic ketoacidosis#how long does it take to die from diabetic ketoacidosis#how long does it take to recover from diabetic ketoacidosis#signs of diabetic ketoacidosis#symptoms of diabetic ketoacidosis#what are the warning signs of diabetic ketoacidosis#what causes diabetic ketoacidosis#what is diabetic ketoacidosis
0 notes
Text
SGLT2 Inhibitors in 2025: Balancing Cardiorenal Benefits with Safety Profiles
The therapeutic landscape for type 2 diabetes has expanded dramatically, with sodium–glucose cotransporter 2 (SGLT2) inhibitors emerging as a cornerstone of modern management. Originally approved for glucose lowering, SGLT2 inhibitors now deliver robust cardiorenal protection, earning guideline endorsements across diabetes and cardiology societies. As of 2025, specialists—from type 2 diabetes specialists to the Best diabetologist in India and diabetic foot specialists—must balance these benefits against safety profiles to optimize patient outcomes.

Mechanism of Action
SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin, canagliflozin) act by blocking glucose reabsorption in the proximal renal tubules, inducing glucosuria and reducing plasma glucose by approximately 1% HbA₁c. Beyond glycemic control, they modulate intraglomerular pressure, promote natriuresis, and improve hemodynamics—mechanisms central to their cardioprotective and renoprotective effects.
Cardiorenal Benefits
Cardiovascular Protection
Large outcome trials have demonstrated that SGLT2 inhibitors significantly reduce hospitalization for heart failure (HHF) by up to 33% and cardiovascular death by approximately 15% in patients with and without type 2 diabetes. Empagliflozin’s EMPA-REG OUTCOME and canagliflozin’s CANVAS program each reported comparable reductions in major adverse cardiovascular events, cementing their role in heart failure management.
Renal Outcomes
Renal trials such as CREDENCE and DAPA-CKD showed SGLT2 inhibitors slow progression of chronic kidney disease (CKD), lowering the risk of end-stage renal disease by roughly 30% and preserving estimated glomerular filtration rate over time. These agents are now recommended for CKD patients regardless of diabetes status in the 2025 ADA Standards of Care.
Safety Profile
SGLT2 inhibitors are generally well tolerated, but awareness of potential adverse events is essential for safe prescribing.
Genitourinary Infections: Increased risk of genital mycotic and urinary tract infections occurs in 4–6% of patients; yeast infections are typically mild and respond to topical antifungals.
Volume Depletion & Hypotension: Natriuresis can lead to orthostatic hypotension, particularly in elderly or diuretic-treated patients; regular blood pressure monitoring is advised.
Euglycemic Diabetic Ketoacidosis (DKA): Rare but serious—often in the perioperative period or during prolonged fasting; educate patients on “sick-day” rules and temporarily hold therapy during acute illness.
Amputation & Fracture Risk: Initial signals in CANVAS suggested higher amputation rates, but subsequent analyses have been inconclusive; monitor foot health closely, especially in patients seen by a diabetic foot specialist.
Fournier Gangrene: Extremely rare but life-threatening; counsel patients to report perineal pain or swelling immediately.
Integrating SGLT2 Inhibitors into Practice
Patient Selection
Ideal candidates include those with established atherosclerotic cardiovascular disease, heart failure (with reduced or preserved ejection fraction), or CKD stage ≥2, especially when HbA₁c targets are unmet despite metformin and lifestyle measures.
Initiation & Monitoring
Baseline Assessment: Evaluate renal function, volume status, and foot examination—critical for the diabetic foot specialist pathway.
Dosing: Common starting doses are dapagliflozin 10 mg or empagliflozin 10 mg daily; adjust in renal impairment per label recommendations.
Follow-Up: Reassess eGFR at 4–12 weeks post-initiation, monitor blood pressure monthly initially, and review signs of hypovolemia or genitourinary symptoms.
Patient Education
Empower patients with clear instructions on hydration strategies, self-monitoring for infections, and foot care routines in collaboration with a diabetic foot specialist. Provide multilingual brochures and leverage telehealth for remote check-ins, a tactic often used by the Best diabetologist in India to reach diverse populations.
Collaborative Care Models
Multidisciplinary teams—including type 2 diabetes specialists, cardiologists, nephrologists, podiatrists, and diabetes educators—enhance adherence and outcomes. Shared decision-making tools can help patients understand the dual benefits of SGLT2 inhibitors, fostering engagement and trust.
Future Directions
Emerging studies are exploring combination therapies (e.g., SGLT2 inhibitors plus GLP-1 receptor agonists) for synergistic cardiorenal benefits, as well as personalized approaches guided by pharmacogenomics. Ongoing surveillance of real-world data will clarify long-term safety in diverse populations, informing updates to guidelines and practice.
Conclusion
By 2025, SGLT2 inhibitors represent a paradigm shift—delivering meaningful cardiorenal protection while maintaining a favorable safety profile. Type 2 diabetes specialists, the Best diabetologist in India, and diabetic foot specialists can harness these agents to reduce cardiovascular events, slow kidney disease, and enhance patient quality of life. Through careful patient selection, vigilant monitoring, and multidisciplinary collaboration, clinicians can maximize benefits and minimize risks, ensuring that every patient receives the most effective, personalized care.
1 note
·
View note
Text
a peculiar comorbidity, part three
And to close this off, I want healthcare providers to do a few things. There are going to be a lot more cases like me. There are people out there who are fucking struggling. In fact, I'm sure most of the diabetes-related suicides out there were from late-in-life diabetics with an autism comorbidity. this shit isn't easy to deal with, especially when your comforts are now lethal. and it's not like you can just say "well, don't do it." do you have any idea how super-ingrained these comforts, these stims, these safe foods are to an autistic person? they run deep. and they run deep even when you're a kid. it's the main reason why applied behavior analysis is straight-up considered psychological torture in the autistic community - people suggest that just to rip an autistic person away from bad actions, only to realize way too late they're making them miserable. and right now, I'm going through one hell of an ABA session, only that it's my fucking pancreas that's playing pretend-psychiatrist. combine that with the "gotta keep you alive no matter what" mindset of every type 1 resource, endocrinologists, diabetes educators, and PCPs and you have yourself a system that is designed to kill neurodivergent late-in-life diabetics in a short amount of time. in a way, it's genocide. you're getting rid of one group of people in order to not have to deal with them down the line. in another way, it's a form of eugenics since it's designed to weed out the undesirables from the health pool, so they can take their time delaying closed artificial pancreas loops, fool-proof insertion kits that can't be ripped out during sleep or strenuous activity, 10/20-minute-peak insulins with two-hour total lifespan, seven-day patch pumps, stuff that doesn't exactly benefit a neurotypical diabetic at the moment since they're easily adaptable (plus there's this dogged "can't teach an old dog new tricks" mindset you see a lot in diabetic circles) but benefits a neurodivergent diabetic who has way more to worry about than high and low blood sugars. the healthcare industry doesn't give a shit about me. in fact, i'm pretty sure it wants me to die either by my own hand or by theirs.
but here I am, asshole. and here's my final demand: I want Tzield to be approved for honeymooning patients NOW.
I want late-in-life diabetics (priority going to those with neurodivergences) to automatically be added to pancreas and islet cell transplant lists upon diagnosis. you will see significantly less suicides, less deaths, less eugenics, less murder, less mistakes, less meltdowns, less burnout - if you let them on those lists and not just relegated those to life-long diabetics whose organs are starting to crap out on them.
I want all next-gen ultra-rapid-acting insulins to be released now. again, they're just Humalog with more shit.
I want insulin to be totally free. Forever.
I want, upon diagnosis, all diabetics to receive lifelong healthcare from the government, even after remission and surgical intervention. In fact, I want all healthcare to be free.
I want all clinicals for stem-cell effective-cures to widen their criteria to include cases like mine that are way more susceptible to early-onset DKA and euglycemic DKA. those are as lethal as severe hypoglycemic events, but you just wanna blame DKA on not having enough insulin in your system. that way, you can see if stuff like VX-880 and VX-264 have an Awakenings effect (works for a bit before it stops working) or if manages to stick around for longer. I want all clinicals for immunotherapies to have their ages expanded to 35.
And I want Beyond Type 1 to publish all three of my posts - uncensored - on their website if they ever run into it. No edits save for some basic proofreading.
Anything else is genocide.
#autism#type 1 diabetic#type 1 life#type 1 problems#autistic life#comorbidities#insulin#demands#healthcare
1 note
·
View note
Text
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors
Canagliflozin, Dapagliflozin, and Empagliflozin
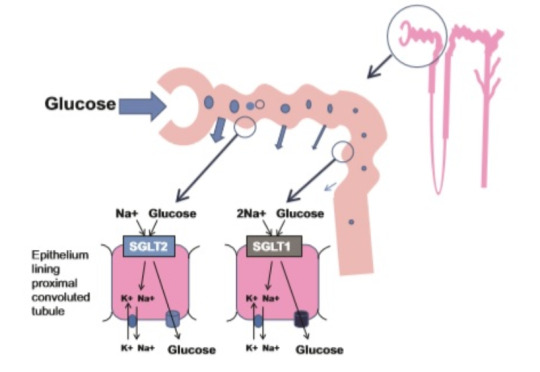
Reduces reabsorption of glucose in the kidney in proximal convoluted tubule
Side effects:
Euglycemic DKA-> Ketones in urine, though BG usually <250 due to increased release of glucose in urine.
Hyperkalemia
Hyperlipidemia
Vulvovaginal candidiasis (due to increased glucose in urine)
Fluid loss -> symptomatic hypotension or AKI
0 notes
Text
UK doctor calls for DKA guidelines revision in bid to improve diagnosis
New Post has been published on http://type2diabetestreatment.net/diabetes-news/uk-doctor-calls-for-dka-guidelines-revision-in-bid-to-improve-diagnosis/
UK doctor calls for DKA guidelines revision in bid to improve diagnosis
Related News
Pioneering stem cell transplant could provide future diabetic retinopathy treatment30 March 2017
Low-level laser therapy could be effective pain relief for diabetic neuropathy29 March 2017
Scientists discover what could increase heart attack risk in people with diabetes24 March 2017
Serious failings of GP service ruled major factor in diabetes teen death17 March 2017
A UK doctor has called for an overhaul of guidance related to the diagnosis and management of diabetic ketoacidosis (DKA) in adults. DKA is a complication of type 1 diabetes and, in some cases, latent autoimmune diabetes of adults (LADA), characterised by a lack of insulin aggravated by high blood sugar levels and the build-up of ketone bodies in the blood. In a new editorial written in The Lancet, Dr Ketan Dhatariya, a diabetes and endocrinology consultant based at the Norfolk and Norwich University Hospitals NHS Trust, argues that our national guidance is laconic. He believes that the international recommendations we resort to are largely outdated, and that a number of modifications should be made, highlighting new evidence that has emerged since the American Diabetes Association's (ADA) last position statement on DKA in 2009. Dhatariya's proposed changes include the use of more criteria to define DKA and different management options for short-term complications of DKA. The problem with the diagnosis of DKA, as seen by Dhatariya, is twofold: the blood sugar cut-off point of 13.9 mmol/L to identify DKA is set too high, and DKA is too often diagnosed based on a single risk factor like the disruption of insulin treatment or elevated ketone levels. Drawing from accumulated professional experience, Dhatariya knows that many patients vulnerable to DKA can present with smaller increases in blood sugar levels than this cut-off point after lowering their insulin dose, reducing their food intake, or when ill. By referring to the standardised cut off score of 13.9 mmol/mol, euglycemic DKA (defined as DKA without marked hyperglycemia) seen in patients with gestational diabetes or those treated with SGLT2 inhibitors, can go amiss too. Euglycemic DKA is thought to occur when blood sugar levels are as low as 11.1 mmol/L. Dhatariya would also like to see introduced an alternate ketone testing method in the guidelines. Urine methods for the early diagnosis of DKA test for the ketone body acetoacetate, but do not usually detect for a separate ketone body known as beta-hydroxybutyrate (BHA). Recent studies have found BHA to be the predominant ketone body at the onset of DKA and suggest that the measurement of blood BHA is a more accurate predictor of ketosis than is the detection of acetoacetate through the urine. In terms of in-hospital care, Dhatariya urged simplified DKA management, similar to the Emergency Valuable Approach and Diabetes Education (EVADE) protocol used in US emergency rooms, to treat patients with mild and moderate DKA. Dhatariya concluded by calling for either new national guidelines or revised DKA international guidance that is evidence-based, practical, and easy to follow to be used by healthcare staff managing DKA in the UK.Type 2 Diabetes Treatment Type 2 Diabetes Diet Diabetes Destroyer Reviews Original Article
0 notes
Text
Common Causes of Diabetic Ketoacidosis Explained
Understanding Diabetic Ketoacidosis: Causes, Symptoms, and Treatment Explained Continue reading Common Causes of Diabetic Ketoacidosis Explained
#can you die from diabetic ketoacidosis#diabetic ketoacidosis#diabetic ketoacidosis (dka)#diabetic ketoacidosis icd 10#diabetic ketoacidosis in dogs#diabetic ketoacidosis medication#diabetic ketoacidosis occurs when#diabetic ketoacidosis specialists#diabetic ketoacidosis supportive therapy#diabetic ketoacidosis symptoms#diabetic ketoacidosis treatment#diabetic ketoacidosis treatments#euglycemic diabetic ketoacidosis#how long does it take to die from diabetic ketoacidosis#how long does it take to recover from diabetic ketoacidosis#signs of diabetic ketoacidosis#symptoms of diabetic ketoacidosis#what are the warning signs of diabetic ketoacidosis#what causes diabetic ketoacidosis#what is diabetic ketoacidosis
0 notes
Text
Diabetes Mellitus Type 2
More common (90%), adult, obese body type, rare DKA, strong polygenetic predisposition, treated with lifestyle oral agents or insulin
Initial treatment:
Lifestyle modification (diet, weight loss, exercise) 25% respond to this alone
DM2 Medical Management:
Metformin best initial medical therapy
Second add Sufonylurea if not controlled with metformin
Metformin: Inhibits gluconeogenesis
No risk of hypoglycemia, does not worsen obesity
Conraindicated in renal disease (lactic acidosis), liver disease
Sulfonylureas: Increase insulin secretion and insulin sensitivity
Glyburide, Glimepiride, Glipizide
Can cause hypoglycemia, weight gain, SIADH
DPP-IV Inhibitors: Block metabolism of incretins, increase post prandial glucose utilization
Sitagliptin, Linagliptin, Saxagliptin, Alogliptin
Thiazolidinediones: Increase peripheral insulin sensitivity
Rosiglitazone, Pioglitazone
Can worsen CHF, cause hepatocellular injury
Alpha-glucosidase inhibitors: Block glucose absorption at intestinal lining
Acarbose, Miglitol
Flatulence, GI disturbance, diarrhea (think lactose intolerance)
SGLT2 Inhibitors: Decrease renal glucose absorption
Canagliflozin, Dapagliflozin, and Empagliflozin
UTI, hypoglycemia, euglycemic DKA
*If agents fail to control glucose, may use insulin. Long acting, plus short acting at mealtime
1 note
·
View note