#How to Prevent Infections During Pregnancy
Explore tagged Tumblr posts
Text
सर्दी-जुकाम और घरेलू उपाय
सर्दी-जुकाम एक सामान्य लेकिन कष्टदायक समस्या है जो किसी भी मौसम में हो सकती है। यह खासकर तब परेशानी का सबब बनता है जब मौसम बदलता है। सर्दी-जुकाम होने पर शरीर में कमजोरी महसूस होती है और सामान्य दिनचर्या में विघ्न डालता है। इसकी शुरुआत अक्सर नाक बहने, गले में खराश और धीरे-धीरे बुखार चढ़ने के साथ होती है।खैर, घबराने की जरूरत नहीं है क्योंकि सर्दी-जुकाम के लिए कई कारगर घरेलू उपाय हैं जो आपको इस…
#Boosting Immune System Naturally#Chronic Cough Solutions#Cold and Cough Prevention Tips#Cold and Cough Remedies#Cold and Flu Relief#Cold and Flu Season Prevention#Cold Remedies During Pregnancy#Cold Symptoms and Care#Cough Relief for Kids#Cough Treatment at Home#DIY Cold Remedies#Dry Cough vs. Wet Cough Treatment#Elderberry Syrup for Cough#Eucalyptus Oil for Congestion#Garlic for Cold Treatment#ginger tea for cold#Herbal Remedies for Cold#Herbal Teas for Cold and Flu#Home Remedies for Cold#Home Remedies for Stuffy Nose#Home Treatments for Sore Throat#Honey and Lemon for Cough#How to Get Rid of a Cold Fast#Natural Cold Remedies#Natural Cough Syrup#Natural Treatments for Cough#Natural Treatments for Nasal Congestion#Saltwater Gargle for Sore Throat#Sinus Infection Relief at Home#sore throat home remedies
0 notes
Text
Learn about UTI during early pregnancy including symptoms, potential risks and safe treatment options. Understand importance of medical care to maintain a healthy pregnancy.
#UTI during early pregnancy#causes of uti in early pregnancy#Symptoms of uti in early pregnancy#how to treat uti in early pregnancy#Uti in early pregnancy treatment#How to prevent uti in early pregnancy#urinary tract infections#UTI in early pregnancy#pregnant#pregnancy tips#pregnancy#pregnancy couselors
0 notes
Text
My dear lgbt+ kids,
Let’s talk about miscarriages.
First of all, a simple definition: A miscarriage is when a pregnancy ends on its own before the baby can grow enough to survive outside the womb.
When we say “miscarriage”, we refer to the pregnancy spontaneously ending in the first 20 weeks (so up until halfway through a typical 40-week pregnancy). If it happens closer to birth (after 20 weeks of pregnancy), it’s referred to as a “stillbirth”. We will focus on miscarriages rather than stillbirth in this letter.
A pregnancy spontaneously ending in an early stage is more common than it happening closer to birth. Most miscarriages happen in the first 13 weeks.
A miscarriage usually involves vaginal bleeding. It can range from light spotting to heavy bleeding. It may also include the passing of tissue or blood clots. Abdominal pain or cramps may also be present. (This is why a miscarriage that occurs before the person is even aware they’re pregnant may be confused with a heavy period).
However, some people may only experience the lessening of pregnancy symptoms (such as a sudden stop of morning sickness) that alerts them to the miscarriage. Some miscarriages also occur without any noticeable symptoms at all and may only be discovered at the next ultrasound.
Let’s look at some myths and facts about miscarriages:
Myth: Miscarriages are rare.
Fact: About 10 to 20% of all known pregnancies end in miscarriage (and the “real” number is probably even higher, since many miscarriages happen before the person even knows they are pregnant).
Myth: Miscarriages happen because you do something wrong or aren’t careful enough.
Fact: Most miscarriages happen because of severe problems with the unborn baby’s DNA. These are usually random genetic glitches in the egg or sperm - meaning there’s nobody to “blame”. The baby wouldn’t have survived, no matter how careful the pregnant person is.
Myth: When we talk about “medical treatment” for a miscarriage, we are talking about people who choose to have a miscarriage.
Fact: Nobody chooses to have a miscarriage. It’s by its very definition the spontaneous ending of a pregnancy. A person may need to undergo medically necessary treatment because of a miscarriage. It may be necessary to remove tissue that remains in the uterus. This isn’t the trigger of the miscarriage, it is done after the pregnancy already naturally ended. It is done to prevent infection or stop heavy bleeding. This procedure is called a D & C (dilation and curettage) and it can be a lifesaver!
Myth: If you had a miscarriage, it’s a sign you deep down resented the baby.
Fact: The most wanted pregnancy ever could end in miscarriage. People who tried for years and finally got pregnant could experience a miscarriage. People who jumped through legal hurdles and spend a lot of money to be able to undergo sperm donation or IVF could experience a miscarriage. This is just a horrible and untrue thing to say about people who experience a potentially traumatic health event that’s entirely out of their control.
Myth: It’s easy to get over a miscarriage.
Fact: It’s a life-changing experience. It’s always emotionally challenging. There’s the aspect of the unexpected (and potentially scary) health event, and of course there’s also the aspect of a loss, of grief. It shouldn’t be surprising that, for most people, it’s not something they can easily shrug off. There are a lot of emotions that can come up - during, right after and also months or years after. There’s no time limit on when someone will be “over it”. In fact, they may never feel “over it”, just learn to live with it as part of their reality.
Myth: If it was an unplanned pregnancy, the person should be relieved to have a miscarriage.
Fact: There’s no “Should” in loss. Even if they didn’t want to be pregnant, they may still grieve. Even if they do feel some relief, it may be tinged with emotional pain, frustration, feelings of helplessness or guilt… And all of that is valid. Nobody but the person who experienced the miscarriage has a right to say how they feel about it.
Myth: If you had a miscarriage, it means you’ll never be able to have biological children.
Fact: Nearly 90% of people who miscarry will go on to have normal pregnancies and healthy babies!
With all my love,
Your Tumblr Dad
168 notes
·
View notes
Text
Sometimes I sit back and think about how the IC holds Nesta's "mean words" against her during their time in poverty. A meanness that Feyre herself stated she gave back.
Sometimes I sit back and think about how the IC hates on Tamlin for "ignoring Feyre's needs" despite the BOTH of them deciding to not express too much. Or when they're mad at him for "locking her up" when it was a way to prevent her following him into a ongoing danger that required him to help his people against a direct threat, but she was too stubborn and even refused to take the other options he was presenting to her. Or when he "abused" her due to a magical outburst; ya’know, the same one Feyre had during the HL meeting. Ya'know, the same one Azriel had to protect humans from because Rhysand was mad at Nesta for giving away HER weapon.
The IC, and particularly Rhysand, holds others' actions they view as a slight against Feyre as the worst sin. It doesn't matter the reason. Because "abuse is abuse" and "failure is failure" as many IC stans would probably wholeheartedly agree with and swear before the Mother with that statement.
And then, sometimes I wonder what the IC would do or think if they found out what Rhysand did the Feyre UTM. Because THEY DON'T KNOW. Not once has anyone been told and I find that to be an interesting choice, because why exactly don't they know. The shadow twins were there and literally painted her and yet they didn't inform Azriel? Weird. What's wrong with physically coercing another into a bargain with violence and getting them drunk until the point of blacking out and body being weak? For Feyre to be sexually exposed in front of Amarantha and everyone trapped night after night for 3 months straight? Well, I guess the sexual exposure wouldn't be a big crime for them; I mean, look at the recreation of the scene when they all went to HC and no one bat an eye lid.
All this to say that bad actions, no matter their intentions from other characters are unnecessarily dragged out. But the very bad action of Rhysand in that single moment (nevermind the rest - he has a lot) is never brought up or made public knowledge to his "Family." I'd want them to react. To be disgusted. But whats sad is that they'd probably just excuse it away anyway. I could already predict it. "He had to." "Rhys had a plan." "There was no other choice that could have been made." Know this for certain because look at how they all defended him when it came to knowing that Feyre would literally DIE during pregnancy and how DANGEROUS a non Illyrian carrying an Illyrian child IS. But I bet if they knew about that death pact earlier they'd be more up in arms - because then HIS life would be at risk, Feyre would want to know and should have a CHOICE when more would seem to be at stake. I think she'd risk shifting, ultimately choosing her mate than just willing to risk herself in a "complicated pregnancy."
The IC irritates me. And if someone comes to talk about grey morality, I'd like to remind them that for that to be true, the narrative would treat horrendous behaviour the same across the board. Not try to retcon or openly minimise it in a pointless monologue while simultaneously not giving the same grace to others. All or nothing, baby. Otherwise, I can't take anything presented to be as "right" seriously. Especially when it comes from a hypocritical camp.
He didn't have to do that to Feyre UTM, he chose to. And Feyre wouldn't have died due to infection, because though Tamlin couldn't physically help, he had Lucien do what he couldn't. LUCIEN would have helped Feyre, but Rhysand just got there first and scared her. She agreed to a bargain under duress. Rhysand wanted something to irritate Tamlin with. Not just to "get him angry" (Rhysand's help was not required for that), but to overwhelming punish him over his mother and sister's deaths even he doesn't have the full story of, nor us as readers. Rhysand is petty and didn't care about Feyre at all - he didn't know her to care. They didnt have lovely sit down conversations during the time of her recovering from a drunken stupor night after night to build a beautiful connection they always knew was there, let alone anything to fall in love with, tf. I don't know why SJM has him lie this badly. I don't know why some fans get angry when you point this out.
Anyway, the IC holds everyone else accountable but each other.
#this was longer than intended#sjm critical#acotar#acotar critical#anti rhysand#anti feysand#anti ic#feyre archeron critical#pro tamlin#tamlin#nesta archeron#anti acomaf#anti acowar#pro lucien vanserra
124 notes
·
View notes
Text
Also preserved in our archive
A new Cleveland Clinic-led study published in The EMBO Journal shows that mild and asymptomatic SARS-CoV-2 infections can trigger immune responses in a pregnant individual that may cause serious inflammatory responses in the developing fetus. The study's findings also suggest that vertical transmission of the virus from a pregnant individual to the fetus is more common than previously estimated; and that even without this transmission, a pregnant individual's immunological response to infection may impact the fetus.
Typically, healthcare providers test for SARS-CoV-2 infection, the virus that causes COVID-19, in a newborn through a nasal swab after birth. For this study, Cleveland Clinic researchers collected samples from the placenta and the fetal compartment (tissues that surround a fetus while still in utero), and then analyzed them for the presence of inflammatory markers and virus. They found higher instances of the virus in those tissues than what could be found in a traditional nasal swab, and even in the absence of a full infection they found small proteins from the virus had passed through the placenta. The researchers hope their study will help ensure pregnant individuals can rapidly and reliably receive evidence-based medical care needed during novel outbreaks and public health crises.
When the COVID-19 pandemic first began, OB/GYN Ruth Farrell, MD, and colleagues at Cleveland Clinic and other major medical centers wanted to determine the best way to prevent and manage the infection in their pregnant patients. Pregnant individuals required different medical considerations during the pandemic compared to their nonpregnant counterparts; Dr. Farrell notes that many of the prevention and treatment approaches used in non-pregnant patients either did not have enough data to use in pregnant patients or were not feasible to perform.
"During the early stages of the pandemic, there were significant delays in determining how best to prevent and treat pregnant patients with SARS-CoV-2 infection," explains Dr. Farrell, who also serves as the Vice Chair of Research for Cleveland Clinic's Obstetrics & Gynecology Institute.
Dr. Farrell worked with clinical colleagues across the Clinical and Translational Science Collaborative (CTSC) of Northern Ohio to develop methods for examining the impact of SARS-CoV-2 infection on pregnant patients, including researchers from University Hospitals of Cleveland and MetroHealth Medical Center.
She then teamed up with Cleveland Clinic maternal-fetal virologists Jolin (Suan Sin) Foo, PhD and Javier (Weiqiang) Chen, PhD from the Infection Biology Program to determine how the virus impacted the immune systems of both mother and child.
When the standard-of-care COVID-19 test is used to detect the virus in newborns (nasal swabs upon birth) they only detect infections in about 2% of children whose mothers tested positive for the virus during pregnancy. However, when Drs. Chen and Foo looked at tissues that surrounded the newborns when they were still in utero-; including the amniotic fluid, chorion and umbilical cord plasma -; they detected high levels of the virus in over a quarter (26%) of study participants.
The team also found elevated immune and inflammatory responses affecting the pregnancies of about 66% of study participants. Dr. Foo had previously shown elevated levels of fetal inflammation in pregnant individuals who experience severe SARS-CoV-2 infections during pregnancy, but few had asked whether asymptomatic or mild infections had the same effect. Now that they have their answer, however, the team were faced with even more questions.
"Even though we only saw vertical transmission of the full virus infection a quarter of the time, we saw strong immune and inflammatory responses in over two thirds of the cases," Dr. Foo says. "It was clear that even when the fetuses were not technically infected, they were still being impacted by their mothers' viral infection. But we weren't quite sure how."
Elevated levels of inflammation during pregnancy, in COVID and other conditions, can have negative impacts on the offspring long after birth. Further research can define how inflammation affects children in the long term.
Dr. Chen noted that the SARS-CoV-2 virus has a protein called ORF8 that physically resembles a human immune protein called immunoglobulin G that passes through the placenta from mother-to-fetus during development. He wondered whether the viral protein could also pass through the placenta's defenses to cause inflammation in the fetal compartment.
Drs. Foo and Chen, alongside co-first authors Tamiris Azamor, PhD and Débora Familiar-Macedo, PhD (a former and current postdoctoral researcher, respectively, in Dr. Foo's lab), were able to prove that the virus-made ORF8 did indeed pass through the placenta into the fetus. ORF8 then bound to immune proteins and "turned on" a process called the complementary immune response.
At normal levels, the complement system is a good thing during pregnancy and helps the fetus develop properly, Dr. Familiar-Macedo explains. At higher levels, the complement system can cause dangerous inflammation in a developing fetus. Lab studies supported that this immune response directly led to the elevated levels of inflammation seen in the fetuses of pregnant patients infected with the SARS CoV-2 virus.
"Our findings challenge the currently accepted definition of vertical transmission, or what it means to transmit an infection from mother-to-fetus," Dr. Chen says. "We have shown that it is indeed possible for only a small part of a virus to slip through and affect a pregnancy."
Dr. Foo adds that she hopes her team's findings will serve as guidance for healthcare practitioners, researchers and policymakers alike on further research into vertical transmission and long-term care.
"We've shown that the misconception that uninfected babies born from infected mothers are fine, is sometimes just that: a misconception," she says. "Pregnancy is such a vulnerable nine-month period where any change from the norm can cause long-term impacts on the baby, so we need to work more closely with these individuals to understand their unique healthcare needs during public health crises. It's the only way to make sure they receive the care they need."
Source: Cleveland Clinic
Journal reference: Azamor, T., et al. (2024). Transplacental SARS-CoV-2 protein ORF8 binds to complement C1q to trigger fetal inflammation. The EMBO Journal. doi.org/10.1038/s44318-024-00260-9. www.embopress.org/doi/full/10.1038/s44318-024-00260-9
#mask up#covid#pandemic#public health#wear a mask#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2#covid in pregancy
75 notes
·
View notes
Note
I have a question about which I have found surprisingly deferring information online. It's about the process of delivering babies in the 1850s to 1890s, particularly the process of the preparation. Would the mother getting into labor be rushed to a hospital and be shown in public or would she remain in the house and then they would telegram a doctor or a nursemaid? I imagine both processes would take hours until the woman got assisted. I'm also wondering if the time's mores prevented anyone but medical staff to be present.
This is a really interesting question! I found the snappily-titled Advice to a Wife on the Management of her own Health, and on the Treatment of some of the Complaints incidental to Pregnancy, Labour, and Suckling, by Pye Henry Chavasse. The earliest edition I can find is 1854, but it was reprinted at least 15 times throughout the 19th century and translated into multiple languages. I also had a read of Hints to Mothers on the Management of Health During the Period of Pregnancy, and in the Lying-in-room by Thomas Bull, from the mid-century, which similarly went through dozens of editions. They're broadly in agreement, although Chavasse opposes all blood-letting for pregnant women, and Bull thinks it might be appropriate sometimes (yikes).
Looking specifically at Chavasse, I was ready to find something truly horrendous, but the bits I've read are sensible. He starts with the observation that women's ignorance of their own bodies is dangerous not only to themselves but to their children, and that they often go to friends for advice who are just as ignorant as them. Hence, he wrote a book so that they could get answers without embarrassment. Good work, Mr Chavasse.
(There's then some advice on going to bed early and going on long walks that's half sensible, half very patronising, but he is a Victorian man so I suppose that's to be expected).
Hospital births were rare until the 20th century, and Chavasse assumes that women will give birth at home. He advises having no more than three attendants: a female friend (who should be a mother herself, and cheerful), a nurse, and a "medical man" (his term). He suggests that the woman's mother should be in the house but not in the room, "as they tend, from their anxiety, rather to depress than to cheer the spirits of the patient".
The nurse and the female friend would be in the house a few days before the due date, but he suggests only calling the medical man once labour is established. This is so that there wouldn't be unnecessary and possibly damaging medical intervention. Despite other concerns about intervention, Chavasse is happy for chloroform to be used as an anaesthetic in labour, which was increasingly common in the mid-1800s. Queen Victoria famously used it in childbirth in 1853.
Chavasse's description of how labour should proceed look broadly in line with modern approaches. In the context of the time, his attitude to medical intervention is also pretty sensible. When his book was first published, it wasn't yet routine for doctors to wash their hands. This blog notes:
Given the importance of both the quality of care at the birth and the underlying health of the mother, it is surprising that most privileged members of British society, the peerage, had higher maternal mortality than the general population until the early 20th century. The explanation lies in the fact that the elite were more likely to have been attended by doctors in childbirth, who were more likely to actively ‘assist’ in the delivery, often unnecessarily and always with the risk of introducing infection.
Where the husband should be during labour isn't mentioned so I think we can safely assume that he wouldn't be anywhere nearby; in face husbands are mentioned only five times in the entire book. He particularly advises that a woman who has had a miscarriage should be away from her husband for several months. There's a lot of waffle about diet and horse-hair mattresses and things, but I suspect that this is mostly a tactful way to ensure that the woman doesn't have to have sex again before she's ready. That's not relevant to what you asked but I thought it was interesting.
Given some of the horrors of Victorian medicine, it was pleasant to find something that broadly followed common sense and - patronising moments aside - seemed to have the woman's best interests at heart.
20 notes
·
View notes
Text
Let's take a quick look at some of the body parts that women need to be acquainted with.
Here's a detailed illustration, lest you think the female reproductive system is some damn easy bake oven. But we're starting with the basics!
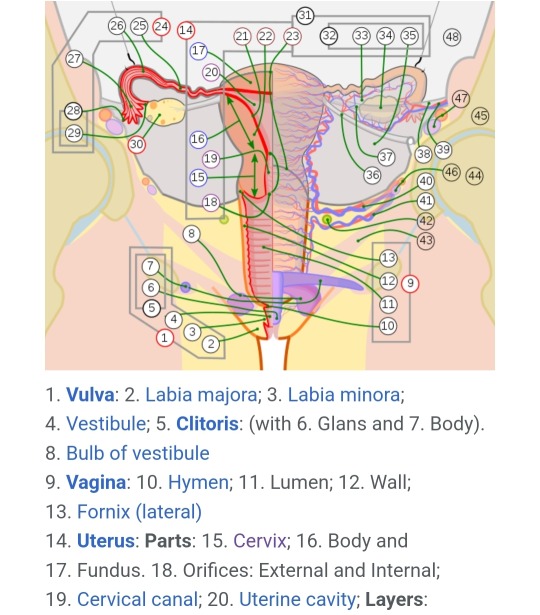
Bartholin's Glands: These are located on either side of the vaginal canal and emit mucus that ranges from almost watery to thick and gooey depending on the need. This mucus combines with the plasma produced by the vaginal walls during arousal. The mucus from the Bartholin's gland is acidic, ranging from 3.8-4.5 on the pH scale (7.0 is neutral).
Cervix: The cervix functions as a gate between the vagina and uterus. It is a deceptively small part of the system when "inactive" but it can dilate significantly to accommodate a fetus. While something inserted into the vagina may touch the outer opening of the cervix, the cervix sits closed most of the time, so you're at no risk of losing a tampon. The cervix opens a little bit during ovulation, menstruation, and childbirth.
Clitoris: Research into the functions of the clitoris has been extremely limited. It has both an internal and external aspect, with the external being located above the urethra, and the internal wrapping around either side of the vagina. The only known function is arousal and sexual stimulation, which also improves fertility.
Fallopian Tubes: The fallopian tubes catch eggs released during ovulation and hold them in the ampulla until the egg is either fertilized - when the then-zygote is sent into the uterus to attach - or not, and released during menstruation.
Labia Majora: The external set of labia is called the labia majora. The labia majora functions to protect the rest of the vulva, the urethra, and the vagina. The labia majora typically swells with blood and slightly parts during arousal.
Labia Minora: The labia minora are the small, inner set of skin folds going from the clitoris to the bottom of the vaginal opening. Like the labia majora, their role is to protect everything encased in them. Unlike with labia majora, it isn't common to grow hair on the labia minora, which may cause discomfort and ingrown hair, leading to infection risks.
Ovaries: Ovaries are small round-ish sacs that contain eggs, the female half of the human gamete. Every month, a new egg drops out of the ovaries and floats (hopefully) to the fallopian tubes. Ovaries aren't attached to the fallopian tubes, so sometimes the eggs just get released into the abdominal cavity. During sex, sperm typically also ends up in the abdominal cavity, and that's how we get extrauterine pregnancies (ectopic pregnancy). Even without a uterus or fallopian tubes, a woman with even just one ovary can still experience pregnancy. Ovaries are also one of the biggest hormone controlling mechanisms in the female body.
Pubic Hair: Beginning at the start of puberty, girls develop pubic hair. By womanhood, this hair typically comes from the pelvis all the way down, covering the labia majora, extending onto the inner thighs, and down and back over the perineum and up around the anus. Pubic hair is there to help us keep clean. Typically the texture is springy, coarse, and curled. This helps prevent detritus from reaching the inner labia and vagina, which can cause irritation and infection. Pubic hair also wicks sweat and moisture away from the vulva. This is a very important function as the vagina and vulva are typically a little wet, due to discharge, and that moisture needs to be removed as it is replaced.
Skene's Glands: Located on either side and slightly under the urethra, these glands can release an "ultrafiltrate" of blood plasma, but typically only during (a really good) orgasm in a phenomenon known as female ejaculation/squirting/gushing. This is not urine. Fun fact: The fluid from Skene's glands is sweet, and has a very high concentration of both glucose and fructose.
Uterus: The uterus is an interesting and multi-purpose structure. Most commonly referenced, the uterus holds a fetus, develops the placenta, and does most of the work in reproduction. However, the uterus also serves as a "weight bearing" organ helping to define and maintain the structure of the abdominal cavity. Newer research is also indicating that the uterus plays an important part in hormone control, and overall health - for example, a hysterectomy increases your chance of developing dementia later in life.
Vagina: The vagina is a tube-like muscle organ that connects up to the cervix. When 'at rest' the vagina is quite short, but when a woman is aroused it lengthens. (Average vagina depth directly correlates to average penis length within a group - if the average penis length is 4-5 inches, the average vaginal depth when aroused is 4-5 inches.) As it's made of muscle, the vagina is highly maneuverable and can be clenched and released whether to increase pleasure during stimulation, or to help push a baby out.
Vulva: The external portion of the female reproductive system, comprising of the labia majora, labia minora, vaginal opening, clitoris, urethra, and associated glands. Everything you can see is the vulva. (|i|) << all vulva.
38 notes
·
View notes
Text
Premature birth rate above global average in Brazil

The commonly cited "nine months" of pregnancy oversimplifies a much more complex process: human gestation lasts about 40 weeks, with a "full-term" pregnancy considered to be between 37 and 42 weeks. However, in 2023, nearly 12 percent of births in Brazil occurred before reaching this milestone, totaling around 300,000 premature babies. These infants face varying health risks, depending on how early they were born. Brazil not only exceeds the global average of around 10 percent but is also one of the top ten countries with the highest number of premature births annually.
According to Denise Suguitani, executive director of the Brazilian Association of Parents, Families, Friends, and Carers of Premature Babies, most of these cases are preventable. She explains, "In Brazil, these rates are closely linked to social factors, including access to healthcare and education. Adolescent pregnancy, for instance, is a risk factor for premature birth because the girl’s body is not yet fully prepared. On the other hand, a planned pregnancy is less likely to result in premature birth, making family planning crucial. And, of course, access to prenatal care is essential. It’s not just the number of appointments that matters, but the quality of care and the information provided."
Obstetrician Joeline Cerqueira, a member of the Prenatal Care Commission of the Brazilian Federation of Gynecology and Obstetrics Associations (Febrasgo), highlights some conditions that can be detected and treated during prenatal care to prevent premature birth and other complications. She explains, "Infections, premature rupture of the amniotic sac, and hypertensive disorders during pregnancy are among the leading causes of premature birth."
Continue reading.
6 notes
·
View notes
Text
Some period pants sold by high street retailers contain high levels of silver that could have health and environmental implications for consumers, an investigation has found.
Silver is used as an antimicrobial agent and is typically added to period pants to combat user concerns about smell and hygiene.
However, scientists have increasingly warned about the potential health effects. The US Food and Drug Administration found that nanosilver can kill lactobacillus, the healthy bacteria in the vagina that help fight off infection. This can put period pant users more at risk of harmful bacteria, potentially leading to an increased risk of bacterial infections and pregnancy complications.
Natalie Hitchins, the head of home products and services at Which?, said: “Consumers should be cautious buying period pants which contain silver as experts have concerns about the health implications.
“Which? believes brands should also clearly state which products contain silver so shoppers can make informed decisions about what they are buying and the possible risks.”
The consumer rights group worked with an Italian consumer organisation, Altroconsumo, to independently test popular brands and check if they contained any chemicals of concern. They were worried to find that some products contained significant levels of silver, and this was not always made clear on the packaging.
Intima by Bodyform and pants by Marks & Spencer in particular contained notably more silver than other brands, at 126.7mg/kg and 57.8mg/kg respectively. Other brands contained 8.3mg/kg, 7.4mg/kg, and 0.9mg/kg.
Essity, the owner of Bodyform and Modibodi, said silver copper zeolite was used to “prevent odour when wearing the pants for up to 12 hours”. It added that all of its “washable underwear is certified according to Oeko-Tex Standard 100, which means that every single component has been tested for harmful substances” and “that the underwear has been designated as harmless for human health”. An M&S Spokesperson said: “We do not use either nano silver or silver zeolite and, like many brands, use a small amount of silver chloride in the middle part of the gusset – away from the skin – which is perfectly safe, approved by the UK and EU, and designed to combat odour.”
Which? said it believed the use of silver was unnecessary and that previous testing by Altroconsumo had shown that textile items treated in this way did not have the promised antimicrobial properties.
The European Chemicals Agency says silver treatments, such as nanosilver and silver zeolite, are toxic to aquatic life with long-lasting effects.
The tests Which? carried out can detect any silver above 0.1mg/kg, and it found none in Primark, Repeat, Wuka, Lovable and Sloggi pants. Sloggi’s website says it does use a silver-based antimicrobial, and Primark says it uses Micro-Fresh, which contains silver chloride.
A Primark spokesperson said: “The nature of period pants means there is a potential for odour to develop during wear (in the same way that bacteria can cause socks and shoes to develop odours during wear) and our antimicrobial finish minimises such odours.”
Sloggi did not reply to Which? at the time of publication.
There are no legal limits in the UK about how much silver can be added to period pants. Manufacturers do not have to declare the presence of silver on their packaging or website.
45 notes
·
View notes
Note
Which member would like to go raw and cum inside everytime?
I want to be very clear on this - personal pleasure is not to be at the expense of lifelong consequences.
Do not allow someone to convince you that your mental and physical health are less important than them getting off.
I know this is meant to be a fun question, however this stuff is important to me. Does it feel better for the dick? Always. I won't lie about that. But there are also very real risks for the receiver that need to be taken into consideration. For those of us concerned about pregnancy, selecting your type of birth control should be dependent on how it affects only you. There's a reason all of them come with many warnings of physical and mental side effects. And even if preventing pregnancy is not a concern, you are trusting the other person with your general physical health. Sexually transmitted infections can be acute (temporary) or chronic (rest of your life).
Sex is also a physical act that some use as a mental weapon. Potential psychological manipulation at play that may be too nuanced for you to pick up on during an emotionally charged situation. Even small comments said without much thought can have lasting effects.
Please think deeply about what you are doing for what could possibly be fleeting pleasure.
Who would like it raw? They all would. And every single one of them should also be responsible and mature enough to have discussions with their partner about whether or not that is appropriate to do with before doing it.
To be honest, I have trouble believing that sex feels that much different for the receiver. More likely it is knowing that it is raw that is more arousing than an actual physical difference. It is not different for me. I feel everything. Sometimes, the lubed condom is preferred if I want the instant plunge in with little prep. The clean up is so much easier too. The latex scent is different than the cum scent that comes out of you. You'll notice. Condoms are also made very well nowdays. There are so many more options compared to when I was first having sex. There's non-latex ones if needed. You can get incredibly thin ones that don't break even with rough sex. There are also many options for additional ridges if that's something you're into. There are also the less effective spermicides and such. It is true that the one with the dick feels less. But also they might want to consider how long they want to last. Sure, it might feel better, but if it feels better? Then they cum faster. If you're a one and done, well, that could be embarrassing.
I am asking you to think about what you're doing before you do it. Stand firm on your boundaries. Don't let someone else ruin your health and happiness. Ruin it yourself! Ahem.
Sorry about the rant. I can't bring myself to take this at face value. There are too many truths of people being coerced into having unprotected sex simply because it "feels better" and I hate that.
12 notes
·
View notes
Text
Canada recently issued a travel advisory following the emergence of the Oropouche virus, also known as the 'sloth virus', transmitted through flying insect bites, causing outbreaks in Cuba and South America. Below is an explanation of what the virus is and how it spreads.
Written by Cameron Webb, University of Sydney and Andrew van den Hurk, The University of Queensland
International authorities are issuing warnings about “sloth fever”. Despite the name, it’s not contracted via contact with sloths. Rather, you should avoid contact with mosquitoes and biting midges.
So how can Canadians protect themselves from sloth fever when travelling to South and Central America? And how does “sloth fever” compare with other mosquito-borne diseases, such as Zika?
What is ‘sloth fever’?
Sloth fever is caused by Oropouche virus and is formally known as Oropouche virus disease or Oropouche fever.
The virus is an orthobunyavirus. So it’s from a different family of viruses to the flaviviruses (which includes dengue, Japanese encephalitis and Murray Valley encephalitis viruses) and alphaviruses (chikungunya, Ross River and Barmah Forest viruses).
Oropouche virus was first identified in 1955. It takes its name from a village in Trinidad and Tobago, where the person who it was first isolated from lived.
Symptoms include fever, severe headache, chills, muscle aches, joint pain, nausea, vomiting and a rash. This makes it difficult to distinguish it from other viral infections. Around 60% of people infected with the virus become ill.
There is no specific treatment and most people recover in less than one month.
However, serious symptoms, including encephalitis and meningitis (inflammation of the brain and membranes surrounding the brain and spinal cord) have occasionally been reported.
What’s happening with this latest outbreak?
In July, the Pan American Health Organization issued a warning after two women from northeastern Brazil died following infection with Oropouche virus, the first fatalities linked to this virus.
There has also been one fetal death, one miscarriage and four cases of newborns with microcephaly, a condition characterized by an abnormally small head, where infection during pregnancy occurred. The situation is reminiscent of the Zika outbreak in 2015–16.
Oropouche had historically been a significant concern in the Americas. However, the illness had slipped in importance following successive outbreaks of chikungunya and Zika from 2013 to 2016, and more recently, dengue.
How is Oropouche virus spread?
Oropouche virus has not been well studied compared to other insect-borne pathogens. We still don’t fully understand how the virus spreads.
The virus is primarily transmitted by blood-feeding insects, particularly biting midges (especially Culicoides paraensis) and mosquitoes (potentially a number of Aedes, Coquillettidia, and Culex species).
We think the virus circulates in forested areas with non-human primates, sloths and birds as the main suspected hosts. During urban outbreaks, humans are carrying the virus and blood-feeding insects then go on to infect other people.
The involvement of biting midges (blood sucking insects mistakenly known as “sandflies”) makes the transmission cycle of Oropouche virus a little different to those only spread by mosquitoes. The types of insects spreading the virus may also differ between forested and urban areas.
Why is Oropouche virus on the rise?
The United States Centres for Disease Control and Prevention (CDC) recently issued a warning about rising cases of Oropouche in the Americas. Cases are rising outside areas where it was previously found, such as the Amazon basin, which has authorities concerned.
More than 8,000 cases of disease have been reported from countries including Brazil, Bolivia, Peru, Colombia and Cuba (as of August 21, 2024).
Cases of travellers acquiring infection in Cuba and Brazil have been reported on return to Europe and North America, respectively. On September 3, the Government of Canada issued a health advisory for international travellers after several travel-related cases of Oropouche were reported internationally, the majority of which were in travellers returning from Cuba.
While a changing climate, deforestation and increased movement of people may partly explain the increase and geographic spread of the virus, something more may be at play.
Oropouche virus appears to have a greater potential for genomic reassortment. This means the evolution of the virus may happen faster than other viruses, potentially leading to more significant disease or increased transmissibility.

Areas in South America with reported cases of Oropouche as of September 4, 2024 (Source: CDC)
What can travellers do to protect themselves?
There are no vaccines or specific treatments available for Oropouche virus.
If you’re travelling to countries in South and Central America, take steps to avoid mosquito and biting midge bites.
Mosquito repellents containing diethytoluamide (DEET), picaridin and oil of lemon eucalyptus have been shown to be effective in reducing mosquito bites, and are expected to work against biting midge bites too.
Wearing long-sleeved shirts, long pants and covered shoes will further reduce the risk.
Sleeping and resting under insecticide-treated mosquito bed nets will help, but much finer mesh nets are required as biting midges are much smaller than mosquitoes.
Although no specific warnings have been issued by Canadian authorities, the CDC and European Centre for Disease Prevention and Control have warned that pregnant travellers should discuss travel plans and potential risks with their health-care professional.
10 notes
·
View notes
Note
you ask raditz to wear a condom and he’s like.. a what? once you explain it to him he thinks you’re fucking with him like i gotta wrap my dick in something? doesn’t say no but is just… confused… lol 💜
"You want me to wear a what?" Raditz is looking at you, confused and a little annoyed, and it's hilarious.
"A condom."
"The hell is that? A costume?"
"No." You laugh, covering your mouth in amusement. "It's, uh... something made of latex to put on your... penis."
"Is it like a kinky thing?" His eyebrow raises high in his forehead, before his grin turns mischievous.
This is not going how you expected.
"No, no! God... It's for protection!"
"Protection?"
"Yes! It prevents pregnancy and infections and-"
"You're fucking with me, aren't you?"
You bury your face in your hands and groan. Luckily he hasn't lost his erection during your definitely not at all explanatory description.
But after Bulma got pregnant in what could only be a case of incredibly bad luck, you just had to be careful. It's a miracle you haven't gotten pregnant yet.
"I'm not, it's literally a rubber 'coat' you put on your dick."
"I know you must be making this up." Raditz points an accusatory finger at you, and you jolt, surprised. "I gotta put something on my cock? And it's not kinky at all?"
"It's not, it's-" You stop in your tracks, an idea popping in your head. A bad idea but might as well. "You know what? It's definitely kinky. Totally like a cock ring."
"The fuck is a cock ring?"
"It's... I'll show you. Some other time."
#truly how do you explain what a condom is to someone who's never seen one.#drabbles#yes. i'm capable of those. sometimes#raditz x reader#replies#anonymous
103 notes
·
View notes
Text
*Dr. Smita Goel Homeopathy Clinic*
www.thehomeopathyclinic.co.in
Infertility case is increasing in all over world. The main causes of this is change our life style, foods, hight stress level etc. Around 10% - 15% is facing to infertility problems.
Causes in Men:
• Low sperm count: The man ejaculates a low number of sperm. A sperm count of under 15 million is considered low. Around one third of couples have difficulty conceiving due to a low sperm count.
• Low sperm mobility (motility): The sperm cannot “swim” as well as they should to reach the egg.
• Abnormal sperm: The sperm may have an unusual shape, making it harder to move and fertilize an egg.
• Genetic factors: A man should have an X and Y chromosome. If he has two X chromosomes and one Y chromosome, as in Klinefelter’s syndrome, the testicles will develop abnormally and there will be low testosterone and a low sperm count or no sperm.
• Mumps: If this occurs after puberty, inflammation of the testicles may affect sperm production.
• Hypospadias: The urethral opening is under the penis, instead of its tip. This abnormality is usually surgically corrected in infancy. If the correction is not done, it may be harder for the sperm to get to the female’s cervix. Hypospadias affects about 1 in every 500 newborn boys.
• Cystic fibrosis: This is a chronic disease that results in the creation of a sticky mucus. This mucus mainly affects the lungs, but males may also have a missing or obstructed vas deferens. The vas deferens carries sperm from the epididymis to the ejaculatory duct and the urethra.
• Radiation therapy: This can impair sperm production. The severity usually depends on how near to the testicles the radiation was aimed.
• Some diseases: Conditions that are sometimes linked to lower fertility in males are anemia, Cushing’s syndrome, diabetes, and thyroid disease.
Causes in Women:
• Age: The ability to conceive starts to fall around the age of 32 years.
• Smoking: Smoking significantly increases the risk of infertility in both men and women, and it may undermine the effects of fertility treatment. Smoking during pregnancy increases the chance of pregnancy loss. Passive smoking has also been linked to lower fertility.
• Alcohol: Any amount of alcohol consumption can affect the chances of conceiving.
• Being obese or overweight: This can increase the risk of infertility in women as well as men.
• Eating disorders: If an eating disorder leads to serious weight loss, fertility problems may arise.
• Diet: A lack of folic acid, iron, zinc, and vitamin B-12 can affect fertility. Women who are at risk, including those on a vegan diet, should ask the doctor about supplements.
• Exercise: Both too much and too little exercise can lead to fertility problems.
• Sexually transmitted infections (STIs): Chlamydia can damage the fallopian tubes in a woman and cause inflammation in a man’s scrotum. Some other STIs may also cause infertility.
• Exposure to some chemicals: Some pesticides, herbicides, metals, such as lead, and solvents have been linked to fertility problems in both men and women. A mouse study has suggested that ingredients in some household detergents may reduce fertility.
• Mental stress: This may affect female ovulation and male sperm production and can lead to reduced sexual activity.
• Surgery: Pelvic surgery can sometimes cause scarring or damage to the fallopian tubes. Cervical surgery can sometimes cause scarring or shortening of the cervix. The cervix is the neck of the uterus.
• Submucosal fibroids: Benign or non-cancerous tumors occur in the muscular wall of the uterus. They can interfere with implantation or block the fallopian tube, preventing sperm from fertilizing the egg. Large submucosal uterine fibroids may make the uterus’ cavity bigger, increasing the distance the sperm has to travel.
• Endometriosis: Cells that normally occur within the lining of the uterus start growing elsewhere in the body.
• Previous sterilization treatment: In women who have chosen to have their fallopian tubes blocked, the process can be reversed, but the chances of becoming fertile again are not high.
Homeopathy has very effective medicines for these problems. And they give good results.

#health & fitness#health and wellness#chronic illness#homeopath#homeopathy#mental illness#ghaziabad#greater noida#indirapuram#new york#doctor odyssey#doctor strange#doctor who#twelfth doctor#tenth doctor#hazaribagh#hazaribag#kanpur#lucknow#fatehpur#jharkhand#jharkhandnews#uttarakhand news#uttar pradesh#uttarakhand#health products#good health#health insurance#health#health tips
3 notes
·
View notes
Text
Today in 'too little, too late'
Also preserved on our archive
It's frustrating how this is being billed as a preemptive measure when covid wastewater levels have been high or very high since at least June. Better than nothing, but we should demand better than "better than nothing."
by PK Hattis
SANTA CRUZ — In anticipation of respiratory virus levels spiking during the coming fall and winter months, Santa Cruz County’s top public health official issued a protective order Wednesday that will take effect in a few weeks.
County Health Officer Lisa Hernandez declared that, starting Nov. 1, masks will be required among all visitors and personnel working in local acute care facilities, nursing facilities, surgical and maternity centers and infusion centers — including dialysis and chemotherapy — to tamp down the spread of respiratory viruses among vulnerable communities and the general population.
The three familiar culprits — influenza, respiratory syncytial virus, or RSV, and COVID-19 — have been known to spread widely during the colder months and this year is not expected to be any different, carrying potential for serious consequences.
“These respiratory viruses can lead to severe illness especially among certain groups such as infants, older adults, pregnant women, and those with a weakened immune system,” Hernandez said in the release. “This Order is issued to curb the spread of these viruses to vulnerable populations and minimize the risk of severe illness and death.”
The order applies to all health care personnel and visitors regardless of vaccination status and masks must be worn at all times while indoors and conducting direct patient care or while visiting patient care areas.
Still, that doesn’t mean vaccines should be ignored. In fact, quite the opposite, the release noted. Vaccination remains the best way to protect individuals from infection, hospitalization or death from COVID-19 and influenza while also reducing the risk of spreading the viruses to others, according to the release. The updated recipe for the COVID vaccine was given final approval for release last month by national health authorities and doses have since become available at local health care providers and pharmacies across the county. Community members can reach out to their primary care provider or a pharmacy at a local Safeway, Walgreens or CVS, among others, for scheduling and availability.
The Centers for Disease Control and Prevention has also recommended that adults 75 years and older receive the RSV vaccine as well as individuals 60 years and older who are at increased risk for severe RSV illness. The RSV vaccine is also recommended for pregnant people between 32-36 weeks of pregnancy.
When it comes to COVID specifically, public health preparations for the long winter ahead come on the heels of a busy summer season of infections. According to the county’s COVID tracker, the virus was actively spreading in the community from about mid-April to early August. Wastewater and other data models indicate virus levels have continued to drop ever since.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
32 notes
·
View notes
Text
The Lifecycle of Cat Worms and How Deworming Medicine Helps
Worm infestations are a common issue for cats, and understanding the lifecycle of these parasites is essential for ensuring their health. Regular deworming is key to keeping your feline friend safe and comfortable. In this article, we’ll explore the lifecycle of common cat worms and how effective deworming medicine, like Puainta, helps combat these pests.

The Lifecycle of Common Cat Worms
Common worms that infest cats include roundworms, tapeworms, hookworms, and whipworms. Each type of worm has its own lifecycle, but most follow a similar pattern of transmission. For example, tapeworms often enter a cat's system through fleas, which they ingest while grooming. Roundworms are typically passed through infected feces or through the placenta during pregnancy. These worms lay eggs that hatch into larvae, which then mature and continue the cycle inside the host cat.
In the wild or in environments where hygiene is poor, cats are more likely to encounter these worms through contact with contaminated areas or prey. Since worms can be difficult to spot in their early stages, regular monitoring and deworming are crucial.
Symptoms of Worm Infestation in Cats
When cats are infected with worms, they may exhibit several telltale signs. Symptoms can include vomiting, diarrhea, weight loss, lethargy, and even visible worms in their feces or around the anus. Left untreated, a worm infestation can lead to more severe health problems, such as malnutrition or damage to internal organs. Therefore, recognizing these signs early is critical for a quick recovery.
How Puainta Deworming Medicine Helps
Puainta deworming medicine for cats is an effective solution for tackling worm infestations. This chewable tablet works by targeting and eliminating common intestinal parasites, including roundworms, tapeworms, hookworms, and whipworms. Puainta is safe for both puppies and adult cats, providing fast and reliable relief from the discomfort caused by worms.
The medicine works by disrupting the worms’ lifecycle, preventing them from reproducing and eliminating existing infestations. Puainta's formula is designed to act swiftly, with many cats showing noticeable improvements within a few days. Its ease of use—simply giving your cat a chewable tablet—makes it a stress-free option for both pet owners and their cats.
Fenbendazole is a broad-spectrum deworming agent commonly used to treat various parasitic infections in both cats and dogs. Fenbendazole works by interfering with the metabolism of parasitic worms. It inhibits the worms' ability to absorb nutrients, leading to their eventual death. This action is effective against many common intestinal parasites, including tapeworms (Dipylidium caninum), roundworms, hookworms, whipworms, and nematodes, as well as other parasites like Paragonimus kellicotti (lung fluke). Fenbendazole does not pose a risk to pets when used correctly and is widely regarded as a safe and effective treatment.
Conclusion
Regular deworming is an essential part of your cat’s overall health care routine. Puainta deworming medicine for cats offers an effective, easy-to-administer solution for eliminating common worms and ensuring your feline friend remains healthy and happy. Always consult your vet to determine the best deworming schedule for your cat, and consider Puainta for safe, reliable protection.
3 notes
·
View notes
Note
How bad are strikers injuries??
Bunny: Striker’s injuries are serious but not quite life-threatening
1. Stab Wound (Shoulder): This is one of the worst injuries. It’s deep, still bleeding, and will need stitches to prevent infection. It’s also left him with reduced mobility and pain in his left arm, which could take weeks to fully heal.
2. Burns: Striker has fresh burns on parts of his chest and arms, sustained from his recent job. The burns are severe enough that they’ll scar even after they heal, adding to the permanent marks on his body. These will require frequent dressing changes and, ideally, some kind of ointment to prevent infection and help with pain. Not to mention the cattle prod burns around his neck.
3. Internal Injuries: From the beating he took, Striker likely has bruised ribs and may even have a minor fracture. This would explain his labored breathing and general stiffness. He’ll need to take it easy with any heavy lifting or strenuous activity.
4. Broken/Loose Teeth: A couple of his fangs were knocked out or loosened during the fight. He’s experiencing pain and sensitivity in his mouth, which makes eating difficult and increases his risk of infection.
With these injuries on top of his pregnancy, Striker’s body is under serious strain. Without proper rest and care, he could face complications in his recovery or even his pregnancy.
#striker’s injuries#he’ll need to rest completely#striker#striker helluva boss#striker mpreg#helluva boss#helluva boss au
4 notes
·
View notes