#Hashimoto's thyroiditis treatment
Explore tagged Tumblr posts
Text
Low Thyroid Treatment In Homeopathy

Homeopathy is emerging as a safe treatment forow thyroid problems. A high TSH (thyroid stimulating hormone) is the main sign that you have hypothyroidism. Your major thyroid hormones, T3 and T4, maybe low or normal. But if your TSH is high you have hypothyroid or a low thyroid problem.
Start homeopathic treatment for thyroid if you want to treat hypothyroidism in a natural and holistic way.
Homeopathic medicines have no side effects. Hence patients want to consult a good homeopathy doctor for low thyroid treatment. The trend is rising in Mumbai, Bangalore, Pune, Indore and several cities in India. People are experiencing the benefits of homeopathy treatment in thyroid hormone problems.
To book your appointment with Dr. Chintan Mehta call or Whats app +91 9869021226.
Start treatment for thyroid and other hormonal problems at Dr. Mehta’s Standard Homeopathy Clinic in Mumbai, India.
#homeopathy doctor#thyroid treatment#homeopathy doctor for thyroid#low thyroid treatment in Mumbai#homeopathic clinic for thyroid problems#Hashimoto's thyroiditis treatment#thyroid#hypothyroidism#hormones#endocrinologist
0 notes
Text
i can project anything onto any character no matter how specific. xavier gonzales has hashimotos disease
#BECAUSE !! 2 me he’s already type 1 diabetic coded cause of his strong feelings abt the heist (not saying that u have to be afflicted by-#an illness to be empassioned abt those who have it being exploited but . yknow …)#and you’re more likely to develop hashimotos w/type 1 and vice versa.. and i can give any character i want my hypoglycemic tendencies too ❤#plus the treatment for a good amt of hashimotos cases are thyroid replacement hormones … so i think it’d be very funny for him to-#be technically on hrt but Not In That Way. yknow…
16 notes
·
View notes
Text
well i didn’t get my paycheck in the mail but i did get a referral notice from my doctor saying that i can expect to see an endocrinologist... in SIX. FUCKING. MONTHS.
#no. fucking. no#i can barely get out of bed on a good day. i've been feeling this way for months.#bloodwork says i HAVE hashimoto's disease. i have a family history of thyroid issues on both sides#i am NOT in acceptable health to be waiting six months. i wanna cry. maybe i will#tales from diana#another fucking phone call i have to make on monday. i still haven't called the other specialist i need to see to make an appointment#the secretary told me they'd take care of this one and schedule it for me#they said it might take until the fall#i can't wait until the fucking winter solstice#i have so much anxiety on top of all of this health shit i have barely been able to think straight this week#everything in my life is falling apart#reducing/managing stress is all they told me i can do for now (until i potentially start a treatment course)#to prevent myself from developing full-blown hypothyroidism#AND LET ME TELL YOU... CIRCUMSTANCES IN THE LAST WEEK HAVE NOT BEEN GREAT FOR THAT#i'm gonna have to drop out of society and be a recluse again at this rate. this is so discouraging#i'm not gonna be able to continue my education or pick up a steady job#luckily being a substitute teacher is super flexible but i wanna fuckin be able to pick up hours at that job#i haven't been able to work more than two fucking days a week since april#i don't leave the house to see ppl anymore bc if i so much as walk in a parking lot im unable to get up for the rest of the day#im PISSED#i do wanna cry#ok bye i can't be ranting like this anymore i wanna cry
2 notes
·
View notes
Text
🌿 21 Ways to Naturally Start Reducing Your Hypothyroidism & TSH Levels
Living with hypothyroidism can feel like a daily battle—constant fatigue, stubborn weight gain, brain fog, and feeling like your body is working against you. I know this struggle all too well because I’ve lived it. But here’s the good news: you don’t have to stay stuck. There are natural, proven ways to support your thyroid and start feeling like yourself again. That’s why I wrote books like: 📖…
#Best foods for hypothyroidism#Foods to avoid with hypothyroidism#Hashimoto’s natural treatment#Healing recipes for hypothyroidism#How to balance thyroid hormones#Hypothyroidism meal plan#Hypothyroidism success stories#Natural remedies for hypothyroidism#Reduce TSH levels naturally#Thyroid healing diet
0 notes
Text
This Explains a Lot
Hey folks, I don’t want to drama queen all over you. I know you all have big problems. But there’s been a recall of medication I take to manage Hashimoto’s Disease.

Hasimoto’s Disease affects something like 1% of the population (depending on who you ask). It’s an autoimmune disorder that causes the immune system to attack your thyroid gland.
The thyroid is sort of like your body’s throttle. If it doesn’t work properly, a lot of other things won’t work properly.
Symptoms include (from the Mayo Clinic Website):
Fatigue and sluggishness
Increased sensitivity to cold
Increased sleepiness
Dry skin
Constipation
Muscle weakness
Muscle aches, tenderness and stiffness
Joint pain and stiffness
Irregular or excessive menstrual bleeding
Depression
Problems with memory or concentration
Swelling of the thyroid (goiter)
A puffy face
Brittle nails
Hair loss
Enlargement of the tongue
For my part, the big issues are the fatigue, aches and pains (my hands are sometimes so stiff I cannot move my fingers, and right now my back is killing me,) depression, and memory problems. As in, I will be sitting there working on a drawing and between the time I look at my reference and the time I look at my drawing I can’t remember what I just saw in my reference.
That’s not good.
Also not on the above list: edema, anxiety, high cholesterol, poor heart function, an enlarged heart and irregular heartbeats. I had to have a CAT scan in December, and my anxiety has been swinging back and forth into the red zone for months.
When well managed, I don’t notice it much, but when not well-managed, my life grinds to a halt.
Since cancer treatment, I’ve felt the usual fallout from all that cancer entails. But I honestly thought I should have been feeling much better by now.
But I’m not. I’ve been up and down, but mostly down.
Finding out I’ve been improperly medicated for 7 months certainly explains a lot. A friend of mine who got the defective medication notice from her doctor thought she felt poorly due to long Covid. Another was sinking for months, unable to understand why.
Well, at least we know why.
This doesn’t affect everyone on the medication, just those with certain lot numbers from certain manufacturers. And if you are highly sensitive to hormone fluctuations, even a small variation will knock you right on your keister.
Several people I know heard from their health care providers. Others heard nothing until they asked.
It’s not like I don’t have a lot of stress right now, and figured my anxiety, poor mood, and weight gain originated from dealing with what I’m dealing with.
Well, at least some of it is because my medication hasn’t been hitting the sweet spot.
Bad luck, but it is what it is.
It’s going to take about 6 weeks before I start to feel better, but at least I am working it.
Best Wishes.
151 notes
·
View notes
Text
EMERGENCY; Longterm assault has led to the deterioration of my health + avoiding homelessness
I’ve been life-haltingly sick going on 7 years now, with several outside factors either exacerbating things or keeping me from getting treatment. The short version is, I did not ask for the things that happened to me that led to my health issues, I have fought like hell to stay afloat anyway. In my childhood I lost my trust, power, community, sense of self and my autonomy. In my adulthood I lost my time, health, stability, my home and any feeling of safety and its only getting worse because I can not afford to be this sick and pay my bills. **Now I’ve lost the ability to even eat.**
**I can not stress enough these are ACCUMULATIVE AMOUNTS. this is not money that I HAVE, this is money that has gone into rent, bills, doctors, moving to a cheaper place, medications, mobility aides, etc. it has gone to things that are necessary.**
I have not had a life of my own since 2017. I have worked tirelessly with measly breaks when I can’t take it anymore. My mental health is collapsing and it makes me ashamed when it shows. If I am not medicated, I am not even a person anymore- it feels like I am just the fear.
Any time I’ve started to see savings come together It all ends up going to the extraordinary taxes required as a freelance artist. An ultrasound recently showed there is barely anything left of my thyroid and my new endocrinologist tested for hashimoto’s again, and it came back negative- meaning a great majority of issues I’ve had doctors blaming my thyroid for are completely unrelated and caused by something else. Currently looking into internal brain injury, but the need for financial support in order to pay bills and afford medical help is incredibly dire. Please help and reblog this GFM anything quite literally helps.
#mutual aid#health crisis#gofundme#gfm#fundraiser#donation#donations#fundraising#emergency#crowdfund#trans crowdfund#please boost#trans mutual aid#donate#urgent
60 notes
·
View notes
Text
So, I’m not proud of it, but I’m back to ask for help again. Above is the link to my Ko-Fi account; I can accept donations via Stripe and Paypal; I don’t have a preference of which method you use. Below is a more detailed explanation of the events that have led to my current predicament; it’s not entirely necessary to understand, but it should make sense of why this happened to me.
I’m dealing with some health problems and a recent car accident and I need help paying my bills for the next few months while I use that time to finish incomplete coursework for classes I took last year. In case it’s not clear, an “Incomplete” is a grade that can be given by instructors at some schools in situations where a student wasn’t able to complete a major assignment for a class due to circumstances outside their control, and allows students a pre-determined amount of time to finish that work beyond the end of the course. I had a plan for covering my expenses with a summer job at the Oregon State University Arthropod Collection (OSAC) while I finished the incomplete work, but the nature of my health issues, an outbreak of fleas, and a car accident have all prevented me from making it work. Now I’m kind of trapped; the cost of living in Corvallis is too high for food stamps to last an entire month, I don’t have a car anymore, and I’ll probably end up homeless if I can’t pay October rent and also pay November rent on time. I’ve managed to find some work doing landscaping and yardwork in my neighborhood, but I’ve realized that it’s impossible to make enough money and also handle the incomplete coursework; focusing on the former will impact the completion of my degree in June, while focusing on the latter will likely result in homelessness. The loss of my car is exacerbating all of this, in part because I live further away from all of the stores/banks/etc. in Corvallis, and public transit here is not very good.
Since late 2022, I’ve been experiencing sleep apnea-like health problems arising from swollen turbinate glands. I have some known allergies, but they’ve never caused swollen turbinate glands. The impact on my sleep quality became so severe that I had to resort to nasal strips every night. I saw doctors about this problem as early as spring of 2022, but none of them were helpful; most of them didn’t listen to me, and none of them considered trying any kind of testing. This ineptitude continued even after directly asking my primary doctor about autoimmune conditions and how we could test for them. Despite how obviously informative blood samples can be, nobody suggested a blood test. I finally lost my patience and demanded they give me a blood test for hypothyroidism at the end of August. Lo and behold, my thyroid hormone levels were an order of magnitude out of the normal range. Autoimmune problems run in my mother’s family, and it’s likely that I have Hashimoto’s thyroiditis; this disease is rarer in men, and the symptoms appear very gradually. While I can understand how this would delay detection of the disease, there were FIVE different doctors who saw me in relation to the sleep/allergy problems and none of them considered a blood test. I started taking levothyroxine the same day as the test results, but before being treated, my symptoms became so severe that my ADHD medication stopped working, my OCD symptoms went out of control, and I was experiencing severe brain fog. This is what forced me to request incomplete grades for my courses; I was trying to complete coursework despite all of this, and I was barely able to keep up. Once treatment begins, it takes at least a month to take effect, so my symptoms didn’t start improving until early October. Most recently, I found out that I needed to increase my dosage, but thyroid problems often have complex consequences, and any changes to the dose of the medication will result in unwanted side effects.
My original plan for this summer was to work at OSAC to cover my expenses while I tackled the incomplete coursework. I calculated the gross income I’d need to meet my expenses, and working 30 hours a week at this position well exceeded that amount. My duties as a curatorial assistant change slightly depending on the tasks at hand, but because I am paid from grant money, I must work efficiently, accurately, and in an organized manner. Because I have ADHD, extra measures are necessary in order to meet these requirements. I’ve worked this job intermittently since 2018, so I know how prevent my ADHD symptoms from interfering with my work. Because of the failures by my doctors to address my health problems, I was already struggling to arrive at work on time by June. By July, my symptoms had worsened to the point that I was no longer able to focus on work consistently, voluntarily cutting some days short because I wasn’t accomplishing much, and continuing to work in that state was inherently a waste of grant money. By August I could only make it to work sporadically. As a result, I missed most of the income I could have earned for August and September of this year. I was able to make up for some of this impact by selling old trading cards and video games from childhood, but that money didn’t last very long.
I was also confronted with a flea infestation that suddenly appeared in August. I rent a bedroom in a house with housemates; we tried to eradicate them ourselves, but the landlord suddenly informed us in early September that he hired an exterminator, who was arriving in less than 24 hours. I have some pet reptiles and pet invertebrates I needed to protect from pesticide exposure, so I suddenly had to move my pets to a friend’s house. I also had to re-arrange my bedroom to accommodate the exterminators. Based on the chemicals that were used, the only way I could make room safe again for my pets was by mopping the floor in my bedroom and the adjacent hallway three times. This ultimately cost me four days, and then the exterminators came back in early October, which forced me to repeat the process.
As if this wasn’t enough, I had a serious car accident in late September that annihilated my car and left me with severe lacerations to my left arm and a fracture in my thumb. The car spun out and flipped in the process, landing in the opposite lane. If another car had been about to pass me, it would have caused a direct collision at around 55 mph, and I probably wouldn’t have survived that. I realized the danger immediately and crawled out of the car, but most of the other possible outcomes would have involved my demise. I’m very lucky, but it took almost a month for the lacerations to heal, and one of them was deep enough to cause nerve damage, which hasn’t completely healed yet. My left hand has healed enough for me to use it, but I’m still having some issues with my thumb.
I wish I could say that I had help from my family, but my parents were impacted by both of the recent hurricanes that made landfall in western Florida. Even before the hurricanes, my parents weren’t really willing to understand what I was dealing with. I grew up in an abusive household; my sister and I were neglected by our parents, and we experienced emotional abuse from them as young adults. This is particularly true of my father, who himself is the product of a highly abusive upbringing. Unfortunately, research on the dynamics of child abuse has shown that children from abusive households often suffer a lack of economic mobility relative to children from more supportive family backgrounds as a result of mental health impacts. This has absolutely been the case with my sister and I; both of us are well into our 30s, and neither of us is anywhere close to long-term financial stability. That’s why it was deeply hurtful to hear my father blame me for being unable to fly to Florida on a whim to help him clean up the house, blame me for paying $950 a month for rent, and shame me for being 35 years old without a “stable job”. Both of my parents visited me in Corvallis in late July; they could tell that I was struggling, they apologized for neglecting me, and they told me they’d be more supportive, but apparently everything they said to me then must have been an act.
Hopefully, this explanation sufficiently articulates the situation I’ve ended up in. I almost have enough money to pay my October rent, and I need to have my November rent paid by 11/5. I would have tried using Ko-Fi sooner, but in the interest of upholding my own responsibility, I wanted to exhaust my other options before resorting to donations again
63 notes
·
View notes
Text
Small health update 2:
My other doc calmed me down quite a bit in terms of my MRI - he said that the gadolinium contrast makes the scanning go so sensitive that it finds even the most minute changes in brain. Therefore, the results might seem worrying but are, in fact, not that terrible. The small change they found is/was most likely a tiny mini-stroke that left a small scar, probably due to prolonged stress (no kidding xD). Doc said it is to be observed, but that is likely nothing more than a scar, and that my neurologist will mostly confirm and/or suggest more tests.

Booked an appointment at the endocrinologist as well, will see if he will biopsy my thyroid gland's tiny tumour or just let it be and watch it. *sigh* The truth of Hashimoto's treatment is that I only have to swallow a pill daily and watch my diet... and that's pretty much it. It is not all that great but then again, I got away with this way lighter than others in my family (my mom had her thyroid gland entirely removed in her late '30 and still deals with tumours growing on its stumps).
Thank you all for your warm words and for keeping fingers crossed, it definitely helped a ton! 💪💕🫡
...this is my life from now on, if I start speaking Suomi then you know 🤣 🇫🇮

24 notes
·
View notes
Text
Story at-a-glance
Vitamin D is crucial for immune system regulation and helps manage autoimmune conditions like Hashimoto’s thyroiditis by inhibiting proinflammatory cytokines and reducing thyroid peroxidase antibodies
Having optimal vitamin D levels help improve thyroid function by decreasing TSH levels and increasing FT3 and FT4 levels, with active vitamin D (calcitriol) being more effective than other vitamin D supplements
Low vitamin D levels are correlated with an increased risk of autoimmune thyroid diseases, acting as an immunomodulator to balance proinflammatory and anti-inflammatory cells
Vitamin D has shown promise in reducing disease activity and improving treatment outcomes in autoimmune thyroid disorders by enhancing the innate immune response
Despite some conflicting results, vitamin D’s potential in managing autoimmune diseases is promising, offering a noninvasive strategy to mitigate the impacts of conditions like Hashimoto’s disease
8 notes
·
View notes
Text
What really pisses me off is that if they just prescribed me methimazole or propylthiouracil when they first determined I was getting *very* hyperthyroid periodically and that it wasn't dying as expected, I would not have been having daily heart attacks as a post covid symptom. That attack of symptoms I had to manage wouldn't have lasted a year and 3 months of me having to take obscene levels of magnesium to counteract the cardiac spasms, these two recent flares would never have happened, and all the damage to my liver, kidneys and heart and unknown other tissues or the neurological damage NEVER WOULD HAVE HAPPENED.
And these meds are standard treatment for hyperthyroidism...
But they don't want to prescribe them to someone who's hyper thyroid but *technically* has hashimoto's instead of graves.
Better to just leave me unable to tolerate iodine or b vitamins so if I die they can just blame me.
And if they had of even just TOLD me it might be my thyroid when that first attack started, I could have halted that attack in half the time or less, and avoided this one completely, but instead I have been horridly ill and barely able to move on most days since last june or july.
This is why the disabled end up hating doctors.
This is why we end up not even bothering to go in for severe seeming issues.
Because even once they have proven on paper what the problem is, they just keep pretending you are just anxious, and start avoiding any test they know will be diagnostic.
Even without treatment if I had just KNOWN I could have been avoiding iodine this entire time and have still managed the attacks.
They have known I am hyperthyroid since before the first time Trump was elected and are still just banking on my thyroid gland dying on its own so they don't have to do anything.
3 notes
·
View notes
Text

Two weeks after this photo was taken, I received a phone call that nobody ever wants to receive.
I was dealing with a slew of health issues: an inability to lose weight, hair loss, swollen lymph nodes, fatigue so intense that getting out of bed felt like a miracle, and severe brain fog. My joints were in so much pain that I found myself using a heating pad for most of the day.
I consulted my aunt, who is a pediatrician, and she reviewed my recent blood work. She observed that my TSH levels were consistently borderline high, often surpassing the normal threshold. Encouraged by her insight, I visited my OBGYN and shared my symptoms. She ordered hormone testing and referred me to a rheumatologist, given that lupus runs in my family. The results indicated elevated TSH, DHEA, and C-reactive protein levels.
I then saw a remarkable rheumatologist who conducted over 120 tests. All came back normal except for my thyroid antibodies, and I was diagnosed with arthritis in my hands. Around this time, my neck began to swell, feeling as though something was stuck in my throat. My primary care physician scheduled an ultrasound, which revealed swelling in my neck and a lymph node, and identified a nodule or "ectopic" tissue.
Returning to my primary care doctor, I was told my lab results were normal and advised to follow up in a year, despite continuing to experience swollen lymph nodes and being told that the neck nodule was unrelated to the swelling. At this point had been to urgent care 3 times, completed 3 rounds of steroids, a z-pack, and tested negative for mono, Covid, and strep.
Despite my tendency to avoid conflict, something felt off, and I knew I wasn't okay.
I requested a referral to an endocrinologist, which I received, but they couldn't see me until after Christmas. Not wanting to wait, I found another endocrinologist who could see me on Halloween. At my first appointment, I was diagnosed with Hashimoto’s thyroiditis and hypothyroidism. She ordered a biopsy "to be safe," emphasizing that a finding warrants investigation. Even at the hospital for my biopsy, the PA questioned its necessity given my primary care's advice to wait a year.
On 12/22, my endocrinologist informed me that the biopsy results were suspicious for thyroid carcinoma. I returned on 1/5 to discuss the findings.
They had sent my sample for Afirma testing, a genetic test for medullary thyroid cancer, due to the unusual results and the aggressive nature of the potential cancer.
I was then referred to an ENT, who suspected the nodule might actually be a lymph node. A CT scan confirmed this suspicion, revealing a lymph node suspicious for thyroid cancer, yet with no nodules on my thyroid itself.
The decision was made to remove the lymph node, with intraoperative pathology consultation to decide whether to also remove the thyroid.
On 2/24, the lymph node was removed, but pathology was indeterminate, leading to the decision not to remove the thyroid.
The following week, I was informed that my results had been sent to a larger university hospital for further analysis and a second opinion, an ominous sign according to my ENT.
Ultimately, it was confirmed as papillary thyroid cancer that had begun to metastasize to the lymph nodes, indicating occult thyroid cancer, typically undetected until it spreads to the lymph nodes. Likely, there are microcarcinomas on my thyroid undetectable by imaging. Thus, another surgery is required.
My complete thyroidectomy is scheduled for 4/24.
Honestly, none of this truly sank in until I received a call from the hospital's oncology department to schedule a radiation consultation for post-surgery RAI treatment.
It’s been an incredibly tough start to the year, to say the least.
8 notes
·
View notes
Text
Thyroid: A Comprehensive Guide
The thyroid gland, a small butterfly-shaped organ located at the base of the neck, is a powerhouse for regulating essential bodily functions like metabolism, energy levels, and hormone balance. Unlike temporary health concerns such as diarrhea, thyroid conditions often require long-term care and attention to maintain overall health.
This blog explores the thyroid's role, common disorders, symptoms, causes, treatments, and tips for keeping it healthy.
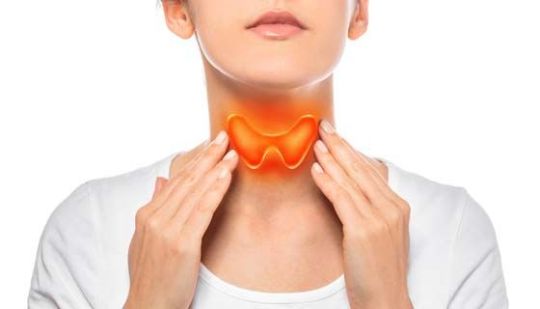
What is the Thyroid Gland?
The thyroid gland produces two primary hormones:
Triiodothyronine (T3)
Thyroxine (T4)
These hormones regulate metabolism, which influences energy use, body temperature, and weight. The gland's activity is managed by the pituitary gland through thyroid-stimulating hormone (TSH), ensuring proper hormone levels are maintained.
Common Thyroid Disorders
Hypothyroidism (Underactive Thyroid)
What Happens? Insufficient hormone production slows the body’s metabolism.
Symptoms:
Fatigue
Weight gain
Hair thinning
Dry skin
Sensitivity to cold
Depression
Causes:
Hashimoto's thyroiditis (an autoimmune condition)
Iodine deficiency
Thyroid surgery or radiation therapy
Treatment:
Synthetic hormone replacement (e.g., Levothyroxine)
Hyperthyroidism (Overactive Thyroid)
What Happens? Excessive hormone production speeds up metabolism.
Symptoms:
Weight loss
Anxiety
Palpitations
Excessive sweating
Tremors
Insomnia
Causes:
Graves' disease (an autoimmune disorder)
Thyroid nodules
Overconsumption of iodine
Treatment:
Antithyroid medications
Radioactive iodine therapy
Surgery in severe cases
Thyroid Nodules and Cancer
Nodules: Lumps in the thyroid that may cause imbalances or indicate cancer.
Cancer: Rare but treatable with early detection. Symptoms include a persistent lump in the neck or difficulty swallowing.

Tips for Maintaining Thyroid Health
Balanced Nutrition:
Eat iodine-rich foods like fish, dairy, and iodized salt.
Include selenium (e.g., Brazil nuts) and zinc (e.g., nuts, seeds) in your diet.
Regular Checkups:
Monitor hormone levels if you have a family history or symptoms.
Stay Active:
Exercise reduces stress and helps regulate metabolism.
Stress Management:
Techniques like yoga or meditation can improve hormonal balance.
Avoid Self-Medication:
Excess iodine or unprescribed supplements can worsen thyroid issues.
When to Seek Medical Attention
If you experience symptoms like persistent fatigue, weight changes, or swelling in the neck, consult a doctor immediately. Early diagnosis and treatment are key to preventing complications such as heart disease, infertility, or severe metabolic imbalances. Your thyroid’s health is essential for your overall well-being. Addressing thyroid concerns early can significantly improve your quality of life.
For more expert advice on thyroid health and personalized consultations, visit CongoRx. Learn more about thyroid care and related conditions, or explore our blogs like diarrhea causes and symptoms.
4 notes
·
View notes
Text
I was diagnosed with Hashimoto's when I was six. I had a fairly large thyroid nodule removed the same year. My thyroid function was monitored until I was about... 10? 11? And then stopped. I strongly suspect this was because my mom's private insurance wouldn't pay for the testing. I didn't get ANY treatment for hypothyroid until I was twenty. Complete thyroidectomy at 22.
Seeing people who are diagnosed with Hashimoto's in their 30s, their 40s, and they talk about how debilitating it is is just like.... I've had what you have all my life. This thing that destroyed your hobbies and job and life.
Have I EVER known what normal feels like?
3 notes
·
View notes
Text
I got sent an article on Liam Gallagher talking about hashimoto's thyroiditis and the effect it has on his life. I think it's great he's talking about it, since people don't know much about the symptoms and I've read it is more common in women, so men might not be as aware and be less likely to seek treatment because it's less likely. But less likely does not mean impossible.
Hashimoto's is when your autoimmune system produces thyroid antibodies which disrupt thyroid function and make it underactive. The symptoms are broad and varied. Cold extremities is common, fatigue, brittle hair, goiter, dry scaly skin, it also causes swelling of the joints resulting in pain, abdominal swelling, facial swelling, slow heartrate.... and more. It can be hard to even suspect one illness might behind them and seek treatment.
The Mirror article in question
7 notes
·
View notes
Text
i can’t wait to get treatment not cause i’m sick of being in pain and tired and cold all the time but because the way to treat hashimotos is usually thyroid hormone replacements. i can literally say i’m on hrt
6 notes
·
View notes
Text
Hey guys, it’s me. I just wanted to give an update on things since I’ve very inactive over the last several months.
I recently got diagnosed with Hashimotos, and for those of you who don’t know what it is, it’s an auto immune disorder that has to do with the inflammation of your thyroid, a tiny little butterfly like organ in your neck. Because the thyroid is directly tied to one’s immune system, this means I’ve been getting sick a lot over the past few months. It’s taken a lot out of me, and I haven’t had the energy to do as much as I used to. I feel bad that I don’t interact a lot on posts anymore, I think that’s maybe why I’m making this post in the first place. I’m sick now, but I’m getting better, it’s just I’ve been in limbo trying to get treatment for this disorder, and because of that wait I keep getting sick, and it doesn’t help that my entire job is to be around people who need help with sickness of their own. I just wanted to let you guys know. Thank you for your understanding. I’m going to try and interact and post more, but if I go quiet for a little (or maybe a long while) that’s why. I know it’s silly to say but I miss you guys.
I’ll probably delete this post later. I don’t usually talk about personal stuff like this, so maybe this is just sickness brain getting the better of me. I hope all of you are doing well, I may not show it but I get so happy when I see your art and headcanons. Thank you for your understanding guys. I have an appt with my doctor on the third, so hopefully that will get this cleared up and back to my normal self. Until then, I wish all of you a happy new year, and some very very wholesome thoughts with your favorite characters. Thank you.
13 notes
·
View notes