#Epilepsy Diagnosis & Treatment
Explore tagged Tumblr posts
Text
my head is covered in blue gunk that they used for all the wires & electrodes to do the sleep deprived EEG this morning and i both look and feel like i walked straight outta professor hidgens lab
#i have had only one hour of sleep in the last almost 48 hours :D#im feelin gREAT#but she said they’ll post the results in a few days or so to see if i have epilepsy#i am collecting diagnosis’ like pokemon cards at this point#but in a WILD twist of events#i was chatting with the woman who was doing my eeg#and she has ALL THE SAME DIAGNOSIS I DO#so the appointment lasted like an extra hour cause we were just relating to each other#and she told me about practices and treatments that have helped her#and wrote them all down for me with her email which has me so 🥺#feeling hopeful about my health for the first time in a long time!!!#she’s only the second ever person (that im aware of at least) that i’ve met who has the same diagnosis!!#so anyways#gonna take a shower and prob pass out soon#if i start being able to sing the first 16 bars of moana in tune i expect y’all to ole yeller me 🫡#health mention tw#epilepsy mention tw#🪓 𝐭𝐡𝐞𝐲 𝐰𝐢𝐥𝐥 𝐧𝐨𝐭 🎶 𝒔𝒉𝒖𝒕 𝒕𝒉𝒆 𝒇𝒖𝒄𝒌𝒌 𝒖𝒑𝒑𝒑 🎶・❥✐ ᵒᵒᶜ.
3 notes
·
View notes
Text
The Role of Brain Imaging in Epilepsy Diagnosis
Brain imaging is essential for diagnosing and planning treatment for epilepsy, as it helps doctors identify areas of abnormal brain activity that may lead to seizures. Techniques such as MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans enable specialists to examine the brain's structure in detail, allowing them to spot lesions, scarring, or other structural issues. More advanced imaging methods, like functional MRI (fMRI) and PET scans, can illustrate brain activity, revealing which regions are more active or impacted during seizures. This information is crucial for customizing treatment, whether through medication adjustments or exploring surgical options for better seizure management.
For patients with drug-resistant epilepsy, brain imaging is vital in assessing their eligibility for surgery, as it accurately pinpoints the origins of seizures. If you or someone you care about is dealing with ongoing seizures and requires specialized care, our epilepsy clinic and surgical hospital offers cutting-edge diagnostic tools and tailored treatment plans aimed at improving seizure control and enhancing quality of life.
1 note
·
View note
Text
https://neurologistinjaipur.com/blog/7-main-causes-of-epilepsy-in-childhood/
Epilepsy in Childhood, diagnosis, and Treatment of Epilepsy:-
There are many causes of Epilepsy in Childhood. What effects epilepsy in childhood, information about diagnosis and treatment of epilepsy.
0 notes
Text

All about epilepsy patients
0 notes
Note
Obligatory 'in good faith' but when you talk about mental diagnoses not being legitimate - do you mean universally? Like, brains are organs and things can go wrong in ways that can be identified and dealt with, and families can have longstanding histories of these things. Is your point that these just aren't identifiable in distinct groups/'diagnosis'? am I using a different idea of what a diagnosis is? Is it just 'yeah brain conditions exist but the field is so fucked 50% of them are bullshit'?
it is more the latter than anything else. obviously some neurological conditions are 'real', in that they are terms that identify discrete and consistently diagnosable conditions -- e.g. epilepsy and TBIs. when i made that post i was talking about psychiatric diagnoses specifically, which despite using a similar language to that of medical diagnostics are basically just made up as hell. like, the DSM is just made up as all hell. the diagnoses in it (and, indeed, the processes provided for making those diagnoses) are not rigorous or consistent.
sure, some of those diagnoses can be useful for treatment and understanding of the conditions in question under some circumstances. but the idea that psychiatry is, like, 'a biological medicine of the brain', while flattering to psychiatrists, is basically totally disconnected from the realities of psychiatric research and practice. for the most part, psychiatry is not concerned with 'brain conditions' but instead with the categorization and pathologization of behaviour.
256 notes
·
View notes
Text
Wouldn't Want To Be Anywhere Else ❀Megumi Masterlist HFBU


You’re lying in bed, staring at the ceiling. The room is dim, the only light coming from the digital clock on the nightstand. Megumi lies next to you, his steady breathing the only sound breaking the silence. His presence is comforting, a warm anchor in the cool, quiet night. You turn your head slightly, looking at his relaxed face, his dark hair tousled against the pillow. You feel a surge of affection and a hint of anxiety, the latter always lurking in the background since your diagnosis.
Living with epilepsy is a constant balance of caution and normalcy, and having Megumi by your side has made it easier. He’s calm, reliable, and incredibly understanding. He never makes you feel like a burden, which is something you’ve feared with previous partners. Instead, he treats your condition with a practical matter-of-factness that helps you feel safe.
You remember the first time you told him about your epilepsy. It was early in your relationship, a time when revealing such personal details felt like peeling back layers of vulnerability. You’d been at a small café, the buzz of conversation and the clinking of cups creating a cozy backdrop. Megumi had listened intently, his eyes never leaving yours, and when you were done, he’d simply nodded.
“I understand,” he’d said. “We’ll handle it together.”
And you have. From keeping track of your medication schedule to learning the best ways to support you during and after a seizure, Megumi has become an expert on the intricacies of your condition. He’s attended appointments with you, asked the right questions, and even researched new treatments and support groups. His dedication is unwavering, and it fills you with gratitude and love.
Tonight, though, you’re restless. You shift slightly, trying not to disturb him, but Megumi is a light sleeper. His eyes flutter open, and he turns his head to look at you.
“Hey,” he murmurs, his voice husky with sleep. “You okay?”
“Yeah, just can’t sleep,” you whisper back, trying to keep your voice steady.
He reaches out and gently squeezes your hand. “Want to talk about it?”
You hesitate, then nod. “I’m just… worried, I guess. About the future. About having another seizure.”
Megumi shifts closer, his presence a solid, reassuring weight beside you. “I know it’s hard,” he says softly. “But we’re in this together. You’re not alone.”
You smile, feeling a little better. His words, simple as they are, hold a lot of weight. You turn on your side to face him, taking comfort in his familiar features. His eyes, usually sharp and focused, are soft in the dim light, full of concern and love.
“Thank you,” you whisper, your voice trembling slightly.
He cups your cheek, his thumb brushing gently against your skin. “You don’t have to thank me. I love you, and that means being here for you, no matter what.”
You feel tears prick at the corners of your eyes, but they’re the good kind—tears of relief, of gratitude. You lean in, and he meets you halfway, your lips brushing in a tender kiss. It’s a reminder that you’re not facing this alone, that Megumi is right there with you, every step of the way.

The next day, you’re at the park, enjoying the warmth of the sun on your face. Megumi is next to you, his hand entwined with yours as you stroll along the path. It’s a beautiful day, the kind that makes you forget about your worries, even if just for a little while. You’re both quiet, content to just be in each other’s company.
As you walk, you see a group of children playing nearby, their laughter ringing out across the park. You watch them for a moment, feeling a pang of longing. You’d love to have a family someday, but the thought of raising children with your condition is daunting.
Megumi seems to sense your shift in mood. He gives your hand a gentle squeeze. “What’s on your mind?”
You glance at him, considering how to put your feelings into words. “I was just thinking about the future,” you say slowly. “About having a family. It feels… complicated.”
Megumi nods, his expression thoughtful. “It’s something we’d have to plan for, sure. But I don’t think it’s impossible. We’d just need to be careful and make sure we have the right support in place.”
His words are reassuring, and you find yourself relaxing a little. “You’re right. I guess I just worry about the ‘what ifs’ sometimes.”
“We all do,” Megumi says quietly. “But we can’t let them stop us from living our lives. We’ll figure it out, together.”
You smile, feeling a weight lift off your shoulders. You know that with Megumi by your side, you can face whatever challenges come your way.

Later that evening, you’re at home, preparing dinner together. Megumi is chopping vegetables while you stir a pot on the stove. It’s a simple, domestic scene, but it’s moments like these that you cherish the most. The comfortable routine, the easy conversation, the way you move around each other in perfect sync.
As you set the table, you feel a familiar aura begin to settle over you. It’s a sensation you’ve come to recognize all too well—the onset of a seizure. Your heart starts to race, and you clutch the edge of the table, trying to steady yourself.
“Megumi,” you manage to say, your voice strained.
He’s at your side in an instant, his eyes sharp with concern. “It’s happening?”
You nod, and he gently guides you to the couch, helping you to lie down on your side. He moves quickly and efficiently, making sure the area around you is safe. He’s done this so many times, and his calmness helps to ground you.
“I’m here,” he says softly, holding your hand. “I’m right here.”
The seizure takes hold, and everything becomes a blur. But through it all, you’re aware of Megumi’s presence, his steady voice, and the comforting feel of his hand in yours. It’s over relatively quickly, but it leaves you exhausted and disoriented.
When it’s over, Megumi helps you sit up, his eyes full of concern. “Are you okay?”
You nod weakly, leaning against him for support. “Yeah, I think so. Just tired.”
He wraps his arms around you, holding you close. “Rest for a bit. I’ll finish up dinner.”
You’re too tired to argue, so you let him take care of everything. As you rest on the couch, you watch him move around the kitchen, marveling at how effortlessly he seems to handle everything. His quiet competence and unwavering support make you feel incredibly lucky.
After a while, he brings over a plate of food and sits down next to you. You eat together in companionable silence, the simple act of sharing a meal grounding you after the seizure. Megumi’s presence is a constant reminder that you’re not alone, that you have someone who loves you and will always be there for you.
As you lie in bed that night, you think about the future again. This time, though, it doesn’t seem quite so daunting. With Megumi by your side, you know you can face whatever comes your way. You reach out and take his hand, feeling a sense of peace settle over you.
“Thank you,” you whisper, your voice full of emotion.
He turns to you, his eyes soft and full of love. “For what?”
“For being here. For everything.”
He smiles, squeezing your hand gently. “I wouldn’t want to be anywhere else.”
You drift off to sleep, feeling safe and loved. And as you do, you know that no matter what challenges lie ahead, you’ll face them together.

#jjk angst#jjk fluff#jjk x y/n#jjk x you#jjk x reader#fushiguro megumi x reader#megumi x reader#megumi fushiguro#jjk megumi#epilepsy awareness#epilepsy#megumi x you#megumi x y/n#fushiguromegumi
127 notes
·
View notes
Text
The largest study of its kind has identified individual genes, gene sets, and gene variants that increase risk of developing epilepsy – vital discoveries to improve diagnosis and treatment for one of the most common neurological conditions . A collaboration between 40 research groups around the world has released its collected data in an interactive web portal for further analysis. Understanding more about the genes linked to the condition can now allow more targeted investigation of the different mechanisms at play.
Continue Reading.
80 notes
·
View notes
Text
Just headcanons with Leon and his daughter who has a chronic illness
Leon x daughter!sick (diabetes, epilepsy or any other severe chronic disease)

√ Hey, Leon carefully guards his child! however, there are not always things from which he can protect his daughter.
√ I see Leon as a very caring father. He will worry if his daughter's knee is torn from a fall from a bicycle and carefully treat her wound and bind it up if necessary. He will also monitor how her childhood injuries are healing.
√ Having seen so many horrors in the world, Leon takes even a simple cold seriously. If the temperature does not decrease even after taking an antipyretic, Leon will prefer to take his daughter to the hospital.
√ Leon hardly knows the symptoms of the diseases, but he noticed an unusual dryness of the skin and the smell of acetone in combination with other symptoms. If his daughter loses consciousness in front of him, it will drive him crazy. All the way to the hospital, Leon will hold her in his arms and kiss her on the forehead or the top of her head.
√ Nevertheless, he will not allow himself to show fear of his daughter. No matter at what age she is diagnosed with it, Leon will be her strongest support. He will learn everything about this disease and his concern will only increase.
√ He is paid very well for risks at work, so the question of money is never acute. Leon will make sure that his baby receives good treatment, which will be corrected by doctors in time and he will repeatedly take her to an endocrinologist and other necessary examinations.
√ Measure your blood sugar level every day and make sure that the insulin injection is done on time? Papa Leon is watching this very carefully. He even keeps a blood sugar control log.
√ Does she need a home education? Leon will study this issue, and if necessary, then no problem.
√ It is important to understand that under no circumstances will he leave his child alone with these diseases. He will never tell his wife/girlfriend to deal with this shit alone.
√ Will take her to all medical procedures.
√ He's such a loving dad. He always convinces his little girl that her illness does not make her inferior. Spends time with her looking for classes available to her.
√ He will definitely not allow his child to be offended.
√ He will turn on her cartoons and lie next to her in the nursery until she falls asleep. Actually, Leon, because of his daughter's illness, can check her well-being even at night.
√ He definitely knows how to provide first aid, but for the sake of his daughter, learn to put injections more carefully so as not to leave bruises and not cause her great pain.
√ Always consults with specialists on any medical issues.
√ Leon will always take care of his child's well-being. This is what he highlights, if nerves or stress affect her health, then he will comfort her and say that no excitement is worth her well-being. For Leon, the daughter is a little diamond, no matter what she is ill with.
√ If a chronic illness is caused by a severe injury (for example, a traumatic brain injury), Leon will literally hate himself for not looking after his child well.
√Again, medications are very expensive, as well as treatment, but Leon is ready to do everything possible so that his child does not need anything. If she gets epilepsy later, Leon will try to always be there to help his baby.
√ Leon will always try to be there. When she is in the hospital, he will provide her with the full care that is possible.
√ It does not matter what kind of disease she has, he will still study the Internet and books studying this diagnosis in order to know better how to help his child.
√ Perhaps his daughter will be banned from playing sports or attending summer camps, depending on how serious everything is, then Leon will try to find a good alternative with her.
√ All medicines will always be at hand.
#leon kennedy#leon scott kennedy#leon s kennedy#resident evil#leon scott kennedy x daughter#dad leon s kennedy#dad leon kennedy#older leon kennedy#leon kennedy resident evil#papa leon#leon#leon kennedy headcanons#resident evil headcanons#headcanon#leon Kennedy dad#papa leon s kennedy#resident evil leon
194 notes
·
View notes
Note
How is your health going with your seizures? Did you get a diagnosis? Is treatment helping you? We all hope you get better at dealing with it 💜💜💜💜💜
i’m doing a lot better!! it’s epilepsy, it took me a while to find a medication that works but i’m around 3 months seizure free now!!
21 notes
·
View notes
Text
okay okay hear me out HEAR ME OUT
F09!Kim
(or postconcussion!Kim there his concussion was non treated well and did things to his health. F09 is ICD code of most close diagnosis to described and by that i mean i have it)
detailed scenario (prompt?) under cut
after concussion he start to get strange weird "something wrong" feeling for hours which he can't describe and find any info anywhere.
other symptoms came too, vision affected, migraines, hallucinations, stress, all feelings and thoughts turned to gray mash. He mostly just lay in bed trying to rest but 24/7 in bed is not rest it's depression. harry came to him more and more often for "giving a thing back" [kim care for harry after tribunal] but from some moment he just stays because Kim feels * really * bad. Lay, staring into the wall, sleep, getting out of bed to just eat, sleep on table, not getting out of bed, getting fried eggs with ketchup smile to the bed, sleep sleep sleep, starting to make just "mmmm" "nnnnnnggghhhh" sounds instead of words. not going to doctors at first because "i am fine" then "i. don't. care" and at this stage just "...". just gray nothing in his thoughts
untill first epilepsy seizure with passing out.
harry tries to make "self kim care day" (which is "hey let's watch some old ass cop film with popcorn". [i mean. it's harry]).
some intense action scene with flashes, boom, eyes rolled foam in mouth kim waking up in hospital, harry running all around. but there is some good doctor, and after month of Kim being in clinic, shivering from IV, not being able to focus visually at anything, walking only with hand on walls, some most intense hallucinations - which all was part of the process of figuring " what the hell is happening with this guy " and trying which meds work, Kim finally gets treatment. which start helps
Healing finally happening
He finally getting explanation of that "something wrong" feeling thing - turned to be epilepsy aura type [epilepsy aura is a real med term. yep]). it stop happening after some time on meds. Less migraines, less hallucinations, mostly at time then he is at bed late and stresed again, which is now happens rare. vision don't really go better, accept being able to focus came back, but he learns how to live with almost complete blindness, going to places with a lot of not visual senses interests, like nature or music concerts, which harry know all about, all bands in town, all clubs, and takes kim to places where he knows will not be flickering lights or sudden loud music
Gray mash of feelings and thoughts turns into fine life and Kim can finally Taste what flavor is the syrup on pancakes harry making him on breakfast.
mm absolutely not based on my life of course it's based on my life
#disco elysium#epilepcy headcanon#kim kitsuragi#disco elysium headcanon#postconcussion!kim#disco elysium spoilers#kind of?#also#i am inviting you to slap all your mentall illness on kim#like#do it#he is jpeg you can do whateva#can print you permission diploma in my office which i of course have#i mean like you even have canon reason#you don't need it but you have#why is your kim is so mentally siick - he got hit to the head did you play the game#if it was a drawing or comics i would draw him also fat#it's my style now i dont care#do whateva you want people really#really want to see your versions#you can @ me if you will want to add smth to this#you go go
28 notes
·
View notes
Text
🗝️
i have plenty to say about the syscourse on this site, but it would inevitably invite bad actors and harassment so i'll start simple.
to those who quote the DSM-5 and the medical industry to proclaim that endogenic systems aren't genuine plurals, please keep in mind that the DSM-5 also encourages doctors to dismiss and refuse diagnosis if it can be 'explained away' by other conditions such as schizophrenia or epilepsy, despite it being known that DID has a large overlap with those conditions.
also, this stance of refusing to acknowledge a possible diagnosis or treatment if they can pin the symptoms on a comorbid or 'easier to treat' diagnosis is why there's a widespread problem within the american medical industry of misdiagnosing and refusing to treat ADHD, BPD, PTSD, eating disorders, and practically anything that can be dismissed as obesity or gendered issues.
even without including endogenic systems, DID itself is severely under-diagnosed and poorly researched specifically because of this counterproductive practice of trying to oversimplify the patients' issues to fit under preexisting bias or to save effort and money.
i understand the concern about bad actors, but you really shouldn't be making your point using hypocritical ableism. :p
74 notes
·
View notes
Text
I've posted before about my mamaw and how in the last few years of her life she finally got diagnoses and treatment for issues that had been plaguing her for her entire life.
The neurologist responsible for that has opened a new clinic in town. I had tried to get a referral previously, only to be told my diagnosis wasn't under their umbrella of care.
We assumed this was because one definition of it implies it's psychological, which my therapist, who specializes in trauma seizures, disagrees with. So my internist's referral coordinator put in a second referral specifying this.
The lady I talked to today told me it wasn't the "possibly psychological" that they had a problem with, it's that their practice is so new that they only have people to treat this neurologists specialties, which is concussions and cognitive impairments. They don't yet have capability for testing/treatment of seizures at all.
But she also said that they were looking to expand, and they could have that capability in the future, so they would keep my referral on record and I should check back with them in a few months.
Which is better than my previous hospital-connected neurology center, who completely dumped me as a patient because my seizures weren't epileptic (which we'd told them before they wanted me to do a study to prove it) and epilepsy is all they treat.
8 notes
·
View notes
Text

Ever since my epilepsy diagnosis I have come across people who view me as a burden and treated me as such. I accepted this treatment for so long and believed everything they said.
It's taken a long time to realize they were wrong.
I'm not a burden to those who love me.
19 notes
·
View notes
Text
Finding the Best Neurologist in Dubai: A Comprehensive Guide
Navigating Complex Neurological Conditions
When faced with neurological conditions, seeking expert care is paramount. In Dubai, a city renowned for its world-class healthcare, finding the best neurologist can significantly impact your health and well-being. This comprehensive guide will help you navigate the process of finding the right neurologist in Dubai.

Understanding Neurological Conditions
Neurological conditions affect the brain, spinal cord, and nerves, leading to a wide range of symptoms. Some common neurological conditions include:
Stroke
Multiple Sclerosis (MS)
Parkinson's Disease
Alzheimer's Disease
Epilepsy
Headaches and Migraines
Neuropathies
Spinal Cord Injuries
Why Choose a Neurologist in Dubai?
Dubai has emerged as a global healthcare hub, attracting renowned medical professionals from around the world. When you choose a neurologist in Dubai, you can expect:
World-Class Expertise: Access to highly skilled neurologists with extensive experience in diagnosing and treating complex neurological conditions.
Advanced Technology: State-of-the-art diagnostic tools and treatment options, including advanced imaging techniques and minimally invasive procedures.
Comprehensive Care: A multidisciplinary approach involving neurologists, neurosurgeons, physical therapists, and other specialists to provide holistic care.
International Standards: Adherence to international standards of medical practice and patient care.
Multicultural Environment: A diverse healthcare environment that caters to patients from various cultural backgrounds.
Tips for Finding the Best Neurologist in Dubai
Seek Recommendations: Ask your primary care physician, friends, or family members for recommendations. Word-of-mouth referrals can be invaluable.
Check Credentials: Ensure the neurologist is board-certified and has relevant qualifications and experience.
Research Online: Utilize online resources to research neurologists, read patient reviews, and check their credentials.
Consider the Clinic or Hospital: The reputation of the clinic or hospital where the neurologist practices can also influence the quality of care.
First Consultation: Schedule a consultation to discuss your medical history, symptoms, and concerns. A good neurologist will listen attentively and answer your questions.
Communication Skills: Effective communication is crucial. Choose a neurologist who can explain complex medical information in a clear and understandable way.
Comfort Level: A good doctor-patient relationship is essential. Choose a neurologist with whom you feel comfortable discussing your health concerns.
Conclusion
Finding the best neurologist in Dubai is a crucial step in managing neurological conditions. By following these tips and seeking expert advice, you can make informed decisions and receive the highest quality care. Remember, early diagnosis and prompt treatment can significantly improve outcomes.
4 notes
·
View notes
Note
Listening to BiB is like:
*song starts playing*
"oh this is a really good one!"
Autism, also called autism spectrum disorder[a] (ASD) or autism spectrum condition (ASC),[11] is a neurodevelopmental disorder characterized by symptoms of deficient reciprocal social communication and the presence of restricted, repetitive, and inflexible patterns of behavior that are impairing in multiple contexts and excessive or atypical to be developmentally and socioculturally inappropriate.[12][13] Other common signs include difficulty with social interaction, verbal and nonverbal communication, along with perseverative interests, stereotypic body movements, rigid routines, and hyper- or hypo-reactivity to sensory input. Autism is clinically regarded as a spectrum disorder, meaning that it can manifest very differently in each person. For example, some are nonspeaking, while others have proficient spoken language. Because of this, there is wide variation in the support needs of people across the autism spectrum.
Psychiatry has traditionally classified autism as a mental disorder, but the autism rights movement (and an increasing number of researchers) see autistic people as part of humanity's natural neurodiversity.[14][15] From this point of view, autistic people may also be diagnosed with a disability of some sort, but that disability may be rooted in the systemic structures of a society rather than in the person;[16] thus, proponents argue that autistic people should be accommodated rather than cured.[17] The neurodiversity perspective has led to significant controversy among those who are autistic and advocates, practitioners, and charities.[18][19]
There are many theories about the causes of autism; it is highly heritable and mainly genetic, but many genes are involved, and environmental factors may also be relevant.[20] The syndrome frequently co-occurs with attention deficit hyperactivity disorder, epilepsy and intellectual disability, and research indicates that autistic people have significantly higher rates of LGBTQ+ identities and feelings than the general population.[21][22][23] Disagreements persist about what should be included as part of the diagnosis, whether there are meaningful subtypes or stages of autism,[24] and the significance of autism-associated traits in the wider population.[25][26] The combination of broader criteria, increased awareness, and the potential increase of actual prevalence, has led to considerably increased estimates of autism prevalence since the 1990s.[27][28] The World Health Organization estimates about 1 in 100 children had autism between 2012 and 2021, as that was the average estimate in studies during that period, with a trend of increasing prevalence over time.[b][9][10] Boys are also significantly far more frequently diagnosed than girls.[29] The increasing prevalence has reinforced the myth perpetuated by anti-vaccine activists that autism is caused by vaccines.[30]
There is no cure for autism. Although early intervention services based on applied behavior analysis (ABA) can help children gain self-care, normative social, and language skills,[31][32][33][34] independent living is unlikely with more severe forms of the condition. Some in the autism rights movement consider ABA therapy unethical and unhelpful due to a perception that it emphasizes normalization instead of acceptance and its potential for causing harms.[35][36][37] ABA's prioritization of compliance and behavioral modification over a person's needs can lead to harmful consequences, including prompt dependency, loss of intrinsic motivation, and even psychological trauma. Curtailing self-soothing behaviors is potentially classifiable as a form of abuse.[38] Speech and occupational therapy, as well as augmentative and alternative modes of communication, are effective adjunctive therapies. Pharmacological treatments may also be useful; the atypical antipsychotics risperidone and aripiprazole are empirically validated for alleviating comorbid irritability, though they tend to be associated with sedation and weight gain.[39]
5 notes
·
View notes
Text
Blanche Wittman and PNES (Psychogenic Non-Epileptic Seizures)
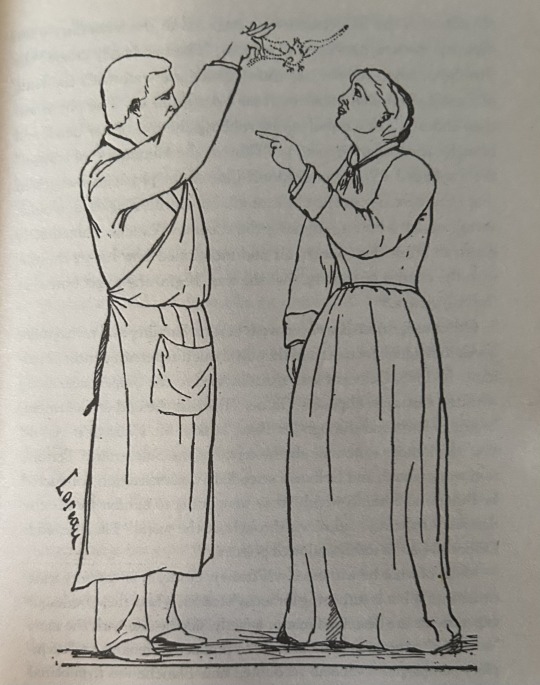
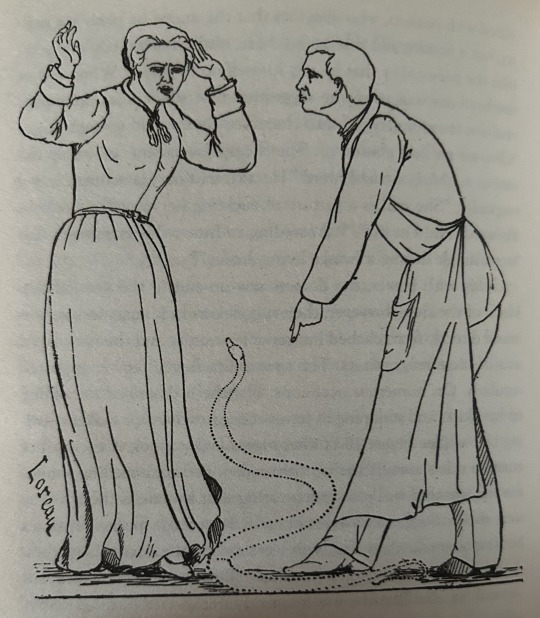
Blanche Wittman, famed La Salpêtrière hysteric is the pinnacle of what the modern-day public thinks of when they imagine "female hysteria" that being young women institutionalized and used as entertainment. In fact, most of our modern understanding of what hysteria was comes from Jean-Martin Charcot's work on La Salpêtrière's hysterics, one of the most notable examples being Blanche Whittman, forever immortalized in photographs and of course the famous André Brouillet painting "Une leçon clinique à la Salpêtrière"


Her dramatized and public portrayal of hysteria has led to an increase in awareness of neurological and psychiatric conditions primarily effecting women, PNES (Psychogenic Non-Epileptic Seizures) which falls somewhere between psychiatric and neurological being one of these conditions, which seems a likely diagnosis for her if Blanche were to visit a modern neurology clinic.
What is PNES? PNES (Psychogenic Non-Epileptic Seizures) are seizure episodes that highly resemble that of an epileptic seizure, though no brain activity resembling epilepsy is present. These seizures have a psychological basis, instead of a neurological one, though neurological imaging may be used in diagnosis before treatment is turned over to a psychologist or psychiatrist.
Blanche Wittman's symptoms present in her public case information across volumes of "Iconographie photographique de la Salpêtrière" line up very well with the current diagnostic criteria of PNES.
When Blanche was first admitted into La Salpêtrière in 1877, she was 18 years old, 1.62 meters tall (considered above average in this period) and weighing in at 70kg. Being raised in a troublesome and poor family, she was never taught to read and her intelligence was labeled as being below average by the hospital.
As stated before, Blanche was raised in a troublesome family, having nine siblings, including five who died in childhood from epilepsy and convulsions. Her father was prone to "fits of rage" and physically abused the young Blanche in many instances, and her mother died when Blanche was young, though the exact age varies from source to source.
She began a sexual relationship with her employer, a furrier, by force at the age of 15. She then admitted herself to a hospital (unclear exactly where) to escape the abuse eight months after it began. A while later she reported another sexual relationship with a boy called Alphonse. It seems to be unclear whether this relationship was consented to by Blanche, or another example of sexual abuse against her.
Abuse, especially sexual is an extremely common background in those with PNES. A diagnosis of PTSD or C-PTSD with PNES is quite common. It seems extremely likely that her abuse she went through played a role in these "hysterical attacks"
After some time taking refuge at a convent (Blanche seems to have been a devout Catholic, wearing a scapular and collecting various pieces of Christian iconography) she began working as a servant at La Salpêtrière, thinking this would make it easier for her to be eventually admitted into the hospital after they see her attacks.
Blanche eventually succeeded in her goal of being admitted to La Salpêtrière in 1877, at the age of 18. Her time there coincided with the peak of Jean-Martin Charcot's studies on hysteria, and she quickly became one of his star patients. Charcot’s research focused on hysteria as a neurological disorder, and his methods of public "demonstrations" of hysterical patients, including Blanche, led to increased attention to the condition. These public displays, often featuring dramatic reenactments of symptoms, cast a long shadow over how hysteria and by extension, women’s health was perceived for decades.
Blanche’s displays of hysteria to the public were not only attended by a medical crowd, but was also popular among a non-medical crowd, including that of actors, who would come to study Blanche’s intense displays of emotion under hypnosis.
Hypnosis was frequently used on Blanche during these displays, often to achieve the state of somnambulism, or extreme suggestibility, where the hypnotist could make her to believe just about anything they so desired, the effects sometimes even lasting long after the trance.
While the primary purpose of these displays was supposedly to educate on hysteria, they often came off as more entertaining stage hypnosis than anything. Some of this was mindless entertainment, though some was clearly intended to use Blanche’s fear and distress for laughs, whether to the audience or the hospital staff themselves, often young male medical students, finding it hilarious to sexualize and upset her.
During her intense states of somnambulism, she was often made to hallucinate snakes and rats at her feet. She would hike up her skirt and squeal, prompting voyeuristic laughs from the audience.
Unlike the many “wandering womb” theories we often associate with hysteria today, Charcot was among the first who believed hysteria had a neurological origin, attributing symptoms like convulsions, paralysis, and loss of consciousness to issues within the brain. This makes sense as Charcot was most certainly extremely knowledgeable about neuroscience. In fact, he was the first to identify and name multiple sclerosis as it’s own distinct condition, pioneered much amyotrophic lateral sclerosis research (the disease even being known as Charcot’s disease in parts of the world) and is associated with at least 15 different diseases named after him. For this reason, it only makes sense that a condition with invisible physical pathology must be caused by nervous system abnormalities, this being even more apparent when remembering this was a time before complex brain imaging and EEG technology was in use, it was nearly impossible to know whether something was psychological or neurological, and Charcot believed the latter.
However, many of these symptoms would align more closely with what we now understand as psychogenic non-epileptic seizures (PNES), a condition rooted in psychological trauma rather than physical abnormalities in the brain. Today, PNES is understood as a dissociative disorder, often linked to past trauma, which manifests in seizure episodes without the electrical disruptions seen in epilepsy.
Before her time institutionalized, Blanche's life was full of trauma and abuse, often seen in PNES patients. Not only that but Blanche also demonstrated a good example of "the teddy bear sign" a frequent pattern in PNES patients and an aid in diagnosis. A majority of PNES patients show up to EEG monitoring appointments with a comfort item, most often a stuffed animal. While we don't know exactly what Blanche would have done in the modern day, we do know she was an avid collector of stuffed animals and various little trinkets. This was common behavior among hysterics, suggesting what in the modern day we would call PNES was common among hysterics.
The "hysterical attacks" that made her a spectacle were, in all likelihood, trauma responses—demonstrations of a mind and body deeply affected by abuse. While these days are long gone, it's important to see just how much this outdated understanding of the brain both holds back and progresses our knowledge of the connection between body and brain.
3 notes
·
View notes