Note
Honestly my biggest problem with self diagnosis is people deciding that they have something, inserting themselves into the community, and then acting like authorities on that condition and talking over people who actually have it.
I have autism and I'm really active in the communities so I'll use that as an example.
I very frequently see self diagnosed people insisting that being autistic is an amazing, wonderful superpower that causes them no problems whatsoever, and saying that the only reason it's considered a disability is because society is ableist.
They come into the community, see that the rest of us are struggling with our literal disability, and then go "Um, autism isn't a disability, it's amazing! I love being autistic, so if you don't, you just have internalized ableism and you hate yourself :)"
Which is, uh, certainly an interesting take considering the diagnostic criteria in the DSM-V and ICD-11 states that to be diagnosed with autism the symptoms must cause significant impairment.
And like, even if we did live in a magical utopia where autism is 100% accepted and no one is ever ableist (which will not exist in my lifetime, if ever), I would still hate being autistic!
I would still be unable to wear clothes that I want to wear or eat food that I want to eat because the texture makes me want to cry, and I would still have horrible meltdowns that result in me punching and biting myself.
We're also shamed and silenced for wanting actual, effective treatments, which is fucking insane. Why is it okay if I want medication to treat my ADHD, but if I want medication to stop my nervous system from overloading and breaking down over normal stimuli like wearing jeans or hearing a dog bark, I'm an evil ableist eugenicist?
I have no problem with people who take the time to read through the diagnostic criteria, read posts from people in the community, and then go, "Yeah, you know what, I've ruled out everything else it could be, I'm probably autistic."
But if someone's just going to watch a few Tiktoks with vague, cutesy symptoms and go "Omg I tap my fingers, that's stimming! And I really love cartoons, and I'm super shy and awkward sometimes! I'm definitely neurospicy :3" and then come into the community and demand that we sanitize everything and stop talking about our scary, yucky, unpleasant symptoms like incontinence and meltdowns and executive dysfunction, then yeah, get the fuck out.
--
It's always annoying when someone enters a space that's essentially about providing resources and starts hogging them or blocking others' access.
98 notes
·
View notes
Text
On Nesta and Alcoholism
I’ve seen a couple takes recently saying essentially “Nesta is not an alcoholic bc xyz”. The spirit it’s said in is usually supportive of her and based in countering the way the IC dehumanizes and stigmatizes her, which is great AND there are some common stereotypes about alcoholism that can deter people from seeking treatment or realizing their alcohol use is hurting them. Alcohol is the 4th leading cause of preventable death in the United States, and ~11% of people over 18 qualify for an alcohol use disorder every year.
Creds: am a currently practicing counselor with specialization in addiction treatment
So a few basic points on problematic alcohol use:
Risk exists on a spectrum from no risk to imminent fatality. Most users fall in the middle. We have a very narrow portrait of what alcoholism looks like in popular media, especially in women, and it’s almost always the most severe end of the spectrum.
Use does not have to be 24/7 to be risky. Binge drinking, as defined by 4+ drinks for afab people and 5+ drinks for amab people in one drinking episode, has just as much potential for chemical dependency and damage.
A person does not have to be chemically dependent (“addicted”) or have cravings to have an alcohol use disorder, nor does everyone with an AUD go through withdrawal.
Using alcohol as a tool for emotional regulation, sleep, social anxiety, etc outside of rare occasions qualifies as problematic use. This kind of drinking is, unfortunately, very socially acceptable.
Problem drinking is progressive, and tends to get worse without conscious choice or effort to change
You can have a dysfunctional relationship with alcohol without having an AUD. You can have an AUD while still being a fully functioning person on the outside.
Risky or problematic use is often a symptom of a deeper emotional wound, which should be treated with care and seriousness even if someone doesn’t meet the criteria for an AUD.
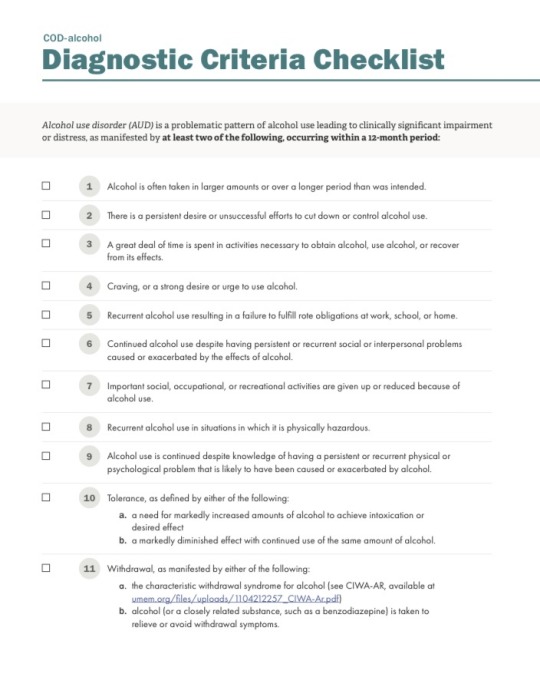
They don’t have the DSM in Prythian obviously, but for us mere mortals here are the criteria. A person only needs TWO to qualify for a diagnosis:
As a clinician, I usually look for a few hallmarks.
Alcohol is one of or is the primary strategy a person uses to regulate emotion and stress, or is a common way someone rewards or incentivizes themselves
Alcohol is an important “character” in at least one sphere of someone’s life and they feel the absence when it’s not there, eg. social activities all center around drinking, essential part of dinner/sleep routine etc
The client has feelings of shame or guilt around drinking, choices they make while drinking, or the consequences it’s had in their life. oR they feel a defensiveness about their drinking and distress at the idea of stopping.
Anyway, that’s my PSA. I would diagnose Nesta with an AUD, but I would also diagnose her with PTSD, and also diagnosis is a horribly flawed system that allows people to access their insurance benefits. I guess I just want to say that you don’t have to look like the media version of alcoholism to be concerned about your drinking or to deserve quality treatment. If you’re concerned, help is available.
36 notes
·
View notes
Text






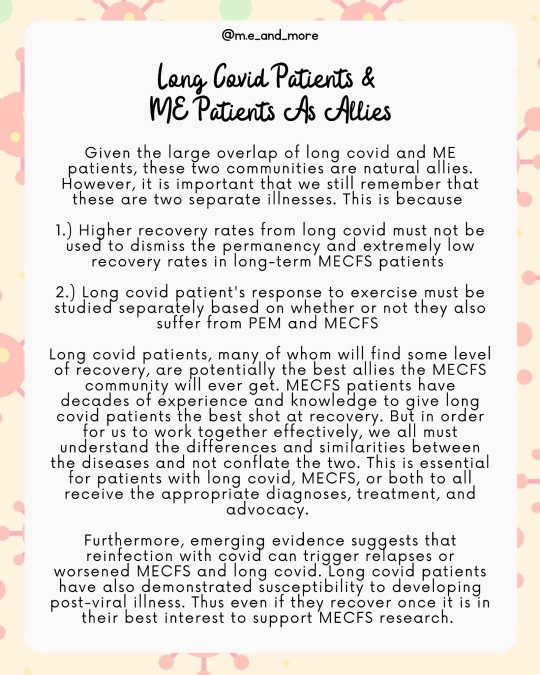
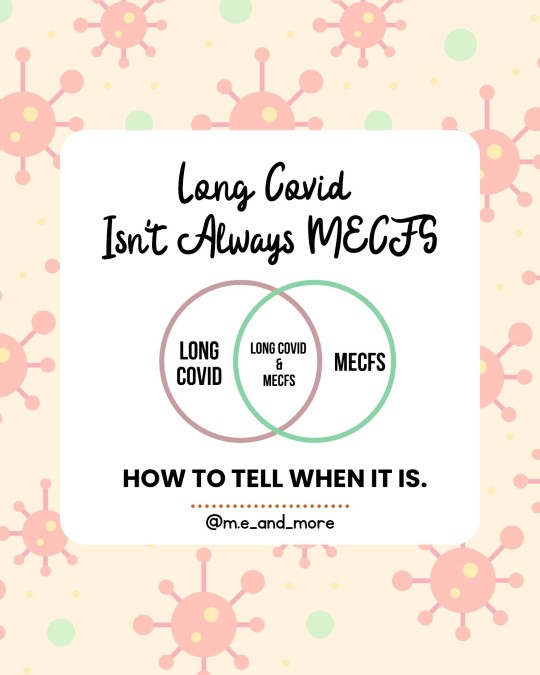
Not all #LongCovid is #myalgicEncephalomyelitis.
While its super important to raise awareness of the simularities of the #millionsMissing with #MECFS and #millionsMore with #LongC it is also essential to recognize that only a subset of #covid #longhaulers meet the criteria for a diagnosis of ME.
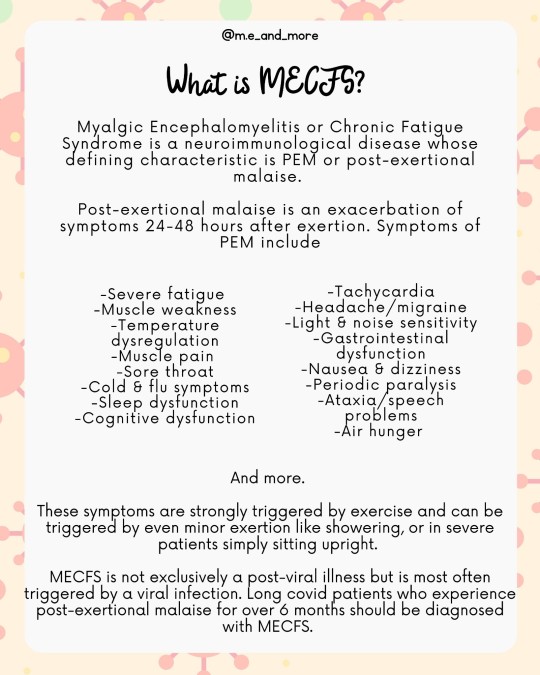
ME aka #ChronicFatigueSydnrome is not the same as #chronicFatigue. The defining symptom of ME / #CFS is #PostExertionalMalaise or an exhasurabtion of metabolic, neurological and immune dysfunction symptoms 24-48 hours after exertion.
When you are talking about long covid patients who experience #PEM you should talk about MECFS because that is what these patients have.
When you are talking about long covid patients be clear that only the subset with PEM have MECFS.
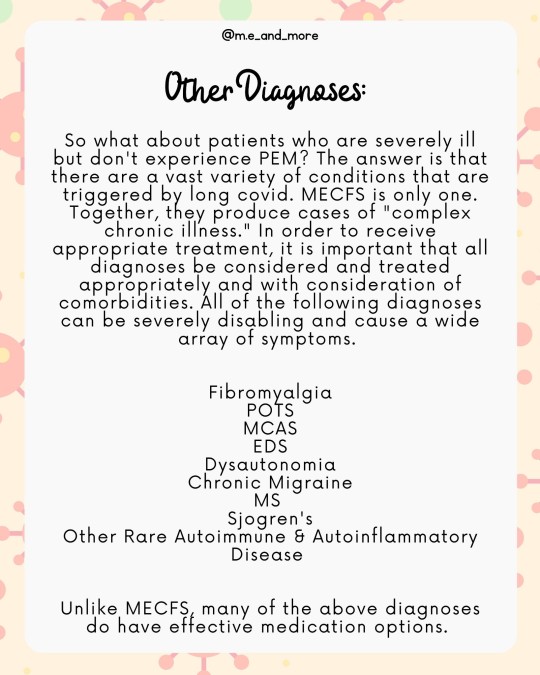
It is important for patients with long covid to receive the correct diagnoses, because while there are no FDA approved treatments for ME, many commorbidities do have effective medication options. Management of ME must also be tailored based on a patients commorbidities.
Patients with MECFS and post viral fatigue syndrome must not be prescribed GET or CBT. This includes all long covid patients with PEM.
Long covid patients who experience PEM should be advised to #StopRestPace and informed about the importance of pacing agressively not just to prevent symptoms from fatigue but to prevent PEM in the following days. This is regardless of whether they have PVFS (less than 6 months post covid) or MECFS (more than 6 months)
Because long covid is a broad category that encompasses patients MECFS #MCAS #fibromyalgia #POTS #dysautonomia #autoimmune and #autoinflammatory diseases in many combinations the prognosis for long covid patients is much more variable than that of ME patients and recovery is more likely in early stages of ME, long covid patients who recover should not generalize their experience onto MECFS patients more broadly and should continue to support MECFS research.
MECFS patients have decades of experience with pacing, medical gaslighting, chronic illness, housebound and bedbound life and more. We hope that #covidLonghaulers will #LearnFromME and ally with us to end #postViralIlness
#mecfs#long covid#long haul#millions missing#millions more#post viral illness#post viral syndrome#post viral fatigue#chronic fatigue#chronic fatigue syndrome#myalgic encephalomyelitis#education#health#evidence based medicine#covid#chronic illness#chronically ill#pots#mcas#dysautonomia#fibromyalgia
321 notes
·
View notes
Text
Understanding PCOS: Unravelling the Complexity of a Common Hormonal Disorder
Hello and welcome back to Shining Through PCOS! I’m Luciana, your guide on this journey through the complexities of PCOS and its impact on our skin, hair, and overall confidence. Today, we’re diving deeper into what PCOS really is, how it’s diagnosed, and the unique ways it affects women.
What is PCOS?
Polycystic Ovarian Syndrome (PCOS) is more than just a hormonal imbalance; it's a multifaceted condition that affects approximately 1 in 10 women of reproductive age around the globe (Singh et al., 2023). The symptoms can vary significantly, from irregular menstrual cycles to the presence of polycystic ovaries and elevated levels of androgens—often referred to as male hormones (Singh et al., 2023). One of the most challenging symptoms is hirsutism, characterised by the growth of coarse, dark hair in areas typically associated with male hair patterns, such as the face, chest, and back (Spritzer et al., 2022).
For many women, including myself, the emotional toll of excess hair growth is profound. It can feel like a constant battle against your own body, leading to feelings of frustration and embarrassment, especially when it’s in visible areas. I remember feeling overwhelmed by societal expectations of beauty while grappling with my own unwanted hair growth, leading me to seek out various treatments such as depilatory creams and shaving that only exacerbated my issue.
Diagnosing PCOS: The Complexity of Symptoms
Diagnosing PCOS is not always a straightforward process. This can be quite difficult because it can manifest so differently from woman to woman. In an attempt to help doctors better identify the condition, the Rotterdam criteria were introduced (Smet & McLennan, 2018). This diagnostic tool provides a standardised way to assess whether someone has PCOS by looking at three key factors:
Irregular or absent periods – This signals potential ovulatory dysfunction.
Signs of hyperandrogenism (excess androgens) – Such as excess hair growth, acne, or thinning hair on the scalp.
Polycystic ovaries on an ultrasound – Where the ovaries show multiple, small cysts.
To meet the diagnosis of PCOS, two out of these three criteria must be present. What’s important to note is that you don’t need to meet all three, which can lead to different manifestations of PCOS depending on the patient (Smet & McLennan, 2018). However, the absence of a universal diagnostic test can lead to delays in receiving proper care.
Many women find themselves navigating a confusing landscape where symptoms overlap with other conditions, making it crucial for us to advocate for our health. Often, healthcare providers may overlook the complexity of PCOS, attributing symptoms solely to lifestyle factors or weight issues, rather than considering the broader hormonal picture (Dewani et al., 2023).
The Hormonal Landscape and Its Impact on Women
The hormonal imbalance at the heart of PCOS doesn’t just affect our reproductive health; it also has significant implications for our metabolic and emotional well-being. Women with PCOS are at a higher risk of developing insulin resistance, which can lead to weight gain and complicate our ability to manage our symptoms (Barber et al., 2019). This can create a vicious cycle, where weight gain exacerbates hirsutism, making it even more challenging to feel a sense of autonomy over our bodies (Barber et al., 2019).
Moreover, the psychological aspects of PCOS are often overlooked. Many women report feelings of anxiety and depression associated with their symptoms, which can be exacerbated by societal pressures and beauty standards (Almhmoud et al., 2024). When we look at the prevalence of conditions such as generalised anxiety and depressive disorders amongst diagnosed women with PCOS, the rate is between 28% and 39% for anxiety, and 11% to 25% for depression (Dewani et al., 2023). This makes it all the more essential to recognise that PCOS is not just a reproductive disorder but a condition that impacts many facets of our lives.
The Role of Laser-Based Hair Reduction (LBHR)
For women dealing with hirsutism, finding effective and long-lasting treatment options can feel like a constant battle. One treatment that has gained significant attention is Laser-Based Hair Reduction (LBHR), which offers a long-term solution for managing excessive hair growth (Hosseini et al., 2022). Although it's not a cure for PCOS, LBHR can help in controlling a key symptom: unwanted hair growth.
As someone who has experienced this issue firsthand, and as a dermal clinician who has seen numerous patients benefit from LBHR, I truly feel that this treatment can help empower women by giving them a sense of control over their bodies. I’ve seen women come into the clinic feeling closed off, hesitant, and unsure during their first consultation. But as their treatments progress, something amazing happens—their confidence begins to grow. Session after session, they become more comfortable in their own skin, seeing results and no longer feeling defined by their unwanted hair. It’s truly rewarding to witness that transformation, especially as this is something that hits very close to home.
In saying this, it's important to have a clear understanding of what LBHR can—and cannot—achieve. While LBHR significantly reduces the rate of hair regrowth, it does not address the underlying hormonal imbalances that cause hirsutism in PCOS. PCOS is a chronic hormonal condition, and excess androgens (male hormones) will continue to trigger hair growth even after several laser sessions (Kopera et al., 2010). What LBHR does is target the melanin within the hair follicle, slowing down the process by damaging these follicles, leading to thinner, finer hair that delays the growth process over time (Bhat et al., 2020).
It’s important to note that LBHR typically requires multiple sessions spaced out over several weeks to months, as hair grows in cycles, and laser treatments target hair follicles during their active growth phase (anagen phase). In my experience, patients usually see optimal results after 6 to 8 sessions, but individual responses vary based on factors like skin type, hair texture, and hormonal fluctuations (Bhat et al., 2020). This makes a personalised treatment plan crucial.
One thing I always emphasise to patients is that LBHR isn’t a quick fix, but rather a long-term management tool. Even after completing the initial series of treatments, most women with PCOS will need maintenance sessions to keep hair growth under control. While it can significantly improve quality of life by reducing the need for constant hair removal methods like shaving, waxing, and depilatory creams, LBHR should be viewed as part of a comprehensive approach to managing PCOS—not a stand-alone solution (Sheehan, 2004).
Combining LBHR with treatments that address hormonal imbalances, such as medication (like anti-androgens) or lifestyle changes, ensures the most effective, lasting results (Tan et al., 2024). Think of it as attacking an issue from every angle to ensure the best outcome. In this way, LBHR becomes a cornerstone in a broader PCOS management plan, helping to reduce the emotional and physical toll of hirsutism while maintaining realistic expectations for long-term hair control.
Finding the Right Treatment Path for You
Navigating PCOS requires a holistic approach. From my experiences, having a healthcare provider who understands both the medical and aesthetic aspects of treatment is essential. We spoke earlier about combination therapies, but a similar multidisciplinary approach, including endocrinologists, dermatologists, and even nutritionists, can help us manage our symptoms in the most effective way.
In my own journey, I learned that addressing the root causes of PCOS—rather than just its symptoms—is the key to achieving lasting relief. This isn’t a standalone task and involves lifestyle changes alongside medical treatments tailored to my needs.
In future posts, we’ll explore these topics in more depth, discussing the science behind PCOS, how it affects hair growth specifically, and how we can navigate the challenges many women face while managing this condition. My hope is that by sharing these insights, we can create a supportive community for all of us living with PCOS as a collective.
Thank you for joining me as we unravel the complexities of PCOS and its impact on our lives. Together, let’s empower ourselves and others to take control of our health and well-being.
Until next time, Luciana ᥫ᭡
References
Almhmoud, H., Alatassi, L., Baddoura, M., Sandouk, J., Alkayali, M. Z., Najjar, H., & Zaino, B. (2024). Polycystic ovary syndrome and its multidimensional impacts on women’s mental health: A narrative review. Medicine, 103(25), e38647. https://doi.org/10.1097/md.0000000000038647
Barber, T. M., Hanson, P., Weickert, M. O., & Franks, S. (2019). Obesity and polycystic ovary syndrome: Implications for pathogenesis and novel management strategies. Clinical Medicine Insights: Reproductive Health, 13, 117955811987404. https://doi.org/10.1177/1179558119874042
Bhat, Y. J., Bashir, S., Nabi, N., & Hassan, I. (2020). Laser treatment in hirsutism: An update. Dermatology Practical & Conceptual, e2020048. https://doi.org/10.5826/dpc.1002a48
Dewani, D., Karwade, P., & Mahajan, K. S. (2023). The invisible struggle: The psychosocial aspects of polycystic ovary syndrome. Cureus. https://doi.org/10.7759/cureus.51321
Hosseini, M. H., Ehsani, A. H., Fakour Y., Aryanian Z., Elhamfar M., & Noormohammadpour P. (2022). Effect of Laser-Assisted Hair Removal (LAHR) on the Quality of Life and Depression in Hirsute Females: A Single-Arm Clinical Trial. J Lasers Med Sci, 13. https://doi.org/10.34172/jlms.2022.46
Kopera, D., Wehr, E., & Obermayer-Pietsch, B. (2010). Endocrinology of hirsutism. International Journal of Trichology, 2(1), 30. https://doi.org/10.4103/0974-7753.66910
Sheehan, M. T. (2004). Polycystic ovarian syndrome: Diagnosis and management. Clinical Medicine & Research, 2(1), 13-27. https://doi.org/10.3121/cmr.2.1.13
Singh, S., Pal, N., Shubham, S., Sarma, D. K., Verma, V., Marotta, F., & Kumar, M. (2023). Polycystic ovary syndrome: Etiology, current management, and future therapeutics. Journal of Clinical Medicine, 12(4), 1454. https://doi.org/10.3390/jcm12041454
Smet, M. E., & McLennan, A. (2018). Rotterdam criteria, the end. Australas J Ultrasound Med, 21(2), 59-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8409808/
Spritzer, P. M., Marchesan, L. B., Santos, B. R., & Fighera, T. M. (2022). Hirsutism, normal androgens and diagnosis of PCOS. Diagnostics, 12(8), 1922. https://doi.org/10.3390/diagnostics12081922
Tan, K., Coster, T., Mousa, A., Mar, A., Piltonen, T., Boyle, J. A., Teede, H., Joham, A., Romualdi, D., & Tay, C. T. (2024). Laser and light-based therapies for hirsutism management in women with polycystic ovarian syndrome. JAMA Dermatology, 160(7), 746. https://doi.org/10.1001/jamadermatol.2024.0623
7 notes
·
View notes
Text
A lot of this "but the point of DID/OSDD is to hide trauma!" garbage, because it IS garbage, comes from the fact that people keep seeing DID/OSDD as a "trauma disorder" and not a dissociative disorder. As it really is.
DID/OSDD is a dissociative disorder. Dissociation is where you distance from your own mind/body. Everyone does it at some point. It's a normal function of the brain, especially in response to stress, though it doesn't ONLY happen as a stress/trauma response.
Disorder is when something becomes distressing and/or dysfunctional. No distress/dysfunction? No disorder. Basically, a dissociative disorder is when distancing from your mind/body-- often as a stress/trauma response-- takes an "unhealthy" turn.
What ARE trauma disorders?
Reactive Attachment Dis
Disinhibited Social Engagement Dis
Posttraumatic Stress Dis
Acute Stress Dis Adjustment Dis
Other Specified Trauma- and Stressor-Related Dis
Via the DSM 5. Note that DID/OSDD... aren't there, anywhere.
Dissociative disorders are "frequently found in the aftermath of trauma", with "many of the symptoms ... influenced by the proximity to trauma". They "are placed next to, but are not part of, the trauma- and stressor-related disorders". Again, via the DSM 5.
Saying that the "point" of DID/OSDD is to "hide trauma" is a fundamental misunderstanding of what dissociation is, ignores that amnesia isn't always required (for OSDD), and that even if amnesia is present... it doesn't always hide trauma or sysmates.
Calling trauma the "point", and calling it a "trauma disorder", centers trauma in a disorder where trauma isn't even a dx criterion. Nowhere in the DSM or ICD does it say that criterion A-- essentially, plurality-- must be formed by trauma.
Because they don't KNOW if trauma/stress is the only thing that can cause DID/OSDD... because it's not the only thing that can cause dissociation. They just kind of assume, for the MOST part, that yeah DID/OSDD is caused by trauma/stress. It's a fair idea!
Like if a mind is dissociating to the point that other minds start to form, it makes sense that it's usually something like trauma at the root. But it's not to hide the bad, it's to COPE with it. There's a difference. Amnesia might be part of that, sure.
But again, not all with DID/OSDD have amnesia, or amnesia surrounding the trauma they may have experienced. (We remember ours.) Some may have a "trauma holder", but that's a specific role that not all with DID/OSDD have. Not all need it.
So then, what is the "point".
Kinda simple. There isn't one, singular "point", because DID/OSDD-- and plurality in general-- isn't a movie with the same beginning, middle, and end every time. It's like asking the "point" of autism, OCD, or phobias.
While trauma work is sometimes involved in DID/OSDD treatment, decent professionals focus on cooperation, communication, and reducing distress/dysfunction. Dissociation doesn't, inherently, hide trauma. It helps cope with it. Sometimes amnesia sets in after.
Dissociation, plurality, disorder, amnesia, and trauma are all different things. When it happens all at once, that's usually DID! But all of those things can exist separately, or combine in other ways. Trauma doesn't need to be, and isn't always, the "point".
And once again... DID/OSDD aren't the only kinds of plurality. If ALL plurality was disordered, it wouldn't exist as it's own lil' dx criteria. So no, plurality isn't a "trauma disorder". Neither's DID/OSDD. Stop it.
#plurality#actuallyplural#actuallymultiple#plural systems#endo positive#endo safe#sysmeds fuck off#syscourse
25 notes
·
View notes
Note
hello!!
i was just going through your blog and you have mentioned a anxiety disorder a few times, i do not really know anything about it so if you want to please educate me on this concept, if you dont wanna its all good. just know i am here if u wanna talk any time :)))))))))
HI!! I absolutely wanna educate you, thanks for asking :) This is suuuper long though, I'm so sorry :´(
There's a few anxiety disorders out there but the most common ones are social anxiety disorder or panic disorder, and then there's GAD which is short for Generalized Anxiety Disorder, and I have GAD.
Stress and anxiety is an evolutional response to danger more commonly known as fight or flight, which is the sympathetic nervous system being activated. GAD is the body being stuck in fight or flight mode, whereas social anxiety, for instance, generally means that the sympathetic nervous system kicks in in social environments (like a phone call or meeting a person).
GAD, usually presents as excessive worry about anything and everything. My grandmother will cough and my brain will think "she has lung cancer and she's dying". When I didn't know I was ill I was basically living in a nightmare. I've had a lot of therapy so nowadays I can identify it as an anxiety thought and ignore it. Some days I can't shake them, and those days are just bad anxiety days. And I can either power through it or I can take anxiety medication, but I can't work on those because they make me really drowsy.
You can develop GAD at any age, really. All it takes is being under extreme stress for a period of time, I think the criteria is like 6 months or something. There are differential diagnoses like chronic fatigue syndrome, ADHD/ADD, bipolar disorder and clinical depression that have to be excluded that early on, though. It's fairly easy to treat if caught early. It's hell, but they'll most likely have you on antidepressants and or something that helps you sleep and give you therapy. Therapy will help you deal with your triggers through cognitive behavioural therapy, exposure therapy (where you're literally exposed to your trigger/fear in a controlled environment) and that will in theory treat the disorder. You're never gonna remove anxiety because it's a survival instinct, but you're basically telling your brain that it's overreacting, and if you get help early you can actually be cured.
I have GAD because I was bullied between ages 10-16, and there's also a probability that my parents' divorce started the whole thing. The problem was that I didn't get proper help until I was 19 and I didn't even meet with a psychiatrist until I was 25 (I'm 29 now). I'm never gonna be cured, we're basically just looking for ways to help me live WITH my anxiety. I just have too many triggers and my body is too used to being in this state that there's currently no way of fixing it.
GAD sometimes comes with executive dysfunction which is where you just physically can't do things. It's a very common ADHD symtom as well. You know you need to do it but you can't, and it essentially becomes a handicap. My most common triggers for executive dysfunction is school work of any kind, opening my mail or important phone calls. In Sweden this is actually recognized as a handicap, which means that I can get help faster. But I have to make the call, which I can't do because of my anxiety so idk how foolproof that safeguard is. I'm on sick leave right now because of extreme stress (it could be chronic fatigue syndrom, but it's too early to tell rn) and now my executive dysfunction is everywhere, so like showering, cleaning my flat or making food is extremely tough and usually doesn't happen, so I have to take shortcuts (like eating at my parents' house, not washing my entire body and only cleaning small parts of my flat a a time).
Apart from being afraid anxiety triggers a lot of physical responses in your body because it is designed to keep us alive. If you have social anxiety you might have issues with your stomach (like stress pooping or nausea) when you have to engage with others or even, like, ride a train. GAD patiens almost always have chronic IBS (irritable bowel syndrome) and muscle pains because our bodies are constantly preparing for flight. I have really bad chronic muscle pain in my neck and upper back which leads to tension headaches. So on any given day, I'd rate my pain at a 5, and that's just. A thing I have to live with.
Physical activity generally alleviates the pain and the endorphins from workout are really beneficial but you can't exercise GAD away. It's just something that helps.
I'm on a high dose of antidepressants, antihistamines to make me sleep and quetiapine/seroquel, which is a mood stabiliser that basically reduces my executive dysfunction, and my medication is always gonna change depending on what my life looks like. Realistically I'm always gonna be on some form of antidepressant. I'm on SNRI's, which control the serotonin and noradrenaline in my brain.
Naturally, my serotonin is really low and my noradrenaline is really high, but in a healthy person the serotonin is high and the noradrenaline is low. The body typically restores the serotonin/noradrenaline levels during sleep, but my brain does the exact opposite so I just have extreme anxiety during the night, which is why I'm on medication to sleep bc otherwise I a) don't sleep and b) have terrible nightmares. I still have those nightmares, but the antihistamine I'm on is a muscle relaxant as well as an anxiety medication so it helps calm me down so I don't really remember my nightmares and it reduces my muscle pain by quite a bit. I still have bad nights that lead to bad days when I'm in a lot of pain. I sleep in a fetal position and tense up at night and I have a weighted blanket to help me relax so during those bad days I have trouble walking becausec my hip muscles are locked.
I think i basically covered everything. There's a lot more to it if you have any questions. I'm super open about this, and have been since I started therapy when I was 19 because I literally did not know I was sick until I was 17 and it took another two years to understand just how bad it was so I like to be as vocal as possible so people might find out and get help.
I'm SO SORRY for this long ass post though.
11 notes
·
View notes
Text
Accidentally deleted an ask about how mental disorders and mental illnesses are different things that I wanted to answer, so here we go
So we have three different sources all saying different things. Source 1 is a Cambridge study from 2002 that says the definitions of both terms, mental disorder and mental illness, are too vague to properly determine the difference between the two, and that more effective treatment of both might make the distinction easier to determine.
Source 2 is a health and wellness blog that says the two terms are often used interchangeably, and that there are subtle differences. A disorder is when there's not enough clinical evidence to diagnose an illness.
Source 3 is a health website that references The American Heritage Stedman's Medical Dictionary definitions of the words "disorder" and "illness". According to the Dictionary, "a disorder is A disturbance or derangement that affects the function of mind or body, such as an eating disorder or the abuse of a drug." And an illness is "A pathological condition of a body part, an organ, or a system resulting from various causes, such as infection, genetic defect, or environmental stress, and characterized by an identifiable group of signs or symptoms." Except, for some reason, they use the definition for "disease" instead of "illness". I want to keep this source even though it's inaccurate, because it will come into play in a minute.
Source 4 is from the online medical dictionary that reference multiple medical sources, including Stedman's. It's first definition defines a mental illness as "a broadly inclusive term, generally denoting one or all of the following: 1) a disease of the brain, with predominant behavioral symptoms, as in paresis or acute alcoholism; 2) a disease of the "mind" or personality, evidenced by abnormal behavior, as in hysteria or schizophrenia; also called mental or emotional disease, disturbance, or disorder, or behavior disorder"
and a mental disorder as
"any clinically significant behavioral or psychological syndrome characterized by distressing symptoms, significant impairment of functioning, or significantly increased risk of death, pain, or other disability. Mental disorders are assumed to result from some behavioral, psychological, or biological dysfunction in the individual. The concept does not include deviant behavior, disturbances that are essentially conflicts between the individual and society, or expected and culturally sanctioned responses to particular events."
So, we have four sources and four different ideas of what the difference between a mental illness and a mental disorder are. More, if you keep scrolling down on the online dictionary and see results from even more sources. You have one source that blatantly uses the definition of disease as the definition of illness. That article has not been updated since 2019.
The point of all this is to show how frustratingly inexact and inconclusive the definitions of terms are when it comes to psychology. Depending on what you're referencing, you'll be getting different, sometimes very different, definitions of what things are. There's no one answer to "What is the difference between a mental illness and a mental disorder". So to say that something that effects someone's mental image of themselves, for example, is not an illness but a disorder isn't based on objective, proven fact.
That's not to say mental illness isn't real, or any specific illness doesn't exist. But there's a huge difference between something like depression which is shown to be most likely caused by chemical imbalances in the brain, and something like gender dysphoria, which still has no known cause. Even the "solid" definition of depression isn't consistent across all medical sources. All this shows how inexact and open to interpretation psychology is. And, yes, how open it is to personal bias as well.
13 notes
·
View notes
Text
Liver transplantation.
The one time you might actually want cancer.
Why? Because having a primary liver cancer bumps you up on the liver transplant list. But it can't just be any cancer - there's a criteria for acceptable cancer burden for adult liver transplant, which is known as Milan Criteria. Essentially one big tumor smaller than 5 cm or 3 small tumors less than 3 cm each. The tumor can't have left the liver either aka metastasis. However if it's too small (<2 cm ), you don't get priority listing for having that cancer. Kind of like Goldilocks - the tumor has to be just right.
Now first off, you almost never get a primary liver tumor aka hepatocellular carcinoma (HCC) without something wrong in the liver in the first place.
This is usually Cirrhosis aka fibrosis of the liver, which can be caused by Hepatitis C or more commonly drinking too much alcohol too often. The liver fails cause its cells are dead or dying, and the resulting scarring prevents blood from your GI tract from returning properly to your systemic blood. This pseudo-blockage results in fluid backing up in your body, resulting in ascites (fluid in the belly) and pleural effusion (fluid in the lung space) and generalized soft tissue swelling.
The body tries to compensate for this by making alternate paths. Problem is the liver is also a filter, and bypassing the filter through an alternate path affects the brain - a common symptom is confusion and sometimes coma in these patients. Official term is hepatic encephalopathy.
Cirrhosis patients can also literally turn yellow because bilirubin, which occurs from the normal breakdown of red blood cells, can't be processed well by a dysfunctional liver. Liver does a lot of other important stuff too, but I'd go on forever with that - so I'll end that here.
In any case, the only treatment for cirrhosis is getting a new liver - once cirrhosis occurs, it cannot reverse, only worsen. The liver transplant list uses its own criteria known as MELD which I also won't get into here, but generally the sicker you are, the higher you are on the transplant list.
Cirrhosis is essentially a breeding ground for primary liver cancer because cirrhosis is essentially repeated constant inflammation - and all it takes is one cell to heal in the absolutely worst way - and then you have a cancer. This is why cirrhosis patients get yearly liver imaging screening to detect that.
Milan Criteria was created because a good number of liver transplants in cancer patients turned out to have recurrent liver cancer in the new liver. After Milan was implemented, long-term recurrence-free survival improved from 30% to 75%. I believe the sizes used in Milan acts as a surrogate for the likelihood of microscopic metastasis, cancer that's left the liver but too small to be seen in imaging, but don't quote me on that.
Now why did I bring this up? One of the residents asked out loud about why we don't just cut out the cancer.
For one, cirrhosis ensures another one will pop up eventually, and for two, cutting a cancer out also means cutting out good tissue (or semi-okay in a cirrhotic's case) to create the disease-free margin. You don't have much good tissue left in a cirrhosis liver.
You could ablate the cancer by frying it with heat or freezing it, but you again have the issues of damaging normal tissue. Typically excision or ablation is done when there's no chance patient will get a donor liver.
There's also TACE (transarterial chemoembolization) which can be used to shrink tumors, usually back into the limits imposed by Milan criteria. Because if your cancer is too big for Milan, you don't get a liver. There are strict rules for that, and if you break them, your liver transplant service is not getting donor livers.
4 notes
·
View notes
Text
Common Leadership Mistakes to Avoid
Common Leadership Mistakes to Avoid http://jerryswon.com/common-leadership-mistakes-to-avoid/?utm_source=rss&utm_medium=rss&utm_campaign=common-leadership-mistakes-to-avoid Any organization that wants to succeed must have effective leadership, yet even the most seasoned executives occasionally make typical mistakes that compromise their capacity to lead. Maintaining employee morale, creating a healthy work environment, and accelerating organizational success depends on identifying and avoiding these problems. Here are some common leadership mistakes to avoid: Micromanaging: Micromanaging occurs when a leader excessively monitors or controls the work of their team members, leading to decreased autonomy, morale, and productivity. Instead of empowering their team to make decisions and take ownership of their work, micromanagers create a culture of dependency and stifle creativity. Trust your team members to do their jobs effectively and provide guidance and support when needed, rather than hovering over their shoulders and dictating every detail. Lack of Communication: Effective communication is the cornerstone of successful leadership. Failing to communicate openly and frequently with your team can lead to misunderstandings, confusion, and disengagement. Keep your team informed about organizational goals, expectations, and changes, and encourage open dialogue and feedback. Failure to Delegate: Leaders who need help to delegate effectively often become overwhelmed and burn out quickly. In addition to reducing your workload, assigning duties and responsibilities to your team members encourages them to grow as individuals and take responsibility for their work. Assign work according to your team members’ skills and interests and have faith in their abilities and strengths. Ignoring Feedback: Leaders who dismiss or ignore feedback from their team members miss valuable opportunities for growth and improvement. Whether positive or constructive, feedback provides useful insights into areas for improvement, blind spots, and growth opportunities. Create a culture where feedback is encouraged, welcomed, and acted upon, and be open to receiving feedback from your team members. Favoritism or Bias: Playing favorites or demonstrating bias towards certain team members can erode trust, morale, and team cohesion. Treat all team members fairly, respectfully, and equally, regardless of their seniority, background, or personal relationships. Base your decisions on merit, performance, and objective criteria, and avoid showing favoritism or allowing personal biases to influence your judgment. Avoiding Difficult Conversations: Avoiding difficult conversations or conflict resolution can lead to unresolved issues, resentment, and dysfunction within the team. As a leader, it’s essential to address conflicts, performance issues, or other challenging situations promptly and directly—approach difficult conversations with empathy, sensitivity, and a focus on finding solutions rather than placing blame. Lack of Vision and Direction: Leaders who must articulate a clear vision and direction for their team leave their members feeling lost, unmotivated, and disengaged. Define a compelling vision and set ambitious but achievable goals that inspire and motivate your team. Communicate your vision and expectations clearly and consistently, and involve your team in the goal-setting process to foster buy-in and alignment. Avoiding common leadership mistakes requires self-awareness, humility, and a commitment to continuous improvement. Recognizing and addressing these pitfalls can cultivate a positive work environment, build trust and rapport with your team, and lead effectively toward organizational success. The post Common Leadership Mistakes to Avoid first appeared on Jerry Swon | Financial Consultant |NJ.
0 notes
Text
Choose the Right Manufacturer for Boldenone Undecylenate Equipoise Steroid Powder and Ciallis Powder
In today's competitive pharmaceutical market, choosing the right manufacturer is crucial for ensuring quality, safety, and compliance. Whether you're sourcing boldenone undecylenate Equipoise steroid powder or Ciallis powder, finding a trusted supplier can make a significant difference in product efficacy and reliability. This guide will help you understand how to choose the best manufacturers for these specific compounds, and what to look for to ensure you're making the right decision. We'll dive into industry standards, key qualities to expect, and the unique challenges in manufacturing these products.

Understanding Boldenone Undecylenate and Ciallis Powder
Before diving into the process of selecting a manufacturer, it’s important to understand the nature of these compounds.
Boldenone undecylenate Equipoise steroid powder is commonly used in veterinary medicine, especially in the context of performance enhancement in horses. However, due to its anabolic properties, it has also gained popularity in the bodybuilding world for muscle growth and increased strength. It’s a synthetic derivative of testosterone, designed to promote lean tissue growth without the harsh side effects associated with other steroids.
On the other hand, Ciallis powder is a widely used ingredient in medications for erectile dysfunction. The active ingredient, Tadalafil, works by relaxing blood vessels and increasing blood flow to particular areas of the body, making it a popular choice for improving sexual performance. Given the critical nature of this compound, the quality and consistency of Ciallis powder play a significant role in its effectiveness and safety.
Now, let's discuss how to find a reliable boldenone undecylenate Equipoise steroid powder manufacturer and Ciallis powder manufacturer to ensure you get the best quality products.
Main Criteria for Selecting a Manufacturer
When sourcing these two compounds, certain factors are essential to consider for a successful partnership with the manufacturer.
1. Manufacturing Standards and Certifications
One of the most critical factors to consider when choosing a manufacturer is their adherence to manufacturing standards and certifications. A reputable boldenone undecylenate Equipoise steroid powder manufacturer and Ciallis powder manufacturer should comply with international standards such as Good Manufacturing Practice (GMP) and ISO certifications. These certifications ensure that the manufacturer is following strict guidelines related to quality control, cleanliness, and product consistency. Additionally, having these certifications reflects the company's commitment to delivering high-quality products in a regulated environment.
2. Product Quality and Purity
The potency and purity of the boldenone undecylenate Equipoise steroid powder and Ciallis powder can dramatically impact their efficacy. When looking for a supplier, always verify the product’s purity level. Most manufacturers will provide a Certificate of Analysis (CoA) with detailed information on the chemical composition, ensuring that the product meets industry standards. For pharmaceuticals, any deviation in purity can lead to ineffective results or even harm, so always choose a manufacturer with stringent quality assurance protocols.
3. Research and Development (R&D) Capability
An innovative manufacturer invests in research and development. The ability to innovate is particularly important in the pharmaceutical sector, where formulations can be improved, and production methods optimized. A boldenone undecylenate Equipoise steroid powder manufacturer and Ciallis powder manufacturer with robust R&D capabilities is more likely to offer cutting-edge solutions and ensure long-term reliability. Look for manufacturers that regularly update their production processes and are at the forefront of new technological advancements.
4. Regulatory Compliance and Export Experience
Regulatory compliance is another essential criterion, especially if you’re importing products from international markets. Manufacturers should follow local and international laws regarding the manufacturing and sale of anabolic steroids and erectile dysfunction medications. A reliable Ciallis powder manufacturer and boldenone undecylenate Equipoise steroid powder manufacturer should be familiar with export regulations, making the transaction smoother and ensuring that the product arrives with all necessary legal documentation.
Choosing Between Local and Overseas Manufacturers
The Benefits of Working with Local Manufacturers
Working with a local manufacturer comes with several advantages. First and foremost, you can communicate and collaborate more easily, without the challenges of different time zones, languages, or shipping delays. Additionally, you may have the opportunity to visit the manufacturing facilities and verify the conditions firsthand. For boldenone undecylenate Equipoise steroid powder and Ciallis powder, local manufacturers may also have a better understanding of regional regulations and market needs.
The Benefits of Overseas Manufacturers
However, overseas manufacturers, particularly in regions known for pharmaceutical production like China or India, often offer more competitive pricing. A company like Horster Biotek, which specializes in producing various pharmaceutical powders, is known for adhering to global standards at a lower cost. When choosing an overseas Ciallis powder manufacturer or boldenone undecylenate Equipoise steroid powder manufacturer, make sure to verify their reputation, certifications, and client feedback to ensure you’re getting a good deal without sacrificing quality.
Why Horster Biotek Stands Out
When looking for reliable manufacturers of boldenone undecylenate Equipoise steroid powder and Ciallis powder, Horster Biotek is a name you can trust. As an industry leader, Horster Biotek boasts cutting-edge production facilities, strict quality control measures, and adherence to GMP standards, ensuring that every batch of product meets the highest standards of purity and efficacy. With years of experience in both domestic and international markets, Horster Biotek has earned a reputation for being a reliable supplier, helping customers maintain product quality and consistency.
Subheading: Customer Support and Long-term Relationships
Another key reason to choose Horster Biotek is their commitment to customer support. Whether you’re placing a bulk order or require smaller quantities for specific markets, Horster Biotek provides customized solutions. Building a long-term relationship with a manufacturer ensures stability in your supply chain and helps in negotiating better deals over time. It’s not just about making a one-time purchase but establishing a partnership that benefits both parties.
Choosing the right boldenone undecylenate Equipoise steroid powder manufacturer or Ciallis powder manufacturer can be a game-changer for your business. By focusing on manufacturing standards, product quality, R&D capabilities, and regulatory compliance, you can ensure a successful partnership with a trusted supplier. Horster Biotek stands out as an ideal choice, offering a blend of high-quality products, competitive pricing, and exceptional customer service. In the end, finding the right manufacturer is about building a relationship that ensures consistent supply, compliance with regulations, and, most importantly, high-quality products.
0 notes
Text
Emancipated Minor: Key Steps and Legal Advice from GetLegal

Becoming an emancipated minor is a significant legal step for a young person seeking independence from their parents or guardians. Emancipation grants minors the legal status of an adult, allowing them to make decisions and take responsibility for their own lives. This process, however, is complex and varies depending on your location.
Understanding the key steps and legal implications is crucial for anyone considering this path. In this blog, GetLegal will provide a comprehensive guide on the emancipation process, focusing on key steps, legal advice, and frequently asked questions.
What is Emancipation?
Emancipation is a legal process that grants a minor independence from their parents or guardians before they reach the age of majority. This process grants minors the legal status of an adult, enabling them to make decisions and take on responsibilities typically reserved for adults. Emancipated minors have the authority to manage their finances, enter into contracts, make medical decisions, and assume full legal responsibility for their actions.
The criteria and procedures for emancipation vary by jurisdiction. Still, common requirements often include demonstrating financial self-sufficiency, living independently, and providing valid reasons for seeking independence. The process usually involves:
Filing a petition with the court.
Attending a hearing.
Giving evidence that emancipation is in the minor's best interest.
Once granted, emancipation can have significant implications, including changes in legal obligations and access to certain benefits. It is crucial for minors considering this path to understand the requirements and responsibilities involved thoroughly.
Why Consider Emancipation?
Several reasons may lead a minor to seek emancipation, including:
Complicated Family Dynamics: In cases where the family environment is abusive or dysfunctional.
Financial Independence: When minors are financially self-sufficient and can support themselves.
Educational or Career Opportunities: To pursue educational or career goals that require independence.
Key Steps to Emancipation
1. Understanding Local Laws
Each state or jurisdiction has its laws and procedures for emancipation of minors. It's essential to understand the specific requirements in your area. For instance:
California: Minors must be at least 14 years old and able to demonstrate financial independence.
New York: The process involves a court petition and requires the minor to prove they can support themselves.
2. Meet Eligibility Requirements
To qualify for emancipation, a minor must generally meet several criteria:
Age: Most jurisdictions require the minor to be at least 14.
Financial Independence: The minor must prove they can support themselves financially.
Ability to Live Independently: Demonstrating the ability to live independently and make responsible decisions is crucial.
3. Prepare the Necessary Documentation
The emancipation process requires various documents, including:
Petition for Emancipation: A formal request submitted to the court.
Proof of Income: Documentation showing the minor's financial stability.
Personal Statements: A statement outlining why emancipation is in the minor's best interest.
4. Filing a Petition
The petition must be submitted to the appropriate court. The process typically includes:
Completing Forms: Filling out necessary legal forms.
Submitting Evidence: Providing evidence of financial independence and maturity.
Court Hearing: Attending a court hearing where a judge will review the petition.
5. Attend the Court Hearing
The minor must present their case to a judge during the court hearing. Key aspects include:
Demonstrating Maturity: Showing the court that they can handle adult responsibilities.
Explaining Reasons: Clearly explain the reasons for seeking emancipation.
6. Await the Court's Decision
After the hearing, the court will decide based on the evidence and testimony presented. If granted, the minor will receive a formal emancipation decree.
7. Follow Up on Legal Obligations
Post-emancipation, the minor must comply with all legal obligations, including:
Financial Responsibilities: Managing personal finances and living expenses.
Legal Contracts: Being able to enter into contracts and make legal decisions independently.
Unique Insights on Emancipation
Varied State Requirements: Emancipation requirements vary significantly between states, so it's important to research local laws thoroughly.
Impact on Social Services: Emancipated minors may lose access to certain social services and benefits, making financial planning essential.
Legal Advice: Consulting with a legal professional can provide guidance tailored to your specific situation and help navigate the complexities of the emancipation process.
FAQs
What is an Emancipated Minor?
An emancipated minor is a person under 18 legally granted independence from their parents or guardians. They are treated as adults for most legal purposes.
How Do I Apply for Emancipation?
To apply for emancipation, you must typically file a petition with the court, provide evidence of financial independence, and attend a court hearing.
What Are the Benefits of Being Emancipated?
Emancipation allows minors to make independent decisions, enter into legal contracts, and assume responsibility for their own lives without parental consent.
Are There Risks to Emancipation?
Yes, risks include financial instability and lack of parental support. It is crucial to be prepared for the responsibilities that come with independence.
Can an Emancipated Minor Still Receive Child Support?
Typically, once emancipated, minors no longer receive child support from their parents. However, the particular circumstances may differ by jurisdiction.
How Does Emancipation Affect Education?
Emancipated minors can make their own educational decisions, including enrolling in school or pursuing other educational opportunities.
Conclusion
Emancipation is a significant step that grants a minor legal independence, but it requires careful consideration and preparation. By understanding the local laws, meeting eligibility requirements, and following the proper procedures, a minor can successfully navigate the path to emancipation. Always consult a legal professional to ensure you fully understand the implications and responsibilities involved.
For more detailed guidance and personalized legal advice on emancipation, contact GetLegal. Our experts are here to help you through every step of the process and ensure that your transition to independence is as smooth as possible.
If you're considering emancipation or need help navigating the legal process, GetLegal is here to assist. Contact us today to schedule a consultation and get the expert advice you need to make informed decisions about your future.
1 note
·
View note
Text
https://www.cosmeticdermatologistindia.com/dermatology-solutions/psoriasis-treatment/
Psoriasis, a chronic autoimmune condition affecting millions globally, manifests in various forms, causing discomfort and affecting one’s quality of life. In bustling Mumbai, where healthcare options abound, finding the right treatment for psoriasis can be a daunting task. To assist those seeking relief from this condition, we delve into the top treatment centers in Mumbai known for their expertise and advanced therapeutic approaches.
Understanding Psoriasis
Psoriasis presents as red, scaly patches on the skin, often accompanied by itching and discomfort. While its exact cause remains elusive, genetics and immune system dysfunction play significant roles. The condition not only impacts the skin but can also affect nails, joints, and overall well-being.
Criteria for Selecting the Best Treatment Centers
When considering psoriasis treatment centers in Mumbai, several factors are pivotal:
1. Expertise of Dermatologists: Specialized knowledge in treating psoriasis is essential. Look for centers with experienced dermatologists who stay updated on the latest treatments. 2. Range of Treatments Available: Effective treatment plans often combine various therapies. Centers offering phototherapy (UVB/UVA), systemic medications, biologics, and newer modalities like laser therapy provide comprehensive care.
3. Patient-Centric Approach: Each patient’s condition differs. Opt for centers that tailor treatment plans to individual needs, considering factors such as severity, affected areas, and previous treatment history.
4. Technology and Infrastructure: Advanced equipment and facilities enhance treatment outcomes. Centers equipped with state-of-the-art technology for accurate diagnosis and treatment monitoring are preferable.
5. Patient Reviews and Testimonials: Insights from previous patients can provide valuable feedback on the center’s efficacy, patient care, and overall experience.
Conclusion
Finding the best psoriasis treatment in Mumbai involves considering various factors such as expertise, range of treatments, patient-centric care, technology, and patient feedback. Each of the aforementioned centers excels in different aspects, catering to diverse patient needs. Mumbai offers a spectrum of choices for individuals battling psoriasis.
When embarking on the journey to manage psoriasis, thorough research and consultation with specialists are essential. By choosing a reputable treatment center that aligns with individual preferences and medical requirements, individuals can take significant strides towards managing their condition effectively and enhancing their quality of life.
1 note
·
View note
Text
Understanding the Impact of Environmental Pollutants: PFOS and Chronic Kidney Disease, Secondhand Smoke and Hypertension

PFOA and Chronic kidney disease
The significant finding regarding serum levels of perfluorooctane sulfonate (PFOS) and its association with an increased risk of chronic kidney disease (CKD) within the general US population is both alarming and indicative of broader environmental health concerns. This revelation, as outlined in a study by Dr. Anoop Shankar and team, underscores the intricate interplay between environmental pollutants and human health.
PFOS, a chemical compound, has long been scrutinized for its persistence, bio accumulative properties, and toxicity across various mammalian species. A 2002 study by the Environmental Directorate of the OECD highlighted these concerns, emphasizing the need for rigorous assessment and regulation of such substances.
What makes this finding particularly concerning is its implication for human health. The association between elevated serum PFOS levels and an increased risk of CKD underscores the potential systemic impact of environmental pollutants. Importantly, the study notes that this association persists even after adjusting for several confounding factors, including age, sex, race/ethnicity, body mass index, diabetes, hypertension, and serum cholesterol level. Such robust findings lend credence to the notion that PFOS may indeed pose a significant risk to renal health within the general population.
Moreover, this research underscores the interdisciplinary nature of environmental health. Collaboration between scientists, clinicians, policymakers, and advocacy groups is essential in mitigating the adverse effects of pollutants like PFOS on human health. By fostering dialogue and implementing evidence-based interventions, we can strive towards a healthier, more sustainable future for all.
Second Hand Smoke and Hypertension
Secondhand smoke exposure has been consistently linked to an increased risk of hypertension. Even brief exposure to secondhand smoke can lead to immediate adverse effects on cardiovascular health, including elevated blood pressure. Chronic exposure to secondhand smoke is associated with long-term consequences, including the development and exacerbation of hypertension.
Studies have shown that the chemicals present in secondhand smoke can disrupt normal vascular function, leading to endothelial dysfunction and arterial stiffness. A study conducted by Dr. Omayma Alshaarawy, Jie Xiao, and Dr. Anoop Shankar investigates the association between serum cotinine levels, a biomarker of secondhand smoke exposure, and hypertension among never smokers.
The study analyzed data from the National Health and Nutrition Examination Survey (NHANES) conducted between 2005 and 2008, involving 2,889 never smokers. Serum cotinine levels were used as a measure of secondhand smoke exposure, while hypertension status was determined based on clinical criteria. The results revealed a positive association between higher serum cotinine levels and hypertension among never smokers.These effects contribute to the development of hypertension over time. Additionally, the inflammatory and oxidative stress responses triggered by exposure to secondhand smoke further exacerbate cardiovascular risk.
Public health efforts to reduce secondhand smoke exposure, such as smoke-free legislation and smoking cessation programs, have proven effective in lowering hypertension rates and improving overall cardiovascular health. By raising awareness about the dangers of secondhand smoke and implementing policies to limit exposure, we can mitigate the adverse health effects associated with this pervasive environmental pollutant.
0 notes
Text
Cosmetic Surgery Vs Plastic Surgery. Know the Difference!
Cosmetic surgery and plastic surgery are two terms often used interchangeably, which can lead to confusion among people. While they both involve surgical procedures aimed at enhancing one's appearance, there is a significant difference between the two. In this article, we will dive into the details of cosmetic surgery and plastic surgery and highlight their differences.
What is Cosmetic Surgery?
Cosmetic surgery, also known as aesthetic surgery, focuses on improving the physical appearance of an individual. It involves altering or reshaping a part of the body to enhance its aesthetic appeal. Common procedures in cosmetic surgery include facelifts, breast augmentation, liposuction, and rhinoplasty.
Cosmetic surgery is typically elective and chosen by individuals who are not satisfied with their physical appearance and want to make improvements for personal reasons. These procedures are not medically necessary and are often performed solely for aesthetic purposes.
What is Plastic Surgery?
Plastic surgery, also known as reconstructive surgery, is a broad field that involves restoring or correcting defects in the body caused by birth abnormalities, trauma, disease, or aging. It focuses on repairing and reconstructing damaged or dysfunctional body parts to improve their function and appearance.
Some common procedures in plastic surgery include breast reconstruction, cleft lip and palate repair, hand surgery, and scar revision. Plastic surgery is often necessary to improve a person's quality of life, functionality, and self-esteem.
The Key Differences
The main difference between cosmetic surgery and plastic surgery lies in their goals and motivations. Cosmetic surgery focuses on enhancing one's appearance, whereas plastic surgery aims to correct or restore body function and appearance.
Another key difference between the two is their eligibility criteria. Cosmetic surgery is typically performed on healthy individuals who want to make aesthetic improvements, while plastic surgery can also be performed on people with medical conditions or physical abnormalities.
Similarities between Cosmetic Surgery and Plastic Surgery
Although there are significant differences between cosmetic and plastic surgery, they do have similarities. Both types of surgeries involve altering the body through surgical procedures and may use similar techniques and tools.
Additionally, both types of surgery require a highly skilled and experienced surgeon to achieve optimal results. They also carry potential risks and complications that should be carefully considered before undergoing any procedure.
Choosing the Right Procedure
Deciding between cosmetic surgery or plastic surgery can be challenging. It is essential to understand the differences between the two and consult with a qualified surgeon to determine which procedure is best for your needs.
If you are seeking to improve your appearance, cosmetic surgery may be the right choice. However, if you have a medical condition or physical abnormality that affects your function and quality of life, plastic surgery may be necessary.
Conclusion
In conclusion, both cosmetic surgery and plastic surgery have their unique purposes, benefits, and risks. Whether you're considering cosmetic surgery in Toronto to enhance your appearance, or you're exploring Toronto plastic surgery options to rectify a medical condition, it's important to make an informed decision. Consulting with experienced, reputable surgeons can help guide your decision and ensure that you choose the procedure that best aligns with your individual needs and expectations. Remember, the goal is not just to change how you look, but to enhance your overall quality of life.
Consider cosmetic surgery Toronto professionals for a transformative journey. Trust Toronto plastic surgery experts for top-notch, life-enhancing results. Contact us today!
0 notes
Text
Analyzing the Epidemiology of Painful Diabetic Neuropathy
Painful Diabetic Neuropathy (PDN) is a debilitating complication of diabetes characterized by chronic pain, tingling, and numbness in the extremities. Painful Diabetic Neuropathy Epidemiology Analysis It significantly impacts the quality of life of affected individuals and represents a substantial burden on healthcare systems worldwide. In this analysis, we delve into the epidemiology of PDN, examining prevalence rates, risk factors, regional variations, and implications for public health.
Prevalence of Painful Diabetic Neuropathy
The prevalence of PDN varies widely depending on population characteristics, diagnostic criteria, and study methodologies. However, epidemiological studies consistently indicate that a significant proportion of individuals with diabetes experience neuropathic pain. Estimates suggest that approximately 20% to 50% of patients with diabetes may develop PDN during the course of their disease, with prevalence rates increasing with disease duration and severity.
Risk Factors and Contributing Factors
Several factors contribute to the development and progression of PDN, including:
Duration and Control of Diabetes: Long-standing diabetes and poor glycemic control are major risk factors for PDN. Chronic hyperglycemia contributes to nerve damage and dysfunction, leading to the development of neuropathic symptoms over time.
Age and Disease Duration: Older age and longer duration of diabetes are associated with an increased risk of developing PDN. Aging-related changes in nerve structure and function, coupled with prolonged exposure to metabolic abnormalities, contribute to the pathogenesis of neuropathic pain.
Metabolic Factors: Obesity, dyslipidemia, hypertension, and other metabolic comorbidities commonly associated with diabetes may exacerbate neuropathic symptoms and contribute to the progression of PDN.
Genetic Predisposition: Genetic factors play a role in the susceptibility to PDN, with certain genetic polymorphisms implicated in the pathogenesis of diabetic neuropathy and pain perception.
Regional Variations and Healthcare Disparities
The epidemiology of PDN exhibits regional variations influenced by factors such as population demographics, healthcare infrastructure, access to diabetes care, and cultural practices. Developed countries with aging populations and high prevalence of diabetes tend to have higher rates of PDN, while low- and middle-income countries may face challenges in diagnosis, management, and access to neuropathic pain treatments.
Healthcare disparities also exist within regions and populations, with underserved communities, racial/ethnic minorities, and individuals with lower socioeconomic status experiencing disproportionate burden of PDN. Barriers to healthcare access, inadequate screening and diagnostic resources, and limited availability of specialized neuropathy care contribute to disparities in PDN prevalence, management, and outcomes.
Public Health Implications and Healthcare Strategies
The growing burden of PDN underscores the importance of comprehensive diabetes care, early detection of neuropathic symptoms, and multidisciplinary management approaches. Public health initiatives aimed at diabetes prevention, education, and access to quality healthcare services are essential for reducing the incidence and impact of PDN on individuals and communities.
Healthcare strategies for PDN management include:
Multimodal Pain Management: Pharmacological interventions, such as anticonvulsants, antidepressants, opioids, and topical agents, are commonly used to manage neuropathic pain in PDN. However, a multimodal approach that integrates pharmacotherapy with non-pharmacological interventions, such as physical therapy, cognitive-behavioral therapy, and lifestyle modifications, is recommended for optimal pain control and functional improvement.
Patient Education and Self-management: Empowering patients with knowledge about diabetes self-care, neuropathy prevention, and pain management strategies is crucial for enhancing treatment adherence, self-efficacy, and quality of life. Educational interventions that emphasize lifestyle modifications, glucose monitoring, foot care, and early symptom recognition can help individuals with PDN better cope with their condition and reduce the risk of complications.
Healthcare Provider Training and Guidelines: Training healthcare providers in the diagnosis and management of PDN is essential for improving clinical outcomes and quality of care. Evidence-based guidelines and treatment algorithms for PDN can help standardize practices, promote adherence to best practices, and optimize resource allocation in healthcare settings.
Research and Innovation: Continued research into the pathophysiology of PDN, biomarkers for early detection, and novel therapeutic targets is needed to advance our understanding of the disease and develop more effective treatments. Collaborative efforts between academia, industry, and government agencies are essential for driving innovation and translating scientific discoveries into clinical practice.
Conclusion
Painful Diabetic Neuropathy represents a significant public health challenge with implications for individuals, healthcare systems, and society at large. By understanding the epidemiology of PDN, addressing risk factors, reducing healthcare disparities, and implementing evidence-based interventions, we can improve the prevention, diagnosis, and management of PDN and enhance the quality of life for individuals living with this debilitating condition.
To gain more information on the PDN market forecast,��download a free report sample
0 notes
Text
Exploring the Interplay Between Diseases and Liver Transplant
Understanding the Complexities and Implications
Liver transplant surgery is a life-saving procedure that offers hope to patients with end-stage liver disease and certain liver-related conditions. However, the decision to undergo a liver transplant is often influenced by the underlying disease or condition that necessitates the procedure. In this article, we delve into the intricate connection between diseases and liver transplants, exploring the complexities, implications, and considerations involved.

Liver Diseases Leading to Transplant: Liver transplant is commonly indicated for patients with end-stage liver disease (ESLD), a condition characterized by irreversible liver damage and loss of function. Chronic liver diseases such as cirrhosis, hepatitis B and C, alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), and autoimmune hepatitis are among the primary causes of ESLD. These diseases progress over time, leading to liver failure and ultimately necessitating a transplant to restore liver function and prolong survival.
Hepatobiliary Cancers: Hepatocellular carcinoma (HCC), the most common type of liver cancer, often develops in the setting of chronic liver disease or cirrhosis. In cases where the cancer is confined to the liver and has not spread beyond, liver transplant may be considered as a curative treatment option. However, stringent criteria and careful patient selection are essential to ensure favorable outcomes and prevent cancer recurrence post-transplant.
Metabolic Liver Diseases: Inherited metabolic disorders such as Wilson's disease, hemochromatosis, and alpha-1 antitrypsin deficiency can affect liver function and lead to progressive liver damage. For patients with severe and unmanageable symptoms, liver transplant may offer a chance for improved quality of life and long-term survival. However, the presence of underlying metabolic abnormalities may pose challenges during the transplant process and require specialized pre-transplant evaluation and management.
Acute Liver Failure: Acute liver failure (ALF) is a rare but life-threatening condition characterized by rapid onset of liver dysfunction and hepatic encephalopathy. Causes of ALF include viral hepatitis, drug-induced liver injury, autoimmune hepatitis, and acute fatty liver of pregnancy, among others. Liver transplant may be considered for select patients with ALF who fail to respond to medical therapy or develop complications such as hepatic coma. Timely referral and evaluation are crucial in optimizing outcomes for these patients.
Autoimmune Liver Diseases: Autoimmune liver diseases, including autoimmune hepatitis, primary biliary cholangitis (formerly known as primary biliary cirrhosis), and primary sclerosing cholangitis, are characterized by immune-mediated damage to the liver and biliary tract. While medical therapy is the mainstay of treatment for most patients, those with advanced disease and progressive liver failure may require liver transplant as a definitive treatment option. Careful management of post-transplant immunosuppression is essential to prevent disease recurrence and graft rejection.
Challenges and Considerations: Despite the potential benefits, liver transplant poses inherent challenges and considerations, particularly in the context of underlying diseases. Patient selection, pre-transplant evaluation, and post-transplant management require a multidisciplinary approach involving hepatologists, transplant surgeons, oncologists, and other specialists. Additionally, the shortage of donor organs, immunosuppression-related complications, and the risk of disease recurrence post-transplant are important factors to consider when weighing the risks and benefits of liver transplant in patients with underlying diseases.
The interplay between diseases and liver transplant is multifaceted and complex, with diverse implications for patient management and outcomes. While liver disease treatment in Bangalore, offers a lifeline to patients with end-stage liver disease, hepatobiliary cancers, metabolic disorders, acute liver failure, and autoimmune liver diseases, careful consideration of the underlying disease, patient characteristics, and transplant-related factors is essential in optimizing outcomes and ensuring long-term success. Through continued research, innovation, and collaboration, clinicians and researchers strive to advance our understanding of this intricate connection and improve the care and outcomes of patients undergoing liver transplant for various diseases.
Let’s know what are approaches taken to Liver transplant
Deceased Donor Liver Transplantation (DDLT) and Living Donor Liver Transplantation (LDLT) are two approaches to liver transplantation, each with its own distinct characteristics and considerations.

Donor Source:
Deceased Donor Liver Transplantation: Deceased Donor Liver Transplantation in Bangalore, the liver is procured from a deceased donor who has been declared brain-dead and has consented to organ donation either during their lifetime or by their family after death.
Living Donor Liver Transplantation: In Living Donor Liver Transplantation, the liver is donated by a living donor, typically a family member or close relative of the recipient. The donor undergoes a thorough evaluation process to assess their suitability for donation, including medical, psychological, and ethical considerations.
Timing of Transplantation:
Deceased Donor Liver Transplantation: The timing of Deceased Donor Liver Transplantation depends on the availability of deceased donor organs, which can vary depending on factors such as organ donation rates, waitlist prioritization, and organ allocation policies.
Living Donor Liver Transplantation: Living Donor Liver Transplantation offers the advantage of scheduling the transplant at a time that is convenient for both the recipient and the donor, minimizing the risk of disease progression and optimizing outcomes for both parties.
Graft Size and Compatibility:
Deceased Donor Liver Transplantation: The size and compatibility of the deceased donor liver may not always match the recipient's requirements, leading to potential mismatches in size or blood type. This can sometimes result in a longer wait time on the transplant waitlist or the need for additional surgical techniques to adapt the donor liver to the recipient's anatomy.
Living Donor Liver Transplantation: Living Donor Liver Transplantation allows for a more tailored approach to graft selection, as the donor liver can be selected based on size, blood type compatibility, and other factors specific to the recipient's needs. This often results in a better match and reduces the risk of graft rejection or complications post-transplant.
Waiting Time and Urgency:
Deceased Donor Liver Transplantation: Due to the limited availability of deceased donor organs, patients awaiting Deceased Donor Liver Transplantation may experience longer wait times on the transplant waitlist, particularly for those with less severe illness or lower priority status.
Living Donor Liver Transplantation: Living Donor Liver Transplantation offers the advantage of shorter waiting times, as the transplant can be scheduled based on the recipient's clinical status and urgency of need. This can be particularly beneficial for patients with rapidly progressive liver disease or acute liver failure who may not have the luxury of waiting for a deceased donor organ.
Risk to Donor:
Deceased Donor Liver Transplantation: There is no risk to the donor in Deceased Donor Liver Transplantation, as the liver is procured from a deceased donor who has already passed away.
Living Donor Liver Transplantation: Living Donor Liver Transplantation carries inherent risks to the living donor, including potential complications related to the surgical procedure, anesthesia, and recovery process. However, advances in surgical techniques and donor selection criteria have significantly reduced the risk of complications for living donors in recent years.
while both Deceased Donor Liver Transplantation and Living Donor Liver Transplantation in Bangalore, offer life-saving options for patients with end-stage liver disease, each approach has its own unique characteristics, considerations, and advantages. The choice between Deceased Donor Liver Transplantation and Living Donor Liver Transplantation depends on various factors, including the recipient's clinical status, urgency of need, compatibility, and availability of suitable donor organs. Ultimately, the goal of liver transplantation is to provide the best possible outcome for the recipient while ensuring the safety and well-being of the donor.
For details get the specialists for the Best Liver Transplant Center in Bangalore
#fatty liver treatment in Bangalore#Liver inflammation treatment in Bangalore#Liver disease treatment in Bangalore#Liver transplantation surgery in Bangalore#Deceased Donor Liver Transplantation in Bangalore#Living Donor Liver Transplantation in Bangalore#best liver transplant center in Bangalore#fatty liver#liver treatment center#liver treatment#fastrecoveryoffattyliver#liver care center Bangalore
0 notes