#Disease prevention and quality healthcare access
Explore tagged Tumblr posts
Text
Unleashing the Power of Goal 3: Good Health and Well-being for a Thriving World

In our quest for a better world, one of the most fundamental goals we must strive for is Goal 3: Good Health and Well-being. Recognized as a crucial part of the United Nations Sustainable Development Goals (SDGs), Goal 3 aims to ensure healthy lives and promote well-being for all at all ages. This ambitious goal encompasses a wide range of factors, including disease prevention, access to healthcare, mental health, and the promotion of healthy lifestyles. By addressing the challenges and opportunities presented by Goal 3, we have the potential to transform societies, empower individuals, and create a healthier and more prosperous world.
The Importance of Good Health and Well-being
Good health and well-being serve as the foundation for individuals, communities, and nations to thrive and prosper. When individuals enjoy good health, they are more equipped to actively participate in their communities, pursue education, and engage in productive work. Healthy individuals have the energy, physical strength, and mental resilience to contribute meaningfully to society. They can be more productive, innovative, and creative, leading to overall progress and development.
Conversely, poor health poses significant challenges to individuals and society as a whole. When individuals suffer from ill health, their ability to contribute to their communities becomes constrained. Limited physical capabilities, chronic illnesses, and mental health issues can hinder their participation in various aspects of life, including education, employment, and social activities. This not only diminishes their own potential but also limits the overall productivity and growth of communities and nations.
Moreover, the impact of poor health extends beyond individual well-being and has broader socio-economic implications. Inadequate health systems, prevalence of diseases, and lack of access to healthcare services can hamper economic growth and exacerbate existing inequalities. When a significant portion of the population is burdened by illness, it leads to increased healthcare costs, reduced workforce productivity, and higher rates of absenteeism. The consequences of poor health ripple through society, hindering progress and perpetuating cycles of poverty and inequality.
Recognizing the significance of good health and well-being, Goal 3 of the United Nations Sustainable Development Goals (SDGs) places a strong emphasis on ensuring healthy lives and promoting well-being for all at all ages. It acknowledges that achieving good health is not only a moral imperative but also a strategic investment in human capital and sustainable development.
By investing in healthcare infrastructure, disease prevention, and health promotion initiatives, nations can lay the groundwork for a healthy and productive population. Accessible and affordable healthcare services, including preventive care, vaccinations, and treatment options, play a crucial role in reducing the burden of diseases and improving overall health outcomes. Strengthening health systems and ensuring universal healthcare coverage is not only a matter of justice but also a smart investment in the well-being and economic stability of a nation.
Promoting good health and well-being is not limited to physical health alone. Mental health, often overlooked or stigmatized, is an integral component of overall well-being. Mental health issues, such as depression, anxiety, and stress, can significantly impact an individual's quality of life and ability to function effectively. By prioritizing mental health, providing access to mental health services, and fostering supportive environments, societies can create conditions that enable individuals to thrive holistically.
Furthermore, achieving Goal 3 requires addressing the root causes of health disparities and inequalities. Socioeconomic factors, including income inequality, education, and social determinants of health, can significantly influence an individual's health status. Vulnerable populations, such as women, children, older adults, and marginalized communities, are often disproportionately affected by health inequities. To achieve good health and well-being for all, it is essential to implement policies and programs that specifically target these groups and reduce disparities.
Technology and innovation also play a vital role in advancing Goal 3. The integration of digital health solutions, telemedicine, wearable devices, and data analytics can enhance healthcare delivery, improve access to services, and facilitate preventive care. These advancements have the potential to bridge geographical barriers, reach remote populations, and empower individuals to take control of their health. By harnessing the power of technology and encouraging further innovation, we can overcome challenges in healthcare delivery and maximize the potential for good health and well-being worldwide.
Good health and well-being are not only essential for individuals to flourish but also for communities and nations to thrive. By prioritizing Goal 3 and investing in disease prevention, access to healthcare, mental health support, healthy lifestyles, and addressing inequalities, we can create a society where everyone has the opportunity to lead a healthy and fulfilling life. Achieving good health and well-being is not just a moral obligation; it is a strategic investment in human capital and sustainable development that will pave the way for a brighter and more prosperous future.
Disease Prevention and Universal Healthcare
At the heart of Goal 3: Good Health and Well-being lies the fundamental objective of disease prevention and ensuring access to quality healthcare for all individuals, regardless of their socio-economic background. This objective encompasses a range of strategies and initiatives aimed at reducing the burden of diseases, improving health outcomes, and promoting overall well-being.
Effective disease prevention is a cornerstone of achieving good health. Immunization programs have proven to be one of the most successful public health interventions, preventing millions of deaths each year from vaccine-preventable diseases. Through vaccination campaigns, individuals are protected from diseases such as measles, polio, hepatitis, and influenza. Immunization not only safeguards individual health but also contributes to herd immunity, reducing the overall transmission and impact of infectious diseases within communities.
Furthermore, clean water and sanitation initiatives play a crucial role in disease prevention. Access to safe drinking water and proper sanitation facilities is essential for preventing waterborne diseases, such as cholera, typhoid, and diarrhea. Improved sanitation practices, including the provision of adequate toilets and waste management systems, help minimize the spread of pathogens and promote better hygiene practices.
In addition to disease prevention measures, health education campaigns are essential for promoting awareness and empowering individuals to make informed decisions about their health. These campaigns provide valuable information about disease prevention, early detection, and healthy lifestyles. By educating communities about the importance of hygiene, nutrition, sexual and reproductive health, and other health-related topics, individuals can take proactive steps to protect themselves and their families from diseases.
Universal healthcare coverage is a crucial aspect of Goal 3, ensuring that everyone has access to essential healthcare services without facing financial hardships. It means that individuals should be able to access healthcare when needed, without fear of incurring catastrophic expenses that could push them into poverty. Universal healthcare coverage encompasses a broad range of services, including preventive care, primary healthcare, emergency care, essential medications, and specialized treatments.
Achieving universal healthcare coverage requires a comprehensive approach that addresses both financial and non-financial barriers to accessing healthcare. Governments and policymakers must work towards developing robust healthcare systems that are accessible, equitable, and efficient. This involves establishing healthcare facilities, training healthcare professionals, ensuring the availability of essential medicines and technologies, and implementing health financing mechanisms that protect individuals from financial hardships.
The importance of disease prevention and access to quality healthcare for all cannot be overstated. Timely access to healthcare services enables early detection and treatment of diseases, reducing the burden on individuals and society. It also promotes preventive care, which focuses on addressing risk factors and promoting healthy behaviors to prevent the onset of diseases.
Moreover, universal healthcare coverage contributes to reducing health inequalities. It ensures that individuals from all socio-economic backgrounds, including marginalized populations, have equal opportunities to access healthcare services. By addressing disparities in healthcare access, we can work towards creating a fairer and more just society, where everyone has the chance to live a healthy and fulfilling life.
Disease prevention strategies, clean water and sanitation initiatives, and health education campaigns are crucial components of achieving Goal 3. These measures help reduce the burden of communicable diseases and improve overall health outcomes. Additionally, ensuring universal healthcare coverage is vital to guarantee that everyone has access to essential healthcare services without facing financial hardships. By prioritizing disease prevention and working towards universal healthcare coverage, we can lay the foundation for a healthier and more equitable society, where good health and well-being are attainable for all.
Mental Health and Well-being
While the focus on physical health is essential, it is crucial to recognize that mental health and well-being are equally significant components of Goal 3: Good Health and Well-being. Mental health issues affect millions of people worldwide, cutting across age, gender, and socioeconomic boundaries. However, these issues often go unnoticed, undiagnosed, or stigmatized, resulting in individuals suffering in silence and without appropriate support.
Promoting mental well-being requires a multifaceted approach that addresses both the societal and individual aspects of mental health. Firstly, it is vital to destigmatize mental health conditions and raise awareness about the prevalence and impact of mental illnesses. Challenging misconceptions and educating the public can help dismantle the barriers that prevent individuals from seeking help and support.
Integrating mental health into healthcare systems is another crucial step in promoting well-being. Mental health services should be accessible, affordable, and integrated into primary healthcare settings. This integration allows for early identification, intervention, and treatment of mental health conditions, ensuring that individuals receive the support they need in a timely manner.
Mental health promotion should extend beyond healthcare settings and encompass various sectors of society. Schools, workplaces, and community organizations play a significant role in fostering mental well-being. Implementing mental health programs in schools that focus on emotional literacy, stress management, and resilience building can equip young people with the tools they need to navigate the challenges of life.
In the workplace, creating a supportive environment that values employee well-being can significantly impact mental health outcomes. Encouraging work-life balance, providing mental health resources, and promoting open dialogue about mental health can help reduce stress and improve overall employee well-being.
Community organizations and grassroots initiatives also play a vital role in promoting mental health. Support groups, helplines, and community-based mental health services can provide individuals with a safe space to seek support and share their experiences. These initiatives foster a sense of belonging, reduce isolation, and promote social connections, which are crucial protective factors for mental health.
Investing in research and evidence-based practices is essential to inform mental health policies and interventions. By prioritizing research, policymakers can make informed decisions, allocate resources effectively, and develop targeted interventions that address the specific needs of diverse populations.
Furthermore, addressing the social determinants of mental health is integral to promoting mental well-being. Factors such as poverty, inequality, discrimination, and violence can significantly impact an individual's mental health. By addressing these social determinants, societies can create the conditions that support mental well-being for all.
Prevention is a key aspect of promoting mental health. By focusing on early intervention and prevention strategies, societies can reduce the incidence and severity of mental health conditions. This includes promoting healthy coping mechanisms, resilience-building programs, and providing support for individuals who may be at higher risk, such as survivors of trauma or individuals experiencing significant life transitions.
Creating a more compassionate and supportive society requires collaboration and the involvement of various stakeholders. Governments, healthcare systems, educational institutions, employers, communities, and individuals all have a role to play in promoting mental health and well-being. By working together, we can create an environment that fosters understanding, empathy, and support for individuals facing mental health challenges.
In conclusion, while physical health is essential, mental health and well-being must be equally prioritized in achieving Goal 3. Promoting mental well-being requires destigmatization, increased awareness, and the provision of accessible mental health services. By recognizing the importance of mental health and integrating it into healthcare systems, educational settings, workplaces, and communities, we can create a more compassionate and supportive society where individuals can thrive and achieve overall well-being.
Promoting Healthy Lifestyles
Promoting healthy lifestyles is a proactive and preventive approach to achieving Goal 3: Good Health and Well-being. Encouraging individuals to adopt healthy habits, such as engaging in regular physical activity, maintaining balanced diets, and avoiding harmful substances, can have a profound impact on their overall well-being and contribute to the prevention of various health conditions.
Regular physical activity is crucial for maintaining good health and preventing chronic diseases. Engaging in physical activities such as walking, jogging, cycling, or participating in sports not only improves cardiovascular fitness but also strengthens muscles and bones, enhances mental well-being, and reduces the risk of conditions like obesity, diabetes, and heart disease. Governments, educational institutions, and communities should collaborate to provide accessible recreational spaces, sports facilities, and promote physical education programs to encourage individuals of all ages to engage in regular exercise.
Balanced diets are essential for providing the body with the necessary nutrients for optimal functioning. Encouraging individuals to consume a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can promote overall health and prevent nutritional deficiencies. Governments can implement policies that support the availability and affordability of nutritious food options, while educational institutions can incorporate nutrition education into curricula to empower individuals with the knowledge and skills to make informed dietary choices.
Avoiding harmful substances, such as tobacco, excessive alcohol consumption, and illicit drugs, is crucial for maintaining good health and preventing a range of health problems. Governments play a significant role in implementing and enforcing policies and regulations to control the availability and marketing of harmful substances. Educational institutions and community organizations can provide education and awareness campaigns to highlight the detrimental effects of these substances and promote healthy lifestyle choices.
Collaboration between various stakeholders is essential to promoting healthy lifestyles effectively. Governments can enact policies that create supportive environments for healthy choices, such as implementing taxes on unhealthy products, restricting advertising of unhealthy foods to children, and creating smoke-free public spaces. Educational institutions can integrate health education into curricula, teaching students about the importance of physical activity, nutrition, and the risks associated with substance abuse. Communities can establish initiatives that provide access to nutritious food options, create safe spaces for physical activity, and organize community events that promote healthy lifestyles.
Furthermore, utilizing technology and digital platforms can be effective in promoting healthy lifestyles. Mobile applications, wearable devices, and online platforms can provide individuals with tools and resources to track their physical activity, monitor their diet, and receive personalized recommendations for healthy living. These technological advancements can facilitate behavior change, provide motivation and support, and connect individuals with a community of like-minded individuals striving for healthy lifestyles.
It is crucial to recognize that promoting healthy lifestyles is not just about individual choices but also about addressing the underlying social and environmental factors that influence behavior. Socioeconomic factors, such as income, education, and access to resources, can significantly impact an individual's ability to adopt and maintain healthy habits. Therefore, efforts should be made to reduce health inequalities and create equitable environments that enable and empower individuals from all backgrounds to make healthy choices.
Promoting healthy lifestyles is a proactive approach to achieving Goal 3. Encouraging individuals to engage in regular physical activity, maintain balanced diets, and avoid harmful substances can have a positive impact on their overall well-being and prevent various health conditions. Governments, educational institutions, and communities should collaborate to provide resources, education, and infrastructure that support healthy choices and facilitate behavior change. By fostering environments that promote and support healthy lifestyles, we can create a society where good health and well-being are accessible to all individuals.
Addressing Inequalities and Vulnerable Populations
Achieving Goal 3: Good Health and Well-being for all requires a comprehensive approach that addresses inequalities and reaches out to vulnerable populations. Various factors, including socioeconomic status, gender disparities, and geographic location, can significantly impact individuals' access to healthcare services and their overall health outcomes. In order to create a more equitable society and ensure that no one is left behind, it is crucial to implement policies and programs that prioritize the needs of marginalized groups, including women, children, older adults, and those living in poverty or conflict-affected areas.
Socioeconomic factors play a significant role in determining an individual's access to healthcare. Poverty and income inequality can limit individuals' ability to afford essential healthcare services, medications, and treatments. Lack of access to quality education and employment opportunities can further perpetuate health disparities. To address these issues, governments should implement policies that focus on poverty reduction, promote inclusive economic growth, and provide social safety nets to support vulnerable populations. It is crucial to ensure that healthcare services are affordable, and financial barriers are minimized, allowing individuals from all socioeconomic backgrounds to access the care they need.
Gender disparities also have a profound impact on health outcomes. Women and girls often face unique health challenges and may encounter barriers to accessing healthcare services. This includes limited access to reproductive health services, maternal healthcare, and gender-based violence. Governments and organizations should prioritize gender-responsive healthcare policies that address the specific needs of women and girls, including reproductive health services, access to family planning methods, and support for maternal and child health. Furthermore, efforts should be made to empower women through education, economic opportunities, and gender equality initiatives, as these factors have a direct impact on their health and well-being.
Geographic location is another critical factor that can influence access to healthcare. Individuals living in remote or rural areas often face challenges in accessing healthcare facilities, transportation, and specialized services. This issue is compounded in conflict-affected regions, where infrastructure and healthcare systems may be disrupted. To overcome these barriers, governments should invest in healthcare infrastructure in underserved areas, provide mobile healthcare units or telemedicine services, and implement strategies to attract healthcare professionals to remote regions. Additionally, humanitarian organizations and international efforts should prioritize providing healthcare assistance to populations affected by conflicts and disasters, ensuring that those in crisis situations receive the necessary support.
Addressing health inequalities and reaching out to vulnerable populations requires a multi-sectoral approach. Governments, healthcare systems, non-governmental organizations, and community-based initiatives must collaborate to develop targeted programs that address the specific needs of marginalized groups. This includes raising awareness about health issues, providing culturally sensitive healthcare services, and integrating community health workers who can bridge the gap between healthcare providers and underserved communities.
In addition to addressing immediate healthcare needs, it is essential to focus on long-term preventive strategies. This includes health promotion and disease prevention initiatives that target vulnerable populations. For example, promoting sexual and reproductive health education among adolescent girls can empower them to make informed decisions about their health and well-being. Implementing nutrition programs in schools and communities can address malnutrition and promote healthy eating habits among children. Moreover, focusing on geriatric care and providing specialized healthcare services for older adults can support healthy aging and enhance the quality of life for this population.
Achieving good health and well-being for all requires addressing inequalities and reaching out to vulnerable populations. Socioeconomic factors, gender disparities, and geographic location significantly impact individuals' access to healthcare and health outcomes. By implementing policies and programs that prioritize the needs of marginalized groups, we can work towards creating a more equitable society. It is imperative to address poverty, gender disparities, and geographic barriers to healthcare, while also focusing on preventive strategies and long-term health promotion. Through concerted efforts and collaborative actions, we can strive towards ensuring that everyone, regardless of their background, has the opportunity to lead a healthy and fulfilling life.
Technology and Innovation in Healthcare
Technology and innovation have the potential to transform healthcare and play a pivotal role in achieving Goal 3: Good Health and Well-being. The rapid advancements in technology, such as telemedicine, mobile health applications, electronic health records (EHRs), and artificial intelligence (AI)-based diagnostics, are revolutionizing healthcare delivery, making it more accessible, efficient, and cost-effective. By harnessing the power of these tools and promoting further innovation, we can bridge gaps in healthcare delivery and significantly enhance health outcomes on a global scale.
Telemedicine, or remote healthcare consultations, has emerged as a game-changer in healthcare accessibility. It allows individuals to consult with healthcare professionals from the comfort of their homes, eliminating the need for physical visits to healthcare facilities, especially in remote or underserved areas. Telemedicine facilitates timely access to medical advice, follow-up care, and specialist consultations. Moreover, it can improve healthcare outcomes by enabling early detection and intervention, particularly for chronic conditions that require ongoing monitoring and management.
Mobile health applications, or mHealth apps, have gained popularity as powerful tools for health promotion and disease management. These apps offer a wide range of features, including personalized health tracking, medication reminders, fitness monitoring, and access to educational resources. mHealth apps empower individuals to actively participate in their own healthcare, promoting self-management and preventive behaviors. Additionally, these apps can facilitate remote patient monitoring, allowing healthcare providers to track patients' vital signs and provide timely interventions when necessary.
The adoption of electronic health records (EHRs) has transformed healthcare documentation and data management. EHRs enable the secure storage and exchange of patient information among healthcare providers, improving coordination and continuity of care. They streamline administrative processes, reduce medical errors, and facilitate evidence-based decision-making. EHRs also serve as valuable repositories of health data that can be utilized for research and population health management, leading to better understanding of diseases, treatment outcomes, and public health trends.
Artificial intelligence (AI) and machine learning algorithms have shown great promise in healthcare diagnostics and decision support. AI-powered diagnostic tools can analyze medical images, such as X-rays and MRIs, with remarkable accuracy, aiding in early detection and diagnosis of diseases. AI algorithms can also analyze large datasets to identify patterns, predict outcomes, and personalize treatment plans. These advancements have the potential to revolutionize disease management, improve patient outcomes, and optimize healthcare resource allocation.
Furthermore, wearable devices and remote monitoring technologies are becoming increasingly prevalent in healthcare. These devices, such as smartwatches and fitness trackers, can monitor vital signs, physical activity levels, and sleep patterns. They provide valuable data for individuals to track their health and wellness, while also enabling healthcare providers to remotely monitor patients with chronic conditions, detect abnormalities, and intervene when necessary.
Innovation in healthcare technology is not limited to high-income countries. Low-cost and scalable solutions are being developed to address the unique challenges faced by resource-constrained settings. For example, mobile-based diagnostic tools, point-of-care testing devices, and low-cost telemedicine solutions are being deployed in underserved areas to improve access to healthcare and diagnostics.
However, it is important to acknowledge that technology is not a panacea for all healthcare challenges. It should be seen as a complementary tool that works in synergy with healthcare professionals' expertise and human touch. Ethical considerations, privacy, and data security must also be taken into account to ensure that technological advancements are used responsibly and to the benefit of patients.
To fully leverage the potential of technology and innovation in healthcare, it is essential to foster an ecosystem that encourages collaboration between healthcare providers, technology developers, policymakers, and researchers. Governments should support research and development initiatives, promote regulatory frameworks that facilitate the safe and effective deployment of healthcare technologies, and invest in digital infrastructure to enable widespread adoption.
Technology and innovation have the power to revolutionize healthcare and drive progress towards Goal 3. Advancements such as telemedicine, mobile health applications, EHRs, and AI-based diagnostics are already transforming healthcare delivery and improving access to quality care. By embracing and further promoting these technological tools, we can bridge gaps in healthcare delivery, enhance health outcomes, and bring us closer to achieving universal good health and well-being. It is crucial to foster an ecosystem that supports collaboration, research, and responsible use of technology to ensure equitable access to healthcare for all individuals, regardless of their geographic location or socioeconomic status.
Conclusion
Goal 3: Good Health and Well-being is a critical pillar of sustainable development that demands our attention, collaboration, and innovation. By working towards disease prevention, universal healthcare coverage, mental health support, healthy lifestyles, and addressing inequalities, we can build resilient communities and ensure that everyone has the opportunity to lead a healthy and fulfilling life. Together, let us unleash the power of Goal 3 and create a world where good health and well-being are within reach for all.
#Importance of good health and well-being#Achieving Goal 3: Good Health and Well-being#Disease prevention and quality healthcare access#Promoting mental health and well-being#Healthy lifestyle and well-being#Addressing inequalities in healthcare#Reaching vulnerable populations for Goal 3#Technology and innovation in healthcare#Telemedicine and its impact on healthcare#Mobile health applications for well-being#Role of electronic health records in healthcare#Artificial intelligence in healthcare diagnostics#Promoting preventive healthcare strategies#Bridging gaps in healthcare delivery#Health disparities and their impact on Goal 3#Gender disparities in healthcare access#Geographic barriers and healthcare access#Socioeconomic factors and health outcomes#Innovations for healthcare in resource-constrained settings#Wearable devices and remote monitoring for well-being#Integrating technology in healthcare systems#Ethical considerations in healthcare technology#Role of governments in promoting healthcare innovation#Collaborative efforts for Goal 3 achievement#Empowering women in healthcare access#Promoting healthy habits for overall well-being#Preventive strategies for chronic disease management#Improving healthcare outcomes through innovation#Implications of technology on healthcare privacy and security#Enhancing healthcare accessibility through technology
0 notes
Text
Love in the big city and HIV
So, I have recently watched one of the best dramas of the year, “Love in the big city”, in which HIV is a major theme.
The show portrays really well the stigmatized scenario around HIV: as a person living with the virus, Go Young feels exactly as if he's carrying some kind of curse. He can't accept it, but who can blame him for that, if "Kylie", as he calls the virus, is always around like an inconvenient person? In his sex life, while applying to a job, and even while hanging out with friends.
Society doesn't make it easy for a person living with HIV to accept the condition and that's essential when it comes to healthcare, which is what I want to address today.
First, let me introduce myself: my name is Nico and I'm a Medicine student in Brazil. Here, we have probably one of the biggest public health system in the world, the Unified Health System (a.k.a. SUS). In this essay, I intend to share some general information about HIV, its treatment and prevention, by using some parts of “Love in the big city” to discuss this theme, because although the show did an amazing job when it comes to talking about it, there are some points I found needed some better explanation.
HIV is a sexually transmitted infection (STI) that can also be transmitted by the contact with infected blood (e.g: incompatible blood transfusion; use of shared needles) or from the mother to a child inside the womb or during labor. The virus uses a specific type of immune cell to multiply. Explaining it in a very simple way, he gets inside the cell, uses its components to produce new viral copies and then ruptures the cell membrane to release these new copies in the blood, killing the cell by doing so. For this reason, untreated HIV is very dangerous, since it can cause immunodeficiency (failure of the immune system), making the person susceptible to acquire opportunistic infections, which are diseases that usually don’t occur in people with regular immune systems. When someone has immunodeficiency caused by HIV, this person is diagnosed with Acquired ImmunoDeficiency Syndrome (AIDS). That being said, AIDS and HIV are not the same. There are many people living with HIV that don’t have AIDS, thanks to appropriate treatment.
There are multiple ways a person can discover about having HIV: you can be notified because the person you have had relations with discovered the infection, or by taking blood tests for blood donation, or in the worst case scenario, when you are already suffering from an opportunistic infection. Go Young, for example, discovered it because of the blood tests results while he was in the army. One thing I found very outrageous was that the physician instantly inferred that Go Young was gay because of that, but this is impossible, since anyone can get the virus, regardless of their sexual orientation. This appointment was like a death sentence: the unempathetic doctor as a ruthless judge, blaming the patient and not offering a single word of comfort. (Quite the opposite: he even asked that very intimate question about sex positions. Seriously, I wanted to punch this doctor so hard.)


Nonetheless, even if it was made in a very inappropriate way, diagnosis is still very important, because that is the only way one can have access to treatment. Each patient must be evaluated separately, since treatment may vary due to the different genetic subtypes of the virus and the person’s own body response. Medication can also be adjusted until satisfactory results are accomplished. Overall, all patients are submitted to a lifetime antiretroviral therapy in order to stop the virus from multiplying and to keep immune cells at a higher level. In the series, we can see Go Young asking for any antiretroviral in a pharmacy, but in real life, he would be very specific about the drugs.

If done properly, treatment can provide quality of life and long life expectancy (very similar to people who don’t have HIV), prevent opportunistic infections and, most importantly, transmission! Yes, that is exactly what you read: treatment can result in really low levels of HIV in the blood, which is called “undetectable viral load” if it happens for at least six months. There is even a saying which goes “Undetectable = untransmittable”. In this scenario the patient can even have sex without a condom with their partner, which is what happened with Go Young and Gyu Ho in the series. However, it is important to mention that this only applies to HIV: one can still get other STIs while having unprotected sex.


In addition to condoms and proper treatment, there are other ways of preventing HIV infection. Susceptible people can use the pre-exposure prophylaxis (PREp) medication, which highly reduces the risk of getting HIV from intercourse (and also from blood contact in a less effective way). There is also the post-exposure prophylaxis (PEP), which can prevent infection if taken within 72 hours after possible exposure. Treating other STIs, not sharing needles, using lubricant (less chance of injury during intercourse) and avoiding sex while in use of alcohol or drugs are some other habits we can do ourselves to minimize the risk of acquiring HIV.
Nevertheless, individual actions can help only until a certain point, given that the best prevention is the “combination prevention”, which includes not only behavioral and biomedical approaches, but also structural interventions. Every country should have their own public policies to assist people living with HIV and to prevent transmission. I’m proud to say that, in Brazil, thanks to our public health system, everyone has access to condoms, lubricants, tests, treatment, PREp and PEP - all free of charge. The system also has policies of damage control, providing all of these strategies to the population of risk, such as sex workers and people with a substance use disorder, including kits with individual needles to prevent sharing and, consequently, blood transmission. No wonder we are an international reference for HIV/AIDS treatment and prevention.
To conclude, I also need to remind you that you can actively help in this cause by simply showing support. As we all watched in “Love in the big city”, a person living with HIV faces all kinds of prejudice in society. Go Young carried a heavy burden for years, not being able to share it with anyone until Gyu Ho embraced him. Sometimes, patients have these prejudices themselves and it can deeply hinder treatment. I have seen this myself: a patient that denied the diagnosis and returned to the hospital sometime later with a severe health condition.
You can be the person that will accept and embrace this other person, who is only living with a chronic condition, such as many people who live with hypertension or diabetes, for example. You can be the person that will call out on others for their preconceived opinions. You can be the person who will share high-quality information to your friends, family, fellow workers or students (There are links in the last paragraph with reliable information for those who want to do some further research).
Finally, I can’t stress enough how much I loved “Love in the big city” for addressing so many types of love and so many sensitive topics, including this one, in such a beautiful way. It has been a long time since I had felt so connected to a story, to a character so human like Go Young.
I hope this essay provided a little bit of information to you. I mostly used the knowledge I have learned in college and sites of well-recognized organizations, such as the UNAIDS, the World Health Organization (WHO) and, for the Portuguese speakers, the Brazilian Ministry of Health (Ministério da Saúde). Thank you for reading, and please, feel free to send me any questions you might have, I’ll do my best to answer them. Also, if you notice any English mistakes, please let me know so I can correct them.
#love in the big city#HIV#aids#health and wellness#healthcare#medicine#SUS#Unified health system#Sistema único de saúde#Viva o SUS#Proteja o SUS#go young#gyu ho
80 notes
·
View notes
Note
Hello, so maybe I’m misunderstanding something based on the bits and pieces I know about ethics and philosophy :what kinds of things constitute as morally good? You said and someone else said health is morally neutral. Which I get the individual part but wanting for others to be educated and healthy I thought * would be examples of moral goodness?¿ Help me to see more pf your point if you are willing
okay, let's talk about education and health.
those are both really big factors in a lot of people's lives, and of course it's good when people have access to opportunities for education and healthcare. I'm not arguing against that at all.
but there is no component of morality to people's level of education or health. attending college, for instance, does not make someone a better person than someone who dropped out of high school. a person with a college degree is likely to have access to better-paying jobs and impact their quality of life, sure, and higher education is desirable to many people because of that; totally understandable. but that's completely different from what I'm talking about, which is whether or not being educated is innately virtuous, which it's not. at an early age, especially, education is something that happens mostly at random, determined primarily by the opportunities available to the family someone is born into.
health is something that is moralized RELENTLESSLY, especially in American culture. many fat activists talk at length about how fatness is seen as a failure of both health and morality - the assumption being that a.) fat people are innately unhealthy and b.) a responsible person would make an effort not to be fat and therefore not to be unhealthy - and that's only one particularly visible example. think about the tendency, for instance, to suggest that people who die of COVID must deserve it based on assumptions made about their masking/vaccine status, as if thousands of people who took every possible precaution didn't also die. in my field, sex education, there's also a TERRIBLE tendency to stigmatize people with sexually transmitted infections and treat them as dangerous, irresponsible, and undeserving of sex of physical intimacy, the most prominent example being the AIDS epidemic during which many people very literally believed that the epidemic was a divine punishment for the "sin" of homosexuality.
of course, health has nothing to do with morality. terrible people live long and healthy lives, the kindest and most selfless people you'll ever meet die in agonizing pain from preventable diseases. similarly to education, it's largely determined by social position.
similarly, activities considered "healthy" carry no moral weight. if you want to eat your veggies or run marathons or never smoke a day in your life, awesome! that's great for you! and I'm right there with you, I love veggies and yoga and rock climbing and all kinds of activities, and I myself don't smoke. but nothing about any of those activities are like, divinely virtuous and make you a certifiable better person than someone who never exercises and lives on cheese and weed. that person is equally allowed to do that and is not an inferior person for choosing that path for their life.
again, healthcare and education are important to many people's quality of life, but they're human rights, not moral measurements.
135 notes
·
View notes
Text
The Impact of COVID-19 on Healthcare Systems
Written by Dev
The COVID-19 pandemic hit healthcare systems worldwide, exposing serious weaknesses and forcing rapid changes. Hospitals were overwhelmed with patients, leading to shortages of beds, oxygen, and protective gear. In places like India, where the healthcare system was already under pressure, these shortages were especially severe, with many patients struggling to get care.
As hospitals focused on treating COVID-19, many regular services like surgeries, cancer treatments, and vaccinations were delayed or canceled. This led to other health issues, like an increase in maternal and child deaths due to lack of access to basic care. For children, interrupted vaccination programs risked future outbreaks of preventable diseases, making this health crisis even worse in the long run. Additionally, multiple countries lacked the proper monetary resources and funding to effectively handle this disaster, aggravating the strain on resources, since the ones that were able to receive healthcare were receiving the same in poor quality, leading to occasional incomplete treatments of the same.
Since all medical resources went towards Covid-19 patients, there was a strain on treating other diseases like Cancer, multiple STDs, etc. Additionally, the lockdown also prevented routine check-ups, leading to a surge in patients with worsening conditions, not necessarily involved with Covid-19. The frequent postponing of health check-ups caused multiple disadvantages, and is a variable that could have lessened the load on the healthcare system.
The pandemic also triggered a disturbing rise in attacks on healthcare workers. According to the World Health Organization (WHO), healthcare staff worldwide faced violence, abuse, and stigma. In many cases, healthcare workers were wrongly seen as “spreaders” of COVID-19, leading to harassment and even physical assault. This fear and misinformation affected not only healthcare workers’ safety but also made it harder to provide medical care.
Mental health issues increased during the pandemic too. Many healthcare workers struggled with stress, burnout, and trauma due to high patient death rates and long hours. The importance for mental health was severely underscored during the time of the pandemic, considering extreme levels of anxiety between not only patients but also regular people. People outside the healthcare field also faced mental health challenges from lockdowns, isolation, and fear of infection. With demand for mental health services rising, healthcare systems struggled to keep up. Health scares combined with break in routine spread widespread paranoia within the people.
However, the crisis did lead to some useful changes, like the growth of telemedicine, which allowed patients to talk to doctors remotely. This made it easier for people to get healthcare without leaving their homes and helped hospitals reduce patient crowding. Many healthcare providers also set up drive-through testing and vaccination centers to make these services more accessible. These new methods of delivering healthcare might continue to improve access even after the pandemic.
Additionally, it introduced newever, more enhanced protocols when faced with death or serious situations, which only improved time and response of healthcare systems. The anxiety and mental stress caused by the pandemic also increased the availability of mental health resources and help to people, a part that helped reduced the stigma surrounding mental health.
COVID-19 has shown that healthcare systems need to be stronger and more flexible to handle future crises. Governments and healthcare leaders are encouraged to invest more in public health, improve safety protections for healthcare workers, and support mental health resources. By learning from COVID-19, healthcare systems can better protect both patients and providers when the next crisis comes.
#covicare#covid#covid 19#group#health#post covid#awareness#mental health#team#wellbeing#article#blog#healthcare system#healthcare
4 notes
·
View notes
Text
The Key to a Healthy Mind: Understanding Brain Health
Brain health is a cornerstone of overall well-being, yet it often doesn’t receive the attention it deserves. The brain, a marvel of complexity and adaptability, governs everything from our thoughts and emotions to our memory and coordination. Prioritizing brain health is not just about preventing cognitive decline; it’s about fostering mental clarity, emotional resilience, and the ability to adapt to life’s challenges.
In this article, we’ll explore the importance of brain health, factors influencing it, and actionable strategies to keep your brain functioning at its best.
Why Brain Health Matters
A healthy brain is essential for:
Cognition: Sharp thinking, learning, and problem-solving skills.
Emotional Well-Being: Managing stress, regulating emotions, and maintaining a positive outlook.
Physical Coordination: Governing motor skills and body functions.
Long-Term Health: Reducing the risk of neurodegenerative diseases like Alzheimer's, Parkinson's, and dementia.
Maintaining brain health isn’t just about aging gracefully. It’s about thriving in daily life, staying productive, and enjoying meaningful relationships.
Factors Influencing Brain Health
Several factors can enhance or impair brain health:
Lifestyle Choices: Diet, exercise, and sleep play a significant role in maintaining cognitive functions.
Stress Levels: Chronic stress can lead to hormonal imbalances that negatively affect the brain.
Mental Stimulation: Learning new skills and engaging in challenging activities keeps the brain active.
Social Connections: Healthy relationships promote emotional well-being and cognitive resilience.
Environmental Factors: Exposure to toxins or a lack of access to quality healthcare can impact brain health.
Strategies to Boost Brain Health
1. Nourish Your Brain
Consume a diet rich in omega-3 fatty acids, antioxidants, and vitamins. Foods like fatty fish, berries, nuts, and leafy greens are excellent choices.
Stay hydrated, as dehydration can impair cognitive functions.
2. Stay Physically Active
Regular exercise improves blood flow to the brain, reduces inflammation, and encourages the release of brain-derived neurotrophic factor (BDNF), which supports neuron growth.
3. Prioritize Quality Sleep
Sleep is critical for memory consolidation and toxin removal in the brain. Aim for 7-9 hours of sleep each night and maintain a consistent sleep schedule.
4. Keep Learning
Challenge your brain by learning a new language, playing a musical instrument, or solving puzzles. Lifelong learning promotes neuroplasticity, the brain's ability to adapt and grow.
5. Manage Stress
Practice mindfulness, meditation, or deep breathing techniques to reduce stress. Chronic stress can lead to brain shrinkage in areas responsible for memory and emotion regulation.
6. Build Social Connections
Spend time with friends and family, join clubs or groups, and maintain strong social ties. Social interaction is crucial for emotional and cognitive health.
7. Protect Your Brain
Wear helmets during physical activities, avoid smoking, and limit alcohol consumption. Protecting your head and overall health is key to preserving brain function.
Signs Your Brain May Need Extra Care
While occasional forgetfulness or mental fatigue is normal, certain signs may indicate the need for more attention:
Persistent memory problems.
Difficulty concentrating or solving problems.
Mood swings or depression.
Trouble with balance or coordination.
If you notice these symptoms, consult a healthcare professional for guidance.
The Future of Brain Health
Advances in neuroscience and technology continue to shed light on brain health. Emerging therapies, wearable devices for cognitive tracking, and personalized health plans are paving the way for innovative care. However, the foundation of brain health remains rooted in everyday habits and choices.
Conclusion
Your brain is your most valuable asset. By nurturing it through a healthy lifestyle, lifelong learning, and stress management, you can unlock its full potential and enjoy a vibrant, fulfilling life. Start small—whether it’s eating a handful of nuts daily or dedicating 10 minutes to mindfulness—and build from there. Your brain will thank you.
youtube
#youtube#bruce wayne#dc comics#fitness#health#lando norris#viral#dnp#medicine#phan#brain health supplement
2 notes
·
View notes
Text
Comprehensive Health Checkups: Detect Problems Before They Start
In today’s busy world, taking care of our health often takes a back seat. Routine health checkups are essential for identifying potential issues early, before they develop into more significant concerns. At Shivaay Hospicare, Dr. Reema Solanki Chauhan, a highly experienced primary physician and Medical Director, is dedicated to offering comprehensive and affordable preventive care services that focus on early detection, personalized treatment, and patient well-being.
Recognized as the Best MD Physician Doctor in Vadodara, Dr Chauhan ensures that Shivaay Hospicare stands out as the Best MD Physician Hospital in Vadodara, providing exceptional care for individuals and families.
Why Preventive Care Matters
Many health issues—such as hypertension, diabetes, and chronic infections—develop silently over time, showing no early symptoms. Regular checkups can:
Detect problems early, enabling timely intervention.
Stop minor issues from turning into major complications.
Improve long-term health outcomes with affordable and accessible care.
Dr. Reema Solanki Chauhan brings over 14 years of experience in clinical practice, advocating for a patient-centred, holistic approach to healthcare.
Healthcare Services at Shivaay Hospicare
Dr. Chauhan at Shivaay Hospicare delivers a comprehensive selection of treatments and services suitable for individuals across all age groups. Whether it’s routine preventive care or managing acute or chronic conditions, the hospital ensures high-quality care under one roof.
General Health Services
Health Checkups (General)
Wellness Screenings for Men, Women, and Seniors
Vaccinations and Immunizations (including Travel Vaccination)
Electrocardiography (ECG) for Heart Health Monitoring
Chronic Disease Management
Diabetes Management (Type 1, Type 2, and Diabetic Ulcers)
Hypertension Treatment
Arthritis Management
Chronic Obstructive Pulmonary Disease (COPD) Treatment
Thyroid Disease Treatment (including Thyroid Issues in Children)
Infectious Disease Treatment
Dengue Fever, Malaria, and Typhoid Fever Treatment
Tuberculosis (TB) Management
Childhood Infections and Measles Treatment
Herpes Infection Treatment
Gastrointestinal Care
Abdominal Pain and Gastritis Treatment
Irritable Bowel Syndrome (IBS) and Gastroenteritis Treatment
Peptic/Gastric Ulcer Management
Constipation and Acute Diarrhea Treatment
Respiratory Care
Cough Treatment and Lower/Upper Respiratory Tract Infection Management
Bronchial Asthma Treatment
Nebulisation Services
Specialized Care for Common Conditions
Headache and Migraine Treatment
Joint and Muscle Problems
Skin Allergies and Rash Treatment
Hair Treatment and Acne/Pimples Treatment
Anemia Treatment
Gout and Fibromyalgia Treatment
Additional Services
Addiction Management
Dressings and Preoperative Treatments
Immunity Therapy for Overall Well-being
Female Sexual Problems Treatment
Bad Breath (Halitosis) Management
A Doctor Who Cares: Dr. Reema Solanki Chauhan
At the heart of Shivaay Hospicare is Dr. Reema Solanki Chauhan, a primary physician with a strong commitment to holistic and equitable healthcare. With degrees in MD (Physician), Industrial Health Certification, and an MBA (Health), Dr. Chauhan blends medical expertise with a deep understanding of patient needs.
Her specialties include managing hypertension, diabetes, and infectious diseases, along with offering preventive care services that improve quality of life.
Recognized as the Best MD Physician Doctor in Vadodara, Dr. Chauhan’s dedication to her patients has earned Shivaay Hospicare a reputation as the Best MD Physician Hospital in Vadodara.
“Preventive care is about staying one step ahead—detecting health concerns early and empowering patients to live healthier lives,” says Dr. Reema Solanki Chauhan.
Why Choose Shivaay Hospicare?
Affordable and Comprehensive Health Checkups
Comprehensive Care for Acute and Chronic Conditions
Personalized Patient Care from an Experienced Physician
Preventive Care Focus for Early Detection and Wellness
Holistic Treatment Approach to Target the Underlying Causes of Health Problems
Take Control of Your Health Today
Your health is too valuable to wait for symptoms to appear. At Shivaay Hospicare, Dr. Reema Solanki Chauhan guarantees that each patient receives the care and focus they are entitled to.
Book your Comprehensive Health Checkup today at the Best MD Physician Hospital in Vadodara and experience care from the Best MD Physician Doctor in Vadodara because early detection saves lives. https://g.co/kgs/7kxizNg
2 notes
·
View notes
Text
Why Allied Health Is the Backbone of Holistic Healthcare Systems

In today’s rapidly evolving healthcare environment, the concept of holistic care has gained significant prominence. Holistic healthcare focuses on treating the whole person—mind, body, and spirit—rather than just addressing specific symptoms or illnesses. At the centre of this comprehensive approach lies allied health, a vital but often underappreciated sector of the healthcare system. Allied health professionals form the backbone of holistic care, offering a wide range of services that complement traditional medicine and enhance the overall quality of patient outcomes.
What Is Allied Health?
Allied health encompasses a diverse group of healthcare professionals who are not doctors, nurses, or dentists but who work collaboratively with these primary care providers to support patients. This field includes roles such as physiotherapists, occupational therapists, dietitians, speech pathologists, radiographers, and paramedics, among others. These professionals are highly trained in their respective disciplines and focus on prevention, diagnosis, treatment, and rehabilitation, ensuring that patients receive well-rounded care.
The Role of Allied Health in Holistic Healthcare
Holistic healthcare requires a multidisciplinary approach, and allied health professionals are uniquely equipped to address the diverse needs of patients. Their specialised expertise contributes to physical, emotional, and social well-being, ensuring that no aspect of a patient's health is overlooked.
1. Addressing Physical Health Needs Allied health professionals play a critical role in improving physical health. Physiotherapists and occupational therapists help patients recover from injuries, manage chronic pain, and regain mobility. These services are not just about fixing a problem but also about empowering patients to take charge of their health through exercise, education, and preventive strategies.
2. Supporting Mental and Emotional Well-being Holistic care also prioritises mental health, recognising the connection between emotional well-being and physical health. Speech pathologists and audiologists, for example, help individuals with communication disorders regain confidence and improve their quality of life. Similarly, social workers and counsellors assist patients in navigating emotional challenges, fostering resilience and stability.
3. Promoting Nutritional Health Dietitians are another key component of allied health, offering tailored nutrition plans that address a variety of health concerns, from weight management to chronic conditions like diabetes and heart disease. By focusing on dietary habits, these professionals empower patients to make sustainable lifestyle changes that support long-term well-being.
4. Bridging Gaps in Healthcare Access Allied health professionals often work in community settings, ensuring that healthcare services are accessible to all, including underserved populations. Paramedics, for instance, provide critical care during emergencies, while community health workers deliver education and preventive care in remote areas. This accessibility is a cornerstone of holistic care, as it ensures that every individual has the opportunity to achieve optimal health.
The Collaborative Nature of Allied Health
One of the defining features of allied health is its collaborative approach. These professionals work alongside doctors, nurses, and other healthcare providers to create a unified care plan tailored to the patient’s unique needs. For example, a patient recovering from a stroke may require input from a physiotherapist, speech pathologist, dietitian, and social worker, all working together to support their recovery journey.
This interdisciplinary teamwork not only improves patient outcomes but also enhances the efficiency of the healthcare system. By addressing various aspects of health simultaneously, allied health professionals help reduce hospital readmissions, shorten recovery times, and minimise healthcare costs.

Allied Health and Preventive Care
Preventive care is a cornerstone of holistic healthcare, and allied health professionals are at the forefront of this movement. Through education, screenings, and early interventions, they help patients identify and manage risk factors before they develop into serious conditions.
For example:
Physiotherapists educate patients on posture and ergonomics to prevent musculoskeletal issues.
Dietitians provide nutritional counselling to combat obesity and related diseases.
Speech pathologists offer early interventions for children with developmental delays, setting them up for success later in life.
By focusing on prevention, allied health professionals not only improve individual health outcomes but also contribute to the long-term sustainability of the healthcare system.
Challenges Faced by Allied Health Professionals
Despite their critical role, allied health professionals often face challenges, including limited recognition and funding. Many people are unaware of the full scope of services offered by allied health, leading to underutilisation of these resources. Additionally, workforce shortages in certain disciplines can strain healthcare systems and limit access to care.
Addressing these challenges requires increased investment in allied health education, public awareness campaigns, and policies that prioritise integrated care models. By supporting the growth and development of this sector, healthcare systems can fully harness the potential of allied health professionals to deliver holistic care.
The Future of Allied Health in Holistic Healthcare
As healthcare continues to evolve, the demand for holistic and patient-centred care will only grow. Allied health professionals are poised to play an even greater role in meeting this demand, thanks to their ability to adapt to new technologies, research advancements, and changing patient needs.
For example, telehealth has expanded the reach of allied health services, allowing professionals to provide care remotely and bridge gaps in access. Similarly, advancements in rehabilitation technology, such as virtual reality and robotic devices, are revolutionising the way allied health professionals deliver care.
Conclusion
Allied health professionals are the backbone of holistic healthcare systems, offering a wide range of services that address the physical, emotional, and social dimensions of health. Their collaborative approach and emphasis on prevention make them indispensable in creating a more inclusive, patient-centred healthcare model.
As society increasingly recognises the importance of holistic care, the role of allied health will continue to expand, transforming the way we approach health and well-being. By supporting and investing in this vital sector, we can ensure that healthcare systems are equipped to meet the diverse needs of individuals and communities alike.
2 notes
·
View notes
Text
Mobile Lab Services
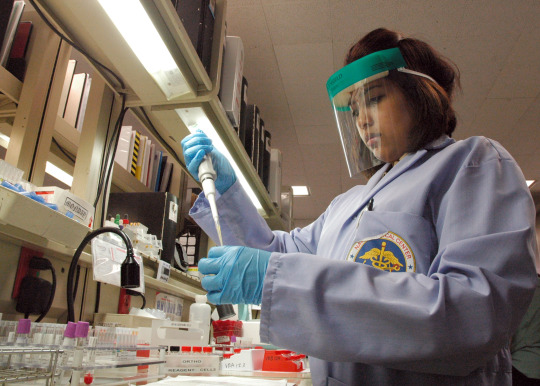
Mobile lab services are transforming healthcare. These services bring diagnostic and laboratory testing directly to your doorstep, eliminating the need for time-consuming trips to medical facilities. At MobileBloodDrawServices, we specialize in providing high-quality, reliable, and patient-centered mobile lab services. This innovative approach ensures you receive the care you need with minimal disruption to your daily routine.

What Are Mobile Lab Services?
Mobile lab services involve professional healthcare providers performing diagnostic tests at a location convenient for the patient, such as their home or office. These services typically include:
Why Choose Mobile Lab Services?
The shift towards mobile healthcare is driven by the growing need for personalized and convenient care. Here are the top reasons to choose mobile lab services at MobileBloodDrawServices:
Convenience and Accessibility Traditional lab visits often involve long waits, scheduling conflicts, and travel. With MobileBloodDrawServices, lab technicians come to you, saving you time and effort.
Patient Comfort For individuals who experience anxiety in clinical settings, mobile lab services offer the comfort of staying in familiar surroundings during testing.
Time-Saving Solutions Busy schedules make it challenging to prioritize healthcare. MobileBloodDrawServices ensures you don’t need to compromise your time, providing quick and efficient services at your preferred location.
Ideal for Vulnerable Populations Elderly individuals, disabled patients, or those with chronic illnesses benefit immensely from mobile services, as they eliminate the challenges of transportation and accessibility.
Services Offered by MobileBloodDrawServices
At MobileBloodDrawServices, we provide a comprehensive range of diagnostic and laboratory services designed to meet diverse patient needs.
Blood Draw Services Our certified phlebotomists are skilled in collecting blood samples for routine and specialized tests. Whether it’s a one-time test or part of ongoing health monitoring, we ensure accuracy and comfort.
Specimen Collection We collect various samples, including urine, saliva, and stool, for diagnostic purposes. Our processes adhere to strict hygiene and safety protocols.
Diagnostic Screenings From cholesterol and glucose testing to vitamin deficiency panels, we offer a wide array of diagnostic screenings to support preventive care.
Health Monitoring For patients managing conditions like diabetes, heart disease, or kidney issues, our mobile lab services provide regular monitoring, ensuring proactive health management.
Why Choose MobileBloodDrawServices?
At MobileBloodDrawServices, we are committed to delivering exceptional care. Here’s what sets us apart:
Experienced Professionals Our team of certified phlebotomists and lab technicians is trained to provide accurate, efficient, and compassionate care.
Advanced Technology We use state-of-the-art equipment to ensure precision in every test, from sample collection to laboratory analysis.
Flexible Scheduling We understand that everyone’s schedule is different. MobileBloodDrawServices offers appointments during evenings and weekends to accommodate your needs.
Transparent Pricing Our services are designed to be affordable, with no hidden fees. You’ll know exactly what to expect before your appointment.
Stringent Hygiene Standards We follow rigorous safety and hygiene protocols to protect patients and staff, ensuring a safe and clean testing environment.
Frequently Asked Questions (FAQs)
Is mobile lab testing accurate? Yes. MobileBloodDrawServices uses the same certified laboratories and advanced equipment as traditional facilities, ensuring accurate and reliable results.
How do I book a service? Simply visit our website or call our customer support team to schedule an appointment at your convenience.
What areas do you serve? We provide services across [specific service regions], including urban and suburban locations.
Are mobile lab services covered by insurance? Many insurance providers cover mobile lab services. Contact us to discuss your insurance plan and payment options.
Mobile lab services offered by MobileBloodDrawServices are revolutionizing the way patients access diagnostic testing. Combining convenience, comfort, and accuracy, these services cater to diverse needs while prioritizing patient care. Whether you’re managing a chronic illness, juggling a busy schedule, or seeking preventive screenings, MobileBloodDrawServices ensures a seamless and stress-free healthcare experience.
Contact US Phone : 703-689-1585 Fax : 1-800-887-9017 Email : [email protected] or [email protected] Address : 3057 Nutley Street, Suite 193, Fairfax Va 22031, United States Website: http://www.mobileblooddrawservices.com/home/
#Mobile Lab Services#mobileblooddrawservices#Mobile blood draw services#Stat blood draw#Blood draw at home services near me#Mobile blood tests
2 notes
·
View notes
Text
The Impact Of Visual Communication In Public Health Campaigns: The Use of Infographics & Videos To Convey Health Messages
Hello! This blog will be the final blog post :) Let’s get started!
Effective communication is vital in public health campaigns to educate and influence public behaviors. Visual communication, through infographics and videos, plays a significant role in conveying complex health messages in a way that is both engaging and accessible. This approach combines clarity, creativity, and emotional appeal to foster better understanding and action (StudySmarter, 2024).
In recent years, digital platforms have become integral to health communication, enabling the use of interactive and animated content. These innovations capture attention and actively involve audiences, encouraging behaviors like staying physically active or keeping up with vaccinations (StudySmarter, 2024). The shift toward digital visual communication has broadened its global impact, offering both opportunities and challenges related to accessibility, cultural appropriateness, and adapting to technological advancements.
Health Communication Through Data Visualisation 👁️
Advancements in technology have transformed data visualization tools, enabling real-time insights through dashboards and interactive platforms. These tools showcase current health data and forecast future trends by analyzing existing patterns. With the integration of artificial intelligence, dashboards are now more personalized, delivering tailored health recommendations based on user input and preferences (StudySmarter, 2024).
Examining different examples of visual health communication highlights the variety of strategies used to convey health messages effectively. These examples demonstrate how visual elements can inform and shape public health behaviors.
Infographics in Public Health 🌡️
Infographics are visual tools that present data and information in an easily digestible format. They combine text, visuals, and design to summarize and explain key messages (Maa Illustration, 2023).
Visual Storytelling
Visual storytelling is powerfully enhanced through medical illustration, which can effectively and engagingly convey complex health concepts, disease transmission patterns, and preventive measures. These illustrations help make the importance of health-related behaviors more understandable and memorable to the public.
Disease Prevention & Awareness Campaigns
Disease prevention and awareness campaigns, such as those promoting vaccination or healthy eating, are central to public health initiatives. Medical visuals can help make these concepts clearer and more convincing to a broader audience by breaking down the science behind them.
Digital & Interactive Tools
Digital and interactive tools, such as infographics, animations, and interactive modules, have expanded the reach and effectiveness of public health campaigns. These dynamic visuals help convey information in an engaging and memorable manner.

Image credit: Canva Pink and Blue Illustrated World Diabetes Day Infographic
Tools like Canva, Piktochart, and Adobe Illustrator offer intuitive interfaces and customizable templates for creating eye-catching infographics. These platforms provide a wide range of design elements, icons, and fonts, making it easy to craft impactful visuals that effectively communicate key messages (MeDesk, 2024).
Infographics are a creative and engaging way to present information in a visually appealing and concise format, and they have gained significant attention in both the commercial and healthcare sectors (AD McCrorie, C Donnelly, KJ McGlade, 2016).
Videos In Public Health 📹
Video campaigns are a compelling form of visual health communication, leveraging motion, sound, and storytelling to capture and hold attention (Maa Illustration, 2023). Effective campaigns typically include:
Storytelling
Emotional narratives that connect with audiences, making messages more memorable.
High-Quality Production
Professional visuals and audio that enhance credibility and ensure clarity.
Call to Action
Clear prompts encouraging viewers to take steps like changing behaviors or seeking further information.
For instance, short videos on COVID-19 symptoms and prevention shared on social media have proven effective in rapidly educating large audiences.
Youtube
YouTube is the second most popular search engine globally, with about one-third of all online activity dedicated to watching videos. Health communicators can leverage the World Health Organization’s (WHO) YouTube channel, which hosts hundreds of videos, to enhance knowledge and raise awareness about health issues (World Health Organization, 2024).
youtube
Video credit: Stanford Center for Health Education
Conclusion
Visual communication through infographics and videos enhances the impact of public health campaigns by making health messages more accessible, engaging, and memorable. By addressing diverse audience needs and preferences, these tools help bridge knowledge gaps and drive positive behavioral changes.
Thank you for reading this far! :)
References
StudySmarter. (2024). Visual Health Communication: Examples & Media
https://www.studysmarter.co.uk/explanations/media-studies/health-communication-in-media/visual-health-communication/
MeDesk. (2024). 7 Use Cases for Visual Communication in Healthcare
https://www.medesk.net/en/blog/visual-communication-in-healthcare/
AD McCrorie, C Donnelly, KJ McGlade. (2016, January 2). Infographics: Healthcare Communication for the Digital Age
https://pmc.ncbi.nlm.nih.gov/articles/PMC4920488/
World Health Organization. (2024). Tactics to apply to make your communications understandable
https://www.who.int/about/communications/understandable/visuals
Maa Illustration. (2023, February 11). Impact of Medical Illustration in Public Health Campaigns
https://www.maaillustrations.com/blogs/magazine/impact-of-medical-illustration-in-public-health-campaigns
2 notes
·
View notes
Text
Understanding Different Types of Health Centers: A Comprehensive Report
Quality healthcare is a fundamental right, especially for a less privileged population. Throughout the United States, health centers are serving important roles in delivering care to populations that would otherwise lack access to medical services. Did you know that there are actually various types of health centers designed to meet various needs? Read below to see what the different types of health centers do and how they work towards improving communities' health.
Community Health Centers (CHCs)
Community Health Centers (CHCs) are likely one of the most common categories of health centers. These centers give primary, integrated care to low-income and medically underserved populations. Be it in cities or rural locations, CHCs give quality health services, even to some in health professional shortage areas (HPSAs).
Common services of CHCs include:
Primary care
Dental care
Mental health and substance abuse
Vaccinations
Chronic diseases management
CHCs are patient-centered, providing any patient any time with the assurance that everyone will receive care regardless of ability to pay. The majority of CHCs operate off a sliding fee scale. What patients pay depends on their income.
Migrant Health Centers (MHCs)
Migrant Health Centers (MHCs) are tailor-made services to meet the specific healthcare needs of migrant and seasonal agricultural workers. Such workers often face major health issues due to their migratory lifestyle, hazardous conditions, and lack of easy access to consistent healthcare. MHCs fill in such gaps, ensuring that the vulnerable populations get necessary healthcare.
Services offered by MHCs include:
Primary and preventive care
Occupational health services
Chronic condition management education
Pediatric and maternal care
The MHCs play an important role in providing health care to workers and their families who may often be moving between different parts of the country and need to have access to continued care.
Health Care for the Homeless Centers
Homelessness can be related to extreme challenges to health services. Health Care for the Homeless Centers (HCHs) are organized for the needs of the homeless. In addition to medical services, they provide crucial support services aimed at assisting stabilization.
Services HCHs:
Primary Care and Preventive Services
Behavioral Health Treatment
Case Management and Social Services
Housing Assistance and Benefits
HCHs represent a comprehensive, integrated model of care that addresses both physical and mental health needs while helping patients access housing and financial resources.
Public Housing Primary Care Centers (PHPCs)
Public Housing Primary Care Centers (PHPCs) are located in or around public housing developments. These centers orient to providing care near where the majority of residents live, thus increasing accessibility in terms of convenience and affordability. Situated close to where people live eliminates barriers to care and makes services accessible to them because residents do not have to travel far.
Common services available at PHPCs:
Routine medical examinations
Vaccinations
Follow-up management of chronic conditions
Health instruction
These offer an important resource in the way of providing primary care and prevention services for those living in public housing.
School-Based Health Centers (SBHCs)
School-Based Health Centers (SBHCs) have emerged as an innovative approach to bringing health care to the school. Medical, mental health, and sometimes dental services are provided in these centers to the students, staff, and the community at large. To most of the students—mostly in low-income schools—it may be the only source of health care.
Services provided at SBHCs include:
Physical check-ups, immunization against common contagious diseases
Common illnesses and injuries
Psychological Counseling
Health education
Health centers directly provide care at schools; therefore, the students are kept healthy and ready for school.
Why Health Centers Matter
Health centers are crucial for the reduction of health disparities. They bridge gaps in healthcare access for populations who often fall between the cracks in traditional healthcare systems. Whether it is a Community Health Center in a rural area or a Healthcare for the Homeless Center in a city, these facilities are necessary for closing gaps in healthcare access.
How to Find the Right Health Center for You
Each type of health center serves a specific population, but all are available to any individual who requires care. To find a health center near you, use our Health Centers Directory to search for locations, services, and programs. Whether you require primary care, mental health services, or assistance in managing a chronic condition, you likely have access to a health center that can meet your needs.
Conclusion
Health centers are the backbone of accessible healthcare in many underserved communities. Knowing the difference between various types of health centers will help you make an informed choice about where to seek care. In any of these situations, these centers exist to provide affordable and compassionate care to you and your family, ensuring that no one is left without the healthcare they deserve.
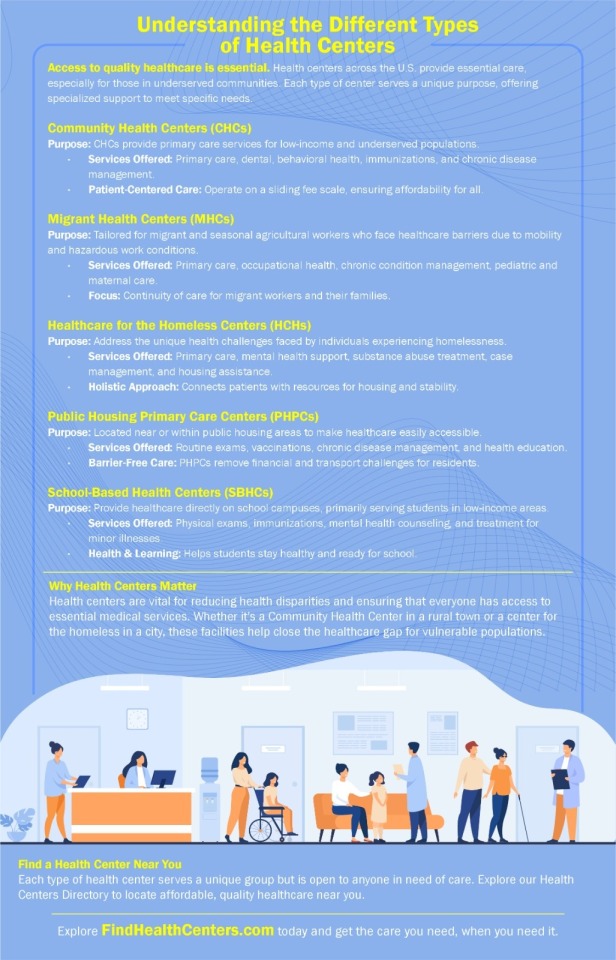
#HealthCenters#HealthcareAccess#CommunityHealth#PublicHealth#HealthServices#PrimaryCare#TypesOfHealthCenters#HealthPolicy#HealthDisparities#HealthcareSystems#PatientCare#WellnessResources#PreventiveCare#HealthEducation#HealthEquity
2 notes
·
View notes
Text
Raised Toilet Seats: A Simple Solution for Dignified Mobility

Imagine this: The 72-year-old grandma Margaret has always taken great satisfaction in her independence. From gardening to cooking her family’s favorite meals, she’s lived an active life. However, after undergoing hip surgery, the simple act of sitting down on and getting up from the toilet became a painful and difficult task. For Margaret, the raised toilet seat wasn’t just a piece of medical equipment—it was a lifeline that gave her back her independence and dignity.
For individuals recovering from surgery, living with arthritis, or dealing with limited mobility due to aging, everyday activities like using the bathroom can become overwhelming. The raised toilet seat is designed to provide comfort and safety by elevating the seat height, reducing the amount of bending required and making the process easier and less painful.
The Growing Need for Raised Toilet Seats
As the population ages, the demand for assistive devices that enhance mobility and accessibility has risen. According to the Centers for Disease Control and Prevention (CDC), over 23% of adults aged 65 and older suffer from arthritis, which often affects their ability to perform daily tasks. Furthermore, research from The National Institutes of Health indicates that falls in the restroom account for 80% of all incidents involving senior people suffering injuries.
A raised toilet seat can reduce the risk of falls by minimizing the amount of strain placed on muscles and joints, allowing individuals to sit and stand with minimal discomfort. It is more than just decoration; it is a vital instrument for maintaining independence.
How Comfort and Safety Are Improved by Raised Toilet Seats
The key benefit of a raised toilet seat is that it elevates the height of the toilet by 2 to 6 inches, reducing the need for users to bend their knees and hips when sitting or standing. This simple adjustment makes a world of difference for those with mobility issues, as it decreases pain and the risk of losing balance during transitions.
Moreover, many raised toilet seats come with added safety features such as padded handles or non-slip surfaces. These elements provide additional support and stability, preventing accidents and giving users greater confidence when using the toilet.
Moovkart: Your Partner in Medical Supplies
At Moovkart, we understand the importance of high-quality, accessible medical equipment. Because of this, we supply a wide range of raised toilet seats that are designed to accommodate different requirements. Whether you're recovering from surgery or dealing with a chronic condition like arthritis, our Medical Equipment Online platform makes it easy to find products that enhance comfort, safety, and independence.
Our raised toilet seats are built with durability and safety in mind, offering features such as easy-to-clean surfaces, adjustable heights, and secure mounting options to ensure the best fit for any bathroom setup.
The Benefits of Raised Toilet Seats in Daily Life
For individuals with reduced mobility, even small modifications can drastically improve their quality of life. According to a study conducted by The American Geriatrics Society, individuals who use raised toilet seats report a 40% reduction in pain when sitting or standing, compared to those who use standard toilet seats. Additionally, healthcare providers observe a 35% decrease in fall-related injuries in patients who utilize raised toilet seats as part of their home care equipment.
Raised toilet seats are especially beneficial for individuals recovering from surgeries such as knee or hip replacements, where bending at the joint should be minimized to avoid strain. These simple devices can make recovery faster and less painful, allowing patients to regain their mobility and confidence sooner.
Independence with Dignity
For those who have experienced limited mobility, using assistive devices can feel like a loss of independence. However, raised toilet seats are designed to enhance dignity by allowing users to perform personal tasks with minimal assistance. The improved height and safety features ensure that individuals can maintain their privacy and autonomy, without the constant fear of falling or experiencing pain.
Conclusion
Raised toilet seats are a simple yet effective solution for individuals facing mobility challenges, offering both safety and comfort. For anyone dealing with chronic conditions or recovering from surgery, this small addition to the bathroom can make a significant impact on day-to-day life. By reducing strain and improving stability, a raised toilet seat allows users to maintain their independence and perform essential tasks with dignity.
Our goal at Moovkart is to give our clients medical goods that enhance their quality of life. Through our Medical Equipment Online store, you can find the right raised toilet seat to meet your needs, ensuring safety and comfort for yourself or a loved one.
Could a raised toilet seat be the simple solution that enhances your daily comfort and safety?
2 notes
·
View notes
Text
Our Greatest Treasure Dear readers, health is undoubtedly the most valuable resource we have. According to the World Health Organization (WHO), health is a state of physical, mental, social, and spiritual well-being, not merely the absence of disease or infirmity. It involves a harmony between the various aspects of our lives.
1. Physical Health. Physical health refers to the optimal functioning of our bodies.
It includes:
Proper Nutrition: Eating nutritious and balanced meals provides the vitamins, minerals, and energy needed to stay active and healthy. For example, a diet rich in fruits, vegetables, lean proteins, and healthy fats helps prevent chronic diseases.
Regular Exercise: Consistent physical activity, such as walking, running, swimming, or yoga, helps maintain muscle strength, flexibility, and cardiovascular health.
Sufficient Rest: Quality sleep is essential for the recovery and regeneration of the body. Adults need around 7-9 hours of sleep per night to function at their best.
Disease Prevention: Regular medical check-ups, vaccinations, and preventive screenings help detect and prevent health issues early.
2. Mental Health. Mental health is equally important. This includes:
Stress Management: Relaxation techniques like meditation, deep breathing, and hobbies can reduce stress and anxiety levels. Chronic stress can lead to health problems, so it's important to manage it effectively.
Managing Anxiety and Depression: Counseling and therapy may be necessary for those dealing with anxiety or depression. Seeking professional help when needed is crucial.
Emotional Well-being: Maintaining a positive and balanced mood contributes to a happier and more fulfilling life. Activities that bring joy and satisfaction, such as hobbies and spending time with loved ones, are essential.
3. Social Health. Social relationships and connections with others play a crucial role.
Emotional Support: Help and understanding from family and friends make it easier to overcome difficult times. Strong, trustworthy relationships are vital for mental and emotional health.
Interpersonal Relationships: Building and maintaining healthy relationships contribute to overall well-being. Effective communication and mutual respect are key elements.
Combating Isolation: Participating in social and community activities helps us feel connected and avoids feelings of loneliness. Volunteering, support groups, and social clubs are good ways to get involved.
4. Spiritual Health. Our connection to the Universe and Divinity can be nurtured through:
Prayer: Spiritual connection through prayer can offer peace of mind and a sense of belonging and purpose. Prayer can bring comfort and hope during difficult times.
Meditation: Practices of introspection and deep relaxation, such as meditation, help us focus the mind and calm the soul. Meditation can reduce stress and anxiety, improving overall well-being.
5. Homeostasis. Our body strives to maintain internal balance, called homeostasis.
Regulation of Internal Variables: Temperature, blood sugar levels, and chemical balance are constantly adjusted to keep us healthy. For instance, when our body overheats, it begins to sweat to reduce its temperature.
6. Influencing Factors. Health is influenced by a variety of factors:
Healthcare System: Access to medical services, health education, and disease prevention is essential. An efficient healthcare system ensures we receive necessary treatment on time.
Environmental Factors: Air quality, clean drinking water, living conditions, and exposure to toxic substances significantly impact health. For example, air pollution can cause respiratory problems.
Genetic Factors: Genetic predisposition can affect the likelihood of certain conditions. Knowing our family medical history can help prevent or better manage certain diseases.
Lifestyle: Diet, physical activity, sleep, and personal habits play a major role in maintaining health. For example, smoking and excessive alcohol consumption can negatively affect our health.
Health is not just the absence of disease but a holistic state of well-being where the body, mind, and social relationships blend harmoniously. It's important to care for all these dimensions to achieve optimal balance and enjoy a healthy, happy life.
Take care of yourselves and your loved ones because health is the key to a fulfilling life!
#healthcare#health & fitness#healthylifestyle#health and wellness#healing#mental health#wellness#medicine#prevention#health#love#self care#self love#life#life lessons#lifestyle#understanding
2 notes
·
View notes
Text
Partnering with the Marpu Foundation for Enhanced CSR Efforts and SDG Achievement

Partnering with the Marpu Foundation can significantly boost a company’s Corporate Social Responsibility (CSR) efforts and contribute to achieving Sustainable Development Goals (SDGs). The Marpu Foundation is known for its impactful projects focusing on environmental conservation, community development, education, and healthcare. By collaborating with the foundation, companies can enhance their CSR initiatives and make a positive impact on society and the environment.
1. Environmental Conservation Projects
One key area where partnering with the Marpu Foundation can amplify CSR efforts is environmental conservation. The foundation is actively involved in various projects aimed at preserving and restoring the natural environment. These initiatives include:
Reforestation Programs: Marpu Foundation organizes reforestation programs to restore degraded ecosystems and enhance biodiversity. Companies can support these programs financially or through employee volunteer programs, showcasing their dedication to environmental sustainability.
Endangered Species Protection: The foundation's efforts to protect endangered species through habitat conservation and anti-poaching initiatives can be bolstered by corporate partnerships. Companies can contribute resources or technology to aid in monitoring and protecting wildlife.
Clean Energy Projects: Marpu Foundation promotes clean energy solutions such as solar and wind power. By funding or collaborating on these projects, companies can help reduce carbon footprints and advance SDG 7 (Affordable and Clean Energy).
2. Community Development Initiatives
The Marpu Foundation's community development projects aim to uplift marginalized communities, providing essential services and infrastructure. Companies can enhance their CSR impact through:
Poverty Alleviation Programs: Collaborating with Marpu on initiatives that provide employment opportunities, vocational training, and micro-financing can significantly reduce poverty levels in underprivileged areas, contributing to SDG 1 (No Poverty).
Access to Clean Water and Sanitation: Partnering with Marpu to build wells, sanitation facilities, and water purification systems helps ensure clean water access, aligning with SDG 6 (Clean Water and Sanitation).
Healthcare Services: Supporting the foundation’s efforts to set up clinics and mobile health units improves healthcare access in remote regions, addressing SDG 3 (Good Health and Well-being).
3. Education and Healthcare Programs
Education and healthcare are pillars of sustainable development, and Marpu Foundation's programs in these sectors are transformative:
Educational Outreach: By partnering with Marpu to build schools, provide scholarships, and supply educational materials, companies can contribute to SDG 4 (Quality Education). Employee volunteer programs can also enhance the educational experiences of children and adults in these communities.
Healthcare Improvement: Supporting Marpu’s healthcare initiatives, such as vaccination drives, maternal health programs, and disease prevention campaigns, ensures better health outcomes for vulnerable populations.
Examples from Marpu’s Projects
Project A: Reforestation Initiative: This project focuses on planting native trees in deforested areas to restore ecosystems, increase biodiversity, and combat climate change. Companies can participate by funding tree planting events and engaging employees in volunteer activities.
Project B: Community Health Clinic: Establishing health clinics in underserved areas to provide primary healthcare services. Corporate partners can fund the construction and operation of these clinics, supply medical equipment, and support health awareness campaigns.
Project C: Solar Energy Installation: Installing solar panels in rural communities to provide sustainable and affordable energy solutions. Companies can sponsor solar projects, provide technical expertise, and promote renewable energy adoption.
Conclusion
By engaging in such projects with the Marpu Foundation, companies can align their CSR efforts with sustainable development goals while making a tangible difference in the lives of people and the environment. This collaboration not only enhances the company's social and environmental impact but also strengthens its reputation as a responsible and forward-thinking entity. Through strategic partnerships with organizations like the Marpu Foundation, businesses can contribute meaningfully to global efforts in creating a more sustainable and equitable world.
2 notes
·
View notes
Text

Wrote a thing for the Outer Space Arcata ig, thought I'd put it here too.
Big thank you to everyone who wears masks at Outer Space, and HUGE shoutout to @maskbloceastbay for donating 100 kn95 masks this month so we can provide them for free. Mutual aid is the future! Wearing a mask helps keep our events accessible to everyone! We encourage you to support @maskbloceastbay or your local mask bloc if you can. I think we can all agree our government and the capitalist healthcare industry has failed us, so here’s a little info to help bridge the public health education gap so you can understand why we still highly encourage wearing a high quality respirator (n95, kn95, kf94, ect.) Every time you are infected with covid, even if you only have mild symptoms, it damages your immune system, and can infect cells in many parts of the body besides the lungs including the heart, brain and blood vessels. So while immunocompromised people are more at risk of long covid from one infection, even the most healthy individuals, if they get repeat infections over the years, will almost certainly end up with a damaged immune system, long covid, heart disease, brain damage, ect. While there’s a lot of things about covid we still don’t know, these things are almost certain: Everyone is at risk. Respirator masks (not surgical or cloth!) are very effective at preventing transmission. Asymptotic spread is very common, you can be contagious even if you don’t feel sick. Covid aerosols travel in the air like smoke and can linger for hours. Even better is using multiple layers of protection like getting the most updated vaccine, improving air quality, and testing regularly. You can still get eight free rapid tests a month with most insurance plans. If you need help accessing free rapid tests, free masks, or have any other questions please reach out to us or your local mask bloc. You can find a great directory at maskbloc.org and lots more info on the science of covid and reality of where we are in the pandemic at peoplescdc.org. Covid justice is disability justice, all our struggles are connected, when the systems fail it’s up to us to protect each other! 😷💉💖
3 notes
·
View notes
Text
BV Circa Medical Centre, Norwest: Comprehensive Healthcare Solutions

BV Circa Medical Centre, situated in Norwest, is dedicated to delivering high-quality healthcare services to the community. This article explores the diverse range of Medical Centre Norwest, the experienced healthcare team, and the center's commitment to patient well-being.
Comprehensive Medical Services
BV Circa Medical Centre offers a comprehensive range of medical services designed to address various health needs:
General Practice: Routine health check-ups, preventive care, and management of chronic conditions.
Specialist Care: Access to specialists in areas such as cardiology, dermatology, and orthopedics.
Women’s Health: Services include gynecological exams, family planning, and menopause management.
Men’s Health: Prostate health, sexual health, and general men’s wellness.
Children’s Health: Pediatric care, vaccinations, and developmental assessments.
Mental Health: Counseling services, mental health assessments, and referrals to psychiatrists.
Geriatric Care: Elderly health assessments, mobility aids, and management of age-related conditions.
Chronic Disease Management: Comprehensive care plans for diabetes, hypertension, and other chronic illnesses.
Experienced Healthcare Team
The centre boasts a team of dedicated healthcare professionals committed to providing compassionate and effective care:
General Practitioners (GPs): Primary healthcare providers offering ongoing management and treatment.
Specialists: Experts in various medical fields, ensuring specialized care for complex health issues.
Nurses and Allied Health Professionals: Supporting patient care through education, rehabilitation, and health promotion.
Patient-Centered Care
BV Circa Medical Centre adopts a patient-centered approach to healthcare delivery:
Personalized Treatment Plans: Tailored to meet individual health needs and preferences.
Holistic Care: Addressing physical, emotional, and social aspects of health.
Health Education: Empowering patients with knowledge to make informed health decisions.
Continuity of Care: Ensuring seamless coordination and follow-up for ongoing health management.
State-of-the-Art Facilities
The centre is equipped with advanced facilities to support comprehensive healthcare services:
Diagnostic Services: On-site pathology and imaging services for accurate diagnosis.
Treatment Rooms: Well-equipped for minor procedures and treatments.
Telehealth Services: Virtual consultations for convenient access to healthcare.
Community Engagement
BV Circa Medical Centre actively engages with the community through health promotion initiatives and educational programs:
Health Workshops: Providing information on wellness and disease prevention.
Community Health Events: Promoting health awareness and early detection of medical conditions.
Conclusion
BV Circa Medical Centre in Norwest is committed to providing exceptional healthcare services tailored to the needs of the community. With a focus on patient-centered care, an experienced healthcare team, and advanced facilities, the center ensures comprehensive health solutions for all patients.
To learn more about the services offered or to schedule an appointment, visit the BV Circa Medical Centre website or contact their friendly staff directly.
2 notes
·
View notes
Text
Home Visit Doctor: Bringing Healthcare to Your Doorstep
Access to quality healthcare is a fundamental right, yet many individuals face barriers that prevent them from receiving timely medical attention. For the elderly, individuals with chronic conditions, and those with mobility issues, visiting a doctor’s clinic can be challenging. The concept of a home visit doctor service addresses these challenges by bringing healthcare directly to the patient’s home. This article explores the benefits, services, and considerations of home visit doctor services.
The Need for Home Visit Doctor Services
Accessibility Issues
Mobility Challenges: Elderly and disabled individuals often find it difficult to travel to healthcare facilities.
Geographical Barriers: Those living in remote areas may have limited access to medical services.
Convenience
Busy Schedules: Working professionals and caregivers may struggle to find time for clinic visits.
Comfort: Receiving care in the comfort of one’s home can be less stressful for patients.
Continuity of Care
Chronic Conditions: Patients with chronic illnesses require regular monitoring and follow-up.
Post-Hospitalization Care: Continued medical supervision at home can aid in recovery after hospital discharge.
Benefits of Home Visit Doctor Services
Personalized Care
Individual Attention: Doctors can spend more time with each patient, providing thorough examinations and personalized treatment plans.
Comfort: Patients feel more at ease in their own environment, which can improve communication and compliance.
Comprehensive Services
Routine Check-Ups: Regular health assessments and monitoring of chronic conditions.
Diagnostic Services: On-site diagnostic tests such as blood tests, ECGs, and ultrasounds.
Preventive Care: Vaccinations, health education, and lifestyle counseling.
Improved Health Outcomes
Early Detection: Regular home visits can lead to the early detection of health issues, allowing for timely intervention.
Reduced Hospitalizations: Continuous care at home can prevent complications that require hospital admissions.
Enhanced Quality of Life
Patient Comfort: Receiving care at home reduces the stress and discomfort associated with clinic visits.
Family Involvement: Family members can be more involved in the patient’s care, providing support and encouragement.
Services Offered by Home Visit Doctors
General Medical Care
Health Assessments: Comprehensive physical examinations and health evaluations.
Chronic Disease Management: Monitoring and management of conditions such as diabetes, hypertension, and heart disease.
Diagnostic Services
Laboratory Tests: Blood tests, urine tests, and other diagnostic procedures conducted at home.
Imaging Services: Portable equipment for ECGs, ultrasounds, and X-rays.
Preventive Care
Vaccinations: Immunizations for influenza, pneumonia, and other preventable diseases.
Health Screenings: Regular screenings for conditions like high blood pressure, cholesterol, and cancer.
Post-Hospitalization Care
Recovery Support: Assistance with recovery and rehabilitation after surgery or hospital discharge.
Wound Care: Management of surgical wounds, pressure sores, and other types of injuries.
Palliative and End-of-Life Care
Comfort Care: Providing relief from pain and symptoms for terminally ill patients.
Emotional Support: Counseling and support for patients and their families during difficult times.

How to Access Home Visit Doctor Services
Finding a Provider
Online Search: Look for home visit doctor services in your area through online directories and healthcare platforms.
Referrals: Ask for recommendations from primary care physicians, friends, and family members.
Booking an Appointment
Online Platforms: Many providers offer online booking through their websites or mobile apps.
Phone Call: Call the provider’s office to schedule an appointment and discuss your needs.
Preparing for the Visit
Medical History: Have your medical records and history ready for the doctor.
Medications: Keep a list of all medications you are currently taking.
Home Environment: Ensure a clean and quiet space for the examination.
Considerations for Home Visit Doctor Services
Cost
Insurance Coverage: Check if your insurance covers home visit doctor services.
Out-of-Pocket Expenses: Be aware of any additional costs for the convenience of home visits.
Availability
Service Areas: Ensure the provider offers services in your area.
Specialty Care: Confirm that the provider has doctors specializing in your specific health needs.
Quality of Care
Credentials: Verify the qualifications and experience of the doctors.
Reputation: Look for reviews and testimonials from other patients.
Safety and Privacy
Infection Control: Ensure the provider follows strict hygiene and infection control protocols.
Confidentiality: Confirm that patient privacy and confidentiality are maintained.
Conclusion
The concept of a home visit doctor service is revolutionizing healthcare by making it more accessible, convenient, and personalized. By bringing medical care directly to patients’ homes, these services address the challenges faced by those with mobility issues, chronic conditions, and busy schedules. With comprehensive care, improved health outcomes, and enhanced quality of life, home visit doctor services are a valuable addition to modern healthcare. Whether you need routine check-ups, chronic disease management, or post-hospitalization care, home visit doctor services provide a practical and compassionate solution to your healthcare needs.
2 notes
·
View notes