#Behavioral Health Billing
Explore tagged Tumblr posts
Text
PROs and CONs of TMS therapy
Transcranial magnetic stimulation, or TMS therapy, is a non-invasive medical procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression and other psychiatric disorders. The procedure involves placing a magnetic coil on a patient's scalp near the forehead and delivering repetitive magnetic pulses to the brain. While TMS therapy has shown promising results, it is also accompanied by potential risks and limitations. In this article, we will explore the pros and cons of TMS therapy.
PROs and CONs of TMS therapy

Pros of TMS Therapy:
Non-Invasive: TMS therapy is a non-invasive procedure that does not require anesthesia or surgery. Unlike other treatments for depression like electroconvulsive therapy (ECT) which involves using electrical currents to induce seizures, TMS therapy is painless and does not require the use of sedatives or muscle relaxants. This makes it a safer alternative for patients who are unable to undergo surgery or have a fear of anesthesia.
Effective for Treatment-Resistant Depression: TMS therapy has been found to be effective in treating treatment-resistant depression (TRD), a condition where individuals do not respond to traditional antidepressant medications. A study published in the Journal of Clinical Psychiatry found that TMS therapy resulted in remission rates of up to 58% in patients with TRD. Additionally, TMS therapy has been shown to have fewer side effects than traditional antidepressant medications.
Convenient and Time-Efficient: TMS therapy sessions typically last between 30-60 minutes and can be conducted in an outpatient setting. Unlike other therapies that may require daily or weekly appointments, TMS therapy is often administered twice a week for several weeks. This allows patients to maintain their daily routine while receiving treatment.
Fewer Side Effects: TMS therapy has fewer side effects than traditional antidepressant medications. Common side effects of TMS therapy include mild scalp discomfort, headaches, and mild-to-moderate muscle contractions in the face. These side effects are typically mild and temporary, resolving within a few hours of treatment.
Cons of TMS Therapy:
Expensive: TMS therapy is an expensive treatment option. The cost per session can range from $300-$500, with a typical course of treatment involving 20-30 sessions. While some insurance companies may cover TMS therapy, it may still be out of reach for many individuals who do not have adequate coverage.
Limited Availability: TMS therapy is not widely available across the United States and may not be covered by insurance in certain states or regions. Additionally, TMS therapy requires specialized equipment and trained personnel to administer the treatment, which may limit its availability in certain areas.
Potential for Relapse: While TMS therapy has been shown to be effective in treating depression, there is a potential for relapse following treatment. A study published in JAMA Psychiatry found that while TMS therapy resulted in reduced symptoms of depression, patients who received maintenance therapy (ongoing treatment) were less likely to experience relapse than those who did not receive maintenance therapy.
Limited Efficacy for Other Disorders: While TMS therapy has been found to be effective in treating depression, its efficacy for other psychiatric disorders such as anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder is limited. Further research is needed to determine the effectiveness of TMS therapy in treating these conditions.
Conclusion:
TMS therapy is a promising treatment option for individuals with TRD who are unable to respond to traditional antidepressant medications. It is a non-invasive procedure that is convenient and time-efficient. However, TMS therapy is also accompanied by potential risks and limitations. It is an expensive treatment option that may not be widely available or covered by insurance in certain regions. There is also a potential for relapse following treatment and its efficacy for other psychiatric disorders is limited. Despite these limitations, TMS therapy represents a significant advancement in the treatment of depression and has the potential to improve the lives of many individuals struggling with this condition.
0 notes
Text
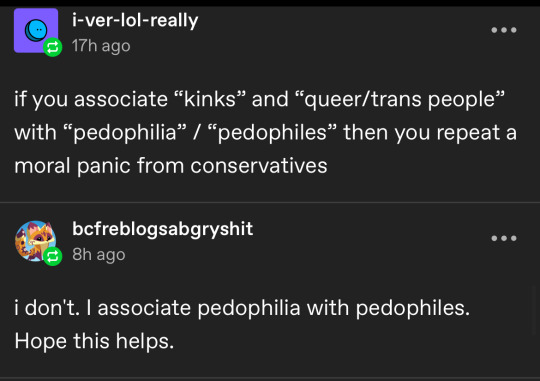
Are you truly anti-harassment, @ anti-paradise?
Before we begin with this post, we would like to make the following clear:
asks, submissions and notifications have been turned off. We will not be looking at or answering any comments or reblogs, should there be any
we do not like being called proship, anti anti, anti or anti-shipper. We are critical of "both sides"
we are aware that most of the depicted accounts are owned by teenagers, with two or maybe three exceptions.
we are strictly against harassment and do not wish for the individuals here depicted or anyone else to be harassed
at the same time we are aware that there is at least one harasser who keeps interacting with the individuals described in this post, and who these individuals call "shoo". We condemn any harassers' actions
we collected screenshots from different posts, but we are not associated with any person
Now with that out of the way let's talk about the "infamous" anti proship group that has been making the rounds on tumblr. If you know who we are talking about, it is the individuals frequently found defending, following and or reblogging from the blog "anti-paradise" who was previously known as antiproshipconfessions.
We decided to categorize the group as "anti-fans". Unlike normal fans who interact with media or a person they are a fan of with genuine passion, anti-fans invest time and "passion" into mocking, criticizing, spreading bad faith rumors, and posting malicious posts or articles about the media, person or group they hate. This may also border sometimes on strong and negative obsession.
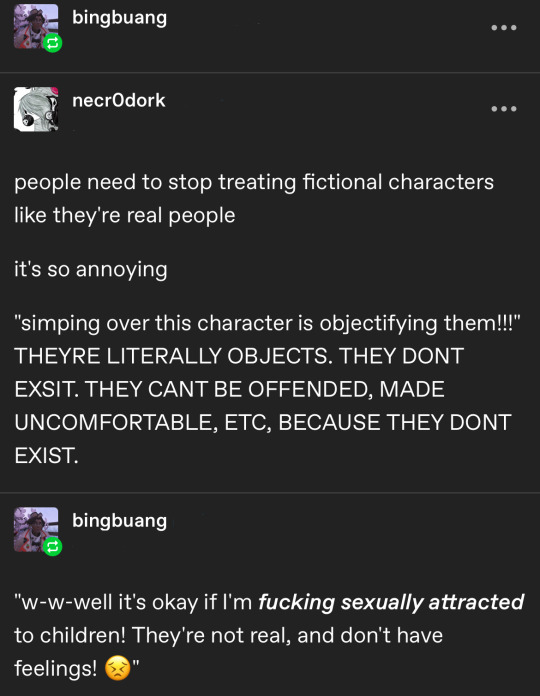
This specific group shows clear signs of this preciously mentioned anti-fan behavior.
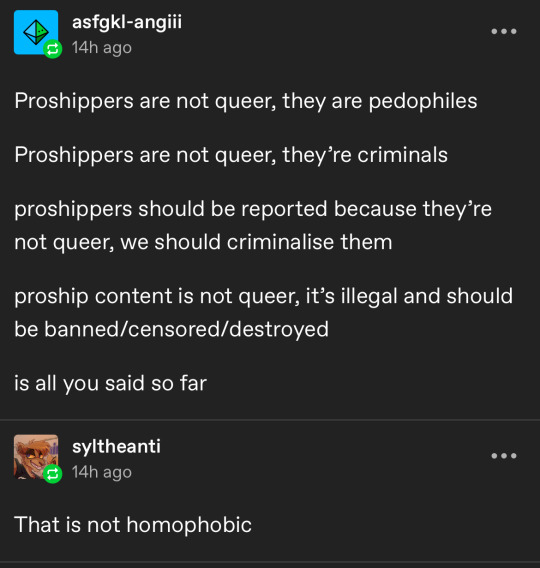
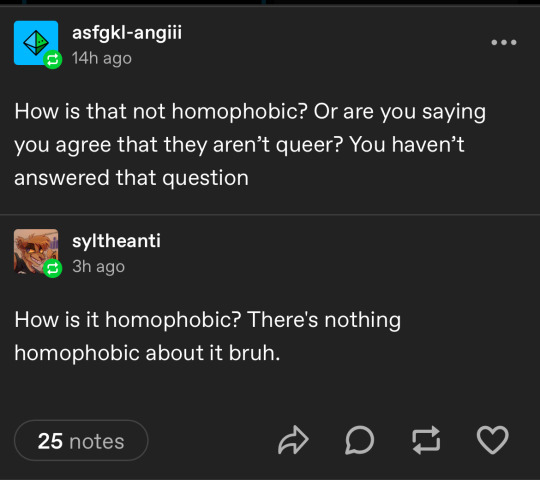
We also need to mention that all of the people within their circle want fictional characters to be treated like human people, and anyone who tells them that fictional characters do not have human rights is quickly slandered as "insane".
They are invested in denying people of their humanity, their identity and are constantly breaking their own DNI as seen in the first screenshot above. They pretend that they are just "criticizing" people, but genuine criticism does not give anyone the right to make false accusations. If you want to criticize a work posted online, you begin with analyzing it, giving your thoughts and offering improvements.
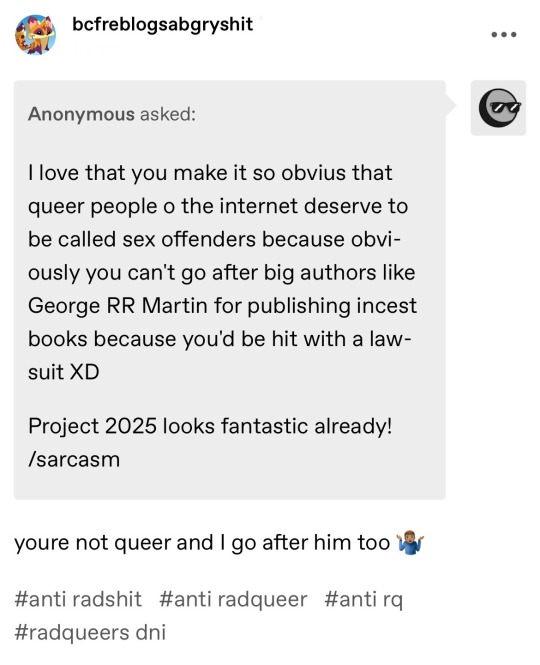
Instead, these people made clear that their goal is to attack any small fish they perceive as "different" or "weird". They have not spoken up about bigger and controversial personalities whose works have wider reach such as Colleen Hoover, George R.R. Martin, Neil Gaiman, or Maïmouna Doucouré (Director of the movie "Cuties" - which was criticized for sexualizing the cast members, most of which were young girls)
We have also looked through all of the accounts they have targeted in the past or present, and none showed any sign of worrying behavior towards or about (prepubescent) minors.
However, we are excluding people who identify as radqueer from this. We do not support them, but we believe that they should be left alone as well.
But why are these haters making these false accusations?
One of the major reasons is the concept of reciprocity: negative energy or behavior can be mirrored and reciprocated by those who encounter it.
Or simply said: haters attract hate. And haters rarely hate alone, they feel empowered when they hate the same thing together, and will encourage others into hating the same thing or people.



Hate groups form identities through symbols, rituals, myths and conspiracy theories, which enhance the members' status and, at the same time, degrade the object of their hate.
We would like to emphasize on the word "degradation". In the beginning of the post, we have described that these anti-fans deny their enemies their humanity and their identity.
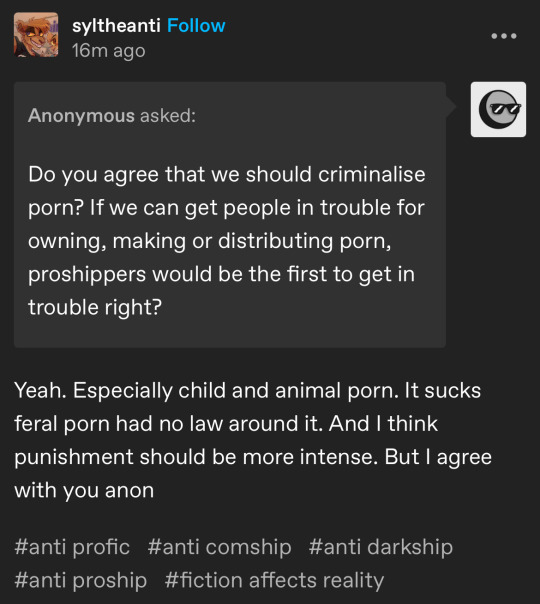
This hate group has been noticed by both anti-shippers and pro-shippers because they have decided to use the loaded term "degenerate" and its variants against pro-shippers, and continue to defend the usage of this term.

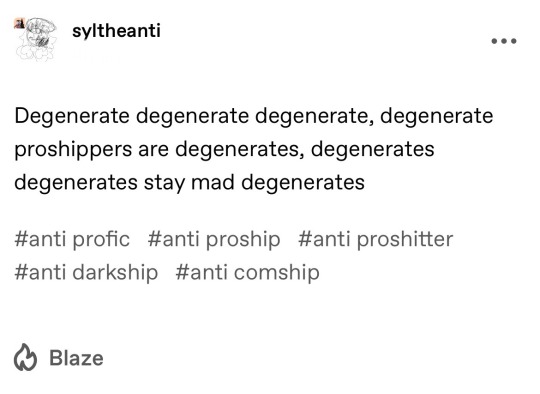
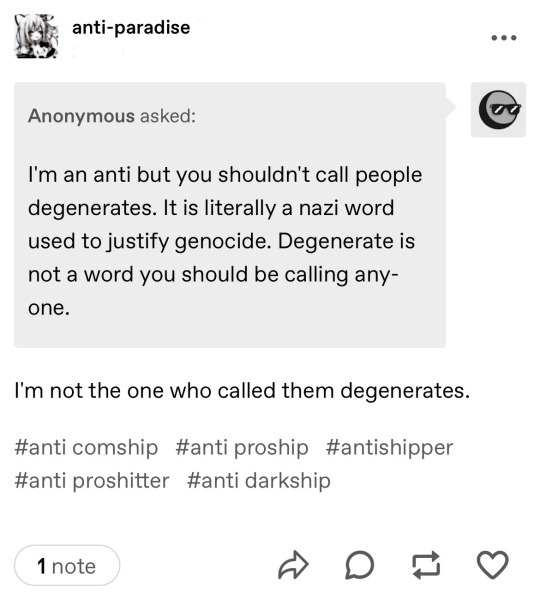
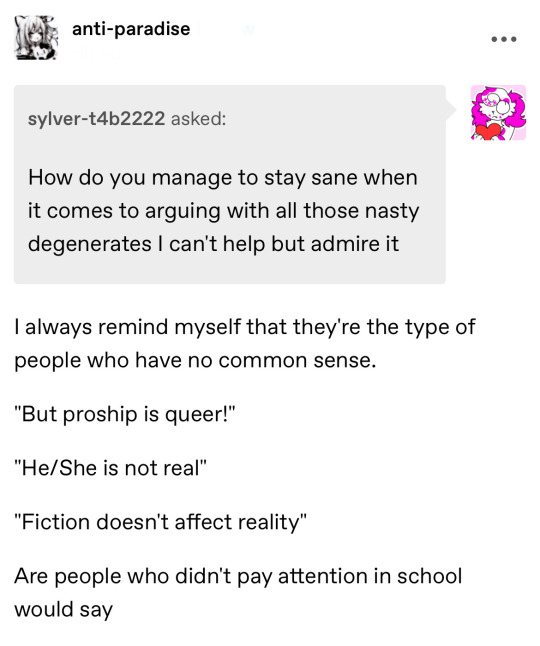
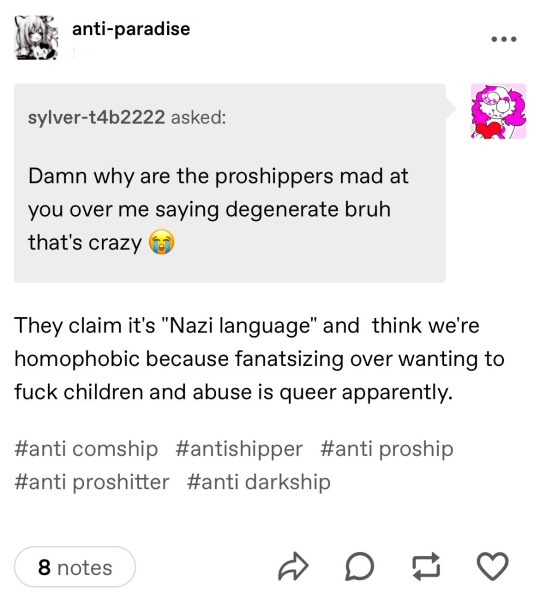
The screenshots above show that these people have been educated about the term and why they should not use it (by anti-shippers as well), but they ignored it in favor of continuing to defend and "giggle" about the controversy. It's just a "silly word" and using Nazi terms is no big deal apparently
And for those unaware, here is a small history lesson on why "degenerate" has explicit Nazi origins.
It was used centrally within their ideology since the 1920s to describe any group varying from their notion of the ideal human ("Aryan," straight, cis, etc). During the 1930s, the term was most known for the 1933 Nazi book burning (the destruction of literature considered as "Un-German") and the infamous 1937 Nazi exhibit "Degenerate Art."
Today, people like Nick Fuentes, Richard Spencer, and Donald Trump continue to use the term degenerate to attack minoritized people and political opponents.
Anyone who seriously uses the term "degenerate" is invoking Nazi ideology. When they call POC, Jews, queer/trans people, or anyone who may differ from them "degenerates," they're calling for our extermination. This is also something anti-paradise has not only "joked" about, the other hate group members supported it as well.
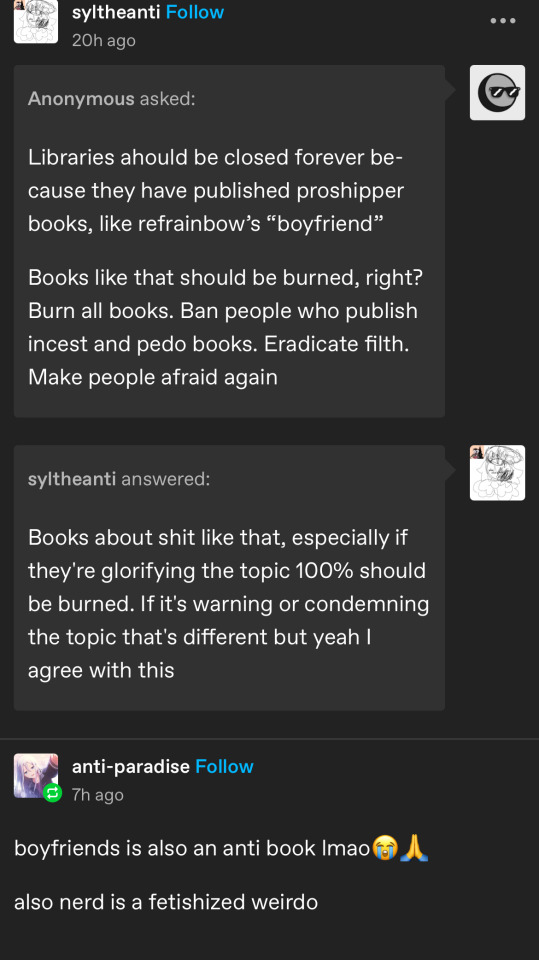

The extreme radicalization or just reactionary behavior, the need to defend open death threats, book burning, the erasure of their enemies' (proshippers) humanity, the eagerness to call them "illegal aliens" like racists call immigrants and refugees, the call to criminalize adult material, which will always affect and hurt minoritized people, the accusations that their enemies are "faking" their trauma, and denying that they are also LGBTQ+ or BIPOC/Jewish is extremely worrying.

Some people have played their behavior down as "rage bait" coming from "uneducated" teenagers, but the eagerness they display when they degrade people they hate tells, in our humble opinion, a different story. We also believe that most anti-shippers at least respect pro-shippers' basic human rights and identities - these hateful people do not.
The accounts with the random usernames and standard tumblr profile picture is the previously mentioned harasser "shoo". Most of their accounts are deactivated
Curiously enough they want to "redeem" pro-shippers of their wrongdoings, but to do that you must actually see "wrongdoers" as human. People who merely exist in their own spaces and who do not intrude in yours are not evil. People who respect internet etiquette are not criminals, nor can someone "recover" from being in favor of letting people be, even if someone ships something they dislike.
You must respect a human person on grounds of being a human if you want to redeem them.
And to be human means that no one is good or bad, we are simply people.
Secondly, these people erroneously compare being in favor of letting people ship whatever they want as long as it's fictional to a coping mechanism. But being in favor of or against ships is not a coping mechanism, and they never suggest a coping mechanism that, in their eyes, is better than adhering to fandom and internet etiquette.

We also find it quite interesting that an adult, rainbow-starheart, has come to the defense of yet another hateful person (or teenager, we are not sure), who keeps using the term "degenerate", who agreed with the intent to criminalize adult material and who called for the destruction of a queer webtoon.
Naturally we do not see issue with people disliking "Boyfriends", but just because you may not like it doesn't mean you should wish for its or any art piece's destruction.
We also have reason to believe that the hate group members do not care about copying and or indirectly supporting Republicans and their plans to harm and censor LGBTQ+ people. They most likely know who they're sounding like - and chose not to care

The screenshot above depicts the Heritage Foundation's "Project 2025"

And this screenshot is Oklahoma's new planned bill to criminalize adult material. This bill doesn't directly name trans people, it makes a reference to gay and trans people instead ("warps young people's perception of the opposite sex").
Have you noticed that the Republican Senator is calling adult material "degenerate material" and likens it to a highly addictive drug? These people also believe that one can "recover" from a nonexistent porn or sex addition despite the fact that major health organizations recognize it as a behavioral problem rather than an addiction instead.


Our belief is that people like these, despite identifying with left leaning identities and movements such as LGBTQ+, have never truly unlearned internal biases or have picked up anti-kink rhetoric and sex negativity from conservatives.
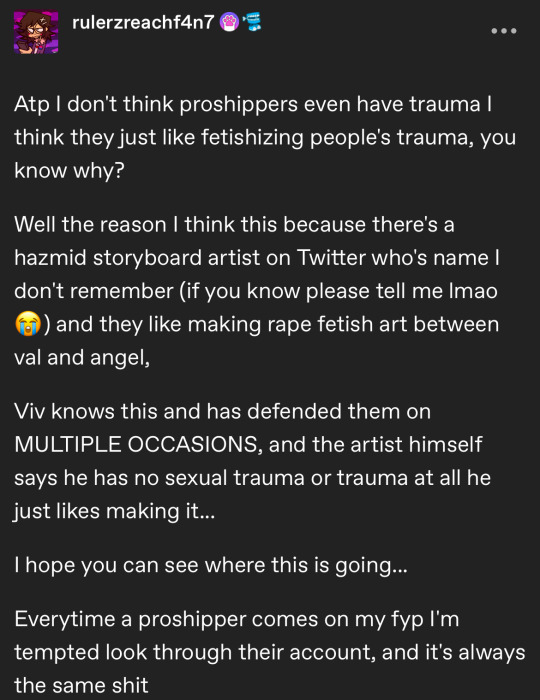
This is made evident as they only target anything related to sex, sexual assault and sexual health or kink, and associate transgressive fiction and kink with pedophilia.
The screenshot of rulerzreachf4n7's complaint about Medrano's show "Hazbin Hotel" proves this as well, to them the only problem lies in the fetishization of sexual assault. Other problematic behavior such as Val's love-bombing, violence and the manipulation of Angel is ignored.
Lastly, we are concerned that this inappropriate and concerning behavior is encouraged by another adult. We do not know how connected they are to the hate group above as they have previously never interacted with each other before until the harassment started.
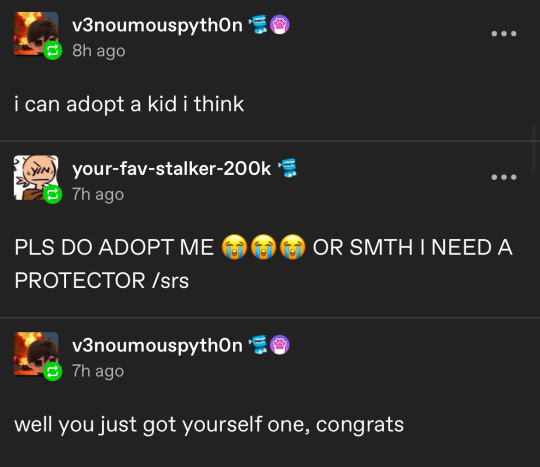
The conversation in this screenshot shows that this adult and rainbow-starheart have become "protectors" to (these) minors, and this inappropriate behavior has unfortunately been normalized in fandoms.
Do not misunderstand, we are not accusing either adult of grooming, we simply criticize inappropriate behavior some of them (may) have shown such as:
promoting anti science beliefs and encouraging youths to trust random bloggers more than medical professionals
seeking validation and emotional support from minors
posing as "one of the good ones"; a self proclaimed protector of children and the vulnerable.
showing minors 18+ material to "warn them" about certain artists
encouraging minors to openly discuss pedophilia and sexual abuse in art
casually discussing sexual topics openly or privately with minors.
reblogging public posts from or encouraging minors to publicly discuss the "ethics" of kink based on personal disgust
making themselves seem safe compared to artists who draw or write the "nasty" media they or the minors they encourage cause scenes over
bonding over how "gross" certain sexual topics are
encouraging minors to catfish people they believe to be pedophiles and or sexual predators to "expose" them or to gain evidence
encouraging minors to seek out and "criticize" adults (random strangers) about (their) kink(s)
A true "safe adult" who has the best intentions for a minor or minors would not encourage them to "make connections" to or discuss pedophilia so openly. Minors should not discuss or be encouraged to talk (to random strangers) about any of these things on a public platform, it is inappropriate and unsafe for them especially

Now we would like to finish this post with the following:
You are allowed to dislike or feel disgusted about anyone and anything, for any or no reason at all
remember that anyone can be a predator regardless of the ideology they have, the things they support or how they treat others
disgust is a defense mechanism that protects us from harm, but not everything that triggers feelings of disgust is harmful
if you are truly disgusted by someone or something, it is healthier and easier to avoid the person or the thing rather than mocking, attacking or verbally abusing the person or the thing
blocking people is not censorship, it is a tool to make your internet experience more pleasant
to any harasser/to anti-fans/to shoo: do not engage or stop engaging, move on and leave people alone
here is your chance to let this discourse finally die. Do not contribute more to it because it will affect you too
Fandoms are for many a place to escape life. Do not join fandoms if your intent is to be a hater
please do not encourage for the censorship of art in an age where this is happening again. It does not benefit you at all
remember that trauma is always dark and never clean, as such healing process of a survivor may be messy
education and information is power. Do your own research instead of blindly believing others or rumors
verdict: anti-paradise and followers are not anti harassment
#fandom#fandom discourse#anti fandom#anti-fan#antiship#proship#proship vs anti#tw death threats#tw pedophila mention#tw grooming mention#inappropriate behavior#proshippers#antishippers#far right#book burning#censorship#tw fetishization#tw harassment#tw mental health#fandom etiquette#internet etiquette#tw hazbin hotel#boyfriends webtoon#tw republican bills#anti-paradise#antiproshipconfessions
3 notes
·
View notes
Text

19 Rare Albino Animals
#memes#lol#funny#humor#mental health#adulthood#bill cipher#batman#artists on tumblr#agatha harkness#billford#gravity falls#free palestine#agatha all along#cats of tumblr#fiddleford mcgucket#animals#fauna#animal behavior#wildlife#dogs#animal friends
5 notes
·
View notes
Text
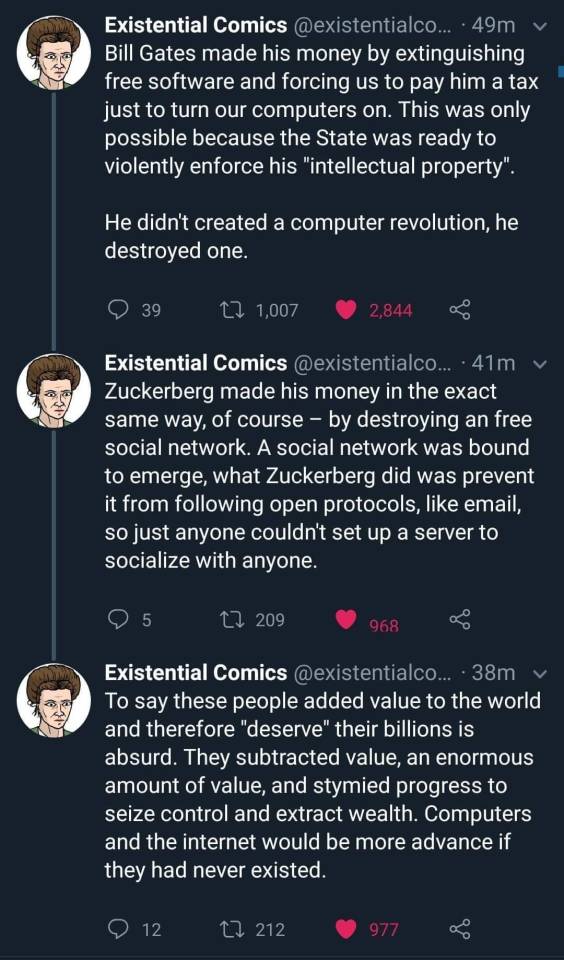
[Image captions: tweets by @existentialcomics reading as follows.]
Bill Gates made his money by extinguishing free software and forcing us to pay him a tax just to turn our computers on. This was only possible because the State was ready to violently enforce his "intellectual property". He didn't create a computer revolution, he destroyed one. Zuckerberg made his money in the exact same way, of course - by destroying a free social network. A social network was bound to emerge; what Zuckerberg did was prevent it from following open protocols, like email, so just anyone couldn't set up a server to socialize with anyone. To say these people added value to the world and therefore "deserve" their billions is absurd. They subtracted value, an enormous amount of value, and stymied progress to seize control and extract wealth. Computers and the internet would be more advanced if they had never existed.
[End caption.]
#i follow video game modding (specifically 20yo need for speed games) intently and it's fucking amazing what they're doing#like literally if you give a bunch of people relative free rein over software and tell them to go wild - the stuff they come up with is nut#like yeah you have more forking and less standardization but honestly that's a good thing for the health of projects most of the time#software#free software#bill gates#mark zuckerberg#anticompetitive behavior#monopoly#monopolism#capitalism#rentiership#enclosure of the commons
26K notes
·
View notes
Text
Innovating Mental Health Care The Critical Role of CCBHCs and EHR Integration
In recent years, the integration of technology and mental health care has transformed the way behavioral health services are delivered. At the forefront of this transformation are Certified Community Behavioral Health Clinics (CCBHCs), which provide comprehensive, high-quality care to individuals struggling with mental health and substance use disorders. Central to the success of these clinics is the adoption of advanced medical electronic record systems (EHRs), which streamline operations, enhance patient care, and ensure compliance with CCBHC certification requirements.
What is a Certified Community Behavioral Health Clinic (CCBHC)?
A Certified Community Behavioral Health Clinic (CCBHC) is a specialized facility designed to offer a wide range of mental health and substance use disorder services. These clinics are part of a federal initiative to improve access to care, particularly for underserved populations. To achieve CCBHC certification, clinics must meet stringent criteria, including the provision of CCBHC core services such as crisis mental health services, outpatient mental health and substance use treatment, and integrated care coordination.
The Importance of CCBHC Core Services
The CCBHC core services are the foundation of these clinics, ensuring that patients receive holistic and coordinated care. These services include:
Crisis Mental Health Services: Immediate support for individuals experiencing a mental health crisis.
Outpatient Mental Health and Substance Use Treatment: Ongoing care for individuals with chronic conditions.
Integrated Care Coordination: Seamless collaboration between mental health, physical health, and social services.
Screening, Assessment, and Diagnosis: Comprehensive evaluations to identify patient needs.
Peer Support and Family Support Services: Encouraging recovery through community and family involvement.
Veteran-Specific Services: Tailored care for veterans and their families.
The Role of Medical Electronic Record Systems in CCBHCs
A robust medical electronic record system (EHR) is essential for the efficient operation of a Certified Community Behavioral Health Clinic. EHRs enable clinics to:
Streamline Documentation: Automate the recording of patient information, treatment plans, and progress notes.
Enhance Care Coordination: Facilitate communication between providers, ensuring that all aspects of a patient’s care are integrated.
Improve Billing Accuracy: Simplify CCBHC billing processes, reducing errors and ensuring timely reimbursement.
Support Compliance: Maintain accurate records required for CCBHC certification and audits.
Enable Data-Driven Decisions: Analyze patient data to improve outcomes and tailor services to community needs.
CCBHC Billing and Certification Challenges
One of the most complex aspects of running a Certified Community Behavioral Health Center is managing CCBHC billing. The unique reimbursement model for CCBHCs requires clinics to bill for a wide range of services, often involving multiple payers. A sophisticated medical electronic record system can simplify this process by automating billing codes, tracking claims, and ensuring compliance with payer requirements.
Achieving and maintaining CCBHC certification also demands rigorous documentation and reporting. EHRs play a critical role in meeting these requirements by providing real-time access to patient data, generating reports, and ensuring that all CCBHC core services are properly documented.
The Future of CCBHC Mental Health Care
As the demand for mental health services continues to grow, Certified Community Behavioral Health Clinics are poised to play a pivotal role in addressing the crisis. By leveraging advanced medical electronic record systems, these clinics can enhance their efficiency, improve patient outcomes, and expand access to care.
The integration of technology into CCBHC mental health services is not just a trend—it’s a necessity. With the right tools, Certified Behavioral Health Clinics can continue to lead the way in providing compassionate.
Conclusion
The combination of Certified Community Behavioral Health Clinics (CCBHCs) and advanced medical electronic record systems represents a powerful solution to the challenges facing mental health care today. By embracing these innovations, clinics can ensure they meet
CCBHC certification standards, deliver high-quality CCBHC core services, and streamline CCBHC billing processes. Together, these advancements are paving the way for a brighter future in mental health care.
For more Info Visit https://drcloudehr.com/
#medical electronic record system#certified community behavioral health clinic#certified community behavioral health center#ccbhc mental health#certified behavioral health clinic#ccbhc billing#ccbhc certification#ccbhc core services#ccbhc program
0 notes
Text
How CCBHCs Are Revolutionizing Behavioral Health Care
The Certified Community Behavioral Health Clinic (CCBHC) program is a transformative initiative designed to improve access to comprehensive mental health and substance use disorder services. Established to address gaps in behavioral health care, CCBHCs provide a wide range of required services to ensure individuals receive the support they need. Let’s explore the core aspects of the CCBHC program, its required services, certification process, and the role of technology like EHR (Electronic Health Records) in enhancing care delivery.
What is a CCBHC?
A Certified Community Behavioral Health Clinic (CCBHC) is a specially designated clinic that offers a holistic approach to mental health and substance use treatment. The CCBHC program was created to expand access to high-quality care, particularly for underserved populations. These clinics are required to provide a comprehensive set of CCBHC required services, ensuring that patients receive integrated and coordinated care.
CCBHC Certification
To become a Certified Community Behavioral Health Clinic, organizations must meet strict criteria set by the Substance Abuse and Mental Health Services Administration (SAMHSA). The CCBHC certification process involves demonstrating the ability to provide all required services, maintain high-quality care standards, and meet specific reporting and outcome measures. Certification ensures that clinics are equipped to deliver evidence-based, patient-centered care.
The Role of EHR in CCBHCs
Electronic Health Records (EHR) play a critical role in the success of CCBHCs. An EHR for CCBHC streamlines care coordination, improves communication among providers, and enhances patient outcomes. Key benefits of EHR systems in CCBHCs include:
Integrated Care: EHRs allow for seamless sharing of information between behavioral health and primary care providers.
Efficient Billing: CCBHC billing processes are simplified through automated coding and claims management.
Data Reporting: EHRs help clinics meet CCBHC reporting requirements by tracking patient outcomes and service delivery.
CCBHC Mental Health Impact
The CCBHC model has significantly improved access to mental health services, particularly for vulnerable populations. By offering a wide range of services under one roof, CCBHCs reduce barriers to care and ensure that individuals receive timely and effective treatment. The integration of mental health and substance use services also addresses co-occurring disorders, leading to better overall health outcomes.
Conclusion
The CCBHC program represents a major step forward in behavioral health care. By providing comprehensive, high-quality services, CCBHCs are transforming the way mental health and substance use disorders are treated. With the support of EHR systems and a focus on patient-centered care, CCBHCs are well-positioned to meet the growing demand for accessible and effective behavioral health services. Whether through crisis intervention, outpatient care, or peer support, CCBHCs are making a lasting impact on communities across the nation. Visit https://drcloudehr.com/ for More Info
#ccbhc certification#ccbhc core services#ccbhc program#ccbhc required services#certified community behavioral health clinic ccbhc#ccbhc mental health#ccbhc billing
0 notes
Text
🎉 This Thanksgiving, Give Your Psychiatry Practice the Gift of Efficiency! 🍂
Attention, Pennsylvania Psychiatry Specialists! 🌟
Simplify your billing process and boost your revenue with Instapay Healthcare Services—your trusted partner for Psychiatry Health Billing in Pennsylvania.
🦃 Special Thanksgiving Offer: 👉 Special Offer on our services for a limited time! Offer ends November 30th—don’t miss out!
Why choose us? ✅ Accurate coding for maximum reimbursement ✅ Streamlined claim management ✅ Pennsylvania-specific expertise
💡 Focus on your patients while we handle the numbers!
📞 Contact us today for a FREE consultation and take the first step toward stress-free billing.
🌟 Act now to secure your savings! Let’s make this Thanksgiving truly rewarding for your practice.
Fax:- 9179607960 📞: +1(646) 851-2115 📧: [email protected]
#Top Behavioral and Psychiatry Health Billing Services in Pennsylvania#Behavioral and Psychiatry Health Billing Services in Pennsylvania#Psychiatry Health Billing Services in Pennsylvania#Best Behavioral and Psychiatry Health Billing Specialist in Pennsylvania#Pennsylvania Psychiatry Health Billing Specialist#Mental Health billing services in Pennsylvania#Psychiatry revenue cycle management services
0 notes
Text
Enhancing Efficiency with Behavioral Health Billing Services

In today’s healthcare landscape, the demand for behavioral health services has risen significantly as more patients seek treatment for mental health conditions, addiction recovery, and counseling. However, the billing process for behavioral health services is complex and often differs from traditional healthcare due to varying treatment plans, frequent patient visits, and evolving insurance policies. Medical billing services play a crucial role in ensuring that healthcare providers offering behavioral health services are accurately reimbursed. By streamlining the billing process, these services reduce errors and optimize the financial management of behavioral health practices, allowing providers to focus on patient care.
What Are Behavioral Health Billing Services?
Behavioral health billing services are specialized financial management solutions designed to meet the unique needs of providers who offer mental health, addiction recovery, and other behavioral health treatments. These services are a vital part of Revenue Cycle Management (RCM) services, which manage the entire financial life cycle of a patient’s interaction with a healthcare provider, from scheduling appointments to receiving payments. RCM services for behavioral health handle the complexities of insurance verification, claims submission, and follow-ups to ensure that healthcare providers are properly compensated for their services. Given the diverse nature of behavioral health care, these billing services are crucial for streamlining the process and preventing revenue loss.
The Importance of Medical Billing and Coding in Behavioral Health
Accurate medical billing and coding are fundamental for the financial health of any behavioral health practice. Coding for behavioral health can be particularly complex, as treatments often involve ongoing care, varying session lengths, and diverse therapeutic approaches. Improper coding can lead to claim denials or underpayments, which can severely impact a practice’s revenue. Medical billing and coding professionals ensure that all services are coded correctly according to industry standards, reducing the risk of errors and improving claim approval rates. For behavioral health providers, partnering with an expert in medical billing and coding is essential to ensure that they receive timely and accurate payments for the care they provide.
The Role of Healthcare IT in Behavioral Health Billing
The integration of Healthcare IT has revolutionized the billing process, making it more efficient and accurate for behavioral health providers. Advanced billing software and electronic health record (EHR) systems help streamline the entire process, from data entry to claim submission, while ensuring that patient records are securely stored and easily accessible. Healthcare IT reduces human error, improves communication between providers and insurers, and speeds up the billing cycle. Additionally, it provides real-time insights into the status of claims and payments, allowing providers to track and manage their revenue flow more effectively. By leveraging Healthcare IT, behavioral health practices can enhance both their financial and operational efficiency.
Behavioral Health Billing Services at Mediclaim Management
Mediclaim Management offers comprehensive Behavioral Health Billing Services tailored to meet the unique needs of mental health professionals and behavioral health providers. Our team of billing experts understands the complexities of the behavioral health field, from coding for diverse treatments to managing insurance claims for long-term care. By partnering with Mediclaim Management, behavioral health practices can reduce billing errors, increase claim approval rates, and improve their overall revenue cycle. Mediclaim Management’s Behavioral Health Billing Services are designed to handle the financial side of your practice, allowing you to focus on delivering exceptional care to your patients.
With Mediclaim Management’s Behavioral Health Billing Services, providers can rest assured that their billing processes are in capable hands. This partnership allows practices to maximize their revenue while ensuring that their financial operations run smoothly, enabling them to continue providing vital mental health services to their communities.
0 notes
Text
Overcoming the Complexities: Navigating the Challenges in Behavioral Health Billing
As the demand for mental health and substance abuse treatment services continues to rise, so does the need for efficient behavioral health billing services. Managing the intricacies of medical billing and coding for behavioral health requires specialized knowledge, from navigating complex regulations to understanding insurance policies and coverage limits. The delicate nature of mental health care and the constantly evolving healthcare landscape make the billing process challenging. Ensuring accuracy in claims submission and maximizing reimbursement through claims management services are crucial steps in maintaining a healthy revenue cycle management system for providers. Let’s explore the common challenges faced in behavioral health billing and strategies to overcome them.
Complex Medical Billing and Coding Requirements
One of the greatest challenges in behavioral health billing services is mastering the intricacies of medical billing and coding specific to mental health services. Unlike general medical billing, behavioral health codes must account for different treatment approaches, therapy sessions, group counseling, substance abuse treatments, and medication management. Each of these services requires the application of accurate CPT and ICD-10 codes to ensure proper billing.
Errors in coding can lead to claim rejections or underpayment, slowing down the provider’s cash flow. The complexity is further compounded by frequent changes in coding guidelines and payer-specific rules, creating the need for continual updates and staff training. Providers must maintain thorough documentation to support each service billed, ensuring that the codes assigned reflect the specific treatments delivered.
Frequent Claim Denials and Rejections
Mental health billing tends to face a higher rate of claim denials compared to other specialties. This is often due to the nuanced nature of behavioral health services, which can be subject to varying interpretations by insurance companies. Many insurance plans impose limits on the number of therapy sessions, types of treatments, or length of care, which can result in claim denials if not managed properly.
In such cases, denial management services play a critical role. Providers must implement robust systems for tracking claims and responding promptly to denials. Understanding the reasons for denials—whether it's due to incorrect coding, missing documentation, or authorization issues—is the first step toward correcting and resubmitting claims. A well-organized claims management services process can drastically reduce the rate of denied claims and improve overall reimbursement.
Navigating Insurance and Authorization Requirements
Insurance companies often impose strict requirements for behavioral health services, including prior authorizations and stringent medical necessity criteria. Verifying a patient’s insurance benefits and securing prior authorization before treatment begins is vital. However, this process can be time-consuming and complex, requiring constant communication with insurance providers.
Missteps in securing authorization or failing to meet insurance company criteria can lead to non-payment for services rendered. Providers must ensure that their revenue cycle management process includes a solid verification and authorization system to avoid unnecessary delays in payment. A dedicated team or service for handling prior authorizations can streamline this process, ensuring services are approved before they are delivered.
Balancing Regulatory Compliance and Patient Privacy
Compliance is another significant hurdle in behavioral health billing. Providers must adhere to strict privacy regulations, such as HIPAA, while also ensuring their billing practices comply with federal and state laws, including the Mental Health Parity and Addiction Equity Act (MHPAEA). This act mandates that mental health and substance abuse treatments be covered at the same level as physical health services, but navigating its application in different insurance plans can be challenging.
Moreover, maintaining compliance with government programs such as Medicaid and Medicare introduces additional layers of complexity. Providers participating in these programs must follow specific coding and billing guidelines, often requiring additional documentation. Failure to comply can result in audits, fines, or loss of program participation, making it crucial for providers to stay up-to-date on regulatory changes.
The Importance of Streamlined Revenue Cycle Management
Effective revenue cycle management is the backbone of any successful behavioral health practice. Managing the entire billing cycle—from patient intake and insurance verification to claims submission, payment posting, and denial resolution—requires a streamlined process to prevent cash flow disruptions. Behavioral health billing services must ensure that every step of the billing process is optimized for efficiency and accuracy.
Outsourcing these tasks to a professional billing service can alleviate many of the challenges mentioned above. A specialized billing partner can offer dedicated claims management services and denial management services, ensuring that claims are submitted accurately and promptly, denials are swiftly addressed, and reimbursement is maximized. This allows providers to focus on delivering high-quality care to their patients rather than spending time navigating the billing process.
Conclusion
In the ever-evolving field of behavioral health, the billing process presents unique and complex challenges. From mastering the nuances of medical billing and coding to managing frequent claim denials and staying compliant with regulatory requirements, providers face a host of obstacles that can affect their financial health. However, with the right strategies—such as investing in professional behavioral health billing services, utilizing denial management services, and maintaining efficient revenue cycle management—behavioral health providers can overcome these challenges, ensuring their practice remains financially healthy while delivering essential care to their patients.
By implementing these solutions, providers not only reduce the administrative burden but also improve their bottom line, allowing for more time and resources to be devoted to what truly matters: patient care.
#medical coding#healthcareclaims#claims management software#claims processing#healthcare information management#revenue cycle management#medical billing and coding#denial management services#behavioral health billing services
0 notes
Text
#behavioral health#behavioral health billing#behavioral health billing and coding#behavioral health billing services
0 notes
Text
https://myworldgo.com/blog/104072/streamlining-your-practice-the-critical-role-of-behavioral-and-mental-health-billing-services-with-instapay-healthcare

#Behavioral & Mental Health Billing Services#Behavioral & Mental Health Billing Services in US#best mental health billing services#Mental Health Billing Services#mental health services in US
0 notes
Text
Behavioral Health Billing Solutions for Optimal Reimbursement
https://optimalbillingsolutions.com/medical-billing/https://pinterest.com/pin/1044905551034376813https://www.diigo.com/item/image/ay1f0/d63qhttps://app.screencast.com/Ua55j78mCCqn0?tab=Details&conversation=W2JP1i6aV4hS5HPTV7wO8lhttps://www.pearltrees.com/optimalbillingsolutions/behavioral-reimbursement/id77667622https://ibb.co/DDcykVFhttps://www.edocr.com/user/designedbillingsolutionshttps://gravatar.com/designedbillingsolutionshttps://www.scoop.it/u/designedbillingsolutions-gmail-comhttps://hubpages.com/@optimalbillingsolutionshttps://leasedadspace.com/dashboard.phphttps://graphs.net/submit/success1/https://www.slideshare.net/slideshow/behavioral-health-billing-solutions-for-optimal-reimbursement/267694272https://www.tumblr.com/optimalbillingsolutions/749267066206502912/behavioral-health-billing-solutions-for-optimal?source=sharehttps://pinterest.com/pin/1044905551034378241https://www.behance.net/gallery/197531243/Behavioral-Health-Billing-Solutions-for-Optimal-Healthhttps://www.slideshare.net/slideshow/behavioral-health-billing-solutions-for-optimal-reimbursement-233f/267695616https://www.slideserve.com/Optimal10/behavioral-health-billing-solutions-for-optimal-reimbursementhttps://www.diigo.com/user/optimalbilling/b/745916947https://www.mediafire.com/file/th0ze4ia6xsuq68/Navigating_the_Maze.pdf/filehttps://www.pearltrees.com/optimalbillingsolutions/item592258457
#mental health billing solutions#optimal behavioral health#php billing guidelines#behavioral health billing solutions
0 notes
Text
How CCBHCs Are Redefining Access to Mental Health Services
Certified Community Behavioral Health Clinics (CCBHCs) are a groundbreaking model in the mental health and behavioral health care landscape. Established under the Excellence in Mental Health Act, CCBHCs are designed to provide comprehensive, integrated, and high-quality care to individuals with mental health and substance use disorders. These clinics are certified to meet stringent criteria, ensuring they deliver a wide range of core services to meet the diverse needs of their communities.
What is a CCBHC?
A Certified Community Behavioral Health Clinic (CCBHC) is a specially designated clinic that provides a holistic approach to mental health and behavioral health care. CCBHCs are required to offer a broad spectrum of services, including crisis mental health services, outpatient mental health and substance use treatment, patient-centered treatment planning, and integrated care coordination. The CCBHC model emphasizes accessibility, affordability, and quality, ensuring that individuals receive timely and effective care.
CCBHC Certification and Program Requirements
To become a CCBHC, clinics must undergo a rigorous certification process. This includes demonstrating the ability to provide all required services, meeting staffing requirements, and ensuring compliance with state and federal regulations. The CCBHC certification process also involves regular audits and reporting to maintain high standards of care. The CCBHC program is funded through Medicaid, making it a sustainable model for delivering mental health services.
CCBHC Billing and Funding
CCBHCs operate under a unique billing structure that allows for flexible and comprehensive reimbursement. The CCBHC billing model is designed to cover the full cost of delivering core services, ensuring that clinics can provide care without financial barriers. This model supports the integration of services, reducing fragmentation and improving outcomes for patients. For clinics looking to streamline their billing processes, solutions like DrCloudEHR offer specialized tools to manage CCBHC billing efficiently.
.Conclusion
Certified Community Behavioral Health Clinics (CCBHCs) are a vital component of the mental health care system. By offering a wide range of core services, adhering to strict certification standards, and utilizing innovative billing practices, CCBHCs ensure that individuals receive the care they need. As the demand for mental health services continues to grow, the CCBHC model stands out as a beacon of hope, providing accessible, integrated, and effective care for all. Whether it’s through crisis intervention, outpatient treatment, or peer support, CCBHCs are transforming lives and strengthening communities.
For clinics seeking to enhance their operations, tools like DrCloudEHR provide comprehensive solutions to manage CCBHC billing, certification, and service delivery efficiently. By focusing on the CCBHC program, required services, and certification process, this model is setting a new standard for behavioral health care, ensuring that no one is left behind in their journey toward recovery and wellness.
#certified community behavioral health clinic#certified community behavioral health center#ccbhc mental health#certified behavioral health clinic#ccbhc billing#ccbhc certification#ccbhc core services#ccbhc program#ccbhc required services
0 notes
Text
✨ The holiday season is here, and it's the perfect time to give your practice the gift of stress-free billing! At Instapay Healthcare Services, we handle your Mental Health Billing Services in Texas, so you can focus on what matters most: caring for your patients.
🎁 This season, let us take the burden off your plate: ✅ Accurate claim submissions ✅ Faster reimbursements ✅ Support tailored for mental health providers
💚 Your patients' peace of mind starts with yours!
📞 Contact us today to unwrap the joy of seamless billing.
Fax:- 9179607960 📞: +1(646) 851-2115 📧: [email protected]
#Top Mental Health Billing Services in Texas#Top Behavioral and Mental Health Billing Services in Texas#Texas Mental Health Billing Services#Best Mental Health Billing Services in Texas#Behavioral and Mental Health Billing Specialist in Texas#Outsourced Mental Health Medical Billing Services in Texas
0 notes