#Alzheimer’s and oral bacteria
Explore tagged Tumblr posts
Text
The Impact of Oral Microbiome on Systemic Health: A Deeper Look at How Oral Health Affects the Body
The human body is a complex ecosystem, and one of the most fascinating areas of ongoing research is the role of the oral microbiome in influencing systemic health. While most people associate oral hygiene with preventing cavities and gum disease, the truth is that maintaining a healthy mouth may have far-reaching implications beyond just dental health. Recent studies suggest that the balance of…
#Alzheimer’s and oral bacteria#Alzheimer’s disease#bacteria in the mouth#cardiovascular disease#diabetes#diabetes and oral health#gum disease#healthy mouth#heart disease#oral hygiene#oral microbiome#periodontal disease#systemic health
0 notes
Text




‘Fragile Microbiomes’ by bio-artist Anna Dumitriu
1. SYPHILIS DRESS- This dress is embroidered with images of the corkscrew-shaped bacterium which causes the sexually transmitted disease syphilis. These embroideries are impregnated with the sterilised DNA of the Nichols strain of the bacterium - Treponema pallidum subsp. pallidum - which Dumitriu extracted with her collaborators.
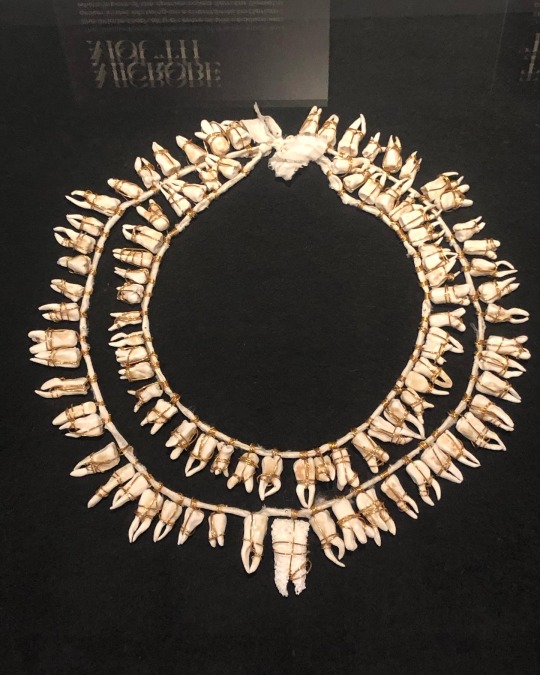
2. MICROBE MOUTH- The tooth at the centre of this necklace was grown in the lab using an extremophile bacterium which is part of the species called Serratia (Serratia N14) that can produce hydroxyapatite, the same substance that tooth enamel is made from.
The handmade porcelain teeth that make up this necklace have been coated with glazes derived from various bacterial species that live in our mouths and cause tooth decay and gum disease, including Porphyromonas gingivalis, which can introduce an iron-containing light brown stain to the glaze.
3. TEETH MARKS: THE MOST PROFOUND MYSTERY- In his 1845 essay “On Artificial Teeth”, W.H. Mortimer described false teeth as “the most profound mystery” because they were never discussed. Instead, people would hide the stigma of bad teeth and foul breath using fans.
This altered antique fan is made from animal bone and has been mended with gold wire, both materials historically used to construct false teeth (which would also sometimes incorporate human teeth). The silk of the fan and ribbon has been grown and patterned with two species of oral pathogens: Prevotella intermedia and Porphyromonas gingivalis. These bacteria cause gum disease and bad breath, and the latter has also recently been linked to Alzheimer’s disease.
4. PLAGUE DRESS- This 1665-style 'Plague Dress' is made from raw silk, hand-dyed with walnut husks in reference to the famous herbalist of the era Nicholas Culpeper, who recommended walnuts as a treatment for plague. It has been appliquéd with original 17th-century embroideries, impregnated with the DNA of Yersinia pestis bacteria (plague). The artist extracted this from killed bacteria in the laboratory of the National Collection of Type Cultures at the UK Health Security Agency.
The dress is stuffed and surrounded by lavender, which people carried during the Great Plague of London to cover the stench of infection and to prevent the disease, which was believed to be caused by 'bad air' or 'miasmas'. The silk of the dress references the Silk Road, a key vector for the spread of plague.
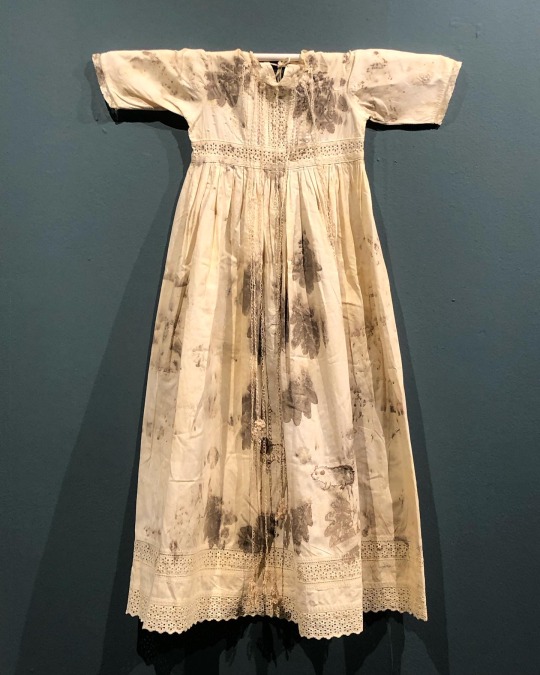
5. BACTERIAL BAPTISM- based on a vintage christening gown which has been altered by the artist to tell the story of research into how the microbiomes of babies develop, with a focus on the bacterium Clostridioides difficile, originally discovered by Hall and O’Toole in 1935 and presented in their paper “Intestinal flora in new-born infants”. It was named Bacillus difficilis because it was difficult to grow, and in the 1970s it was recognised as causing conditions from mild antibiotic-associated diarrhoea to life-threatening intestinal inflammation. The embroidery silk is dyed using stains used in the study of the gut microbiome and the gown is decorated with hand-crocheted linen lace grown in lab with (sterilised) C. difficile biofilms. The piece also considers how new-borns become colonised by bacteria during birth in what has been described as ‘bacterial baptism’.
6. ZENEXTON- Around 1570, Swiss physician and alchemist Theophrastus Paracelsus coined the term ‘Zenexton’, meaning an amulet worn around the neck to protect from the plague. Until then, amulets had a more general purpose of warding off (unspecified) disease, rather like the difference today between ‘broad spectrum’ antibiotics and antibiotics informed by genomics approaches which target a specific organism.
Over the next century, several ideas were put forward as to what this amulet might contain: a paste made of powdered toads, sapphires that would turn black when they leeched the pestilence from the body, or menstrual blood. Bizarre improvements were later made: “of course, the toad should be finely powdered”; “the menstrual blood from a virgin”; “collected on a full moon”.
This very modern Zenexton has been 3D printed and offers the wearer something that genuinely protects: the recently developed vaccine against Yersinia pestis, the bacterium that causes plague.
#my favourite pieces from this exhibition that I visited last month at the Thackray medical museum in Leeds#absolutely fascinating reading about the process and meanings behind these works#mine#anna dumitriu#works
2K notes
·
View notes
Text
Potential Health Benefits
Honey has many potential health benefits, including: (here's just a Few)…
Anti-inflammatory
Honey contains an enzyme called catalase that can help relieve minor inflammation. It can be used topically to treat burns and wounds, and orally to treat coughs and sore throats.
Antibacterial and antiviral
Honey can help fight infections caused by bacteria, viruses, and fungi. It can also be used to treat acne by dabbing a small amount onto pimples to reduce swelling and fight bacteria.
Antioxidant
Honey contains antioxidants like phenolic acids and flavonoids, which may help improve cholesterol levels and decrease the risk of heart disease. Honey can also help prevent and treat degenerative diseases.
Studies suggest that honey might offer antidepressant, anticonvulsant and anti-anxiety benefits. In some studies, honey has been shown to help prevent memory disorders. Wound care. Topical use of medical-grade honey has been shown to promote wound healing, particularly in burns.
-------
Cinnamon has many potential health benefits, including:
Blood sugar
Cinnamon may help lower blood sugar levels, which can be beneficial for people with type 2 diabetes. It may also improve insulin sensitivity and glucose tolerance factor (GTf), which can help with weight loss.
In addition to being an antioxidant, anti-inflammatory, antidiabetic, antimicrobial, anticancer, lipid-lowering, and cardiovascular-disease-lowering compound, cinnamon has also been reported to have activities against neurological disorders, such as Parkinson's and Alzheimer's diseases.
-------
Ginger has many health benefits, including:
Digestion: Gingerol, a natural compound in ginger, can help with digestion, nausea, and vomiting from motion sickness, pregnancy, and cancer chemotherapy. It can also help with mild stomach upset.
Anti-inflammatory: Ginger contains over 400 natural compounds, some of which are anti-inflammatory. It can help with bloating, gas, and reducing inflammation.
Pain relief: Ginger can help with osteoarthritis pain, menstrual cramps, and sore muscles.
Blood sugar: Ginger can help improve blood sugar regulation and lower blood sugar.
Heart health: Ginger can help lower blood pressure and cholesterol, which can help prevent heart disease. It can also improve circulation and promote the breakdown of fats in the bloodstream.
Immune system: Ginger can help strengthen the immune system and fight germs.
-------
Turmeric ~ In addition to these conditions, research studies have shown some possible benefits of turmeric for:
Inflammation
Degenerative eye conditions
Metabolic syndrome
Arthritis
Hyperlipidemia (cholesterol in the blood)
Anxiety
Muscle soreness after exercise
Kidney health
In India, it was traditionally used for disorders of the skin, upper respiratory tract, joints, and digestive system. Today, turmeric is promoted as a dietary supplement for a variety of conditions, including arthritis, digestive disorders, respiratory infections, allergies, liver disease, depression, and many others.
.......
Chili peppers contain many compounds that may have health benefits, including:
Capsaicin The chemical that gives chili peppers their heat, capsaicin may help with:
Pain relief: Chili peppers can help with headaches, migraines, and joint pain. You can apply chili peppers directly to the skin to reduce the amount of a chemical that sends pain signals to the brain.
Metabolism: Capsaicin can increase your metabolic rate, which can help you burn more calories and eat fewer unhealthy foods. Some studies have also shown that capsaicin can reduce appetite and increase fat burning, which may help with weight loss.
Inflammation: Capsaicin is one of the most studied natural ingredients for its anti-inflammatory properties.
Digestion: Capsaicin can help clear phlegm and congestion, and may promote a healthy gut microbiome, which is important for a healthy immune system.
Vitamin A and vitamin C: Chili peppers are a great source of both vitamins, which can help boost your immune system and support eye health. Vitamin C can also help your body absorb iron and promote healthy skin.
Carotenoids: Chili peppers contain carotenoids, which may help protect against cancer. Some research suggests that capsaicin may also contribute to cancer cell death.
Keep in Mind
Take charge of your health—talk with your health care providers about any complementary health approaches you use. Together, you can make shared, well-informed decisions.
Using Dietary Supplements Wisely
Know the Science: How Medications and Supplements Can Interact
Know the Science: How To Make Sense of a Scientific Journal Article
17 notes
·
View notes
Text
Periodontal disease, also known as gum disease, is a common yet often overlooked condition that affects the tissues surrounding your teeth. While many people focus on the impact periodontal disease has on their oral health, research has shown that this condition can also have significant implications for your overall well-being. In fact, gum disease has been linked to a variety of serious health issues, ranging from heart disease to diabetes and even Alzheimer’s disease. Understanding the connection between periodontal disease and overall health is crucial not only for your dental hygiene but for your general health as well.
What is Periodontal Disease?
Periodontal disease is an infection of the tissues that hold your teeth in place. It typically starts as gingivitis, a mild form of gum disease that causes redness, swelling, and bleeding of the gums. If left untreated, gingivitis can progress to periodontitis, a more severe form of gum disease where the infection spreads deeper into the tissues and can cause tooth loss.
The primary causes of periodontal disease include poor oral hygiene, smoking, genetics, certain medications, and conditions that affect the immune system. Factors like age, poor nutrition, and stress can also contribute to the development of periodontal disease. Regular dental checkups and good oral hygiene practices, such as brushing and flossing, are essential to preventing gum disease.
The Link Between Periodontal Disease and Heart Disease
One of the most significant connections between periodontal disease and overall health is the increased risk of heart disease. Studies have shown that people with gum disease are more likely to suffer from heart disease and other cardiovascular issues.
The bacteria from infected gums may enter the bloodstream, leading to an increased inflammatory response in the body. Chronic inflammation is a known risk factor for atherosclerosis (narrowing of the arteries), which can contribute to heart attacks, strokes, and other cardiovascular problems.
Diabetes and Periodontal Disease: A Two-Way Street
Diabetes and periodontal disease have a complex, bidirectional relationship. People with diabetes are more susceptible to gum disease because high blood sugar levels can weaken the immune system and make it harder for the body to fight infections, including gum infections.
The inflammation associated with gum disease can lead to higher blood sugar levels, increasing the risk of complications for people with diabetes. Research has shown that treating periodontal disease can improve blood sugar control in people with diabetes, further emphasizing the importance of maintaining good oral health in managing this chronic condition...Read More
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
The Connection Between Oral Health and Overall Health: Why Your Mouth is the Gateway to Your Body
When we think about health, we often focus on heart, brain, or muscle wellness. But did you know that your oral health plays a crucial role in your overall well-being? Your mouth isn’t just for eating and smiling; it’s a gateway to your entire body. Ignoring oral hygiene can have far-reaching effects on your general health. In this post, we explore the fascinating link between oral health and…
#Alzheimer’s and oral bacteria#dental-care#diabetes and oral health#diet#gum disease and heart disease#health#oral health and overall health#oral-health#pregnancy and dental care#respiratory infections oral health
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
What Causes Dry Mouth? Symptoms and How to Relieve Them

Do you often wake up with a parched throat or experience a sticky feeling in your mouth throughout the day? You might be dealing with dry mouth, a condition medically known as xerostomia. While it might seem like a minor inconvenience, chronic dry mouth can affect your overall oral health, leading to issues like bad breath, tooth decay, and even difficulty speaking or swallowing.
In this blog post, we’ll explore the common causes of dry mouth, why it’s important to address the issue, and how to manage it effectively.
What Is Dry Mouth?
Dry mouth occurs when the salivary glands in your mouth don’t produce enough saliva to keep your mouth moist. Saliva is essential for oral health—it helps wash away food particles, neutralize acids, and prevent the growth of harmful bacteria. When saliva production is reduced, it can lead to a dry, uncomfortable feeling in the mouth and other related symptoms.
Common Causes of Dry Mouth
There are several potential reasons why you might be experiencing dry mouth. Below are some of the most common causes:
1. Medications
Certain prescription and over-the-counter medications are one of the most frequent causes of dry mouth. Medications for allergies, colds, high blood pressure, and depression often list dry mouth as a side effect. Some of the most common types of medications that cause dry mouth include:
Antihistamines
Decongestants
Antidepressants
Diuretics
Pain medications (especially opioids)
2. Dehydration
Dehydration is a leading cause of temporary dry mouth. If your body doesn’t have enough fluids, your salivary glands may produce less saliva. This can happen if you don’t drink enough water, especially after intense exercise, or if you're experiencing vomiting, diarrhea, or fever.
3. Medical Conditions
Certain health conditions can affect the salivary glands, leading to dry mouth. These conditions include:
Diabetes: High blood sugar levels can lead to dehydration and dry mouth.
Autoimmune disorders: Conditions like Sjogren’s syndrome specifically target the salivary glands.
Parkinson’s disease and Alzheimer’s disease: Neurological conditions can interfere with saliva production.
Stroke: Damage to nerves that affect the salivary glands may result in a dry mouth.
4. Aging
As we age, dry mouth tends to become more common. This is often due to changes in health, the use of multiple medications, and reduced salivary gland function.
5. Tobacco and Alcohol Use
Smoking, chewing tobacco, and excessive alcohol consumption can all reduce saliva production, leading to dry mouth. People who use tobacco products or drink alcohol frequently are more likely to experience this condition.
6. Mouth Breathing
Breathing through your mouth, especially while sleeping, can lead to dry mouth. People who snore or suffer from sleep apnea may wake up with a particularly dry mouth in the morning. This can also be common in individuals with nasal congestion or allergies.
7. Cancer Treatments
Radiation therapy aimed at the head or neck and chemotherapy can damage the salivary glands, leading to temporary or permanent dry mouth. Patients undergoing cancer treatments often report significant dry mouth symptoms, which can persist after treatment.
Symptoms of Dry Mouth
The most obvious symptom is a dry, sticky feeling in your mouth, but there are other signs to watch out for, including:
Difficulty swallowing or speaking
A sore throat or hoarse voice
Thick, stringy saliva
Bad breath
Cracked lips
Changes in taste
Increased tooth decay and gum disease
How to Relieve Dry Mouth
Managing dry mouth often depends on its cause. Here are some general tips to help relieve symptoms:
1. Stay Hydrated
Drinking plenty of water throughout the day is one of the simplest ways to combat dry mouth. Aim for at least 8 glasses of water daily and avoid caffeinated or sugary drinks, which can make dehydration worse.
2. Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candy can stimulate saliva production. Look for products containing xylitol, a natural sweetener that also helps protect your teeth.
3. Use Artificial Saliva Products
Artificial saliva sprays, gels, and mouthwashes can help keep your mouth moist and relieve discomfort. These products are often available over the counter and can be a helpful solution for those with chronic dry mouth.
4. Avoid Tobacco and Alcohol
Cutting back on smoking, chewing tobacco, and drinking alcohol can help increase saliva production and improve your overall oral health.
5. Humidify Your Home
Using a humidifier in your bedroom can add moisture to the air, especially if you tend to breathe through your mouth while sleeping. This can reduce nighttime dryness.
6. Visit Your Dentist Regularly
Since dry mouth can increase the risk of tooth decay and gum disease, regular dental check-ups are crucial. Your dentist can recommend treatments like fluoride applications or special mouth rinses to protect your teeth.
Conclusion
Dry mouth can range from a mild inconvenience to a serious oral health issue. If you’re experiencing persistent dry mouth, it’s important to identify the underlying cause and take steps to manage it. Whether it’s adjusting your medication, staying hydrated, or seeking dental advice, treating dry mouth can improve your quality of life and keep your teeth and gums healthy.
If you're struggling with dry mouth, contact your dentist to discuss potential treatments and solutions tailored to your needs.
0 notes
Text
Comprehensive Guide to Dry Mouth Treatment: Everything You Need to Know

Dry mouth, or xerostomia, is a common condition that affects many people at various points in their lives. While it might seem like a minor inconvenience, chronic dry mouth can significantly impact your quality of life and oral health. This comprehensive guide will delve into the common topics related to dry mouth treatment, the challenges faced by those dealing with it, and a step-by-step guide to managing the condition. We'll also include a case study to provide real-life context and conclude with key takeaways.
Understanding Dry Mouth: What Is It?
Dry mouth occurs when the salivary glands in your mouth don't produce enough saliva to keep your mouth moist. This can be due to various reasons, including certain medications, medical conditions, lifestyle choices, and even aging. Saliva is crucial for maintaining oral health as it helps in digestion, protects teeth from decay, and prevents infection by controlling bacteria and fungi in the mouth.
Common Causes of Dry Mouth
Medications: Hundreds of medications, including over-the-counter drugs, can cause dry mouth. Common culprits include antihistamines, decongestants, pain relievers, diuretics, and medications for hypertension and depression.
Medical Conditions: Diseases like diabetes, Alzheimer's, Parkinson's, and Sjogren's syndrome are often associated with dry mouth.
Lifestyle Choices: Smoking, chewing tobacco, and excessive alcohol consumption can contribute to dry mouth.
Aging: As we age, our salivary glands may not work as effectively.
Symptoms of Dry Mouth
A sticky, dry feeling in the mouth and throat
Frequent thirst
Sores or split skin at the corners of the mouth
Cracked lips
A dry, rough tongue
Mouth sores
Bad breath
Difficulty chewing, swallowing, or speaking
Challenges in Managing Dry Mouth
Managing dry mouth can be challenging due to the diverse causes and symptoms associated with the condition. Here are some common challenges:
Identifying the Cause
One of the biggest challenges is identifying the underlying cause of dry mouth. With so many potential triggers, pinpointing the exact cause can be difficult, often requiring a comprehensive medical evaluation.
Finding Effective Treatment
Another challenge is finding an effective treatment. What works for one person may not work for another, and it can take time and experimentation to find the right solution.
Lifestyle Adjustments
Making lifestyle changes to manage dry mouth can be challenging. This might include quitting smoking, reducing alcohol intake, or changing medications, all of which require commitment and support.
Psychological Impact
Chronic dry mouth can have a significant psychological impact. It can affect your self-confidence, especially if it leads to bad breath or difficulty speaking.
Step-by-Step Guide to Managing Dry Mouth
Step 1: Hydration is Key
Drink Plenty of Water: Keeping yourself well-hydrated is the first and most straightforward step. Sipping water throughout the day can help keep your mouth moist.
Use a Humidifier: Using a humidifier, especially at night, can add moisture to the air and help with dry mouth.
Step 2: Stimulate Saliva Production
Chew Sugar-Free Gum: Chewing sugar-free gum or sucking on sugar-free candies can help stimulate saliva production.
Eat Moist Foods: Include foods with high water content, such as fruits and vegetables, in your diet.
Step 3: Avoid Irritants
Reduce Caffeine and Alcohol: Both can dehydrate your body and contribute to dry mouth.
Quit Smoking: Smoking can reduce saliva production and exacerbate dry mouth symptoms.
Step 4: Oral Care Routine
Brush and Floss Regularly: Maintaining good oral hygiene is crucial. Use fluoride toothpaste and brush at least twice a day.
Use an Alcohol-Free Mouthwash: Alcohol-based mouthwashes can dry out your mouth further. Opt for a mouthwash specifically designed for dry mouth.
Step 5: Medical Interventions
Consult Your Doctor: If you suspect your medication is causing dry mouth, consult your doctor. They may adjust your dosage or prescribe an alternative.
Prescription Medications: In some cases, doctors may prescribe medications that stimulate saliva production.
Case Study: Overcoming Dry Mouth - Sarah's Story
Background
Sarah, a 45-year-old woman, began experiencing chronic dry mouth symptoms about a year ago. She noticed a persistent dry feeling in her mouth, difficulty swallowing, and bad breath. These symptoms started affecting her daily life and confidence.
Diagnosis
After visiting her dentist and primary care physician, Sarah was diagnosed with xerostomia. Her doctors determined that her dry mouth was likely caused by a combination of her antihypertensive medication and her habit of drinking several cups of coffee daily.
Treatment Plan
Medication Adjustment: Her doctor adjusted her antihypertensive medication to one less likely to cause dry mouth.
Lifestyle Changes: Sarah reduced her coffee intake and started drinking more water throughout the day.
Oral Care Products: She began using an alcohol-free mouthwash and sugar-free gum to stimulate saliva production.
Outcome
Within a few months, Sarah noticed a significant improvement in her symptoms. Her mouth felt less dry, and her confidence returned. By making these changes and sticking to her new routine, Sarah successfully managed her dry mouth.
Conclusion
Dry mouth is a common condition that can significantly impact your quality of life. However, with the right treatment plan and lifestyle adjustments, it is manageable. By understanding the causes, recognizing the symptoms, and following a step-by-step guide, you can effectively manage dry mouth and improve your overall oral health. If you suspect you have dry mouth, consult your healthcare provider to determine the best course of action for your specific situation.
0 notes
Text
What Causes Dry Mouth?

Understanding Dry Mouth: Causes, Challenges, and Solutions
Dry mouth, or xerostomia, is a condition that affects many people, causing discomfort and potential health issues. It can interfere with daily activities such as speaking, eating, and swallowing. In this blog post, we will explore what causes dry mouth, discuss common challenges, provide a step-by-step guide to managing the condition, and present a case study to illustrate real-life impact and solutions. Let’s dive in to understand this condition better and discover effective ways to alleviate it.
What Causes Dry Mouth? The Key Factors Everyone Should Know
Dry mouth occurs when the salivary glands in your mouth don't produce enough saliva to keep your mouth moist. Understanding the causes of dry mouth is essential for finding the right treatment and management strategies. Here are some common causes:
1. Medications
A variety of medications can cause dry mouth as a side effect. These include:
Antihistamines
Decongestants
Pain relievers
Diuretics
Antidepressants
Medications for high blood pressure
2. Aging
As we age, our bodies undergo various changes, including reduced saliva production. Older adults are more likely to experience dry mouth due to medications, health conditions, or changes in the body's ability to process medications.
3. Cancer Therapy
Radiation treatment for cancers of the head and neck can damage salivary glands, leading to decreased saliva production. Chemotherapy drugs can also change the nature and amount of saliva produced.
4. Nerve Damage
Injuries or surgeries that cause nerve damage in the head or neck area can result in dry mouth.
5. Lifestyle Choices
Habits such as smoking or chewing tobacco can affect saliva production and contribute to dry mouth. Alcohol and caffeine consumption can also lead to dehydration and reduce saliva flow.
6. Health Conditions
Several health conditions are associated with dry mouth, including:
Diabetes
Sjogren's syndrome
HIV/AIDS
Alzheimer's disease
Stroke
7. Dehydration
Not drinking enough fluids can lead to dehydration, which is a common cause of dry mouth. This can occur due to fever, excessive sweating, vomiting, diarrhea, blood loss, or burns.
Challenges of Living with Dry Mouth
Living with dry mouth presents several challenges that can affect your quality of life. These challenges include:
1. Difficulty Eating and Swallowing
Saliva plays a crucial role in the initial stages of digestion. Without adequate saliva, chewing and swallowing can become difficult and uncomfortable.
2. Speech Problems
Dry mouth can make it hard to speak clearly. Saliva helps to keep the mouth moist, facilitating smooth movement of the tongue and lips necessary for speech.
3. Oral Health Issues
A lack of saliva can lead to an increased risk of cavities, gum disease, and oral infections. Saliva helps to neutralize acids produced by bacteria in the mouth, wash away food particles, and provide disease-fighting substances.
4. Taste Alterations
Dry mouth can affect your sense of taste, making it less enjoyable to eat and drink. This can lead to changes in appetite and nutritional deficiencies.
Step-by-Step Guide to Managing Dry Mouth
Managing dry mouth involves a combination of lifestyle changes, medical treatments, and home remedies. Here’s a step-by-step guide to help you manage this condition effectively:
1. Stay Hydrated
Drink plenty of water throughout the day.
Avoid beverages that can dehydrate you, such as alcohol and caffeinated drinks.
2. Use Saliva Substitutes
Over-the-counter saliva substitutes can help keep your mouth moist.
Use mouthwashes designed for dry mouth, which can provide moisture and protection.
3. Chew Sugar-Free Gum
Chewing sugar-free gum can stimulate saliva production.
Choose gums that contain xylitol, which can also help reduce the risk of cavities.
4. Maintain Good Oral Hygiene
Brush your teeth at least twice a day with fluoride toothpaste.
Floss daily to remove food particles and plaque from between your teeth.
Visit your dentist regularly for check-ups and professional cleanings.
5. Avoid Tobacco and Alcohol
Quit smoking and avoid chewing tobacco.
Limit or eliminate alcohol consumption to reduce its dehydrating effects.
6. Use a Humidifier
Using a humidifier in your bedroom can help keep the air moist, which may alleviate dry mouth symptoms, especially at night.
7. Adjust Your Diet
Eat soft, moist foods that are easier to chew and swallow.
Avoid salty, spicy, and acidic foods that can irritate a dry mouth.
8. Medications and Medical Treatments
Talk to your doctor about your medications. They might adjust your dosage or switch you to a different medication that doesn't cause dry mouth.
For severe cases, medications that stimulate saliva production, such as pilocarpine or cevimeline, may be prescribed.
Case Study: Managing Dry Mouth Successfully
Case Study: Emily's Journey with Dry Mouth
Emily, a 55-year-old woman, began experiencing dry mouth after starting medication for her high blood pressure. She noticed difficulty eating, speaking, and an increase in dental problems. Emily sought help from her dentist and primary care physician to manage her condition.
Initial Challenges:
Emily had trouble chewing and swallowing food, which affected her nutrition.
She experienced frequent mouth sores and bad breath.
Her speech was often unclear due to a lack of moisture in her mouth.
Steps Taken:
Hydration: Emily increased her water intake, carrying a water bottle with her at all times.
Saliva Substitutes: She started using over-the-counter saliva substitutes and a mouthwash designed for dry mouth.
Chewing Gum: Emily chewed sugar-free gum, which helped stimulate her saliva production.
Oral Hygiene: She followed a strict oral hygiene routine, brushing and flossing diligently.
Diet Adjustments: Emily adjusted her diet to include more soft, moist foods and avoided irritants like spicy and acidic foods.
Medical Consultation: Her doctor adjusted her medication dosage, which helped reduce the severity of her dry mouth symptoms.
Results:
Emily noticed a significant improvement in her ability to chew and swallow food.
Her mouth sores and bad breath decreased.
She felt more comfortable speaking, and her speech became clearer.
Emily’s journey highlights the importance of a comprehensive approach to managing dry mouth, involving hydration, the use of saliva substitutes, chewing gum, maintaining oral hygiene, and making dietary adjustments. Medical consultation played a crucial role in adjusting her medication and reducing symptoms.
Conclusion
Dry mouth is a common condition that can significantly impact your quality of life. Understanding what causes dry mouth, recognizing the challenges it presents, and implementing effective management strategies are essential for alleviating symptoms and maintaining oral health. By staying hydrated, using saliva substitutes, chewing sugar-free gum, maintaining good oral hygiene, and consulting with your doctor, you can manage dry mouth effectively.
Emily’s case study illustrates how a combination of these strategies can lead to successful management of dry mouth symptoms. If you experience persistent dry mouth, it’s important to seek professional advice to identify the underlying cause and receive appropriate treatment. With the right approach, you can improve your comfort, oral health, and overall well-being.
0 notes