#Acromioclavicular Joint Sprain
Text
Putting this in a pinned post to make it easy to find/share. We all know how Tumblr is about things (and to be fair, I'm terrible and inconsistent as hell with tags).
Link to the "shoulder release" document:
Notes about this guide:
This is a WIP, and still very much in the rough draft phase. Please forgive typos/errors. I literally haven't done a single edit yet.
The document focuses on releasing shoulders as a way to treat neck tension and migraines. Seriously, just trust me. It helps.
Carpal tunnel? Tennis elbow? Golfer's elbow? AC (acromioclavicular) joint injury? Rotator cuff problems? Tight upper back? Sporadic numbness in your arm? Seriously, just try the muscles already listed. You'll likely find at least some relief. Like, if it involves the upper body, release your shoulders.
I've done my best to make this able to be understood by people without massage training. So if it seems like it's covering really "obvious" info, that's intentional. Just skip the section if you already know things.
A lot of massage therapists may balk at me telling you to dig around in your own armpit. We're taught in school to avoid the area. Why? Because there's a crap ton of nerves and blood vessels there. *Which is precisely why releasing this area is so powerful.* There's also a ton of muscle (on yes, basically everybody) here that will protect all those structures. It's honestly really safe so long as you stick to "In pain, refrain!" And read the other rules too.
90% of the time, the culprit is one of the four muscles listed (or any combination of them). If you are someone who exercises a lot/does yoga/is otherwise pretty physically active, you are more likely to fall into the 10% of people who will have their issue somewhere else/it will just be really hard to find. So bear that in mind.
Sadly, this sort of thing will probably never be a "one and done" type of deal. Most of the things we do every day steadily build up to cause problems, and you have to constantly work to undo that entropy. So save these notes for future you.
And just in case you want to know what the hell qualifies me to make this sort of document, here are my "quals."
My first career attempt was nursing. While this did not go well (doctors don't really appreciate autistic students willing to question their authority) I learned a shit ton about the body. I became a student teacher for the anatomy and physiology class because I was so good at it (and that professor used to teach the pre-med students). A&P is now literally one of my special interests.
8 years as a licensed massage therapist focused exclusively on injury therapy. I studied Rolfing techniques, and primarily used trigger point therapy, structural integration, and myofascial release as my tools. Clients liked to joke that going to see me was like seeing the physical therapist (they weren't wrong).
Some of the stuff I share is literally self taught through "following the tension" in clients bodies. Like, I developed some of my protocols. And then practiced and refined them over 100s of bodies. The goal was always the most efficient and least painful way to achieve lasting release.
I eventually destroyed my shoulder doing massage (which was injured long before this career due to an AC joint sprain gotten when I was 20). Bonus, this means I'm *very* practiced at releasing my own shoulders.
I'm now a mechanical engineer, which just means I now have the engineering knowledge to understand to the force transferrence patterns I saw in clients all the time. Kinesiology is the same thing as statics and dynamics.
Hopefully that helps put perspective into things. I'll update this post as new versions of the document come out. I have a ton on my plate right now (who am I joking; I always have a ton on my plate), so please be patient waiting for updates.
#massage#active release techniques#shoulder release#migraine treatment#self massage#trigger point therapy
30 notes
·
View notes
Text
Understanding the Different Types of Ligament Reconstruction Procedures

Ligament injuries are common, often resulting from sports-related activities, accidents, or repetitive strain. When ligaments tear or become damaged, they can significantly impact mobility and stability. Ligament reconstruction procedures are surgical interventions aimed at restoring function and stability to affected joints. Understanding the various types of ligament reconstruction procedures is crucial for patients and healthcare professionals alike.
Types of Ligament Reconstruction Procedures:
Anterior Cruciate Ligament (ACL) Reconstruction:
The ACL is one of the most commonly injured ligaments in the knee. ACL reconstruction involves replacing the torn ligament with a graft, typically sourced from the patient's own tissue (autograft) or a donor (allograft). Common autograft options include the patellar tendon, hamstring tendon, or quadriceps tendon. Allografts are often sourced from cadavers. Surgeons use arthroscopic techniques to perform ACL reconstruction, minimizing tissue damage and promoting faster recovery.
Posterior Cruciate Ligament (PCL) Reconstruction:
PCL injuries are less common than ACL injuries but still require surgical intervention in severe cases. PCL reconstruction aims to restore stability to the posterior aspect of the knee joint. Similar to ACL reconstruction, surgeons utilize grafts to replace the damaged ligament. The choice of graft material depends on factors such as patient age, activity level, and surgeon preference.
Medial Collateral Ligament (MCL) Reconstruction:
MCL injuries often result from direct impacts or sudden twisting motions. While conservative treatments suffice for many cases, severe tears may require surgery. For optimal care, reach out to an orthopedic hospital in Indore. MCL reconstruction entails repairing or replacing the damaged ligament to restore stability to the inner knee. Surgeons may employ grafts or synthetic materials to reinforce the MCL, ensuring proper healing and preventing instability.
Lateral Collateral Ligament (LCL) Reconstruction:
LCL injuries are less common than MCL injuries but can occur due to trauma or overuse. LCL reconstruction aims to restore stability to the outer aspect of the knee joint. Surgical techniques involve repairing or replacing the damaged ligament with grafts or synthetic materials. LCL reconstruction may be performed in conjunction with other knee ligament surgeries to address multiple sources of instability.
Ankle Ligament Reconstruction:
Ankle ligament injuries, particularly involving the lateral ligaments, are prevalent among athletes and individuals with a history of ankle instability. Ankle ligament reconstruction typically targets the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). Surgeons may utilize tendon grafts or synthetic materials to reconstruct the damaged ligaments, restoring ankle stability and preventing recurrent sprains.
Shoulder Ligament Reconstruction:
Shoulder ligament injuries, such as those affecting the glenohumeral ligaments or the acromioclavicular (AC) joint, can result from sports-related trauma or repetitive overhead activities. Shoulder ligament reconstruction aims to restore stability and function to the shoulder joint. Surgeons may perform procedures such as Bankart repair for anterior shoulder instability or AC joint reconstruction for AC joint separations. Grafts or synthetic materials may be used to reinforce the repaired ligaments, promoting long-term stability.
Recovery and Rehabilitation:
Recovery from ligament reconstruction surgery varies depending on the specific procedure performed and individual factors such as age and overall health. Following surgery, patients typically undergo a structured rehabilitation program aimed at restoring strength, flexibility, and range of motion. Physical therapy plays a crucial role in the recovery process, helping patients regain functional mobility and prevent future injuries.
Ligament reconstruction procedures are crucial in restoring stability and function to joints affected by ligament injuries. Whether it's the knee, ankle, or shoulder, there are various surgical techniques available to address different types of ligament damage. Both patients and healthcare professionals need to understand the intricacies of each procedure to make informed decisions and achieve the best possible outcomes. With advancements in surgical techniques and rehabilitation protocols, ligament reconstruction is continuously evolving, providing patients with the chance to regain mobility and resume their active lifestyles. If you're seeking consultation with an orthopaedic surgeon in Indore, they can guide you through the process and help determine the most suitable course of action for your specific needs.
#best orthopedic doctors in indore#best orthopedic doctor in indore#best department of orthopedics in indore#department of orthopedics in indore#orthopedics treatment in indore#best orthopedics treatment in indore#orthopedics hospital in indore#best orthopedics hospital in indore#multispeciality hospital in indore#city nursing home in indore#best hospital in indore#hospital in indore
0 notes
Text
What steps should individuals in South Delhi take when experiencing shoulder pain, and how does consulting the best shoulder pain doctor contribute to accurate diagnosis and effective treatment for conditions like shoulder sprains?
In South Delhi, individuals experiencing shoulder pain, potentially stemming from a sprain or dislocation, should seek the expertise of the best shoulder pain doctor. The acromioclavicular joint is often affected, leading to pain, swelling, and altered shoulder shape. Sporting activities with repetitive overhead arm movements elevate the risk. Medical evaluation includes a physical examination and imaging tests for an accurate diagnosis.
#BestShoulderpainDoctorinSouthDelhi#ElbowreplacementinWestDelhi#ElbowFractureTreatmentinSouthDelhi#WeightliftershoulderrepairinWestDelhi#WeightLiftersbankartrepairinWestDelhi#ArthroscopicRotatorcuffrepairinSouthDelhi
0 notes
Text
AC (Acromioclavicular) Joint Pain in Manhattan, NY

The AC joint, or acromioclavicular joint, is the junction where the clavicle, or collar bone, attaches to the shoulder blade. This joint is a small joint that can be felt over the top of the shoulder especially if there has been a previous injury. The AC joint is stabilized by ligaments that can be injured by a direct fall onto the front or top of the shoulder. This type of injury is called an AC joint sprain or separation. It can vary in severity and cause pain that is made worse with shoulder motion or when pressure is applied over the joint.
read more
0 notes
Link
0 notes
Text
𝐓𝐡𝐞 𝐁𝐞𝐚𝐭 𝐨𝐟 𝐘𝐨𝐮𝐫 𝐇𝐞𝐚𝐫𝐭
Summary: Despite Y/N’s blood status and House, she happens to be the only witch in the entirety of the wizarding world that Draco gives the time of day. A fellow Healer, close confidant, and dare he say, best friend, she’s always managed to make his life exceedingly tolerable, particularly when he finds himself thrust into a weekly gathering or dinner that his parents have set up to find him a suitable wife. But when an accident threatens to tear the two apart, it matters not what Draco is feeling, because the fate of their friendship and their future relationship lies in the beat of Y/N’s heart.
Warnings: Mentions of injuries and blood
Pairing: Healer!Draco x Muggleborn!Reader
Genre: Angst | Fluff
Word count: 4.5K
All Masterlists | Draco Malfoy Masterlist

𝐓𝐡𝐞 𝐰𝐡𝐞𝐞𝐥𝐬 𝐨𝐟 𝐟𝐚𝐭𝐞 𝐰𝐞𝐫𝐞 𝐚 𝐩𝐚𝐢𝐧 𝐢𝐧 𝐭𝐡𝐞 𝐚𝐬𝐬, 𝐭𝐡𝐚𝐭 𝐦𝐮𝐜𝐡 𝐃𝐫𝐚𝐜𝐨 𝐤𝐧𝐞𝐰 𝐟𝐨𝐫 𝐬𝐮𝐫𝐞. No different than the sickening feeling of anticipation at the sight of the revolving roulette almost coming to an end or the tingling sensation of doubt when faced with the final choice in wizard poker. The man was beyond certain that misfortune would always find a way to strike him long before he had the chance to think of victory.
Tired and exhausted from the patient he had the displeasure of overseeing, he puffed out the air wedged in his lungs, heading to the comfort of his office. Once there, Draco threw the clipboard and files he held on the desk, wasting no time to slump in his chair. He craned his neck, attempting to relieve some of the pain while his fingers swiftly moved to untie the fabric of his tie.
Just when he took a deep breath, ready to relax, he grumbled in displeasure at the sound of someone knocking on his door. Draco rubbed his tired eyes with his palms, looking up at the white lights illuminating his office. “This better be good,” he whispered to himself before calling in whoever was behind the mahogany door.
The door creaked as the person behind it pushed it open, causing Draco to make a mental note to fix the bloody sound before it drove him mental. A Healer peeped her head inside, a crooked smile governing her lips. “Hey, grumpy dwarf. What’s got you all worked up?”
Draco shook his head with an amused smirk, the tension he harbored slowly evaporating. “Y/N,” he greeted the witch, his stormy eyes following her every step once she closed the door behind her and strolled inside. “Kindly never compare me to a dwarf ever again. We both know that you tick every box when it comes to that description.”
Y/N feigned hurt, placing a hand on her heart. “Oi, you’re mean! But then again, you do make a more fitting Snow White.”
“I have no idea who that is.” Draco laughed at her remark without taking his eyes off her. He watched her gracefully sit on his desk, frivolity nestling comfortably in her big doe eyes.
“It doesn’t matter as long as I know what that is,” Y/N teased. She kicked her legs in the air, her eyes skimming over the mess of papers and files on Draco’s desk. With curiousness in her gaze, she reached out for the file closest to her. “Harry Potter? Three broken ribs, flail chest, concussion, fractured hip, and–”
“Acromioclavicular joint sprain, yes,” Draco continued.
Y/N’s brows knitted as she read over the patient file. “Must have been one bloody fight. Literally.”
Draco chuckled in response. He took the file from her hands, reaching for his quill. “It wasn’t exactly a walk in the park admitting Auror Potter here.” He dipped the quill in the onyx ink bottle, beginning to add his own notes on the papers.
Y/N eyes wandered to Draco, studying his figure. She crossed her hands over her chest, peering at him. “Is that what’s got your knickers in a twist? That he’s here, and you had to treat him?”
Draco didn’t spare Y/N a look, but from the way he had stopped writing, she figured he must’ve rolled his eyes. “No. Treating him was far easier than expected. It was having to listen to the whines of the Weaslette and Granger, among other things. That was the most irritating part of it all.”
Y/N leaned back to get a better look at Draco. She shook her head at his statement, drumming her fingers on the table. “Aren’t you a tad bit exaggerating, perhaps?”
“On the contrary. As if seeing Potter wasn’t dreadful enough, it was exceptionally irksome having to be in the presence of the other two witches.”
“Well, Hermione is his best friend,” Y/N argued, trying to reason with the blond. “And wasn’t Ginny his fiancee? Or did he not propose yet?”
“In case you’ve missed it, darling. I’m a Healer, not an editor at Witch Weekly or The Daily Prophet,” Draco cynically replied, waving his quill in the girl’s face.
Y/N huffed at his response. She took out a pile of papers, spewed lazily on his desk, and hit him with it on the head. Draco winced, shooting daggers at Y/N. “You’re a pompous arse.”
“Is there a reason for you being in my office other than to continuously insult me?”
“Yes,” Y/N replied with a smirk. “To grace you with my presence.”
Draco blinked, attempting to hide the glint of amusement swirling in his irises. “How charming,” he told Y/N, continuing to fill Harry’s file.
Y/N kept her focus on Draco, watching as his fingers moved around, gracefully guiding the feather on top of the parchment. Mesmerized by the sight, and falling to the realization that she had been silent for too long, she loudly cleared her throat. “Why are you bothered so much? Did they say something bad? Please don’t tell me they refused to have you as Harry’s Healer because of it.”
“No,” Draco rushed to say, sensing the worry in Y/N’s tone and feeling a slight itch on his left forearm. “No, darling. They never said anything about that. It was just hard to concentrate with them breathing down my neck.”
Y/N half-laughed, her shoulders looking less rigid. She played with the papers on the desk, her eyes narrowing at the Healer in front of her. “Come on, Draco. Plenty of people have done that too when their loved ones were in our care.”
“Well, then. Perhaps people need to learn to control their emotions in times of distress.”
Y/N raised an eyebrow in disbelief. “Not everyone is an established Occlumens like yourself. I may be a Healer, but I know I’d lose my composure if someone I cared about entered the doors of St. Mungo’s all bloodied and bruised.”
Draco rolled his eyes indignantly. He didn’t have enough energy to argue with Y/N, and knowing her, she would be about ready to argue all night. For two days straight if she had a drop of coffee in her system. So, Draco decided that it would be best to change the subject.
“So.” He cleared his throat, taking his eyes off the files. “Care to tell me about how your day went? Hopefully it was better than mine.”
Y/N’s facial expressions changed, the light that was once in her eyes dimming. It was then Draco noticed the black circles beneath her eyes and the tiredness that lingered on her face.
“It… was okay, I guess. I just have a night shift today, which I’m not looking forward to.”
“Right,” Draco hummed as he remembered. “My offer still stands, you know? I’d be more than happy to take your place.”
Y/N bit on her lower lip, her gaze flickering straight to Draco’s. He watched her carefully, his own silver orbs glued to her teeth as she chewed on her lip to contain a laugh. But eventually, Y/N had failed miserably and ended up clutching her stomach, chuckling aloud.
That woman is unbelievable. Draco mentally thought, watching as tears streamed down Y/N’s cheeks from the sincerity of her laughter.
“You got roped into another dinner with a potential wife, didn’t you?”
“No,” Draco scoffed incredulously, running away from Y/N’s burning gaze. He looked at his left, which was perhaps a wrong move because he caught Y/N’s eyes in the mirror. “Yes. Now, stop looking at me like that!”
“Like what?” Y/N feigned innocence, her lips contorting into a bashful smile.
“Like you’re trying to get into my head.”
“Don’t be ridiculous. I can’t do that. I’m not a Legilemens.”
You don’t need to be one, Draco mentally fired back, but he never dared to say it aloud. “The point is, you look like you could use a break while I could use an excuse. So, why don’t you let me handle your shift?”
“Because you’re going to have to admit to your parents that you’re above all this, Draco,” Y/N explained, seemingly more serious than she ever was before. “And if not tonight, then when?”
Draco groaned, rubbing the back of his neck. “It’s not easy, and you know that.”
“Yes, fairly well, too. I may not be a pureblood, but my parents are as strict as muggles come.”
“At least yours don’t have a list of suitors as party guests,” Draco said, cringing at the thought of the many women he had met and had yet to meet as per his parents’ demands.
Y/N merely rolled her eyes as a response to his behavior. And knowing her, she was starting to get annoyed. “Need I remind you that the last time I spoke with them, they had attempted to set me up with some ostentatious muggle prick of their choosing?” Y/N spat, a flicker of pain outlining her irises. “I don’t exactly live up to the Y/L/N name with me being a witch and all.”
Draco closed his eyes as he let out a breath. How stupid of him to forget such a massive detail. He moved out of his chair and towered over Y/N, his stormy silver eyes roaming her figure. Draco’s hands cupped her cheeks, and before he knew it, he was kissing the crease that formed between her brows.
“I’m sorry, darling. It’s not you that doesn’t live up to that last name. It’s that last name that doesn’t do you justice.”
Y/N’s mouth twitched, Draco’s words tugging at her heartstrings. She blinked, looking down at her feet as she attempted to hide the pink tint that formed on her cheeks. “Thank you,” she whispered meekly, looking up at Draco from underneath her lashes.
Draco’s hands lingered on Y/N’s rosy cheeks for a moment, losing themselves in the softness and warmth of her skin. Eventually, his hands fell back to their place.
“You sure you don’t want me to fill in for you?” Draco asked. “Even if it’s just for a bit? It looks like you could use some sleep.”
Y/N pursed her lips in thought, beginning to fiddle with the fabric of her green coat. “As enticing as this sounds, I’ll pass. I’ll just take a power nap and get back to work then.”
“Fine. If you insist.”
Draco left Y/N sitting on his desk and moved to the other side of the room. He rummaged through one of his cabinets, and judging by the fact that he spent a good minute or so searching for whatever it was he was looking for, Y/N figured he had placed an Extension Charm on it.
“What are you looking for?” she wondered aloud, curiously trying to see what it was that Draco was looking for.
A beat passed before Draco pulled out what appeared to be a white blanket from the drawer. He moved with steady steps toward his couch on the left side of the room, dropping the blanket. He quirked an eyebrow, gesturing to the couch. “Well, what are you waiting for?”
Y/N’s eyes sparkled. She hopped down from the desk, making her way to the makeshift bed with a lopsided smile, her eyes fixed on silver hues that were as magnetizing as the night sky. “Forget Snow White.” She took off her shoes and nestled herself comfortably on the couch as Draco draped the blanket over her body. “You’re my own fairy godmother.”
“I have no idea what that is either,” Draco replied. His fingers twitched as he got the urge to brush the hair out of Y/N’s face. But before he got the chance to do it, she moved her hand to her face and placed the stray strands behind her ears.
Y/N closed her eyes, tugging the blanket higher. “That’s your loss.”
Draco looked away, his eyes alight with mirth–a sight that only Y/N could paint with her simple presence. He took his wand from the pocket of his coat, waving it around to turn the lights off. “Don’t sleep too much.” Draco placed a gentle kiss on Y/N’s forehead, admiring the way her long lashes lifted to expose her crystalline eyes. “I’ll send you a Patronus to make sure you wake up.”
“Enjoy dinner, Draco,” Y/N called, closing her eyes and surrendering to a much-needed sleep.
Draco stood by the doorframe, watching her drift to sleep. “Sweet dreams, darling.” He gently closed the door and walked down to the hospital’s apparition point, looking forward to get this pathetic dinner over and done with so that he could laugh about it the next day with Y/N.

To say that dinner was a complete catastrophe would be an understatement. It was an utter debacle. Draco’s parents didn’t settle for setting him up with a potential pureblooded wife. They went as far as attempting to sever relationships to secure him one.
Lucius and Narcissa Malfoy desperately tried to match him with his Hogwarts classmate and friend Daphne Greengrass. However, their perpetual attempts at laying the red carpet for Daphne and creating utopian scenarios were proven futile when Draco disclosed that his potential wife was already involved in a relationship.
And when his parents had found out that she was dating a halfblood, they tried to convince Mr. and Mrs. Greengrass to consider a betrothal between the two families to strengthen ties and remain within the bounds of the sacred twenty-eight.
When the Greengrasses refused to entertain this notion, Draco was sure that whatever his parents were planning next was going to be disastrous. He had already rejected the idea of courting his best friend Pansy Parkinson. At this rate, the next candidate was either going to be Millicent Bulstrode or his parents were going to wait for the birth of Avery’s daughter to wed her to Draco when she becomes of age.
It was seven in the evening when Draco opened the door to his office, sauntering in with a steamy cup of coffee in his hand. His eyes couldn’t help but travel to the couch, finding the blanket that Y/N was covered with neatly folded.
He smiled, an image of Y/N’s sleeping figure popping into his head. He decided to leave the blanket, knowing that she was most likely going to need a nap sometime during the day, considering she was spending hours on end at the hospital.
A knock echoed in Draco’s ears, causing him to slightly wince. Whoever was assaulting the door, he was sure wasn’t Y/N. “Yes?” he sighed, leaning back against the chair and placing his hands on the armrests. His door creaked open as another Healer walked in.
“Healer Malfoy,” his colleague, Healer Abbott, greeted. She walked further inside the office with papers in her hand.
“Abbott,” Draco nodded, eyeing the papers. “What’s that you got?”
“A couple of papers that need your signature. They’re discharge orders for Auror Potter.”
Draco’s nose wrinkled in disgust. “He was just admitted yesterday.”
Healer Abbot pursed her lips, extending the papers. “I’m well aware. Except that he says he doesn’t require our services anymore.”
That bloody wanker. “Believe me, Abbott. I want him out of this establishment far more than he does,” Draco admitted. He pushed back the papers that the Healer brought, looking for Harry’s file. “But even ‘The Chosen One’ doesn’t have the healing abilities of a bloody phoenix. I’m going to need someone to check on him, preferably Y/N if she’s here or coming in later.”
Healer Abbott shook her head. “Healer Y/L/N is not coming in today.”
“Why?” Draco asked, not recalling Y/N having told him that she’s taking the day off.
“She had a particularly long shift yesterday. From what I heard, Head Healer Malachai told her to get some rest today.”
“Fine,” Draco sighed, handing Healer Abbott Harry’s file. “He’s your responsibility until I get back. Don’t let him out of your sight.”

“For the last time, Mrs. Hoffman. I’m not interested in courting your granddaughter.”
“Well, it’s a shame to hear you say that, dearie,” the old woman said. She looked up at the young Healer, her brown eyes shifting color when touched by light. “Such a handsome young man like yourself deserves a charming young witch by their side.”
“Perhaps, but not as young as your granddaughter,” Draco replied. He let his focus back on the clipboard he was holding onto, jutting down notes based on the diagnostic charm he casted on Mrs. Hoffman a few minutes ago.
“She’ll be of age in just a few months time.”
Draco quirked an eyebrow, his squill scratching against the parchment. “And when will that be exactly?”
Mrs. Hoffman’s eyebrows knitted in focus. She tapped her index finger against her chin, trying to remember the exact date of her granddaughter’s birthday. Draco waited patiently for her to answer, holding his breath as he counted down the seconds. “I have no clue.”
“Do you at least remember her name?”
Mrs. Hoffman looked confused. “Who’s name, dearie?”
Draco sighed, marking down the new information on his clipboard. While the witch didn’t seem to be making too much progress, her state was much better than Lockhart’s. Draco winced as he remembered that buffoon, thankful that he was someone else’s responsibility and not his. The last time the Head Healer assigned him Lockhart, the man tried to convince him to frame one of his autographed headshots. The man might’ve been dealing with permanent memory loss, but even a charm as strong as Obliviate never managed to wipe out his narcissism or his putrid attitude.
Draco bid his goodbyes to Mrs. Hoffman, promising to check on her again tomorrow. He closed the door behind him, strolling down the corridor to check on his other patients. As soon as he exited the Fayette Barlowe Ward, he found himself almost tackled to the ground by one of his colleagues.
“Abbott, what the bloody hell is wrong with you?” Draco snarled, holding Healer Abbot by the elbows.
The Healer stepped back, trying to catch her breath. “Malfoy,” she exhaled, placing one hand on her heart. “I’ve been searching the entirety of St. Mungo’s for you!”
Draco looked her up and down, his nose scrunching. “What do you want that’s so urgent?”
“We need you for an emergency surgery.”
“And why exactly is that? The last time I checked, this institution is overflooding with Healers, so why is it that you need me in particular?” Draco watched as Healer Abbot shifted uncomfortably in place. Her eyes darted from side to side, trying their best to avoid being caught by Draco’s silver hues. “Don’t tell me it’s bloody Potter again. I swear if–”
“It’s Healer Y/L/N,” the woman blurted, looking remorseful. “She’s in a critical state and needs immediate medical attention.”
The world tilted on its axis without prior warning, causing a sudden static noise to echo in Draco’s ears. The Healer paled, stricken by fear as he watched with dazed and frantic eyes the woman in front of him. “Y/N?” he whispered. Without waiting for an answer, Draco made a mad dash toward the Operations Ward, pushing and screaming at anyone who stood in the way. With a shaky breath and unsteady heartbeats, he pushed the doors of the ward open. “Where the bloody hell is Healer Y/L/N?”
“In here, Healer Malfoy,” one of the junior Healers called.
Draco threw his clipboard and quill aside, urgently moving to assess Y/N. “Preliminary diagnostic results?” he asked, his eyes skimming over her frail figure.
Y/N’s skin was ashen, even paler than his own. A trail of blood hugged the side of her forehead, oozing from a large gash that taunted Draco. Her long lashes met together, keeping her eyes away from sight. The veins on her eyelids ice blue like frozen constellations engraved on her skin. Her chest barely rose and fell, her figure appearing almost dead.
Draco hurried to press his fingers against the side of her neck, next to her Adam’s apple, checking with unsteady fingers for any sign of a pulse. He searched for a good couple of seconds, holding his own breath to make sure his thundering hope wouldn’t be deceiving him.
“Concussion, Bradycardia, Pneumonitis.”
“Fuck,” Draco breathed as he hurried to place the pulse oximeter on Y/N’s finger. His eyes hurried to check the value, his heart falling to the pit of his stomach when it showed 88%. “Hypoxemia.”
“Healer Malfoy,” Healer Bones said, her eyes switching between Y/N and Draco. “What’s the best course of action to take now?”
Draco gulped. He swayed on his feet, his hands rushing to grab the bars around Y/N’s bed. Blood rushed to his head, invading all his senses. A tumultuous surge of fear and trepidation froze him in place.
The sight of Y/N’s lips turning blue with every beep from the ECG monitor caused him to lose his mind. A hot and scorching sensation shot through his whole body, rendering him unable to do anything but internally scream.
He attempted to occlude all those thoughts of Y/N being covered by a white cloth and taken away from him, but no matter how much he tried to compartmentalize, he found himself failing miserably.
Healer Bones leaned over Y/N’s frail body, slightly obscuring her from sight. “Healer Malfoy?” she asked, loud and clear. Concern was evident in her eyes along with a look of distress.
Suddenly, Y/N’s voice rang in Draco’s ears. ‘I may be a Healer, but I know I’d lose my composure if someone I cared about entered the doors of St. Mungo’s all bloodied and bruised.’
His fear almost caused him to rush out the doors of the Operations Ward and request for another Healer to come and heal Y/N before it was too bloody late. But a part of him couldn’t let her out of his sight. When the ECG monitor beeped continuously, indicating that Y/N’s already scarce heartbeat was coming to a stop, something snapped in Draco.
“Bones, administer muggle CPR to Y/N at once. Elliot, clear her airways, Abbott, do something about that concussion, and leave the rest to me.” Draco took out his wand, pointing it at Y/N’s chest, watching with a sweaty forehead the ECG monitor while everyone began to tackle their assigned tasks. “You’re not dying on me, darling. Or else you’ll be giving me a reason to commit the crime I was once too bloody petrified to go through.”

Y/N’s eyelids felt heavy, as if something was weighing them down. Her chest constricted, pain surging through her veins all the way to her heart when she breathed too hard. The darkness behind her eyelids was too much to bear. The possibility of never opening her eyes again caused her to fight for the light she wished to feel.
Her fingers twitched, involuntarily at first. But as soon as she felt someone’s soft fingers curled around hers, she fought the feeling of numbness that immobilized her. With great effort, she moved her fingers once more. She could feel the chill that sparked through her body, recognizing the familiar metal of a ring against her skin. “Draco,” she whispered, the hand that held hers intertwining their fingers together.
“Y/N, darling.” A voice said, sounding hoarse. “Open your eyes for me.”
She followed after the voice like a lovesick teenage girl following after her crush. Y/N clung to the softness of that voice, its mellifluous sound carrying itself in her ears. She suddenly found herself opening her eyes to the world, infinite possibilities unveiling before her as though she was just reborn.
Clearing her throat, she craned her neck to the side, finding her favorite pair of silver eyes already staring at her. “Hey, dragon.” Y/N smiled, losing herself in the feeling of ecstasy that governed her senses when a laugh escaped his lips. “Fancy seeing you here.”
“You are unbelievable, witch. You almost die, and that’s the first thing that comes out of your mouth when you wake up?” Draco asked, absentmindedly tracing stars on Y/N’s skin.
“I missed you. Is that better?”
“Much better,” Draco grinned, gazing at the witch who inhabited his mind. He moved his hand to touch her cheek, letting his fingers trail across her slightly heated skin. Y/N closed her eyes, humming in contentment at the magic that coursed through her blood due to Draco’s touch. “I love you.”
Y/N eyes shot open, afraid that she was diving too deep into the feeling to find the shore. But when she laid her alert eyes on Draco, she found him smiling at her with nothing but sheer adoration in his eyes. “I’m sorry. I think I misheard you.”
“No, you didn’t,” he replied swiftly, keeping a tight hold on her hand. His heartbeats thundered in his chest as love rippled in his very core. “I love you. Not as a friend, not as a sister. As the one person that made my world crash and burn when they wheeled her into the bloody Operations Ward.”
“Draco, where’s all that coming from?” Y/N said, her other hand reaching to cradle her bandaged head, attempting to fight the dizziness that threatened to rip her away from this moment.
Draco looked her in the eye, feeling his knees weaken at the sight of the universe that unveiled before his own silver orbs. “When I heard that you were caught in that bloody attack, and when I saw you lifeless on that bed, Y/N, I almost died.”
“You… you what?”
“I almost died,” he admitted. “Out of fear, despair, anger. Out of every dark emotion out there. Because… because you’re the reason I’m so alive, Y/N. You are, and always have been, the one person that makes me forgo of every bit of control I foolishly assume I hold when in your presence.”
“Draco,” Y/N breathed, a single tear falling from the edge of her lashes. “Do you mean that?”
“Yes. I’ve never meant anything more than this.”
Y/N smiled, her tears welling up with more tears. She reached for Draco’s face, cradling his cheeks. “I love you too, Draco Malfoy. With every beat of my heart.”
Draco captured Y/N’s lips in his, melting against the sweetness of her blazing touch. He smiled, capturing her bottom lip and nibbling slightly on it, feeling the whole world fall into place. Maybe fate wasn’t such a pain in the ass; maybe it was even appealing. Because Y/N’s kisses made him believe in fate–in a world where everything was right, and all the stars were aligned just for them.
-----------------------
taglist: @marajillana
I absolutely loved this request and was so excited to work on it!
For those who want to be tagged, head over to “The Owlery” section on my profile and send me a message! If you wish to send me a request, then simply click on "Requests." 🤍
Now, what do you think this witch is brewing next? 🪄
Help me decide between another mini-series, a one-shot, or maybe a request! Comment what you want to see next.
#draco malfoy x reader#draco x reader#draco x y/n#draco x you#draco malfoy fanfiction#harry potter fanfiction#draco malfoy#draco malfoy x y/n#draco malfoy x you#draco imagine#draco malfoy imagine#healer!draco#healer!draco x y/n#draco x muggleborn!reader
656 notes
·
View notes
Text
Physical Therapy Modalities and Alternative Methods in Treatment of Soft Tissue Lesions _ Crimson Publishers

Physical Therapy Modalities and Alternative Methods in Treatment of Soft Tissue Lesions by Elizabeta Popova Ramova* in Crimson Publishers: Peer Reviewed Orthopedic Research Journals
Purpose: To present the role of physical therapy and some alternative medicine methods to improve recovery after soft tissue muscles skeletal trauma in athletes and physical active people.
Introduction: Soft tissue injuries are common in physical active people, vary from minor to major complex trauma. Soft tissue injuries include sprains, strains and bruising. Any soft-tissue injury can lead to a tenderness, swelling, haematoma, scarring, fibrosis and loss of function. In the next few days after injury, we can greatly improve recovery time by taking medicaments that decrease inflammation and speed healing. The case of treatment in PH&Reha is soft tissue injuries of muscles skeletal system. There are onlower limb(ankle, knee, hip), the other on the shoulder (dislocations, acromioclavicular joint injuries, rotator cuff injuries), elbow and wrist.The aims of physical therapyare to relieve pain, control inflammation, hasten resolution of a haematoma, and accelerate repair, to restorate function and recovery muscle power.
Discussion: There are a variety of choices available which can provide specific and individualized results. Integration of conservative treatment and surgery with physical therapy, can decrease a time of rest and inactivity. The physical therapy has used follow physical therapy modalities: Light therapy, electro therapy, sonotherapy, hydro therapy, cold and warm applications, with proved effect. However, once the injury is stabilized, patient should take an alternative treatments for ssoft tissue injuries like acupuncture, masasage, functional taping, and herbal therapy from medicaments to greases.
Conclusion: Modern Physical therapy can improve fast recovery and functional impairment, on science base, with physical therapy modalities and alternative medicine methods. Evaluation of effect of treatment can be with ultrasonography, and clinical test and scores.
For more Open access journals in Crimson Publishers please click on below link https://crimsonpublishersresearch.com/
For more article in Peer Reviewed Orthopedic Research Journals please click on below link https://crimsonpublishers.com/oproj/
0 notes
Text
Best Shoulder Pain Treatment
If you are experiencing shoulder pain, you may be wondering what to do. Genesis orthopedics provides Best Shoulder Pain Treatment. The Internet has an abundance of self-directed material pertaining to shoulder physical therapy, but oftentimes these self-directed approaches fail to address the underlying problem. Before undergoing shoulder physical therapy, you should get a proper diagnosis from Genesis near Chicago. We'll be the first to tell you if shoulder physical therapy is the best next step (surgery is always the ultimate last resort). The problem is that shoulder physical therapy sometimes isn't enough, and you can't figure out how to fix it without a clear diagnosis. At Genesis Orthopedics and Sports Medicine we treat following elbow conditions: Acromioclavicular joint sprain, Adhesive capsulitis, Bicep tendon tear, bicipital tendonitis, Impingement syndrome , Instability syndrome of the Glen humeral joint, Labrum Tears, Rotator Cuff injuries or tears, Shoulder fractures, Shoulder instability or dislocation and Sub acromial bursitis.

0 notes
Text
How I Got Trigger Finger and What I Did to Treat It
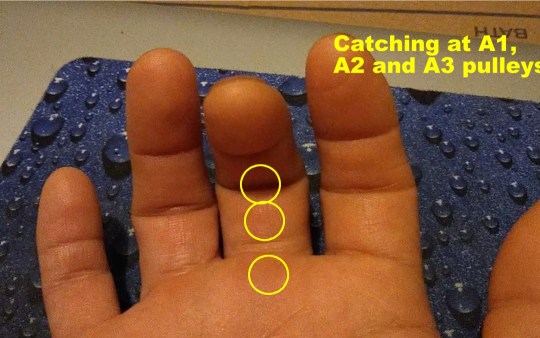
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
It’s been a while since my last article. Between the weekly-changing COVID restrictions in my area and major house renovations, I have been delinquent with my life mission of helping others manage and heal their pain and injuries, on their own. But today, I’m back on track. Today, I’ll talk about a peculiar condition known as Trigger Finger.
But first, a little background:
For those who ever engaged in do-it-yourself home renovations such as landscaping, fence building, paver-laying and bathroom and kitchen remodeling you know how much stress it can put on your body. This is my story of how I developed trigger finger for the first time in my life, and serves as a “lessons learned” opportunity for others so that they can be spared the inconveniences of this condition..
For the last 10 years, I would categorize my daily physical activity as “moderate.” I would go the gym and lift free weights (reps over max); do various cardio fitness classes such as the Les Mills classes and Bootcamp; and run 3 miles about 3x/week. My average time in the gym I would say was 60-90 minutes, with about half of that actual exercising. At home, I would be working on my website and producing videos. This did require prolonged sitting, but I would get up every 30 minutes or so to walk around to relieve pressure to my lumbar spine.
Starting the second week of this past July, I started the aforementioned home renovation projects. I basically went straight from moderate activity to short bursts of sustained intense activity, daily for over four weeks. Since I didn’t have any major musculoskeletal impediments other than a chronic right AC (acromioclavicular) joint sprain, I moved freely as though I was in my 20s, which wasn’t such a good idea. The combination of the intense movement patterns my body wasn’t used to, plus my age, took a significant toll after four weeks.
Here are some of the heavy labor activities that I engaged in:
Carrying heavy lumber from Home Depot and loading into a pickup truck, about 10 trips
Carrying 50 and 80 pound bags of concrete mix and sand, for my paver project, about 5 trips.
Used a 2-person auger (about 120 pounds; gasoline powered) to drill several 3’ deep post holes
Shoveled piles and piles of dirt (pickup truck loads—about 10x)
Hauled away bulk trash to the dumpster
Carried 100 clay 12”x12” paver squares (bricks) from a truck to my yard and positioned them carefully
Used hand tools that required hard gripping and/or twisting including various types of saws, wrenches and screwdrivers
Used vibrational tools including a miter saw, reciprocating saw, drill, and nail gun
By the third week, I was starting to feel pain at my right AC joint, my left wrist, and both hands especially my right, dominant hand. Thankfully, despite frequent bending at the waist my lower back wasn’t affected. I attributed the AC join pain to aggravation of the old strain (I rate it a Grade 2 or 3 sprain – partial tearing, but intact). What happened is the heavy lifting placed a repetitious load on that unstable joint, causing the acromion and distal clavicle to aggravate surrounding soft tissues, particularly the supraspinatous tendon, and the insertion points of the ligament. My doctor suggested my pain was impingement syndrome—compression of the supraspinatous tendon where it passes below the acromion– which could be occurring, but I’m certain most of the pain is emanating from the joint itself because I can reproduce the pain simply by pressing it with my fingertip. I’ll tell you how I’m treating this in the next article.
I believe my left wrist pain is a Grade 2 strain of the flexor ulnaris tendon where it inserts into the distal ulnar’s styloid process; caused when I lost control of the auger. The auger is a very powerful machine that requires two people to operate (see picture above). Not being familiar with using one, I wasn’t prepared for the powerful torque it generated, and lost control of it, hurting my wrist.
The third problem that I’m dealing with is trigger finger. This is the first time I’ve had it and let me tell you, it’s not very pleasant.
Trigger finger is so named because as you attempt to straighten out your finger after closing your hand, the finger “catches” mid-way, and pain is felt in one or several joint capsules usually on the palmar side. Then, as you power through the restriction the pain increases and a popping/snapping sensation occurs right before it straightens out, just like how a gun trigger offers gradual resistance then suddenly releases at a point. See the short video below of my actual trigger finger taken this morning that explains this.
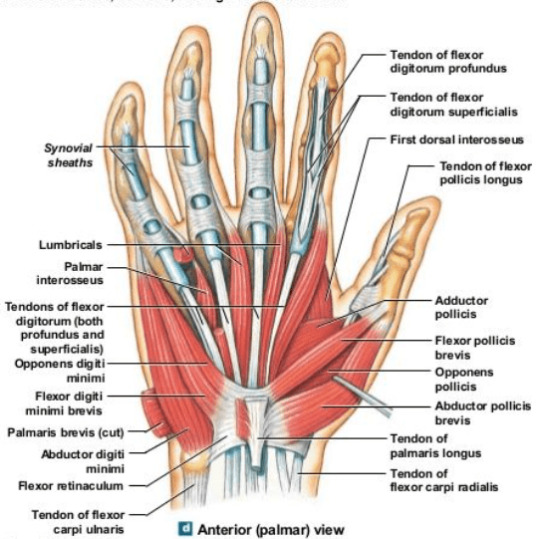
Trigger finger is a stenosing tenosynovitis disorder. Stenosing means narrowing of a passageway in the body; tenosynovitis refers to inflammation of the tendon and synovium. The synovium is a specialized layer of tissue surrounding the tendon in areas where it rubs against other structures in the body. Synovium secretes synovial fluid, a biological lubricant that helps reduce friction where the tendon moves. Synovium also lines the synovial joints of the body which include the hips, knees, shoulders, elbows, spine and joints of the hands and feet.
There are three, main populations of trigger finger sufferers: young children (up to 8 years old); trigger finger as a comorbidity to a primary disease; and adults experiencing trauma/ stress to the hands, typically in the 40s-50s. It tends to affect women more, and the most common finger is the thumb although it can occur in any finger, and in multiple fingers at the same time.
In children, trigger finger is believed to be due to uneven growth rates of the hand flexor tendons and the ligaments, where the tendon growth outpaces the growth of the ligaments that hold them against the finger bones.
Trigger finger is observed to often occur alongside certain other diseases such as carpal tunnel syndrome, diabetes, hypothyroidism, gout, rheumatoid arthritis, and amyloidosis; each probably having different etiologies involving the dysfunction causing the primary disease. Diabetics seem to be affected by trigger finger at a higher rate than the regular population, and it is uncertain why. With diabetes mellitus, there are high levels of glucose in the blood, and usually high insulin levels. Insulin is considered an anabolic hormone associated with tissue growth, so this may be a possible explanation for the increased incidence of trigger finger in diabetics, if the growth leads to tendon hypertrophy (enlargement).
For the third group, which the rest of this article will address, trigger finger is caused by hypertrophy and inflammation of the finger flexor tendons at the synovial sheath, typically from repetitious hand movements, especially those involving power gripping and vibration, making them chafe against the ligaments that hold them down to the finger bones (phalanges). (Remember, ligaments connect two bones, while tendons connect a muscle to a bone; both are components of all moveable joints). Imagine these ligaments as slips of Scotch tape forming a tunnel over the bone. As the hypertrophied (enlarged) section of the tendon enters the narrow tunnel during extension (straightening out of the finger), it gets stuck in that tunnel momentarily; much like how a big person trying to climb out of a small bathroom window can get stuck before being able to make it through. Then, as the tendon makes it past that entrance, it causes the popping sensation.
Orthopedic specialists identify the tendon-ligament structures involved in hand movement as pulleys. Remember from basic physics, a pulley is one of the simple machines (the others being a lever, plane and gear). This is an appropriate name because the tendons and ligaments accomplish work just like the cables and pulleys used in cranes.
Image courtesy of OrthoBullets.com
The A1 pulley is at the metacarpo-phalangeal joint, commonly called the knuckles. It’s where the proximal phalanx connects to the respective metacarpal bone. This is where trigger finger usually occurs. Those who have it here feel the pain and popping/snapping on the palmar side of the knuckle.
The A2 pulley encircles the proximal phalanx, or first finger bone, from the knuckle.
The A3 pulley is at the PIP, or proximal interphalangeal joint—the first joint from the knuckle connecting the proximal and intermediate phalanges (first and second bones of the finger). This is also a common area of trigger finger.
The A4 pulley encircles the intermediate phalanx (second bone of the finger from the knuckle).
The A5 pulley is at the DIP, or distal interphalangeal joint, the furthest joint of the finger connecting the intermediate and distal phalanges (second and third bones of the finger, from the knuckle). Although triggering can happen here, it is less common.
Since the thumb is comprised of only two phalanges, it has an A1 and A2 pulley only. Trigger finger affecting the thumb almost always occurs at the A1 pulley. Unlike the other fingers, your thumb can move in multiple planes, much like the shoulder joint. It has a unique pulley called the oblique pulley that allows it to touch the pinky, a movement called thumb opposition.
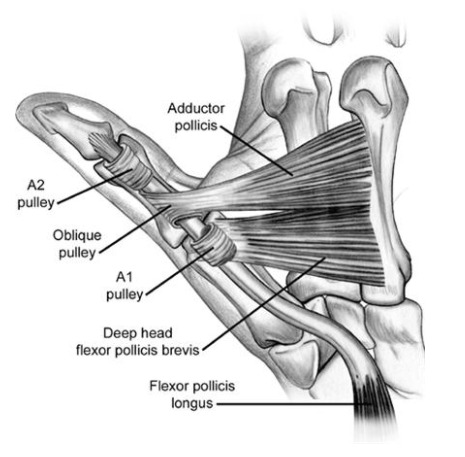
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
1 note
·
View note
Photo

Shoulder Sprain (Acromioclavicular (AC) Joint Separation) and Shoulder Strain: https://iamaprilphillips.com/welcome/shoulder-sprain-acromioclavicular-ac-joint-separation-and-shoulder-strain/
The shoulder is formed where the humerus, collar bone (clavicle), and scapula join. The rotator cuff holds the humerus in place. The muscles that form the shoulder are the supraspinatus, infraspinatus, tres minor, subscapularis, and deltoid. There are four rotator cuff tendons and two biceps tendons that make up the shoulder. These tendons connect the deep layers of the muscles to the scapula and humerus and provide support to the glenohumeral joint. The supraspinatus tendon is the most affected tendon due to overuse and trauma. The supraspinatus muscle is responsible for lifting the arms out to the side. An injury to this muscle can result in a rotator cuff tear or tears. Overuse can lead to shoulder (subacromial) impingement.
0 notes
Photo

Acromioclavicular Joint Sprain
Acromioclavicular Joint (ACJ) Sprain or Separation describes an injury to the ligaments between the Acromion of the Scapula (shoulder blade) and the Clavicle (collar bone).
The Acromioclavicular ligament is commonly affected, but injuries can also affect the Coracoclavicular or Coracoacromial ligament. Injuries are often caused by a fall to an outstretched arm.
Ligament injuries vary from Grade I (minor separation) - Grade III (severe separation, resulting in total rupture and joint deformity).
Symptoms
Pain (local or global)
Pain on moving arm above head
Swelling and/or bruising
Loss of movement
Physiotherapy
At Jonathan Clark Physiotherapy, we provide advice and education to help you protect your injury. We will often advise the use of ice, anti-inflammatory medication and rest in order to reduce inflammation and pain. Further treatment will focus on providing appropriate support such as taping, as well as ultrasound to aid healing.
Our therapists will aim to normalise your range of movement and provide strengthening rehabilitation to allow you to return to normal levels of functional activity. All treatment is tailored to help avoid long term shoulder problems including weakness and instability.
#ACJ#acromioclavicular#coracoclavicular#coracoacromial#shoulder#scapula#acromion#shoulderblade#injury#shoulderinjury#physio#physiotherapy#rehabilitation#ligamentinjury#ligament
2 notes
·
View notes
Text
Hockey
Hockey relies heavily on both upper and lower body musculoskeletal anatomy, as well aerobic and cardiovascular endurance. Among the most critical muscles used are: abdominal muscles, oblique muscles, erector spinae muscles and associated back muscles, hip extensors including the gluteal and hamstring muscles and hip flexors and quadriceps muscles. Muscles of the core are particularly critical for hockey. Core muscles include the abdominal muscles (such as the rectus abdominus and more importantly, the transverse abdominus), and the internal and external oblique muscles. Quadriceps and gluteal muscles, particularly the gluteus maximus are relied on for power. The gluteus maximus is used to extend the leg at the hip. Quadriceps muscles in the thighs also play an important role. The inner thigh muscles are used in abduction. Among upper body muscles, the anterior and middle deltoids and biceps muscles are the most heavily used.
Most Common Hockey Injuries
Hockey players are prone to a variety of overuse injuries due to movement inherent in the game, as well as assorted acute or traumatic injuries. Back muscle strain or back ligament sprain, groin strains, hip flexor strain, adductor strain, and tendonitis of the hip, pelvis, and groin; hip, knee or shoulder injury, wrist, hand and finger injuries, head and neck injuries including concussion and assorted contusions are all commonplace. Risk of traumatic injury comes from possible impact with hockey sticks and balls. The most common injuries include:
Contusions, which may occur in the upper or lower body
Neck and spine injuries
Knee injuries, particularly sprains to the medial collateral and capsular ligaments
Shoulder injuries, including acromioclavicular, or AC joint separation, (also known as a separated shoulder) as well as shoulder dislocation
Gamekeeper's thumb, resulting from the tearing of the ulnar collateral ligament
Fractures of the hand and wrist
Concussion, ranging from mild to severe and involving brief to extended periods of unconsciousness.
Injuries to the shoulder joint occur frequently in the game. The shoulder joint is composed of the humeral head and the glenoid fossa of the scapula. This highly mobile joint is relatively exposed, making it highly vulnerable to injury. Subluxation of the shoulder occurs when the humeral head slips out of joint, occasionally causing temporary paralysis. Fractures of the clavicle are also a common affliction, requiring proper medical attention.
Injury Prevention Strategies
Always properly warm-up (including practice skating) prior to play
Allow an adequate cool-down period and perform after-game stretching
Three Hockey Stretches
Reaching Lateral Side Stretch: Stand with your feet shoulder width apart, then slowly bend to the side and reach over the top of your head with your hand. Do not bend forward.
Kneeling Quad Stretch: Kneel on one foot and the other knee. If needed, hold on to something to keep your balance and then push your hips forward.
Kneeling Heel-down Achilles Stretch: Kneel on one foot and place your body weight over your knee. Keep your heel on the ground and lean forward.
0 notes
Text
What are the reasons for shoulder partition?
Shoulder Separation
Acromioclavicular joint (AC joint) disengagement or shoulder division is a standout amongst the most widely recognized wounds of the upper arm.
Ac Joint Surgery New York
It includes division of the AC joint and damage to the tendons that help the joint. The AC joint structures where the clavicle (collarbone) meets the shoulder bone (acromion).
Ac Joint Surgery NYC
What are the reasons for shoulder partition?
A shoulder division usually happens in athletic youthful patients and results from a fall specifically onto the purpose of the shoulder
A Type 1 bear partition happens when there is an AC tendon sprain that does not uproot the collarbone.
In a Type 2 damage, the AC tendon tears and the coracoclavicular (CC) tendon sprains or tears somewhat causing misalignment in the collarbone.
Ac Joint Shoulder New York
In the Type 3-5 bear partition wounds, both the AC and CC tendons are torn and the AC joint isn't appropriately adjusted..
0 notes
Text
The Most Common Sports Injuries In Malaysia
Malaysians love sports just as much as we love our foods. Badminton, running, futsal, and cycling are all common pastimes. However, are familiar you with the injury risks of staying active? A study reported on by the New Straits Time showed that 51% of exercisers from a younger age group suffer some sort of injury; with the risk of getting injured increasing as they age. For the majority, these conditions are not severe, being mainly obtained through overuse of a limb. Notably, most of these injuries occur at lower extremities. The thing about a sports injury is it is impossible to avoid it, no matter how careful you are being. That said, it doesn’t mean you can’t take precautionary steps to minimise the damage. Which is why knowing the most common sports injuries that occur to average Malaysians is extremely important.
Hamstring injuries
Sports that require sudden bursts of speed, power, and agility - like in football - result in a high risk of hamstring strains. In this case, you’ve overstretched the tendons on the back of your thigh or caused damage to the muscle. This isn’t life threatening, but it can be immensely painful. A hamstring injury is classified according to how much damage has been done. It could be as mild as a hamstring strain (which heals itself after a few days of rest) or it could be a complete muscle tear (taking months to recover).
Ankle Sprain
The occurrence of ankle sprains is extremely common, even if you're not doing any sports. It happens when you overextend and damage the ligaments in your ankle. These ligaments are what hold are the connective tissue that hold the bones of your joint together, and damaging them could have long term consequences. A mild sprain will go away after a few days of bed rest, but a bad sprain could end up weakening the ligaments. This eventually leads to an increased chance of spraining your ankle again, chronic pain, and even stability problems. An adequate warm-up regimes like proprioceptive and balance training can reduce the chance of ankle sprains.
Knee Injuries
Runner's knee, also known as Patellofemoral Pain Syndrome (PFPS) is common among runners (hence the name). The pressure of running can cause irritation where the kneecap (patella) lies on the thigh bone. You know you have a runner’s knee when your over-exercise regime leads to irritation of the tendon below the kneecap or when the region underneath the kneecap is worn or afflicted with arthritis. As a result tenderness and pain usually occurs near the front of the kneecap. This injury does not only affect runners but also cyclists, swimmers, people who practice aerobics, footballers, basketballers, and volleyball players. Knees are also vulnerable to the tearing of the anterior cruciate ligament or ACL. Those that follow sports will have come across the ACL tear explanation for why athletes miss games. In this case, the ligaments holding the knee together have been damaged; making it very difficult to walk. ACL tears cannot heal naturally and require surgery to be repaired.
Arch Pain (Plantar Fasciitis)
The elastic covering the sole of the foot is the plantar fascia which covers the foot and holds up the arch. When this shock-absorbing pad becomes inflamed, it causes a dull ache along the length of the arch and heel. The ache is due to overstretching or partial tearing of the arch pad. This happens to people with rigid, high arches; resulting in pain when they put weight on their foot or walk. Pain is particularly intense upon standing up after sitting for a long while. Plantar fasciitis is common among middle-aged people who have been inactive and who suddenly increase their level of physical activity. Runners are most vulnerable but almost any sport that keeps the athlete standing can cause arch pain.
Shoulder Impingement
The shoulder bones are held together by a group of muscles known as the rotator cuff muscles. When the shoulder joint is continually moved with the arm in an overhead position, as it is in tennis or lifting weights, the small rotator cuff muscles begin to stretch out. This loosens the head of the joint within the shoulder socket over time. If your shoulder has a shallow socket and lack of ligament strength, it is easy for the head of the shoulder to slide around in the joint. Tennis players and golfers are the most likely to suffer from this problem, but it could happen to anyone doing physical activity.
Tennis Elbow (Lateral Epicondylitis)
Tennis elbow is often caused by over-exercise. When the muscles and tendons in your forearm are strained due to a repetitive activity; it could also occur after taking a hard bump to your arm. This is a condition that causes pain around the outside of the elbow.
Fractures
Things are pretty serious when you get a fracture, also usually referred to a broken bone. Fractures are common sports injury caused by one-time injury to the bone which is an acute fracture. Repeated stress - mostly from repetitive impact like running or jumping - on a bone over time can also cause a stress fracture. Most are classified as an emergency and acute fractures may require surgery to completely repair.
Injuries weigh more than you think
We all should know to warm up ourselves before any exercise to avoid these injuries. Yet, if the things were to go sideways, you will be surprised at how much it can cost you. Treating sports injuries may be not enough with just a one-time visitation to the doctor or just resting at home. It could require physiotherapy, surgery, proliferation therapy over a span of time, depending on each individual's recovery progress. While the government regulates the maximum price that a hospital can charge for treatment, it still translates into thousands of Ringgit. For example, a reconstruction surgery of the acromioclavicular joint on your shoulder alone can cost at least RM2705 in a private hospital - not including fees for hospitalisation and medication. Hence, taking a precautionary step does not only mean for your body, but for your finances as well by taking upon an affordable insurance plan that suits your need. Most insurance plans will cover exercise and sports related injuries, taking some pressure off you if the unthinkable happens. Even if it’s just a short visit to the doctor for a sprained ankle.
The post The Most Common Sports Injuries In Malaysia appeared first on iMoney Malaysia.
0 notes
Text
Physical Therapy Modalities and Alternative Methods in Treatment of Soft Tissue Lesions_Crimson Publishers

Physical Therapy Modalities and Alternative Methods in Treatment of Soft Tissue Lesions by Elizabeta Popova Ramova in Orthopedic Research Online Journal
Purpose: To present the role of physical therapy and some alternative medicine methods to improve recovery after soft tissue muscles skeletal trauma in athletes and physical active people.
Introduction: Soft tissue injuries are common in physical active people, vary from minor to major complex trauma. Soft tissue injuries include sprains, strains and bruising. Any soft-tissue injury can lead to a tenderness, swelling, haematoma, scarring, fibrosis and loss of function. In the next few days after injury, we can greatly improve recovery time by taking medicaments that decrease inflammation and speed healing. The case of treatment in PH&Reha is soft tissue injuries of muscles skeletal system. There are onlower limb(ankle, knee, hip), the other on the shoulder (dislocations, acromioclavicular joint injuries, rotator cuff injuries), elbow and wrist.The aims of physical therapyare to relieve pain, control inflammation, hasten resolution of a haematoma, and accelerate repair, to restorate function and recovery muscle power.
Discussion: There are a variety of choices available which can provide specific and individualized results. Integration of conservative treatment and surgery with physical therapy, can decrease a time of rest and inactivity. The physical therapy has used follow physical therapy modalities: Light therapy, electro therapy, sonotherapy, hydro therapy, cold and warm applications, with proved effect. However, once the injury is stabilized, patient should take an alternative treatments for ssoft tissue injuries like acupuncture, masasage, functional taping, and herbal therapy from medicaments to greases.
Conclusion: Modern Physical therapy can improve fast recovery and functional impairment, on science base, with physical therapy modalities and alternative medicine methods. Evaluation of effect of treatment can be with ultrasonography, and clinical test and scores.
Keywords: Soft tissue injuries; Physical therapy
#OPROJ#Peer review journal of OPROJ#Crimson journal of orthopedics#open access journal of orthopaedics OPROJ
0 notes
Text
The Non-Surgical Solution to Heal Your Shoulder Pain
Sometimes, we feel sharp and shooting pain in our shoulders and spinal cord region. However, many of us do not pay much attention to it until the pain gets unbearable. Most of us believe that the only way to treat chronic shoulder pain is surgery. Regenerative medicine has revolutionized the world of medicine and has emerged as an effective alternative to surgery. Through regenerative medicine, shoulder pain can be treated without any side effects through injection of stem cells at affected site.

Stem Cell Institute of America offers several advanced therapies and treatments to deal with shoulder pain, which could be due to tendonitis, bursitis, rotator cuff tears, ligament sprains or dysfunction of the acromioclavicular joint. The team of highly professional medical experts at our institute are experienced in different kinds of regenerative medicinal treatments and will make sure that your shoulder pain is treated without any surgery or use of steroids.
The shoulder pain and shoulder conditions like rotator cuff tears, labarum tear, arthritis and glenohumeral sprains of the ligament are treated with the help of regenerative medicine.
So if you have been suffering from a prolonged shoulder injury or pain, give a call today to Stem Cell Institute of America today. Avail the best regenerative treatment and lead a painless life.
0 notes