#voluntary apnoea
Explore tagged Tumblr posts
Text
Voluntary Apnoea
Voluntary apnoea: the suspension of breath as a conscious decision made by an individual, to hold one’s breath.
The woman’s grip on the back of his head tightened, pulling at the thick mess of his unkempt locks. His scalp burnt as her nails pierced his flesh as she hurled him forward into the bathwater.
Erupting waves rose around him like the parted Red Sea before pulling back over him and dragging him beneath the surface.
Small bubbles tickled his cheeks as they rose, escaping the turbulent water. He felt his eyes burn with redundant tears that were swept away by the waves of bathwater that lashed at him. He thrashed about, desperately trying to break free of his mother’s tight grip as she pulled at his hair and pushed him further under the water.
This head thumped against the side of the bathtub, the sound ominously echoing through the water.
He could hear his mother’s frustrated cries, the sound muffled by the water. He could hear the crashing water as the waves collided with each other and the bathwater spilled over the edge of the tub and crashed onto the tiles. He imagined the water shattering like a glass knocked from the counter, each fragment glistening before melting and rolling across the smooth tiles like the tide caressing the shore.
It felt as if his lungs were consumed by a raging inferno, the jagged claws of firebirds tearing at the tissue as they tried to dig their way out of his chest.
He felt his chin tremble as he fought to keep his mouth shut but the longer he was beneath the water, the harder it became. He was fighting off the instinct to draw breath, knowing there was nothing around him but merciless water.
He pushed at the bottom of the bathtub, his arms trembling and muscles burning as his body threatened to give out beneath him. He tried to fight his way back to the surface, but it was no use; he wasn’t as strong as the enraged woman that held him down.
He held his breath and closed his eyes, but no matter how much he willed it away, the water was still there, his mother’s grip was still burning at his scalp and the reality of his mortality was creeping closer ever so slowly. Every second dragged on as if time was suspended in oblivion, making every second of pain and torment longer and more agonising.
He felt another wave of tears well in his eyes as thick saliva rose in his throat, suffocating him. His body shuddered as he fought back his sobs.
No-one’s coming to help him this time, no-one’s coming to save him.
Dad, the boy cried silently, helplessly. Dad, please, help.
The pain was too much; his head was exploding, his lungs were burning, his arms were trembling, and his vision was a kaleidoscope of stars.
He tried to distract himself, to let his mind wander and distract himself from the agony that consumed his body.
He opened his eyes, the glossy white bathtub glistening with the rippling shadows as the water swayed back and forth, dancing the way his parents would, turning and swaying.
He remembered the dress his mother wore to her last birthday party – the last time he saw her smile. He would imagine that the dress was made of the sea, the frail white lace and gleaming pearls that adorned the Grecian collar of her dress looked like foaming white waves and the fabric faded to shifting shades of blue, green and black as the skirt drifted around her slender figure. He remembered the way the skirt would sway and billow like the tide lapping against the shore. He remembered the bright smile that lit her face as she took his hands in hers and danced with him around the lounge room, moving effortlessly around the furniture like swirls around the rocky cliffs.
What went wrong? the boy asked himself. Why did she stop smiling?
He had asked his dad the very same question many times, but every time he did he was met with the same response: “She’s sick.”
The doctors said it was called schizophrenia, and it was emphasised by her dissociation. His dad explained it differently, he said his mum would see and hear things that weren’t real, she would forget where she was and who they were, she would get scared and angry at the world around her.
His dad assured him that the medication would help, but it didn’t.
He watched as his mum grew sicker, every day chipping away at her like the thrashing waves wore away at bluffs and she began to forget who she was.
When his dad’s back was turned, she would unleash hell on her son and he could do nothing but suffer the beatings and relentless verbal abuse.
He convinced himself that if he stayed small and defenceless then maybe she’d realise he wasn’t a threat, maybe she’d recognise him, remember him. But she never did.
And no-one was there to help him.
What if help doesn’t come? the boy asked himself. What if no-one comes and I die here?
His body weakened, his limbs falling still and drifting lifelessly in the water. His soft pink lips were tinted blue, his cheeks flushed red as his lips slowly parted and he breathed in.
Help will come, he tried to assure himself. Help always comes… Doesn’t it?
His eyes fell shut, the darkness creeping in like swirls of ink that dissolved through the water and pulled him back into the dark abyss. He felt weightless as he drifted into nothingness.
There was no pain, there was no fear.
It was surreal, peaceful.
…
The first thing he heard from outside their house was gut-wrenching and fear-inducing sound of his wife’s frustrated cries and panicked sobs, the sound drifting through the open windows and out onto the streets.
Nathan felt his heart sink into his gut, his limbs feeling heavy as the fear set in. He kicked up his heels and ran inside. He shoved open the front door and raced inside with his friend, Elle, following behind him, only to be met by the heart-lurching sound of silence.
They hurried upstairs, feet pounding against the stairs as their hearts thumped against their ribs.
He shoved the bathroom door open, his heart rising into his throat as his eyes fell upon his son’s body: limp and unmoving, drifting like a piece of debris in the water.
He leapt forward and pulled his wife away from the bathtub, feeling her go limp in his arms as she sighed with relief and said, “He’s gone. We’re safe now; he’s gone.”
There was an indescribable sense of fear as he watched Elle lift his son’s lifeless body from the bathtub and set him down on the wet tiles. He watched as Elle brushed back the soaked mess of the boy’s dark hair and checked for any signs of life.
From where he stood, he could tell that his son wasn’t breathing. He held his wife tight, pulling her away and pinning her flailing arms to her side as she began to kick and scream. He ignored her cries and fought back against her thrashing body as she begged Elle not to save the boy, to ‘just let the monster die’.
He watched, heartbroken and helpless, as Elle began CPR, rhythmically compressing the boy’s chest and breathing air back into his lungs.
Time seemed to slow.
He stood still, hot tears welling in his eyes as he looked down at his son.
Elle did her best to resuscitate him, but there was no response.
We’re too late, Nathan thought. He’s gone.
“No,” Sophie screamed. “Let him die!”
Elle ignored her, her composure fractured as she started to realise the boy wasn’t responding. Fear began to seep through the cracks, tears welling in her eyes as she began to mutter under her breath, talking softly as if to encourage the boy back to consciousness.
My boy… My boy is gone, he thought. We’re too late… we’re too late.
His thoughts were silenced by the sound of painful coughing as a spout of water spewed from the boy’s blue lips.
Elle turned him on his side, holding him in place and talking softly to him as he hurled up a lungful of water.
They waited, the air heavy with tension as they waited for one sound. Then, finally, they heard the soft sound that brought them sweet relief; he drew breath.
“No!” Sophie wailed.
Elle moved the boy’s trembling limbs into the recovery position, talking softly to him as she gently brushed back his limp, wet hair. She left the boy’s side and took Sophie in her own arms, leading the screaming woman to her bedroom and gently shushing her.
“You don’t see the way he looks at me,” Sophie cried, her voice echoing down the hall. “He’s a monster. He’s going to kill us all!”
“He’s your son. He’s eight years old,” Elle reminded her friend, her voice soft and comforting as she reminded Sophie that her schizophrenia made her think that way and that she didn’t know what she was doing.
Nathan stood still for a moment, staring down at his son’s shuddering body.
He’s alive.
His limbs ached as he told himself to go to his son, but he couldn’t move.
“Dad,” the boy rasped, coughing violently and shaking the man from his thoughts.
Nathan stepped forward and knelt by the boy’s side, lifting the child into his lap and cradling him against his chest. He felt the boy’s shoulders rise and fall with shaky breaths.
The boy’s voice was weak as he rasped, “Dad, what did I do wrong?”
“Nothing, kiddo, you did nothing wrong,” he assured his son, pressing a tender kiss to the crown of the child’s head.
“Then why did she-?” The rest of his question died away as he coughed and spluttered, his frail body shaking violently.
He gently shushed the boy, holding him close and patting his back soothingly as the boy began to cry into the man’s shirt.
Nathan sighed heavily.
He didn’t know why she thought that way. Yes, there was science and logic to it: it was a mental illness, a psychosis, that results from the brain developing differently and results in the person being subjected to an alternated experience of reality. He could recite that a thousand times, but he could never give his son the answers he needed.
He replied instinctively, “Because she’s sick.”
They stayed like that for a while, the two of them sitting on the bathroom floor while he listened to the boy’s shaky breaths.
Elle stepped back into the bathroom, resting her hand on her friend’s shoulder as she asked, “Nathan, how long has this been going on?”
“I don’t know,” he admitted. “I’ve only ever seen her throw small tantrums when she gets confused. I’ve never seen her act out in aggression… I never thought she’d hurt him. I never thought she’d try to kill him.”
“Has she been taking her medication?”
Nathan nodded.
Elle let a heavy sigh fall from her lips.
Nathan knew what she was about to say.
“You have to get her away from him, Nathan,” Elle said quietly, her voice soft but firm. “We talked about this. You need to put her into care before this gets any worse.”
“I know, I know,” he replied, “I just… I can’t abandon her like that.”
“You’re not abandoning her,” Elle said reassuringly. She sighed heavily, speaking softly as she pointed out, “If you don’t get her the help she needs, then next time we won’t be able to save him. Next time, we’ll be seconds too late and all we’ll find is his body.”
He paused for a moment, remembering how she was on her birthday a few weeks ago, spinning about with joyous abandon, laughing and singing like she didn’t have a care in the world, and smiling that gorgeous smile that he fell in love with; the same smile that his son had gotten from her.
Nathan cradled his son to his chest and pressing a kiss to the boy’s temple. He felt the boy tremble in his hold, the shock wearing off and fatigue letting him drift into sleep in the safety and warmth of his father’s arms.
“Call the hospital,” Nathan muttered, glancing up at his friend. “Tell them I’m putting her into care.”
“You’re making the right choice,” Elle assured him.
“It’s the only choice I have,” he replied. “I can’t lose him.”
#voluntary apnoea#writing#my writing#fiction#short story#tw: drowning#tw: depressing#tw: near death experience#tw: death
18 notes
·
View notes
Photo
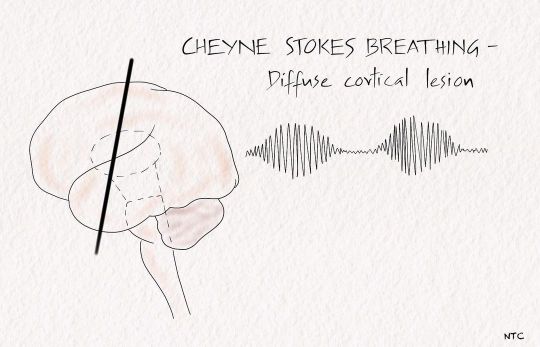
Respiratory abnormalities in coma. The full details are available in episode 13 of ‘Clinical neurology with KD’ podcast. Cheyne -stokes breathing. There are brief periods of hyperpnoea regularly alternating with an even shorter duration of apnoea. After the apneic phase, respiratory movement's amplitude increases to a peak before slowly waning off to the following apnea. It represents a more severe degree of normal post-hyperventilation apnea due to bilateral cortical dysfunction. Brainstem hyperventilation Patients with midbrain and pontine lesions can have rapid and prolonged hyperventilation. Lowering the local CSF pH and stimulating the respiratory centre of the medulla is one of the postulated mechanisms. Kussmaul's breathing is deep, rapid breathing seen in metabolic acidosis. Apneustic breathing In apneustic breathing, there is a prolonged inspiratory time followed by a long inspiratory pause. The air is retained for several seconds and released. The expiratory time is short, and a pontine lesion usually causes it. Cluster breathing It is a cluster of breaths following each other in an irregular sequence. It results from low pontine or high medullary lesions. Ataxic breathing The breathing pattern is entirely irregular. It is called the atrial fibrillation of breathing. The inspiration is of different amplitudes and lengths and intermixed with variable periods of apnea. It is often seen in terminally ill patients and suggests impending respiratory failure. The site of the lesion is the dorsomedial medulla. A paramedian medullary infarct, bleed, or tumour can produce it. The classical breathing described by Biot in severe meningitis is ataxic. Central hypoventilation The pathway of voluntary respiration from the cortex descends via the corticospinal tract. The automatic respiration fibres from the medulla descend in the ventrolateral cord, with anatomic separation of inspiratory and expiratory pathways. #neurology #neuroscience #coma #emergencymedicine #criticalcare #internalmedicine #neuro #neurologyteachingclub #clinicalneurology #respiration #respiratorymedicine #neurocriticalcare #neuroresident #medicineresidency #neetss https://www.instagram.com/p/ChEkwNAvGSl/?igshid=NGJjMDIxMWI=
#neurology#neuroscience#coma#emergencymedicine#criticalcare#internalmedicine#neuro#neurologyteachingclub#clinicalneurology#respiration#respiratorymedicine#neurocriticalcare#neuroresident#medicineresidency#neetss
0 notes
Text
Shrewsbury + Social prescribing event in Shrewsbury is great success
Over 60 organisations and groups attended an event to find out more about social prescribing, supporting people’s health and well-being in Shrewsbury.
The social prescribing workshops hosted by Shropshire Council on Tuesday 19 June 2018 gave attendees the opportunity to find out more about Shropshire’s social prescribing programme, how it’s going to be rolled out in Shrewsbury and how they can get involved.
Social prescribing in Shrewsbury event. Left to right: Kate Garner, Steve Latham-White, Claire Sweeney, Katy Warren, Linda Monteith, Val Cross, Laurel Roberts and Jo Robins.
Shropshire’s social prescribing programme is being led by Shropshire Council and its Help2Change service. The programme involves working with a range of organisations such as GPs and community and voluntary organisations to provide non-medical support for people to help them take greater control over their own health.
The event was opened by Lee Chapman, Shropshire Council’s Cabinet member for adult services, health and social housing, who said he was very committed to the approach of social prescribing, seeing it as a key cornerstone for creating good health and well-being.
Lee Chapman commented about the event:-
“Our social prescribing event provided a great opportunity to raise awareness of the positive benefits social prescribing can bring to local communities.
“I was really pleased and encouraged to see so many organisations at our event. There was a lot of interest and enthusiasm from people around how we can work together to develop and deliver Shrewsbury’s social prescribing programme.”
Speakers at the workshops included local GP Dr Finola Lynch and Laurel Roberts from the Qube in Oswestry.
Both speakers spoke positively about the role of social prescribing, Dr Lynch talked about the benefits to patients, the invaluable contribution of the voluntary sector and how social prescribing could become part of the solution to reducing isolation and loneliness.
Laurel Roberts commented on how better links can be made between public services and the voluntary and community sector to ensure people receive a more holistic and joined up approach to support them with their health and well-being.
Organisations taking part in the workshops got to hear about real life stories from people who had gone through the social prescribing experience. One story spoke about a local man who suffered from sleep apnoea and weight issues. After his appointment with a social prescribing adviser, he began attending a local Walking for Heath group. This has led to him losing weight and making new friends; he’s also now looking at other activities in his community.
It is estimated that around 20% of patients consult their GP for what is primarily a social problem rather than a clinical problem.
Shropshire’s social prescribing programme will enable doctors to refer those patients to a social prescribing adviser who will work with the individual to access services and support in their own communities. This could be anything from taking part in group learning sessions, sports, arts activities, volunteering, gardening, befriending services to healthy eating advice.
Dr Finola Lynch, Shropshire GP and social prescribing champion for Shropshire Clinical Commissioning Group, said:-
“Socially isolated people use a third more GP appointments, and while it’s always a privilege to chat to them, the help and support they need is not necessarily found in a prescription or a pill, but in social prescribing.
“Finding an exercise activity or a social group that’s suited to you does wonders for your mental health and well-being, and we know it’s good for your physical health too. I wholly endorse social prescribing as a means of supporting patients and their communities, and I’m very proud about the fact that Shropshire is a national leader in this movement.”
Attendees were also encouraged to contribute to Shropshire’s social prescribing network by signing up to Shropshire’s community directory to promote their organisation. The directory provides information on a wealth of local services and activities.
Shrewsbury’s event is one of many that is being rolled out across the county. An event has already taken place in Albrighton, with another being planned for Bridgnorth this summer.
Social prescribing in Albrighton
For more information about the workshop or Shropshire’s social prescribing programme in Shrewsbury, contact Linda Monteith at [email protected] or call 07990 085443.
Further information
The overall aim of social prescribing is to prevent worsening health for people with long-term health conditions, reduce the number and intensity of costly interventions in urgent or specialist care, and offer an alternative to those people with non-medical conditions presenting at GP practices. Social prescribing schemes can involve a variety of activities.
Shropshire’s Healthy Lives Programme
Social prescribing forms part of Shropshire’s Healthy Lives programme, which supports individuals, families and communities to take more control over their health and reduce their risk of chronic disease. The scheme also links to the Resilient Communities work being undertaken by Shropshire Council with the support of NHS colleagues and voluntary sector organisations who are working together to design targeted interventions and activity in localities. The aim of this work is to connect up people and activities in our neighbourhoods so that they all know more about what is going on, and have the choice and opportunity to get involved in the things they are interested in, and which can make people happier and healthier.
The post Social prescribing event in Shrewsbury is great success appeared first on Shropshire Council Newsroom.
https://ift.tt/2KwDnDD
0 notes
Text
Obesity - The Increment You Don’t Want
A lot has been said and described about obesity in the past decade, we know how bad it is for our physical, mental & social health. Yet here I am writing this article again on a topic which has already been discussed to unfathomable limits in all forms of media. So, the question arises why am I writing an article on a topic that has already been bleached super white. The answer is a gigantic cliche, because it is that important, significant and beneficial to know about obesity. Therefore when you are writing a series of articles on health, obesity is that big white elephant that cannot and should not be ignored at any cost. Obesity is a booming pandemic that has to be addressed every time so that every other person is aware about it’s extremely alarming and doomful consequences.
What is overweight / obesity?
According to WHO, Overweight and obesity are defined as abnormal or excessive fat accumulation that may impair health.
How can one assess if he / she is overweight / obese?
Calculating a person’s Body Mass Index (BMI) is the most effective way to assess if one is obese / overweight.
The formula is Weight in Kgs / Height in metre2
Overweight is a BMI greater than or equal to 25.
Obesity is a BMI greater than or equal to 30.
Problems & Complications of obesity?
Raised BMI is a major risk factor for a number of noncommunicable diseases such as:
A. Cardiovascular diseases (mainly heart attack and paralysis)
B. Diabetes
C. Musculoskeletal disorders (especially osteoarthritis)
D. Cancers (including endometrial, breast, ovarian, prostate, liver, gallbladder, kidney, and colon).
E. Sleep disturbances like OSA (Obstructive Sleep Apnoea)
F. Overall decrease in meaningful life span & total life span.
Advantages of having a healthy weight?
Advantages are:
A. Reducing greatly the risk of various serious diseases mentioned above.
B. Having more energy, feeling fit & energetic to do more work / performance.
C. Better sleeping pattern and waking up feeling afresh.
D. Having fewer aches and pains
E. Improved ability to move easily and faster
F. Finding it easier to breathe
G. Improved immune system (ability to fight off illness)
How can you reduce weight?
This is a question that has an unlimited answer but in short, weight can be reduced by the following methods:
A. Role of Diet :- Diet plays a significant role in losing weight. Eighty percent of the role in significant weight loss is played by diet alone. Therefore consuming a good nutritious balanced diet is essential to achieve a weight loss goal. A 1200 Kcal diet is a good start. There are many free dieting apps available on Google Play Store which you can use to smartly keep a check on your calories and reduce weight, some examples are ‘Obino’, ‘Diet Plan’ etc.
B. Role of Active Exercise :- Active exercise is voluntary physical exertion. Active exercise is important to improve strength & cardiovascular health. According to WHO, 30 minutes of brisk walking six days a week is highly beneficial in losing weight.
C. Role of Drugs :- Though there are various anti-obesity medications available, these are not actually helpful in losing weight significantly. At most it can only prevent weight gain to a very limited extent. Hence diet & exercise remain the unchallenged choice for weight loss.
D. Role of Surgery :- The most common surgical techniques for weight loss include Gastric Balloon, Gastric Bypass & Sleeve Gastrectomy. Each of these techniques has its own advantages and disadvantages which needs to be discussed with the required qualified doctor. Surgical intervention in general is only recommended when a patient has a BMI greater than 40.
I would end by saying that the road to weight loss is no doubt indeed difficult, but certainly not unachievable, with a little persistence, patience and hard work you can and you will get there. There will be times when it will seem impossible but the only advice I can give you is that when you are going through hell, keep going, do not stop. Believe in yourself when no one else does.
/��܇�
0 notes