#vasoconstriction
Explore tagged Tumblr posts
Text

#cold#body temperature#blood flow#extremities#hypothermia#vasoconstriction#survival mechanism#hands#feet#vital organs
72 notes
·
View notes
Text

The Science Research Notebooks of S. Sunkavally, p 692.
#hypothalamus#NADPH#superoxide#water flea#alkaline water#alkaline lakes of Africa#spotted hyena#scent glands#caffeine#wound healing#Namib elelphant#vasoconstriction#Raynaud's phenomenon#melatonin
2 notes
·
View notes
Text
Hypothalamus does vasopressin/ADH elevates blood pressure.
Glomerulus secretes renin, vasoconstricts to increase blood pressure.
Erythropoietin stimulates the bone marrow to produce more red blood cells.
1,25-dihydroxyvitamin D activated in kidney.
Renal disease decreases glomerular filtration and creatinine clearance rate (labs: GFR, BUN, creatinine. BUN and Cr elevated.
In acute kidney injury, a BUN:Cr of 20:1 indicates a pre-renal state in which BUN is increased due to acute kidney damage. AKI may be reversible, not requiring dialysis.
Reduced BUN reabsorption indicated by a BUN to creatinine ratio of less than 10:1, suggests need for dialysis.
Renal solute load = solutes excreted in 1L of urine. MAIN SOLUTES: nitrogen and sodium.
Anemia, upset blood pressure, and decreased activation of vitamin D involved in renal insufficiency (due to the hormones released by kidney and hypothalamus).
TO BE ADDED TO...
#dietetics#kidney#hormones#blood pressure#vasoconstriction#vasopressin#ADH#antidiuretic hormone#erythropoietin#vitamin D
3 notes
·
View notes
Text
Worrying or stimming? Looking at an overactive mind from a neurdodivergent point of view
It’s fair to say, I have an extremely overactive mind, a trait so built into me that it predates any “need” to worry about anything very much in my life really, however tempting it is to try and dig up reasons why my infant nervous system may have been sent into fight or flight on a regular basis. Overthinking is just part of the fabric of who I am and has delivered some of my most contented and…

View On WordPress
#ADHD strategies#anxiety or ADHD#articles#burnout#default mode network#dysautonomia#environmental sensitivity#hypoxia#insomnia#ME/CFS#mental stimming#neuropathy#overthinking#sensory processing sensitivity#vasoconstriction
0 notes
Link
Migraine is one of the most prevalent and disabling neurovascular disorders worldwide. However, despite the increase in awareness and research, the understanding of migraine pathophysiology and treatment options remain limited. For centuries, migraine was considered to be a vascular disorder. In fact, the throbbing, pulsating quality of the headache is thought to be caused by mechanical changes in vessels. Moreover, the most successful migraine treatments act on the vasculature and induction of migraine can be accomplished with vasoactive agents. However, over the past 20 years, the emphasis has shifted to the neural imbalances associated with migraine, and vascular changes have generally been viewed as an epiphenomenon that is neither sufficient nor necessary to induce migraine. With the clinical success of peripherally-acting antibodies that target calcitonin gene-related peptide (CGRP) and its receptor for preventing migraine, this neurocentric view warrants a critical re-evaluation. This review will highlight the likely importance of the vasculature in migraine.
Intracranial vessel dilation has been implicated in migraine, specifically meningeal arteries. In one study, during experimental induction of migraine, dilation of both middle meningeal and middle cerebral arteries was observed.
Using the vascular hypothesis as inspiration, several studies have shown that migraine attacks were associated with release of vasoactive peptides. The vasodilatory peptides calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating polypeptide (PACAP-38), as well as the neurotransmitter nitric oxide (NO), are all potent vasodilators implicated in migraine pathophysiology.
CGRP is a multifunctional neuropeptide found on sensory nerve fibers (Russell et al., 2014). These fibers innervate vessels where CGRP receptor activation can cause both smooth muscle-dependent and endothelium-dependent activation (Wang et al., 1991; Raddino et al., 1997; Brain and Grant, 2004). Infusion of CGRP in migraine patients results in a delayed migraine-like headache, occurring around 1–5 h after treatment. However, this study also reported a decrease in blood pressure following infusion of CGRP that returned to levels similar to baseline within 60 min of administration (Lassen et al., 2002). To understand the mechanisms of migraine, several studies have induced migraine-like behavior via administration of CGRP.
Although most studies focus on vasodilatory agents implicated in migraine, the role of vasoconstrictors must not be ruled out. There have been observations that plasma levels of endothelin-1 (ET-1), a potent vasoconstrictor, were increased during early stages of a migraine attack, but rapidly decreased at the onset of the headache (Kallela et al., 1998). ET-1 is an important regulator of cerebral blood flow and its receptors are found in endothelium and vascular smooth muscle cells of the arterial system and throughout the CNS (Arai et al., 1990; Sakurai et al., 1990). Kallela et al. (1998) observed that even though ET-1 was elevated during early phases of the migraine attack, the cubital vein blood pressure measurements were unchanged. ET-1 levels rapidly decline approximately 3–4 h after the initiation of the attack, which coincides with reports of headache onset (Kallela et al., 1998). However, the authors did not report the actual blood pressure values and the observation time points are unclear.
It is important to note that ET-1 has the ability to either induce vasoconstriction or an initial vasodilation followed by vasoconstriction depending on whether it is activating endothelin type A receptor (ETA) or endothelin type B (ETB). ETA activation causes sustained vasoconstriction via smooth muscle and can inhibit NO synthesis (Arai et al., 1990; Ikeda et al., 1997) however, ETB activation initially increases release of NO and prostacyclin, which are known vasodilators, followed by sustained vasoconstriction via endothelial cells (de Nucci et al., 1988; Hoffman et al., 1989; Winquist et al., 1989; Sakurai et al., 1990). Furthermore, the non-specific endothelin receptor (A/B) antagonist bosentan inhibits neurogenic inflammation but not vasoconstriction and is not effective for the treatment of migraine (May et al., 1996). However, the ability of bosentan to act on the initial vasodilation that occurs with ETB activation was not assessed. This, along with other studies showing inhibition of neurogenic inflammation is not enough to abort migraine, supports a possible vascular role in migraine. Future studies dissecting the temporal relationship among the release of vasoactive agents such as CGRP, NO and ET-1 in migraine patients are necessary.
Vascular inflammation is a mechanism that may contribute to migraine pathogenesis. Dural vessels are thought to contribute to neurogenic inflammation, an event that activates sensory neurons and is characterized by vasodilation, plasma extravasation, and release of pro-inflammatory molecules from mast cells (Raddant and Russo, 2011). These non-vasomotor roles may involve all three layers of vessels: the inner endothelium layer, the middle smooth muscle layer and the outermost adventitia layer of fibroblasts and connective tissue.
The endothelium can both send and respond to signals via release of vasoactive substances to maintain vessel homeostasis (Tomiyama and Yamashina, 2010; Jacobs and Dussor, 2016). For example, when perturbed, cells of the vasculature can release ATP, consequently activate purinergic receptors, stimulate release of NO and pro-inflammatory mediators from endothelial cells (Burnstock, 2016; Jacobs and Dussor, 2016). Endothelium-induced NO release is then capable of sensitizing nearby afferents and possibly contributing to pain experienced during migraine. Two studies reported migraineurs have a decreased count of circulating endothelial progenitor cells (Hill et al., 2003; Rodríguez-Osorio et al., 2012). These cells are a marker of endothelium integrity and function, and a reduction suggest endothelial cell dysfunction (Hill et al., 2003). Additionally, there is mounting evidence of circulating endothelial microparticles in female migraine patients, particularly those diagnosed with migraine with aura (Liman et al., 2015). Tietjen et al. (2009) concluded that decreased concentrations of urinary NO stable metabolites in migraineurs in between migraine attacks compared to control subjects was indicative of endothelial cell dysfunction. Reports from the Levine lab suggest that vascular endothelial cells play a role in enhanced peripheral hyperalgesia via endothelin-1 and both β-adrenergic antagonist ICI-118551 and sumatriptan, both which have receptors on endothelial cells, attenuated endothelin-induced enhancement of hyperalgesia (Joseph et al., 2013). These findings suggest that anti-migraine drugs can produce anti-nociceptive effects by actions on endothelial cells. Conversely, Napoli et al. (2009) concluded that endothelial cells were properly functioning in migraineurs, however, smooth muscle cells failed to function properly following a diminished response to NO. Thus, there is evidence of endothelial dysfunction in migraine, although it is not without controversy.
Smooth muscle cells are of particular interest in migraine although studies that focus on their non-vasomotor contributions are limited. However, one promising area is the ability of NO to activate soluble guanylyl cyclase (sGC) in vascular smooth muscle cells. Recently sGC has been implicated in migraine pathogenesis (Ben Aissa et al., 2017). sGC is a major NO receptor and has been reported as a mediator of nitroglycerin-induced migraine pain (Ben Aissa et al., 2017). While NO induction of sGC causes vasodilation, it can influence dural nociceptors via the NO-cGMP pathway (Levy and Strassman, 2004). More recently Zhang et al. (2013) showed that this NTG infusion has been shown to cause delayed meningeal inflammation via vascular phosphorylated ERK expression. These data, though few, warrant more comprehensive studies to determine the role of smooth muscle activation in migraine models.
Finally, an unexpected contribution of the fibroblasts has recently been suggested by the Dussor lab (Wei et al., 2014). Cultured fibroblasts from the dura are capable of releasing mediators that sensitize dural afferents and induce-migraine-like behavior in rodents (Wei et al., 2014). These cells release IL-6 which is elevated during migraine attacks.
One theory is that neurogenic inflammation caused by activated mast cells can sensitize nociceptors and thus trigger headache (Theoharides et al., 2005; Waeber and Moskowitz, 2005; Levy, 2009). While direct evidence is lacking, clinical studies have reported increased circulating intracranial inflammatory mediators during an attack (Sarchielli et al., 2006; Goadsby and Edvinsson, 1993). Moreover, activated mast cells release histamine, prostaglandins and a host of pro-inflammatory peptides (Roberts et al., 1979; Heatley et al., 1982; Lewis et al., 1982; Tetlow et al., 1998; Theoharides et al., 2005; Aich et al., 2015). Specifically, tryptase and histamine release have been reported to release neuropeptides from proximal nerve endings and contribute to hyperalgesia (Kleij and Bienenstock, 2005; Aich et al., 2015). This along with the ability of mast cells to increase pERK, cfos, and excitation of meningeal nociceptors provide insight into a mechanism of how mast cells might contribute to peripheral sensitization.
Histamine has been reported to be increased in plasma levels during a migraine attack (Heatley et al., 1982; Moskowitz, 1993; Theoharides et al., 2005). Also, infusion of histamine in migraineurs causes a severe pulsating headache compared to controls (Krabbe and Olesen, 1980). Although with some debate, anti-histamines have been effective in treating migraine in some clinical studies and their potential role in migraine is nicely summarized by Silberstein (Yuan and Silberstein, 2018). Histamine causes dilation of cranial arteries via activation of endothelial histamine receptor H1 and inducing formation of NO (Toda, 1990; Ottosson et al., 1991). Moreover, histamine disrupts endothelial barrier formation by altering vascular endothelial cadherin and inducing dilation of vessels (Ashina et al., 2015).
There is an overwhelming abundance of evidence that suggest inflammatory pain states can alter blood brain barrier (BBB) permeability. The BBB is a selective barrier that limits paracellular diffusion via tight junctions between endothelial cells (DosSantos et al., 2014). Given that migraine has increased release of pro-inflammatory peptides, it could involve BBB disruption, although this is still controversial. In a mouse model of cortical spreading depression, the detection of brain edema, plasma extravasation, and altered metalloprotease and matrix proteins were indicative of BBB dysfunction (Gursoy-Ozdemir et al., 2004). In addition to barrier dysfunction, alterations in gap junctions may play a role in migraine. Gap junctions are specialized regions of the plasma membrane that connect cytoplasms of adjacent cells. Tonabersat, a gap junction inhibitor that binds to connexin 43, has been shown to be effective in a subset of migraine patients with aura (Sarrouilhe et al., 2014). Of particular interest, connexin 43 is found on neuronal cells and is one of the connexin proteins associated with cells of the cardiovascular system (Figueroa and Duling, 2009). Given these data, the efficacy of tonabersat suggest a possible role for dysfunction of gap junctions in migraine.
Based on these observations, we propose a possible mechanism for how an altered trigeminovascular microenvironment may initiate vascular-neural cross talk (Figure 1). The meninges are densely vascularized and the layers are innervated by sensory fibers that relay information from the periphery to higher order neurons in the brain. Distention of intracranial blood vessels, possibly from the dura, mechanically activates trigeminal perivascular afferents (Davis and Dostrovsky, 1986; Buzzi et al., 1995). Those activated neurons can release molecules that cause mast cell activation and vasodilation of the nearby vessels in a feed-back loop (Figure 1). In this model, mast cell activation increases vascular permeability and/or causes neuronal activation and neuropeptide release, which causes subsequent release of inflammatory mediators from the vessels that modulate sensory input. Most studies focus on the effect of mast cells on neurons in migraine. Future studies that examine the effect of mast cells on vasculature in translational models of migraine could reveal a role for mast cells in vascular-neural coupling.
It is known that triptans are 5-HT1B/D/F serotonin receptor agonists that can inhibit the release of neuropeptides involved in migraine and act as vasoconstrictors (Jansen et al., 1992; Nozaki et al., 1992; Williamson et al., 1997; Knight et al., 2001; Wackenfors et al., 2005). Moreover, sumatriptan treatment reduced plasma levels of CGRP in humans (Goadsby and Edvinsson, 1993; Juhasz et al., 2003) and animal models (Buzzi and Moskowitz, 1990; Buzzi et al., 1991; Nozaki et al., 1992). Vascular studies of triptans in people have given insight into its mechanism of action and the roles vessels might play in migraine. In fact, a study using single-photon emission computed tomography combined with Doppler sonography showed that if sumatriptan is infused in people, only the abnormally dilated vessels were reversed back to normal (Asghar et al., 2010, 2011). This observation suggests that triptans only cause significant vasoconstriction on dilated vessels during a migraine. Furthermore, it is interesting to note that triptans work best if used within the first 2 h of the attack (Linde et al., 2006). This coincides with the vasodilatory period following CGRP administration (Lassen et al., 2002). In addition, sumatriptan does not appear to be effective for relieving pain in other disorders (Ahn and Basbaum, 2005), which may be due to the vascular events in migraine. These observations suggest that the vasoconstrictor activity of triptans should not be ignored.
CGRP receptors are found throughout the cranial vasculature. Olcegepant is a non-peptide CGRP antagonist that has high specificity for human CGRP receptors and reported to be efficacious in migraine (Edvinsson, 2008, 2015). Olcegepant blocks dilation of the middle meningeal and extracranial temporal arteries. Similarly, the CGRP receptor antagonist telcagepant has also been shown to inhibit vasodilation of cultured human cerebral and meningeal arteries (Edvinsson et al., 2010). These observations leave open the possibility that some of the CGRP receptor antagonist efficacy might involve the vasculature.
[A] study that corroborates a role in migraine is a genome wide association meta-analysis in 2016 by Gormley et al. (2016) that identified 38 susceptibility loci that were enriched for genes associated with arterial tissue. Moreover, several of these genes are associated with smooth muscle dysfunction and cardiovascular disorders linked to migraine as a comorbidity.
The renin-angiotensin system (RAS), which is involved in hypertension, has been thought to be involved in migraine pathogenesis (Ba’albaki and Rapoport, 2008). Indeed, the efficacy of angiotensin converting enzyme inhibitors in migraine treatment is indicative of a link between migraine and hypertension (Tronvik et al., 2003). Additionally, blood pressure homeostasis is maintained by close communication between the RAS and natriuretic peptides. It has been reported that brain natriuretic peptide (BNP), which is produced by cardiac cells, is elevated in migraine (Uzar et al., 2011). However, BNP is reported to negatively regulate sensory neuron excitability (Vilotti et al., 2013). Further investigations are necessary to elucidate the role of BNP, RAS and hypertension in migraine.
The ability of vasoactive substances to induce migraine, effective drugs to have a vascular site of action, and the associated correlation of migraine and cardiovascular disease convey that vascular contributions should not be considered an epiphenomenon, but more so a causative component in migraine. Yet, clearly many lines of evidence establish that migraine is a neural disorder. We suggest that the vascular and neural theories can be linked by vascular activation of the nervous system (Figure 1). Understanding the communication between blood vessels, neurons and possibly mast cells will be integral in unraveling the pathophysiology of migraine and future studies should focus on dissecting this intersection of vascular and neural actions in migraine.
0 notes
Text
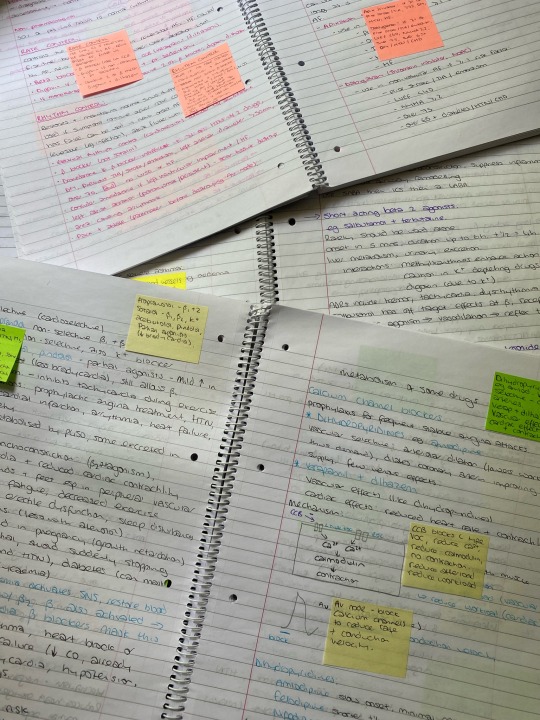
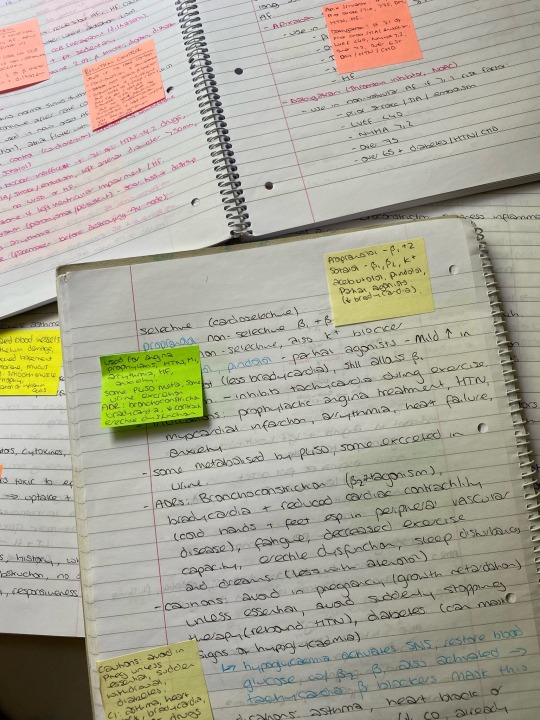
28/5/23 // 13.46
Yes these are my uni notes from 2018. Yes I’m glad I’ve kept them because today, I, a fully qualified pharmacist, could not figure out how beta blockers work and had to use these notes. Help
#I know they block beta but I don’t understand how that affects circulation#turns out they reduce CO and cause a tiny tiny bit of vasoconstriction which makes so much sense on the cold peripheries#because I was like??? but salbutamol causes dilation so how can beta blockers be used in htn#this is too much pharmacology. also I’ve spent an hour on this to write one line in my 2000 word assignment#help I’m a pharmacist get me out of here#mine#studyblr#studyspo#notes#studying#pharmblr#pharmacy#medblr#nurblr#pharmacology#pharmacodynamics#Maria does diploma#biology#pharmacy student#pharmacyblr
74 notes
·
View notes
Text
Famous angels never come through England &c.
5 notes
·
View notes
Text
tee emm eye but why is it that every time it gets cold out i get THEE worst cramps. i don't even have periods this should not be something i have to deal with
#speak friend and enter#it's chilly out today and i'm at that place in my birth control cycle that would normally be my period but instead of bleeding i just. hurt#and it's like 10x worse in the winter/fall. i know it's bc of the temp causing vasoconstriction and whatnot but still. blargh#i mean it's better than it used to be (i have anemia so you can connect the dots there) but words cannot describe how much i want a hysto
4 notes
·
View notes
Text
Sucks when your meds do something weird and you know you can't look it up. My adhd meds don't crash me very hard because they operate as ndris, only moreso, but there are definite things that happen when they wear off. Like the heat and the itch. As best as I can tell, it's a vasodilation effect that occurs when the stims, which constrict blood vessels by their nature (that's what all those warnings about high blood pressure are about) wear off and all the veins widen again. But there's no way to know and the good guess doesn't make me need my cooling towel any less. Still, I had a good day being back on them and I think the tradeoff is worth it for now.
#You can imagine the variables thrown into sinuses and stuff too when vasoconstriction can ease symptoms#And even prevent a migraine#Oh well#For now time for sleep
8 notes
·
View notes
Text
Took my second night of fluticasone, but it makes me so tired and achy and brain foggy and HUNGRY and gives me a sore throat and a cough and a headache ☹️ Makes me feel flu-y. I'm like weed/alcohol-tier dizzy. And nauseous (but hungry). Can't even see straight, my vision's so blurry. Godawful
#i already feel like shit constantly so i hope to god these side effects ease#i slept like twelve hours last night and remained so fucking groggy and fatigued after i woke up. fluticasone? maybe#i'm aware a lot of the side effects are due to the vasoconstriction#which raises blood pressure but i normally have LOW blood pressure so what gives. shouldn't that make me feel better#OH and this shit gives you thrush if you don't rinse your mouth after taking it! ain't chronic illness fun#personal#asthma#drug mention#alcohol mention
2 notes
·
View notes
Text
1 note
·
View note
Text

TSRNOSS, p 667.
#expansion of the Alu sequence#sialoproteins#glomerulus#xenobiotics#adrenal medulla#female infidelity#glycogenolysis#ACTH#norepinephrine#vasoconstriction#thermal conductivity of water#pregnancy#cortisol levels#antifreeze#glycerol#photolytic cleavage#water formation in the mitochondrion#Carboniferous#paraffin#oxygen levels#catalase#potassium permanganate#light petroleum
1 note
·
View note
Text
Son of a...
#tired of these wack side effects from strattera -_-#my face is so flushed and red I looked it up and it says its from the vasoconstriction#but its sooo annoying#and my heart rate keeps spiking too -_-#ill give it another week n see if i get acclimated
0 notes
Text
Only way to find out is to join the Sharing!
I wonder if a yeerk could fix my migraines. like how much power do they have over brain chemicals?
295 notes
·
View notes
Text
𝐬𝐭𝐮𝐝𝐢𝐞𝐬 | 𝐜𝐥𝟏𝟔
summary… charles tries to help his girlfriend study but that proves to be difficult when he doesn’t understand a single thing requested… yes! warning… none. pure fluff.
note… another old drabble request from the graves of my inbox. also as a med student, i adore this idea so much
𝙢𝙖𝙨𝙩𝙚𝙧𝙡𝙞𝙨𝙩

charles has never been the brightest tool in the shed when it came to academics. he supposes it comes with the occupation. growing up, he cared far too much about racing that he had no space left in his mind to care about school too. he was always meant to be a formula one driver so he never cared about the cell or the mitochondria.
ironically, you were the exact opposite. like him, you’ve known what you were meant to be the moment you got ahold of your first book. you’re going to be a doctor, a healer and you’ve dedicated yourself to that dream.
the human body is a beautiful machine, much like the universe. every little cell and atom circulating its vessel holds a purpose, creating a balance between life and death. it’s majestic, truly and a little bit scary. if one thing failed then the entire system could collapse and so you studied and studied and studied for ways to keep that system going, to cure ailments and diseases.
you thrive off academic validation and a minor superiority complex and yet somehow you’re the most anxious person charles has ever met.
he’s madly in love with you. this is a fact. him and his dream that required him to constantly put his life at risk and you with your dream of helping and saving people. really it was a match made in heaven. and charles is madly madly in love with you.
that’s the only reasonable explanation as he pulled himself out of his sim practice, seamlessly moving around the kitchen of your shared apartment as he prepared an ice coffee for you.
you’re drained and you’re on the verge of breaking down and so when he wrapped his arms around you and offered to help you study for your finals, you’d all but cried in gratitude.
no, charles leclerc didn’t care about the cell and mitochondria and but he cares greatly for you and so he’d study it if it meant you’d finally allow yourself to rest.
unfortunately for him, you’re way past learning about the mitochondria. instead you’re studying your worst enemy aka pharmacology.
“angiotensin receptor blockers prevent vasoconstriction and aldosterone release, causing a decrease in blood pressure and peripheral resistance,” you recite from the top of your head, still looking like you’re on the verge of tears but slightly better.
charles shook his head as he held the book you’d given him to help you study, his glasses on. “non, non, amour. it says here it’s ‘angiotensin receptor blockers selectively bind to the angiotensin I receptors in the blood vessels to prevent vasoconstriction and in the adrenal cortex to prevent release of aldosterone then lead to decrease in BP caused by decrease in peripheral resistance and blood volume.’”
you sigh again but couldn’t help the chuckle that escaped you. the first time he did it, you’d gotten frustrated but at this point, your brain is far too fried to even get annoyed at him. especially when even he looks like he’s about to start crying.
you pushed away the book from his hand, clumsily crawling over to him as you wrapped your arms around his neck, pushing him down so he’d be laying on the sofa and you on top of him.
“my love, i don’t need to memorize everything word for word from the book,” you explain as gently as you can for the third time. you know he’s just trying his best to help you.
“why?” he frowned. “wouldn’t it be better if you knew it exactly from the book?”
you giggled. “perhaps but no med student would ever survive memorizing twelve inch books word for word. we’d simply all break down and die.”
you hold yourself up, pushing his hair off his forehead before removing his glasses. he still looks confused but a lot of things honestly confused charles. thank god he has a smart girlfriend to explain everything to him.
“stop worrying about it,” you say. “i’ve studied enough and we both need a break.”
he sighed in relief, tightening his arms around you. “thank god i felt like my brain was put on a pressure dryer for a minute there.”

taglist: @ricsaigaslec @dragon-of-winterfell @coffeehurricanes @privcherry7 @miniminescapist @sebsdaniel @strelcka @writing-about-current-obsessions @amsofftrack @lostinketterdam @bisexual-desi @cialovessirlewis @multilovebot @lovelynikol16 @troybolton-14 @ohthemissery @dr3lover @myescapefromthislife @sunf1owerrq @the6ccnsp6cyy @t-nd-rfoot @navixfr @xjval @gridbunny
#charles leclerc#charles leclerc fluff#charles leclerc x reader#charles leclerc x y/n#charles leclerc imagine#charles leclerc one shot#charles leclerc x you#formula 1#f1#f1 x reader#f1 one shot
1K notes
·
View notes
Note
Hey, so this isn't meant as advice for you, this is me asking if you have experience with trying a bit of advice I heard, and what your experience was with it? Basically I was told that two things that can help with migraines is soaking your feet in hot/warm water (possibly with ginger?) and to do breathing exercises where you exhale more than you inhale. Have you heard this advice before? Did you try it and if so, did it work for you? I get migraines pretty rarely but it's always so debilitating when they do happen and "go somewhere quiet and dark for 2 days" isn't always viable but is the only reliable method Ive had so far, but Id be down to try something like this if it has any validity to it?
I have tried them, and they have never worked for me. Alternating ice and heat directly over the pain helps me more (especially heat over my "trigger" eye), but usually, just so I can try to sleep through the pain, otherwise I'm going to be awake the whole 20+ hours, and that's never fun.
Your mileage may vary, and tbh, it's worth trying as they are fairly easy to do -- and who knows, you might get lucky and have "easy*" migraines that respond to deep breathing and soaking your feet.
For what it's worth, I've heard some people get more out of the foot-soaking thing by also putting a cold cloth/ice pack on the back of their neck. It helps aid with vasodilation and vasoconstriction, which can sometimes be a factor in migraines.
Aside from correcting my atypical binocular vision disorder with vision therapy and corrective tinted prisms, the biggest help I've had for my migraines has been from taking B2 supplements as recommended by my neurologist.
There's some evidence to show that taking 400mg of b2 for 3+ months can help lessen migraine intensity and perhaps even prevent them. Supposedly it works better if you also take magnesium.
I used to just take magnesium which is a common migraine "hack," but it never did much for me. Adding in the high dose of B2 was what finally made a difference. My migraines are still 20+ hours, but they're less painful, and I can be somewhat functional with them.
Obligatory: Talk to your doctor before starting any new medications, including supplements.
Good luck. I hope you find a solution that works for you.
---
*No migraines are easy, but some of us have harder-to-treat migraines that don't respond to "easy" solutions. Whenever someone asks me if I've tried deep breathing and Excedrin because it always works for them, I am both happy for them but also want to throttle them, lol.
442 notes
·
View notes