#urine glucose test
Explore tagged Tumblr posts
Text
Vital Easy Elderly Care Kit for Home Wellness Monitoring
Ensure the well-being of your loved ones with the Vital Easy Elderly Care Kit! Designed to support the unique health needs of seniors, our comprehensive kit provides essential tools for monitoring and maintaining health at home.
At Vital Easy, we understand the importance of proactive care for elderly individuals. Our Elderly Care Kit includes:
Blood Pressure Monitor: Keep track of blood pressure levels easily and accurately.
Blood Glucose Meter: Monitor blood sugar levels to manage diabetes effectively.
Thermometer: Quickly and reliably check body temperature.
Medication Organizer: Stay on top of medication schedules with a user-friendly pill organizer.
Urine Test Strips: Detect key health markers such as glucose, protein, and pH levels.
Health Journal: Record vital signs, symptoms, and health observations for easy reference and communication with healthcare providers.

Why choose the Vital Easy Elderly Care Kit?
Convenience: Conduct essential health checks at home, reducing the need for frequent doctor visits.
Comprehensive Monitoring: Track multiple health indicators to ensure holistic care and early detection of potential issues.
Ease of Use: User-friendly tools designed with seniors in mind, ensuring ease and comfort.
Peace of Mind: Stay informed and proactive about the health of your loved ones, providing reassurance and support.
Empower your loved ones with the Vital Easy Elderly Care Kit – a complete solution for home health monitoring. Order now and take the first step towards comprehensive, compassionate care for the elderly. With Vital Easy, caring for your loved ones has never been simpler or more effective.
#elderly care kit#at home glucose test kit#urine calcium test at home#home health care kits#at home blood sodium test#urine sample test kits
0 notes
Text
Feedism health - Diabetes Mellitus
TW: feederism, feedism reality, medical issues, explicitly explained medical conditions
Hi! This post gonna be long, it is a bit more medical again. We are feedists, right. Many of us are overweight or obese, some also have high blood pressure and many other comorbidities. We overeat a lot, stuffing so much sugar and fat into our bellis or bellies of our feedees so that we gain as much as we want. Therefore we are at HIGH risk of developing diabetes.
I am a student of physical therapy, NOT A DOCTOR. But I kinda feel the need to educate our community a bit 📚. So there are some facts (from medical literature which i study for my exames) about diabetes that I think should be commonly known. It may scare you, it may make you horny (we are weird, especially death feedists, hi guys 🖤), I just want you to know this, if you feel strong enough:
What it is and important vocabulary:
It is a disease caused by malfunction of insulin secretion from pancreas, or by insulin resistence of target tissue (such as muscles) or combination -> in every case you have a problem with insulin and glucose in your body.
There are two types, type I (DMI) that is caused by autoimunne reactions and you can not prevent it. And type II (DMII) which is hella important for our community because you can literally eat yourself into it. The more you over eat, the more you weight, the less you move, the higher the probability of developing that disease. This post is mainly about DMII.
Glycaemia = how much glucose (form of sugar) is in your blood
Norm is 3,9-5,5 mmol/l. After eating usually max 7,8 mmol/l
Hypoglycemia = less than 3,3 mmol/l
Hyperglycemia = over 11 mmol/l
Insulin causes that glucose goes from blood to your cells so it can become part of your metabolism. On the other hand there are hormones that causes the opposite - more sugar in your blood (by various mechanisms) and those are adrenaline, kortisol, growth hormone and glukagon.
How to get diagnosis of diabetes mellitus type II:
Doctor takes a sample of your blood plasma and tests its glycaemia:
If it is done in two different days and in both cases your glycaemia is over 11 mmol/l
OR if it is over 7 mmol/l after not eating for at least 8 hours*
OR if you undergo oral glucose tolerancy test and it is positive (you drink 75 g of glucose in 200 ml of water, wait for 2 hours and your glycaemia is over 11 mmol/l)
...in any of these cases they probably give you a diagnosis of Diabetes Mellitus. This apllies for my country in the middle of Europe, idk about your countries but it could be very similiar.
OR! I know that in USA they are also supposed to measure glucated hemoglobin (HbA1c) and diagnose you with DM if it is over 48 mmol/l.
*if your results are between 5,6 to 6,9 mmol/l, you are prediabetic which means that your body already suffers but you can stop it and go back to full health by changing your lifestyle (read more bellow).
Smyptoms of DMII:
I gonna explain them in "normal" language. You may have just some or all of them:
you are thirsty a lot, you drink a lot, you pee a lot, you are still thirsty though
there is glucose in your urine which definitely should not (you will not notice it, lab will)
you lose weight, you feel tired
your vission is blurred
you have some of acute or chronical complications (more bellow)
Complications of diabetes AKA what may happen to you:
They are usually devided into two groups - acute that actually can kill you pretty quickly and chronic that deteriorate your quality of life. (In the worst hypothetical case you can become blind, with neurological pain, amputated leg and close to a stroke that may kill your ability to move and speak. Nice, isnt it? 🤢) So lets get a closer look into that. These things happen when you do not treat your diabetes well or ignore it at all (for example continue in overeating and gaining even after being diagnosed):
Acute complications:
Hypoglycemia - may occur in patients that are treated with insulin (or glinids or derivates of sulfonylurey), also after drinking alcohol (even when you eat with it or dink juice etc). You do not have enough glucose in your blood so your brain cells become to die and in the worst case you will fall "asleep" (into coma) in the evening at party and will not wake up in the morning because you simply die. Your body fights hypoglycemie by making more glucose from storages in your liver, muscle and fat mass. Symptoms are anxiety, blurred vision, inability to concentrate but also seizure and coma.
Diabetic ketoacidosis - occurs in patients with DMI, very dangerous, also can lead to death. If you dont aplicate insulin when you should, you become hyperglycemic, dehydrated and your body catabolise fat into ketone bodies.
If you overdo it with your stuffing session while you are diabetic you may hypothetically cause yourself a hyperglycemic hyperosmolar coma. You are dehydrated, pee a lot, your blood pressure is very low, so low that it can reach hypovolemic shock and you faint. Also you kinda damage your kidneys.
Cronic complications:
Instability between insulin and glucose causes damage to your blood vessels and nerves which may result in
Retinopathy - you slowly lose your vision or even become completely blind
Nephropathy - if you ignore that you have diabetes, you damage your kidneys, it is asymptomatic for a long time but may result in need of dialysis or even transplantation if not treated.
Neuropathies - very common and very annoying. Harms your nerves - all kinds of nerves which means motor (problems with movement), sensoric (problems with feeling anything - touch, pressure, pain, cold, warmth, vibrations etc. and "problems" means you feel it less, more or differently so for example contant pain tha cannot be stopped) and autonomus (causes erectile dysfunction and decrease of libido, slows down motility in your stomach and gut, makes you feel sick, causes vomiting, constipation and diarrhoea and many more)
Diabetic foot - tissues in your leg are so damaged that it may literally start to rot and in the worst cases leads to amputations. This complication is related to many things from little injuries to ulcerations to gangrenes with bacterias that kinda eats your fat, muscles and bones.
Aterosclerosis - higher risk for ischemic heart disease (angina pectoris, heart attack), lower limb ischemia (may cause pulmonary embolism) and stroke.
Other problems such as: inflamation of thyroid gland, celiac disease (you can not eat anything with wheat, barley and others), diseases of skin, mycotic infections, urological infections etc.
Treatment:
I hope you are at least a bit frightened now... So what can we do when we are prediabetic or even diabetic? Three things!
Diet - if you are overweight or obese then it is weight-loss diet plus diet counting how many carbohydrates and fat you eat. Losing weight really works honestly.
Physical activity - helps so much!!! In general you should walk at least 10k steps per day and do some aerobic exercise for at least 30 minutes 3-4 times per week. And it should be on 75 % of your maximal heart rate (how to count that at home: "220 - your age = ideal load") plus ofc any sport you like. If you do have diabetes, be very careful about any injuries because it can lead to the diabetic foot.
Meds - DMI insulin for sure. DMII usually gets first oral antidiabetics and only in some cases insulin. But over all meds are only part of the treatment, it reallly does not work well without taking care of your food or exercising. You need to change your lifestyle if you wanna get better (I know that some of you don't).
______________________________________
I hope this post gave you something, tought you something new and you know the risks of our kink better now. I do not want to tell you not to do it - I have that kink too and love it, gonna continue gaining. Just be aware about the consequences 💕
Uffff... that was long and complicated, I actually did my research for that and spent few hours making that post 😂. But it is still possible that i did some mistakes, did not understand something well etc - I am NOT a doctor, please believe more your health proffesionals than me, thank you. Im sorry if anything does not make sense or if I use some words in a strange way - english is not my native language and I do not know many medical terms and phrases, know them only in czech and latin so I translate it somehow based on that XD
Enjoy the candy that our kink brings to our life and stay as healthy as you wish 💕💕💕
~ Your Tessie
#feedism.#feederism.#feedism health#diabetes#feedism consequences#kink education#feedism education#feedee girl
37 notes
·
View notes
Note
Pregnancy still going okay?
Alastor has successfully survived through the first trimester of pregnancy.
But in the deer's opinion the ‘success’ is debatable. Not that anything abnormal happened, but he's simply exhausted by it. Now at 14, it is high time for another checkup. Last time Doctor Chaim had done more extensive tests, to make sure their children are developing at a normal rate.
Dr. Chaim: "I'm happy to let you know that we have the results back from the NT ultrasound and the NIPT blood test, and everything looks normal. The measurements for all three babies were within the expected range, and the blood test didn't show any signs of chromosomal abnormalities.
Lucifer, excited: “That's great!”
The king slings his arms around the demon who fondly rolls his eyes. Lucifer starts to play with his hair.
Alastor: “It is excellent”
Lucifer: “You know, you really should wear your hair like that more often”
Alastor: “Not a chance”
Hormonal changes made it harder to straighten, and to make matters worse, Alastor had overslept. So instead of having a half done job, the demon has simply put his hair into a little ponytail. Much to have s partners delight.
Dr. Chaim: “Okay, only a few things left. Please get in the scale”
Alastor, ears lowering: “It is rather obvious, that I put on weight”
Dr. Chaim: “Looks can be deceiving and I need the specific numbers”
Alastor: “Fine, fine!”
Reluctantly, he steps out of his shoes and on the scale, decidedly not looking down. His doctor, though, looks very closely.
Dr. Chaim: “Yes, all in order. You may step off”
Lucifer had been correct, the new set of clothes had been a welcomed change, and made him more comfortable in his own expanding skin. Well, as long as there isn't too much focus on it. But it is getting better with time. Especially since it now looks more like pregnancy and not just like he put on some weight.
Dr. Chaim: “Okay, that leaves us with one last thing!”
He hands Alastor a small cup.
Dr. Chaim: “I need a urine sample”
Alastor, glaring at him: “You are testing my patience, Doctor”
Dr. Chaim: “Yes, but mainly I'm testing your children, so go on. I am checking for glucose, bacteria, Ketone and so much more.”
The glare gets redirected to Lucifer, who looks slightly amused.
Alastor: “I'm holding you accountable for this misery”
Lucifer, nervous laugh: “Yeah, sorry about that.”
He makes quick business of it, and gets the doctor the urine sample.
Dr. Chaim: “Thank you very much. I should have the results ready by next time”
Alastor, sarcastic: “Wonderful. Shall I bring an entire canister next time?”
Dr. Chaim: “One of those cups is more than enough”
Lucifer: “Al, common, he's just trying to help”
Dr. Chaim: “Don't worry your majesty. I get all kinds of patients, I have thicker skin than that”
The doctor waves it off dismissively and goes over his checklist one more time.
Dr. Chaim: “That would be all I am checking today. Do you have any questions?”
Alastor: “Yes, actually. Regarding the magical growths. I could hardly find anything”
Dr. Chaim: “It varies from person to person. Especially if the children build stronger capabilities, their needs might fluctuate intensely. You might go from next to nothing to pretty solid magic reserves within the day. Just listen to your body and don't overexert yourself.”
Alastor, tense: “Right. Thank you, that would be all.”
The two leave after bidding goodbye.
Lucifer: “Are you worried about the magic thing?”
Alastor: “... A tad, admittedly. I do not enjoy being more… ugh vulnerable. But I suppose we will handle it, as always”
Lucifer: “Yeah! You bet!”
The enthusiasm does calm the demon.

#ask#send asks#ask blog#ask me anything#hazbin hotel ask blog#alastor the radio demon#hazbin alastor#hazbin hotel alastor#alastor#hazbin hotel lucifer#lucifer x alastor#lucifer hazbin hotel#lucifer#hazbin lucifer#lucifer morningstar#alastor x lucifer#radio demon#radioapple#mpreg#pregnant with triplets#triplets
26 notes
·
View notes
Text
welp today is my 20th diaversary! i could never bring myself to celebrate it, but always acknowledge the date. but to be honest, it's funny to me that i don't remember 17th of october, 2004. probably a mix of trauma and me being so severely ill that my memories of the weeks leading up to diagnosis are quite spotty. and i only got diagnosed because my mother put her foot down after doctors were set on sending me home without so much as a urine glucose test; this after weeks of endless doctor trips blaming my weight loss, incessant vomiting, and tiredness on anxiety. i was really close to dying. but here i am. two years ago when it was my 18th diaversary i joked about sending her to university. she should be getting close to getting a bachelor's degree by now and at times it feels like i am struggling to get a bachelor's degree worth of knowledge on diabetes management, but that is that. 20 years of diabetes and so far i have no complications even after struggling with it for a few years as a teen. here's to hoping i can get 20 more good ones
7 notes
·
View notes
Text
I really do feel like I can go conspiracy about porphyria brain because so much "information" about it is just 100% factually incorrect

^ like. Skin blisters are a symptom of CHRONIC porphyrias. Because it's a whole ass family of diseases. The ACUTE porphyrias do NOT affect the skin!! They're incredibly different diseases, like the only thing in common is that symptoms are caused by porphyrins, everything else is wildly different.
And yet so many ArTiClEs conflate them. So yeah idk I'm automatically incredibly skeptical of porphyria information in the first place, so ofc i find it odd that there's now websites for acute intermittent porphyria drugs talking about how important the treatment is to prevent permanent damage, and now most other sites list all that permanent damage shit. I know i sound kinda crazy here, but i don't even think this is a case of intentional malice necessarily. I mean MAYBE it could be i guess, manufacturers influencing websites to make ppl more likely to think they need the treatments, but honestly my main theory is just that other sites ripped from the drug websites like they rip other widely circulated porphyria misinformation because it's so rare that there's almost no one calling it out
Like the whole porphyria historically being associated with vampires thing and it causing King George's (iirc) madness are also 100% completely made up and still get endlessly regurgitated as fact :/
And like ive said literally every woman on my mom's side of the family has had AIP attacks and no one has had permanent damage from it. Even my sister's kidney thing that was only partially related completely went away. I know anecdotal evidence aint it sometimes, but this is a disease where you look up the safety of a drug and see that 3 people with aip took it and didn't have problems and it's therefore considered a safe drug bc the disease is so fucking rare that a sample size of 3 is pretty good because there jusr aren't enough ppl with the disease to get a larger sample size (it's also hard bc you cant just have ppl who have aip and have taken a drug and been fine. bc drugs can be completely safe for ppl when asymptomatic and not trigger attacks, but become unsafe once smth else triggers an attack and make it worse)
so in conclusion im not going to stress myself out further dooming about how this muscle/nervous system stuff could last forever bc i just don't believe that's the case. Im normally pretty strongly trust doctors, but so many doctors have tried to give my sister and mom incorrect treatments for AIP, not believed when my sister would say she had it, refuse to even test for it. So this is the one area where i absolutely do believe i know more than doctors. And tbf some doctors would agree. My mom once saw a hematologist for smth unrelated but mentioned the porphyria and he immediately said that she would have to go somewhere else for anything related to that because she was the first person in his MANY DECADES long career with aip and that he didn't feel comfortable even attempting to treat it bc she probably knew more about than him, bc his only experience was reading abt it in a textbook once
And like even if it's true theres nothing i could do abt it. My mom would take me to the ER if i asked, but there's no point bc they wouldn't give me the glucose/heme. I mean one of my past attacks i went and said that i was almost certain i was having an acute intermittent porphyria attack, and the doctor was super shitty going like "oh, what makes you think you have that?" and I said family history and she didnt give a shit. Wouldnt order the super simple urine test every single hospital in the country is capable of performing in less than an hour. Just said i had a virus and discharged me saying i was fine. And like i said my mom and sister habe had doctors that believed them when they said they had it but still refused to give them the right meds. In fact my mom's been given meds that are in the UNSAFE category of rhe porphyria drug database, meaning they actively make porphyria attacks worse.
Doctors don't know shit about porphyria, im genuinely better off staying home to ride it out. I'll eat a shit load of foods w lots of carbs/sugar which isnt as good as iv glucose but since getting that prescribed is apparently impossible it's better than nothing, if the pain's really bad i still have oxycodone left over from oral surgery, if i get nausea i have zofran on hand im prescribed for my migraines. Which is most likely exactly what i'd get in the hospital. My mom had an attack only like a month ago and despite her and my brother and my brother's very assertive friend who was also worried and showed up all told the doctor that it was porphyria and she needed iv glucose, and what happened? Doctor said she had food poisoning and she got painkillers and zofran, nothing actually addressing porphyria. So hospital would be giving me stuff i could have just taken here whilr also exposing me to all the bad respiratory junk going around
2 notes
·
View notes
Text
March 30th - April 25th
April 5th 2023
Apologies in advance cause this post is going to be lonnnnnnnng but I have chosen to share something very personal and real. So here it goes;
I always knew I wanted children. I have known ever since I was old enough to comprehend what having children & a family would actually mean. I was always set on having a baby the good old fashioned way. Toughing it out and delivering vaginally. Of course, I always understood that things could happen and that circumstances could change. Although, that couldn’t happen to me... right? Wrong.
When I first found out I was pregnant with our daughter, I was in disbelief. I think I bought about seven or eight pregnancy tests because I was in such disbelief at the first one. The initial feeling of ‘oh my god’, quickly turned into, ‘OH MY GOD I’M HAVING A BABY!’. I went into our room and told my partner (let’s call him J) I needed to talk to him about something. After he had finished up on his computer, I held out 3 positive pregnancy tests. J said, “Why are you showing me your positive COVID test”. He quickly realised it wasn’t a COVID test and he was over the moon.
Fast forward to being 33 weeks pregnant; I had done all of my scans. Which showed normal growth, normal sizing, and most importantly, a healthy baby. I had done not one, but two glucose tolerance tests. I found them not to be as bad as what everyone says they are. It just tastes like really strong lemon cordial. I had all my blood work come back normal, with just a minor iron deficiency. This is very common in pregnancies because bubba gets majority of it. I had just finished at my last growth scan and was headed home. I was feeling good, I had just seen my baby girl and was told/shown that she was measuring well and was healthy. As to be expected, I had gained some weight from being pregnant. Although, I was just happy that our baby was getting the nutrition she needed.
It was about 9:30, just after my Mother was due to start work, when I started to get a headache. So I had some water and went to bed. I woke up around midnight with a pounding headache, seeing stars in my vision and just feeling unwell and not myself. I messaged Mum and told her what was going on. She told me to get J to help take my blood pressure, have some Panadol & water and lie down with calming rain sounds to help. J helped me do my BP, which I thought was relatively okay (given I was a tad agitated and in pain from my headache). So I did what Mum told me to do and went to sleep. Woke up the next day and was feeling my normal self, so I went about my day as normal.
That evening, I started to feel the same way that I felt the previous night. This time, I kept it to myself. I thought it would go away just like it did the night before. Around 5/6pm, I went outside and sat in the pool because this strange feeling just wouldn’t go away. I spent a good 30-45 minutes out there. I went inside for dinner and to chill out whilst I tried to figure out what was causing me to feel so off.
Mum and I sat in the lounge room, watching TV, when she asked me if I wanted her to do my blood pressure. She asked because I was looking agitated and uncomfortable. She did it, and when I looked at her to ask how it was, she had this smile on her face. It was the type of smile one gives another person when they are trying to dull down how serious a situation. I asked Mum if it was good or bad. She just said, “I think you need to call the hospital and see what they say.” My blood pressure was 180/100mmHg. Which is very, very high.
I rang the maternity ward at the hospital. Sure enough, they said I needed to come in as soon as possible. We quickly packed a small bag with all the essentials for a SHORT hospital stay. I thought that we would only be in overnight and maybe the next day. When J and I got to the hospital, the first thing they did was reassess my blood pressure, take a urine sample, and some blood tests. All came back elevated. My blood pressure remained alarmingly high. My urine test came back with elevated protein and my bloods were marginally worrisome. I just kept asking if the baby was okay. I kept asking if this was causing her distress and what we could do to stop it. I was given medication, after medication, to try and bring my blood pressure down. However, nothing was seeming to work definitively. After multiple doses of anti-hypertensives, my blood pressure started to plateau around the 140-150’s. This was still not ideal, but better than what it was. I was feeling like rubbish at this point because of the anti hypertensives, pain medication, antacids, and anti nausea medications I had been given.
Our doctor came in at around 1am. She was was able to give us some news that, quite literally, made me sick to my stomach. It was from nerves, stress, and an entire range of other emotions. I was diagnosed with sudden onset severe pre-eclampsia. She told me that, if left untreated, could be fatal to Bub and I.
Preeclampsia is a complication of pregnancy which is detected by women having high blood pressure, high levels of protein in their urine (that indicates kidney damage) and/or other signs of organ damage such as epigastric pain (indicating the liver damage). The doctor then told me that I would be staying for almost 2 weeks. However, it ended up being a few days longer. It was all starting to make sense and fall apart, simultaneously. My general feeling of being unwell, the headaches, the rapid weight gain and fluid retention (I probably tripled in size within a week due to fluid retention which was a big yikes), the blurred vision and visual disturbances; the lot. And I was sick, I mean physically I threw up after we were told. I think it was from anxiety but it was probably because of all the medications I had been given. Our doctor reassured us and tried to calm our nerves, but I know I was out of my mind worried about bubba. As was J. Funnily enough, our daughter was healthy and unaffected by what was going on & it was my body that wasn’t coping however that very well could’ve changed at any given time.
That first night I would like to say was the worst it got. Unfortunately, it wasn’t. I was admitted to the maternity ward the next day where we received nothing but the best from the midwives. They were kind, caring, and were always checking in on us to see how we were coping. I think it was because they could see the mental and physical toll it was taking on not only me, but J and my Mum as well. During my stay on the ward, I had multiple different tests and scans to monitor by blood pressure, kidney, liver functions, and my overall health. I won’t lie, I really was unaware as to how unwell I was and how serious the situation was.
Due to the severity of my preeclampsia, we were told that our daughter would probably have to be born early around 37 weeks. At 37 weeks, a baby is considered to be full term. They have fully mature lungs, as the baby is getting ready to be born. I had asked the doctor, and the midwife, if it was still possible to follow our birthing plan of having a water birth. Unfortunately, as we were now a ‘high risk’ pregnancy, a water birth was out of the question. Then came the question of, "will I be able to have a vaginal birth with our baby?". This was an aspect of pregnancy that I was actually very eager to be able to experience. Originally, I wanted a water birth with as minimal medical intervention as possible. I felt like, as painful as Labor may be, it would be equally as beautiful to be able to bring our daughter into the world this way. My treating doctor told me that, although labor was not impossible, it was highly unlikely that I would be able to safely go through labor. She explained that I would likely need to have a caesarean. I was obviously 100% on board with whatever our little baby needed to be happy and healthy, but it still felt like I was stripped of having the birthing experience that I wanted.
It was a few days after I was admitted that we were informed that we wouldn’t be able to make it to 37 weeks. The doctors were worried my body and organs would give up due to the stress they were under. I said to the doctors I would at least get to 34 weeks (which was 4 days away). They were hesitant to wait that long. I thought I would be able to, because it was only just a bit of high blood pressure right? Clearly I was in a bit of denial about everything. Over the next few days, I had multiple blood tests, CTGS and vital signs attended. All showing that my body was struggling. My liver functions were declining. My kidneys were struggling. I was struggling to move due to the fluid retention. I was having issues breathing and doing everyday activities that I usually would’ve been able to do independently. My blood pressure, although much more controlled due to being on two different anti hypertensives 4-5 times a day, was still elevated. The CTG’s weren’t bad, but they weren’t good. So I was sent for an ultrasound to check on the baby’s measurements & they showed that the baby was measuring smaller than expected. Meaning she wasn’t getting everything she needed to grow healthily. That’s where I actually became concerned.
It all came to a head the morning of the 05/04/23, after a shitty sleep and another 2-3 hour CTG tracing. Mum had stayed overnight with me (she and J often took turns doing this). I turned to her and said, “I can’t do this anymore”. She could already see how exhausted I was (physically and mentally). I made a decision to let the treating team know that I needed something to be done that day. We weren’t seen by the initial obstetrician. Another obstetrician (let’s call him Doctor A) who works along side the obstetric team came to review me. Straight away, he asked how long the CTG trace had been trending that way. He asked how long it had been on for, if anyone was monitoring it, and what was the point if nothing was being done about it. The doctor asked me a few more questions about how I was feeling. They asked if I was I struggling, coping, etc... I told him that I was trying to make it to the 34 week mark, but I was unsure how much longer my physical and mental health could last. He left to discuss things with ‘the team’ and to see if a decision would be made that day. Around lunchtime, Mum and I had just taken a bite of our sandwiches when Doctor A came back. He asked how I felt about having a baby that afternoon. It was a definitive ‘let’s have a baby’. Mum and I (more so Mum who is a midwife and wasn’t letting on just how unwell and dangerous my situation was) felt relieved. Someone had decided on a plan, instead of just sitting and waiting.
That afternoon, after a quick phone call to J telling him to get his ass to the hospital ASAP, I was prepped. We went downstairs where we were about to meet our little girl. After about 45 minutes of trying to be cannulated, I was wheeled into the theatre room. They told me what the process would be, how long things would take, etc... It was time for me to have a spinal anaesthetic (that thing with the big needle. The one that numbs you so you don’t feel anything. Yeah... That thing...). I will admit that it was not as bad as I expected. It took two tries, but the most unpleasant part of it was losing feeling and control of my legs so fast. I still had to try and move around to get into position, but that’s just me whining. It all happened pretty quick after the spinal anaethetic. Or that’s how it felt to me at least. The anaesthetist asked us what we would like to listen to, music wise, whilst the procedure was happening. Obviously, it was a no brainer. The 1975 was the only option. Before we knew it, the doctor was telling us to "look up... look here....", and there she was. Our little girl. She was looking like a “mandrake” from Harry Potter, but she was healthy, breathing on her own, and squawking.
I think I was in some kind of trance or something, because it was all feeling so surreal. I mean... This little bundle of love wasn’t due for another month and a half. Yet here she was wrapped up in a blanket and in her Dad's arms. It's safe to say that I was in a bit of shock, but the best kind. It was a pretty quick ending of the caesarean. I was stitched back up and sent round to recovery, whilst Dad and Bub went to the special care nursery. This is where we would spend the next few weeks. I think I was delirious after everything happening so quickly, but I was stable. When I was taken back to the ward, the first thing I asked was "When can I see bub?" and "How is she doing?". Being wheeled back into an empty maternity ward room without my husband, my mother , or baby was very confronting. I felt alone, but not upset, because I knew they were with my baby girl. I felt really good. I think it was the best I had felt since I had been in the hospital.
However, after I returned to the ward, my midwife attended my vital signs. My blood pressure and other symptoms resulted in her calling a medical emergency. I was given more medication and they increased my observations overnight. Unfortunately, I had another medical emergency. They sent me back to the birth suit for 1:1 care. I had a 24 hour magnesium sulfate infusion running (to help bring down my blood pressure). I had a catheter re-inserted (was not a happy little Vegemite) and I spent the next 24hours having half hourly vital signs, hourly catheter output/input measures, and barely any sleep. This entire time, I hadn't even been able to hold my baby yet. I had minutes with her briefly, after she was born, before she was wrapped up and sent up to the special care nursery. It was a lot to internalise. I felt guilty because I hadn’t been able to cuddle our little girl since she had entered the world. During the night spent in birth suite, the midwife that took care of me was nothing but an angel. She could obviously see the toll that not being able to see (or hold) our baby was having on me. She could see how uncomfortable I was with being pricked, prodded, and my catheter blocking. I think it was just after 11pm when, after checking my blood pressure, our midwife said we could go and see our daughter. She would have to accompany us as I had IV’s running and I would have to go in a wheelchair, given my recent surgical wound and how unwell I was.
Seeing our little girl in the incubator, with an IV line in (along with all the other lines), was the hardest thing I think either of us have had to see. Seeing a little baby with lines and tubes in is hard; but when it is your child, I think it just stings that little bit more. Our daughter weighed 1780 grams when she was born. Our daughter had a nasogastric tube inserted, as she was too little to breastfeed or bottle feed. This was another blow, as I felt like I was letting my baby down by not being able to breastfeed. She was given IV glucose drips until she decided to yank her IV out. Just like her mother, she gave the doctor’s a challenge to reinsert the IV. Ultimately, they gave up because she was doing so well on just her 3r hourly feeds via the feeding tube. Her feeds were majority expressed breast milk, but in the beginning days (when my milk supply was just coming in) she had formula as a substitute. It was a relief that once my milk did start flowing. I was able to express and bottle it for her without any issues. I think we had about 6-7 litres of frozen breast milk in our freezer at one point. It was one less thing to worry about, given everything we had going on. Our daughter spent almost 4 weeks in the special care nursery. She recieved the absolute best care possible. I cannot thank the nurses and midwives enough for the care they gave my daughter & I. After those four weeks, we brought our little girl home. She looked a little bit funny sitting in such a big car seat.
4 weeks of visiting the hospital at all hours of the day. The hours spent holding our baby girl, giving her the tube feeds, changing her nappies, leaving the hospital in tears, feeling like the world was against me and sleepless nights at home wishing our baby was at home with us; it was a very tough time. I remember speaking to J in the hospital cafeteria “I feel like the world is against me, like I’m the butt of a bad joke and it’s not fair”. The guilt I felt over leaving our girl... I would leave the hospital either in tears, or angry at the world for our situation. I felt a lot of emotions at once. I was feeling guilty for not being able to hold my new baby and have a normal first interaction with our daughter. I missed out on the first few hours of skin to skin contact... Just because I was sick? I was angry at myself for being unwell and I felt like I had let our daughter down, beause I wasn’t there. I still get angry at times over this and it’s still something I have to deal with on the daily.
I take my hat off to all midwives, special care nurses, and neonatal nurses. I could not do what they do. Our daughter received the absolute best care from the most beautiful people in the special care nursery. We were reassured and checked in on every time we were there. They had offered support, given education, and assisted with her care when it was our turn to take the ropes. Those amazing people will always hold a special place in our hearts. I will never forget the kindness and care given to our family, especially when I wasn’t well enough to be able to.
I spent two weeks in hospital being pricked with needles, having constant CTG’s to monitor the baby, multiple blood tests, scans, and had numerous sleepless nights. I even had two emergency calls due to my BP being elevated. I had sudden weight gain and large amounts of swelling all over my body. The swelling was not just in my legs, but my arms and fingers as well. My hands still tingle from time to time due to the swelling and carpal tunnel I experienced. I was retaining large amounts of fluid, which was shown by my size and by how difficult it was for me to physically move. I have never felt so humiliated and disgusting. I relied on others to be able to help me move, wash, and do everything I am usually able to do.
I have never thought so lowly of myself. I refused to look in the mirror in the bathroom because I thought I looked disgusting and gross. I still felt this way after being told it wasn’t actual weight, it was the oedema that caused me to get so big. I have to continue to remind myself that the strectch marks and baggy skin is a normal part of pregnancy. I have bruises and scars from constantly being stuck with needles, multiple cannulas, and having blood tests. My liver functions and renal functions are only now starting to improve. However, I’ve had multiple follow ups with doctors from different departments and my GP to monitor these. I physically feel weaker. I can feel when my muscles are close to giving up, but that is slowly starting to change since I started exercising again. I struggle with anxiety from leaving the house, wondering if our daughter is unwell, and taking her out in public. Although, I am starting to slowly get better at managing these anxieties. I am still struggling to deal with how my body looked/looks now. Body image has always been a big issue for me. It will be an ongoing process, but one step at a time. Walking by myself, and walking with our daughter, has helped me cope with a lot of these negative thoughts. It has helped my mental and physical health immensely.
I’m slowly learning to accept that, while I might not have experienced giving birth how I would’ve liked, I am so very blessed and thankful to have a healthy and happy baby girl. She is thriving and becoming her own (very small) person. I have been left with some physical and mental scars from this entire ordeal, but I remind myself everyday about how lucky I am. I'm a Mum and our baby made it home safely. It has taken my almost 3 months for me to finally finish writing this. It brought back a lot of negative thoughts and upsetting memories, but getting my thoughts out on paper has helped me process this traumatic (yet wonderful) experience. It’s also made me so thankful that our little girl, who is just like her Mumma, is tough and resilient. Seeing her smile and laugh, makes everything I went through worth it.
31 notes
·
View notes
Text
Mobile Lab Services
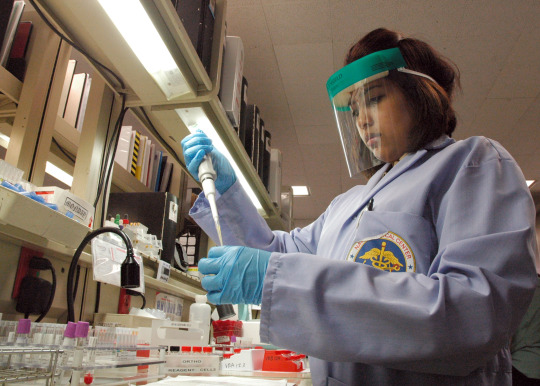
Mobile lab services are transforming healthcare. These services bring diagnostic and laboratory testing directly to your doorstep, eliminating the need for time-consuming trips to medical facilities. At MobileBloodDrawServices, we specialize in providing high-quality, reliable, and patient-centered mobile lab services. This innovative approach ensures you receive the care you need with minimal disruption to your daily routine.

What Are Mobile Lab Services?
Mobile lab services involve professional healthcare providers performing diagnostic tests at a location convenient for the patient, such as their home or office. These services typically include:
Why Choose Mobile Lab Services?
The shift towards mobile healthcare is driven by the growing need for personalized and convenient care. Here are the top reasons to choose mobile lab services at MobileBloodDrawServices:
Convenience and Accessibility Traditional lab visits often involve long waits, scheduling conflicts, and travel. With MobileBloodDrawServices, lab technicians come to you, saving you time and effort.
Patient Comfort For individuals who experience anxiety in clinical settings, mobile lab services offer the comfort of staying in familiar surroundings during testing.
Time-Saving Solutions Busy schedules make it challenging to prioritize healthcare. MobileBloodDrawServices ensures you don’t need to compromise your time, providing quick and efficient services at your preferred location.
Ideal for Vulnerable Populations Elderly individuals, disabled patients, or those with chronic illnesses benefit immensely from mobile services, as they eliminate the challenges of transportation and accessibility.
Services Offered by MobileBloodDrawServices
At MobileBloodDrawServices, we provide a comprehensive range of diagnostic and laboratory services designed to meet diverse patient needs.
Blood Draw Services Our certified phlebotomists are skilled in collecting blood samples for routine and specialized tests. Whether it’s a one-time test or part of ongoing health monitoring, we ensure accuracy and comfort.
Specimen Collection We collect various samples, including urine, saliva, and stool, for diagnostic purposes. Our processes adhere to strict hygiene and safety protocols.
Diagnostic Screenings From cholesterol and glucose testing to vitamin deficiency panels, we offer a wide array of diagnostic screenings to support preventive care.
Health Monitoring For patients managing conditions like diabetes, heart disease, or kidney issues, our mobile lab services provide regular monitoring, ensuring proactive health management.
Why Choose MobileBloodDrawServices?
At MobileBloodDrawServices, we are committed to delivering exceptional care. Here’s what sets us apart:
Experienced Professionals Our team of certified phlebotomists and lab technicians is trained to provide accurate, efficient, and compassionate care.
Advanced Technology We use state-of-the-art equipment to ensure precision in every test, from sample collection to laboratory analysis.
Flexible Scheduling We understand that everyone’s schedule is different. MobileBloodDrawServices offers appointments during evenings and weekends to accommodate your needs.
Transparent Pricing Our services are designed to be affordable, with no hidden fees. You’ll know exactly what to expect before your appointment.
Stringent Hygiene Standards We follow rigorous safety and hygiene protocols to protect patients and staff, ensuring a safe and clean testing environment.
Frequently Asked Questions (FAQs)
Is mobile lab testing accurate? Yes. MobileBloodDrawServices uses the same certified laboratories and advanced equipment as traditional facilities, ensuring accurate and reliable results.
How do I book a service? Simply visit our website or call our customer support team to schedule an appointment at your convenience.
What areas do you serve? We provide services across [specific service regions], including urban and suburban locations.
Are mobile lab services covered by insurance? Many insurance providers cover mobile lab services. Contact us to discuss your insurance plan and payment options.
Mobile lab services offered by MobileBloodDrawServices are revolutionizing the way patients access diagnostic testing. Combining convenience, comfort, and accuracy, these services cater to diverse needs while prioritizing patient care. Whether you’re managing a chronic illness, juggling a busy schedule, or seeking preventive screenings, MobileBloodDrawServices ensures a seamless and stress-free healthcare experience.
Contact US Phone : 703-689-1585 Fax : 1-800-887-9017 Email : [email protected] or [email protected] Address : 3057 Nutley Street, Suite 193, Fairfax Va 22031, United States Website: http://www.mobileblooddrawservices.com/home/
#Mobile Lab Services#mobileblooddrawservices#Mobile blood draw services#Stat blood draw#Blood draw at home services near me#Mobile blood tests
2 notes
·
View notes
Text
lmao realizing afterward that they didn't run a full urinalysis on me, just a strip and pregnancy test (after i said i had a hysterectomy)
was positive for glucose
then told "you dont have a uti you're fine" and also "your stones are in your kidney you wouldn't be able to feel them"
motherfucker do you know how many urines i've read where the strip was COMPLETELY normal and the sediment was RAGINGLY infected?
the worst part of working in a medical field is knowing exactly how much you're getting fucking ignored and glossed over
2 notes
·
View notes
Text

Kazu is at the vet being treated today. He is not feeling well. Friday Night I noticed he didn't want to eat as much and not eating from the table at night. We were still able to coax him to eat through the weekend with his paste treat on top of his food and gave him Cerenia tablet for nausea. This morning Kazu had an exam, bloodwork, and urinalysis done at our vet. He is slightly dehydrated, has too much glucose in his urine. He has never had ketones before. They said he had ketones now .5 , a slight UTI - Cocci 1+. His blood glucose was 379 before I took him to the vet. It was over 400 at the vet. They think this could be why he doesn’t feel good and doesn’t want to eat with all of these issues going on. They kept Kazu to give him an IV with fluids, she also said they were going to give him some regular insulin (I don’t know what that is) to try and bring his blood glucose down. Also based on what kind of UTI he has, they are starting him on Clavamox. They are also going to send off a fructosamine test. I really hope he’s going to be OK. I am so upset & worried about him. He has to be ok! We are picking him up later this afternoon. I will update you on how he’s doing then. I’m a stressed out worried sick mess! ❤️
4 notes
·
View notes
Text
Diabetes in Dogs

Even dogs eating healthy diets can suffer from diabetes. As with diabetes in humans, sometimes a dog’s body’s stops producing enough insulin or the cells of a dog’s body are unable to use the insulin that is produced. When either condition occurs, the result is diabetes mellitus, which causes excessive thirst and urination and extreme hunger accompanied by weight loss. To stabilize sugar levels, insulin therapy is the treatment at the outset and is usually required for the life of the dog.

Symptoms and Identification
Excessive thirst and urination: This happens because the huge quantity of sugar in the bloodstream spills into the urine and pulls water out of the bloodstream along with it, thereby causing increased urine production and urination. Increased drinking is the body’s way of trying to compensate for increased water loss through urination. Due to the high levels of bacteria-attracting sugar in the urine, urinary tract infections are also a routine finding.
Appetite increase paired with weight loss: This happens because when sugars cannot enter cells, the body is unable to effectively use the food it takes in as energy. Hunger is never satisfied despite a typically ravenous appetite, and weight loss is almost always a feature.
Other symptoms may include:
Urinary accidents in the house
Vomiting
Dehydration
Lethargy (tiredness)
Veterinarians may suspect canine diabetes if any suspicious clinical signs, such as increased drinking and/or urinating, have been observed at home. After performing a thorough physical examination, your veterinarian may recommend some of these tests to help confirm a diagnosis:
CBC (complete blood count) and chemistry profile: When a pet is ill, these tests are commonly performed together during initial blood testing to provide information about the pet’s organ systems. The CBC and chemistry profile may show dehydration, an elevated blood sugar level, or other changes that can occur with diabetes.
Urinalysis: Evaluation of a urine sample may show the presence of sugar (glucose) in the urine if a dog has diabetes.
Fructosamine: Fructosamine is a protein in the blood that binds very securely to glucose. The fructosamine level is therefore a close estimation of the blood glucose level, but it is less likely to change due to stress and other factors that affect the blood glucose level. Additionally, the fructosamine level indicates where the blood sugar levels have been during the previous two to three weeks. In a dog with diabetes, the blood sugar levels are usually high for long periods of time, which would be reflected by an increased fructosamine level.

Affected Breeds
Predisposed breeds include the Miniature Schnauzer, Standard Schnauzer, Poodle, Australian Terrier, Spitz, Bichon Frise, Samoyed, and Keeshond. Dogs of any breed, however, may acquire diabetes.
Treatment
In the long term, dogs with diabetes are often treated by insulin injection to help the body’s needy cells use sugar more efficiently. Dietary changes can also help, by tempering sudden spikes in blood sugar levels. Insulin injections, however, are generally started at the time of diagnosis and required long term to control the disease.
In the short term, some patients require hospitalization. Some may even need intensive care should their presentation be complicated by a variety of other problems secondary to the diabetes (this is a common scenario).
After treatment begins, periodic blood and urine tests are generally recommended. This helps ensure that the insulin dosage is right for your dog. Your dog’s weight, appetite, drinking and urination, and attitude at home can all provide useful information that helps determine if his or her diabetes is being well managed. Your veterinarian will consider all of these factors when making recommendations for continued management.
Many dogs live active, happy lives once their diabetes is well regulated. However, insulin therapy and regular monitoring at home and by your veterinarian are necessary for the rest of your dog’s life.
Prevention
Keeping your dog at a healthy weight can help reduce his risk of developing diabetes. However, for dogs that are genetically predisposed, their risk for developing disease remains higher even if they maintain a healthy weight.
9 notes
·
View notes
Note
Congrats on being a urine test overachiever! You’re going to give them a full cup! 😂 (kudos on using an emoji that looks like a puddle) I had surprise blood work at a recent dr appointment and was anxious my iced mocha latte was going to spike my glucose.
did it? i never thought about that but now i'm curious because i just sucked down an iced latte.
this is tmi and gross but i have to give urine a lot and i have an internal competition to try and make my pee as clear as possible. this stemmed from a nurse shaming me once for having dark colored urine and i explained to her that it was because i hadn't been drinking much water that day and she lied and said it was clearly indicative of a perpetual problem. which it wasn't. and i refuse to let anyone comment on the color of my urine again LMAO. if you're gonna judge my pee you're not gonna judge the color!!!!
4 notes
·
View notes
Text
Diabetes and Kidney Disease: The Connection and How to Protect Your Kidneys

Looking for a doctor near you in Brooklyn 11213 to help you manage your diabetes and kidney disease?
Visit Prasad Medical Center, where our team of experts will work with you to develop a personalized treatment plan to help you control your blood sugar levels, protect your kidneys, and improve your overall health.
Introduction:
Diabetes is a chronic health condition that affects how your body turns food into energy.
When you have diabetes, your body either resists the effects of insulin—a hormone that regulates the movement of sugar into your cells—or doesn’t produce enough insulin to maintain normal glucose levels.
Over time, high blood sugar can damage many parts of your body, including your kidneys.
Diabetic kidney disease, also known as diabetic nephropathy, is a common complication of diabetes.
It occurs when high blood sugar damages the tiny blood vessels in your kidneys, making it difficult for them to filter waste products from your blood.
If diabetic kidney disease is not treated, it can lead to kidney failure, a serious condition that requires dialysis or a kidney transplant.
You can reach our dialysis centers in Brooklyn in these places
What happens to your kidneys when you have diabetes?
When you have diabetes, high blood sugar can damage the tiny blood vessels in your kidneys.
This damage can make it difficult for your kidneys to filter waste products from your blood.
Over time, as the blood vessels in your kidneys become more damaged, your kidneys may not be able to function as well as they should.
This can lead to a buildup of waste products in your blood, which can cause a variety of health problems, including:
High blood pressure
Fluid retention
Anemia
Weakness and fatigue
Bone disease
Heart disease
Stroke
Kidney failure

How to protect your kidneys if you have diabetes:
The best way to protect your kidneys if you have diabetes is to control your blood sugar levels. You can do this by following your treatment plan, which may include taking medication, eating a healthy diet, and exercising regularly.
Know more about: OUR SPECIALIZED TREATMENTS - NEPHROLOGY
Here are some other tips for protecting your kidneys:
Monitor your blood pressure regularly: High blood pressure can damage your kidneys even further, so it’s important to monitor your blood pressure regularly and work with your doctor to keep it under control.
Maintain a healthy weight: Obesity is a risk factor for both diabetes and kidney disease. If you are overweight or obese, losing weight can help improve your blood sugar levels and reduce your risk of kidney disease.
Eat a healthy diet: A healthy diet for people with diabetes and kidney disease is low in saturated and trans fats, sodium, and sugar. It is also high in fruits, vegetables, and whole grains.
Exercise regularly: Exercise can help improve your blood sugar levels, blood pressure, and overall health. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Don’t smoke: Smoking damages your blood vessels and can make kidney disease worse. If you smoke, talk to your doctor about quitting.
When to see a doctor:
If you have diabetes, it is important to see your doctor regularly for checkups and kidney function tests. This is especially important if you have any of the following symptoms:
Swelling in your feet, ankles, or hands
Fatigue
High blood pressure
Blood or protein in your urine
Changes in urination
If you have any of these symptoms, your doctor may refer you to a nephrologist, a specialist in kidney diseases in Brooklyn.
Finding the best doctor near you in Brooklyn:
If you are looking for a doctor in Brooklyn to help you manage your diabetes and kidney disease, there are a few things you can do to find the best doctor near you:
Ask your primary care physician for a referral
Search for doctors in your area who specialize in diabetes and/or kidney disease
Read online reviews of doctors in your area.
Talk to your friends and family members who have diabetes and/or kidney disease to see who they recommend.
Once you have found a few doctors that you are interested in, you can schedule a consultation to learn more about their approach to treating diabetes and kidney disease.
Conclusion:
Diabetes and kidney disease are serious conditions, but they can be managed with proper care. By following your treatment plan, eating a healthy diet, and exercising regularly, you can help protect your kidneys and live a long and healthy life.
If you are looking for a doctor to help you manage your diabetes and kidney disease, there are a few things you can do to find the best doctor near you in Brooklyn.
#best doctor in brooklyn#doctors near brooklyn#best neurologist doctor in new york#clinic near me brooklyn#doctors near new york ny#the best neurologist in brooklyn#the best doctors in new york#medical doctor in brooklyn#best doctors in brooklyn#doctor in brooklyn ny#brooklyn clinic near me
2 notes
·
View notes
Text
Sooooo. Nephew Too may have Type 1 Diabetes. GP has sent him up the hospital for tests. His blood glucose and urine test are thru the roof apparently.
No idea how he's gonna cope with it if that's the case. Obvs Sis is gonna have to do most of the coping for him, which isn't gonna be fun. He's absolutely triggered by blood so regular fingerprick tests are out of the question, and I dunno if he'd put up with a flash monitor.
What a mess, eh?
Oh yeah, and a mistake at the vet meant Harley pretty substantially OD'd on her blood thinner last week. Caught the error after one dose, but it was *a lot* more than she should've had. Cue frantic call to out-of-hours vet, then the poison helpline (which cost 40 quid upfront!!!). She's been okay, but she's been vomiting for the last 24hrs. Vet says it could be a side effect, so we're watching her like a hawk.
Fucking hell.
ETA: Looks like they're keeping Nephew Too overnight. Poor mite's not handling it well, as I feared. He won't let them take blood coz blood terrifies him and he's scared of needles. He just wants to go home. Whole thing is really traumatic for him 😔.
Just hope the staff have experience dealing compassionately with autistic kids in this kinda situation.
ETA 2: They managed to take bloods finally. Dunno all the details yet, but from the sounds of things it's good news, so 🤞.
3 notes
·
View notes
Text
GOLDEN RULES FOR NURSES
NURSES
Golden Points to Remember
➥ Antiemetic drugs prevent vomiting.
➥ Intraosseous injections are given into the bone marrow.
➥ Intrathecal injections are given into the spinal cavity.
➥ Intramuscular injections should be given on 90° angle.
➥ Subcutaneous injections should be given on 45° angle.
➥ Intradermal injections should be given on 15° angle.
➥ Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
➥ Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
➥ For giving enema, left lateral position should be given.
➥ Air cushion is used to prevent bed sores.
➥ Hey’s test is performed for identify bile salts in urine
➥ Smith’s test is performed to found out presence of bile pigments in urine.
➥ Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
➥ Insulin may be added to TPN to offset the high concentration of glucose and heparin may be added to limit the formation of a fibrous clot at the tip of the catheter.
➥ The bones in the forearm act as a natural splint by providing support to an I.V. access site.
➥ Don’t select an I.V. site on a paralyzed or traumatized arm.
➥ The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
➥ Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
➥ If a client has a high temperature, notify the physician before administering any blood product.
➥ No solution or product other than normal saline should be added to blood or blood product.
➥ Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
➥ To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
➥ Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
➥ The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
➥ The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
➥ Heat loss due to contact with circulating air movement is known as Convection.
➥ The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
➥ Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature).
➥ Rectal temperature is the most reliable.
➥ Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks.
➥ Rigor: Sudden rise in body temperature with shivering as seen in malaria.
➥ Increased depth of breathing with normal respiratory rate is called Hyperpnea.
➥ Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
➥ Pulse deficit refers to the difference between apical pulse and radial pulse.
➥ A Blood Pressure Cuff that is too large will give falsely low reading of BP.
➥ Beneficence: Doing good for clients and providing benefit balanced against risk.
➥ Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
➥ Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
🛑 Explanation
1. Antiemetic drugs prevent vomiting.
Antiemetic drugs are medications used to prevent or treat nausea and vomiting. They work by targeting different receptors in the body, including those in the gastrointestinal tract and the central nervous system.
There are several types of antiemetic drugs available, including:
1. Serotonin antagonists: These drugs block the action of serotonin, a neurotransmitter involved in nausea and vomiting. Examples include ondansetron, granisetron, and dolasetron.
2. Dopamine antagonists: These drugs block the action of dopamine, a neurotransmitter involved in nausea and vomiting. Examples include metoclopramide and prochlorperazine.
3. Histamine antagonists: These drugs block the action of histamine, a neurotransmitter involved in nausea and vomiting. Examples include dimenhydrinate and meclizine.
4. Cannabinoids: These drugs work by activating cannabinoid receptors in the body, which can help to reduce nausea and vomiting. Examples include dronabinol and nabilone.
Other types of antiemetic drugs include benzodiazepines, which can help to reduce anxiety and nausea, and corticosteroids, which can help to reduce inflammation and swelling that can contribute to nausea and vomiting.
Antiemetic drugs may be prescribed for a variety of conditions, including chemotherapy-induced nausea and vomiting, postoperative nausea and vomiting, and motion sickness, among others. It is important to note that antiemetic drugs may have side effects, and should only be taken as directed by a healthcare professional.
GOLDEN POINTS FOR NURSES
2. Intraosseous injections are given into the bone marrow.
Intraosseous injections are given directly into the bone marrow, typically of the long bones such as the femur, tibia, and humerus.
This route of administration is used when intravenous access is not feasible or when a more rapid onset of action is needed, such as in emergency situations.
Intraosseous injections are commonly used in pediatric patients, as well as in adult patients in emergency and critical care settings.
The technique involves using a specialized needle to penetrate the bone and access the marrow cavity, where medications or fluids can be injected directly into the bloodstream.
GOLDEN POINTS FOR NURSES
3. Intrathecal injections are given into the spinal cavity.
Intrathecal injections are given directly into the spinal cavity, specifically into the subarachnoid space surrounding the spinal cord.
This route of administration is used to deliver medications or other substances directly to the central nervous system, bypassing the blood-brain barrier. Intrathecal injections may be used to treat conditions such as chronic pain, spasticity, and certain types of cancer, among others.
The technique involves using a specialized needle to puncture the spinal canal and access the subarachnoid space, where medications or other substances can be injected. Because of the risks associated with this procedure, including infection, bleeding, and damage to the spinal cord or nerves, it is typically performed under strict sterile conditions by trained medical professionals.
Golden rules for NURSES
4. Intramuscular injections should be given on 90° angle.
The angle at which an intramuscular injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 90-degree angle is appropriate for most adult patients receiving intramuscular injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less muscle mass, such as the deltoid muscle in the upper arm, a 45-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intramuscular injection.
Golden rules for NURSES
5. Subcutaneous injections should be given on 45° angle.
The angle at which a subcutaneous injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 45-degree angle is appropriate for most adult patients receiving subcutaneous injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less fat, such as the abdomen, a 90-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering a subcutaneous injection.
Golden rules for NURSES
6. Intradermal injections should be given on 15° angle.
Yes, that's correct. Intradermal injections are administered at a shallow angle, typically between 5 and 15 degrees, into the dermis layer of the skin.
The angle used for an intradermal injection is much shallower than for an intramuscular or subcutaneous injection, as the goal is to inject the medication just under the surface of the skin.
This type of injection is commonly used for skin testing, such as for tuberculosis or allergies, and is typically given on the inner forearm or upper back. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intradermal injection.
Golden rules for NURSES
7. Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
Yes, that's correct. Blood group AB is known as the universal recipient because individuals with this blood type can receive blood from any other blood type without experiencing an adverse immune reaction. This is because they have both A and B antigens on the surface of their red blood cells, and therefore do not produce antibodies against either antigen.
On the other hand, blood group O is known as the universal donor because individuals with this blood type can donate blood to individuals with any other blood type without causing an adverse immune reaction. This is because they do not have A or B antigens on the surface of their red blood cells, and therefore do not produce antibodies against these antigens. However, individuals with blood group O can only receive blood from other individuals with blood group O, as their immune system will recognize the A and B antigens as foreign and produce antibodies against them.
Golden rules for NURSES
8. Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
Yes, that is correct. Mercury is often used in thermometers because it is a liquid metal that has a high coefficient of thermal expansion, which means that it expands and contracts in response to changes in temperature. This makes it very sensitive to even small changes in temperature and allows for accurate temperature readings.
In addition, mercury has a low freezing point and a high boiling point, which means that it remains in a liquid state over a wide range of temperatures. This allows it to be used in both low-temperature and high-temperature applications.
However, it is important to note that mercury is a toxic substance and can be harmful if ingested or inhaled. For this reason, many countries have banned the use of mercury in thermometers and other consumer products, and alternative substances such as alcohol or digital thermometers are often used instead.
Golden rules for NURSES
9. For giving enema, left lateral position should be given.
Yes, the left lateral position is commonly used for administering an enema. This position helps to promote the flow of the enema solution into the rectum and prevents it from flowing back out.
To assume the left lateral position for an enema, the patient should lie on their left side with their left leg straight and their right knee bent slightly. They should bring their right knee up towards their chest to further open the rectal area. This position helps to straighten out the rectum and makes it easier to insert the enema tip.
It is important to follow proper enema administration technique and to use sterile equipment to minimize the risk of infection or injury. A healthcare provider should be consulted if you have any questions or concerns about administering an enema.
Golden rules for NURSES
10. Air cushion is used to prevent bed sores.
Air cushions can be used as part of a preventative strategy to help reduce the risk of bed sores, also known as pressure ulcers. Pressure ulcers can occur when there is prolonged pressure on a particular area of the skin, often caused by immobility or being in a seated or lying position for an extended period of time.
Air cushions are designed to distribute pressure evenly over the surface of the cushion, which can help reduce pressure on any particular area of the body. This can help to prevent the development of pressure ulcers and also provide greater comfort for the person sitting or lying on the cushion.
However, it is important to note that air cushions are just one component of a comprehensive pressure ulcer prevention plan. Other strategies may include repositioning the patient regularly, maintaining good skin hygiene, and providing adequate nutrition and hydration. It is important to work with a healthcare provider to develop an individualized care plan for preventing pressure ulcers in each patient.
Golden rules for NURSES
11. Hey’s test is performed for identify bile salts in urine
Hey's test is a laboratory test used to detect the presence of urobilinogen in urine, not bile salts. Urobilinogen is a colorless substance that is produced in the liver during the breakdown of bilirubin, a yellowish substance that is formed when old red blood cells are broken down.
Hey's test involves adding a chemical reagent to a urine sample, which causes any urobilinogen present to oxidize and turn pink or red in color. The intensity of the color change is used to determine the concentration of urobilinogen in the urine.
While Hey's test is not used specifically to identify bile salts in urine, elevated levels of urobilinogen in the urine can be an indication of liver disease or other medical conditions affecting the liver or biliary system, which can lead to the accumulation of bile salts in the urine. It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition.
Golden rules for NURSES
12. Smith’s test is performed to found out presence of bile pigments in urine.
No, Smith's test is not used to detect the presence of bile pigments in urine. Smith's test is a laboratory test used to detect the presence of protein in urine.
Bile pigments, such as bilirubin and urobilinogen, may be present in urine in certain medical conditions affecting the liver or biliary system. However, there are other laboratory tests that are more commonly used to detect these substances in urine, such as the bilirubin test or the urobilinogen test.
It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition that may be affecting the urinary system or other organ systems in the body.
Golden rules for NURSES
13. Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
Yes, that is correct. Total parenteral nutrition (TPN) is a form of nutrition therapy that delivers all of the necessary nutrients, including carbohydrates (glucose), amino acids, lipids, vitamins, minerals, and electrolytes, directly into the bloodstream through a vein. TPN is typically administered when a patient is unable to obtain adequate nutrition through the gastrointestinal tract, such as in cases of severe malabsorption, intestinal obstruction, or other medical conditions.
The specific components and concentrations of TPN are tailored to the individual patient's needs based on factors such as age, weight, medical condition, and laboratory values. TPN is typically administered in a hospital setting and requires close monitoring by a healthcare provider to ensure proper dosing and to monitor for any potential complications or side effects.
Golden rules for NURSES
14. The bones in the forearm act as a natural splint by providing support to an I.V. access site.
Yes, that is correct. The bones in the forearm, specifically the radius and ulna, can act as a natural splint by providing support and stability to an IV access site. When an IV catheter is inserted into a vein in the arm, it can be secured in place using a dressing or tape to prevent movement or dislodgement. However, the bones in the forearm can also provide additional support and stability to the IV catheter, which can help to prevent accidental dislodgement or complications such as infiltration or extravasation.
It is important to ensure that the IV catheter is properly placed and secured, and to monitor the IV site for signs of complications such as swelling, redness, pain, or leakage. If any of these signs are present, it is important to notify a healthcare provider immediately.
Golden rules for NURSES
15. Don’t select an I.V. site on a paralyzed or traumatized arm.
Yes, that is correct. When selecting an IV site, it is important to avoid areas that are paralyzed or traumatized. A paralyzed limb may have reduced blood flow and sensation, which can increase the risk of complications such as infiltration or extravasation. Additionally, a traumatized limb may have damaged blood vessels or tissues, which can also increase the risk of complications.
When selecting an IV site, healthcare providers typically look for a site that has good blood flow, easy access, and minimal risk of complications. The most common sites for IV access are the veins in the arms, but other sites such as the hands or feet may be used if necessary. Factors such as the patient's medical condition, age, and overall health may also be taken into consideration when selecting an IV site.
It is important to properly assess the patient's veins and select the most appropriate site for IV access, while also considering the patient's comfort and safety. Proper insertion and maintenance of the IV catheter, as well as monitoring for signs of complications, can help to ensure optimal outcomes for the patient.
Golden rules for NURSES
16. Don’t select an I.V. site on a paralyzed or traumatized arm.
It is important to avoid selecting an intravenous (IV) site on a paralyzed or traumatized arm. There are several reasons for this:
Risk of further injury: If the arm is already traumatized or paralyzed, there is a risk of further injury or damage to the arm if an IV is inserted in that area. This can result in nerve damage, muscle damage, or other complications.
Difficulty monitoring: If the arm is paralyzed, it may be difficult to monitor for signs of infection or other complications at the IV site. This can lead to delayed diagnosis and treatment of any problems that may arise.
Reduced blood flow: A paralyzed or traumatized arm may have reduced blood flow, which can affect the delivery of fluids and medications through the IV. This can result in poor IV access or incomplete delivery of medication.
In general, it is important to choose a site for IV insertion that is healthy, well-vascularized, and free from any injuries or abnormalities. If a patient's arm is paralyzed or traumatized, it is best to select a different site for the IV. This can help ensure that the IV is placed safely and effectively, without causing any further harm to the patient.
Golden rules for NURSES
17. The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
The basilic vein is one of the veins that can be used for a peripherally inserted central catheter (PICC) line. A PICC line is a long, thin tube that is inserted through a peripheral vein (usually in the arm) and passed through to the larger veins near the heart. This type of catheter is often used for patients who require long-term intravenous (IV) access for medications, fluids, or other treatments.
The basilic vein is located on the medial (inner) side of the upper arm, and it runs from the elbow to the axilla (armpit). It is one of the larger veins in the arm, making it a good candidate for a PICC line insertion. Other veins that can be used for a PICC line include the cephalic vein and the brachial vein.
When a PICC line is inserted, the healthcare provider will use ultrasound guidance to locate the basilic vein and insert the catheter through the skin and into the vein. The catheter is then advanced through the vein and into the larger veins near the heart. Once the catheter is in place, it can be used for the administration of medications, fluids, or other treatments.
It is important to note that while the basilic vein is a common choice for a PICC line insertion, the healthcare provider will consider several factors when choosing the best vein for each patient. These factors may include the patient's medical history, the size and condition of the veins, and the specific needs of the patient's treatment plan.
Golden rules for NURSES
18. Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
While it is true that the insertion of a peripherally inserted central catheter (PICC) line is typically done below the level of the heart, an air embolism can still occur during the insertion process or while the catheter is in place.
An air embolism occurs when air bubbles enter the bloodstream and block the flow of blood to vital organs. While air embolisms are rare, they can be life-threatening if not promptly recognized and treated.
During the insertion of a PICC line, there is a risk of air entering the catheter or the bloodstream. Healthcare providers take precautions to minimize this risk by carefully priming and flushing the catheter and using specialized techniques to insert and position the catheter.
However, even with these precautions, it is still possible for air to enter the bloodstream. This can happen if the catheter becomes disconnected or if the patient experiences a sudden change in position that allows air to enter the catheter.
To minimize the risk of air embolism, healthcare providers carefully monitor patients during and after PICC line insertion. They may use ultrasound or other imaging techniques to confirm proper catheter placement and check for any signs of air in the bloodstream.
If an air embolism is suspected, immediate treatment is required. This may include stopping the infusion, administering supplemental oxygen, and positioning the patient in a way that prevents the air from traveling to the heart or lungs. In severe cases, more advanced treatments may be necessary, such as hyperbaric oxygen therapy or surgery.
Golden rules for NURSES
19. If a client has a high temperature, notify the physician before administering any blood product.
If a client has a high temperature, it is important to notify the physician before administering any blood product. This is because a high temperature can be a sign of infection or another underlying condition that may be exacerbated by the administration of blood products.
Blood products are typically used to treat a variety of conditions, including anemia, bleeding disorders, and immune system disorders. While these products can be life-saving, they also carry certain risks, such as infection, allergic reactions, and transfusion reactions.
One of the key steps in ensuring the safe administration of blood products is to carefully screen patients for any underlying conditions or risk factors that may increase their risk of complications. This includes monitoring for signs of infection, such as a high temperature, before administering any blood products.
If a client has a high temperature, the physician may want to delay or modify the administration of blood products until the underlying cause of the fever can be identified and treated. This may involve further testing or evaluation to determine if the client has an infection or other condition that could increase their risk of complications from the blood product.
By notifying the physician of any signs of infection or other concerns before administering blood products, healthcare providers can help ensure the safe and effective use of these important treatments.
Golden rules for NURSES
20. No solution or product other than normal saline should be added to blood or blood product.
It is generally recommended that no solution or product other than normal saline should be added to blood or blood products. This is because the addition of other substances can increase the risk of adverse reactions and other complications.
Normal saline, also known as 0.9% sodium chloride, is a sterile solution of salt and water that is used to replace lost fluids and restore electrolyte balance in the body. It is often used as a diluent for blood and blood products because it is compatible with these substances and does not increase the risk of adverse reactions or complications.
Adding other solutions or products to blood or blood products can alter their composition and increase the risk of adverse reactions, such as transfusion reactions, allergic reactions, or infections. For example, adding medications or other substances to blood products can increase the risk of medication errors and other complications.
In some cases, healthcare providers may need to add a medication or other substance to blood or blood products to meet the specific needs of the patient's treatment plan. When this is necessary, it is important to carefully follow established protocols and guidelines to minimize the risk of adverse reactions or other complications.
Overall, the addition of any solution or product to blood or blood products should only be done under the direction of a healthcare provider with appropriate training and expertise in transfusion medicine.
Golden rules for NURSES
21. Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
Maslow's hierarchy of needs is a theory that suggests that human needs can be organized into a hierarchy, with lower-level needs taking priority over higher-level needs. According to Maslow's theory, the hierarchy of needs must be met in a specific order, with lower-level needs needing to be met before higher-level needs can be addressed.
The hierarchy of needs includes the following levels, in order from lowest to highest:
Physiological needs: These are the most basic needs, including the need for oxygen, food, water, shelter, sleep, and other bodily needs.
Safety needs: Once physiological needs are met, individuals have a need for safety and security, including physical safety, financial security, and stability.
Love and belonging needs: After safety needs are met, individuals have a need for love, affection, and a sense of belonging, including relationships with family, friends, and community.
Esteem needs: Once the need for love and belonging is met, individuals have a need for self-esteem and recognition from others, including achievement, status, and respect.
Self-actualization needs: Once all of the other needs are met, individuals have a need for self-actualization, including personal growth, self-fulfillment, and realizing their full potential.
In order to meet higher-level needs, lower-level needs must first be met. For example, an individual who is hungry and thirsty will not be able to focus on safety needs until their basic physiological needs are met. Similarly, an individual who is struggling to find a sense of belonging may have difficulty focusing on self-esteem needs until they feel a sense of connection with others.
By understanding Maslow's hierarchy of needs, healthcare providers can better understand the needs and priorities of their patients and develop treatment plans that address their most pressing needs first. This can help promote better outcomes and improve patient satisfaction.
Golden rules for NURSES
22. To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
To avoid staining the teeth, it is recommended that the client take a liquid iron preparation through a straw. Iron supplements can cause staining of the teeth, which can be unsightly and difficult to remove. By using a straw to take the supplement, the liquid can bypass the teeth and reduce the risk of staining.
In addition to using a straw, there are other strategies that can help minimize the risk of staining from iron supplements. For example, the client can rinse their mouth with water after taking the supplement to help remove any residual liquid from the teeth. They may also want to avoid brushing their teeth immediately after taking the supplement, as this can actually spread the iron around and increase the risk of staining.
If the client does experience staining from the iron supplement, there are several options for addressing the issue. One approach is to switch to a different form of iron supplement, such as a tablet or capsule, which may be less likely to cause staining. Alternatively, the client may be able to use a whitening toothpaste or receive professional teeth whitening treatment to help remove the stains.
Overall, while liquid iron preparations can be an effective treatment for iron deficiency, they can also cause staining of the teeth. By using a straw and taking other steps to minimize the risk of staining, clients can help ensure that they receive the benefits of iron supplementation without experiencing unwanted side effects.
Golden rules for NURSES
23. Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
Fluid oscillation in the tubing of a chest drainage system does not necessarily indicate that the system is working properly. In fact, fluid oscillation can be an indication of a problem with the system that requires attention from healthcare providers.
A chest drainage system is typically used to remove excess air or fluid from the pleural space in the chest. The system consists of a drainage tube, a collection chamber, and a series of tubing that connects the drainage tube to the collection chamber. The tubing is often clear, allowing healthcare providers to observe the movement of fluid and air through the system.
Fluid oscillation refers to the movement of fluid back and forth in the tubing of the chest drainage system. While some oscillation is normal and can indicate that the system is functioning properly, excessive oscillation can be a sign of a problem. For example, if there is a blockage in the tubing or collection chamber, fluid may be unable to flow freely and can cause increased oscillation. Similarly, if the drainage tube is not properly inserted into the pleural space, air may be drawn into the tubing and cause oscillation.
If a healthcare provider observes excessive fluid oscillation in a chest drainage system, they may need to take steps to address the underlying issue. This may involve adjusting the placement of the drainage tube, clearing any blockages in the tubing or collection chamber, or replacing a malfunctioning component of the system.
Overall, while some fluid oscillation in the tubing of a chest drainage system can be normal, excessive oscillation can be a sign of a problem that requires attention from healthcare providers.
Golden rules for NURSES
24. The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
The type of assessment that includes data related to a client's biological, cultural, spiritual, and social needs is indeed called a comprehensive assessment.
A comprehensive assessment is a holistic approach to assessing a client's health status that takes into account various aspects of their life, including their physical health, cultural background, spiritual beliefs, and social environment. By gathering information on these different factors, healthcare providers can gain a more complete understanding of the client's health status and develop a care plan that addresses all of their needs.
In a comprehensive assessment, healthcare providers may gather data through a variety of methods, including interviews, physical exams, laboratory tests, and observation of the client's behavior and interactions with others. They may also use standardized assessment tools to gather information on specific aspects of the client's health, such as their mental health status or their risk for falls.
Overall, a comprehensive assessment is an important tool for healthcare providers in understanding their clients' needs and developing an effective care plan that addresses all aspects of their health and well-being.
Golden rules for NURSES
25. The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
The vital signs are indeed a set of important measurements that healthcare providers use to assess a client's overall health status. The five vital signs are:
Temperature: The measurement of the body's core temperature. Normal body temperature ranges from 97.7°F to 99.5°F (36.5°C to 37.5°C).
Pulse: The measurement of the heart rate, or the number of times the heart beats per minute. A normal pulse rate for adults is between 60 to 100 beats per minute.
Respiration: The measurement of the breathing rate, or the number of breaths taken per minute. A normal respiration rate for adults is between 12 to 20 breaths per minute.
Blood pressure: The measurement of the force of blood against the walls of the arteries as the heart pumps blood throughout the body. Blood pressure is expressed in two numbers, with the systolic pressure (the top number) indicating the pressure when the heart beats, and the diastolic pressure (the bottom number) indicating the pressure when the heart is at rest. A normal blood pressure reading for adults is typically around 120/80 mmHg.
Pain: The subjective experience of discomfort or distress. Pain is assessed using various scales, such as the numeric rating scale (NRS) or visual analog scale (VAS).
Overall, the vital signs are important indicators of a client's overall health status, and healthcare providers regularly assess these measurements to monitor changes in the client's condition and develop an effective care plan.
Golden rules for NURSES
26. Heat loss due to contact with circulating air movement is known as Convection.
Yes, that is correct. Convection is the transfer of heat from a surface to a fluid (e.g. air or water) that is moving. When air moves over a surface, it carries away heat, causing the surface to cool.
This is why we feel cooler when there is a breeze or wind blowing, even if the air temperature is the same.
Convection is an important factor to consider when designing heating and cooling systems, as well as in understanding the behavior of the atmosphere and oceans.
Golden rules for NURSES
27. The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
Glass or clinical thermometers typically have a range of markings from 95-110°F (Fahrenheit) and 35-43.3°C (Celsius), which is the normal range of human body temperature.
The thermometer works by using a liquid, usually mercury, that expands or contracts as it is heated or cooled.
The length of the liquid column inside the thermometer changes depending on the temperature, and this is what is used to determine the temperature reading.
It is important to use the thermometer correctly and to read the markings accurately to get an accurate measurement of body temperature.
Golden rules for NURSES
28. Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature)
The normal rectal temperature is generally considered to be about 1°F (0.6°C) higher than the normal oral temperature, which is typically around 98.6°F (37°C).
This is because the rectum is a more accurate indicator of core body temperature, as it is located closer to the internal organs and is not affected by external factors such as food or drink.
However, rectal temperature measurement is generally reserved for medical purposes and is not recommended for routine temperature checks at home.
Oral temperature measurement is a more convenient and less invasive method that can provide a good approximation of core body temperature.
Golden rules for NURSES
29. Rectal temperature is the most reliable
Rectal temperature is generally considered to be the most reliable method of measuring body temperature because it provides a more accurate reflection of core body temperature.
This is because the rectum is located in the central part of the body, close to the internal organs which generate heat, and is not affected by external factors such as food or drink.
However, rectal temperature measurement may not be suitable for all individuals, especially for those who are uncomfortable with the procedure, those who have certain medical conditions, or those who have undergone rectal surgery.
Oral temperature measurement is a convenient and non-invasive alternative that can provide a good approximation of core body temperature for most people.
Other methods of temperature measurement include axillary (underarm) measurement, ear measurement, and forehead measurement, which may be suitable for certain populations or situations.
Golden rules for NURSES
30. Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks
Relapsing fever is a type of fever caused by certain bacterial infections, such as Borrelia species.
The fever episodes in relapsing fever are characterized by sudden onset of high fever, chills, headache, muscle aches, and other flu-like symptoms.
These episodes typically last for several days to a week or more, and are then followed by a period of normal temperature, which can last for days or weeks.
During the periods of normal temperature, the patient may feel completely well and may not have any symptoms.
However, the fever episodes can recur, often with different symptoms or severity, leading to a relapsing pattern of illness.
Treatment for relapsing fever typically involves antibiotics, such as doxycycline or penicillin, and may require several courses of treatment to fully eradicate the bacteria.
Golden rules for NURSES
31. Rigor: Sudden rise in body temperature with shivering as seen in malaria.
Rigor is a medical term used to describe a sudden onset of fever with chills and shivering. In the context of malaria, rigor is a common symptom that occurs during the febrile (fever) episodes, which are a hallmark of the disease.
Malaria is a parasitic infection caused by Plasmodium species, which are transmitted to humans by the bite of infected mosquitoes.
The febrile episodes in malaria are typically cyclical, with sudden onset of high fever, rigor, and other flu-like symptoms such as headache, muscle aches, and fatigue.
The fever may last for several hours to a few days, and is then followed by a period of normal or subnormal temperature.
The cyclical nature of the fever episodes is a key diagnostic feature of malaria, and helps to distinguish it from other febrile illnesses.
Treatment for malaria typically involves antimalarial medications, such as chloroquine, artemisinin-based combination therapy (ACT), or other drugs depending on the species of Plasmodium involved and the location of the infection.
Golden rules for NURSES
32. Increased depth of breathing with normal respiratory rate is called Hyperpnea.
Hyperpnea is an increase in the depth and intensity of breathing, without an increase in the respiratory rate.
It is often seen during exercise or other physical activity, as the body needs more oxygen to meet the increased demand.
It can also occur in response to certain medical conditions, such as metabolic acidosis or congestive heart failure.
Golden rules for NURSES
33. Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
Cheyne-Stokes respiration is a type of abnormal breathing pattern that is characterized by a cycle of alternating periods of tachypnea (rapid breathing) and apnea (temporary cessation of breathing).
The cycle typically lasts between 30 seconds to 2 minutes, and can be seen in patients with various medical conditions, such as heart failure, stroke, and traumatic brain injury.
It is caused by an abnormality in the respiratory centers in the brain, which affects the regulation of breathing.
Golden rules for NURSES
34. Pulse deficit refers to the difference between apical pulse and radial pulse.
Pulse deficit is a condition where there is a difference between the apical pulse (the heartbeat heard through a stethoscope over the apex of the heart) and the radial pulse (the pulse felt at the wrist).
It occurs when some of the heartbeats are not transmitted to the peripheral arteries, leading to a discrepancy between the apical and radial pulse rates.
Pulse deficit can be caused by various medical conditions, such as atrial fibrillation, premature ventricular contractions, and heart block. It is often an indication of an underlying heart problem and should be evaluated by a healthcare provider.
Golden rules for NURSES
35. A Blood Pressure Cuff that is too large will give a falsely low reading of BP.
No, that is not correct.
A blood pressure cuff that is too large will actually give falsely high readings of blood pressure.
This is because the cuff will not be able to adequately compress the artery, leading to an overestimation of the blood pressure.
Conversely, a cuff that is too small will give falsely low readings of blood pressure, as it will compress the artery too much, leading to an underestimation of the blood pressure.
It is important to use the appropriate size of blood pressure cuff for accurate readings of blood pressure.
Golden rules for NURSES
36. Beneficence: Doing good for clients and providing benefits balanced against risk.
Beneficence is one of the four main ethical principles in healthcare, which refers to the obligation of healthcare providers to do good and to promote the well-being of their clients.
This principle requires that healthcare providers act in the best interests of their clients and provide care that maximizes benefits and minimizes risks.
Beneficence also requires that healthcare providers make decisions that are based on the best available evidence and that they continually seek to improve the quality of care that they provide.
Balancing the benefits of treatment against the risks is an important aspect of beneficence, as healthcare providers must weigh the potential benefits of a particular treatment against the potential risks and side effects in order to make informed decisions about the best course of action for their clients.
Golden rules for NURSES
37. Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
An isotonic solution is a solution that has the same concentration of solutes as the fluid inside the cells of the body.
When an isotonic solution is administered, water moves freely across the cell membrane in both directions, without changing the concentration of solutes on either side of the membrane.
This is because the concentration of solutes in the isotonic solution is equal to the concentration of solutes inside the cells, so there is no gradient to drive the movement of water in one direction or the other.
One example of an isotonic solution is 0.9% NaCl (normal saline), which is commonly used for intravenous fluid administration to replace lost fluids and electrolytes in the body.
Golden rules for NURSES
38. Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
No, that is not entirely correct.
A hypertonic solution is a solution that has a higher concentration of solutes than the fluid inside the cells of the body. When a hypertonic solution is administered, water moves out of the cells and into the extracellular fluid, causing the cells to shrink.
This is because the concentration of solutes in the hypertonic solution is greater than the concentration of solutes inside the cells, creating a gradient that drives the movement of water out of the cells.
An example of a hypertonic solution is 3% saline, which is used to treat hyponatremia (low sodium levels). 5% dextrose is actually an isotonic solution, because dextrose (a form of glucose) is rapidly metabolized by the body, leaving only water and a small amount of electrolytes in the solution. When 5% dextrose is administered, it initially acts as an isotonic solution, but once the dextrose is metabolized, the remaining fluid becomes hypotonic (lower concentration of solutes than inside the cells).
It is important to note that the effects of hypertonic and hypotonic solutions on the body depend on the concentration of the solutes in the solution, as well as the rate and volume of administration. Administration of hypertonic or hypotonic solutions must be carefully monitored to avoid adverse effects on the body.

2 notes
·
View notes
Text
Discover Fast, Reliable Medical Care at Tarpon Springs’ Trusted Walk-In Clinic
When unexpected health issues pop up, knowing where to go for fast, reliable treatment is a game-changer. Whether it’s a sore throat that won’t quit, a sprained ankle from a weekend activity, or a last-minute physical for school or work, walk-in clinics like the one in Tarpon Springs offer a convenient and dependable solution.
In a world where waiting weeks for a doctor’s appointment or spending hours in an emergency room isn’t always realistic, more families are turning to local urgent care centers for same-day attention—and for good reason.
Why More People Are Choosing Walk-In Clinics in Tarpon Springs
Walk-in clinics have become the go-to for patients who need quick access to medical professionals without the hassle of scheduling. These facilities are designed to handle non-life-threatening conditions, helping you save time and money while still receiving expert care.
At our trusted Tarpon Springs location, patients ages 3 months and older can be seen for a broad range of common illnesses, injuries, and preventive services—all under one roof.
What You Can Expect at a Walk-In Clinic
Not sure if your condition is appropriate for a walk-in visit? Here are some of the most common reasons people seek urgent care services:
Sore throat, flu, and cold symptoms
Bronchitis and breathing issues
Sprains and minor fractures
Allergies and sinus infections
Stomach flu symptoms like nausea, vomiting, or diarrhea
Burn care and minor skin injuries
Eye infections and irritation
Lab testing and rapid diagnostics
One of the biggest advantages of a walk-in clinic is flexibility. These centers offer extended hours—open 8 a.m. to 8 p.m., seven days a week—so you can get care without disrupting your work, school, or family schedule.
Highlighted Services That Set Tarpon Springs Apart
The medical team at this location goes beyond just basic care. Patients can also access a variety of specialty services, including:
Lab draws and diagnostics such as hemoglobin and glucose levels
Flu testing and COVID-19 testing for seasonal protection and peace of mind
Urine pregnancy tests for early detection and guidance
Rapid RSV and mono testing to diagnose quickly and treat efficiently
Abscess drainage and minor procedures, performed on-site
Occupational health services for employees and employers
School, sports, and camp physicals, often with same-day availability
These options make it easy to address several health needs in a single visit.
Benefits of Choosing Walk-In Clinics Over Traditional Appointments
Still wondering if a walk-in clinic is right for you? Consider these benefits:
No appointment needed – perfect for sudden health concerns
Lower cost compared to emergency room visits
Minimal wait times and efficient check-ins
Extended hours, including weekends
On-site lab work and imaging, reducing the need for follow-ups
Plus, with the “Save My Spot” feature, you can check in online to further reduce your waiting time upon arrival.
What Makes This Tarpon Springs Clinic Unique
Unlike many facilities that only treat a narrow range of symptoms, this location stands out by offering a holistic mix of urgent and preventive services. Whether you're managing allergies, concerned about a child’s lingering cough, or simply need a flu shot, the clinic is equipped to deliver personalized, compassionate care.
If you're looking for accessible healthcare that doesn't sacrifice quality, the Tarpon Springs urgent care team offers the perfect blend of expertise, convenience, and reliability.
Other Helpful Services You Should Know About
Here are a few more examples of what’s available when you visit:
Mono Testing Tarpon Springs
Eye Infections/Problems Tarpon Springs
Burns Tarpon Springs
Breathing Treatment Tarpon Springs
Physicals Tarpon Springs
Stool Guaiac Testing Tarpon Springs
Glucose and Hemoglobin Testing Tarpon Springs
These services are essential for families, working professionals, and seniors alike, offering easy access to necessary care, all from one location.
Final Thoughts: Making Healthcare Easier, One Visit at a Time
Life is unpredictable. Fortunately, your healthcare doesn’t have to be. For residents and families in and around Tarpon Springs, walk-in care offers the ideal mix of convenience, affordability, and expert service.
Urgent care near me at Tarpon Springs Urgent Care 40545 US Hwy 19 N unit a, Tarpon Springs FL 34689
Whether it’s your child’s unexpected fever, a work-related physical, or a sudden stomach bug, you can count on your local clinic to get you back on your feet quickly—and with the care you deserve.
#TarponSprings#UrgentCare#WalkInClinic#FamilyHealth#SameDayCare#MedicalServices#FluSeason#HealthcareAccess#PreventiveCare#NoAppointmentNeeded#LocalHealthcare#FastTrackUrgentCare#AffordableCare#EverydayHealth
0 notes
Text
Your Guide to a Trusted Primary Care Clinic in San Antonio, Texas
When searching for a Primary Care Clinic in San Antonio, finding a provider that offers both physical and mental health services is essential. At Renew Health Center, we deliver compassionate, affordable, and personalized care for individuals and families—whether you’re uninsured, underinsured, or simply need reliable healthcare near me.
Why Choose Renew Health Center?
Located at 7434 Louis Pasteur Drive #209, San Antonio, TX 78229, our clinic is just minutes away from key neighborhoods and major medical districts. We focus on building long-term relationships and providing a one-stop solution for your health concerns—no matter your background or health history.
What Sets Our Primary Care in San Antonio Apart?
Complete Chronic Care From diabetes and high blood pressure to hormonal imbalances, we help manage ongoing conditions with tailored plans.
Full Diagnostic Services Need a quick flu test, urine pregnancy test, or RSV check? Our walk-in clinic near me ensures rapid diagnostics.
Urgent & Preventive Services We treat minor injuries, provide physicals, and focus on preventive screenings to catch issues early.
Mental Health Support Our holistic care includes mental wellness, ensuring your emotional and psychological health is prioritized.
Affordable Options We accept most insurance and offer discounted self-pay rates—making care accessible to all.
Extended Hours Open daily from 8 a.m. to 8 p.m., we accommodate your schedule with same-day appointments.
Local & Accessible – Primary Care Near Me
Conveniently located on Google Maps, our clinic offers an easy-to-reach solution when you search for primary care near me or need help navigating sudden health concerns.
Services You Can Rely On:
Respiratory Care: Asthma, pneumonia, and bronchitis treatment
Infections & STDs: Comprehensive testing and treatment
Pediatric to Geriatric: Serving all ages with family medicine
Lab Services: On-site blood tests, glucose checks, and more
Men's and Women's Health: Preventive screenings and hormone support
We’re proud to serve as your Primary Care Clinic in San Antonio, Texas, providing both immediate and continuous care.
#PrimaryCareClinic#SanAntonioHealthcare#WalkInClinicNearMe#MentalHealthSupport#SanAntonioDoctors#FamilyMedicine#PreventiveCare#ChronicCareManagement#AffordableHealthcare#PrimaryCareNearMe#RenewHealthCenter#SanAntonioPrimaryCare
0 notes