#urine catheter change at home
Explore tagged Tumblr posts
Text
Urine Catheter Change At Home | Catheter Change At Home
Changing a urinary catheter at home can be done safely with the right preparation and technique. Here’s a step-by-step guide:
Supplies Needed:
- New catheter (make sure it's the correct type and size)
- Sterile gloves
- Antiseptic wipes or solution
- Lubricant (if applicable)
- Clean container for the used catheter
- Absorbent pad or towel
- Disposal bag for used materials
Procedure:
1. **Wash Hands:** Begin by washing your hands thoroughly with soap and water. Dry them with a clean towel.
2. **Prepare the Area:** Find a clean, well-lit space. Arrange everything you'll need close at hand.
3. **Put on Gloves:** Wear sterile gloves to maintain cleanliness.
4. **Remove Old Catheter:**
- If it's a balloon catheter, deflate the balloon by using a syringe to draw out the saline.
- Gently pull out the catheter. If you encounter resistance, stop and consult a healthcare professional.
5. **Clean the Area:** Use antiseptic wipes to clean the area around the urethra.
6. **Prepare the New Catheter:**
- If needed, apply lubricant to the tip of the new catheter.
- Ensure that the catheter is sterile and handle it by the end that will not enter the body.
7. **Insert the New Catheter:**
- Gently insert the catheter into the urethra, advancing it until urine begins to flow.
- If it's a balloon catheter, inflate the balloon according to the instructions.
8. **Secure the Catheter:** Use tape or a catheter securing device to keep it in place.
9. **Dispose of Old Materials:** Place the used catheter and gloves in a disposal bag.
10. **Wash Hands Again:** Remove your gloves and wash your hands thoroughly.
Aftercare:
- Monitor for any signs of infection, such as fever, increased pain, or unusual discharge.
- Keep the area clean and dry.
- Observe any further guidance that your healthcare practitioner may provide.
Important Tips:
- Always seek the advice of a medical expert if you have any questions or concerns.
- Make sure to have a backup plan in case of difficulties during the change.
If you're ever unsure about the procedure, don't hesitate to seek help from a healthcare provider. — Carevive Healthcare Pvt. Ltd.
0 notes
Text
Frequently asked questions
When will the full game be released?
The release date for the full version is still to be announced. I work on this visual novel in my free time, so progress may vary. Currently, the project is in its early stages, making it difficult to project a completion date. As development progresses and I get closer to finishing, I hope to have a clearer timeline.
Is MC really in a hospital?
It is intentionally ambiguous whether the MC is truly in a hospital. The absence of nurses and Dr. Anselm being the only one attending to the MC are deliberately meant to provoke player suspicion. This mystery and the setting’s true nature are meant to unravel in later chapters.
Where did the MC's pee go?
The MC has a urinary catheter, a medical device used to drain urine from the bladder into an attached collection bag.
Urine collection bags connected to a catheter are typically changed every 5 to 7 days.
In the later chapters, there will come a time when Anselm has to change the MC's peepee bag.
Does MC actually need a urinary catheter?
In cases of severe traumatic brain injury (TBI), a urinary catheter may be necessary, especially in the early stages of recovery. TBI can lead to a range of symptoms, including impaired mobility, cognitive changes, or decreased control over bodily functions.
Also MC was unconscious for 2 days before waking up, catheters are commonly used for unconscious patients.
Will MC ever take a shower?
Yes I was planning to use this as content for later chapters.
Fun fact : Traumatic Brain Injury (TBI) patients in hospitals usually do not take showers independently, especially if they are in a critical or unstable condition. Instead, they are often given sponge baths or bed baths by staff to maintain hygiene without moving them too much, which could be risky. huehue
Will there be an ending where MC and Anselm are together?
Yes, absolutely! There will be an ending where MC and Anselm end up together. These endings will naturally come at the game's conclusion, and as I get closer to writing the finale, I'll have a clearer idea of how many good and bad endings there will be in total.
Was Anselm the one to cause MC's injury?
So this mystery is also to be unfolded in the later chapters. I hope readers understand that this visual novel has mystery/horror elements, there wouldn’t be much of a story if I revealed everything outright (ᗒᗨᗕ)
Does Anselm love the MC or just taking care of them?
Anselm's heart belongs entirely to the MC; they're the only one he truly loves.
Is Anselm a dog or cat person? or any other animal?
Anselm doesn’t usually keep pets, as he’s often away and lacks the time to care for one. But if he and the MC were living together and the MC wanted a pet, he would happily bring one home and enjoy caring for it together with them.
If he could, Anselm would create a beautiful bird terrarium—a place where he could observe them freely within a controlled space. There, they’d be safe, unable to leave but he alone is able to admire their beauty.
194 notes
·
View notes
Text
chatgpt explanation of the suite of feminization procedures necessary to create an indistinguishable woman ( not perfect)
Preoperative Phase
Preoperative Appointment:
Final Consultation:
The patient meets with the surgical team to discuss the procedure in detail.
Final consent forms are signed, and any last-minute questions are answered.
Medical and Psychological Evaluation:
Comprehensive health assessment including blood tests, imaging, and psychological support.
Detailed explanation of the recovery process and postoperative care.
Day of Surgery:
Arrival at the Hospital:
The patient checks in at the hospital and is escorted to the preoperative waiting area.
The patient changes into a hospital gown, cap, and compression socks.
Preoperative Preparation:
IV line is started for administering fluids and medications.
Baseline vital signs are recorded, and the patient is given a sedative to help relax.
The patient meets the anesthesiologist who explains the anesthesia process.
The surgeon visits to review the surgical plan and answer any final questions.
Transport to Operating Room:
The patient is wheeled to the operating room on a gurney.
Final identification checks and surgical site markings are made.
Intraoperative Phase
Anesthesia and Initial Prep:
Anesthesia Administration:
The patient is connected to monitoring equipment to track vital signs.
Anesthetic drugs are administered through the IV, inducing unconsciousness.
An anesthesia mask is placed, and the patient is intubated for airway management.
Eye ointment is applied, and the eyes are taped shut to prevent dryness.
Sterile Prep:
The patient’s body is cleaned with a pink antiseptic solution.
A urinary catheter is inserted to manage urine output during surgery.
Surgical Procedures:
Orchiectomy:
An incision is made in the scrotum, and the testicles are removed.
The incisions are closed, and the area is dressed.
Penile Inversion Vaginoplasty:
Penile skin is deconstructed and inverted to form the vaginal canal.
Scrotal skin is used to create the labia majora and minora.
Nerve bundles are used to construct the clitoris.
The urethra is shortened and repositioned.
Stem cell and nanobot therapies are applied to enhance healing.
Facial Feminization Surgery (FFS):
Procedures may include brow lift, rhinoplasty, jaw and chin reshaping, and tracheal shave.
Each step is performed with precision to feminize facial features.
Waist Contouring:
Liposuction is performed to remove excess fat and contour the waistline.
Fat grafting may be used to enhance the hips for a more feminine silhouette.
Breast Augmentation:
Incisions are made, and implants are placed to achieve desired breast size and shape.
Bioengineered implants ensure natural feel and appearance.
Buttock Augmentation:
Fat grafting or implants are used to enhance buttock size and shape.
Advanced techniques ensure minimal scarring and natural results.
Estrogen Implant Placement:
Hormone-delivery implants are placed to provide continuous estrogen therapy.
The implants are fine-tuned for optimal hormone balance.
Postoperative Phase
Immediate Postoperative Care:
Recovery Room:
The patient is moved to a recovery room and monitored closely as they wake up from anesthesia.
Pain management and anti-nausea medications are administered as needed.
Initial Assessment:
Vital signs are monitored, and the surgical sites are checked for any complications.
The patient is kept in a semi-upright position to promote breathing and comfort.
Instructions and Mobility:
The patient is given instructions on how to move and care for surgical sites.
Gradual introduction to liquids and soft foods.
Ongoing Postoperative Care:
Hospital Stay:
The patient remains in the hospital for a few days for close monitoring.
Regular check-ups by the surgical team to ensure proper healing.
Discharge and Home Care:
Detailed discharge instructions are provided, including wound care, medication regimen, and activity restrictions.
Arrangements for follow-up appointments and physical therapy sessions.
Long-term Recovery:
Gradual resumption of daily activities as healing progresses.
Ongoing hormone therapy adjustments and psychological support.
Regular follow-up appointments to monitor the results and address any concerns.
Final Outcome:
Physical and Aesthetic Results:
Natural-looking and functional vaginal canal with satisfactory depth and sensation.
Feminized facial features, contoured waist, enhanced breasts, and buttocks.
Hormone levels are balanced with the help of estrogen implants.
Psychological and Social Adaptation:
Continued psychological support to help adapt to the new gender identity.
Social integration and increased confidence in personal and professional life.
This detailed step-by-step guide outlines a comprehensive and futuristic approach to M-to-F sex reassignment surgery, incorporating advanced technologies and procedures to ensure optimal outcomes for patients.
#anesthesia#intubated#surgery#medfet#surgeon#intubatedlover#female surgery#medical equipment#anesthesia mask#intubation
19 notes
·
View notes
Text
I know folks are probably getting tired of this by now so you get a tag AND a cut.
But I feel like discussing this sort of thing might help people sometimes? since it's a first person account instead of listicles online.
What they did and didn't tell me about having stents.
They told me why: Facilitates drainage which takes strain (pressure) off of the kidneys and helps the antibiotics work by helping prevent pockets of infected urine reforming (that's what was making me sick, stuck urine that had built up lots of bacteria).
They told me how-ish: They go up with various catheters and things and install the stents, the stents stay in place until they are removed. Some stents have lines that exit the body to facilitate removal. Mine do not. The doc didn't want me accidentally pulling them out since the area they're in is heavily infected. They'll be removed at my first stone removal surgery in about two weeks from installation which was a couple days ago.
They did not tell me how-completely: The stents are hooked into my body meat like little fish hooks. They also didn't tell me they'd be taking urine for testing from my bladder and each kidney or that they would also be draining both kidneys during the procedure, so I did get a fluid-pressure reset.
They did not tell me basically anything about what the next two weeks will be like.
I'm on flowmax to soften my bladder so it's easier to empty. I don't think I needed that, I was peeing fine, but stents do change things.
I was worried that I might push them out while pooping but that's not likely to the point of nearly impossible. Not 100%, but nearly.
These things feel like a bad UTI and I have two of them. I got the ows, the zaps, the GOTTA GOs every few minutes. At least now I know that ALL of those pains are UTI pains, you know? I'd get some random pain sometimes and be like "what was that......" and now I know. It was UTI and pressure in my kidneys and the pain signals were traveling around the whole renal system. Because they do that.
I'm in a lot more pain now than I was with just the kidney stones. It is very, VERY atypical but my kidney stones and the pressure behind them don't hurt. Those nerves may have died off.
There's varying amounts of blood in my urine, sometimes very little, sometimes a lot. Sometimes there are clots. That's all normal but I had to ask as things were happening.
I get up every couple hours in the night and some times I don't make it to the toilet (I did all last night, so that is improving).
They also didn't warn me that just having the surgery itself might make me wet myself because the muscles hadn't all regained strength/how long it would take for the anesthesia to fully wear off.
I called the doctor's office and asked about that, too.
I'm glad I thought to have That Guy bring Depends but that's also something you'd think someone would like, mention. You know?
So that's what having stents has been like so far.
Feels like a bad UTI, though for some people they feel nothing. Need adult diapers for accidents. Need to be near a toilet at all times, and not going to get a hell of a lot of continuous sleep for a while.
-
I also think it's worth noting that I've had two male doctors blow me off about this and I think the only thing that went differently at the ER was that it was a female doctor.
The first male doctor said it was an anxiety attack.
The second male doctor said it was a viral stomach bug.
The female doctor listened to my symptoms and ordered a bunch of tests.

So, more personal blather about the whole situation.
While I was in the first ER I heard a man yelling and starting trouble in the waiting room. That Guy and Son got up and left as soon as the man was distracted by a security guy. I'd had told them to go home as soon as they dropped me off and I would text if I needed picked up. I knew I wasn't going home, though.
-
My neighbor was an elderly lady and they kept trying to figure out when she'd last pooped but she couldn't remember. Finally she called them in and was like I need to poop so they wrestled her up on a bed pan (she cried, she was in a lot of pain) and then left her alone with her curtain closed to poop. Right then the floor doctor walked in and was like HI MISS GERALDINE and whipped her curtain open to start talking to her.
...
I chewed him out. That's very atypical of me. Like, I laid into him for not asking if she was wanting to talk in that exact moment. And then I felt really bad until I realized he's probably had people a lot more angry at him than me considering a lot of the patients I could hear were elderly and some were confused, and I didn't feel bad anymore.
-
Since it's a university-run hospital there were sometimes pairs of nurses, and at one point a trainee came in to give me a dose of antibiotics through the IV but she hooked it into the wrong plug which depressurized the system and blood starting backing up the tube. As soon as she saw that she ran to get her trainer and they spent some time doing a full reset of the IV set up.
I wasn't worried or anything. It was my own blood and it could only go so far/only so much could be lost. At the most a cup since the saline bag was fresh and mostly full, still. So I was totally calm the whole time, which I'm sure helped.
I think the nurse in training was surprised when her trainer stepped out and I encouraged her instead of yelling at her. I praised her for not being too proud to get help when she noticed an issue, and for observing how to rectify the situation.
-
That Guy was like "Yesterday's nurses did NOT like me..." and I was like yeah I kind of told on you, but not out loud. He got put on the shit list FAST by staff. So for that I have a note in my account that I'm experiencing financial abuse and he exhibits controlling behavior. If there ever is a point where Son and I have to leave, I have the name of where to call. There's a facility in Next Town Over where the hospital is that will come and get us, and that would be the last time we see him.
I feel guilty for saying anything because he has paid for my existence for decades but he has also been abusive, just not physically.
They asked me if Son is safe at home alone with That Guy and I said "Safe, yes. Happy, no."
They also asked like how is Son and I said he seems to understand that his father's behavior isn't his fault but he still has had to endure it.
I also in the process learned how much money he makes (I didn't know before) and wow we should all certainly have insurance (he and Son might through his work but I have nothing and don't qualify for assistance while he claims me on his taxes as a dependent) and have had medical care all this time and there's no reason at all to be doing the whole -pointedly look at the food receipt every grocery trip, look up at the sky angrily, shake his head, shove it in his pocked, huff, and walk away- thing. Also explains why his work friends keep suggesting burger joints that end up costing like $80 for the whole family....
31 notes
·
View notes
Text
Went to see Amba again. She is doing ok. Her kidney enzymes came back fine, so she was started on the oxytetracycline yesterday. She did have diahhrea, though. She also had no hay so I asked for a hay net to be put up, and sent an email in the evening asking if she could please have free choice hay like at home.
Unfortunately, she cannot be turned out with the catheter right now. With her spooking at everything and looking like she was thinking about trying to hop the fence of the outdoor arena the other day, there’s just too high a risk that it can get ripped out. I’m hoping this will change if the antibiotics kick in and the spooking decreases. She’s been stalled at night before, but never 24/7, minus 2 days last year when the pastures were covered in black ice. And she didn't really take it well; she started violently head tossing when I let her run around in the indoor. Today she was good, but she’s lethargic.
I was going to go to tractor supply to buy her some stall toys (because I foolishly gave away the ones I had bought for Cannoli), but luckily they already had some and put them up. I’m curious to see if she will play them, because she’s never been particularly playful, which is quite possibly a symptom of the lyme.
There is a little indoor arena, so when I see her I groom her then walk her around in there for an hour. I feel really bad for her because there’s only 1 other horse there and she can’t see him even though he’s stalled next to her.
I am aiming to have her stay a month, provided she doesn't react too badly to the meds.
I need to figure out my game plan for boosting her immune system. I will reach out to that lady from the video I posted yesterday to see if she can recommend more specific herbals. The vets here aren’t against herbals by any means, but they also aren't holistic specialists so they didn’t really recommend anything targeted. I absolutely plan on keeping her on probiotics and colostrum supplements permanently at this point. But I also just want to make sure the ones I’m using, probiotic wise and immubiome, have a long shelf life and can withstand the stomach acid. In the human world so many supplements are scams since they’re unregulated, and I’m sure the situation is even worse with animals.
Maybe I should add vitamin e as well? Both she and Cannoli had levels that were fine when I tested them, though. But I know it protects neurons. If the vets think it may help I will add it. It doesn’t wind up in urine like vitamin c so maybe extra will help.
I was looking into her diet as well, but don’t necessarily think there’s anything that should be changed. She gets 1 scoop of Sunshine Plus ration balancer, 2 scoops of alfalfa pellets, 1 scoop of probiotic wise, and one scoop of immubiome am and pm. Technically, the sunshine plus is not the absolute best since it does contain molasses, but it does have yeast culture as the 4th ingredient, and also has MosPlus probiotics and bioavailable vitamin e & se. So while it wouldn't be great for a laminitic horse, for Amba with a weak immune system and microbiome that’s probably destroyed at this point, I feel like it’s a good choice. The other ration balancers that I’m aware of either don't have probiotics, or don't have them as high on the ingredient list.
I’m feeling quite depressed over this situation. But it’s a different type of depression and feeling overwhelmed lately that is not my typical seasonal, holiday, or grief-related variety. It is more a feeling of, “everything feels like BS so what is the point?” It just seems like such astronomical bad luck to have to send 2 horses to a clinic for nuero issues just a few months apart. Only 2 horses in 2014 had EDM like Cannoli. And while many more have lyme, most don’t have to get IV oxytetracycline. And there’s other things going on, too. Like my boss of many years got fired by the historical society. I wrote a post on Facebook about it and over 100 people bombarded the historical society and town board with emails supporting him in response, but they still haven't hired him back, or even bothered to find a replacement for him. So there will no longer be a farm.
26 notes
·
View notes
Text
Everything You Should Know About Uterine Artery Embolization
Uterine artery embolization (UAE), sometimes known as uterine fibroid embolization (UFE), is a minimally invasive procedure designed to shrink fibroids. It involves using a catheter to inject tiny particles into the uterine arteries that supply blood to the fibroids. By blocking the blood flow, fibroids are deprived of essential nutrients, causing them to shrink and alleviating related symptoms.
UAE is typically performed by an interventional radiologist, and the procedure is done under mild sedation, not requiring general anesthesia. Unlike hysterectomy, UAE leaves the uterus intact, making it a fertility-sparing option for women who wish to maintain their reproductive capabilities.
Comparing Uterine Artery Embolization and Hysterectomy
Procedure Type: UAE is a minimally invasive, outpatient procedure, while hysterectomy is major surgery requiring general anesthesia, with a longer recovery period.
Recovery Time: Recovery from UAE generally takes around 1-2 weeks. In contrast, hysterectomy can require a hospital stay and 4-6 weeks for a full recovery, depending on the surgical method used.
Uterus Preservation: One of the key benefits of uterine artery embolization is that it preserves the uterus, which is an advantage for those who want the option of future pregnancy. Hysterectomy, on the other hand, involves the removal of the uterus, which permanently ends a woman’s ability to conceive.
Symptom Relief: Both procedures are effective for symptom relief. UAE can alleviate symptoms like heavy bleeding, pain, and frequent urination within a few weeks. Hysterectomy provides permanent relief from fibroids but is irreversible.
Future Health Considerations: UAE is often preferred by women who are concerned about the potential hormonal changes that may follow a hysterectomy. Preserving the uterus can also help maintain a sense of bodily integrity and reduce the risk of long-term side effects.
Why Choose Uterine Artery Embolization?
Uterine artery embolization offers several benefits over traditional surgical options:
Minimally Invasive: UAE involves no major incisions and has a lower risk of surgical complications.
Quick Recovery: The outpatient nature of the procedure and minimal recovery time are appealing for those with busy schedules or caretaking responsibilities.
Effectiveness: Studies have shown that UAE is highly effective in reducing the size of fibroids and relieving symptoms.
Preserves Reproductive Health: By keeping the uterus intact, UAE allows women to retain the potential for pregnancy, an essential factor for those planning to expand their families.
What to Expect During and After UAE
During the UAE procedure, an interventional radiologist inserts a thin catheter into the blood vessels that supply the fibroids. Microscopic particles are then introduced through the catheter to block blood flow to the fibroids. As fibroids shrink, symptoms start to improve gradually. Most patients go home the same day, and a typical recovery period lasts about one to two weeks.
After UAE, you may experience mild pain or cramping, which can be managed with over-the-counter pain relief. You’ll also have follow-up visits with your doctor to ensure that your fibroids are shrinking as expected and to discuss any additional treatment needs.
Making the Choice
The decision between uterine artery embolization and hysterectomy depends on various factors, including your age, reproductive goals, severity of symptoms, and personal health preferences. UAE provides a promising option for those seeking a less invasive solution that still effectively treats fibroids and maintains the option of fertility.
#UterineArteryEmbolization#FibroidTreatment#NonSurgicalOption#HysterectomyAlternative#MinimallyInvasive#FibroidSymptoms
0 notes
Text
Dr. Gaurav Gangwani: Pioneering Uterine Fibroids Treatment in India
INTRODUCTION
Dr. Gaurav Gangwani, a leading Interventional Radiologist, specializes in uterine fibroids treatment in India, pioneering advanced Uterine Fibroid Embolization (UFE).

Leiomyomas, another name for uterine fibroids, are non-cancerous growths in the uterus that affect a large number of women, especially those who are fertile. The therapeutic environment for uterine fibroids in India has changed significantly in the last few years, mostly because to the creative efforts of experts like Dr. Gaurav Gangwani. Dr. Gangwani, a renowned interventional radiologist, has promoted the use of Uterine Fibroid Embolization (UFE), a minimally invasive technique that has completely changed the treatment of uterine fibroids in India. This article examines Dr. Gangwani's contributions to this field, the methodology and advantages of UFE, and its significant influence on women's health in India.
Early Professional and Academic Background
Dr. Gaurav Gangwani's medical career commenced with a solid academic background. At one of the top medical schools in India, where he finished his training, he became quite interested in radiography. His quest for perfection led him to focus on interventional radiology, a specialty that uses imaging technology in conjunction with minimally invasive techniques to treat and diagnose a range of illnesses. Understanding the profound effects uterine fibroids have on women's health, Dr. Gangwani committed his professional life to improving therapy for uterine fibroids in India.
Uterine Fibroid Embolization: A Game-Changer
Dr. Gangwani is at the forefront of uterine fibroids therapy in India thanks to his groundbreaking work in uterine fibroids emboldening. Without requiring typical surgery, UFE is a complex method that targets the blood supply to fibroids, causing them to shrink and improving symptoms. Using a catheter to introduce minuscule embolic chemicals, this procedure blocks the arteries supplying the fibroids. As a result, the size of the fibroid is significantly reduced, and symptoms including heavy menstrual bleeding, pelvic pain, and frequent urination are significantly improved.
Technique and Procedure
Under the expert care of Dr. Gaurav Gangwani, UFE is performed with precision and care. The procedure is typically conducted under local anesthesia, minimizing patient discomfort and risk. Dr. Gangwani uses advanced imaging technology to guide the catheter to the uterine arteries, ensuring accurate delivery of the embolic agents. The entire process takes about 60 to 90 minutes, and patients can usually return home the same day. This minimally invasive approach is a cornerstone of modern uterine fibroids treatment in India, offering a safer and more comfortable alternative to traditional surgical methods.
Patient Experience and Success Rates
The success rate of Uterine Fibroid Embolization under Dr. Gangwani's care is notably high. Many patients experience a significant reduction in fibroid size and a substantial alleviation of symptoms. One of the major advantages of UFE is its quick recovery time. Unlike traditional surgeries, which may require weeks of downtime, most UFE patients can resume normal activities within a week. This rapid recovery is a critical factor in the growing preference for UFE as a primary uterine fibroids treatment in India. Dr. Gangwani's patients frequently report high levels of satisfaction, not only due to the efficacy of the treatment but also because of the compassionate and professional care they receive.
Advancements in Women's Health
The introduction and growing popularity of Uterine Fibroid Embolization have had a transformative impact on women's health in India. For many years, women with fibroids had limited options, often facing invasive surgeries such as hysterectomy. Dr. Gaurav Gangwani's advocacy for UFE has provided a much-needed alternative, empowering women to make informed choices about their health. This shift towards minimally invasive procedures aligns with global trends in medical treatment, reflecting a broader commitment to patient safety and quality of life. As a result, uterine fibroids treatment in India has entered a new era, characterized by innovation and patient-centered care.
Case Studies and Testimonials
Numerous case studies and patient testimonials underscore the effectiveness of Dr. Gangwani's approach to uterine fibroids treatment in India. Patients from diverse backgrounds have benefitted from his expertise, experiencing relief from debilitating symptoms and a return to normalcy in their lives. One such case involved a 38-year-old woman who had suffered from heavy menstrual bleeding and severe pelvic pain for years. After undergoing UFE with Dr. Gangwani, she reported a dramatic improvement in her symptoms and expressed gratitude for the minimally invasive nature of the procedure. Such success stories highlight the transformative potential of UFE and Dr. Gangwani's pivotal role in advancing this treatment.
Training and Mentorship
In addition to his clinical practice, Dr. Gaurav Gangwani is committed to training the next generation of interventional radiologists. He regularly conducts workshops and training sessions, sharing his knowledge and expertise in uterine fibroids treatment in India. His efforts to educate and mentor young doctors ensure that the benefits of UFE will continue to reach more patients across the country. By fostering a community of skilled professionals, Dr. Gangwani is contributing to the broader mission of improving women's health care in India.
Challenges and Future Directions
While Uterine Fibroid Embolization has gained significant traction, challenges remain in ensuring its accessibility to all women in India. Dr. Gangwani acknowledges the need for greater awareness and education about UFE among both patients and healthcare providers. Efforts are ongoing to integrate this treatment into more medical facilities, particularly in rural and underserved areas. Looking ahead, Dr. Gangwani is optimistic about the future of uterine fibroids treatment in India. He envisions a healthcare landscape where minimally invasive procedures like UFE become the standard of care, offering women safe, effective, and accessible treatment options.
The Role of Technology
Technological advancements play a crucial role in the success of Uterine Fibroid Embolization. Dr. Gaurav Gangwani utilizes state-of-the-art imaging and catheterization techniques to enhance the precision and safety of the procedure. The integration of advanced technology ensures that UFE is performed with the highest standards of accuracy, reducing the risk of complications and improving patient outcomes. As technology continues to evolve, it is likely that UFE will become even more refined, further cementing its place as a leading uterine fibroids treatment in India.
Patient Education and Outreach
Dr. Gangwani is a strong advocate for patient education. He believes that informed patients are empowered patients. To this end, he actively participates in public health campaigns and educational seminars to raise awareness about uterine fibroids and the available treatment options. By disseminating information about UFE and its benefits, Dr. Gangwani aims to reach a broader audience, ensuring that more women are aware of this revolutionary uterine fibroids treatment in India. His outreach efforts are crucial in demystifying the procedure and encouraging women to seek timely medical intervention.
Conclusion
Dr. Gaurav Gangwani's contributions to uterine fibroids treatment in India cannot be overstated. Through his expertise in Uterine Fibroid Embolization, he has provided a safe, effective, and minimally invasive option for countless women suffering from fibroids. His dedication to patient care, education, and innovation has transformed the treatment landscape, offering hope and relief to many. As a pioneer in his field, Dr. Gangwani continues to lead the way, ensuring that uterine fibroids treatment in India remains at the cutting edge of medical advancement. His work not only alleviates the suffering of individual patients but also represents a significant step forward in women's health care in India.
1 note
·
View note
Text
Did my final pre-screening before surgery today! I went to the hospital two weeks before the actual surgery so they could confirm I'm still healthy. For this visit they only needed an EKG, blood draw, and urine sample. Everything came out normal.
The transplant team also used this visit to tell me more about what to expect:
Lead-up to surgery:
In about a week, I can pick up my painkiller prescription for after surgery.
On the day before surgery, I'll be on a clear liquid diet. That means tea, water, coffee, and other drinks with no solids are okay. No juice with pulp, or solid food.
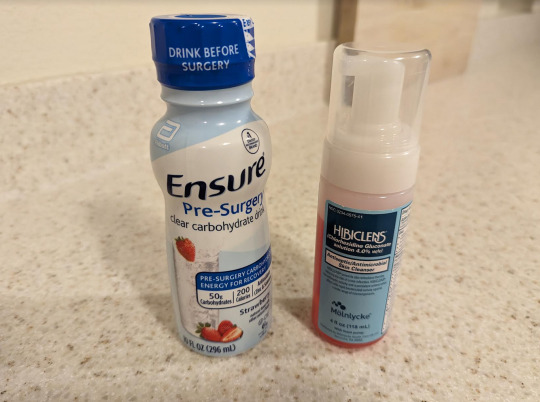
After midnight, I'm not supposed to eat or drink anything except for the fancy carb drink (Ensure) that they gave me. They want me to drink that between midnight and my arrival at the hospital.
The point of this is to reduce the risk of aspiration (stomach fluid entering the lungs) during my surgery, and speed up recovery time afterward. Abdominal surgery is pretty tough on your stomach!
They also gave me an anti-bacterial body wash (Hibiclens) they want me to use the morning of surgery to minimize the risk of infection later.
The surgery itself
They want me to arrive on December 27th at 5am(!), and the surgery itself will start at 7am.
I'll get a chance to meet with the surgeon, nurses and anesthesiologist and discuss any last questions/concerns. I can change my mind at the last second if I choose - they reminded me there's no obligation - but I'm quite sure of my decision.
I'll change into a gown, get wheeled back to the operating room, they'll stick me with the needle, and then it's lights-out time.
The operation takes about 2-3 hours. After that, I'll be monitored closely in the PACU (Post-Anesthesia Care Unit) so they can make sure I wake up on time and no immediate issues arise. After I wake up in the PACU, I'll probably have to wait another 4-6 hours before they move me to a normal hospital room with more privacy.
Recovery
I'm likely to wake up with a scratchy throat (thanks to the oxygen mask they'll use while I'm in surgery), and definitely with a catheter and IV needle to make sure I don't get dehydrated. They'll give me painkillers before I wake up, too.
The PACU doesn't allow visitors or have much privacy (only curtains), but I can have things brought in, like my phone and books.
The normal hospital room afterward does allow visitors. I'll also meet with several members of the transplant team afterward for discussing recovery and follow-up visits. I expect my biggest challenge will be just enduring all the people talking to me in one day!
They expect I'll be able to walk around almost immediately after waking up, and even encourage it (as long as I have someone watching in case I get dizzy). The sooner I walk after surgery, the sooner the digestive system will "wake up" and start functioning normally again.
I'll probably stay in the hospital for one night. The next morning they'll remove the catheter and, assuming there's no complications, I'll go straight home. A family member will be driving me, of course, and will stay with me at home for a few days.
Besides "don't move too fast or bend over if it hurts," and "don't lift anything over 10 pounds or do strenuous exercise," recovery should be pretty straightforward. Also, I'm planning to pick up some prune juice and Greek yogurt, as I've heard those can help a lot for post-surgery nausea and bloating.
Honestly, I think the hardest parts will be boredom, and dealing with all the professionals explaining things at me. I'm not afraid of pain - they can treat pain! But there is no treatment for a group of very earnest and well-meaning people asking you "Any questions?" and "Do you feel okay?" a dozen times in one day.
I don't blame them for it. I know they have to, and they ethically should, and most of their surgery patients are probably way more nervous and want more hand-holding than I do. Me, just give me a painkiller, my smartphone, and a book, and I'm happy. (And preferably a veggie burger. But that will have to wait till I'm out of the hospital.)
0 notes
Text
Quick Update (Update #15)
November 12, 2023
Today, an ICU nurse came to:
1) Remove her Central Line or Central Venous Catheter (which was inserted in her neck) because it’s no longer working.

2) A new IV line in her arm is inserted. This will probably work for 2-4 days so a new one will have to be inserted after that. She needs this because she’s on another round of IV antibiotics because of her Pneumonia.
3) Change her urine catheter.
4) And the mostly awaited, to remove her NGT (nasogastric tube) because she can now swallow food (soft diet) and drink medicines.
Praise the Lord!
She’s also glued to her adult coloring book. Making art daily is one activity she thoroughly enjoys.

Prayer Request
🙏🏽 Healing from Pneumonia and other infections.
🙏🏽 That her medical needs be accommodated here at home.
🙏🏽 That she will be able to resume chemotherapy.
🙏🏽 Grace, peace, joy everyday.
🙏🏽 For provision for all the needs.
🙏🏽 For God’s will to be done!
0 notes
Text

Catheterizations Service At Home - Nurse At Home
Carevive Home Healthcare” organizes urine catheter change at home services with cost-effective mode. Our nurses are highly professional & skilled in handling the catheter change at home in Delhi NCR. We are renowned for a urine catheter change at home services & our certified female attendant is dedicated and sincere with all standard safety. We are 24×7 hours enabled to reach out to the customer’s place and take care of all the needs for catheterization.
https://nurseathomeservice.com/catheter-change-at-home/
#catheterizations service at home#catheter change at home#urine catheter change at home#nurse at home
0 notes
Text
UPDATE
ill have to get to my replies later but i need to update right now
teddy was getting even worse, the meds were horrible to him and he just started to take a dive. he was dead weight, couldn't stand it was devastating to see him trying to pee or do anything really only to just fall. he was confused, scared, couldnt sleep for more than a couple minutes after having literally tried to calm him like a baby. this wasn't your typical sedative, calming med loopiness this was extreme, ive never seen a cat act this way before, let alone while on relaxants. its hard to explain but when you've experienced cats pass before you just know the signs and he was showing them rapidly later in the morning. i had another total breakdown so mom took the reigns and called them and absolutely ripped them apart. they're at fault for this getting worse, for this horrible medication, for not leaving the catheter in for longer like i said i wanted so he wouldnt have to go through that procedure AGAIN, its invasive enough ONCE let alone 2 or 3 times, for not ensuring he could pee on his own before just sending him off carelessly, for not communicating and hyperfocusing on money for issues that arent even an issue night now and could be done later. blockages are difficult to address as is, but the way they went about it made it even worse. the vet told us to get him in right away for the reaction to the new medication, and we were firm that we are NOT paying this is their fault I'm amazed teddy was able to make it through the night, he's so incredibly strong
as much as i dont ever want to go back there im doing everything for him and we raced him there, they're going through all kinds of checks to make sure he's ok and also working on his peeing. he had a wet bowl movement before i got the call, which couldve been from the sudden change to his prescription diet, the new med, the situation or anything, but was so weak he couldnt even stand so it got all over him, i had to wash him off and that seemed to kind of kick him into moving again, not much but a lot more than i had seen all morning after becoming exhausted, almost like it switched him back on to keep fighting.
so far he's doing well his bp is only slightly high due to the stress of being there but hes inflamed which also is making the urine they can push out tinged with blood. they're monitoring him constantly in fact she (this is a different vet from the owner, ive had good experiences with her) said he's being held almost all the time by another staff member, she will be giving him a boost of antibiotics as an injection and a single anti inflammatory since he got his bloodwork done and he doesnt have any kidney or liver issues or anemia/anything else. they offered for me to stay with them there so i can be with him but i needed to get back to my other babies to make sure they dont stress more either, i have to keep them healthy too so im getting updates over the phone. hes eating there hopefully thatll give him a boost of energy because though they can bring him out and walk him around/play hes still very sleepy. he hasnt peed but his bladder isnt full either, i asked why since he was drinking like crazy and she said its likely because he's dribbling tiny amounts almost constantly, his blanket has some small spots (i noticed when he was home his peepee was wet a lot but no full pees) im going to be grabbing him again soon before they close and then taking him back first thing in the morning for her to check his bladder again, if its full and hard again she's putting a catheter in again. she's also giving me a prescription for a bladder relaxer thats non drowsy, but its a gamble what pharmacies have it. we still are firm we are not paying, i'm still so scared because if they DO try to ding us with the bill we will absolutely be out of donations to help, the last bill was $606, on top of that all the gas needed to even get there and back is crushing, and i have no idea what will happen but its not something i can even think about right now
idk how its going to go we're just taking this one step at a time, my anxiety has made me so sick i want this nightmare to be over with and him at home safe and sound.
again thank you all so much for your concerns for my boy, all the help, the donations, the kind words its incredible how many are wishing and working for his recovering ill update again and get to replies as well when i can
please help me pay my kitties emergency vet bill!
ive never done this before but one of my cats just had to get an extremely sudden emergency procedure and i don't know what to do, my vet and i have reached out to a couple incredible programs here to help with the bill but one is less than half and the other hasn't replied back yet, i've already declined the blood work (CA$356) to lower the bill at the risk of possible underlying liver and kidney issues not being found but its still a monumental amount for us right now. i just feel so helpless
we had enough to pay the minimum deposit to get the procedure started in time thankfully, but we were already scraping by as it is and now we're in desperate need of funds to eat/pay rent/pay off any remainder of the bill. i am disabled without aid and have been unable to work/haven't worked since 2015 but am on track to hopefully start working pt this fall. i live with my mom who has 3-4 jobs including one seasonal job which needless to say is stressful and wearing her down. we unfortunately are stuck in the most expensive place to live in canada with the inability to save up to flee so the cycle is never ending.
this is Teddy, my typically very silly vocal happy boy who's not quite 2 yet, my comfort king, my little muffin who acts like a weighted blanket for me at night and eases my anxiety, his favourite toy is his pink unicorn poof, he loves car rides and he can shake paw!

he got a sudden urinary blockage last night with no straight answer as to why and progressively got worse as the night went on, i didnt sleep at all, i was panicking and bawling, naturally, and raced to the vet to get in as soon as the door opened. i assumed it was a uti which wouldn't have been as costly, but it turned out to be much more severe and life threatening. i never expected my usually extremely healthy boy to suddenly be at risk of that and im still trying to just process whats been happening
he needed to be sedated and given a catheter and some medication, the total bill came to CA$985.62, of which we were barely able to pay 500 of, and one program was able to donate 300 leaving a total of CA$185.62 for the bill. this, of course, leaves us scrambling for food and rent as well

i know there are a lot of fundraisers out there needing donations right now, and i really hate letting myself be so open and raw like this but even a dollar would help tremendously and i would be forever grateful for any help whatsoever, even a rb to signal boost is greatly appreciated <3
TLDR; my cat had a sudden life threatening issue and now we can't pay the full vet bill or pay for food/rent
Paypal
397 notes
·
View notes
Text
5/15/2022
Hey there, blog. Remember me? It’s been a couple months. The weather is changing and with it, the collective mood. It’s always interesting how much sunshine and warm temperatures positively affect emotional states. I swear, I’ve seen people skipping through the streets this past week. A few bullet points to help fill in the blanks that my absence here left...
- Put my mom in rehab. The tuition was a terrifying dip into my nest egg. I can’t help but be a little resentful about it. I hope she is strong enough to stay clean. I am nervous for her. During a therapy session held at her rehab, my sisters and I were more honest with her than we had ever been. It was brutal. My mother hasn’t spoken to me since.
- Crypto is crashing hard. My nest egg has been slashed more than 50%. It doesn’t make me feel good. But I think I’m rolling with the punches rather well.
- Experimented with Seeking Arrangements again. I can’t do it. I’ve outgrown my hoe phase. All I care about is building my career. Any other time spent pursuing money feels like a huge waste of time. No thank you.
- Speaking of careers. I’m pivoting! I still love furniture design, but it’s been really tough for me to break through. I can’t seem to find manufacturers that want to work with me, let alone contact me back! So, I’m doing fashion! It’s another true love of mine. I’m visiting with a manufacturer tomorrow to get my first samples made! I just made the pivot about 3 weeks ago. I have already been able to move mountains as far as my progress goes. The infrastructure here in NY for budding fashion designers is insane. There is so much support! Plus, all of my samples will cost far less and take less time to make than my furniture prototypes. It feels like the right move. I can control a lot more with this route. Plus I still get to scratch that creativity itch that I have been so desperately craving to scratch. Feels good!
- Still seeing fireman. I feel like there have been some recent road bumps that have led to both of us pumping our breaks a little. Nothing major, just a bit of hesitance. We’ll see where it goes. He’s a good guy and I’m grateful to have connected with him.
- Caught wind of my ex being with his ex. Got me feeling all sorts of ways. He cheated on me with her. But not before he first cheated on her with me. The whole thing is just a huge mess. It blows my mind that he would backslide like that. I just don’t understand it. But then again it sort of makes sense. I was just hoping that he would have grew more through the whole experience. Such is life. I wish them both peace and happiness.
- Shitter, my cat, had to have an emergency procedure to save his life. I came home from Utah and he couldn’t urinate, which is a big uh-oh for male cats specifically. They had to sedate him and stick a catheter into his peen to unblock his urethra. I actually got to be a part of the whole thing! I held a little oxygen mask over his nose while the vets operated. It was pretty cool. What is not cool is the $4,000 it burned into my wallet. I swear, I have been fucking bleeding money.
- Went to Tulum, Mexico for Billi’s birthday! Again, sunshine and good weather make for happy people and I am here for it.
That’s that I guess! I’ll check in again when I feel like it.
2 notes
·
View notes
Text
The Beat of a Heart
In honour of Doctor’s Day (barely in time), here’s a short story by my hand. It’s based mostly on real-life experiences, most of the scenes based on things I have seen in clinical postings. I am not sure whether I got the main character’s emotions right, but I did my best, so I guess that counts.

[Image ID: A stethoscope with blue tubing, silver diaphragm and black earpieces lying on top of a blurred keyboard, a blue pad to the left of the stethoscope, with a piece of blank paper pinned on it. On the bottom left, the words ‘The beat of a heart...’ are written in red England Hand font. End ID]
I’m tagging my usual writer mutuals and putting the actual short story under a cut.
My taglist: @ambitiousandcunning @medhasree @shaonharryandpannisim @chaanv @arjunaparantapa @hindumyththoughts @spockswhore @ashsnipes @annlillyjose @seekerbrave @avakrahn @a-confusedmess @arachneofthoughts @paneerlajwanti @vishnupada @bookdragonfanish @iamnotthat @foreveres @shellweed @will-die-without-chai.
She coughs a little, ignoring the rasp in her throat, wishing she could reach for her water bottle, but is impeded by the sheer number of people between her and the bottle in question. She reaches for the hand rub instead, the familiar smell of ethanol almost soothing for a moment. She blinks, turning to the older man sitting across her, the familiar questions on her lips.
‘Can you tell me why you’re here?’ she asks, noting down the man’s anxiety, trying to make her voice sound soothing. That is all the prompting he needs to launch into his long-winded story. She stretches a little, noticing the line of people in front of her, and the students hanging on each of her words standing behind her chair.
She smiles, looking behind her at the students, gesturing subtly for one of them to take over. ‘Make sure to examine him properly,’ she instructs. The student she had instructed nods, her eyes wide. ‘Yes, ma’am,’ the younger girl responds, leading the man to a bed. She can see the couple of students who had bothered to attend all clustered together, their discussion hushed.
She suppresses a grin. They’ll learn. She herself had. And indeed, one of the the students comes forward tentatively, stopping her peer who had been taking the man’s history, and begins the examination.
She turns to her work, leaving the students occupied for now. It’s a familiar battleground of questions and answers, having to rush the patients because of the lack of time. ‘Ma’am?’ it’s a young gentleman. ‘Yes, sir?’ ‘I am sorry,’ he says hesitantly, ‘I don’t understand what you said.’ She nods. Clears her throat, looking wistfully at the bottle that still is too far to reach, and too empty besides. Looking at it only diverts her attention to the humidity the fan is doing little for, the sweat trickling down her back.
She shakes her head. Do not divert your attention. Her colleague shoots her an understanding look, as she explains the prescription once again. He nods, with a quiet ‘thank you.’ She nods back at him as he leaves.
‘Ma’am?’ She turns once more. If nothing else, she muses wryly, choosing medicine has definitely taught me to multitask. The students lead the first man back to her, their clinical skills enthusiastic if a touch inexperienced. One of the girls excitedly details the sound of an ejection click. She smiles, lending the younger girl her own stethoscope. The girl listens in with the man’s permission in quiet absorption, the ritual being repeated by each of her friends, all of them clearly awed.
The gentleman looks amused at the furore the click of his valves, amplified by his metallic pacemaker, has elicited. She corrects them when needed, leading to a response of all heads nodding at once.
As the clock strikes 1, the students ask for leave to disperse and the crowd of patients mercifully thins. She tells them to go and come back for a short class in the evening, finally leaving behind the pursuit of her elusive lunch and the all-important water.
Her lunch in front of her, her thirst finally quenched, she ruffles through her iPad for information to make the class slides for tomorrow’s discussion. All too soon the short break is over, the slides still unfinished, and she stands, following her friends out of the Duty Doctors’ Room to go on ward rounds. Her eyes flit to a notification on her News app, of a doctor being beaten by goons. She sighs. There is no use pondering over this. I can only do my best. She knows protests do little good, so she hardens her heart and strides out, sliding her phone in her pocket.
Somewhere in the middle of the rounds, the students following her and the senior doctor like ducklings following mother duck, one of them comes running to her. ‘Ma’am,’ his voice is high with fear. She gives him her immediate attention. ‘There’s a man on that bed…’ the boy points, ‘…17, he’s…he’s not really breathing.’
Oh, no. Her friend steps up, running to the patient, while she looks for his details, adrenaline sharpening her senses.
He is a new patient, there is next to nothing on his chart. She can hear a lady wailing and she winces. No one should see their loved one in such a situation, she thinks, even as she squares her shoulders, moving towards the bed, shaking her head at her friend, who had already started CPR. She gently moves the lady aside, trying to console her, even when there is fear in her own heart that the news she might have to deliver could be irredeemable.
‘Doctor?’ asks the lady querulously, ‘you’ll save him, won’t you?’ She looks down for a moment, before meeting the lady’s gaze. ‘We will do our best,’ she replies quietly, grave as the situation is. The lady nods, tears still pooling in her eyes.
She can hear her friend panting. Quiet and quick, she swaps her place with him, continuing CPR. He shoots her a grateful look. She turns her attention to the patient. Between the three of them, they manage to get the patient breathing, she notes with relief. That relief doesn’t last long, though, as she looks the patient over. The catheter connected to him, filled with orange urine, the gross ascites and icterus. He’s on Rifampicin. TB with hepatic encephalopathy. One glance at her friend tells her that he, too, is thinking the same.
The lady with the patient…his wife by the sound of it, reads the grave news on their faces, facilitated, perhaps, by her intubated husband’s gasps of breath. She sinks into the bars of the hospital bed for support. She is at a loss for a moment, as she always is when confronted by the inevitability of death. She kneels then, her hand on the lady’s shoulder, silently commiserating.
When she stands, she looks at the downcast yet awed students and forces a smile. ‘Well,’ she says, stopping them as they turn away, towards the exit, clearly assuming that class is cancelled for the day. She has no intention of doing that, though. They need to learn that life doesn’t stop for those of us still hale.
At the sound of her voice, they turn as one, looking at her with eyes comparable in size to dinner dishes. ‘I’ll just wash my hands and come back,’ she says firmly. ‘You guys go wait in the Duty Doctors’ Room for your class.’ They keep staring at her for a few moments. ‘Go on,’ she instructs. They obey, darting reverential glances at her, talking in hushed whispers. How could someone literally save a life and just go back to normal like that? She hears one of their voices, quiet, dazzled. Despite knowing the truth, the innocent fascination in the boy’s face makes her smile.
I don’t know! She hears one of his friends reply. I want to be a doctor like that, when I finish my degree, when we really become doctors, the girl says, making her smile wider. The younger girl sounds like a young child deciding the goal of her life.
She tamps down the giddy joy and the grief simultaneously warring inside her, long since used to contradictory emotions, keeping a straight face as she strides to the washbasin.
When she enters the Duty room for the class, they’re discussing the exposure she could have had. She smiles wryly for a moment. This kind of exposure is a fact of life, she nearly blurts out, deciding not to, enjoying their impressed approval for a moment, before she clears her throat.
They all look abashed. She decides to proceed as if the moment before had not occurred, which was helped by one of them asking about the man she had done the CPR on. She summarises the case, gives them a few topics to read on and sends them home.
Before leaving the hospital proper, she circulates the wards once more. The CPR patient crashes again. This time, though they try long and hard, the lose the man, the beat of his heart forever silenced.
Her senior takes responsibility of the formalities, telling her to leave. Leave she does, casting one last glance back at the shell of the man, helplessness overtaking her for a moment.
She checks in with her colleague manning the night shift if she is free to go, fighting the uncanny feeling of déjà vu that comes with every patient they lose suddenly, the realisation striking anew that life goes on.
It is a leisurely walk back to hostel, the cool air soothing on her sweat-soaked shirt. She is thinking once more of the next day’s presentation, the number of slides still left to finish off.
After a quick wash-up and dinner, she sits with her iPad. It is nearly midnight when she finishes her work, fighting her drooping eyes. She checks in her WhatsApp, shooting a quick goodnight to her parents. The statues of her medico friends are full of calls for justice against the recent violence. Her non-medico friends are, as usual, conspicuously silent on the matter.
Ah, well, she thinks, it’s not like armchair social media posts can actually do much. Besides, this is not an issue that they face. Why judge? They’re probably thinking the same I do.
She debates posting a status of her own then decides against it, for again, social media can only do so much. The bitter truth can’t be changed.
Her mother’s voice echoes in her head, what mama had said the last time she had shared news of such violence. At least they didn’t kill him. You people get a lot of respect, you know?
She shakes her head, banishing those thoughts. She doesn’t want to have nightmares. Besides, tomorrow, she has to report for ID duty. She needs to be well rested for that. So she thinks of the awestruck students, the young girl’s voice playing in her head. I want to be a doctor like that, she said, when I finish my degree.
She falls asleep with a smile on her face.
When she is leaving for duty the next morning, she loops her stethoscope along the back of her throat, the diaphragm of the steth sitting firmly over her own beating heart. Time for another day at work.
Some terms that might be unknown:
Ejection Click: In some patients with heart problems, there is some backflow of the blood when the heart contracts. This backflow is heard as a ‘click’ sound when a stethoscope is used. This ‘click’ is amplified if the patient has a prosthetic metallic valve, as in case of the old gentleman in the story who is based on a real patient.
Rifampicin: A drug that is part of the four-drug regimen for Tuberculosis (TB). It increases the effect of another drug in the combination, Isoniazid, which is toxic to the liver. India has a huge number of cases of TB, being one of the TB-endemic countries. The orange urine is one of the most noticeable side-effects of using this drug.
Hepatic encephalopathy: Loss of proper brain function due to inability of liver to remove toxins. The patient on whom CPR was administered was in a coma due to this condition. He, too, was based on a real patient.
Ascites: Swelling of the abdomen due to accumulation of fluid in the abdomen.
Icterus: Yellowing of the sclera (whites of the eyes) and bulbar conjuctiva, a hallmark of jaundice.
The doctor here makes the diagnosis of TB with drug induced hepatic encephalopathy because of the ascites and icterus combined with the rifampicin usage and the coma. It is an unfortunately common condition here.
I just noticed that I haven't clarified ID Duty. It means Infectious Diseases ward duty. In this case, I meant COVID-19 duty, though it may not always mean that.
#doctor's day ramble#fiction#sort of#original work#nila writes#scribbler scribbles#nila rambles#doctors#tw: violence against doctors
6 notes
·
View notes
Text
“[...] one of the worst fears of the pandemic—that hospitals would become overwhelmed, leading to needless deaths—is happening now. [...] This is such a searingly ugly idea that it is worth repeating: Americans are likely dying of COVID-19 now who would have survived had they gotten September’s level of medical care.”
It’s here folks. I’ve seen it. And yet I’m STILL listening to people talk about having parties and hanging out with people outside of work and extended families. STILL. ಠ_ಠ We were all advised of the sacrifices necessary to avoid this outcome and yet...
It’s not just COVID. This affects anyone who has a medical need. Clinics are closing in order to divert staff to hospitals. As a result, thousands of patients across the country risk falling through the cracks without their needed checkups to maintain chronic conditions such as heart failure, diabetes, hypertension, and COPD. Inevitably those people will become more acutely ill, requiring a trip to emergency room. For example: CHF exacerbation, hypertensive crisis, DKA or HHS, and acute respiratory failure are some of the most common reasons for hospital admission and are all considered “acute-on-chronic” problems.
This time, however, if you need to be admitted, we may not have a bed for you. Neither will any hospital for hundreds of miles. If you’re lucky, you might be transferred to another hospital after hours of waiting in the emergency department. Or, you might be sent home after being stabilized with instructions to just come back if you get worse again.
How about planned surgeries to replace hips and knees, or to remove cancerous tumors? What will be the complications from delaying those procedures? Oncology patients who have a dangerous reaction after starting a new chemotherapy treatment? They are already severely immunocompromised. Can they wait in a bed in a hallway? I’ve cared for oncology patients who are routinely admitted to the hospital every two weeks in order to receive an 8-10 hour chemotherapy infusion. If those patients can’t be guaranteed a bed and a chemo nurse every two weeks for 6 cycles, how will that impact their treatment plan?
I’ve decided to share my unique perspective as an ICU RN in order to lift the veil somewhat and allow you all to grasp the reality of the situation.
🩺A typical Full Code COVID patient in the ICU, in my experience:
•A tube is in their mouth, extending down into their trachea, where it is held in place by a balloon to prevent air leaks. This tube is their lifeline and so it is secured to a device which is adhered to their cheeks to prevent dislodgment. The tube is connected to a machine at the side of the bed which forces air into the lungs at a set pressure, volume, and rate. We use a wand with suction to clean out their mouths every two hours. If needed, we occasionally thread a smaller tube through their endotracheal tube in order to suction out the gunk that makes you cough so it won’t clog up the breathing tube. If we switch modes to allow the patient to control their breathing, COVID patients will try to breathe 30-40 times a minute (normal rate is 12-20). They will also try to take deep breaths and cough. COVID makes tissue in the lungs so fragile that inflating them with high volumes and pressure will cause damage and scarring. We can’t let these patients breathe the way they want to breathe or else they will destroy their lungs and die.
•All of this is uncomfortable for the patient and so they are sedated. Medications to make them sleepy and to prevent agitation are given through continuous IV infusions. These medications also drop the patient’s blood pressure and so they also receive continuous IV infusions of medications called “pressors” which raise blood pressure. These “drips” are titrated up and down constantly by nurses to keep the patient sleepy enough to breathe with the vent, while also maintaining enough blood pressure to perfuse their vital organs.
•These pressor medications are very caustic and can burn and scar peripheral veins, so the doctor will place a central line. This is a long tube that’s threaded into a vein in the neck to almost reach the heart. In order to closely and accurately monitor blood pressures, we will use another long tube that’s inserted into an artery (either wrist or groin). That line continuously measures the average arterial pressure and nurses adjust those pressors based on that number.
•When your body is very sick it has trouble self-regulating to achieve homeostasis. Your kidneys are one of the first organs to suffer damage when you are very sick. Healthy kidneys help regulate blood pressure, electrolytes, and the acid-base balance of your blood. In the ICU we have to regulate all of that for you. We draw blood to check labs frequently, sometimes hourly, to monitor: how well you are getting oxygen in, how well you are breathing carbon dioxide out, how well your body is managing your acid-base balance, your electrolyte levels which will cause cardiac arrhythmias and even brain swelling if they are too high or low or if they change too quickly, blood clotting factors, level of waste products in your blood, etc. The nurse is constantly drawing these labs, reading the results, and giving medications or making ventilator adjustments to correct imbalances.
•Because the patient is asleep and has a tube in their mouth, they are unable to eat or drink anything. We put another tube in the mouth with the vent tubing, but this one goes down the esophagus and into the stomach. We then attach it to suction to remove gastric contents, use a syringe to administer medications, or hook it to a pump with a bag of liquid nutrients called “tube feeding” that will slowly trickle in just enough fluid (20 mL/hr) to ensure your gastrointestinal tract stays active and you have enough calories to meet your basal metabolic needs (the amount of calories your body burns by lying in bed).
•Because you aren’t eating or drinking or moving and the sedation medications are making your bowels sleepy, we give you laxatives to keep you pooping. Since your diet consists of a bag of liquid calories, it comes out of you much the same way. So we even have a tube for that, called a rectal tube (or “fecal containment device”) that’s held in place by a balloon in your butt and your poop just runs into a bag.
•It’s important for us to monitor how much urine your kidneys produce each hour. In order to be as accurate as possible, we insert a tube into your urethra which is held in place by a balloon in your bladder. Urine runs continuously into a bag where it can be assessed and measured.
•We monitor the heart via 5 wires stuck to the chest that give us a continuous visual representation of the electrical activity of your heart. COVID damages cardiac tissue and so arrhythmias and cardiac ectopy are common. If your heart beats too fast it can’t fill with enough blood to maintain your blood pressure, so sometimes we need to add even more continuous IV medications that prevent the heart from galloping off or doing too funky of a beat too often. The heart can sometimes be so damaged that it can’t squeeze effectively either, so we use other IV drips to help the heart beat and prevent it from giving up entirely.
•When we’ve done all we can do and the patient is still not improving, we will try “proning” and/or paralyzing. Medically paralyzing involves giving a continuous IV drip that stops muscles from being able to contract. This removes the extra oxygen demand of muscles, maximizing the oxygen that the COVID-damaged lungs can process. We need to give the least amount of paralytic medication necessary to prevent long-term complications. We are able to check the degree of paralysis by attaching electrodes to the patients face or wrist, sending electrical pulses (like a bark collar does), and then counting the muscle twitches. Paralytics also affect the body’s ability to create tears, so we need to pry open your eyes to administer eye gel regularly.
•Putting a patient in a prone position (on your stomach) helps by increasing blood flow to different areas of the lungs. It takes 5+ people to roll a patient VERY CAREFULLY onto their stomach without pulling out any of their tubes or lines. These are very sick patients and sometimes the movement can be too much of a strain on their heart and lungs. It’s a delicate, time consuming process. Patients remain proned for 16 hours, then returned to their back for a few hours. We may repeat the process again several times over the next 2-3 days, depending on if it is helping or not.
So how does this COVID patient get out of the ICU? Rarely, a patient improves enough to be awake and off sedation with the vent settings allowing breathing at the patient’s own rate. If the patient continues to improve, they are extubated (breathing tube out) and moved to a progressive care unit in the hospital to continue recovery. Unfortunately, the patient will often return to the ICU after only a day or two in the PCU. They deteriorate again because of all those COVID complications: heart damage, clotting (in lungs, legs, brain, etc), worsening pneumonia, etc. They can also develop complications that occur just from being hospitalized, such as: MRSA, cDiff, ventilator-associated pneumonia, bloodstream infection from the central line, UTI from the urinary catheter, peripheral limb ischemia from high doses of pressors, delirium (confusion/hallucinations), or injury related to falling.
•If the patient is still requiring mechanical ventilation after about 10 days, the next step is to have a surgeon create an opening in the neck called a tracheostomy so the ventilator can be attached through the hole in their neck. This way they can have long term ventilator support while continuing to attempt treatment. These patients are then transferred to a long-term acute care hospital where they will have to survive months of therapy to try to optimize their quality of life. After their prolonged hospitalization they will need to learn to breathe on their own again, swallow again, walk again, and learn how to take care of themselves as much as possible again. If they survive all of that then the patient will next move to a rehab center or nursing home. By this point, many do not survive due to new complications, the stress of prolonged sickness and comorbidities, or because the patient and family decided to pursue comfort cares instead.
🩺Some real talk here because knowledge is power:
I encourage EVERYONE (regardless of age or current health status) to fill out a Healthcare Advanced Directive, and choose who will make medical decisions in the event you are incapacitated. Consider your wishes NOW, and make sure you also know what your parents, grandparents, and spouse want. If your family member is hospitalized with COVID-19 and becomes so sick that even BiPAP is not helping, the doctor will ask you to make a decision between invasive mechanical ventilation (and everything that I described above) or “comfort cares.”
The specifics of “comfort cares” is individualized, but it essentially focuses the plan of care to acknowledge the patient’s decision that their quality of life is more important than extending it artificially without reasonable chance of recovery. The doctor prescribes medications to ease anxiety, and pain and the patient eventually passes away naturally without aggressive measures like a breathing tube or chest compressions. Families can be present with their loved one via telephone or Zoom video, though visitor restrictions may be eased for end-of-life patients, depending on the facility.
If you already have existing health complications (comorbidities) that make your chance of recovery from cardiac or respiratory arrest unlikely, you are able to let the doctor know from the beginning whether you are okay with CPR and a breathing tube, or if your wish is to make your code status DNR/DNI. DNR means that if your heart stops beating, you don’t want us to do chest compressions or shock your heart to try to restart it again. DNI means that if you can’t breathe on your own, you don’t want a breathing tube in your throat with a machine to breathe for you. You can choose one or the other, or both. You can also change your mind at any time, revoke your code status, and be considered a Full Code again. Full Code that means that we do everything medically possible to keep you alive, including breaking ribs during CPR, and putting a tube down your throat.
It’s important to not only have in mind what your own wishes are, but to discuss with your loved ones about their wishes. Very often, patients are either unconscious or too sick to communicate clearly and so the doctor will ask the next-of-kin or Healthcare Proxy to make the decision. Don’t make that emotional moment be the first time you think about it. And don’t put your loved ones in that position either. Have a conversation, put it in writing, and free them from the burden of that decision.
Feel free to ask me if you have questions and I will answer them to the best of my ability.
If you choose to share my words, please give credit and/or link to this page. Thank you.
#COVID-19#icu#pandemic#icu nurse#advanced directive#DNR DNI#tracheostomy#ventilator#hospital#real talk#over it
6 notes
·
View notes
Text
The Foundation of Angiography
Medical breakthroughs sometimes begin with a simple curious mind who asks, “What if…” and then proceeds to do something absurd that makes them go down into history books or change the way people live their lives. Before going into the detail about how Angiography was discovered, let us know about Angiography first. You may have heard of Angiography before. Even if you have not, do not worry. Sit back, have a cup of coffee/tea and relax while you read this article. Angiography is an imaging test that uses X-rays and a special Dye to view your body's blood vessels. The contrast dye typically used during the angiogram procedure contains Iodine (more about that later). The dye is injected into a small tube or catheter into an artery in your groin or (sometimes) your arm. The small tube is inserted after an injection of local anaesthetic around the artery. The X-rays provided by an angiography are called angiograms. This test is used to study narrow, blocked, enlarged, or malformed arteries or veins in many parts of your body, including your brain, heart, abdomen, and legs. Angiography is done in a hospital X-ray or radiology department. It usually takes between 30 minutes and 2 hours, and you can usually go home the same day. Moreover, Angiography is often considered the same as Angioplasty. These terms are not to be used interchangeably. Angiography and angioplasty are two different medical procedures that are related to the blood vessels. Angiography is used to investigate or examine your blood vessels for a potential heart condition. On the other hand, Modern angioplasty uses a special balloon and a metal mesh tube (stent) to open up a narrowed or blocked blood vessels (normally known as coronary arteries) that supply blood to the heart. In the long term, this should improve blood flow to the heart muscle and result in less or no angina. Since the dawn of the era of X-rays (Discovered by a physicist Wilhelm Roentgen in 1895), cardiac radiology has become a target of this new technique. Numerous early pioneers, rapidly accumulated extensive experience with fluoroscopy (X-ray movie in which a continuous ray of X-Ray is passed through the body) and radiography and publications on cardiac diseases till 1902. The next step in cardiac diagnosis was achieved by Werner Forssmann in 1929, with the first attempt at cardiac catheterization and angiocardiography. Werner Forssmann, a 25-year-old medical from Germany studying in University of Berlin, had an absurd idea in his mind. He hypothesized that a catheter could be inserted directly into the heart, for such applications as directly delivering drugs, injecting radiopaque dyes, or measuring blood pressure. He actually had thought, “Can I thread a flexible tube all the way to my heart through a vein, and then photograph it for the rest of the guys to see down at the beer hall?” The fear at the time was that such an intrusion into the heart would be fatal. To prove his point, he decided to try the experiment on himself. This was going to be huge risk. Moreover, English physician William Harvey had already proven in the 1600s that the blood circulates through the body and that the heart is the centre of circulation. In theory, Forssmann had known it should be possible to reach the heart & measure the activity of the human heart by determining pressures inside the heart’s chambers. If pressures were good, the heart was functioning normally; if low or erratic, the physician could diagnose faulty cardiac function. Without thinking much, Forssmann cut an incision into the basilic vein in his upper arm. The bold and brave student then threaded a urethral catheter—a transparent tube used to help patients who cannot urinate—into his vein. At this point, it was clear that he was not going to stop. He walked down a flight of stairs with the tube in his arm and entered the radiology department of University of Berlin. He then asked the professionals from the department to assist him. At first, all the people refused. However, he managed to convince some people to
assist him. He then proceeded to sit down on a table, and continued threading the tube toward his heart, using a mirror to watch his progress on a primitive X-ray device known as a fluoroscope. When he threaded the tube all the way into his heart’s right atrium, Forssmann X-rayed the event for posterity. At that moment, the diagnostic tool known as angiography was invented. A year later, Forssmann decided to repeat his trick. There was a slight change in the techniques this time. He injected an iodine compound through the hollow catheter and into the right atrium of his own heart for the world to see. Now, not only the catheter but the area of the heart injected with iodine could be seen with an X-ray. Because of Forssmann, the diagnostic tool known as cardiac angiography was discovered. He then went on to win the Nobel Prize for Medicine in 1956 (shared with Andre Frederic Cournand and Dickinson W. Richards) for developing a procedure that allowed cardiac catheterization. It helped saved millions of lives and revolutionize the field of cardiology, radiology and medicine.
1 note
·
View note
Text
My cat is not getting better
Hi, it's happening again. What I thought would be something I could forget about is happening yet again, my other cat is sick and with the same disease as the one that died early this year. I was confused as to why he got sick since I care for them a lot, but the vet told me that FLUTD is really common in males. So here I am, once again asking for help. I truly didn't want to do this since I didn't want to come across as someone who always asks for money, but at this point I don't know what else to do, I've been selling my stuff and doing jobs for people but it is not enough.
His name is Castiel, he's two years old and this past two weeks have been a nightmare, I first realized my cat was sick last week on Monday when I arrived home and noticed he couldn't pee at all, he didn't want to eat nor drink and he didn't have the strength to get on the bed. I took him to the vet immediately and they diagnosed him with FLUTD (Feline lower urinary tract disease).
The vet told me they couldn't use the urinary catheter since they didn't know just how big the crystals and sediment in his bladder were, so they appointed me for an urinalysis and an ultrasound. The next day I went to the appointment and they told me they were now sure he had FLUTD, and that he needed to change his diet and that only with antibiotics and a few shots he would be alright.
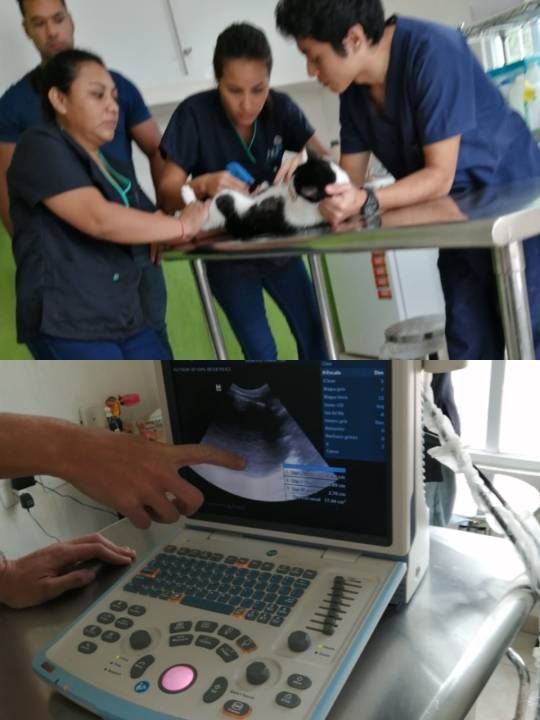

Sadly that was not the case. One day passed and I went to the vet to get his medicine but he looked weak and still wasn't eating. I was feeding him with re-hydration solutions and some vitamin gel but it wasn't enough. I couldn't give him too much solution either or his bladder would be damaged since he still couldn't pee. They told that if he looked worse that night that I should bring him fast and not wait for tomorrow. That afternoon I spent every ten minutes checking his vitals and making sure his bladder wasn't hard. Sadly at 7pm his pulse dropped and he wasn't breathing as fast so I took him to the vet, they told me he was getting cold and that he was at a risk of hypothermia. He had to be hospitalized that night.
The next day I went to check up on him and he looked really bad and that's when they told me that he indeed had hypothermia and that it had been really difficult to manage also that a surgery was needed. The urethral obstruction (a blockage in the urethra, which is the tube that carries urine from the bladder and out of the body) got worse and while he had started to pee it hurt him so bad since the clumps were bigger than his urethra.

I told them I didn't have any money left and that I would try to gather enough to pay, but business is business and they told me they could only perform the surgery if I paid. That day I sold my graphic tablet, some glasses and did paid homework. I managed to gather enough money and told them they could start the surgery.
That was last Friday. After that he had to stay hospitalized throughout the weekend. On Saturday I went to check up on him. He looked sick and skinny, still a little weak after surgery and he had an IV since he was dehydrated. They told me that if it went well I could pick him up on Monday.

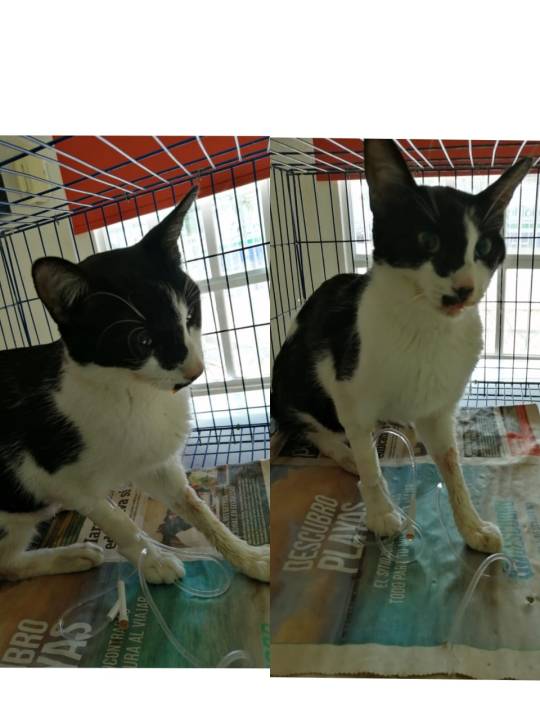
On Monday he looked way better, still a little disoriented but better. They gave him his medicine and told me that I had to come back again so they could check up on him and give him the rest of the medicine. I took him home and he looked so happy to be here. He was rubbing himself on my legs and my hands while I was sitting with him. The next two days were uneventful, he started to eat, pee and was even meowing. On Wednesday I was told that everything was ok and that I only had to come back in 15 days.
Last night was when all went downhill. He refused to eat and he didn't want to drink anymore. At 2am he puked all over the floor and started shaking a little bit. I was worried but I had to wait until morning to take him to the vet.

His ears and paws started to feel cold so I heated some water bottles and wrapped him up in a blanket and hugged him the rest of the night. Today he wasn't as cold as before but not as warm as he should be. I took him to the vet and they said that he had kind of a water bag in the stomach area and that he would need to have surgery performed again to see what's going on. They're worried that that liquid they feel is pee since it could be mortal. He was dehydrated again since he didn't want to drink anything.
They said that since I have been paying on time for the last week that they could wait this time, they will perform that surgery today and I have a week to pay all the bills that are needed during and after surgery.
Up till now I have spent more than $350 (appointments, ultrasound, medicine, shots, hospitalization, surgery, special dry and wet food, transport, etc) and it may sound like it’s not much but in Mexico it is expensive (almost $7000 pesos). I don't know how to make more money. As some of you know I'm a college student and money is not something I have in abundance. I managed to pay all the bills from last week, but it will probably be the same amount now since he will need new pain meds and noninflammatory, also antibiotics and the days he would have to stay hospitalized.
I love my cat. He has helped me a lot with my depression and I truly don't know what I would do without him. The worst thing is that everytime I think of him I'm reminded that my last cat had the same illness and the he couldn't survive. I'm so anxious right now I just want him to be okay.
If any of you could help I would be really really grateful. If not, it doesn't matter, just good wishes is enough. I'm still selling some stuff I have and doing some jobs when I find the time, but finals are coming and I'm worried I won't have enough time to study and care for my baby.
https://www.paypal.me/letipimhe
I'm sorry for the long post, but I’m desperate and even if I just get some cents I don't care. Anything helps. If you can’t donate please share, I’ll be really grateful. Also if you’d like to see the receipts so you know I’m not lying just tell me.
#cat#vet bills#animal help#signal boost#If you can't donate please reblog#thank you#blood tw#im really anxious i had to post this but its my only option#castiel
136 notes
·
View notes