#urinaryincontinence incontinence
Explore tagged Tumblr posts
Text
Urine Leakage Problem & Solutions For Men And Women. @eternelleaesthetics

Looking for urine leakage treatment? Many a times, while laughing, coughing or sneezing, urine leakage happens, typically among middle to old aged women. This is called urinary incontinence. Incontinence is medically categorised into 3 categories for treatment purpose. At our clinic, we have several treatment options like BTL emsella chair, injectables and medication. Swipe through this carousel to know more.
Surgeon: Dr. Maalavika Appasani Board-Certified Cosmetic Gynecologist Experience - 12+ years 09459450888 [email protected] https://lnkd.in/giicBbw2
Plot no 212/a, 3rd & 4th Floor, Rd Number 82, Jubilee Hills, Hyderabad.
#urinaryincontinence#urinary tract infection#urinary tract health#urinary incontinence#cosmeticsurgery#eternelleaesthetics#health#aestheticgynecology#plasticsurgeon#urinaryhealth
0 notes
Text
Incontinence Pads Market: $9.1B in 2023 to $15.4B by 2033 (5.7% CAGR)
incontinence pads market focuses on the production and distribution of absorbent pads designed to manage urinary and fecal incontinence. These products cater to various demographics, including the elderly and individuals with medical conditions, offering discreet and effective solutions that improve quality of life. The market’s growth is fueled by increasing awareness, a growing aging population, and continuous innovations in materials and design, ensuring comfort, protection, and dignity for users.
To Request Sample Report: https://www.globalinsightservices.com/request-sample/?id=GIS25886 &utm_source=SnehaPatil&utm_medium=Article
Market Dynamics
The incontinence pads market is experiencing robust growth, driven by:
Rising Awareness: Increased understanding of incontinence products and their benefits.
Aging Populations: The growing elderly demographic is fueling demand for discreet and effective incontinence solutions.
Innovations: Advancements in materials and design that improve comfort and performance.
Market Insights
The adult incontinence pads segment is the dominant player, capturing the largest share of the market, as the aging population increasingly seeks effective and discreet solutions.
The female incontinence pads sub-segment holds the second-highest position, propelled by a growing focus on women’s health, hygiene, and comfort.
In 2023, the market volume was estimated at 5 billion units, with projections to reach 8 billion units by 2033, reflecting a significant market expansion.
Regional Breakdown
North America leads the market, benefiting from advanced healthcare infrastructure, high consumer awareness, and a large elderly population.
Europe follows, driven by favorable reimbursement policies and a rapidly aging demographic.
Within these regions, the United States stands out as the top performer, thanks to its large elderly population and high disposable income.
Germany ranks second, supported by strong healthcare systems and an increasing inclination toward quality incontinence care.
Market Segmentation
By Type: Disposable, Reusable By Product: Panty Liners, Pads & Guards, Belted & Beltless Underwear, Protective Underwear, Adult Diapers By Material Type: Cotton, Polymer, Super Absorbent Fibers, Non-woven Fabric By Application: Urinary Incontinence, Fecal Incontinence, Post-surgical Care By End User: Hospitals, Clinics, Homecare Settings, Long-term Care Facilities By Technology: Odor Control, Moisture Lock, Breathable Materials By Functionality: Daytime Use, Night-time Use, Heavy Incontinence, Light Incontinence By Form: Thin, Regular, Thick By Deployment: Online Retail, Pharmacies, Supermarkets
Key Market Players
Major players such as Kimberly-Clark Corporation, Essity AB, and Procter & Gamble dominate the market, leveraging advanced absorbent technologies to maintain their market positions and meet the growing demand for quality incontinence care.
#IncontinenceCare #AdultIncontinence #PersonalHygiene #DisposablePads #ReusablePads #AgingPopulation #WomenHealth #HygieneInnovation #ComfortAndDignity #QualityCare #UrinaryIncontinence #FecalIncontinence #HealthcareInnovation #MarketGrowth #HealthAndWellness
The incontinence pads market is set for continued growth, driven by an aging global population, evolving healthcare systems, and increasing awareness about incontinence care. This trend presents significant opportunities for innovation and tailored marketing strategies.
0 notes
Text
🌟 Tired of Leaking? Discover the Secrets to a Dry Life! 🌟 https://thewomenshealth.clinic/ https://youtu.be/Le5NRfqeIQc Urinary incontinence can be a sensitive topic, but you're not alone. Millions of people face this common issue, and there are solutions available to help you regain control. 🚫🚽 In this quick video, we cover: 🔹 Types of urinary incontinence & their causes 🔹 Non-surgical solutions like pelvic floor exercises 🔹 Surgical options for a permanent fix 🔹 Tips to prevent urinary incontinence from taking over your life 🎥 Watch now to learn how you can take back your confidence and live leak-free! #WomensHealth #UrinaryIncontinence #BladderControl #HealthTips #Wellness #ConfidenceBoost #DryLife #PelvicFloorHealth
0 notes
Text

Acupuncture Treatment For Urinary Incontinence in Chennai.
While we specialize in treating urinary incontinence, our clinic offers a wide range of acupuncture services. From fertility acupuncture to migraine headache relief, insomnia management, and more, we’re committed to enhancing your health and well-being. Visit us at our serene clinic in Anna Nagar or Chetpet for personalized care and lasting results.
Acupuncture Treatment For Urinary Incontinence in Chennai.
#ChennaiAcupuncture#AcupunctureChennai#acupuncturetherapy#jayanthacupuncture#acupunctureclinic#acupuncture#BestAcupuncturistChennai#AcupunctureAnnanagar#அக்குபஞ்சர்#AcupunctureTreatment#AcupunctureClinic#AcupunctureTreatmentForUrinaryIncontinence#TreatmentForUrinaryIncontinence#UrinaryIncontinence
0 notes
Text

Types of Urinary incontinence | Best Urology Hospitals in Bellandur | Nelivigi Urology
Best Urology Hospitals in Bellandur | Nelivigi Urology. Know about the types of Urinary incontinence. If you are struggling with any of these problems, consult our urologist in Bellandur, Bangalore today!
To book an appointment reach us @ 070222 09038 / 63662 08767 or log on to http://www.nelivigimultispecialityhospital.com/
#UrinaryIncontinence #UrologicalHealth #urologicaldiseases #UrologyHealthMatters #Urology #UrologyAwareness #urologicalproblem #urologyhospital #urologyproblems #urologydoctors #urologyclinic #NelivigiUrology #NelivigiMultispecialityHospital #DrGirishNelivigi #UrologyHospitals #UTI #UrinaryInfection #UrinaryTractInfection #Bellandur #Bangalore
0 notes
Video
youtube
உங்களது மூத்திரத்தை அடக்க முடியவில்லையா அது Spinal பிரச்சினைகளாக கூட இரு...
Urinary incontinence due to spinal issues உங்களது மூத்திரத்தை அடக்க முடியவில்லையா அது Spinal பிரச்சினைகளாக கூட இருக்கலாம் spinal issues - Like neurogenic Bladder may the reason for urinary incontinence மூத்திர பையின் பலகீனம் முதுகு தண்டு வட நோய்கள் டிஸ்க் நோய்கள் காரணமாக இருக்கலாம் other than pelvic floor muscle weakness and BPH - there are so many reasons for urinary incontinence #urinaryincontinence #urinedripping #யூரின் #மூத்திரம்அடக்கமுடியவில்லையா #தும்மினால்யூரின் #அடக்கமுடியாதயூரின் # யூரின் #மூத்திரம் #alshifaayush
0 notes
Text
What are the suggestions for improving urinary incontinence?
Ingest a moderate amount of fluids.Ingest more fluids(not including alcohol or caffeine) can reduce urinary incontinence. If you don't have enough fluid, your urine will be concentrated. Concentrated urine will irritate your bladder wall, causing it to contract more frequently, making you feel urgency. Of course, avoiding fluid intake before going to bed and before going out can reduce accidents.🔸
Reduce alcohol intake. Drinking alcohol can aggravate urinary incontinence. Alcohol can also cause unnecessary bladder contractions. Reducing alcohol intake or stopping drinking can help improve symptoms.🧡
lose weight. Being overweight can put extra pressure on the pelvic floor muscles. This extra pressure weakens the muscles. If you are overweight, losing weight can improve your symptoms. The best way to lose weight is to change your diet and exercise regularly.🧐
2 notes
·
View notes
Text
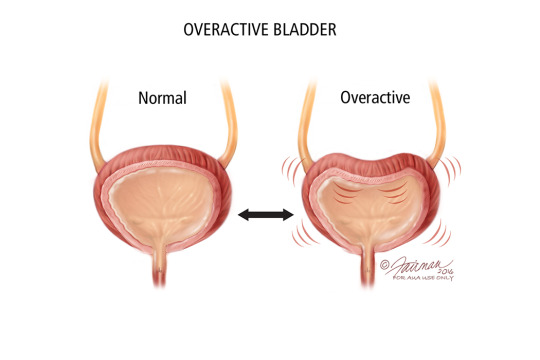
Difference Between Overactive Bladder and Incontinence
Interruptions in the body’s natural way of functioning can be challenging and frustrating to deal with. One such condition—urine leakage can not only restrict a sufferer’s lifestyle and freedom of movement, but also impair their mental health due to prevailing social stigma.

As patients, caregivers or family members the best we can do in such situations is to stay informed and aware of the best practices to help sufferers cope with dignity and ease.
Incontinence Vs Overactive Bladder
We’ve all seen advertisements for adult diapers and are familiar with the product. However, little awareness exists on the conditions that necessitate the use of adult diapers. Two names that commonly come up alongside the mention of disposable adult diapers are urinary incontinence and overactive bladder.
Both these conditions involve malfunctions in the urinary bladder that result in premature or unexpected bladder contractions or pelvic muscle contractions.
However, they are not the same. Overactive bladder is a condition that involves issues with one’s urge to urinate. Urinary incontinence, meanwhile, is not a condition, it is a symptom. This occurs when one loses control of their bladder causing the frequent or uncontrolled leakage of urine.
Let us explain in detail.
Overactive Bladder

Overactive or irritable bladder is basically classified as experiencing sudden, overwhelming urges to urinate.
Usually, after a person’s bladder fills close to its capacity with urine, the bladder sends a signal to the brain. The brain interprets this and sends a message back to the urethra, signalling that it must open and empty the bladder. This same signal is interpreted by our conscious selves as the urge to urinate, requiring us to find a toilet. However, in a patient with an overactive bladder, this system of signals is interrupted.
Instead of starting as a mild need to urinate, getting stronger as the bladder fills; a person with an Overactive Bladder may only receive strong, urgent signals; even when the bladder is not entirely full. An Overactive Bladder can also cause patients to experience a more frequent need to urinate, requiring them to rush to the toilet more than eight times during the day and over twice at night.
Overactive bladders are more commonly experienced by women and may be caused due to neurological conditions such as multiple sclerosis, Parkinson’s, stroke or diabetes. Overconsumption of diuretics such as alcohol and caffeine, which cause the body to produce more urine, can also contribute to the condition. However, for most people the cause is unknown.
Pelvic floor exercises, Kegels, weight loss and bathroom training can help in a large way to manage urinary incontinence. In the last few years with greater access and lowering in prices, the use of adult diapers have become increasingly common. Overnight diapers for adults can especially help both sufferers and their caregivers receive much needed rest at night.
Oral medications and Botox injections are also becoming increasingly popular in dealing with the condition. However, surgeries are not often fool proof especially in elderly patients with other health complications.
Urinary incontinence
Urinary incontinence, meanwhile, has more to do with a failure in the structure of the urinary system. This usually happens when pelvic floor muscles that support the urinary system weaken, allowing urine to seep out of the bladder due to activities that stress these muscles.
Urinary incontinence can be of five types:
Stress incontinence - when activities such as coughing, sneezing, laughing, exercising or lifting something heavy exert a pressure on bladder muscles causing them to squeeze out urine.
Urge incontinence - this resembles an overactive bladder and may be caused due to a sudden urge to urinate followed by the involuntary loss of urine.
Overflow incontinence - when you experience a constant leak or dribbling of urine, perhaps in tiny spurts, due to a bladder that fails to empty completely.
Functional incontinence - when a physical or mental impairment such as say arthritis stops you from reaching the toilet in time.
Mixed incontinence - when one experiences a mixture of these types.
Urinary incontinence is often induced as a by-product of ageing which may cause the loosening and weakening of one’s pelvic muscles; or post-surgery, post-pregnancies and due to obesity. It occurs in both men and women and is often handled simply by the use of disposable adult diapers.
Adult diapers are unisex and easy to use. They come in pant-style and tape-style and also have overnight adult diaper variations. Various brands now manufacture disposable adult diapers that can be used up to 16 hours without discomfort. Adult diapers with anti-bacterial technologies can also help keep dampness and skin rashes caused due to cloth liners at bay.
Differences in Overactive Bladder and Urinary Incontinence
Thus, to recap, the frequent urge to urinate, and use of adult diapers and pelvic floor muscle exercises as methods of management, are common to both overactive bladder and urinary incontinence. The differences between the two are as follows:
Overactive bladder is a condition in itself while urinary incontinence is usually a symptom of a different cause.
Overactive urge has more to do with the urge to urinate while urinary incontinence pertains to the actual leakage of urine.
While both are related to the urge to urinate, the urge caused by an overactive bladder may not actually be followed by urine leakage.
Urinary incontinence has more to do with a weakening of muscles while an overactive bladder is linked to neurological issues.
Overactive bladder commonly affects women, while urinary incontinence, often as a by-product of ageing affects both men and women equally.
The normal adult bladder can hold up to 300-400ml (roughly 2 cups) of urine during the day and up to 800ml (4 cups) during the night. Issues that disrupt the functioning of the bladder can be difficult to deal with. But with the right attitude, support, exercises and a few adult diapers everything can be managed.
Image Source: https://startsat60.com, www.everydayhealth.com
19 notes
·
View notes
Text
Conquering Urinary and Fecal Incontinence

By Kimberly Wilkes
This article originally appeared in Whole Health Insider
If you have urinary or fecal incontinence, it's probably not something you want to shout from the rooftops. So it's not surprising that researchers have found that only 38 percent of women with urinary incontinence talk about it with their doctors.1 And doctors aren't likely to bring up the topic either, as one study found that physicians initiated the conversation about urinary incontinence in only 7 percent of the cases.2 The same is true for fecal incontinence, which is just as embarrassing.
If you're having trouble reaching the bathroom in time, it's frustrating. It can affect your mood and your quality of life. And as you grow older it can take away your independence. But you'll be glad to know it's not hopeless. In this article you'll learn about some ways you can find relief from these two pressing concerns.
Urinary Incontinence
There are several types of urinary incontinence including stress incontinence, urge incontinence and overflow incontinence. Stress incontinence is caused by anything that increases pressure in your abdomen such as coughing, sneezing, exercise and laughing. Urge incontinence is what the name implies—you urgently have to urinate but might not get to the bathroom in time. There's also overflow incontinence, more common in men, where the bladder doesn't empty all the way and urine leaks out.
Urinary incontinence doesn't affect younger women as much as older women. It's most common from menopause into later life. Many people who have incontinence suffer from either stress incontinence or a mixture of stress and urge incontinence. Severe incontinence occurs much less in young women, but its prevalence rapidly rises from age 70 to 80.3 The condition doesn't occur as often in men, but when it does urge incontinence accounts for 40 to 80 percent of all cases in men. Stress incontinence occurs most often in men who have had prostate surgery or neurological injury.3Men also experience an increase in urinary incontinence as they grow older, but even so, the presence of severe incontinence in 70- to 80-year-old males is about half that of females.3
Who's at Risk?
In women, many risk factors exist for incontinence including age, obesity, diabetes, high-impact exercise and estrogen deficiency.4Pregnancy also increases the risk of urinary incontinence because giving birth may damage the nerves that control the bladder, cause the urethra and bladder to move positions. When a doctor delivering a baby performs an episiotomy, an incision in the pelvic floor muscle during delivery to help the fetus emerge more easily, this also increases the risk of urinary incontinence.5 Men who have had their prostate gland removed due to cancer are at an increased risk.6
It also turns out that a weak heart may equal a weak bladder. As many as 50 percent of heart failure patients have lower urinary tract symptoms, including incontinence. Heart failure patients who also have urinary incontinenceare worse off than patients without urinary incontinence and urinary incontinence occurs three times more often in people who have New York Heart Association Class III and IV symptoms compared with people who have less severe heart disease.7The heart failure itself might contribute to the incontinence, but drugs such as diuretics, angiotensin-converting enzyme (ACE) inhibitors and beta-blockers used to treat heart failure may also cause or worsen urinary incontinence.7
Being overweight won't do your bladder any favors, either. Women of all ages who pack on too many pounds are at an increased risk of urinary incontinence.8 When researchers reviewed the medical literature, they looked at six studies including 2,352 subjects and found that non-surgical weight loss improved urinary incontinence.9They concluded that weight loss "should be considered part of standard practice in the management of urinary incontinencein overweight women."
In addition, post-menopausal women who are treated with conjugated equine estrogens as part of hormone replacement therapy are at risk for the development and worsening of stress and urge incontinence.10 However, estrogen applied topically is associated with an improvement in urinary incontinence.
Natural Solutions for Urinary Incontinence
If you have urinary incontinence and you're overweight, losing weight should be the first priority. Not only will your bladder thank you, your wallet will, too. Urinary incontinence costs the United States $20 billion per year. In obese and overweight women who lost weight, improved urinary incontinence resulted in a savings of at least $327 per woman, per year.11
Physical exercise is important, too. Even though high-impact sports increase the risk of urinary incontinence, mild or moderate physical activity—for example, brisk walking—lowers the risk of developing this condition in the first place.12
Exercises to help strengthen the pelvic floor are another way to eliminate urinary incontinence in both women as well as in men who have undergone prostate surgery.
Pelvic floor muscle exercises assist with urinary control by improving the strength, endurance, and coordination of the pelvic floor muscles. The exercises also improves the function of the urethral sphincter, a muscle that controls the exit of urine from the bladder through the urethra.6
To perform pelvic floor muscle exercises, you "lift up" the pelvic floor so that the flow of urine stops. Voluntarily starting and stopping urination can help identify which muscles you need to exercise. In men, a biofeedback session before radical prostatectomy (surgery to have the prostate removed) together with pelvic floor muscle training after surgery and assisted monthly sessions, reduced urinary incontinence.13
There are several different types of pelvic floor muscle exercises, but the best known are Kegel exercises. A study of 38 women with stress incontinence and 34 women with mixed stress and urge incontinence found that 68.4 percent of the women in the stress incontinence group and 41.2 percent of the women in the mixed incontinence group experienced significant improvements after doing home-based Kegel exercises. Women who had stress incontinence experienced the greatest improvements.14
To learn how to do Kegel exercises correctly, take a look at the table below:
How to Do Kegel Exercises
1. Identify the pelvic floor muscles by stopping urinationmidstream. If your urine stops, you've found the right muscles.
2. The exercises can be done in any position, although at first, doing them lying down might be easier.
Once you've identified the muscles, tighten andhold for five seconds, and then relax for five seconds. Do this four or five times. Ultimately, you'll want to work up to keeping the muscles tightened for 10 seconds and then relaxing for 10 seconds before repeating the exercise.
Be certain to tightenonly your pelvic floor muscles and not the muscles in your abdomen, thighs or buttocks. Make sure you're not holding your breath.
For the best results, plan on performing at least three sets of 10 repetitions daily.
Source: mayoclinic.org
Both men and women can benefit from a newer type of pelvic floor muscle exercise known as “Pfilates” (PelvicFloorPilates). Pfilates combines pelvic floor muscle exercises with Pilates, a type of exercise which is performed in order to improve core strength, stability, flexibility and muscle control of the body as a whole, as well as posture and breathing. One study of 62 women found that both pelvic floor muscle training and Pfilates were equally effective in improving pelvic muscle strength.15The women in the study did not have urinary incontinence, but the results are a good sign that both types of exercises may benefit people who have incontinence. A study is also underway of the effectiveness of Pfilates in men who have undergone radical prostatectomy.6You can learn how to do Pfilates by watching these videos.
Nutritional Supplements to Support Pelvic Muscles
First, make sure you're not deficient in vitamin D because some studies have shown that supplementing with vitamin D can result in the resolution of urinary incontinence.16
A combination of horsetail (
Equisetum
arvense
)and Crateva nurvalacan also help get your bladder back on track. Horsetail acts as a mild diuretic without causing your body to eliminate too many electrolytes. In a double-blind, randomized clinical trial of 36 healthy male volunteers, researchers divided the subjects into three groups who received a three-part treatment that included 900 mg/day of horsetail for four days then 25 mg per day of the diuretic drug hydrochlorothiazide for another four days, and then a placebo for another four days. There was a 10-day break between each of the treatments. When they subjects were taking the horsetail, they experienced a diuretic effect equivalent to that of hydrochlorothiazide.
17
Crateva when combined with horsetail can help relieve urinary incontinence. One study investigated the effectiveness of these two botanicals on 34 people (6 males and 28 females) with symptoms of urge incontinence and/or stress incontinence.18The researchers administered two questionnaires to determine how incontinence was impacting the life of the subjects before they were given Crateva and horsetail and at the first, second and third month of treatment. The Incontinence Impact Questionnaire (IIQ) measures impact on daily activities, such as household chores, physical activity and social activities, and the Urogenital Distress Inventory (UDI) measures physical symptoms such as leakage and urgency.
While supplementing with Crateva and horsetail, on average, daytime urinary frequency declined steadily during the three months of treatment. The amount of times the subjects needed to empty their bladders fell from 12.3 times per day before treatment to 9.3 times per day after one month and 7.4 times per day after two months. By month three urination frequency returned to a normal 6.2 times per day.
In addition, the subject's night awakenings to go to the bathroom gradually went from 2.5 times per night to 1.8 times in the first month, 0.94 times in the second month and 0.74 times per night in the third month.
What's more, the results of the UDI and IIQ questionnaires indicated that having symptoms of incontinence negatively impacted quality of life as measured through difficulty in doing daily and social activities as well as emotional health and feelings of frustration caused by incontinence. Yet, after supplementing with the two botanicals, in all of these areas participants felt better about their life in all of these areas and were more confident within four weeks of treatment. And they continued to improve more throughout the rest of the study.
The study authors concluded that Crateva combined with horsetail was a suitable and effective treatment for both men and women with incontinence. Supplementing with the two botanicals was not associated with any adverse reactions.
And if your incontinence is caused by chemotherapy or radiation, try supplementing with L-glutamine. An animal study found that supplementingwith L-glutamine stops the damage that occurs in the bladder wall after radiation therapy.19
Fecal Incontinence
About 10 percent of adults have fecal incontinence.20 It can affect people of all ages, but it's more common in older adults, especially nursing home residents.21Fecal incontinence also is more common in women than men and it often goes hand in hand with urinary incontinence.21
Fecal incontinence falls into three categories: 1) passive incontinence voiding stool when you don't even feel like you have to go to the bathroom; 2) urge incontinence, when you're unable to wait to get to the bathroom; 3) fecal seepage, the accidental elimination of small amounts of stool.
Risk factors for fecal incontinence include anatomical changes that occur due to trauma as well as surgery, vaginal deliveries, radiation therapy for cancer, neurologic disorders, obesity, diabetes, smoking and aging.21,22
The reason why females suffer from fecal incontinence more than males is because of either maternal injuries that happened when they were giving birth or in the case of fecal incontinence that develops later in life, changes in the pelvic floor that occur due to menopause and aging.21If you suffered nerve damage during childbirth in your 20s and 30s, there can be a delayed reaction, with fecal incontinence developing in your 50s as the nerve damage grows worse over time.21
Fecal incontinence can cause a lot of embarrassment, disrupt quality of life and is associated with other complications such as dermatitis of the anal/rectal area.23
Solutions for Fecal Incontinence
If you or somebody you know suffers from this condition, there are several ways you can reduce the chance of any embarrassing accidents. First, try biofeedback, which is a technique that will train you to control muscle tension through the use of electrical sensors. Many studies have shown it's effective in fecal incontinence. For example, in one study of 75 people (mean age about 61) with fecal incontinence both quality of life and embarrassment improved, especially in the younger subjects.24
Biofeedback combined with anal sphincter exercises can re-train anal muscles and is more effective than doing just the exercises alone. Aim for 10 squeezes of five seconds each five times daily.21
Another good option is to take a fiber supplement that contains psyllium. One recent study compared the effects of 16 grams per day of three dietary fiber supplements— carboxymethylcellulose [CMC], gum arabic or psyllium—to a placebo in 189 people with fecal incontinence. In the 32-day study, frequency of fecal incontinence significantly decreased in the subjects supplementing with psyllium while the fiber CMC actually increasedfrequency of fecal incontinence. After supplementation, the number of fecal incontinence episodes per week was 5.5 for the placebo group, 2.5 for psyllium, 4.3 for gum arabic and 6.2 for CMC.20
Fiber lessens fecal incontinence by improving sensory awareness of the need to go to the bathroom, reducing the liquidity of feces or causing more stool to be eliminated during bowel movements, so that less remains in the rectum to leak.20Just be sure not to consume too much fiber or it can backfire. It's a good idea to consume no more than the 16 grams of psyllium, the amount used in the above study.
As with urinary incontinence, with fecal incontinence having your doctor test your vitamin D levels is important. Vitamin Dplays an important role in the functioning of muscles. Women who have fecal incontinence are more likely to have low vitamin D levels and have greater odds of vitamin D deficiency compared to women who don't have incontinence.25
Finally, experiment with avoiding possible food triggers such as caffeine, citrus fruits, spicy foods, alcohol or dairy products to see if it helps.21
When You Gotta Go. . .
Urinary and fecal incontinence are embarrassing problems that can make you avoid social activities and lead to depression. But there are plenty of ways you can help eliminate these two problems. For urinary incontinence, special exercises, supplementation with vitamin D, horsetail (Equisetumarvense)and Crateva nurvala, physical exercise, weight loss and L-glutamine (for incontinence from radiation therapy) can all help stop untimely accidents. For fecal incontinence, vitamin D is also important as well as a psyllium fiber supplement, biofeedback and anal sphincter exercises. Avoiding certain possible trigger foods might also help.
References:
1. Kinchen KS, et al. J Womens Health (Larchmt). 2003 Sep;12(7):687-98.
2. Grzybowska ME, et al. BMC Womens Health. 2015 Sep 30;15(1):80.
3. Nitti VW. Rev Urol. 2001;3(Suppl 1):S2-6.
4. Newman DK, et al. Curr Opin Obstet Gynecol. 2013 Oct;25(5):388-94.
5. WebMD. http://www.webmd.com/urinary-incontinence-oab/america-asks-11/pregnancy
6. Santa Mina D, et al. BMC Urol. 2015 Sep 16;15:94.
7. Tannenbaum C, Johnell K. Drugs Aging. 2014 Feb;31(2):93-101.
8. Wesnes SL. Int Urogynecol J. 2014 Jun;25(6):725-9.
9. Vissers D, et al. Obes Rev. 2014 Jul;15(7):610-7.
10. Waetjen LE, et al. Menopause. 2013 Apr;20(4):428-36.
11. Subak LL, et al. Obstet Gynecol. 2012 Aug;120(2 Pt 1):277-83.
12. Nygaard IE, Shaw JM. Am J Obstet Gynecol. 2015 Sep 5. [Epub ahead of print.]
13. Tienforti D, et al. BJU Int. 2012 Oct;110(7):1004-10.
14. Cavkaytar S, et al. Obstet Gynaecol. 2015 May;35(4):407-10.
15. Culligan PJ, et al. Int Urogynecol J. 2010 Apr;21(4):401-8.
16. Gau JT. J Am Geriatr Soc. 2010 Dec;58(12):2438-9.
17. Carneiro DM, et al. Evid Based Complement Alternat Med. 2014;2014:760683.
18. Schauss AG, et al. Reducing the symptoms of overactive bladder and urinary incontinence: results of a two-month randomized, double-blind, placebo-controlled clinical trial. 2006 (unpublished research).
19. Rocha BR, et al. Nutrition. 2011 Jul-Aug;27(7-8):809-15.
20. Bliss DZ, et al. Res Nurs Health. 2014 Oct;37(5):367-78.
21. Lee YY. Front Med (Lausanne). 2014 Mar 24;1:5.
22. Fox A, et al. FP Essent. 2014 Apr;419:35-47.
23. Rohwer K, et al. J Wound Ostomy Continence Nurs. 2013 Mar-Apr;40(2):181-4.
24. Bartlett L, et al. J Clin Gastroenterol. 2015 May-Jun;49(5):419-28.
25. Parker-Autry CY, et al. Int Urogynecol J. 2014 Nov;25(11):1483-9.
0 notes
Photo

The two most common types of urinary incontinence that affect women are stress incontinence and urge incontinence also called overactive bladder. Urinary incontinence affects more women than men. Women have unique health events like pregnancy, childbirth, and menopause that may affect the urinary tract and the surrounding muscles. Your Urologist will work with you to cure your urinary incontinence completely.
1 note
·
View note
Text
Incontinence Pads Market: From $9.1B (2023) to $15.4B (2033), CAGR 5.7%.
Incontinence Pads Market : Incontinence pads are specialized absorbent products designed to manage bladder or bowel incontinence, providing comfort, hygiene, and confidence to users. These pads are typically disposable and come in various sizes and absorbency levels to suit individual needs. They are widely used by individuals experiencing urinary incontinence, postpartum women, and those recovering from surgery or facing age-related issues. Their design ensures effective moisture control, odor management, and skin protection, enhancing the quality of life for users.
To Request Sample Report: https://www.globalinsightservices.com/request-sample/?id=GIS25886 &utm_source=SnehaPatil&utm_medium=Article
The market segments for incontinence pads include light, moderate, and heavy absorbency pads, catering to different degrees of incontinence. Additionally, the market is divided based on end-users, such as hospitals, nursing homes, and individual consumers. Key trends shaping the industry include the rising adoption of eco-friendly and biodegradable pads, advancements in ultra-thin and discreet designs, and an increasing focus on gender-specific products to better cater to men and women. Moreover, e-commerce platforms are driving growth by making these products readily accessible.
The key drivers of the incontinence pads market include an aging global population, increased awareness of personal hygiene, and the growing prevalence of conditions such as diabetes and obesity that contribute to incontinence. Additionally, innovations in materials and manufacturing have enhanced the comfort and functionality of incontinence products. Leading players in the market include Kimberly-Clark Corporation, Procter & Gamble, Essity AB, HARTMANN Group, Ontex Group, and Domtar Corporation, among others.
#IncontinenceCare #HygieneProducts #PersonalCare #AgingPopulation #SustainableHygiene #HealthcareInnovation #UrinaryIncontinence #AbsorbentProducts #SkinCareProtection #EcoFriendlyPads #GenderSpecificCare #PostpartumCare #ModernHealthcare #ElderlyCare #HealthcareTrends
0 notes
Text

🌟 Tired of Leaking? Discover the Secrets to a Dry Life! 🌟 https://thewomenshealth.clinic/ https://youtu.be/Le5NRfqeIQc Urinary incontinence can be a sensitive topic, but you're not alone. Millions of people face this common issue, and there are solutions available to help you regain control. 🚫🚽 In this quick video, we cover: 🔹 Types of urinary incontinence & their causes 🔹 Non-surgical solutions like pelvic floor exercises 🔹 Surgical options for a permanent fix 🔹 Tips to prevent urinary incontinence from taking over your life 🎥 Watch now to learn how you can take back your confidence and live leak-free! #WomensHealth #UrinaryIncontinence #BladderControl #HealthTips #Wellness #ConfidenceBoost #DryLife #PelvicFloorHealth
0 notes
Link
Medical advances have created a better world. Little inventions aid in patient’s lives helping them thrive with dignity. Urinary incontinence refers to the unintentional passage of urine due to loss of bladder control. There are of course different degrees of the same. Overactive bladder incontinence is the urge to urinate even if the bladder is not full. Stress incontinence refers to leakage caused by a physical strain; examples include laughing or coughing. Reflex incontinence occurs due to some neurological problems such as spinal injury,
#incontinence#incontinenceproducts#incontinencepads#urinaryincontinence#incontinencepants#incontinenceunderwear
0 notes
Text

Urinary Incontinence Facts | Nelivigi Multispeciality and Urology Hospital Bellandur, Bangalore
Urology Hospital Bellandur, Bangalore | Nelivigi Multispeciality and Urology Hospital. Did you know? Urinary Incontinence which is the involuntary loss of urine, is more common in females than in males. Consult our Urologist today!!
To book an appointment reach us @ 070222 09038 / 63662 08767 or log on to http://www.nelivigimultispecialityhospital.com/
#UrinaryIncontinence #UrologicalHealth #urologicaldiseases #UrologyHealthMatters #Urology #UrologyAwareness #urologicalproblem #urologyhospital #urologyproblems #urologydoctors #urologyclinic #NelivigiUrology #NelivigiMultispecialityHospital #DrGirishNelivigi #UrologyHospitals #UTI #UrinaryInfection #UrinaryTractInfection #Bellandur #Bangalore
0 notes
Text

Urinary Incontinence
5 reasons why you shouldn't ignore
CN: 29.09.2021 11:00-13:00
US: 28-09.2021 23:00-03:00
https://watch.alibaba.com/v/fe86b869-b527-4031-8130-611ffab6235a?referrer=SellerCopy
#Urinary #UrinaryIncontinence #Incontinence #incontinencepads #BladderControlPads #GuardsforMen #urinepad #adultincontinencepads #adultpad #Adultincontinence
#Urinary Incontinence#Urinary#UrinaryIncontinence#Incontinence#incontinencepads#BladderControlPads#GuardsforMen#urinepad#adultincontinencepads#adultpad#Adultincontinence#factory
0 notes
Text
Association of Menopause and Incontinence

Millions of women experience “urine leakage” or urinary incontinence. The frequency of involuntary urine leakage will only increase as a women ages. Around 51.9% of women, aged over 70 years suffer from some or the other form of incontinence.
A person is said to not suffer from urinary incontinence if their normal bladder function is as follows:
1. The frequency of urine is 4-6 times during the day and 0 to 1 times at night.
2. On an average 1-2 cups of urine (i.e. approx. 200-500mls) is passed.
3. The bladder can easily hold in the urine for some time till you find a washroom.
4. There are no urine leaks between washroom visits.
5. Urine is passed in a continuous stream until the bladder is empty.
A woman may experience UI across difference stages of her life but most episodes are a result of pressure or a stress on the muscles that help you hold or pass urine. The most common types of urinary incontinence that affects women at large are urge & stress incontinence. Urge incontinence usually occurs when an individual’s bladder muscles squeeze incorrectly or simply lose the ability to relax. This makes them feel a constant urge to urinate, even when their bladder is empty. It may also lead to leaking of urine. This is also known as an “overactive bladder”.
Stress incontinence is the most common form of incontinence. Weakened muscles can’t hold back the urine when you cough, exercise, sneeze, laugh, or lift something heavy. This can result in minor leakage or sometimes complete loss of control. This type of incontinence is often managed by using adult diapers during the day and disposable underpads for adults in the night.
Hormonal changes have a huge impact on the pelvic muscles, making UI common amongst woman who are pregnant, giving birth or going through menopause. Most of them buy adult diapers online to manage UI.
Menopause is a critical phase in a woman’s life. The period of menopausal transition causes metabolic changes that impact the health of every woman. Certain reports suggest that the effects of menopause are visible even before the onset of menopause. Women go through various unpleasant symptoms that worsen the quality of their life. The effects of menopause are many and one of them is weakened pelvic muscles. As menopause approaches the level of estrogen in a woman’s body begins to drop. As the levels of estrogen reduce, they cause the pelvic muscles to weaken therefore reducing their ability to exercise control over the urinary bladder.
As a result of the post-menopausal transition, the estrogen levels continue to drop which further weakens the pelvic muscles thereby worsening the symptoms of UI. There are various diapers for old age women available in the market which can help manage these symptoms. One can buy adult diapers online on friendsdiapers.in.
Image Source: gbmc.org, urologyhealth.org, rcni.com
3 notes
·
View notes