#the unstressed a gets very weakened
Explore tagged Tumblr posts
Text
Jake's name is actually Tsyeyk in Na'vi, as the Na'vi language doesn't have a J sound! As for Norm, his name wouldn't have to change too much. His first name would become Normì (the extra ì is added because in Na'vi consonants can't cluster at the end of a syllable, so we have to add a second syllable to separate the r and the m (nor-mì)).
His last name would actually be pronounced pretty much exactly the same as it is in English, as it doesn't contain any sounds or syllables that don't work in Na'vi, but it would be written Spelmìn!
So, Normì Spelmìn and Popiti te Spelmìn ;)
Norm family lore drop!!
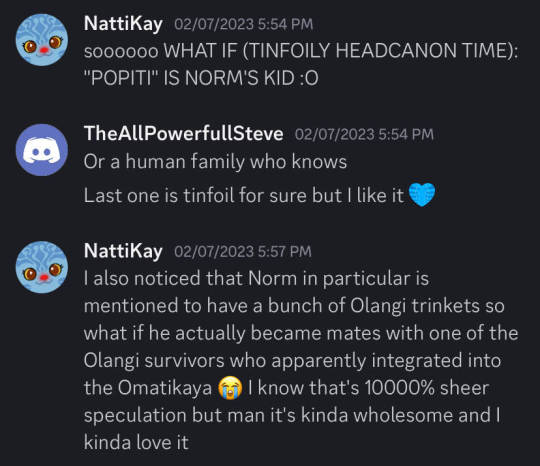
so for Avatar fans who don't already know, Kelutral's "Omaticon" online convention (streamed on their Twitch channel) is going on this weekend, and the kickoff panel earlier this evening featured franchise loremaster Josh Izzo.
Some may remember this little panel in the High Ground, featuring Norm with a Na'vi child addressing him as "Daddy":

In the Visual Dictionary, there's also a very brief mention that Tuk has a best friend named Popiti.

...so here's the fun bit:
Izzo confirmed that this "Popiti" is in fact Norm's kid!!
Apparently Popiti also has a sibling, and her mother/Norm's mate is from the Olangi clan (which makes sense given that the Visual Dictionary mentions Norm having a bunch of Olangi trinkets).
ngl I love this lore drop but now I have so many more questions also!! How old is Popiti (I assume close to Tuk's age since they're best friends but there's still some wiggle room there so)? Is her sibling older or younger and what's his/her name? If they're Norm's biological kids, do either of them have avatar features like Kiri and Lo'ak? What's Norm's wife's name, what's their story? Norm didn't get his consciousness permanently transferred like Jake did, so how does him switching between two bodies affect things? PLZ I NEED TO KNOW

@theoptimistictabby thought you'd be interested in this one ;)
btw let it be known that I speculated all these things like two years ago, my mind is still reeling that what I thought was merely wild wishful-thinking speculation at the time turned out to be CANON lol
#lì'fya leNa'vi#my first thought was actually Spelmän (ä is pronounced like in the English word “man”)#but thinking about it more he doesn't really SAY it like “spell man” even though it's spelled that way#the unstressed a gets very weakened#so I think Spelmìn is closer#(ì is pronounced like in the English word “spin”)#and yeah alas we can't know Popiti's FULL name without knowing her mother's name (izzo plz i beg!!!) but this would be her surname#also 👀 on the sketch hrh#i may or may not also be planning a silly little comic#it's technically still Jeytiri centric but does feature Norm and Popiti 👀👀
223 notes
·
View notes
Text
🍺 About Khleo 🍺

portrait by @artsyaprilmr
“A secretive bartender who likes to bend the rules.”
Full name: Khlee von Heine
Nickname: Khleo (pronounced clay-oh with first syllable slightly unstressed. They k is not as hard as it is in Kipling, but more like the c in “cough.”)
Age: 26
Height: 5′6
Pronouns: she/they
Sexual Orientation: Bisexual
Most likely to... spike their milk before adding the cereal.
Occupation: Bartender / fight club manager
Favorite Food: Spargel
Favorite Drink: Hefeweizen
Zodiac: Aries Sun, Taurus Moon, Scorpio Rising
MBTI: ESTP
Love Languages: Acts of service, physical touch
Patron Arcana: Strength
Upright: inner calm, bravery, focus, patience
Reversed: struggle, anger, rage, pride
Flower: Daisy
Familiar: A lioness named Hefe
Appearance:
Light brown skin, freckles, golden brown afro-textured 3b curls
Most noticeable feature is their arms. They are very strong. Likes to show them off whenever they can (rolled-up sleeves all day long)
Personality: Serious, kind-hearted, and secretive. Big Flirt. Has occasionally been known to brood. Likes to get into things and break the rules. Big night owl. Likes to drink. Khleo is constantly stealing beer and wine from her job. Never gets fired because she’s the only employee willing to break up bar fights and take on the graveyard shifts.
Outside Character Influences: Spike Spiegel (Cowboy Bebop) / Steven/Stevonni (Steven Universe) / Gearless Joe (Megalobox) / Tyler Durden (Fight Club)
Fashion:
Functional, muted colors, comfortable
Lederhosen-inspired shorts, sometimes suspenders over a fitted button-down, sometimes no suspenders and wears a loose, lightly embroidered tunic. Boots with stockings.
Magic: No affinity for magic. Like Ozy and Kipling, they were born a grey mage, but all their magic was stripped from them during a teleportation accident around the age of fifteen. When it happened, Khleo was portaled through their patron Arcana’s gate. They sacrificed their magic for accelerated healing and a boost in strength before they were dumped in Vesuvia with most of their memories erased (wasn’t as bad as when Asra brought Kipling back, but Khleo has no memory of their childhood on their home island.)
Backstory: Khleo grew up in the Republic of Floating Isles in a grey mage monastery with Kipling and Ozy. They were born male. Khleo developed their bond with Kipling first and Ozy later. Though they cared deeply for both of their friends, they had a hard time getting Kip to fully accept Ozy into their inner circle. As a child, Khleo had a strong affinity for grey magic. They spent a lot of time with Kipling and by themself practicing on their own, learning through trial and error. Out of the three children, Khleo was the one who used the portals on themself the most. This affected Khleo’s physical appearance by making them leaner and taller, but also weakening their muscle mass and bone density. By the time Khleo turns fifteen, they have pretty defined features, but a thin frame and noodly arms (for which they are mercilessly teased by Kip and Ozy).
Then one fateful day, Ozy, Kipling, and Khleo were messing around with an ancient teleporting artifact. In the midst of Ozy and Kip’s squabbling, Khleo got sucked into a portal with one of the magical gauntlets. The other was on Kip’s hand. The portal closed before Khleo had a chance to create an exit. So they were trapped and neither Ozy nor Kipling could open the right portal to get them out. While racing through the portal, Khleo attempts to use their gauntlet to create a jump point. They end up passing through one of the gates of the major arcana – Strength. Not surprisingly, Strength is Khleo’s patron arcana. She gives them an ultimatum: Give up all their magic in exchange for something else or stay locked forever in her realm. Khleo, of course, wants to get back to their friends, so they give Strength permission to take their magic. Strength strips them of their magic and their memories. In exchange, she grants them all the “strength” they were lacking in their physical anatomy. Goodbye forever noodle arms. When Khleo is reborn in Vesuvia, they emerge from the portal as a biological female.
Khleo is discovered by one of the people who works in the coliseum. A man named Hans Heine, who feeds the gladiators and cleans the stalls. Hans and his partner, Magda, could not have any children, so when Hans finds Khleo, unconscious and pretty banged up, he brings her home. Hans and Magda are amazed by how quickly Khleo heals on her own. Khleo remains unconscious until Hans receives a vision of a lioness covered in clay. That morning Hans asks Magda if it’s okay to name the child Khlee von Heine because as he puts it, “the dream lion told me so.” This is when Khleo finally wakes up.
Khleo spent the remainder of their childhood growing up around the coliseum until it shut down. Their parents were poor and didn’t have the money to fund an education, so Khleo started fighting for money in underground pits and behind seedy bars. It was also during this time that Khleo’s parents suffered from the Red Plague. Khleo, desperate and afraid for their parents, sought out the Palace physicians and pretty much volunteered themself as a test subject in exchange for speedy medical assistance for their parents. Once Valdemar caught wind of this and got their hands on Khleo.... Long story short, Khleo was brought to the edge of death several times, never passing over due to their healing properties. Meanwhile, their parents never got that assistance and did not make it. When Valdemar tortured Khleo to the point where she seemed very dead, they dumped her body at the Lazaret. Khleo eventually regained consciousness, made their way back home and found their parents passed on from the plague.
After Khleo buried their parents, they became very withdrawn and mistrustful of just about everyone. They constantly fought in the streets. Got locked up a few times for it. For a long time, this was the only way they knew how to deal with their anger. It wasn’t until Khleo met Hefe, their familiar, that they were able to heal from the loss of their parents and deal with their unresolved pain. It took them a full year to work through everything, during which time they took an unofficial vow of silence.
The plague passed. Khleo eased back into society. Broke their silence. Started bartending full time. They still fought for sport, which eventually turned into a small business.
These days Khleo bartends, manages their fight club, and enjoys pissing off authority by bringing Hefe everywhere lions don’t belong. They still have absolutely no idea who Kipling and Ozy are and no knowledge of their origins as a talented grey mage.
@arcana-echoes
#khleo's backstory is a little insane#but i don't care#that's my little lion babe#just a tad feral#about khleo#khleo the barhand#khlee von heine#khleo bio#arcana eotp#door lords#melting world#coco's writing#oc writing
61 notes
·
View notes
Text
How to Care for Cactus and Succulent Plants
Did you know that cacti and succulents have soil, light, and water requirements? While both succulents and cacti store their own water, you can’t simply put them in a sunny corner and forget about them. These seemingly autonomous plants have some specific needs that may come as a surprise to you.
gardeninginfo-online.com gathered essential species information and growing tips to help you care for your cacti and succulents.
Succulent and Cactus Definition
In botany, succulent plants are those that have thick, fleshy parts (with a swollen appearance) that have the capability and are meant to retain water. By this definition, all cacti are considered succulents. However, not all succulents are cacti.
One of the principal differences lies in what are called areoles. Areoles, found on true cacti, appear to be small wads of cotton that roots, spines, and flowers grow from. Some succulents have spines, but look closely, they won’t have areoles.
Succulent and Cactus Soil Requirements
The soil succulents and cacti need to thrive is not the same as your typical garden soil. This soil must physically support the plant, retain some moisture and nutrients, and should be porous so that water is absorbed easily, then drained away quickly.
Succulent and cactus roots experience an essential and rapid exchange between water and air, which cannot take place when water is excessive.
While there is no perfect combination for the ideal soil, the following mix will support healthy growth. Examples of good soil mixes are:
• 2 parts potting soil • 1 part perlite • 1 part small gravel
Or,
• Equal parts potting soil and perlite
The following soil tips will help you get the soil right for your succulents and promote their continued good health:
• If sand is used in the mixture, use horticultural grade coarse sand. Finer non-horticultural sand will compress and harden, and likely contain salt among other impurities, making water drainage more difficult and potentially damaging your plants.
• You can test your soil by wetting it and squeezing it with your hands. If the soil mixture crumbles easily and loosely, you got it right. If it forms a ball or a lump, you may need to add more perlite, gravel, or sand.
• To further promote their good health, your succulents and cacti should be repotted with the appropriate soil every two years.
• As available soil components may vary in texture from region to region, you may need to experiment with several combinations to get your soil to the desired consistency.
Succulent and Cactus Water and Fertilizer Needs
To understand the need for water and fertilizer, you must be knowledgeable of a cactus or succulent’s growing period. For the majority of succulent and cactus species, this growing period begins in spring, slows in the height of summer, and resumes growth as temperatures drop. Then in mid to late fall, the plants enter a state of dormancy.
Watering Requirements – Cacti and succulents should be watered a minimum of once per week while in their growing period. When watering, you should aim to give the soil a good soaking until you see water coming from the drainage holes of the pots.
As cold weather sets in, watering intervals should be lengthened for your outdoor plants. For those plants kept indoors, not so much. In either case, let the potting mixture dry out between watering in the colder months.
Some cacti like the brittle prickly-pear, and some succulents like Sempervivum succulents, are winter growers and will require watering and fertilizing throughout the winter months.
Avoid using tap water or water that has passed through a softening system, over time, minerals and sodium can become trapped in the soil, causing harm to the plants. Purified water or rainwater are preferred for your succulents and cacti.
Fertilizer Needs – Only fertilize your succulents and cacti while in the growing period. Cease fertilization in late summer to avoid encouraging new growth in the winter (unless they are winter hardy).
A 10-10-10 fertilizer containing equal parts of Nitrogen, Phosphorous, and Potassium diluted to one-quarter strength is ideal for succulent and cactus growth. Simply add the solution to the water for each watering.
For more info on cactus and succulent watering and fertilizing, visit csssj.org/welcome_visitors/basic_culture.html
Succulent and Cactus Light Requirements
The majority of succulent and cactus species flourish in bright light. However, intense, direct sunlight coupled with high temperatures can damage your plants.
While the amount of sunlight your plants will thrive in depends on their species, the following indicate that your plants are getting either too much or too little light:
Too Much Light – Succulents and cacti exposed to too much light may change color. Some may appear bleached or lose their color, while others may turn hues of yellow or orange.
When making a diagnosis, bear in mind that this color change may also indicate other stressors like overwatering or disease.
Scorching can occur when a plant is moved to a location with brighter light conditions, or when the weather abruptly changes to hot and sunny conditions. Scorching scars a plant for life and should be avoided.
Too little light – Insufficient lighting may cause your plant to reach for a light source (known as etiolation). To avoid imbalanced growing patterns, you can rotate the pot to help the plant grow in a more balanced fashion.
When moving a plant to a stronger light source or rotating it for balanced growth, use caution to avoid scorching the plant. Slow transitions are a vital element in allowing your plants to adapt to their new conditions.
Etiolation in plant life is typical and somewhat expected. What you are trying to avoid is a condition in which the plant is desperately leaning or reaching for a light source.
A plant grown in optimal light conditions will appear healthy and unstressed. Succulents and cacti are more inclined to flower when kept in optimal light conditions. However, depending on the species, they have differing ages at which they will bloom.
Succulent and Cactus Pest Control
While succulents and cacti are vigorous plants, they do have their pest problems. The following are common pest problems and their treatments:
Spider Mites – These pests can be found in their white webs spun close to the plant’s surface. Spider mites feed on plant sap and cause the plant to develop yellow spots which eventually turn brown.
Treat spider mite infections with a miticide, insecticidal soap, or horticultural oil like neem oil. Insecticides will have little effect as spider mites are not insects.
Mealybugs – These pests appear encapsulated in an oval-shaped cottony covering. Mealy bugs also feed on plant sap and will cause a plant to stop growing, weaken, and eventually die from rot.
For mealybug infestation control, spraying the plant with alcohol or dabbing their cottony covering with an alcohol-dipped cotton swab will dissolve the covering, leaving the insect defenseless to insecticides, neem oil, or a food-grade version of diatomaceous earth. Releasing ladybugs onto your plants can also be a very effective means of control.
Scale – These insects appear as tiny brownish spots on stems and foliage which also feed on sap. Scale infestations can weaken a plant’s health, leaving it susceptible to other insects and diseases.
Scale infestations should be treated in the same way as a mealybug infestation.
Growing Healthy Succulents and Cacti
Your succulents and cacti need your attention and have specific care requirements. Putting them in a well-lit spot is just the beginning of the care they need.
In this article, you discovered succulent and cactus species information, and growing tips to keep your plants in an optimal growth setting.
Merely putting your succulents or cacti somewhere bright and occasionally watering them will ultimately lead to their death. Proper care and treatment are required for them to thrive.
For the succulent and cactus enthusiast, you can join the Cactus and Succulent Society of America at cactusandsucculentsociety.org/ for books, DVDs, news, and journals on the various species and topics concerning succulents and cacti.
Sources: http://cactusandsucculentsociety.org/ https://web.extension.illinois.edu/cfiv/homeowners/170119.html https://www.washington-dc.cactus-society.org/Potting_soils.html
The post How to Care for Cactus and Succulent Plants appeared first on http://gardeninginfo-online.com.
1 note
·
View note
Text
Can Chronic Stress Cause Hypothyroid Symptoms?
Are you one of the 20 million Americans who has thyroid disease? (1) Have you taken proactive steps to improve your thyroid health, such as cleaning up your diet and supplementing with thyroid-supportive nutrients, but with little to no improvement? If this sounds like you, you may be missing a big piece of the thyroid puzzle—chronic stress.
But how does chronic stress cause hypothyroid symptoms? And, if your day-to-day experience is consistently stressful, how can you correct it? Read on to learn more about the stress–thyroid connection and get 12 tips on reducing stress in your daily life.
Long-term stress can have a profound impact on your thyroid gland. Check out this article to learn how chronic stress causes hypothyroidism and what you can do to fix it. #healthylifestyle #wellness #chriskresser
What Is “Adrenal Fatigue” and Is It Real?
Chronic stress has become epidemic in our society. Many people live by the motto “the busier, the better,” adding an ever-increasing number of obligations to their already jam-packed schedules.
Unfortunately, our high-paced lifestyles are not without health repercussions. Sixty to 80 percent of office visits to primary care providers may be stress related, according to statistics. (2) Healthcare practitioners working in the integrative and Functional Medicine communities also see their fair share of patients with stress-related illnesses; for years they’ve used the term “adrenal fatigue” to describe the stress-related health problems observed in these individuals.
The adrenal fatigue hypothesis asserts that chronic stress causes the adrenal glands, which are one component of the body’s stress-management system, to weaken over time. This “weakening” then causes a range of nonspecific symptoms, including:
Fatigue
Insomnia
Brain fog
Joint pain
Allergies
Weight gain
The theory of adrenal fatigue may be popular, but does it hold up to scientific scrutiny? Surprisingly, the answer appears to be a resounding “no.”
When we dig into the science and the studies that back it up, it becomes clear that so-called adrenal fatigue is an oversimplification of the body’s stress response. And while there are some cases in which a person’s adrenal glands are functionally compromised, these situations are rare.
There are three main problems with the adrenal fatigue hypothesis:
Those who subscribe to this theory maintain that the major stress hormone cortisol rises in the early stages of the disorder and decreases in the later stages, depleting as the adrenal glands become “fatigued.” However, many people with stress-related pathology have normal or high cortisol, rather than the low cortisol purported to occur in adrenal fatigue.
They also argue that abnormal cortisol production is the fault of the adrenal glands. However, the adrenals aren’t the primary controllers of cortisol production—the central nervous system is. In stress-related illness, the problem lies in the brain, not the adrenal glands.
The scientific literature does not support the concept of adrenal fatigue. A systematic review of the literature, published in 2016, found no evidence to support it. (3)
If it can’t properly be called adrenal fatigue, then what is it?
A more accurate term that is increasingly used by integrative and functional health practitioners to describe stress-related illness is hypothalamic–pituitary–adrenal (HPA) axis dysfunction.
Unlike adrenal fatigue, HPA axis dysfunction is biologically plausible, well studied, and associated with numerous health problems, including: (4, 5, 6, 7, 8)
Cardiovascular disease
Neurodegenerative disease
Chronic fatigue syndrome
Schizophrenia
Depression
Infertility
If Adrenal Fatigue Isn’t to Blame, What’s Really Happening?
The HPA axis is the body’s central stress response system, formed by an intertwining of the central nervous system and endocrine system. It orchestrates the response of the body and brain to cues from the environment, including positive and negative stressors. The three primary structures that comprise the HPA axis are the hypothalamus and pituitary gland, located in the brain, and the adrenal glands, which sit atop the kidneys.
When the body experiences stress, the following four-step response is normally produced by the HPA axis.
Step 1: In response to a stressor, the hypothalamus releases a hormone called corticotropin-releasing factor (CRF).
Step 2: CRF travels from the hypothalamus to the pituitary gland, where it binds to CRF receptors. This stimulates the pituitary to release adrenocorticotropic hormone (ACTH).
Step 3: ACTH travels in the bloodstream to the adrenal glands, where it promotes the adrenal release of cortisol in the right quantities to protect the body from stress.
Step 4: When the stress response lasts long enough to cause cortisol to reach a certain concentration in the blood, negative feedback is relayed to the hypothalamus. This feedback tells the hypothalamus to stop releasing CRF, effectively halting the stress response.
What You Need to Know about HPA Axis Dysfunction
The stress response described above helps us manage short-term stressors. It evolved over millions of years in our hominid ancestors, enabling them to efficiently respond to short bursts of stress, such as being chased by a predator on the African savanna, and then return to an unstressed state once the stressor was removed. Unfortunately, many of us today live in a state of chronic (ongoing) stress, rather than acute (short-burst) stress.
Chronic stressors such as rush-hour traffic, work-related and financial stress, relationship challenges, gut dysbiosis, blood sugar dysregulation, and environmental toxins overwhelm our HPA axis, which was designed to deal with acute stressors. Long-term activation of the HPA axis reduces our metabolic reserve—the ability of our cells and organs to withstand repeated physiological changes.
Think of metabolic reserve like a rubber band. Stretching the rubber band every now and then doesn’t alter the rubber band very much. However, repeatedly stretching the band eventually causes it to lose elasticity and become permanently elongated. Similarly, short, intermittent bouts of stress are efficiently handled by cells and organs, while chronic stress causes harmful changes to our systems.
In a state of chronic stress, the body does everything it can to preserve metabolic reserve. As a result, one of two situations takes place in the HPA axis:
The negative feedback mechanism in the HPA axis is desensitized, leading to extended HPA axis activation. Think of this as the body’s attempt to continuously stay “on guard” for potential threats.
The negative feedback mechanism becomes overly sensitive and limits the stress response in an attempt to protect the body. In this case, the HPA axis can’t appropriately respond to stressors, leaving the body vulnerable to new threats such as pathogenic bacteria and toxins.
In both cases, these adaptations serve an important immediate purpose: to protect your body’s metabolic reserve. However, if chronic stress continues, metabolic reserve is eventually depleted. This changes cortisol output, increasing or decreasing it, or changing your diurnal cortisol rhythm. (Cortisol is a diurnal hormone, meaning that it’s not secreted uniformly throughout the day; normally it’s highest in the mornings and declines throughout the rest of the day and into the evening.) The production of other hormones and neurotransmitters, such as DHEA, melatonin, and epinephrine (aka adrenaline), is also impaired, which will impact multiple organ systems. HPA axis dysfunction is the term used to describe the physiological changes and associated symptoms that occur in response to chronic stress.
As you can see, stress-induced health problems are not simply the result of “weak” adrenal glands; instead, these issues are manifestations of stress-induced dysfunction that begins in the brain and ultimately affects the entire body. One of the most important organs affected by HPA axis dysfunction is the thyroid gland.
The HPA Axis–Thyroid Connection
Every cell in the body has receptors for thyroid hormone. Thyroid hormones regulate and impact all body systems. When the thyroid malfunctions, it takes the entire body down with it.
If you have thyroid problems, you’re not alone. An estimated 20 million Americans have some form of thyroid disease, and it’s likely that 60 percent of those with a thyroid condition are unaware of it. (9) Hypothyroidism, a form of thyroid disease associated with decreased function of the thyroid gland, causes a variety of symptoms:
Fatigue despite sleeping eight to 10 hours a night; needing naps during the day
Weight gain or inability to lose weight
Mood swings, anxiety, and depression
Brain fog, poor concentration, and poor memory
Constipation
Cold hands and feet
Hair loss
Dry or cracking skin
Neck swelling and a hoarse voice
With 121 million prescriptions written annually, the use of levothyroxine, a synthetic thyroid hormone medication, far outpaces statins and blood pressure medications in the United States. (10) Nonpharmaceutical interventions, such as diets and supplements, are also widely used by patients with hypothyroidism. Unfortunately, the reality is that these interventions will all fail unless people address the underlying causes of their thyroid health issues.
A crucial contributor to thyroid disease that tends to be overlooked by both thyroid disease patients and their doctors is chronic stress.
How Does Your Chronic Stress Cause Hypothyroid Symptoms?
The thyroid gland is intimately connected with the HPA axis. When chronic stress alters HPA axis activity, a cascade of effects ultimately disrupts thyroid function.
Stress Depresses HPA Axis Function
Chronic stress promotes the release of inflammatory cytokines, small proteins that interfere with the HPA axis and reduce hypothalamic and pituitary function. (11, 12) The hypothalamus and pituitary glands are responsible for making thyrotropin-releasing hormone (TRH) and thyroxine-stimulating hormone (TSH), respectively. In a healthy human body, TRH and TSH travel to the thyroid gland and stimulate it to produce the thyroid hormones triiodothyronine (T3) and thyroxine (T4). When the HPA axis is suppressed or slowed down due to stress, TRH and TSH levels decrease. This chain of events leads to lower circulating levels of T3 and T4 and promotes the development of hypothyroidism.
Stress Reduces Active Thyroid Hormone Levels
As I mentioned above, the thyroid gland produces two hormones, T3 and T4. The majority of hormone produced by the thyroid is inactive T4, which must be converted into active T3 in peripheral tissues and organs before binding to thyroid hormone receptors on cells. Stress initiates the release of inflammatory cytokines that inhibit the conversion of inactive T4 to active T3. This results in lower circulating levels of thyroid hormone. Given the fact that all body cells have thyroid hormone receptors, the reduction in active T3 has adverse health implications for many body systems. (13, 14, 15)
Stress Promotes Thyroid Autoimmunity
Chronic stress was first identified as a risk factor for autoimmune disease over 50 years ago by Dr. Hans Selye, a pioneering endocrinologist who dedicated much of his career to studying the stress response. (16) We now understand that stress-induced HPA axis dysfunction changes levels of certain hormones that regulate immunity. These hormones alter cytokine production, which, in turn, can trigger immune dysregulation and autoimmune disease. (17, 18, 19) While scientific evidence demonstrating a direct relationship between stress and autoimmune hypothyroidism is lacking, several studies have identified stress as a factor in the development of Graves’ disease (autoimmune hyperthyroidism) and rheumatoid arthritis. (20, 21)
Given this evidence, it’s likely that stress also plays a significant role in the development of autoimmune hypothyroidism, also known as Hashimoto’s disease.
Stress Causes Thyroid Hormone Resistance
Thyroid hormone receptors control the process of transcription, the first step of gene expression, in which DNA is copied to make RNA. The central role of thyroid receptors in gene expression means that thyroid hormones have effects on all cells of the body. Inflammatory cytokines produced by chronic stress suppress the sensitivity of thyroid hormone receptors to thyroid hormones. (22) Reduced binding of thyroid hormone to its receptors prevents thyroid hormone from performing its crucial gene expression-regulating functions. This means that stress can impair the function of all cells of the body!
Stress Causes Imbalances in Other Hormones
Chronic stress doesn’t just reduce thyroid hormone levels; it also alters levels of other hormones that indirectly influence thyroid function, such as estrogen. It goes something like this: Prolonged cortisol release due to chronic HPA axis activation decreases the liver’s ability to process estrogen. Estrogen increases levels of thyroxine-binding globulin (TBG), a protein that binds thyroid hormones in circulation and inactivates them. High estrogen caused by chronic stress can cause hypothyroidism by reducing circulating levels of free, active thyroid hormone. (23)
These mechanisms indicate that chronic stress can cause hypothyroidism without any problem in the thyroid gland itself. Given the influence of stress on thyroid function, stress-reduction strategies should be a central part of any protocol designed to improve thyroid health.
12 Ways to Reduce Stress and Improve Your Thyroid Function
The implications of stress for thyroid health, and the health of the entire body, can’t be ignored. Thyroid-damaging stress can come in the form of physical, mental, and emotional stressors. Proactively addressing these stressors reduces the burden on the HPA axis and may improve your thyroid health.
1. Balance Your Blood Sugar
As I mentioned earlier, physical stressors activate the stress response and the HPA axis. Blood sugar dysregulation is a significant physical stressor that disrupts HPA axis function. Diabetes has been found to impair the HPA axis response to hypoglycemia, while insulin treatment to reduce blood sugar levels normalizes it. (24) By dampening HPA axis activity and normalizing the stress-related pathways that cause hypothyroidism, improved blood sugar regulation may boost thyroid function. For more information on the relationship between thyroid function and blood sugar, read my article “Thyroid, Blood Sugar, and Metabolic Syndrome.”
2. Heal Your Gut
Gut dysbiosis is another physical stressor that takes a significant toll on the HPA axis and thyroid function. Research has found that germ-free mice, which lack balanced gut microbiota, demonstrate increased HPA axis activity; this finding suggests that an abnormal gut microbiota activates the body’s stress response. (25) The gut–brain axis is linked to the HPA axis through certain neural pathways. Elevated levels of inflammatory cytokines and bacterial lipopolysaccharides in the gut, characteristic of gut dysbiosis, activate the HPA axis and raise cortisol. (26) In addition, multiple studies have linked gut dysbiosis to autoimmune hypothyroidism. (27)
Given the research, it’s reasonable to assume that gut dysbiosis may be a significant stressor underlying hypothyroidism. Correcting gut dysbiosis with antimicrobials, dietary modifications, and probiotics may help reduce the stress response. Probiotic strains that reduce HPA axis activity, as indicated by lowered cortisol and ACTH, include Lactobacillus plantarum, L. helveticus, L. fermentum, L. rhamnosus, and L. casei. (28)
3. Identify Your Food Intolerances
Anything that triggers inflammation in your gut is seen by your body as a physical stressor. Food intolerances are no exception. For example, non-celiac gluten sensitivity (NCGS) has been found to trigger inflammation of the central nervous system and cause gut–brain axis dysfunction. (29) The interconnection between the gut–brain axis and HPA axis suggest that NCGS, and potentially other food intolerances, may represent a form of chronic stress to the body. In the case of NCGS, avoiding gluten may reduce your body’s stress response and normalize your HPA axis activity.
4. If You’re Suffering from a Chronic Infection, Treat It
Chronic infections, such as Epstein-Barr virus and Lyme disease, cause the body to produce large amounts of inflammatory cytokines, which impact the HPA axis. (30) Resolving chronic infections reduces inflammation and can help normalize your HPA axis activity.
5. Avoid Environmental Toxins
Certain environmental toxins can disrupt the HPA axis and set off the stress response. In animal studies, bisphenol A (BPA) can cause hyperactivity of the HPA axis, resulting in anxiety and depression. (31) Lead, a heavy metal and a known neurotoxin, also induces HPA axis dysfunction. (32) Reduce your exposure to these and other environmental toxins by filtering your drinking and bathing water with a high-quality water filter and by using glass or stainless steel storage dishes and water bottles, rather than plastic.
6. Fix Your Sleep Cycle
Circadian rhythm disruption is a grossly overlooked but significant source of chronic stress that we all face in the industrialized world. Circadian rhythms are the set of biochemical processes in our bodies that follow an approximately 24-hour cycle and regulate many aspects of our behavior and physiology. Signals from our external environment such as light exposure, temperature fluctuations, and food intake sync our circadian rhythms. When we receive signals at inappropriate times during a 24-hour cycle, our circadian rhythms are disrupted and the physiological processes governed by those rhythms suffer. The HPA axis is one of the physiological systems impaired by circadian rhythm disruption. (33, 34)
Minimizing disruptions to your sleep cycle is crucial for normalizing HPA axis function and may improve thyroid health. To optimize your circadian rhythm, avoid blue light exposure at night by wearing blue light-blocking glasses. Banish all blue light-emitting devices from your bedroom, as even these seemingly benign light sources disrupt circadian rhythms. You may also want to stop eating at least three hours before bed because late-night eating enhances the stress response and induces circadian disruption. (35)
7. Take Sleep Seriously
Sleep deprivation is a significant source of stress for many people and has been associated with abnormal thyroid function. (36, 37) To reduce your stress and optimize the function of your HPA axis and thyroid, aim for seven to eight hours of sleep each night. The quality of your sleep is just as important as the quantity. Keep your bedroom completely dark and free of light pollution from street lamps, digital alarm clocks, and other electronic devices. If you struggle with disordered breathing issues, such as obstructive sleep apnea, I recommend you seek corrective help. Obstructive sleep apnea is associated with HPA axis dysfunction and a slew of other health problems, including subclinical hypothyroidism. (38) That’s where your TSH may be high, but your levels of other thyroid hormones are within a normal range.
8. Exercise, but Not Too Much
Exercise is essential for optimal health. However, over-exercising is not healthy; in fact, it activates the body’s stress response and causes serious damage both over the short and long term. The amount of exercise that a person can handle without going too far depends on the individual. For guidelines on how to avoid over-exercising while still enjoying yourself and getting benefits from physical activity, check out my podcast “Exercise and ‘Adrenal Fatigue’.”
9. Try Adaptogenic Herbs
Adaptogens are plants that help the body adapt to stress, protecting it through various mechanisms:
Adaptogens induce the production of proteins that protect the cells when the body is under stress (39)
Adaptogens increase neuropeptide Y, a stress-responsive hormone that stops the HPA axis from overactivating (40)
Adaptogens modulate stress-induced gene expression (41, 42)
Ashwagandha, a popular adaptogen that has a long history of use in Ayurvedic medicine, has stress-reducing effects and has been found to improve thyroid function in those with subclinical hypothyroidism. (43) Rhodiola rosea, an adaptogen native to Siberia, increases neuropeptide Y and reduces the hypothalamic expression of the stress-related gene c-Fos. (44, 45) These adaptogens may be beneficial additions to protocols designed to normalize HPA axis activity and improve thyroid function.
10. Think about Your Stressful Experiences Differently
While all of us face stress in our daily lives, we can influence how we respond to stressors by changing how we perceive them. In psychology, this strategy is known as “reframing.” Reframing gives us some control over how we respond to stressful events in life and can thereby reduce our stress levels and HPA axis activity. You can read more about reframing, and how to incorporate it into your life, in my article “5 Simple (But Powerful) Tools for Fighting Stress.”
11. Start a Mindfulness Practice
While stress initiates the release of thyroid-damaging inflammatory cytokines, stress-reduction practices decrease these cytokines and may improve thyroid function. (46, 47) In a group of 80 healthy women, consistent mind–body training (MBT) decreased TNF-alpha and IL-6, two inflammatory cytokines that have been associated with impaired thyroid function. (48, 49) Mind– body training refers to a practice that incorporates rhythmic movements with deep breathing exercises and meditation. Yoga is another mindfulness practice that may improve thyroid function by reducing stress. A small study found that six months of yoga practice decreased TSH, an effect associated with increased thyroid function. (50) Mindfulness practices also tend to have antidepressant effects. Antidepressants have been found to directly improve thyroid function in rats. (51) Other stress-reducing, mood-boosting strategies that don’t involve antidepressants may also help hypothyroidism.
12. Make Play a Part of Your Life
Play is a powerful tool for reducing stress and enhancing resilience. (52) While play can take countless forms, it has one defining factor: it’s an activity you engage in for enjoyment or recreation. Here are just a few examples:
Roughhousing with pets or children
Playing make-believe
Playing organized sports such as soccer, baseball, or basketball
Engaging in other forms of physical activity such as rock climbing, skiing, surfing, or ultimate Frisbee
Playing board games
Dancing
Going outside and walking in nature
Engaging in creative expression such as making art, music, gardening, or cooking a meal
Performing creative, innovative work (yes, work can be play!)
Engaging in playful banter at your job or a party
Having a playful relationship with your partner or spouse
Set aside time in your schedule for play, just as you would for other commitments such as work and exercise. I think you’ll find this to be one of the most enjoyable stress-reduction strategies listed here! You can read more about the benefits of play in my article “10 Benefits of Play.”
If you struggle with hypothyroidism and have tried medications, dietary changes, or supplements with minimal results, it may be time to consider the influence of chronic stress in your life. By taking proactive steps to reduce physical, mental, and emotional stress, you can set your body on the path toward optimal thyroid health.
Now I’d like to hear from you. Do you have questions about how chronic stress causes hypothyroid symptoms? Have you tried any of the stress-reduction strategies outlined in this article? Let me know in the comments below!
The post Can Chronic Stress Cause Hypothyroid Symptoms? appeared first on Chris Kresser.
Source: http://chriskresser.com November 29, 2018 at 03:38PM
8 notes
·
View notes
Text
Can Chronic Stress Cause Hypothyroid Symptoms?
Are you one of the 20 million Americans who has thyroid disease? (1) Have you taken proactive steps to improve your thyroid health, such as cleaning up your diet and supplementing with thyroid-supportive nutrients, but with little to no improvement? If this sounds like you, you may be missing a big piece of the thyroid puzzle—chronic stress.
But how does chronic stress cause hypothyroid symptoms? And, if your day-to-day experience is consistently stressful, how can you correct it? Read on to learn more about the stress–thyroid connection and get 12 tips on reducing stress in your daily life.
Long-term stress can have a profound impact on your thyroid gland. Check out this article to learn how chronic stress causes hypothyroidism and what you can do to fix it. #healthylifestyle #wellness #chriskresser
What Is “Adrenal Fatigue” and Is It Real?
Chronic stress has become epidemic in our society. Many people live by the motto “the busier, the better,” adding an ever-increasing number of obligations to their already jam-packed schedules.
Unfortunately, our high-paced lifestyles are not without health repercussions. Sixty to 80 percent of office visits to primary care providers may be stress related, according to statistics. (2) Healthcare practitioners working in the integrative and Functional Medicine communities also see their fair share of patients with stress-related illnesses; for years they’ve used the term “adrenal fatigue” to describe the stress-related health problems observed in these individuals.
The adrenal fatigue hypothesis asserts that chronic stress causes the adrenal glands, which are one component of the body’s stress-management system, to weaken over time. This “weakening” then causes a range of nonspecific symptoms, including:
Fatigue
Insomnia
Brain fog
Joint pain
Allergies
Weight gain
The theory of adrenal fatigue may be popular, but does it hold up to scientific scrutiny? Surprisingly, the answer appears to be a resounding “no.”
When we dig into the science and the studies that back it up, it becomes clear that so-called adrenal fatigue is an oversimplification of the body’s stress response. And while there are some cases in which a person’s adrenal glands are functionally compromised, these situations are rare.
There are three main problems with the adrenal fatigue hypothesis:
Those who subscribe to this theory maintain that the major stress hormone cortisol rises in the early stages of the disorder and decreases in the later stages, depleting as the adrenal glands become “fatigued.” However, many people with stress-related pathology have normal or high cortisol, rather than the low cortisol purported to occur in adrenal fatigue.
They also argue that abnormal cortisol production is the fault of the adrenal glands. However, the adrenals aren’t the primary controllers of cortisol production—the central nervous system is. In stress-related illness, the problem lies in the brain, not the adrenal glands.
The scientific literature does not support the concept of adrenal fatigue. A systematic review of the literature, published in 2016, found no evidence to support it. (3)
If it can’t properly be called adrenal fatigue, then what is it?
A more accurate term that is increasingly used by integrative and functional health practitioners to describe stress-related illness is hypothalamic–pituitary–adrenal (HPA) axis dysfunction.
Unlike adrenal fatigue, HPA axis dysfunction is biologically plausible, well studied, and associated with numerous health problems, including: (4, 5, 6, 7, 8)
Cardiovascular disease
Neurodegenerative disease
Chronic fatigue syndrome
Schizophrenia
Depression
Infertility
If Adrenal Fatigue Isn’t to Blame, What’s Really Happening?
The HPA axis is the body’s central stress response system, formed by an intertwining of the central nervous system and endocrine system. It orchestrates the response of the body and brain to cues from the environment, including positive and negative stressors. The three primary structures that comprise the HPA axis are the hypothalamus and pituitary gland, located in the brain, and the adrenal glands, which sit atop the kidneys.
When the body experiences stress, the following four-step response is normally produced by the HPA axis.
Step 1: In response to a stressor, the hypothalamus releases a hormone called corticotropin-releasing factor (CRF).
Step 2: CRF travels from the hypothalamus to the pituitary gland, where it binds to CRF receptors. This stimulates the pituitary to release adrenocorticotropic hormone (ACTH).
Step 3: ACTH travels in the bloodstream to the adrenal glands, where it promotes the adrenal release of cortisol in the right quantities to protect the body from stress.
Step 4: When the stress response lasts long enough to cause cortisol to reach a certain concentration in the blood, negative feedback is relayed to the hypothalamus. This feedback tells the hypothalamus to stop releasing CRF, effectively halting the stress response.
What You Need to Know about HPA Axis Dysfunction
The stress response described above helps us manage short-term stressors. It evolved over millions of years in our hominid ancestors, enabling them to efficiently respond to short bursts of stress, such as being chased by a predator on the African savanna, and then return to an unstressed state once the stressor was removed. Unfortunately, many of us today live in a state of chronic (ongoing) stress, rather than acute (short-burst) stress.
Chronic stressors such as rush-hour traffic, work-related and financial stress, relationship challenges, gut dysbiosis, blood sugar dysregulation, and environmental toxins overwhelm our HPA axis, which was designed to deal with acute stressors. Long-term activation of the HPA axis reduces our metabolic reserve—the ability of our cells and organs to withstand repeated physiological changes.
Think of metabolic reserve like a rubber band. Stretching the rubber band every now and then doesn’t alter the rubber band very much. However, repeatedly stretching the band eventually causes it to lose elasticity and become permanently elongated. Similarly, short, intermittent bouts of stress are efficiently handled by cells and organs, while chronic stress causes harmful changes to our systems.
In a state of chronic stress, the body does everything it can to preserve metabolic reserve. As a result, one of two situations takes place in the HPA axis:
The negative feedback mechanism in the HPA axis is desensitized, leading to extended HPA axis activation. Think of this as the body’s attempt to continuously stay “on guard” for potential threats.
The negative feedback mechanism becomes overly sensitive and limits the stress response in an attempt to protect the body. In this case, the HPA axis can’t appropriately respond to stressors, leaving the body vulnerable to new threats such as pathogenic bacteria and toxins.
In both cases, these adaptations serve an important immediate purpose: to protect your body’s metabolic reserve. However, if chronic stress continues, metabolic reserve is eventually depleted. This changes cortisol output, increasing or decreasing it, or changing your diurnal cortisol rhythm. (Cortisol is a diurnal hormone, meaning that it’s not secreted uniformly throughout the day; normally it’s highest in the mornings and declines throughout the rest of the day and into the evening.) The production of other hormones and neurotransmitters, such as DHEA, melatonin, and epinephrine (aka adrenaline), is also impaired, which will impact multiple organ systems. HPA axis dysfunction is the term used to describe the physiological changes and associated symptoms that occur in response to chronic stress.
As you can see, stress-induced health problems are not simply the result of “weak” adrenal glands; instead, these issues are manifestations of stress-induced dysfunction that begins in the brain and ultimately affects the entire body. One of the most important organs affected by HPA axis dysfunction is the thyroid gland.
The HPA Axis–Thyroid Connection
Every cell in the body has receptors for thyroid hormone. Thyroid hormones regulate and impact all body systems. When the thyroid malfunctions, it takes the entire body down with it.
If you have thyroid problems, you’re not alone. An estimated 20 million Americans have some form of thyroid disease, and it’s likely that 60 percent of those with a thyroid condition are unaware of it. (9) Hypothyroidism, a form of thyroid disease associated with decreased function of the thyroid gland, causes a variety of symptoms:
Fatigue despite sleeping eight to 10 hours a night; needing naps during the day
Weight gain or inability to lose weight
Mood swings, anxiety, and depression
Brain fog, poor concentration, and poor memory
Constipation
Cold hands and feet
Hair loss
Dry or cracking skin
Neck swelling and a hoarse voice
With 121 million prescriptions written annually, the use of levothyroxine, a synthetic thyroid hormone medication, far outpaces statins and blood pressure medications in the United States. (10) Nonpharmaceutical interventions, such as diets and supplements, are also widely used by patients with hypothyroidism. Unfortunately, the reality is that these interventions will all fail unless people address the underlying causes of their thyroid health issues.
A crucial contributor to thyroid disease that tends to be overlooked by both thyroid disease patients and their doctors is chronic stress.
How Does Your Chronic Stress Cause Hypothyroid Symptoms?
The thyroid gland is intimately connected with the HPA axis. When chronic stress alters HPA axis activity, a cascade of effects ultimately disrupts thyroid function.
Stress Depresses HPA Axis Function
Chronic stress promotes the release of inflammatory cytokines, small proteins that interfere with the HPA axis and reduce hypothalamic and pituitary function. (11, 12) The hypothalamus and pituitary glands are responsible for making thyrotropin-releasing hormone (TRH) and thyroxine-stimulating hormone (TSH), respectively. In a healthy human body, TRH and TSH travel to the thyroid gland and stimulate it to produce the thyroid hormones triiodothyronine (T3) and thyroxine (T4). When the HPA axis is suppressed or slowed down due to stress, TRH and TSH levels decrease. This chain of events leads to lower circulating levels of T3 and T4 and promotes the development of hypothyroidism.
Stress Reduces Active Thyroid Hormone Levels
As I mentioned above, the thyroid gland produces two hormones, T3 and T4. The majority of hormone produced by the thyroid is inactive T4, which must be converted into active T3 in peripheral tissues and organs before binding to thyroid hormone receptors on cells. Stress initiates the release of inflammatory cytokines that inhibit the conversion of inactive T4 to active T3. This results in lower circulating levels of thyroid hormone. Given the fact that all body cells have thyroid hormone receptors, the reduction in active T3 has adverse health implications for many body systems. (13, 14, 15)
Stress Promotes Thyroid Autoimmunity
Chronic stress was first identified as a risk factor for autoimmune disease over 50 years ago by Dr. Hans Selye, a pioneering endocrinologist who dedicated much of his career to studying the stress response. (16) We now understand that stress-induced HPA axis dysfunction changes levels of certain hormones that regulate immunity. These hormones alter cytokine production, which, in turn, can trigger immune dysregulation and autoimmune disease. (17, 18, 19) While scientific evidence demonstrating a direct relationship between stress and autoimmune hypothyroidism is lacking, several studies have identified stress as a factor in the development of Graves’ disease (autoimmune hyperthyroidism) and rheumatoid arthritis. (20, 21)
Given this evidence, it’s likely that stress also plays a significant role in the development of autoimmune hypothyroidism, also known as Hashimoto’s disease.
Stress Causes Thyroid Hormone Resistance
Thyroid hormone receptors control the process of transcription, the first step of gene expression, in which DNA is copied to make RNA. The central role of thyroid receptors in gene expression means that thyroid hormones have effects on all cells of the body. Inflammatory cytokines produced by chronic stress suppress the sensitivity of thyroid hormone receptors to thyroid hormones. (22) Reduced binding of thyroid hormone to its receptors prevents thyroid hormone from performing its crucial gene expression-regulating functions. This means that stress can impair the function of all cells of the body!
Stress Causes Imbalances in Other Hormones
Chronic stress doesn’t just reduce thyroid hormone levels; it also alters levels of other hormones that indirectly influence thyroid function, such as estrogen. It goes something like this: Prolonged cortisol release due to chronic HPA axis activation decreases the liver’s ability to process estrogen. Estrogen increases levels of thyroxine-binding globulin (TBG), a protein that binds thyroid hormones in circulation and inactivates them. High estrogen caused by chronic stress can cause hypothyroidism by reducing circulating levels of free, active thyroid hormone. (23)
These mechanisms indicate that chronic stress can cause hypothyroidism without any problem in the thyroid gland itself. Given the influence of stress on thyroid function, stress-reduction strategies should be a central part of any protocol designed to improve thyroid health.
12 Ways to Reduce Stress and Improve Your Thyroid Function
The implications of stress for thyroid health, and the health of the entire body, can’t be ignored. Thyroid-damaging stress can come in the form of physical, mental, and emotional stressors. Proactively addressing these stressors reduces the burden on the HPA axis and may improve your thyroid health.
1. Balance Your Blood Sugar
As I mentioned earlier, physical stressors activate the stress response and the HPA axis. Blood sugar dysregulation is a significant physical stressor that disrupts HPA axis function. Diabetes has been found to impair the HPA axis response to hypoglycemia, while insulin treatment to reduce blood sugar levels normalizes it. (24) By dampening HPA axis activity and normalizing the stress-related pathways that cause hypothyroidism, improved blood sugar regulation may boost thyroid function. For more information on the relationship between thyroid function and blood sugar, read my article “Thyroid, Blood Sugar, and Metabolic Syndrome.”
2. Heal Your Gut
Gut dysbiosis is another physical stressor that takes a significant toll on the HPA axis and thyroid function. Research has found that germ-free mice, which lack balanced gut microbiota, demonstrate increased HPA axis activity; this finding suggests that an abnormal gut microbiota activates the body’s stress response. (25) The gut–brain axis is linked to the HPA axis through certain neural pathways. Elevated levels of inflammatory cytokines and bacterial lipopolysaccharides in the gut, characteristic of gut dysbiosis, activate the HPA axis and raise cortisol. (26) In addition, multiple studies have linked gut dysbiosis to autoimmune hypothyroidism. (27)
Given the research, it’s reasonable to assume that gut dysbiosis may be a significant stressor underlying hypothyroidism. Correcting gut dysbiosis with antimicrobials, dietary modifications, and probiotics may help reduce the stress response. Probiotic strains that reduce HPA axis activity, as indicated by lowered cortisol and ACTH, include Lactobacillus plantarum, L. helveticus, L. fermentum, L. rhamnosus, and L. casei. (28)
3. Identify Your Food Intolerances
Anything that triggers inflammation in your gut is seen by your body as a physical stressor. Food intolerances are no exception. For example, non-celiac gluten sensitivity (NCGS) has been found to trigger inflammation of the central nervous system and cause gut–brain axis dysfunction. (29) The interconnection between the gut–brain axis and HPA axis suggest that NCGS, and potentially other food intolerances, may represent a form of chronic stress to the body. In the case of NCGS, avoiding gluten may reduce your body’s stress response and normalize your HPA axis activity.
4. If You’re Suffering from a Chronic Infection, Treat It
Chronic infections, such as Epstein-Barr virus and Lyme disease, cause the body to produce large amounts of inflammatory cytokines, which impact the HPA axis. (30) Resolving chronic infections reduces inflammation and can help normalize your HPA axis activity.
5. Avoid Environmental Toxins
Certain environmental toxins can disrupt the HPA axis and set off the stress response. In animal studies, bisphenol A (BPA) can cause hyperactivity of the HPA axis, resulting in anxiety and depression. (31) Lead, a heavy metal and a known neurotoxin, also induces HPA axis dysfunction. (32) Reduce your exposure to these and other environmental toxins by filtering your drinking and bathing water with a high-quality water filter and by using glass or stainless steel storage dishes and water bottles, rather than plastic.
6. Fix Your Sleep Cycle
Circadian rhythm disruption is a grossly overlooked but significant source of chronic stress that we all face in the industrialized world. Circadian rhythms are the set of biochemical processes in our bodies that follow an approximately 24-hour cycle and regulate many aspects of our behavior and physiology. Signals from our external environment such as light exposure, temperature fluctuations, and food intake sync our circadian rhythms. When we receive signals at inappropriate times during a 24-hour cycle, our circadian rhythms are disrupted and the physiological processes governed by those rhythms suffer. The HPA axis is one of the physiological systems impaired by circadian rhythm disruption. (33, 34)
Minimizing disruptions to your sleep cycle is crucial for normalizing HPA axis function and may improve thyroid health. To optimize your circadian rhythm, avoid blue light exposure at night by wearing blue light-blocking glasses. Banish all blue light-emitting devices from your bedroom, as even these seemingly benign light sources disrupt circadian rhythms. You may also want to stop eating at least three hours before bed because late-night eating enhances the stress response and induces circadian disruption. (35)
7. Take Sleep Seriously
Sleep deprivation is a significant source of stress for many people and has been associated with abnormal thyroid function. (36, 37) To reduce your stress and optimize the function of your HPA axis and thyroid, aim for seven to eight hours of sleep each night. The quality of your sleep is just as important as the quantity. Keep your bedroom completely dark and free of light pollution from street lamps, digital alarm clocks, and other electronic devices. If you struggle with disordered breathing issues, such as obstructive sleep apnea, I recommend you seek corrective help. Obstructive sleep apnea is associated with HPA axis dysfunction and a slew of other health problems, including subclinical hypothyroidism. (38) That’s where your TSH may be high, but your levels of other thyroid hormones are within a normal range.
8. Exercise, but Not Too Much
Exercise is essential for optimal health. However, over-exercising is not healthy; in fact, it activates the body’s stress response and causes serious damage both over the short and long term. The amount of exercise that a person can handle without going too far depends on the individual. For guidelines on how to avoid over-exercising while still enjoying yourself and getting benefits from physical activity, check out my podcast “Exercise and ‘Adrenal Fatigue’.”
9. Try Adaptogenic Herbs
Adaptogens are plants that help the body adapt to stress, protecting it through various mechanisms:
Adaptogens induce the production of proteins that protect the cells when the body is under stress (39)
Adaptogens increase neuropeptide Y, a stress-responsive hormone that stops the HPA axis from overactivating (40)
Adaptogens modulate stress-induced gene expression (41, 42)
Ashwagandha, a popular adaptogen that has a long history of use in Ayurvedic medicine, has stress-reducing effects and has been found to improve thyroid function in those with subclinical hypothyroidism. (43) Rhodiola rosea, an adaptogen native to Siberia, increases neuropeptide Y and reduces the hypothalamic expression of the stress-related gene c-Fos. (44, 45) These adaptogens may be beneficial additions to protocols designed to normalize HPA axis activity and improve thyroid function.
10. Think about Your Stressful Experiences Differently
While all of us face stress in our daily lives, we can influence how we respond to stressors by changing how we perceive them. In psychology, this strategy is known as “reframing.” Reframing gives us some control over how we respond to stressful events in life and can thereby reduce our stress levels and HPA axis activity. You can read more about reframing, and how to incorporate it into your life, in my article “5 Simple (But Powerful) Tools for Fighting Stress.”
11. Start a Mindfulness Practice
While stress initiates the release of thyroid-damaging inflammatory cytokines, stress-reduction practices decrease these cytokines and may improve thyroid function. (46, 47) In a group of 80 healthy women, consistent mind–body training (MBT) decreased TNF-alpha and IL-6, two inflammatory cytokines that have been associated with impaired thyroid function. (48, 49) Mind– body training refers to a practice that incorporates rhythmic movements with deep breathing exercises and meditation. Yoga is another mindfulness practice that may improve thyroid function by reducing stress. A small study found that six months of yoga practice decreased TSH, an effect associated with increased thyroid function. (50) Mindfulness practices also tend to have antidepressant effects. Antidepressants have been found to directly improve thyroid function in rats. (51) Other stress-reducing, mood-boosting strategies that don’t involve antidepressants may also help hypothyroidism.
12. Make Play a Part of Your Life
Play is a powerful tool for reducing stress and enhancing resilience. (52) While play can take countless forms, it has one defining factor: it’s an activity you engage in for enjoyment or recreation. Here are just a few examples:
Roughhousing with pets or children
Playing make-believe
Playing organized sports such as soccer, baseball, or basketball
Engaging in other forms of physical activity such as rock climbing, skiing, surfing, or ultimate Frisbee
Playing board games
Dancing
Going outside and walking in nature
Engaging in creative expression such as making art, music, gardening, or cooking a meal
Performing creative, innovative work (yes, work can be play!)
Engaging in playful banter at your job or a party
Having a playful relationship with your partner or spouse
Set aside time in your schedule for play, just as you would for other commitments such as work and exercise. I think you’ll find this to be one of the most enjoyable stress-reduction strategies listed here! You can read more about the benefits of play in my article “10 Benefits of Play.”
If you struggle with hypothyroidism and have tried medications, dietary changes, or supplements with minimal results, it may be time to consider the influence of chronic stress in your life. By taking proactive steps to reduce physical, mental, and emotional stress, you can set your body on the path toward optimal thyroid health.
Now I’d like to hear from you. Do you have questions about how chronic stress causes hypothyroid symptoms? Have you tried any of the stress-reduction strategies outlined in this article? Let me know in the comments below!
The post Can Chronic Stress Cause Hypothyroid Symptoms? appeared first on Chris Kresser.
Can Chronic Stress Cause Hypothyroid Symptoms? published first on https://brightendentalhouston.weebly.com/
0 notes
Text
Can Chronic Stress Cause Hypothyroid Symptoms?
Are you one of the 20 million Americans who has thyroid disease? (1) Have you taken proactive steps to improve your thyroid health, such as cleaning up your diet and supplementing with thyroid-supportive nutrients, but with little to no improvement? If this sounds like you, you may be missing a big piece of the thyroid puzzle—chronic stress.
But how does chronic stress cause hypothyroid symptoms? And, if your day-to-day experience is consistently stressful, how can you correct it? Read on to learn more about the stress–thyroid connection and get 12 tips on reducing stress in your daily life.
Long-term stress can have a profound impact on your thyroid gland. Check out this article to learn how chronic stress causes hypothyroidism and what you can do to fix it. #healthylifestyle #wellness #chriskresser
What Is “Adrenal Fatigue” and Is It Real?
Chronic stress has become epidemic in our society. Many people live by the motto “the busier, the better,” adding an ever-increasing number of obligations to their already jam-packed schedules.
Unfortunately, our high-paced lifestyles are not without health repercussions. Sixty to 80 percent of office visits to primary care providers may be stress related, according to statistics. (2) Healthcare practitioners working in the integrative and Functional Medicine communities also see their fair share of patients with stress-related illnesses; for years they’ve used the term “adrenal fatigue” to describe the stress-related health problems observed in these individuals.
The adrenal fatigue hypothesis asserts that chronic stress causes the adrenal glands, which are one component of the body’s stress-management system, to weaken over time. This “weakening” then causes a range of nonspecific symptoms, including:
Fatigue
Insomnia
Brain fog
Joint pain
Allergies
Weight gain
The theory of adrenal fatigue may be popular, but does it hold up to scientific scrutiny? Surprisingly, the answer appears to be a resounding “no.”
When we dig into the science and the studies that back it up, it becomes clear that so-called adrenal fatigue is an oversimplification of the body’s stress response. And while there are some cases in which a person’s adrenal glands are functionally compromised, these situations are rare.
There are three main problems with the adrenal fatigue hypothesis:
Those who subscribe to this theory maintain that the major stress hormone cortisol rises in the early stages of the disorder and decreases in the later stages, depleting as the adrenal glands become “fatigued.” However, many people with stress-related pathology have normal or high cortisol, rather than the low cortisol purported to occur in adrenal fatigue.
They also argue that abnormal cortisol production is the fault of the adrenal glands. However, the adrenals aren’t the primary controllers of cortisol production—the central nervous system is. In stress-related illness, the problem lies in the brain, not the adrenal glands.
The scientific literature does not support the concept of adrenal fatigue. A systematic review of the literature, published in 2016, found no evidence to support it. (3)
If it can’t properly be called adrenal fatigue, then what is it?
A more accurate term that is increasingly used by integrative and functional health practitioners to describe stress-related illness is hypothalamic–pituitary–adrenal (HPA) axis dysfunction.
Unlike adrenal fatigue, HPA axis dysfunction is biologically plausible, well studied, and associated with numerous health problems, including: (4, 5, 6, 7, 8)
Cardiovascular disease
Neurodegenerative disease
Chronic fatigue syndrome
Schizophrenia
Depression
Infertility
If Adrenal Fatigue Isn’t to Blame, What’s Really Happening?
The HPA axis is the body’s central stress response system, formed by an intertwining of the central nervous system and endocrine system. It orchestrates the response of the body and brain to cues from the environment, including positive and negative stressors. The three primary structures that comprise the HPA axis are the hypothalamus and pituitary gland, located in the brain, and the adrenal glands, which sit atop the kidneys.
When the body experiences stress, the following four-step response is normally produced by the HPA axis.
Step 1: In response to a stressor, the hypothalamus releases a hormone called corticotropin-releasing factor (CRF).
Step 2: CRF travels from the hypothalamus to the pituitary gland, where it binds to CRF receptors. This stimulates the pituitary to release adrenocorticotropic hormone (ACTH).
Step 3: ACTH travels in the bloodstream to the adrenal glands, where it promotes the adrenal release of cortisol in the right quantities to protect the body from stress.
Step 4: When the stress response lasts long enough to cause cortisol to reach a certain concentration in the blood, negative feedback is relayed to the hypothalamus. This feedback tells the hypothalamus to stop releasing CRF, effectively halting the stress response.
What You Need to Know about HPA Axis Dysfunction
The stress response described above helps us manage short-term stressors. It evolved over millions of years in our hominid ancestors, enabling them to efficiently respond to short bursts of stress, such as being chased by a predator on the African savanna, and then return to an unstressed state once the stressor was removed. Unfortunately, many of us today live in a state of chronic (ongoing) stress, rather than acute (short-burst) stress.
Chronic stressors such as rush-hour traffic, work-related and financial stress, relationship challenges, gut dysbiosis, blood sugar dysregulation, and environmental toxins overwhelm our HPA axis, which was designed to deal with acute stressors. Long-term activation of the HPA axis reduces our metabolic reserve—the ability of our cells and organs to withstand repeated physiological changes.
Think of metabolic reserve like a rubber band. Stretching the rubber band every now and then doesn’t alter the rubber band very much. However, repeatedly stretching the band eventually causes it to lose elasticity and become permanently elongated. Similarly, short, intermittent bouts of stress are efficiently handled by cells and organs, while chronic stress causes harmful changes to our systems.
In a state of chronic stress, the body does everything it can to preserve metabolic reserve. As a result, one of two situations takes place in the HPA axis:
The negative feedback mechanism in the HPA axis is desensitized, leading to extended HPA axis activation. Think of this as the body’s attempt to continuously stay “on guard” for potential threats.
The negative feedback mechanism becomes overly sensitive and limits the stress response in an attempt to protect the body. In this case, the HPA axis can’t appropriately respond to stressors, leaving the body vulnerable to new threats such as pathogenic bacteria and toxins.
In both cases, these adaptations serve an important immediate purpose: to protect your body’s metabolic reserve. However, if chronic stress continues, metabolic reserve is eventually depleted. This changes cortisol output, increasing or decreasing it, or changing your diurnal cortisol rhythm. (Cortisol is a diurnal hormone, meaning that it’s not secreted uniformly throughout the day; normally it’s highest in the mornings and declines throughout the rest of the day and into the evening.) The production of other hormones and neurotransmitters, such as DHEA, melatonin, and epinephrine (aka adrenaline), is also impaired, which will impact multiple organ systems. HPA axis dysfunction is the term used to describe the physiological changes and associated symptoms that occur in response to chronic stress.
As you can see, stress-induced health problems are not simply the result of “weak” adrenal glands; instead, these issues are manifestations of stress-induced dysfunction that begins in the brain and ultimately affects the entire body. One of the most important organs affected by HPA axis dysfunction is the thyroid gland.
The HPA Axis–Thyroid Connection
Every cell in the body has receptors for thyroid hormone. Thyroid hormones regulate and impact all body systems. When the thyroid malfunctions, it takes the entire body down with it.
If you have thyroid problems, you’re not alone. An estimated 20 million Americans have some form of thyroid disease, and it’s likely that 60 percent of those with a thyroid condition are unaware of it. (9) Hypothyroidism, a form of thyroid disease associated with decreased function of the thyroid gland, causes a variety of symptoms:
Fatigue despite sleeping eight to 10 hours a night; needing naps during the day
Weight gain or inability to lose weight
Mood swings, anxiety, and depression
Brain fog, poor concentration, and poor memory
Constipation
Cold hands and feet
Hair loss
Dry or cracking skin
Neck swelling and a hoarse voice
With 121 million prescriptions written annually, the use of levothyroxine, a synthetic thyroid hormone medication, far outpaces statins and blood pressure medications in the United States. (10) Nonpharmaceutical interventions, such as diets and supplements, are also widely used by patients with hypothyroidism. Unfortunately, the reality is that these interventions will all fail unless people address the underlying causes of their thyroid health issues.
A crucial contributor to thyroid disease that tends to be overlooked by both thyroid disease patients and their doctors is chronic stress.
How Does Your Chronic Stress Cause Hypothyroid Symptoms?
The thyroid gland is intimately connected with the HPA axis. When chronic stress alters HPA axis activity, a cascade of effects ultimately disrupts thyroid function.
Stress Depresses HPA Axis Function
Chronic stress promotes the release of inflammatory cytokines, small proteins that interfere with the HPA axis and reduce hypothalamic and pituitary function. (11, 12) The hypothalamus and pituitary glands are responsible for making thyrotropin-releasing hormone (TRH) and thyroxine-stimulating hormone (TSH), respectively. In a healthy human body, TRH and TSH travel to the thyroid gland and stimulate it to produce the thyroid hormones triiodothyronine (T3) and thyroxine (T4). When the HPA axis is suppressed or slowed down due to stress, TRH and TSH levels decrease. This chain of events leads to lower circulating levels of T3 and T4 and promotes the development of hypothyroidism.
Stress Reduces Active Thyroid Hormone Levels
As I mentioned above, the thyroid gland produces two hormones, T3 and T4. The majority of hormone produced by the thyroid is inactive T4, which must be converted into active T3 in peripheral tissues and organs before binding to thyroid hormone receptors on cells. Stress initiates the release of inflammatory cytokines that inhibit the conversion of inactive T4 to active T3. This results in lower circulating levels of thyroid hormone. Given the fact that all body cells have thyroid hormone receptors, the reduction in active T3 has adverse health implications for many body systems. (13, 14, 15)
Stress Promotes Thyroid Autoimmunity
Chronic stress was first identified as a risk factor for autoimmune disease over 50 years ago by Dr. Hans Selye, a pioneering endocrinologist who dedicated much of his career to studying the stress response. (16) We now understand that stress-induced HPA axis dysfunction changes levels of certain hormones that regulate immunity. These hormones alter cytokine production, which, in turn, can trigger immune dysregulation and autoimmune disease. (17, 18, 19) While scientific evidence demonstrating a direct relationship between stress and autoimmune hypothyroidism is lacking, several studies have identified stress as a factor in the development of Graves’ disease (autoimmune hyperthyroidism) and rheumatoid arthritis. (20, 21)
Given this evidence, it’s likely that stress also plays a significant role in the development of autoimmune hypothyroidism, also known as Hashimoto’s disease.
Stress Causes Thyroid Hormone Resistance
Thyroid hormone receptors control the process of transcription, the first step of gene expression, in which DNA is copied to make RNA. The central role of thyroid receptors in gene expression means that thyroid hormones have effects on all cells of the body. Inflammatory cytokines produced by chronic stress suppress the sensitivity of thyroid hormone receptors to thyroid hormones. (22) Reduced binding of thyroid hormone to its receptors prevents thyroid hormone from performing its crucial gene expression-regulating functions. This means that stress can impair the function of all cells of the body!
Stress Causes Imbalances in Other Hormones
Chronic stress doesn’t just reduce thyroid hormone levels; it also alters levels of other hormones that indirectly influence thyroid function, such as estrogen. It goes something like this: Prolonged cortisol release due to chronic HPA axis activation decreases the liver’s ability to process estrogen. Estrogen increases levels of thyroxine-binding globulin (TBG), a protein that binds thyroid hormones in circulation and inactivates them. High estrogen caused by chronic stress can cause hypothyroidism by reducing circulating levels of free, active thyroid hormone. (23)
These mechanisms indicate that chronic stress can cause hypothyroidism without any problem in the thyroid gland itself. Given the influence of stress on thyroid function, stress-reduction strategies should be a central part of any protocol designed to improve thyroid health.
12 Ways to Reduce Stress and Improve Your Thyroid Function
The implications of stress for thyroid health, and the health of the entire body, can’t be ignored. Thyroid-damaging stress can come in the form of physical, mental, and emotional stressors. Proactively addressing these stressors reduces the burden on the HPA axis and may improve your thyroid health.
1. Balance Your Blood Sugar
As I mentioned earlier, physical stressors activate the stress response and the HPA axis. Blood sugar dysregulation is a significant physical stressor that disrupts HPA axis function. Diabetes has been found to impair the HPA axis response to hypoglycemia, while insulin treatment to reduce blood sugar levels normalizes it. (24) By dampening HPA axis activity and normalizing the stress-related pathways that cause hypothyroidism, improved blood sugar regulation may boost thyroid function. For more information on the relationship between thyroid function and blood sugar, read my article “Thyroid, Blood Sugar, and Metabolic Syndrome.”
2. Heal Your Gut
Gut dysbiosis is another physical stressor that takes a significant toll on the HPA axis and thyroid function. Research has found that germ-free mice, which lack balanced gut microbiota, demonstrate increased HPA axis activity; this finding suggests that an abnormal gut microbiota activates the body’s stress response. (25) The gut–brain axis is linked to the HPA axis through certain neural pathways. Elevated levels of inflammatory cytokines and bacterial lipopolysaccharides in the gut, characteristic of gut dysbiosis, activate the HPA axis and raise cortisol. (26) In addition, multiple studies have linked gut dysbiosis to autoimmune hypothyroidism. (27)
Given the research, it’s reasonable to assume that gut dysbiosis may be a significant stressor underlying hypothyroidism. Correcting gut dysbiosis with antimicrobials, dietary modifications, and probiotics may help reduce the stress response. Probiotic strains that reduce HPA axis activity, as indicated by lowered cortisol and ACTH, include Lactobacillus plantarum, L. helveticus, L. fermentum, L. rhamnosus, and L. casei. (28)
3. Identify Your Food Intolerances
Anything that triggers inflammation in your gut is seen by your body as a physical stressor. Food intolerances are no exception. For example, non-celiac gluten sensitivity (NCGS) has been found to trigger inflammation of the central nervous system and cause gut–brain axis dysfunction. (29) The interconnection between the gut–brain axis and HPA axis suggest that NCGS, and potentially other food intolerances, may represent a form of chronic stress to the body. In the case of NCGS, avoiding gluten may reduce your body’s stress response and normalize your HPA axis activity.
4. If You’re Suffering from a Chronic Infection, Treat It
Chronic infections, such as Epstein-Barr virus and Lyme disease, cause the body to produce large amounts of inflammatory cytokines, which impact the HPA axis. (30) Resolving chronic infections reduces inflammation and can help normalize your HPA axis activity.
5. Avoid Environmental Toxins
Certain environmental toxins can disrupt the HPA axis and set off the stress response. In animal studies, bisphenol A (BPA) can cause hyperactivity of the HPA axis, resulting in anxiety and depression. (31) Lead, a heavy metal and a known neurotoxin, also induces HPA axis dysfunction. (32) Reduce your exposure to these and other environmental toxins by filtering your drinking and bathing water with a high-quality water filter and by using glass or stainless steel storage dishes and water bottles, rather than plastic.
6. Fix Your Sleep Cycle
Circadian rhythm disruption is a grossly overlooked but significant source of chronic stress that we all face in the industrialized world. Circadian rhythms are the set of biochemical processes in our bodies that follow an approximately 24-hour cycle and regulate many aspects of our behavior and physiology. Signals from our external environment such as light exposure, temperature fluctuations, and food intake sync our circadian rhythms. When we receive signals at inappropriate times during a 24-hour cycle, our circadian rhythms are disrupted and the physiological processes governed by those rhythms suffer. The HPA axis is one of the physiological systems impaired by circadian rhythm disruption. (33, 34)
Minimizing disruptions to your sleep cycle is crucial for normalizing HPA axis function and may improve thyroid health. To optimize your circadian rhythm, avoid blue light exposure at night by wearing blue light-blocking glasses. Banish all blue light-emitting devices from your bedroom, as even these seemingly benign light sources disrupt circadian rhythms. You may also want to stop eating at least three hours before bed because late-night eating enhances the stress response and induces circadian disruption. (35)
7. Take Sleep Seriously
Sleep deprivation is a significant source of stress for many people and has been associated with abnormal thyroid function. (36, 37) To reduce your stress and optimize the function of your HPA axis and thyroid, aim for seven to eight hours of sleep each night. The quality of your sleep is just as important as the quantity. Keep your bedroom completely dark and free of light pollution from street lamps, digital alarm clocks, and other electronic devices. If you struggle with disordered breathing issues, such as obstructive sleep apnea, I recommend you seek corrective help. Obstructive sleep apnea is associated with HPA axis dysfunction and a slew of other health problems, including subclinical hypothyroidism. (38) That’s where your TSH may be high, but your levels of other thyroid hormones are within a normal range.
8. Exercise, but Not Too Much
Exercise is essential for optimal health. However, over-exercising is not healthy; in fact, it activates the body’s stress response and causes serious damage both over the short and long term. The amount of exercise that a person can handle without going too far depends on the individual. For guidelines on how to avoid over-exercising while still enjoying yourself and getting benefits from physical activity, check out my podcast “Exercise and ‘Adrenal Fatigue’.”
9. Try Adaptogenic Herbs
Adaptogens are plants that help the body adapt to stress, protecting it through various mechanisms:
Adaptogens induce the production of proteins that protect the cells when the body is under stress (39)
Adaptogens increase neuropeptide Y, a stress-responsive hormone that stops the HPA axis from overactivating (40)
Adaptogens modulate stress-induced gene expression (41, 42)
Ashwagandha, a popular adaptogen that has a long history of use in Ayurvedic medicine, has stress-reducing effects and has been found to improve thyroid function in those with subclinical hypothyroidism. (43) Rhodiola rosea, an adaptogen native to Siberia, increases neuropeptide Y and reduces the hypothalamic expression of the stress-related gene c-Fos. (44, 45) These adaptogens may be beneficial additions to protocols designed to normalize HPA axis activity and improve thyroid function.
10. Think about Your Stressful Experiences Differently
While all of us face stress in our daily lives, we can influence how we respond to stressors by changing how we perceive them. In psychology, this strategy is known as “reframing.” Reframing gives us some control over how we respond to stressful events in life and can thereby reduce our stress levels and HPA axis activity. You can read more about reframing, and how to incorporate it into your life, in my article “5 Simple (But Powerful) Tools for Fighting Stress.”
11. Start a Mindfulness Practice
While stress initiates the release of thyroid-damaging inflammatory cytokines, stress-reduction practices decrease these cytokines and may improve thyroid function. (46, 47) In a group of 80 healthy women, consistent mind–body training (MBT) decreased TNF-alpha and IL-6, two inflammatory cytokines that have been associated with impaired thyroid function. (48, 49) Mind– body training refers to a practice that incorporates rhythmic movements with deep breathing exercises and meditation. Yoga is another mindfulness practice that may improve thyroid function by reducing stress. A small study found that six months of yoga practice decreased TSH, an effect associated with increased thyroid function. (50) Mindfulness practices also tend to have antidepressant effects. Antidepressants have been found to directly improve thyroid function in rats. (51) Other stress-reducing, mood-boosting strategies that don’t involve antidepressants may also help hypothyroidism.
12. Make Play a Part of Your Life
Play is a powerful tool for reducing stress and enhancing resilience. (52) While play can take countless forms, it has one defining factor: it’s an activity you engage in for enjoyment or recreation. Here are just a few examples:
Roughhousing with pets or children
Playing make-believe
Playing organized sports such as soccer, baseball, or basketball
Engaging in other forms of physical activity such as rock climbing, skiing, surfing, or ultimate Frisbee
Playing board games
Dancing
Going outside and walking in nature
Engaging in creative expression such as making art, music, gardening, or cooking a meal
Performing creative, innovative work (yes, work can be play!)
Engaging in playful banter at your job or a party
Having a playful relationship with your partner or spouse
Set aside time in your schedule for play, just as you would for other commitments such as work and exercise. I think you’ll find this to be one of the most enjoyable stress-reduction strategies listed here! You can read more about the benefits of play in my article “10 Benefits of Play.”
If you struggle with hypothyroidism and have tried medications, dietary changes, or supplements with minimal results, it may be time to consider the influence of chronic stress in your life. By taking proactive steps to reduce physical, mental, and emotional stress, you can set your body on the path toward optimal thyroid health.
Now I’d like to hear from you. Do you have questions about how chronic stress causes hypothyroid symptoms? Have you tried any of the stress-reduction strategies outlined in this article? Let me know in the comments below!
The post Can Chronic Stress Cause Hypothyroid Symptoms? appeared first on Chris Kresser.
Can Chronic Stress Cause Hypothyroid Symptoms? published first on https://drugaddictionsrehab.tumblr.com/
0 notes