#the current variants are more infectious than measles
Explore tagged Tumblr posts
Text
EVERY SINGLE STRAIN SINCE ALPHA HAS BEEN CAPABLE OF "BREAKTHROUGH" INFECTIONS.
I cannot fucking EVEN with folks who still think the vaccine is having any substantial impact on *transmission*. It isn't, it hasn't since Delta or so, and it *never* was intended to do so.
The goal of the vaccine was to stop *severe* symptoms and *death*.
Please, for the love of your health, your children, your friends' children, your pets, whoever and whatever you love that will get you past this mental barrier, WEAR A RESPIRATOR MASK. GET YOUR KID TO MASK AT SCHOOL AND DAYCARE.
N95, KN95, KF94, ELASTOMERIC, P100 ... whatever seals well your/their face and you/they can comfortably wear.
Cloth masks and those blue surgical masks? Neither are effective against current strains. Please upgrade, I'm begging you.
Covid is not a cold. Covid is not the flu. Covid can and does cause widespread organ and immune system damage, *even in mild and asymptomatic cases*.
While I'm at it....
The current at-home "rapid" tests are generating a lot of false negatives with the current variants. If you suddenly feel like shit, odds are really good it's fucking COVID even if you get a negative rapid / lateral flow / antigen test.
Relatedly, the most accurate way to use those tests is to swab your cheek and throat, then your nose. Nose alone is often not enough these days.
Relatedly, *many* people have been reporting for months that they don't test positive until 2+ days after their symptoms start.
One test alone is NOT an "all clear".
While I'm at it ...
The whole "go back to work after 5 days" thing? ZERO basis in science. It is purely a capitalism thing. Anyone with COVID is almost certainly still infectious after 5 days, and may still be infectious after 10 days.
Also, folks rebound, and not just with/because of paxlovid. SO...
Anyone with COVID should not consider themselves not-infectious until they have two, separate, consecutive negative rapid tests at least 24 hours apart.
While I'm at it ...
Yes, you can get reinfected with a different strain of COVID nearly immediately. There's not much cross-strain immunity anymore and there are *so many* strains going around. So, do NOT rely on a window of immunity after getting it.
While I'm at it ...
CLEAN YOUR AIR. By which I mean run HEPA filters in your homes, classrooms, workspaces, etc.
If you can't afford a commercial HEPA air purifier, look into Corsi-Rosenthal boxes ... they're basically a box fan with a MERV-13 heater filter taped to it.
You need HEPA or MERV-13 level of filtration to clear COVID from the air.
Note: there's a lot of "personal" size air purifiers out there. They're honestly really too small to do much of anything unless it's literally inches from your face the entire time, which is awkward.
While I'm at it ...
Because testing is becoming less available and because official folks are barely or not even reporting deaths and hospitalizations and because many people just do rapid tests at home and don't report the results to anyone and because fucking capitalism... about the only reliable data we have left is wastewater tracking.
Here's the current graph from BioBot, which aggregates the data from what wastewater processing facilities are still doing and reporting their testing:
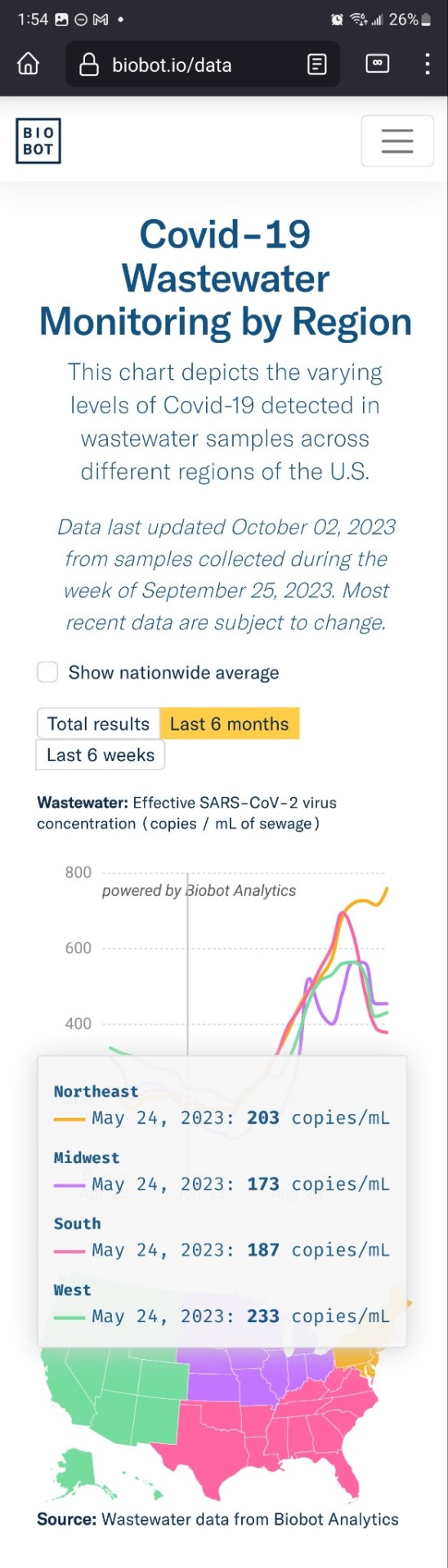
So, especially if you live in the Northeast USA, assume COVID IS RAMPANT right now.
PLEASE take care of yourself and those you love and MASK.
I just want to be able to participate in society again without risking life-long disability and/or death ....
#covid isn't over#covid is airborne#covid is still a thing#the current variants are more infectious than measles#wear a mask#please#I would like to be able to participate in society again#but y'all are out there spreading a level 3 biohazard#wear an N95#wear a KN95#wear a KF94#wear an elastomeric mask#wear a P100#masks are community care#Corsi-Rosenthal boxes#HEPA filters#clean the air
35K notes
·
View notes
Text
without paywall
The outdoors have always been a sanctuary—even more so since the advent of the pandemic.
Spreading COVID outside was possible, but not probable, experts advised in 2020, urging cooped-up citizens to turn to Mother Nature as an antidote to the isolation of lockdowns. Events, dining, and even entire classrooms were moved outside, when feasible.
But Omicron was a game changer, in more ways than one.
The original Wuhan strain of COVID-19 had a reproductive rate—also known as an R0 or R-naught value—of around 3.3, meaning that each infected person infected another 3.3 people, on average. That put COVID-19 among the least transmissible human diseases.
Slightly less transmissible were the 1918 pandemic strain of flu, which had an estimated R0 of 2, as does Ebola. On the higher end of the spectrum, mumps has an R0 of 12; measles tops the list at 18.
In order to outcompete, successful COVID variants have become more transmissible with time. Delta had a slightly higher reproductive rate of around 5.1. Then came Omicron, with an reproductive rate almost twice as large: 9.5.
So called “stealth Omicron,” nicknamed for its ability to evade detection on PCR tests, was about 1.4 times more transmissible than BA.1, so its reproductive rate was around 13.3, Adrian Esterman, a professor of biostatistics and epidemiology at the University of South Australia, recently wrote on academic news website The Conversation.
New studies suggest that BA.4 and BA.5, currently sweeping the U.S. and countries around the globe, have a growth advantage over BA.2 similar to the growth advantage BA.2 had over BA.1. Thus, the latest dominant COVID subvariants have a reproductive rate of around 18.6, tying or surpassing measles, the world’s most infectious viral disease, according to. Esterman.
Greater transmissibility means greater transmissibility in any setting, indoors or outdoors—even if outside is still safer, Maimuna Majumder, an assistant professor at Harvard Medical School and a computational epidemiologist at Boston Children’s Hospital, recently told NPR.
Upping the ante is the fact that recent subvariants like BA.4 and BA.5 are the most immune-evasive yet, with the ability to dodge antibodies from both vaccines and prior infection.
All this to say your protection outdoors isn’t what it was in 2020—and it may be time to begin thinking more critically about outdoor gatherings.
14 notes
·
View notes
Text
NEW COVID-19 Vaccines – Great News;
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19 For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.”
0 notes
Text
Will You Need A Booster Vaccine Against Covid-19?
https://sciencespies.com/news/will-you-need-a-booster-vaccine-against-covid-19/
Will You Need A Booster Vaccine Against Covid-19?
Infectious disease expert Dr. Mark Kortepeter discusses what we know so far about Covid-19 vaccine booster shots and what information scientists need to make the decision.
When President Joe Biden recommended in August that everyone get a booster eight months after their last dose, it caught some people in the scientific community and the government by surprise. Though even in announcing the September rollout, there was a catch. Biden acknowledged the booster plan still needed to be OKed by scientists at the FDA and the CDC. The scientists have now spoken. An FDA advisory committee met on September 17th to review the science of the Pfizer vaccine and after much discussion voted in favor of a third vaccine dose only for people aged 65 and over, as well as those considered at high risk. The committee, however, felt that the safety and efficacy data did not support a third dose for everyone at this time. Here’s what we know about boosters.
What is a booster?
Many vaccines typically consist of a primary series and boosters. The primary series includes one or more doses over the course of several months to years to give someone basic protection against a specific bacterial or viral pathogen, which we refer to as “fully vaccinated.” A booster is an additional dose of the vaccine beyond the primary series.
Boosters are not unusual. For example, the primary series of the vaccine against measles virus is given as a single dose around one year old. We didn’t used to give a booster, because the single dose was so effective. It wasn’t until there was a large outbreak of measles in U.S. school children in 1989 that we realized some children didn’t respond to the first dose. Hence, a second dose is now recommended to be given between ages 4-6 years old.
It is generally harder to maintain immunity against bacterial pathogens, so vaccines against bacteria typically require more shots in the primary series. For example, the vaccine against whooping cough (pertussis) requires five doses over several years for the primary series, followed by a booster at age 11-12.
For the Covid vaccines, the ones made by Pfizer and Moderna currently require two doses and the Johnson & Johnson vaccine requires one dose to be considered fully vaccinated. Under the current emergency use authorization, a third dose of the Pfizer vaccine can also be given to immunocompromised individuals.
Why has it taken so long to decide on Covid vaccine boosters?
Usually, a pharmaceutical company has several years to follow people vaccinated in a research study to determine the duration of protection and the optimal time to give boosters. Because of the pandemic emergency, there was a critical need to roll out vaccines before individuals could be followed for months or years to make this determination. This leaves us trying to make vaccine policy in real-time while the pandemic continues. To use a common analogy, we are “building the plane while flying.”
It is possible to follow the levels of antibodies people have in their blood over time. If the antibody levels drop, then it may indicate someone needs a booster. It isn’t so simple, though. Antibodies are only one piece of the puzzle. The human body has other ways it fights viruses, which are harder to measure. We don’t even know what level of antibodies are required to prevent disease and therefore what level we should strive to reach. The best way to learn how long the vaccines work is to get “real world” data on how many people get infected and sick over time.
What do we know so far?
When the Covid vaccines first rolled out, the early data demonstrated that they were over 90% effective at preventing severe disease and death, but we had no idea how long that protection would last. There was early concern that individuals with compromised immune systems would not respond as well to the vaccines. Consequently, there is already a recommendation for them to receive a third dose at least 28 days after the second one.
For everyone else, as Covid continues to circulate around the world and the new highly contagious delta variant tears through the population as fast as the wildfires engulf northern California, we are seeing increasing “breakthrough” infections in those who were fully vaccinated. However, recent data from the CDC comparing two periods of time in 2021 (April 4-June 19 versus June 20-July 17) indicate that although there have been increasing rates of Covid infection in the vaccinated group over time, protection against severe disease and death has declined only slightly. The decline was greater in those 65 years and older. ICUs across the U.S. continue to be filled mostly with the unvaccinated. The CDC data only goes through July 2021, so it may not be the full picture of where we are headed. Recent data from Israel show declining protection against disease and severe disease (especially in those greater than 60 years old) six months after receiving the second Pfizer vaccine. Could the Israeli experience be a harbinger for what will happen in the US? Possibly, but we won’t know until we have more time to gather more data.
Who makes the decision on boosters?
Despite the White House’s recently announced intention to give people a Covid booster eight months after the primary series, neither the White House nor another country’s policies, a single scientific paper, or your favorite social media blogger determine when a booster is needed. The way the process works is that the company product sponsor has to collect the “real world” data and present it to the FDA, where scientists and regulators pour over it. The FDA has the regulatory authority to make the final decision on whether a particular vaccine has demonstrated safety and efficacy for it to be given as a booster. It is a very deliberate process, and it needs to be, because it impacts peoples’ health. FDA advisory committees are an important part of the process. The September 17th advisory committee considered multiple sources of data, including from the company (in this case, Pfizer). The committee’s determinations may have answered some questions, but they still may have left many confused. We are seeing scientific debate now in sharper focus than usual, because the stakes are high with the ongoing pandemic. However, disagreement among scientists is common and it is a healthy part of the scientific process.
Will you need a booster?
So, should you get a booster now? If you can envision a staircase, consider the top of the stairs as the highest risk for severe disease. Each step, then, adds a risk factor for more severe disease, for example, age over 65 might be one step, immunocompromising illness might be another step or more. If you have a job that puts you at greater risk of interacting with sick people (for example, a healthcare provider, first responder, nursing home aid, teacher), that could be another step. Another might be a longer duration since your second vaccine dose. When you add up all your risk factors, the higher you find yourself on the staircase, the more reasonable it is for you to get a booster.
Keep in mind that if you have been fully vaccinated, your immunity isn’t like a light switch – on one moment and off the next. If it is going to decline, it does so gradually over time. It would be nice if we had a crystal ball to know what the data in three or six months will show, but we don’t have that. People want answers quickly, but science doesn’t move at the speed of social media. It never will – and that is a good thing.
Full coverage and live updates on the Coronavirus
#News
0 notes
Text
Underselling the Vaccine

Want to get The Morning by email? Here’s the sign-up.
Good morning. We explain why the vaccine news is better than you may think.
Early in the pandemic, many health experts — in the U.S. and around the world — decided that the public could not be trusted to hear the truth about masks. Instead, the experts spread a misleading message, discouraging the use of masks.
Their motivation was mostly good. It sprung from a concern that people would rush to buy high-grade medical masks, leaving too few for doctors and nurses. The experts were also unsure how much ordinary masks would help.
But the message was still a mistake.
It confused people. (If masks weren’t effective, why did doctors and nurses need them?) It delayed the widespread use of masks (even though there was good reason to believe they could help). And it damaged the credibility of public health experts.
“When people feel as though they may not be getting the full truth from the authorities, snake-oil sellers and price gougers have an easier time,” the sociologist Zeynep Tufekci wrote early last year.
Now a version of the mask story is repeating itself — this time involving the vaccines. Once again, the experts don’t seem to trust the public to hear the full truth.
This issue is important and complex enough that I’m going to make today’s newsletter a bit longer than usual. If you still have questions, don’t hesitate to email me at [email protected].
‘Ridiculously encouraging’
Right now, public discussion of the vaccines is full of warnings about their limitations: They’re not 100 percent effective. Even vaccinated people may be able to spread the virus. And people shouldn’t change their behavior once they get their shots.
These warnings have a basis in truth, just as it’s true that masks are imperfect. But the sum total of the warnings is misleading, as I heard from multiple doctors and epidemiologists last week.
“It’s driving me a little bit crazy,” Dr. Ashish Jha, dean of the Brown School of Public Health, told me.
“We’re underselling the vaccine,” Dr. Aaron Richterman, an infectious-disease specialist at the University of Pennsylvania, said.
“It’s going to save your life — that’s where the emphasis has to be right now,” Dr. Peter Hotez of the Baylor College of Medicine said.
The Moderna and Pfizer vaccines are “essentially 100 percent effective against serious disease,” Dr. Paul Offit, the director of the Vaccine Education Center at Children’s Hospital of Philadelphia, said. “It’s ridiculously encouraging.”
The details
Here’s my best attempt at summarizing what we know:
The Moderna and Pfizer vaccines — the only two approved in the U.S. — are among the best vaccines ever created, with effectiveness rates of about 95 percent after two doses. That’s on par with the vaccines for chickenpox and measles. And a vaccine doesn’t even need to be so effective to reduce cases sharply and crush a pandemic.
If anything, the 95 percent number understates the effectiveness, because it counts anyone who came down with a mild case of Covid-19 as a failure. But turning Covid into a typical flu — as the vaccines evidently did for most of the remaining 5 percent — is actually a success. Of the 32,000 people who received the Moderna or Pfizer vaccine in a research trial, do you want to guess how many contracted a severe Covid case? One.
Although no rigorous study has yet analyzed whether vaccinated people can spread the virus, it would be surprising if they did. “If there is an example of a vaccine in widespread clinical use that has this selective effect — prevents disease but not infection — I can’t think of one!” Dr. Paul Sax of Harvard has written in The New England Journal of Medicine. (And, no, exclamation points are not common in medical journals.) On Twitter, Dr. Monica Gandhi of the University of California, San Francisco, argued: “Please be assured that YOU ARE SAFE after vaccine from what matters — disease and spreading.”
The risks for vaccinated people are still not zero, because almost nothing in the real world is zero risk. A tiny percentage of people may have allergic reactions. And I’ll be eager to see what the studies on post-vaccination spread eventually show. But the evidence so far suggests that the vaccines are akin to a cure.
Offit told me we should be greeting them with the same enthusiasm that greeted the polio vaccine: “It should be this rallying cry.”
The costs of negativity
Why are many experts conveying a more negative message?
Again, their motivations are mostly good. As academic researchers, they are instinctively cautious, prone to emphasizing any uncertainty. Many may also be nervous that vaccinated people will stop wearing masks and social distancing, which in turn could cause unvaccinated people to stop as well. If that happens, deaths would soar even higher.
But the best way to persuade people to behave safely usually involves telling them the truth. “Not being completely open because you want to achieve some sort of behavioral public health goal — people will see through that eventually,” Richterman said. The current approach also feeds anti-vaccine skepticism and conspiracy theories.
After asking Richterman and others what a better public message might sound like, I was left thinking about something like this:
We should immediately be more aggressive about mask-wearing and social distancing because of the new virus variants. We should vaccinate people as rapidly as possible — which will require approving other Covid vaccines when the data justifies it.
People who have received both of their vaccine shots, and have waited until they take effect, will be able to do things that unvaccinated people cannot — like having meals together and hugging their grandchildren. But until the pandemic is defeated, all Americans should wear masks in public, help unvaccinated people stay safe and contribute to a shared national project of saving every possible life.
THE LATEST NEWS
The Transition
President-elect Joe Biden picked two Obama-era regulators to oversee key financial agencies: Gary Gensler to lead the Securities and Exchange Commission, and Rohit Chopra as the head of the Consumer Financial Protection Bureau.
Here’s Biden’s response to aides who use overly academic or elitist language: “Pick up your phone, call your mother, read her what you just told me,” he likes to say. “If she understands, we can keep talking.”
President Trump’s allies have collected tens of thousands of dollars from people seeking pardons.
Capitol Riot Fallout
From Opinion: Today is Martin Luther King’s Birthday. In a video Op-Ed, Martin Luther King III remembers his father’s economic message.
Media Equation: Fox settled a lawsuit over its lies about a murdered young man, but the network insisted that the settlement had to stay secret until after the 2020 election.
Lives Lived: Phil Spector was a pioneering producer who shaped the sound of pop music in the 1960s but who spent the end of his life in prison after murdering Lana Clarkson at his home in 2003. He has died, from complications from Covid-19, at 81.
Why sea shanties are suddenly viral
On TikTok in December, Nathan Evans, a 26-year-old Scottish postal worker and musician, shared a black-and-white video of himself singing a sea shanty — a traditional sailor’s work song — called “Soon May the Wellerman Come.” In the ensuing weeks, Sea Shanty TikTok was born.
Professional musicians, people driving in cars and even a Kermit the Frog puppet shared videos of themselves singing along. There were electro remixes. Some people began covering other songs, like “All Star” by Smash Mouth, in a sea-shanty style.
While the genre may seem like a strange one to go viral, the songs are relatively easy to learn. They also lend themselves well to collaboration, which TikTok’s functions encourage. An original goal of the sea shanty was to foster community, as sailors worked long hours aboard a ship.
“They are unifying, survivalist songs, designed to transform a huge group of people into one collective body, all working together to keep the ship afloat,” Kathryn VanArendonk writes in Vulture. And they’re especially fitting for a time when people are desperate for connection.
PLAY, WATCH, EAT
What to Cook
Spanakopita, the classic Greek spinach and feta pie, inspired this baked pasta.
What to Watch
“MLK/FBI,” directed by Sam Pollard, draws on long-secret documents to chronicle the F.B.I.’s harassment of the Rev. Dr. Martin Luther King Jr.
What to Listen to
Hear new tracks from Flo Milli, Lana Del Rey and more — including a song that holds the single-day streaming record on Spotify.
Multiple Service Listing for Business Owners | Tools to Grow Your Local Business
www.MultipleServiceListing.com
The post Underselling the Vaccine appeared first on Multiple Service Listing.
from Multiple Service Listing https://ift.tt/2LYyPrd
0 notes
Text
Officials in Britain this past weekend sounded an urgent alarm about what they called a highly contagious new variant of the coronavirus circulating in England.
Citing the rapid spread of the virus through London and surrounding areas, Prime Minister Boris Johnson imposed the country’s most stringent lockdown since March.
“When the virus changes its method of attack, we must change our method of defense,” he said.
On Sunday, European countries began closing their borders to travelers from the United Kingdom, hoping to shut out the new iteration of the pathogen.
In South Africa, a similar version of the virus has emerged, shares one of the mutations seen in the British variant, according to scientists who detected it. That virus has been found in up to 90% of the samples whose genetic sequences have been analyzed in South Africa since mid-November.
Scientists are worried about these variants but not surprised by them. Researchers have recorded thousands of tiny modifications in the genetic material of the coronavirus as it has hopscotched across the world.
Some variants become more common in a population simply by luck, not because the changes somehow supercharge the virus. But as it becomes more difficult for the pathogen to survive — because of vaccinations and growing immunity in human populations — researchers also expect the virus to gain useful mutations enabling it to spread more easily or to escape detection by the immune system.
“It’s a real warning that we need to pay closer attention,” said Jesse Bloom, an evolutionary biologist at the Fred Hutchinson Cancer Research Center in Seattle. “Certainly, these mutations are going to spread, and definitely, the scientific community, we need to monitor these mutations, and we need to characterize which ones have effects.”
The British variant has about 20 mutations, including several that affect how the virus locks onto human cells and infects them. These mutations may allow the variant to replicate and transmit more efficiently, said Muge Cevik, an infectious disease expert at the University of St. Andrews in Scotland and a scientific adviser to the British government.
But the estimate of greater transmissibility — British officials said the variant was as much as 70% more transmissible — is based on modeling and has not been confirmed in lab experiments, Cevik added.
“Overall, I think we need to have a little bit more experimental data,” she said. “We can’t entirely rule out the fact that some of this transmissibility data might be related to human behavior.”
In South Africa, too, scientists were quick to note that human behavior was driving the epidemic, not necessarily new mutations whose effect on transmissibility had yet to be quantified.
The British announcement also prompted concern that the virus might evolve to become resistant to the vaccines just now rolling out. The worries are focused on a pair of alterations in the viral genetic code that may make it less vulnerable to certain antibodies.
But several experts urged caution, saying it would take years — not months — for the virus to evolve enough to render the current vaccines impotent.
“No one should worry that there is going to be a single catastrophic mutation that suddenly renders all immunity and antibodies useless,” Bloom said. “It is going to be a process that occurs over the time scale of multiple years and requires the accumulation of multiple viral mutations. It’s not going to be like an on-off switch.”
He also said that the restrictions Johnson imposed could be in place for months.
Like all viruses, the coronavirus is a shape-shifter. Some genetic changes are inconsequential, but some may give it an edge.
Fortunately, the body’s entire immune system is a much more formidable adversary.
The Pfizer-BioNTech and Moderna vaccines induce an immune response only to the spike protein carried by the coronavirus on its surface. But each infected person produces a large, unique and complex repertoire of antibodies to this protein.
“The fact is that you have a thousand big guns pointed at the virus,” said Kartik Chandran, a virus expert at the Albert Einstein College of Medicine in New York. “No matter how the virus twists and weaves, it’s not that easy to find a genetic solution that can really combat all these different antibody specificities, not to mention the other arms of the immune response.”
In short: It will be very hard for the coronavirus to escape the body’s defenses, despite the many variations it may adopt.
Escape from immunity requires that a virus accumulate a series of mutations, each allowing the pathogen to erode the effectiveness of the body’s defenses. Some viruses, like influenza, amass those changes relatively quickly. But others, like the measles virus, collect hardly any of the alterations.
Even the influenza virus needs five to seven years to collect enough mutations to escape immune recognition entirely, Bloom noted. His lab Friday published a new report showing that common cold coronaviruses also evolve to escape immune detection — but over many years.
Immunizing about 60% of a population within about a year and keeping the number of cases down while that happens will help minimize the chances of the virus mutating significantly, Hodcroft said.
Still, scientists will need to closely track the evolving virus to spot mutations that may give it an edge over vaccines.
Scientists routinely monitor mutations in flu viruses in order to update vaccines and should do the same for the coronavirus, said Trevor Bedford, an evolutionary biologist at the Fred Hutchinson Cancer Research Center in Seattle.
“You can imagine a process like [that] exists for the flu vaccine, where you’re swapping in these variants, and everyone’s getting their yearly COVID shot,” he said. “I think that’s what generally will be necessary.”
The good news is that the technology used in the Pfizer-BioNTech and Moderna vaccines is much easier to adjust and update than conventional vaccines. The new vaccines also generate a massive immune response, so the coronavirus may need many mutations over years before the vaccines must be tweaked, Bedford said.
#news#world news#us news#international news#international#covid-19#coronavirus#coronavirus vaccine#covid response#virology
0 notes
Text
NEW COVID-19 Vaccines – Great News; but COVID Variants and Poor Choices by Governors may Erase all Gains and Extend the Pandemic
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19 For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.”
0 notes
Text
Measles Epidemiology
Measles is a highly contagious infection that is caused by measles virus. It is mostly common for children though anyone can be infected by it. Through vaccination, measles is preventable, most regions and countries that have effective vaccination mechanism for children, report minimal cases of the infection. Measles is highly contagious and is spread through fluid droplets transmissions such as mucus from the nose, throat or mouth. The infection is mostly passed through airborne as the droplets are released when the infected person coughs or sneezes. It is almost guaranteed that when an unimmunized person is exposed to the virus, they will get an infection, only a negligible percentage of the unvaccinated do not get infected.
Measles History
Measles cases can be traced back, up to the seventh century, as it was described in many ancient books. It is reported to have been a leading cause of morbidity and mortality especially among children’s. The contagious infection was perceived differently by people from different regions. The easiness with which the infection spread caused millions of children infected and a lot of deaths. It was perceived as a curse in some regions while other viewed it superstitiously and associated it with supernatural powers such as witchcraft.
The symptoms of measles according to Caserta include running nose, high fever (always greater than 40 c) and coughing. Koplik’s spots (white spots) start forming inside the mouth before spreading to the face and then to the whole body. The symptoms clearly begin to develop after 7-10 days and may last up to ten days before subsidizing or growing out of hand. In some incidences measles infections result in complications that may include brain inflammation, diarrhea or even blindness and pneumonia.
It was till the early 1960s that scientists were able to develop a vaccine for preventing measles. There were two kinds of vaccines opened, like Gallagher, Plotkin, Katz,& Orenstein assert, one variant was discovered from a measles virus that had been killed while the other was prepared from a live measles virus that had been weakened and has no capability of causing an infection to even not perfect immune system. The variant that used the immune system was later dropped as it proved to be ineffective in reducing the ability to prevent the disease infection. The adoption of the weakened live virus proved to be more effective. The weakened live virus has gone through modification since then to make it not only more effective but also to ensure that it does not affect those vaccinated. It worked on the premise that once a child is exposed to the weakened virus, they developed resistance to it, hence, cannot be exposed once there is an infection.
The development of the vaccine has been highly effective in reducing the impact of the disease on the prevalence of measles has been enormously reduced since the vaccine invention in 1963. The continuation scaling up of vaccination has seen the number of children getting measles vaccination increase to the current rate of over 90% of the global children being immunized. There was a reduction in the number of deaths reported as a result of measles infection which averages 75% between 2000 and 2010. This was as a result of the continuous development of the vaccination which has been boosted by the growth in scientific technology coupled with investments by different stakeholders in scientific research and technology. Furthermore, governments, non-governmental institutions, health workers and other stakeholders have enabled more and more children to be reached out.
Prevalence of Measles
Measles was once a common infection, but its impact is on a downwards trend since the invention of the vaccine. The continuous vaccination coverage on the global scale means that the number of people who are at the danger of being infected has significantly reduced. Furthermore, the improved technological and scientific development has seen to it that the more and more effective vaccines continue to be developed hence limiting the effect it may have to an individual.
Measles is predominantly prevalent today in areas where there is inadequate coverage of vaccination. The areas that have well coverage vaccination system like Europe have fewer cases of measles report like those that are inadequately covered like some parts of Africa and Asia. Different factors limit the issue of vaccine coverage in different regions. The factors include the availability of resources and infrastructure, the stability of a region and to some extent beliefs of the people of such a region where the measles vaccination campaigns are being undertaken. In some areas any vaccination has been shrouded with controversies as observes. The targets are fed with malice about the vaccination campaign which is shrouded with conspiracy theories that create apathy among the target hence do not take the vaccine.
Morbidity and mortality among children as a result of measles are still high in developing countries. Though every country offers some of the variants of the measles vaccines, in the developing countries there is poor access to them for the general population.
There is still a high number of morbidity and mortality especially among children as a result of measles. According to Lozano, Naghavi, Foreman, Lim, Shibuya, Aboyans, Abraham, Adair, Aggarwal & Ahn, a total 158,000 deaths were reported globally as a result of measles. Though this was quite a significant drop considering that in 1990 an estimated 65000 deaths had been reported, it pointed out the need to enhance the effectiveness of the vaccine campaign. Boralevi in his study observed that measles remained the primary vicinal infection causing death in the world by 2003. The sickness and suffering caused to children who are not affected relatively high considering only a small percentage of those infected with measles die from the infection.
Geographical Locations of Measles Prevalence
Prevalence of the measles cases is quite high in developing regions. According to WHO, the western Pacific region leads in the number of measles cases reported pointing out to the high prevalence of measles in the region. The African region and the South East Asia follows in the number of cases reported indicating high prevalence. Though European and American regions have a lower level of measles prevalence they still reported relatively high incidences of measles cases; the American region having close to 20000 cases while the European close to 16000 cases in 2014. It is, therefore, good to conclude that though measles is rampant in Africa and Asia; it is an infection that still calls for a global attention for it to be conclusively eliminated.
Measles outbreaks in different countries have been common phenomena which end up infecting a huge population. According to Perry et al., measles outbreaks have been experienced in both developed and developing countries. The United States and Germany were among some of the developed countries that have recently experienced outbreaks. In 2014 measles outbreak was encountered in the United States leading to the death of a woman, such case had occurred in years. In Germany, the late 2014- early 2015 measles outbreak resulted in almost eight hundred cases that had been reported. Though the developed countries have experienced outbreaks, they were able to be contained with minimum cases as compared to the developing countries scenarios. The measles outbreaks situation in Vietnam affected thousands of residents with tens of deaths being reported.
Definition of Measles
Measles is a contagious viral infection that affects the respiratory tract including the throats, bronchial tracts, and the lungs. Measles is characterized by the formation of white spots inside the mouth that then spreads on the face and sometimes the whole of a human's body. Though it is highly preventable through vaccination, measles is a life danger disease and those at risk include the unvaccinated, those traveling to areas of high prevalence and the ones who have a deficiency of vitamin C.
Literature Review
Measles is an infectious disease that poses a great danger to the people who are exposed to it. According to Strebel, Cochi, Hoekstra, Rota, Featherstone, Bellini & Katz measles has been there since time memorial, he observes in his study that the academic work of the Persian physician known as Rhazes (860-932) explored the diseases that were affected them during the era which included measles and smallpox. The diseases were infectious, and there was no medication for them. The impact of measles in causing death and infection in people was greatly reduced with the invention of the vaccine in 1963.
Vaccination concerns
The first measles vaccine was developed in 1963. As Caserta asserts there were two variants of the vaccine that were developed for trails, one variant was developed from a measles virus that had been killed while the other was developed from a live measles virus that had been weakened which has no capability of causing an infection to even a weakened immune system. The vaccine with the weakened virus was officially adopted in 1968 as it had better results when compared to the one with the variant with the dead virus.
People's concern about the vaccines
As Demicheli et al., observe measles infection highly affect children as their immunity is weak hence the need for immunization. Though the immunization has been developed for a while, measles continues to affect people globally as the access to the vaccine is still limited. The ability of measles to infect people within a short period and on a large scale makes it quite a significant public health issue. Furthermore, measles has been one of the leading causes of mortality and morbidity among children for quite long. The suffering and losses caused by the disease make it quite a focus on different stakeholders including governments, international and multinational agencies such as WHO, non-state actors, and other stakeholders to highly focus on the elimination of the virus. Measles can cause some infection to its victims including pneumonia, acute bronchitis and even miscarriage in pregnant women. As Perry et al., observes, the World Health Organization together with its key partners including the Red Cross, Measles Initiative and the Center for Disease Control and Prevention (CDCP) have played a key role in helping address the need for the measles vaccines to be effective and ensure that its access is universal globally.
Though the measles vaccines have been developed to ensure effectiveness over the years, its access is still low because of the sporadic reporting of cases. Furthermore, there are a variety of risks that can expose one to measles that are not controlled by the vaccine. As Strebel et al., urges, the immunity level in an individual, even if they had been vaccinated a critical risk factor. A person with lower immunity once exposed is more likely to be infected with the measles. The need to put in perspective other risk factors that expose one to measles infection is thus critical to be looked upon. According to Zipprich et al., the recent outbreak of measles in the United States that happened in the state of California in 2014, left one person dead. Death as a result of measles had been previously reported almost ten years before the California incident. Though the victim was immunized her lower immunity as a result of the different medication she was taking was highly associated with her death.
Conclusion and Discussion
Report on the findings and conclusion
Measles is still affecting a significant number of people globally, both, in developed and developing countries of the world as both continue to report cases of outbreaks. The development of vaccine over the years has been quite significant as it has been able to reduce the number of infections, hence, mortality and morbidity. There is a need for vaccination to be more universal by undertaking a sound approach that is more holistic in addressing and reaching out to all those at risk. Furthermore, there is a need for the major stakeholders to ensure that the best variant vaccine is accessible to all. Areas with high prevalence and incidences need to be focused on to ensure that children there are not only vaccinated, but all the risk factors that expose the population to measles are wholesomely addressed.
The role of vaccination in combating should, therefore, be supported as it plays the key role in reducing measles. Ensuring that the vaccine is accessible to everyone at risk is crucial in combating the disease globally.
0 notes
Text
NEW COVID-19 Vaccines – Great News!
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19
For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.
0 notes
Text
NEW COVID-19 Vaccines
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19
For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.
0 notes
Text
COVID Variants and Poor Choices by Governors
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19
For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.
0 notes
Text
NEW COVID-19 Vaccines – Great News;
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19
For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
0 notes
Text
NEW COVID-19 Vaccines – Great News; but COVID Variants and Poor Choices by Governors may Erase all Gains and Extend the Pandemic
New vaccines and significant improvements in the implementation of delivering vaccines have dramatically improved the chances of managing the COVID-19 pandemic.
As an ever-increasing number of us are being vaccinated against the COVID-19 virus, it’s important to focus on achieving our National goal of herd immunity to protect ourselves and others. In the last few weeks, things have run more effectively than ever, so it’s important to not let a false sense of security allow complacency.
Herd Immunity and COVID-19 For COVID-19 herd immunity, experts still aren’t sure what the threshold will be. The initial estimates of 60% to 70% were too low, although infectious disease specialist Dr. Anthony Fauci reportedly doesn’t believe this particular virus is as contagious as measles. If that’s the case, we may need between 70% and 95% of people to be vaccinated to achieve herd immunity.
Ref: https://www.goodrx.com/blog/covid-19-herd-immunity/
There remain two core limitations to securing the safety of the nation’s population. The first constraint started with the creation of vaccines and now is the mass production of them. The second is the actual vaccination of the population.
It is imperative that the population reach herd immunity levels before the viral mutations adapt, creating variants that can’t be addressed with the current vaccines. The intentional delays of the previous administration hindered the vaccine rollout, but the accelerated implementation efforts in Q1 and Q2 2021 offer some degree hope.
Does Health Insurance Cover COVID-19 Testing?
Also, there are now three vaccines for the COVID-19 virus. And the good news is that at lead two of them show reasonable effectiveness against the current variants.
The most recent is the single dose Johnson & Johnson vaccine. It was approved on Saturday February 27th and is a major advance both in production capacity and ease of distribution. One of the major advantages is that is doesn’t need to be frozen for transport and requires only one “jab”.
Delivery is of the Johnson & Johnson vaccine is already under way.
Curious about these vaccines? Learn more about them!
The Moderna COVID-19 Vaccine
The Pfizer COVID-19 Vaccine
The Johnson & Johnson COVID-19 Vaccine
Challenges to Vaccinating the entire Country
The logistics of producing, transporting, and inoculation are incredible, but it would appear that despite its magnitude, the task is being accomplished, and wherever there are shortcomings, they are being addressed and mitigated.
The real challenge comes from the citizens themselves. There are two situations causing people to choose NOT to be vaccinated. Without these people being properly vaccinated, the nation will not reach her immunity and the COVID-19 pandemic will continue on, with more and stronger mutations occurring.
One population to resist the COVID-19 vaccination has a long history of medical neglect. From the study “The research, which appears in the journal Social Science & Medicine, found that Black people, women, and those with conservative leanings were most likely to refuse vaccination.
Black respondents were 41% less likely to pursue vaccination. That is significant since numerous studies have found that people who are Black, Asian, or from minority ethnic backgrounds are more likely to acquire COVID-19 and experience worse clinical outcomes.
This is often due to social, economic, and healthcare inequities experienced by these demographics in the United States and elsewhere.”
Get affordable health insurance
Medical professionals can do a better job of connecting with these people by helping them to understand the benefits and necessity of the vaccination.
For Doctors: COVID-19 vaccine hesitancy: 10 tips for talking with Patients
https://bit.ly/3bd3nPR
Disinformation: Frightening, false theories about the two COVID-19 vaccines that have now been administered to more than 24 million Americans
A surprising large group of people have fallen victim to false information spread through social media, and Doctors may have a harder time reaching these people. But in the name of public health, it’s vital that they work hard to do so.
Anti-Vaxxers Wage Campaigns Against COVID-19 Shots
https://www.webmd.com/vaccines/covid-19-vaccine/news/20210129/anti-vaxxers-mounting-internet-campaigns-against-covid-19-shots
In fact, recent decisions by Governors in Texas, and Mississippi, may soon reverse every positive step the US has made in fighting the pandemic:
“The US is at risk of losing all its recent gains in the battle against Covid-19 as highly contagious variants take advantage of Americans getting lax with safety measures.
“Please hear me clearly: At this level of cases with variants spreading, we stand to completely lose the hard-earned ground we have gained,”
Dr. Rochelle Walensky, Director, US Centeres for Disease Control
Image source: https://www.cdc.gov/about/leadership/director.htm#:~:text=Rochelle%20P.%20Walensky%2C%20MD%2C%20MPH%2C%20is%20the%2019,global%20response%20to%20HIV%2FAIDS.
On a very positive note, in an unique partnership between two competitors, the Biden administration is helping to ensure that Merck pharmaceuticals will help their rival Johnson & Johnson boost its vaccine production.
President Biden also said on Tuesday, March 2nd, that the U.S. will produce enough vaccines for every adult in the U.S. by the end of May, while making a fresh push to vaccinate school staff over the next month. “We’re now on track to have enough vaccine supply for every adult in America by the end of May.”
0 notes