#spinal imaging
Explore tagged Tumblr posts
Text
The Global Spinal Imaging Market is Anticipated to Witness High Growth Owing to Rising Incidence of Spinal Disorders

The global spinal imaging market encompasses imaging modalities and procedures used for evaluating spinal disorders and spine-related conditions. Key modalities include X-ray, CT myelography, MRI, nuclear imaging, and ultrasound. Spinal imaging provides detailed anatomical information and helps diagnose spinal disorders effectively. It plays a vital role in evaluating degenerative conditions, infections, masses, fractures, structural deformities, and post-surgical assessment. The growing burden of spinal disorders due to lifestyle changes and rising geriatric population is a key factor fueling demand for spinal imaging procedures worldwide. The Global spinal imaging market is estimated to be valued at US$ 2.10 BN in 2024 and is expected to exhibit a CAGR of 5.4% over the forecast period 2024 To 2031. Key Takeaways Key players operating in the Global Spinal Imaging Market Growth are Shimadzu Corp., FUJIFILM, Hitachi, Ltd., Toshiba Medical Systems, Inc., GE Healthcare, Koninklijke Philips N.V., Siemens Healthineers, Canon Medical Systems Corp., Bruker, and Mediso Ltd. These players are focusing on new product launches and offering advanced imaging modalities to bolster their market position. Major companies are also expanding their geographical presence in emerging markets through partnerships and acquisitions. For instance, in 2021, FUJIFILM acquired Hitachi's diagnostic imaging business to strengthen its position in the medical system business globally. The key opportunities in the market include increasing adoption of hybrid imaging systems, growing demand for minimally invasive procedures, and integration of AI and analytics with spinal imaging modalities. Hybrid imaging systems combine anatomical and functional imaging which help provide better visualization during diagnosis and treatment planning. Moreover, there is high potential for spinal imaging in emerging regions such as Asia Pacific, Latin America, and Middle East & Africa. Factors such as increasing healthcare expenditure, growing awareness about advanced spine care, and initiatives by market players will aid the adoption of spinal imaging in these markets over the forecast period. Market Drivers Rising incidence of spinal disorders due to obesity, trauma, age, and lifestyle changes is a major market driver. Spinal disorders account for a significant proportion of global musculoskeletal disease burden. According to the WHO, around 20% of the world's population is affected by spinal disorders annually. Get More Insights On This Topic: Spinal Imaging Market
#spinal imaging market#spinal imaging market Size#cspinal imaging market Share#spinal imaging#Healthcare#Spinal Infection#Vertebral Fractures
0 notes
Text


not sure where I get the energy, but it's a new day I guess
#working on that self compassion#feeling myself as much as i can#surgery body lol#spinal surgery recovery#selfies#me#smoking#makeup#woman with tattoos#my truck :)#body image#body neutrality
24 notes
·
View notes
Note
IM SO SORRY... I thought artemy's leg pain was popular fanon. I haven't checked pathic 2 in awhile. anyways! happy disability pride
HI YOU'RE GOOD sorry this took forever to get to! off the top of my head this is the line most people reference for it, c.f. this post:
CHILD: You know… Big, fat, dangerous, with bulgy eyes, a weird leg, a scary mug, and a stupid look on his face. Must be you.
and this line to Aspity:
HARUSPEX: My legs aren't that crooked, khetey.
ALSO from lika after the station massacre, implying the haruspex's leg was either (also) injured during that, or looked like it had been:
LIKA: Or do you want my collar? You could fix your leg with it.

honestly so so so so true. I do think part of it's the nature of "posts appreciating X attribute of a character usually won't reference other attributes unless directly related" but there's also such a wide variety of disability in pathologic's canon while I tend to only see discussion of its non-physical disabilities in the wild... we need in-depth essays on the representation of 2006's Some Git npc 1 million notes everywhere
#var's appearance WAS played for shock and disgust value in 1 but at least it affected his person and how other people viewed him... contrast#p2 var's missing eye which never comes up for anything. also I can't forgive it for making mark's cane purely cosmetic re his no longer#having spinal injuries. same w rubin not being brain injured. but it did offer lara's heart condition and YULIA'S leg condition at least :]#asks#anonymous#image described
24 notes
·
View notes
Text

His spinal column snaps like a twig.
(Shadow Hawk #1)
#Shadow Hawk#spinal column#spinal cord injury#karakkkkk#yaaaaa#jim valentino#image comics#comics#90s comics
3 notes
·
View notes
Text
ugghhhhhh I hate seeing shit that's like "omgggg women have to cut off their HEALTHY breast tissue to fit in, we need to change the way we treat women and we need to stop offering breast reduction surgery, and that's how you fix things, not AMPUTATING VITAL ORGANS 😡😡😡" as if breast tissue doesn't cause legit problems that can only be fixed surgically and the benefits usually far outweigh the risks and it's not at all vital
#vera talks#all of these people are always like ''I'm a 30B I know the pain and it's treatable non-surgically!!!''#like okay#there's a very big difference between that and a 26J with osteoporosis and spinal instability#I've literally been begging for that surgery for years and it's opinions like this that make it so hard to get someone to do#I have broken ribs from it don't tell me it's a body image issue#if you couldn't tell I got in a fight sorry#I am very heated right now
15 notes
·
View notes
Text
It is our wonderful day of Halloween. 💀🎃👻😈
I will be accepting trick or treats 😱in my ask box 💌. Just send "trick or treat" and say your costume🧙♂️🧟♂️🧛♂️, and ill give you 🫵 various fun tricks and treats ranging from random in-theme images 🖼️ to Spinal Tap😈🍬🍫🍭 giving you a singular treat or Skeletor💀🪄💥✨ casting a spell on you.
Go crazy with it and start ringing the metaphorical doorbell on my blog. 🚪🏚️⚰️🌕
#knowing me ill prob send everyone an image AND a spinal tap or skeletor doodle#if you sent one already you can also send one again i dont mind#or send me a billion anons idc i just looooove halloween
3 notes
·
View notes
Text










Attack on Titan's Titan Serum
Generated on Bing, by Cosmiccerealbowl
#aiartcommunity#ai artwork#ai image#ai generated#ai#ai art#ai images#attack on titan#attack#titan#syringe#needle#serum#titans#spinal fluid#attack on titan spinal fluid#titan serum#titan spinal fluid#spine#spinal#medical#anime#manga#real#early 1900s#1900s photography#box#supplies
2 notes
·
View notes
Text

Yeah its crazy how his appearance is so different from the shooter's. Almost like he didn't do it.


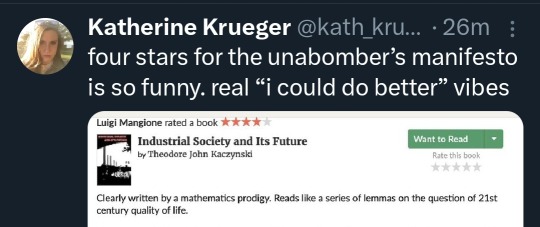


*through tears* ladies and gentlemen, they got him
#Sorry to my followers who will see me repost this image on every post like this I see.#It's insane that we're apparently just letting them make an example out of a random guy with a spinal injury.
31K notes
·
View notes
Text
Counterstrain Manual Therapy Reduces Muscle Spasticity and Neuropathic Pain in Individual with Chronic Spinal Cord Injury: Case Report by David R. Dolbow in Journal of Clinical Case Reports Medical Images and Health Sciences
ABSTRACT
Introduction: Muscle spasticity and neuropathic pain are common comorbidities after spinal cord injury (SCI) that can lead to further disability and the reduction in quality of life. Pharmacologic treatments are used as a standard of care for muscle spasticity and neuropathic pain. A possible adjunct therapy is osteopathic manual manipulation therapy.
Case Report: In this case report counterstrain manual therapy was provided as a novel approach to help provide additional temporary relief of muscle spasticity and neuropathic pain. The 60-year-old African American patient with a C5 motor complete SCI completed six sessions over six months as an adjunct treatment to the standard pharmacologic care of Baclofen and Neurontin. Counterstrain manual therapy was provided to the anterior lumbar region and bilateral legs in the patient’s home.
Discussion: The treatments produced additional temporary relief from spasticity and pain. In both cases the spasticity and pain decreased to greater levels as the number of treatment sessions increased, despite the length of time between treatments. Muscle spasticity decreased in a more consistent and uniform manner than pain although pain decreased significantly during later sessions with the sixth session resulting in the temporary elimination of pain. The patient also reported a significant reduction in interference in the participation of life activities.
Conclusion: The results of this case report cannot be generalized to the overall spinal cord population, but it does indicate the potential benefit of counterstrain manual therapy as an adjunct treatment to decrease muscle spasticity and neuropathic pain after SCI.
Introduction
Individuals with spinal cord injuries (SCI) often experience muscle spasticity and neuropathic pain, which can increase disability and reduce their quality of life. Spasticity affects around 70% of people with SCI, while neuropathic pain affects about 60% [1,2]. Spasticity is characterized by involuntary muscle contractions due to disorganized sensorimotor systems caused by damage to upper motor neurons [3]. Neuropathic pain is caused by disruption of the somatosensory system and can present itself as burning, squeezing, shooting, or pricking pain [4].
There are various pharmacological treatments, such as gabapentin, pregabalin, diazepam, and baclofen, that can help alleviate both spasticity and neuropathic pain [2,5,6]. Additionally, osteopathic manipulation therapy treatments including counterstrain manual therapy can be effective in reducing pain in people with chronic SCI [7]. Counterstrain manual therapy, also known as positional release therapy, may be uniquely suited to counter the effects of muscle spasticity and reduce neuropathic pain after SCI by allowing normal muscle spindle activity to return in those with neuromuscular imbalance due to aberrant neuromuscular activity and sympathetic nervous dysfunction [8].
We provide a case report in which counterstrain manual therapy was used as a novel adjunct treatment to pharmacological treatments to decrease spasticity and pain during six separate treatments.
Case Presentation
A 60-year-old African American woman with chronic C5 SCI, American Spinal Injury Association Impairment Scale B as per International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) presented with lower back and leg pain, bilateral leg spasticity, and difficulty in performing daily activities. The patient was injured in a motor vehicle accident ten years ago. The patient received spinal fusions at C5 and T5. The patient was 162cm in height and 95kg in weight and required assistance with dressing and bathing and could transfer from the bed to her powerchair with the help of an overhead trapeze bar (modified independence). However, the process was slow and fatiguing due to the muscle spasticity in her legs. The patient had been prescribed Baclofen and Neurontin for muscle spasticity and neuropathic pain. The initial evaluation measured the patient's pain level and interference in life activities using numerical rating scales from 0-10, along with the Spinal Cord Injury Spasticity Tool [9]. The same measures were taken after the six sessions of counterstrain manual therapy. The Modified Ashworth Test [10] for muscle spasticity, numerical pain rating scale, and identification of tender points on palpation were performed prior to and after each treatment session. The Modified Ashworth Test was conducted by a licensed physical therapist or students trained by the physical therapist, while tender point identification and counterstrain manual therapy were provided by an osteopathic physician or students trained by the osteopathic physician. Onsite observation or internet connection was used for supervision by a licensed physical therapist and an osteopathic physician. The patient had long-term use of pharmacological treatments to decrease spasticity and pain but had no history of receiving counterstrain manual therapy.
Muscle spasticity was assessed for bilateral hip and knee flexion and extension. To test hip flexion tone, the joint was moved from maximum flexion to full hip extension as quickly as possible. Likewise, for hip extension tone, the joint was moved from maximum hip extension to full flexion as quickly as possible. The same procedure was followed to measure knee flexion and extension tone. The muscle tone was graded from 0 to 4 based on the resistance encountered during the movement (0 = no resistance, 4 = rigid in flexion or extension) [10]. Tender point palpation and counterstrain treatment were performed as described by Bazzi et al.[11].
The areas treated depended on the pain or muscle tone determined with palpation of the tender points in the anterior lumbar (AL) region of the body [11]. Once a tender point was verbalized by the patient or due to tightness determined through palpation by the treatment provider, those regions were treated as described below. Once the patient was repositioned to produce decreased pain and tightness, the position was held for 90 seconds allowing the muscle spindle to relax decreasing tone in the muscle group [11].
AL1 (Medial to Anterior Superior Iliac Spine) – Treatment position was marked hip flexion to L1 level, knees toward the trainer rotating the knees, pelvis and ankles toward the tender point. This rotates the torso away from the side of the tender point.
AL2 (Medial to Anterior Inferior Iliac Spine) – Treatment position was flexion of the knees and hips to the level of the L2 vertebrae, ankles toward the trainer, rotation of the hips 60 degrees toward the trainer to level L2.
AL3 (Lateral to Anterior Inferior Iliac Spine) – Flexion of the knees and hips to L3, ankles and knees toward the trainer, minimal rotation with knees.
AL4 (Inferior to Anterior Inferior Iliac Spine) – Same as AL3 except more flexion than L3.
Discussion
Based on the Modified Ashworth Test scores before and after each session (Table 1), the degree of spasticity was reduced temporarily with greater degrees of reduction as the number of sessions increased. Throughout the initial three sessions, 14 out of 24 muscle group measures demonstrated decreased spasticity after the counterstrain manual therapy. During the last three sessions, all 24 muscle groups decreased in spasticity scores after the counterstrain manual therapy, with 21 of 24 muscle group measures recorded as level one on the Modified Ashworth Scale, which indicates only slight muscle tone. Additionally, the overall pre and post sessions spasticity scores decreased with the greater number of sessions. One possible reason that the counterstrain manual therapy sessions produced greater results as the number of sessions increased is that the patient may have become more relaxed with each session allowing greater benefits. It appears unlikely that the improvements were due to an accumulation effect of treatments because the six sessions were spread over a period of six months.
Spasticity levels as reported by the patient using the numeric rating scales for spasticity and interference in life activities prior to the first counterstarin manual therapy session and after the last manual therapy session demonstrated improvements over the length of the six sessions. The numeric scale regarding the level of interference in life activities by spasticity showed improvement in all categories except relationships. The patient reported scores on the 0-10 scale with 0 = Does not interfere and 10 = Completely interferes, demonstrating that the patient perceived important benefits. Regarding general activity, the patient reported a level 10 indicating maximal interference prior to the sessions but a 50% reduction to level 5 after the six sessions.
According to the participant, mood improved from 5 to 2, a 60% improvement and spasticity interference in work decreased significantly from 8 to 3 (62.5% reduction). Spasticity’s interference with sleep decreased slightly from 10 to 8 which is a 20% improvement. Overall, the patient indicated a noteworthy improvement in quality of life due to a reduction in interference of spasticity from 8 to 5 (37.5%). When asked to provide an overall percentage that the counterstrain manual therapy sessions decreased her spasticity, the patient stated that the treatments reduced spasticity approximately 70-80%, which lasted a few hours to 24 hours allowing her to attend church and other activities more easily. There was a reduction in muscle fatigue level from -3 to -2 as demonstrated by the pre and post Spinal Cord Injury Spasticity Evaluation Tool.
The LANSS pain scale verified the presence of neuropathic pain both prior to and after the counterstrain manual therapy sessions [12]. The overall effect of the counterstrain sessions on the patient’s numeric rating of pain also improved as the number of sessions increased. There were no decreases in pain during the first session with a rating of 9 on the 0-10 point numeric rating scale and a slight increase with the second session moving from an 8 to level 9. Through sessions three and four there was a slight decrease in pain (9 to 8) and then a dramatic decrease in overall pain for the final session 9 to 0. There was a greater decrease in the tender point pain ratings as the number of sessions increased with the greatest decreases coming after sessions 4-6 (Table 2). This was especially true after session 6 as all tender point regions decreased to zero pain. The decrease in pain over the six sessions may be due to the reduced spasticity over the same time period, although the reduction in spasticity was greater than that of pain. It is possible the patient was able to become more relaxed with repeated sessions which may have allowed improved benefits. Because the six sessions were spread over six months it is doubtful that the improvements demonstrate a cumulative effect of the treatments. There were no adverse events associated with the six counterstrain manual therapy treatments during the six month program.
Conclusion
This case report demonstrated that the use of counterstrain manual therapy may be an effective adjunct treatment to standard pharmacological treatments for spasticity and neuropathic pain after SCI. The results were temporary, lasting from a few hours to 24 hours. The reductions in muscle spasticity and neuropathic pain improved with the increased number of sessions regardless of time periods between the sessions. The counterstrain manual therapy demonstrated greater benefits with reduction of spasticity than pain except for the final session which resulted in the elimination of pain entirely. The patient also reported a reduction in the interference of spasticity in daily activities. Because these results reflect changes in a single patient, they cannot be generalized to the overall SCI population. However, it does show what is possible.
Data Availability Statement: Data is available in Tables 1 and 2 and can be received from the corresponding author upon reasonable request. Study protocols listed in ClinicalTrials. gov ID number: NCT05559255.
Authors Contributions: All authors provided substantial contributions to conception and design, acquisition, and interpretation of data. All authors either revised or edited the manuscript and provided approval of the version of the article being submitted for publication. The authors agree to be accountable for all aspects of the work including its accuracy and integrity.
Disclosure of Interests: The authors have no conflicts of interest to report.
Funding: This case report was funded by the American Osteopathic Association G2211485
Acknowledgements: The authors would like to thank Sarosh Din OMSIII and Mary Grimmett PMSIII for developing the initial research question, Aakash Anandjiwala OMSII for his assistance with administering the counterstrain treatment with this participant and Evan Williamson, DO, Faculty.
Statement of Ethics: This study protocol was reviewed and approved by the Institutional Review Board at William Carey University, approval number IRB# 2020-018. The patient reviewed and signed an informed consent form regarding risks and benefits and the non-use of personal identifiers or images. The ethics guidelines from the Helsinki Declaration were observed.
#Counterstrain Manual Therapy#Muscle Spasticity#Neuropathic Pain#Chronic Spinal Cord Injury#Journal of Clinical Case Reports Medical Images and Health Sciences#JCRMHS#Clinical Images journal
1 note
·
View note
Text
360° spinal fixations through posterior only approach in a child with pott’s disease: a case report by Md. Rezaul Amin in Journal of Clinical Case Reports Medical Images and Health Sciences.
Abstract
Tuberculosis (TB) is caused by acid-fast bacilli Mycobacterium tuberculosis and rarely by M. bovis, which is very common in developing countries like Bangladesh. Vertebral bodies are common site of extra-pulmonary involvement by TB. Although spinal TB is not very common in young children, pott’s disease affecting children and requiring surgical intervention have been reported. But in children, this surgery is often challenging due to greater technical difficulty with instrumentation. A 9-year-old girl presented with paraplegia due to compressive dorsal myelopathy due to pott’s disease at D4- D5 level. Anti-TB medication was started and two weeks later she underwent decompression of neural elements by D5 Laminectomy and corpectomy and stabilization by bilateral trans-pedicular screws and rods at D3, D4, D6 and D7 and fusion by mesh cage filled with autologous bone chips. Her post-operative recovery was uneventful. Histopathology report shows Granulomatous inflammation, compatible with tuberculosis. At the last follow-up, the patient was clinically and radiographically stable.
Keyword: 360° spinal fixation, Pott’s disease, Posterior only approach, Childhood spinal TB, Spinal instrumentation.
Introduction
Tuberculosis is a granulomatous inflammation involving various organs. The prevalence of TB is high in developing countries 1. High risk groups include the IV drug abusers, immunocompromised and HIV-infected people, prisoners and nursing home residents2. Vertebral tuberculosis, also known as Pott disease, is relatively common in certain regions of the world and is found in 1%–2% of TB cases worldwide3,4. Spinal TB is the most common site of extrapulmonary TB. The majority of Pott’s disease patients present with destruction and collapse of vertebrae and involvement of adjacent tissue. The disease may end up with spinal deformity and neurological complications like arachnoiditis, intramedullary tuberculoma and epidural abscesses5.
We report upper thoracic Pott’s disease in a 9-year-old girl with myelopathy. She was treated surgically with vertebral column resection and 360º reconstruction via a posterior-only approach to prevent the progression of neurological deficit and stabilize the deformity.
Case Report
History and Presentation
A 09 years old girl, 2nd issue of her non-consanguineous parent presented with the complaints of pain in the upper back for 02 months, weakness in both lower limbs for 2 weeks. Her weakness of lower limbs was sudden, asymmetrical (Left>right) and non-ascending type. Weakness was progressive and she became unable to walk or stand even with support 01 week later. She had no history of fever, convulsion, diarrhoea, vomiting, and headache. There was no history of contact with TB patient. Her bowel and bladder functions were normal.
Physical examination
Her lower limbs reveal visible muscle wasting of both legs, muscle tone was slightly increased, muscle power was MRC grade 0 in both lower limbs, deep tendon reflexes were exaggerated, planter were bilaterally extensor, sensory and autonomic function were intact. Upper limbs were neurologically intact, cerebellar sign absent, cranial nerve palsy absent; gait could not be assessed.
Investigations
CBC: Hb% 12gm/dl, ESR 47 mm in 1st hour, TC of WBC 7000/cmm, Neutrophil 65%,
Imaging: MRI of D/L spine with screening of whole spine shows T1 hypo & T2 hyperintense signal change with heterogenous contrast enhancement at D4 & D5 vertebral bodies and intervening intervertebral disc with almost complete collapse of D5 vertebral body with similar signal intensity pre and para vertebral soft tissue swelling at the same level with epidural extension causing spinal canal stenosis with cord compression and bilateral nerve root compression. Similar lesion is also present at S1 vertebral body.
Operative Procedure
Anti-TB medication started and two weeks later she underwent decompression of neural elements by D5 Laminectomy and corpectomy and stabilization by bilateral trans-pedicular screw and rod at D3, D4, D6 and D7 and fusion by mesh cage filled with autologous bone chips (Fig.2).
Postoperative course
Her post-operative recovery was uneventful. Her back pain was improved and she could walk without support. Histopathology report shows Granulomatous inflammation, compatible with tuberculosis. An 18 months antitubercular therapy was planned. During the first 3 months she got 4 drug regimen and for the rest of the 15 months, 2 drug regimen was advised. Pyridoxin was advised throughout the course of anti-TB therapy.
Follow Up
On 2nd post-operative day her lower limb muscle power improved to 3/5 and 02 weeks post op muscle power was 4-/5 and became able to walk without support and became pain-free. The patient was advised for follow-up in every 3 months (Fig. 3).
Discussion
Spondylitis is the most common manifestation of osseoarticular TB, and 1%–3% of patients with TB have skeletal involvement. It is most common in the first 3 decades of life and is a leading cause of paraplegia6. Vertebral body involvement usually occurs through the extensive venous plexus of Batson, spreading infection to multiple spinal segments while characteristically sparing the disc space7,8. Tuberculous spondylitis without any spinal cord compression or neurological deficits can be treated conservatively with anti-TB medications. Surgery is considered for patients with spinal cord compression or neurological compromise, significant spinal deformity, persistent severe axial pain or disease progression on maximal medical therapy9,10. Multiple surgical approaches are available for treatment of TB spondylitis in the pediatric age group. Outcomes of extensive surgery is similar to debridement alone except better correction of kyphosis and deformity in case of extensive surgery11. In addition, extensive surgery reduces the duration of chemotherapy12. Although Pott’s disease affecting young children are rare but it’s surgical management is technically challenging13. Presentation of vertebral TB in children are often insidious in onset and include back pain, fever and motor, sensory or autonomic dysfunction. Although chemotherapy is the first line of treatment, but surgery may be warranted if spinal cord compression or kyphotic deformity is present. Around 3% of children with pott’s disease develop severe kyphosis (> 60°)14 .Risk factors for kyphotic deformity includes age <10 years; involvement of ≥ 3 VBs; or involvement of thoracic spine15. Severe kyphosis is cosmetically unacceptable and causes spinal cord compression over the apex of the deformity and cardiopulmonary dysfunction from restrictive lung disease. Skeletal immaturity of young children must be taken into account during surgical intervention and number of fused segments should be minimized (particularly in dorsal spine) to avoid complications such as iatrogenic short stature, crankshaft deformity, and restricted growth of the rib cage causing pulmonary hypoplasia. Younger patients exhibit a more aggressive form of TB, with severe extra-pulmonary involvement and progressive VB collapse13, placing them at a higher risk for disabling complications in comparison to adults. So we performed surgery which halted progression of kyphotic deformity and improved neurological symptoms in our patient. The surgical technique of choice for spinal TB has been a matter of continuous debate16. Posterior-only surgical approaches in these cases had unfavorable outcomes because they were usually limited to laminectomy with or without fusion but spinal cord compression is located anteriorly17. In our patient, we performed extensive surgery with vertebral column reconstruction with an anterior titanium cage and posterior instrumentation extending from 2 levels above and 2 levels below the lesion, even in the setting of acute infection which resulted in debridement of infectious focus and a reduced and stabilized kyphotic deformity. Our patient represents one of the few young patients treated with a single-stage, 360 vertebral column reconstruction with an anterior titanium cage and posterior pedicle screw fixation through posterior only approach. At follow-up, our patient’s neurological examination and kyphotic deformity were stable. However, she needs to be followed for the next several years, given her young age and skeletal immaturity, to check for development of complications.
Conclusion
Pott’s disease with spinal cord compression in children is very uncommon. Various treatment options may be considered. We report the successful use of single-stage, 360 vertebral column reconstruction with an anterior titanium cage and posterior pedicle screw fixation through posterior only approach to reconstruct a 9-year-old child’s vertebral column for radical removal of the infectious TB focus and reduction of the kyphotic deformity. Although limited number of literature is available, surgical debridement and spinal fusion via posterior approach appear to provide a safe alternative to conservative treatment with prolonged bed rest.
DECLARATIONS
Authors Contributions:
Conception, Diagnosis and Design, Radiological Diagnosis and Final approval of manuscript:
Dr KM Tarikul Islam, Dr Md Rezaul Amin, Dr Md Ataur Rahman, Dr. Shamsul Alam, Prof. Moududul Haque
Manuscript Preparation, Technical Revision, and Manuscript editing and revision:
Dr KM Tarikul Islam, Dr Md Rezaul Amin, Dr Md Ataur Rahman,
Literature Review: Dr. Md. Rezaul Amin, Dr. Ataur Rahman
ACKNOWLEDGEMENTS: None
FUNDING SUPPORT AND SPONSORSHIP: This research didn’t receive any specific grant from funding agencies in public, commercial or not for profit sector.
CONFLICT OF INTEREST: There are no conflict of interest.
#360° spinal fixation#Pott’s disease#Posterior only approach#Childhood spinal TB#Spinal instrumentation#Journal of Clinical Case Reports Medical Images and Health Sciences.#jcrmhs
0 notes
Text

#tw blood#cw blood#tropical's art#digital art#Messy eater type beat#Though I suppose the meat is the main course so#Perhaps the blood is more like an inconvenience#But the guy likes blood#So messy eater is it#art#The red does look nice on him though#This is basically a redraw of that one Jerma image#I found it on the interwebs as one does#Hopefully this guy avoided the spinal cord and the brain when eating#Though that doesn't really matter for it#I don't think it can catch any disease#Let alone prion diseases#So he can chow down on any part of the body#I wonder what human tarp would even taste like#Or compare to cow tarp or goat tarp#Anyways what am I talking about in these tags#This isn't even a serious drawing#Eh who cares
0 notes
Text
Discover the benefits, pricing, and preparation tips for MRI whole spine screening at Usmanpura Imaging Centre. Learn what to expect during the procedure and how it can help detect spinal issues early.
#MRI#MRI whole spine screening#benefits of MRI screening#MRI screening price#preparing for MRI screening#Usmanpura Imaging Centre#spinal health imaging#MRI procedure expectations#MRI diagnostic imaging#affordable MRI screening#comprehensive spine MRI#diagnosis#usmanpuraimaging#mri scan
1 note
·
View note
Text

The commonly seen congenital disorders are:
1. Down Syndrome:
• Cause: Trisomy 21 during conception, linked to maternal age.
• Characteristics: Includes musculoskeletal issues, thyroid dysfunction.
• Diagnosis: Non-invasive prenatal testing, genetic screening.
• Treatment: Personalized healthcare with early intervention.
2. Cleft Lip and Palate:
• Cause: Genetic predisposition, environmental factors.
• Characteristics: Encompasses visible and psychological aspects.
• Diagnosis: Improved prenatal diagnoses through imaging, genetic testing.
• Treatment: Surgical correction, ongoing regenerative medicine research.
3. Congenital Heart Defects:
• Cause: Genetic, environmental factors, maternal influences.
• Characteristics: Examines neurodevelopment, overall quality of life.
• Diagnosis: AI and machine learning for early detection.
• Treatment: Beyond surgery, regenerative therapies, precision medicine.
4. Neural Tube Defects:
• Cause: Genetics, maternal nutrition, environmental factors.
• Characteristics: Focus on long-term neurological impacts.
• Diagnosis: Advanced imaging, molecular diagnostics.
• Treatment: Surgical interventions, neuroregenerative approaches.
5. Cystic Fibrosis:
• Cause: Complex genetic mutations, cellular mechanisms.
• Characteristics: Beyond respiratory, digestive impacts, considers psychological, nutritional aspects.
• Diagnosis: Precision medicine, advanced genetic testing.
• Treatment: Gene therapies, targeted medications advancements.
6. Sickle Cell Anemia:
• Cause: Genetic, molecular intricacies.
• Characteristics: Examines long-term impacts beyond clinical manifestations.
• Diagnosis: Early detection through genetic testing, newborn screening.
• Treatment: Exciting prospects with gene-editing technologies.
7. Hemophilia:
• Cause: Genetic, molecular underpinnings.
• Characteristics: Broader impact on joint health, quality of life.
• Diagnosis: Precision enhanced by molecular profiling.
• Treatment: Beyond clotting factor replacement, explores gene therapies.
8. Muscular Dystrophy:
• Cause: Specific genetic mutations associated with different forms.
• Characteristics: Progression impacts respiratory function, cardiac health.
• Diagnosis: Advanced imaging, molecular diagnostics.
• Treatment: Research into gene therapies, exon-skipping, pharmacological approaches.
9. Spinal Muscular Atrophy:
• Cause: Genetic intricacies, modifier genes, environmental influences.
• Characteristics: Beyond motor deficits, impact on respiratory function.
• Diagnosis: Advances in genetic testing, newborn screening.
• Treatment: Evolving landscape with gene-targeted therapies.
10. Williams Syndrome:
• Cause: Genetic deletions, insights into neurodevelopment.
• Characteristics: Encompasses delays, facial features, cognitive strengths/challenges.
• Diagnosis: Advanced genetic testing for accurate, early diagnoses.
• Treatment: Tailored education, early intervention, cardiovascular management.
Early diagnosis of the above conditions can be made with the help of regular full body health checkups for your child. You can opt for a full body health checkup at Indraprastha Apollo Hospitals in New Delhi, which is regarded to be one of the finest hospitals in Delhi.
#congenital disorders#down syndrome#muscular dystrophy#williams syndrome#cystic fibrosis#spinal muscular atrophy#hemophilia#sickle cell anemia#neural tube defects#congenital heart defects#cleft lip#cleft palate#genetic testing#newborn screening#imaging tests#full body health checkup#regular health checkups#health checkup packages
1 note
·
View note
Text
How does one determine the cause of lower back pain using anatomy?
Lower back pain is a common complaint that can have various causes. The human spine is a complex structure, consisting of bones, joints, ligaments, muscles, and nerves. Therefore, diagnosing the exact cause of lower back pain can be challenging, but an understanding of the anatomy of the lower back can help. Continue reading Untitled

View On WordPress
#Anatomy#diagnostic imaging#facet joint dysfunction#herniated disc#intervertebral discs#lower back pain#lumbar spine#muscles#nerves#osteoarthritis#physical examination#sciatica#spinal stenosis#spondylolisthesis#treatment options
0 notes
Link
0 notes
Link
0 notes