#rural telehealth
Explore tagged Tumblr posts
Text
AN OPEN LETTER to THE U.S. CONGRESS
Fund the Affordable Connectivity Program NOW!
130 so far! Help us get to 250 signers!
I’m a concerned constituent writing to urge you to fund the Affordable Connectivity Program or ACP. Digital connectivity is a basic necessity in our modern world and the internet must be treated as a public utility. We use the internet to apply for jobs, perform our jobs, receive telehealth medical treatment, and pay bills, and students use it to complete homework assignments. But for millions of people in rural and urban areas, and Tribal communities, the internet is a luxury they cannot afford. Failure by Congress to fund this program will force millions of households already on tight budgets to choose between being able to stay online or potentially losing access to this essential service. If Congress doesn’t act fast, funding for the Affordable Connectivity Program will run out and more than 22 million Americans -- 1 in 6 households -- will lose this vital service. The implications of this will be devastating. In 2019, 18% of Native people living on Tribal land had no internet access; 33% relied on cell phone service for the internet; and 39% had spotty or no connection to the internet at home on their smart phone. The ACP has enrolled 320,000 households on Tribal lands -- important progress. The largest percentage gains in broadband access are in rural areas. Nearly half of military families are enrolled in ACP, as are one in four African American and Latino households. Losing access and training on using computers and the internet will have devastating impacts on all these communities as technology becomes increasingly integral to work, education, health, and our everyday lives. Without moves to address tech inequality, low-income communities and communities of color are heading towards an “unemployment abyss.” The Affordable Connectivity Program has broad bipartisan support because it is working. As your constituent, I am urging you to push for renewed funding for the ACP before it runs out in the coming weeks.
▶ Created on April 11 by Jess Craven
📱 Text SIGN PJXULY to 50409
🤯 Liked it? Text FOLLOW JESSCRAVEN101 to 50409
#JESSCRAVEN101#PJXULY#resistbot#petition#Affordable Connectivity Program#Digital Divide#Internet Access#Broadband Access#ACP Funding#Congress Funding#Public Utility#Internet Equality#Telehealth#Telemedicine#Internet Inequality#Digital Inclusion#Internet For All#Rural Connectivity#Bipartisan Support#Internet Infrastructure#FCC#ACP Support#Digital Navigation#Online Education#Remote Work#Job Access#Telecommunications#Internet Service#Internet Affordability#Digital Equity
4 notes
·
View notes
Text
Virtual Doctor Care: Bridging Gaps in Rural Healthcare

Virtual doctor care bridges gaps in rural healthcare by providing remote access to medical services. Residents in remote areas can connect with healthcare providers via telemedicine, receiving diagnoses, treatment plans, and prescriptions without needing to travel long distances. This improves healthcare access, reduces wait times, and addresses shortages of healthcare professionals in rural areas, ultimately enhancing health outcomes and patient satisfaction in underserved communities.
0 notes
Text
The Crucial Importance of 100 Mbps Download and 20 Mbps Upload Speeds in Rural Areas

In the digital age, the need for high-speed internet has become increasingly important, and rural areas are no exception to this rule. Access to the internet is not just a convenience; it’s a necessity for various aspects of life, including education, healthcare, business, and overall quality of life. In this blog post, we’ll delve into why having internet speeds of at least 100 Mbps download and 20 Mbps upload is crucial for rural communities.
Educational Advancements
Online Learning: The advent of online learning has transformed education, enabling students of all ages to access a wealth of educational resources from the comfort of their homes. A high-speed internet connection is a prerequisite for seamless participation in online classes and accessing educational materials. In rural areas, where traditional educational resources are often limited, these high-speed connections are a lifeline for students.
Interactive Learning: High-speed internet fosters interactive and engaging learning experiences. Students can join video conferences, participate in virtual labs, and collaborate with peers, all of which require robust upload and download speeds. A 100 Mbps download speed ensures that students can stream educational content without buffering, while a 20 Mbps upload speed supports their ability to actively participate in virtual classrooms.
Healthcare Access
Telehealth Services: In rural areas, access to healthcare services can be challenging due to geographical distances and limited healthcare facilities. Telehealth services bridge this gap by allowing individuals to consult with healthcare professionals remotely. A 100 Mbps download speed ensures clear, uninterrupted video consultations, while a 20 Mbps upload speed facilitates seamless communication with medical professionals.
Medical Data Transfer: Fast and reliable internet connections are essential for the transfer of medical records and data. Whether it’s sharing diagnostic images, patient history, or test results, a 20 Mbps upload speed ensures that healthcare providers can access and transmit critical information efficiently, leading to better patient care.
Economic Opportunities
Remote Work: The ability to work remotely has become a standard practice in many industries. High-speed internet empowers individuals in rural areas to take advantage of remote work opportunities, reducing the need to relocate to urban centers for employment. A 100 Mbps download speed guarantees that they can participate in virtual meetings and handle data-intensive tasks, while a 20 Mbps upload speed enables them to contribute effectively to their teams.
Business Growth: Rural businesses also benefit from fast internet speeds. A 100 Mbps download speed allows them to reach a wider customer base, access cloud services, and run e-commerce platforms efficiently. Moreover, a 20 Mbps upload speed supports seamless online communication and data sharing, helping rural businesses expand and thrive.
Quality of Life
Entertainment and Communication: Fast internet enhances the overall quality of life in rural areas. It allows residents to stream high-definition content, connect with loved ones through video calls, and enjoy the conveniences of smart home technologies, just like their urban counterparts.
In conclusion, high-speed internet with 100 Mbps download and 20 Mbps upload speeds is not merely a luxury but a necessity in rural areas. It’s the linchpin for educational advancement, improved healthcare access, economic opportunities, and an enhanced quality of life. As rural communities continue to thrive and evolve, these speeds are vital to ensure they are not left behind in our increasingly interconnected world.
Checkout more topics — https://isprevolution.io/blog/
#remote work#highspeedinternet#rural communities#education#telehealth#businessgrowth#quality of life#DigitalAdvancements
0 notes
Text
Top 4 Nursing Technologies Used Today

Nursing technologies being used now days are on a different level then the last 10 years or so. The healthcare industry has been transformed by technology in recent years. With advances in areas such as telemedicine, wearable, and electronic health records (EHRs) is leading to significant improvements. These improvements can be seen in patient care, clinical workflows, and data management. Other than this technology also changed the common practices used for teaching nurses. In this blog post, we'll explore some of the top 4 nursing technology used today.
Electronic Health Records (EHRs)
An electronic health record is a standardized collection of patient and population health data that has been digitally saved. EHRs have become a standard in healthcare and nursing practice. This enables nurses to access and update patient data in real-time, improving care coordination, patient safety, and clinical decision-making. EHRs also facilitate the use of data analytics to identify trends and patterns in patient data, leading to more personalized and effective treatment plans.
Wearable Devices
Patients are increasingly using wearable technology, such smart watches and fitness trackers, and nurses are now using it to keep tabs on patients' vital signs and health. Wearable can assist nurses in seeing early warning indications of health issues, monitoring patients' progress, and giving patients real-time feedback on their dietary and exercise habits. In addition to enhancing patient outcomes and satisfaction, wearable technology can support patient engagement and self-management.
Telehealth
In nursing practice, telehealth centers has become a crucial tool, especially during the COVID-19 epidemic. Nurses may consult with patients remotely, keep track of their health, and give information and support to patients and their families thanks to telehealth. Patients who may be unable to travel or who reside in under-served areas now have more access to healthcare services because to telehealth. Telehealth has also contributed to lower medical expenses and better patient outcomes.
Simulation Technology
Nursing students may receive practical experience in a secure and regulated setting thanks to the growing use of simulation technology in nursing education. They can strengthen their clinical skills, decision-making abilities, and collaboration via the use of simulation technology, which can model a variety of clinical settings. Nursing teachers may evaluate students' clinical competence and offer comments for development thanks to simulation technologies.
Nursing technology is rapidly advancing, and it has the potential to transform the nursing profession in many ways. From EHRs and wearable to telehealth and simulation technology, the latest advances in nursing technology are helping nurses to provide more personalized, efficient, and effective care to patients. As technology continues to evolve, it will be important for nurses to stay up-to-date with the latest trends and adopt new technologies that can improve patient outcomes and drive nursing practice forward.
0 notes
Text
After Mississippi banned his hormone shots, an 8-hour journey
Katie had done all she could to prepare for this trip. She’d asked a relative to pick up her two younger boys from school. She’d researched how to change a tire, and she’d spent hours on Google Maps, searching for the closest Walgreens in Alabama. She’d finally found a destination in Thomasville, a rural town nearly 200 miles from their suburban Mississippi home, but much remained unclear. Would they make it by noon for Ray’s telehealth appointment? Would the pharmacy give him testosterone?
Katie looked at her boy, a thin 17-year-old with wavy hair and an easy grin, and she asked herself the question that had begun to matter least: Was she breaking the law?
Two months earlier, Mississippi had banned transgender young people, like Ray, from accessing hormones or other gender-transition treatments. By mid-spring, nearly half the country had passed similar bills, according to the Movement Advancement Project, and now, 1 in 3 trans children lives in a state with a ban. Conservative lawmakers said they’d pushed the bills to protect young people, but Katie felt like they’d done the opposite. Testosterone had allowed her son to embody himself for the first time. Ray was present, happy. The ban would take that happiness away.
Across the country, families were doing everything they could to protect their trans children. Some uprooted their lives in red states for the promise of protections in blue ones. Others filed lawsuits. Katie couldn’t afford to move, and she needed a solution faster than the courts could offer, so she’d settled on a cheaper, quicker plan: She’d take a day off from her nursing job, and she and Ray would travel out of state for his medical care.
No one should have to go to these lengths just to access what is essentially basic life-saving heath care.
Also, major shout out to QMed and Dr. Lowell and the Southern Trans Youth Emergency Project for the work that they are doing to help trans youth and adults in red states access gender affirming care.
#trans#trans healthcare bans#trans healthcare#gender affirming hormone therapy#gender affirming healthcare#gaht#transgender#trans rights#trans rights are human rights#protect trans lives#protect trans youth
442 notes
·
View notes
Text
MedAI by Tech4Biz Solutions: Pioneering Next-Gen Medical Technologies

The healthcare industry is undergoing a seismic shift as advanced technologies continue to transform the way care is delivered. MedAI by Tech4Biz Solutions is at the forefront of this revolution, leveraging artificial intelligence and cutting-edge tools to develop next-generation medical solutions. By enhancing diagnostics, personalizing patient care, and streamlining operations, MedAI is empowering healthcare providers to deliver better outcomes.
1. AI-Driven Medical Insights
MedAI harnesses the power of artificial intelligence to analyze complex medical data and generate actionable insights. Its advanced algorithms can detect anomalies, predict disease progression, and recommend treatment pathways with unprecedented accuracy.
Case Study: A large medical center integrated MedAI’s diagnostic platform, leading to:
Faster identification of rare conditions.
A 30% reduction in misdiagnoses.
Enhanced clinician confidence in treatment decisions.
These capabilities underscore MedAI’s role in advancing clinical decision-making.
2. Personalized Patient Care
Personalization is key to modern healthcare, and MedAI’s data-driven approach ensures treatment plans are tailored to individual needs. By analyzing patient histories, lifestyle factors, and genetic data, MedAI offers more targeted and effective interventions.
Example: A chronic disease management clinic used MedAI to create personalized care plans, resulting in:
Improved medication adherence.
Decreased hospital readmission rates.
Greater patient satisfaction and engagement.
MedAI’s solutions allow providers to offer more precise, patient-centered care.
3. Enhanced Operational Efficiency
MedAI goes beyond clinical improvements by optimizing healthcare operations. Its automation tools reduce administrative burdens, freeing healthcare professionals to focus on patient care.
Insight: A regional hospital implemented MedAI’s workflow automation system, achieving:
A 40% reduction in administrative errors.
Faster patient registration and billing processes.
Streamlined appointment scheduling.
These improvements enhance overall operational efficiency and patient experiences.
4. Advanced Predictive Analytics
Predictive analytics play a vital role in preventive care. MedAI’s algorithms identify patients at high risk of developing chronic conditions, enabling early interventions.
Case Study: A primary care network used MedAI’s predictive models to monitor high-risk patients, leading to:
Early lifestyle adjustments and medical interventions.
A 25% drop in emergency room visits.
Higher enrollment in wellness programs.
By shifting to proactive care, MedAI helps reduce healthcare costs and improve long-term outcomes.
5. Revolutionizing Telemedicine
The rise of telemedicine has been accelerated by MedAI’s AI-powered virtual care solutions. These tools enhance remote consultations by providing real-time patient insights and symptom analysis.
Example: A telehealth provider adopted MedAI’s platform and reported:
Improved diagnostic accuracy during virtual visits.
Reduced wait times for consultations.
Increased access to care for rural and underserved populations.
MedAI’s telemedicine tools ensure equitable, high-quality virtual care for all.
6. Streamlining Drug Development
MedAI accelerates the drug discovery process by analyzing clinical trial data and simulating drug interactions. Its AI models help identify promising compounds faster and improve trial success rates.
Case Study: A pharmaceutical company partnered with MedAI to enhance its drug development process, achieving:
Faster identification of viable drug candidates.
Shorter trial durations.
Reduced costs associated with trial phases.
These innovations are driving faster development of life-saving medications.
7. Natural Language Processing for Clinical Data
MedAI’s natural language processing (NLP) capabilities extract insights from unstructured medical data, such as physician notes and discharge summaries. This allows for faster retrieval of vital patient information.
Insight: A healthcare system implemented MedAI’s NLP engine and experienced:
Improved documentation accuracy.
Quicker clinical decision-making.
Enhanced risk assessment for high-priority cases.
By automating data extraction, MedAI reduces clinician workloads and improves care quality.
8. Robust Data Security and Compliance
Data security is paramount in healthcare. MedAI employs advanced encryption, threat monitoring, and regulatory compliance measures to safeguard patient information.
Example: A hospital using MedAI’s security solutions reported:
Early detection of potential data breaches.
Full compliance with healthcare privacy regulations.
Increased patient trust and confidence in data protection.
MedAI ensures that sensitive medical data remains secure in an evolving digital landscape.
Conclusion
MedAI by Tech4Biz Solutions is redefining healthcare through its pioneering medical technologies. By delivering AI-driven insights, personalized care, operational efficiency, and robust security, MedAI empowers healthcare providers to navigate the future of medicine with confidence.
As healthcare continues to evolve, MedAI remains a trailblazer, driving innovation that transforms patient care and outcomes. Explore MedAI’s comprehensive solutions today and discover the next frontier of medical excellence.
For More Reachout :https://medai.tech4bizsolutions.com/
3 notes
·
View notes
Text
No. 46 - Royal Flying Doctor Service

In contravention of my normal operating procedures I've fast-tracked this request to the front of my queue because of how fantastically timed it is. It was requested the day my BermudAir post went up, and the moment I saw it I realized I was going to publish it as the next entry on this blog, because I want to highlight something really important and really positive about aviation. So thank you @alionessespride for the impetus to discuss why aviation is genuinely indispensable, regardless of what cynical things people might use it for.
My most recent post on BermudAir is definitely a major downer, and other posts I've done, like my David Neeleman special and various other assorted brief allusions, have been really distinctly pessimistic and jaded about the motivations of airlines. Which I don't regret or think is bad or wrong - these are very omnipresent specters in the airline industry, which is inherently more than a little predatory both due to its necessity for profit and its very heavy ties to the military-industrial complex, with airlines, governments, and manufacturers ending up in elaborate daisy chains of sweetheart deals and making money being sort of incompatible with anything I'd consider a virtue.
But I went on about this in my Neeleman post and sort of alluded to it with BermudAir as well - aviation isn't just that, and it's really hugely important. In addition to the sheer fact that people who live on islands or in remote places with poor infrastructure can easily access the rest of the world, aviation provides a lot of important services - weather research/surveillance, aerial firefighting, aerial inspection of things like power lines, agricultural work, greatly increasing the speed and thoroughness of search and rescue, and of course air medical services.
If you live in a major city you probably get a handful of ambient helicopters (I've been told a lot of people find them annoying because they tend to fly quite low), and if you've ever wondered what they are, they're probably medevac helicopters. There's a chance they're news, or private helicopters, or something else, but most of the time they're there to airlift people to hospitals if their condition is too dire to wait for the length of time an ambulance would take to get them to the trauma center, and a helicopter can easily land in a small, precise area and bring them there.
Which is all well and good, but that's for large cities. But most of the world actually isn't large cities. Case in point: most of Australia is borderline empty.
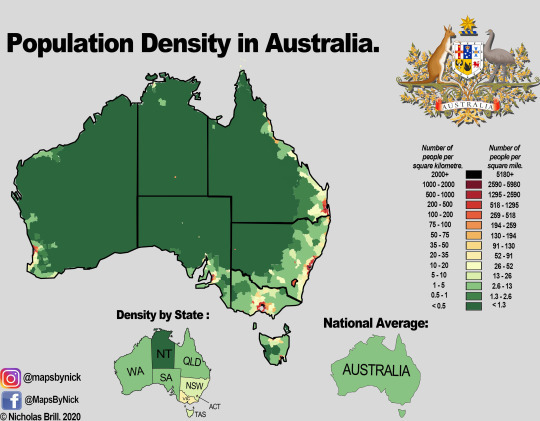
Most of Australia is on par with places like Alaska. While it's overall the fourth least dense country in the world, that density is wildly skewed and the best thing I can say for the dark green section is that it's still denser than Greenland, but not denser than Mongolia. Safe to say you aren't getting an ambulance if you live in there. So what if you have an acute medical problem which needs immediate attention to prevent your death?
The Royal Flying Doctor Service (RFDS) is probably the best-known aeromedical service. It was the first such organization, nearly 100 years old, established in 1928. They provide medical services, particularly in medical emergencies, to the parts of Australia where getting someone to a hospital would probably otherwise take days. They also provide telehealth services, transfer of patients between hospitals, and transport general practitioners to places which lack access to primary care, among other things.
The initial ask requesting them outlined a lot of this:
RFDS is an absolute lifeline in rural, regional, and remote Australia, staffed with flight doctors and nurses that fly out 24/7/365. Often they land on runways that are actually just roads or dirt strips, sometimes with the runway lit up for a night landing with rolls of toilet paper dipped in kerosene and lit on fire. They move patients that may be many many hours from any medical service, as first responders to an incident or as a medical evacuation service for small hospitals to big city hospitals.

It takes a special kind of skill to land a plane somewhere like this, and an even more special kind of skill to do paramedic work while someone is landing the plane you're in somewhere like this.
While initially RFDS just rented their airplanes and pilots from Qantas, these days they have their own fleet and pilots, and while it's hard to find exact numbers because of their several regional branches their planes number in the triple-digits and are mostly small-to-medium and capable of operation on very short, poorly-equipped airstrips (STOL). The most-used models are the Pilatus PC-12 turboprop, Pilatus PC-24 very light jet, and Beechcraft King Air 200 twin-turboprop.
They have a couple of different liveries, presumably varying by time and branch, so I'm going to stick with one I think is both more visibly distinct and more current.

Here's a fairly standard example of this livery. The 7NEWS sticker is, I believe, a sponsor - there are different ones on different planes. As you can see, the livery is primarily red, white, and blue, which I suppose is fair enough for a non-profit service in a country with a flag based on the Union Jack, though I still find it a bit of a pedestrian choice. That said, it's at least quite an ambulancey color scheme, though it's missing giant strobe lights and a siren. I think you could install those on a plane (I mean, strobe lights are actually mandatory, just not that type) but I feel like you also shouldn't, and this is better.

Here's a view from below, so you can see the clear and bright underside with RFDS emblazoned very visibly on it. Being easy to spot and identify is a broadly desirable trait in an emergency medical vehicle, and I love their specific choice in shade of fire-engine red. Note also the suspension on the landing gear and the weather radar on the wing facing towards the camera. The PC-12 is an incredibly designed aircraft which is popular for good reason, and is very well-suited to exactly what the RFDS is doing.

The white is used in a very interesting way, where the transition between it being a dividing line separating red from blue and the main body of the aircraft with the blue as just a swash is very very subtle, and the taper of the red is extremely well-executed. The red underside is excellent because it specifically prevents the blue and white from blending in with the sky, which wouldn't be ideal.
The Royal Flying Doctor Service and/or RFDS name is placed in three distinct places - the underside, the rudder, and above the windows. My gripe is that I wish they were a little bigger and more visible, I think. I'm not sure about the rudder, but I think a relatively easy fix would be to make the text above the windows bold and red - perhaps they just wanted to sequester the red fully to the bottom of the plane rather than having it on both sides of the blue, which I understand but don't think I fully endorse.

Another great view of how the red tapers, though, and the blue's termination just below the nose, far enough back that the end is still clearly visible behind the propeller. I've always felt like PC-12s (and similar single-prop aircraft but for some reason especially the PC-12) look like they have a moustache, and this adds a pair of whiskers. I enjoy that.

Admittedly, with the painted nacelles on the King Air something about it can begin to get a little...plastic-looking, I don't have any way to word it better. The blue in general isn't my favorite - unlike the saturated red's strikingness, it just sort of looks over-saturated in a way that I dislike. I'm not sure what would fix this. Maybe a darker blue?

Now, the RFDS's livery is by far the least worth-discussing thing about them. The service that they provide goes way beyond appearances, and because of that and because of the fact that designing liveries for smaller planes like this begins to get difficult I'm going to not be as harsh to them as I would other subjects. I'm just not really going to take into account the fact that this is a pretty generic scheme, because that's fine, there's no reason to care. My main takeaways are that the placement of the colors is quite well-executed, and that I wish the wordmark on the main fuselage body was more distinct. In photographs it's honestly downright illegible, and the text on the rudder doesn't exactly pop out either. The tailfin, in general, looks a little cluttered, like they didn't want to leave it empty but couldn't figure out what to do with it - the RFDS text doesn't even appear centered. But at the very least it's visible, which is crucial for an air ambulance service. Maybe I wish there was less white, but there's enough red and blue, and it's bright enough, so it's done its job.
That said, I'm giving them a C.

This is exactly what I expect of them. They've done a completely adequate job, and probably in a roundabout way it's good they've been spending their money on things that aren't genius graphic design. So if you have anything to take away from this post, don't have it be the grade, or even the fact that the Pilatus PC-12 is a really fantastic airplane - have it be the fact that aviation isn't just airline startups and massive conglomerates, and that it literally saves lives and provides services that we city-dwellers take for granted to people who would otherwise have to go without.

#tarmac fashion week#grade: c#region: oceania#region: australia#era: 2010s#era: 2020s#(earliest use of this livery I could find was 2013 but I'm sure it's older)#royal flying doctor service#non airline liveries#requests
26 notes
·
View notes
Text
This infographic from NIHCM addresses barriers to health care for Americans in rural areas: https://nihcm.org/publications/rural-health-addressing-barriers-to-care
17 notes
·
View notes
Text
The North Star of communications policy should be to make services faster, better, and cheaper for all. Yet, next year, about 50 million Americans could find that their access to the core communications service of our time—broadband—has become slower, worse, and more expensive, with many even likely to be disconnected. That shift would constitute the biggest step any country has ever taken to widen, rather than close, its digital divide.
The reason for the potential debacle? The Affordable Connectivity Program (ACP), which provides a $30 per month subsidy for broadband to over 16 million households (with the number continuing to grow) will run out of funds.
Congress established the ACP in the Infrastructure Investment and Jobs Act (IIJA) of 2021. That law correctly observed that “a broadband connection and digital literacy are increasingly critical to how individuals participate in the society, economy, and civic institutions of the United States; and access health care and essential services, obtain education, and build careers.”
To assure that all were connected, the law appropriated $65 billion to broadband. Congress devoted most of the funds to network deployments in unserved and underserved areas, but there was another $14.25 billion allocated to the ACP to assure that broadband would be affordable to all. The program is projected exhaust all its funds sometime in the first half of 2024.
The end of the program would be a disaster for families who generally have little savings or discretionary income and will suddenly face monthly broadband charges of $30 or more. It would also rob the broader economy of an opportunity to grow faster due to universal connectivity. As demonstrated by a 2021 study on the employment effects of subsidized broadband for low-income Americans, such programs increase employment rates and earnings of eligible individuals due to greater labor force participation and decreased probability of unemployment, with a benefit of $2,200 annually for low-income households.
Ending the program would also limit the enormous potential for savings in critical services that broadband can deliver. For example, in health care, data from Cigna Healthcare shows that patients save an average of $93 when using non-urgent virtual care instead of an in-person visit. Similarly, patients save an average of $120 when the virtual visit involves a specialist, and $141 with a virtual urgent-care clinic over an in-person one. Given that the Medicaid-eligible population and the ACP-eligible population overlap significantly, the savings for the government in assuring all can afford telehealth likely pays for itself. In addition, as Brookings Metro has previously noted, widespread broadband access also leads to improved outcomes in education, jobs, and social services, which would be lost if the ACP elapses.
The ACP’s expiration will also create problems for the Broadband Equity, Access, and Deployment (BEAD) Program—the $42.5 billion network deployment program Congress created in the IIJA. A study reviewing the ACP’s impact on BEAD concluded that it reduces the subsidy needed to incentivize providers to build in rural areas by 25% per household, writing: “The existence of ACP, which subsidizes subscriber service fees up to $360 per year, reduces the per-household subsidy required to incentivize ISP investment by $500, generating benefit for the government and increasing the market attractiveness for new entrants and incumbent providers.” As the National Urban League has observed, that study demonstrates that “if Congress fails to reauthorize ACP, the federal government likely will end up overpaying for broadband deployments. As a result, the federal dollars will end up funding deployments to significantly fewer unserved and underserved homes and businesses.”
The obvious solution is for Congress to continue funding the program. That is possible, as it enjoys bipartisan support. For example, former Republican FCC Commissioner Michael O’Rielly penned an op-ed titled “A Conservative Case for the Affordable Connectivity Program.” EducationSuperhighway, a national nonprofit with the mission of closing the digital divide, identified 28 governors who have prioritized implementing the ACP, including those from deep-red states such as Alabama, Idaho, and Mississippi. And polling suggests the program is widely popular among the public, with a January poll showing a “strong bipartisan majority of voters (78 percent) support continuing the ACP, including 64 percent of Republicans, 70 percent of Independents, and 95 percent of Democrats.”
But despite the ACP’s importance and popularity, it is questionable whether the Republican-controlled House will continue funding it, given the party’s attacks on other social safety net programs.
Should ACP funding be discontinued, there are alternatives—but all come with their own concerns. The FCC could fund the program itself, through the mechanism by which it funds universal service programs. That framework, however, is already under stress from legal challenges to its constitutionality and a shrinking revenue base, which has declined by 63% in the last two decades. States could design their own programs, such as New York did by requiring providers to offer a $15 broadband service to low-income residents. But in 2021, a judge ruled that the program violates federal law. Moreover, it is questionable whether the country’s universal service ambitions are best served by a fragmented set of state programs.
The National Urban League proposed a promising alternative in its Lewis Latimer Plan for Digital Equity and Inclusion. (Disclosure: The author of this piece assisted the National Urban League in its development of the Latimer Plan and its analysis of the implications of the ACP on the BEAD program.) Noting the cost savings demonstrated through telehealth, the plan proposed allowing Medicaid to enable states to provide broadband vouchers, like what the ACP offers, to eligible persons. This is similar to the way health insurance providers offer non-medical benefits that, over time, reduce the cost of health coverage. Of course, such a plan would require an administrative process to determine if and how to proceed. But it offers an alternative that would provide a sustainable source of funding.
The ACP, like any new program, could use some incremental fixes. As a Government Accountability Office review of the program noted, the FCC could improve performance goals and measures, consumer outreach, and fraud risk management. The FCC is working to do so.
But those reforms should not take our eyes off the crisis close at hand. Two years ago, the government came together in an unusually bipartisan way to assure that all could afford the broadband service they need in their homes to fully participate in the economy and society. Since then, the importance of broadband for accessing essential services has only grown. We should make the years ahead be the ones when we finally close the digital divide—not allow it to grow even more.
2 notes
·
View notes
Text
AN OPEN LETTER to THE U.S. CONGRESS
Fund the Affordable Connectivity Program NOW!
130 so far! Help us get to 250 signers!
I’m a concerned constituent writing to urge you to fund the Affordable Connectivity Program or ACP. Digital connectivity is a basic necessity in our modern world and the internet must be treated as a public utility. We use the internet to apply for jobs, perform our jobs, receive telehealth medical treatment, and pay bills, and students use it to complete homework assignments. But for millions of people in rural and urban areas, and Tribal communities, the internet is a luxury they cannot afford. Failure by Congress to fund this program will force millions of households already on tight budgets to choose between being able to stay online or potentially losing access to this essential service. If Congress doesn’t act fast, funding for the Affordable Connectivity Program will run out and more than 22 million Americans -- 1 in 6 households -- will lose this vital service. The implications of this will be devastating. In 2019, 18% of Native people living on Tribal land had no internet access; 33% relied on cell phone service for the internet; and 39% had spotty or no connection to the internet at home on their smart phone. The ACP has enrolled 320,000 households on Tribal lands -- important progress. The largest percentage gains in broadband access are in rural areas. Nearly half of military families are enrolled in ACP, as are one in four African American and Latino households. Losing access and training on using computers and the internet will have devastating impacts on all these communities as technology becomes increasingly integral to work, education, health, and our everyday lives. Without moves to address tech inequality, low-income communities and communities of color are heading towards an “unemployment abyss.” The Affordable Connectivity Program has broad bipartisan support because it is working. As your constituent, I am urging you to push for renewed funding for the ACP before it runs out in the coming weeks.
▶ Created on April 11 by Jess Craven
📱 Text SIGN PJXULY to 50409
🤯 Liked it? Text FOLLOW JESSCRAVEN101 to 50409
lol. lmao, even
#bills#broadband#utilities#phone#phone access#no pay phones anymore#fcc#distraction politics#distraction#us politics#affordable connectivity program#acp#affordable phone#affordable price#affordable#connection#open letter#petition#closed mouths don't get fed#poverty#working class#affordable internet#services#phone service#internet services#discourse#ivys queue#boost the signal#boosting#signal boost
12K notes
·
View notes
Text
PREPARING FOR MEDICAID BUDGET CUTS: STRATEGIES FOR STATES

Introduction
With ongoing discussions in Congress about federal budget reductions, Medicaid remains at risk for funding cuts. If these cuts occur, states will need to find ways to compensate for the shortfall, potentially leading to decreased benefits, stricter eligibility requirements, and financial strain on healthcare providers. Given Medicaid’s role in supporting low-income individuals, families, and people with disabilities, significant reductions could greatly impact healthcare access and the overall system.
To navigate these challenges, states must take proactive steps to evaluate spending, explore alternative funding sources, and advocate for policy measures that protect vulnerable communities.
Potential Medicaid Cuts and Their Consequences
As a major component of federal expenditures, Medicaid is often targeted for budget reductions. Proposed changes typically include replacing the current federal matching system with block grants, capping federal contributions, or lowering federal matching rates, which would shift more financial responsibility to states. Additionally, stricter eligibility requirements, such as work mandates, could make it harder for certain individuals to qualify.
If these cuts take effect, states will be forced to either increase Medicaid spending from their own budgets or implement reductions in services, eligibility, and provider reimbursements. Given the financial constraints many states already face, these adjustments may come with significant consequences.
Effects on Healthcare Access and State Budgets
Reduced Medicaid funding would likely limit healthcare access for millions of Americans, especially those already struggling financially. Fewer people may qualify, and those who remain eligible could see a decrease in covered services. Populations relying on long-term care, mental health services, and preventive healthcare would be particularly vulnerable.
Healthcare providers that serve a large number of Medicaid patients would also feel the impact. Many hospitals and clinics already struggle with low Medicaid reimbursement rates, and further cuts could force them to scale back services, reduce patient intake, or even shut down—especially in rural and underserved areas.
The financial strain wouldn’t stop at healthcare. State governments might be forced to make difficult budgetary choices, such as cutting funding for education and infrastructure to offset Medicaid shortfalls. Some states may explore tax increases or additional fees, which could introduce new economic challenges.
How States Can Prepare
Given the uncertainty surrounding Medicaid funding, states should take proactive measures to safeguard their healthcare systems and budgets. Key strategies include:
Evaluate and Optimize Medicaid Spending
Conduct a thorough review of expenditures to identify inefficiencies.
Strengthen fraud prevention efforts and minimize improper payments.
Streamline administrative costs to maximize available resources.
Identify Alternative Funding Sources
Explore new revenue streams, such as provider taxes or health-related fees.
Expand public-private partnerships to sustain Medicaid funding.
Implement cost-saving models like value-based payments and telehealth expansion.
Invest in Preventive Care
Expand preventive healthcare initiatives to reduce long-term costs.
Support community-based health programs to improve access and efficiency.
Advocate for Policy Flexibility
Engage in federal advocacy to prevent extreme Medicaid cuts.
Push for greater state flexibility in Medicaid administration.
Defend Medicaid expansion programs to ensure continued coverage.
Strengthen Safety Nets for Affected Individuals
Expand community health centers and hospital charity care programs.
Develop state-run subsidy initiatives for those losing Medicaid eligibility.
Partner with nonprofits to maintain healthcare access for vulnerable populations.
Conclusion
Potential Medicaid budget cuts could pose serious challenges for states, healthcare providers, and millions of low-income individuals who depend on the program. While states have limited control over federal funding decisions, they can take decisive action to minimize disruption. By optimizing spending, adopting technology solutions, securing alternative funding, advocating for flexibility, and reinforcing safety nets, states can better prepare for possible reductions. Strategic planning now can make the difference between a healthcare crisis and a manageable transition. States must remain vigilant in protecting access to essential healthcare services for their most vulnerable populations.
Read more.
0 notes
Text
Top Doctor Recruitment Agencies: Find the Best Medical Talent

Introduction
Finding the ideal medical practitioners for any health institution is important. It may take time, cost a fortune, and become very complicated when employing doctors. Doctor recruitment agencies save the day in such scenarios. They understand the art of finding healthcare professionals a perfect match for the top talent in medicine, ensuring maximum satisfaction for all. But which one do you choose for your needs? We tell you all about it here.
Why Hire Doctor Recruitment Agencies?
Finding the right doctor isn't simply a matter of credentials—it's also about finding an individual who has the right culture, who is the right fit for your organization. Doctor recruitment agencies simplify all this by doing everything from finding candidates to doing initial screenings.
How Do These Agencies Operate?
These agencies are a compromise between healthcare facilities and physicians. They use databases, networking, and targeted searches to find qualified applicants. Their process typically entails:
Understanding the employer's needs
Searching for appropriate candidates
Interviewing and performing background checks
Assistance with licensing and paperwork
Top Benefit of Recruitment through Agencies
Saves Time: Agencies handle most of the recruitment process.
Access to More Talent Pool: They have pools of qualified doctors.
Expert Matching: Matching the correct person for the employer and doctor.
Prioritizing Lower Recruitment Costs: An ill choice is costly; agencies minimize the risk.
What to Look for in a Doctor Staffing Agency
Prior to using an agency, consider these:
Reputation and Client Reviews: View online reviews and client comments.
Experience within the Industry: The longer the experience, the greater the likelihood of success.
Specialization: There are agencies that specialize in specific medical specialities.
Compliance and Licensure: Ensure they comply with industry standards.
Best Doctor Staffing Agencies in the U.S.
Some of the best agencies that recruit doctors include:
Merritt Hawkins – A leader in physician recruitment.
Jackson Physician Search – Known for permanent physician placements.
CompHealth – Specialist in locum tenens and permanent placement.
B.E. Smith – Provides recruitment for healthcare leadership roles.
Global Medical Recruitment Agencies
If you need physicians from foreign countries, here are some international agencies to consider:
Global Medical Staffing
IMS Recruitment
Medacs Healthcare
Specialized Medical Recruitment Services
Others are specialized in specific niches such as:
Locum Tenens Staffing (temporary physician placement)
Telemedicine Recruiting (telehealth practitioners working remotely)
Rural and Underserved Area Recruitment
Agency Recruiting Fees
The fee is negotiable but usually 15-30% of the doctor's first-year salary. Some agencies charge a flat fee, while others charge a contingency fee.
Typical Problems and How to Tackle Them
High Demand, Low Supply: Employ agencies that have extensive networks.
Credentialing Delays: Choose agencies who assist with licence papers.
Cultural Fit Issues: Ensure that the agency has an understanding of your organisation's culture.
How to Get the Best out of a Recruitment Agency
Discuss Your Needs Openly
Be Willing to Receive Guidance
Ask Them About Their Method and Success Rate
Bargain Early
Medical Recruitment Trends
Development of Telemedicine – More jobs from home healthcare.
AI in Hiring – Agencies are using AI for better matching.
Increased Need for Experts – Shortages in certain specialties drive recruitment.
The Doctor Recruitment Agency of the Future
The industry is evolving with technology, global talent pools, and less formal hiring processes. AI and data-driven hiring will continue to shape the future of healthcare recruitment as well.
Last Word
Selecting a proper doctor recruiting agency can spell success in terms of establishing a sound medical staff. Whether a hospital seeking to fill a full-time position or a clinic in need of someone on a short-term basis, an effectively chosen agency like Alliance Recruitment Agency can eliminate the time hassle and stress from finding the right medical professional to fit into your institution. Contact us today to streamline your recruitment process and find top-tier medical talent with ease.
View source: https://allianceinternationalservices.medium.com/top-doctor-recruitment-agencies-find-the-best-medical-talent-12145015ab1c
0 notes
Text
The Rising Demand for General Practitioners in Australian Healthcare

Although the quality and accessibility of Australia’s healthcare system are well known, there are several obstacles that affect its efficacy. The increasing need for general practitioners (GPs) is one of the most urgent problems. Medical staffing companies in Australia face both possibilities and challenges as a result of this increase in demand. In order to satisfy the demands of healthcare practitioners and guarantee the best possible patient care, it is essential to comprehend these dynamics. Australia’s Current Healthcare System
The healthcare system in Australia provides comprehensive services to its residents through a combined public-private paradigm. Access to necessary medical treatments is provided by the public system, which is financed by Medicare, while individuals who choose for private health insurance have more possibilities in the private sector. Although this system guarantees a high standard of treatment, it also puts a great deal of strain on medical professionals, especially general practitioners (GPs), who are often the initial point of contact for patients.
GP demand in Australia A number of variables impact Australia’s need for general practitioners: Population Growth and Ageing: According to the Australian Bureau of Statistics, there were over 26 million people living in Australia as of 2023, with a sizable percentage of them being over 65. Because older persons often need more frequent and complex medical attention, the need for primary care services is increased by this ageing population.
Management of Chronic Illnesses: In Australia, the majority of fatalities are caused by chronic illnesses including diabetes and heart disease. More over one in four (29%) Australian individuals had cardiovascular disease, diabetes, or chronic kidney disease (CKD), according to self-reported and measured statistics from the Australian Institute of Health and Welfare . One percent (182,000) fulfilled all three requirements, and seven percent (1.2 million) had at least two. Demand is further increased by the significant reliance on GPs for the management of these illnesses.
Mental Health Services: In order to diagnose and treat mental health conditions, general practitioners are essential. The need for GP services in mental health has increased due to rising awareness and diagnostic rates. Rural and Remote Areas: Nearly 60% of Australians living in rural areas lack access to specialists in their area, while 20% of people living in remote locations lack GP services nearby, according to the Australian Institute of Health and Welfare.
Let’s understand the impact of rising GP demand on recruitment agencies.
Current Australian General Practitioner Staffing Trends
Australia’s GP hiring practices are changing to accommodate the rising demand in a number of significant ways:
Telemedicine: Especially during the COVID-19 epidemic, the use of telemedicine services has increased access to general practitioner care. In 2023, 25% of all GP consultations were telehealth consultations, which relieved some of the strain on in-person services. Incentives for Rural Practice: The government provides monetary incentives and increased Medicare rebates to general practitioners who agree to practice in underprivileged areas in order to alleviate regional disparities. The goal of these actions is to balance the distribution of medical professionals.
The Needs and Prospects of Australian Healthcare In the future, it is anticipated that Australia’s need for general practitioners would only increase. A number of changes and demands require the healthcare system to change:
Increased GP Training: A research released by the Australian Medical Association (AMA) states that by 2031–2022, Australia will have a shortfall of around 10,600 general practitioners (GPs), since the number of GPs available cannot keep up with the rising demand from the community. The demand for medical services rose by 58% in the ten years leading up to 2019 — enough to cover the workload of 10,200 full-time general practitioners. Only the equivalent of 4,200 full-time general practitioners were recruited to the workforce in the five years leading up to 2021.
Integration of Telehealth: Telehealth’s role is anticipated to grow, offering more complete treatment options and relieving pressure on conventional medical institutions. Improved Recruitment Techniques: In order to draw in and keep GPs, recruitment firms will need to use creative techniques. This entails providing work-life balance programs, career development opportunities, and competitive pay.
Key Challenges
Despite these efforts, several GP recruitment challenges in Australia persist:
Ageing Workforce: A National Library of Medicine article from The National Centre for Biotechnology Information claims that the workforce of general practitioners has gotten considerably older. It was predicted that 43% of general practitioners and 56% of specialists will have retired between 2000 and 2025, respectively. Recruiting New GPs: It is necessary to increase the appeal of general practice among recent medical graduates. This entails raising pay, offering chances for job advancement, and putting in place strong support networks. Balancing Urban and Rural Supply: Reducing the gap between urban and rural GP distribution is still a major obstacle. Ensuring fair access to healthcare requires effective policies and incentives.
How Recruiting Agencies Can Benefit from IMS People Possible
We at IMS People Possible are committed to tackling these issues with customized solutions since we recognize how difficult healthcare hiring can be. In order to guarantee that healthcare facilities have access to qualified general practitioners when needed, we offer expert offshore recruitment services for both permanent and locum tenens roles. We source competent individuals from all around the world by utilizing our vast worldwide network, guaranteeing a consistent supply of healthcare experts to suit Australia’s expanding demands.
Conclusion
There are opportunities as well as challenges associated with the growing need for general practitioners in Australian healthcare. Healthcare institutions should make sure they are prepared to satisfy patient needs by comprehending these dynamics and implementing strategic recruitment initiatives. In order to help close the gap and guarantee a strong and efficient healthcare system, IMS People Possible, your healthcare staffing partner, is dedicated to assisting these initiatives through our expert offshore recruitment services.
0 notes
Text
In case you had paywall issues or found the ads on the site made your computer crash, here's the article:
By Judy Stone
Telehealth will end on December 31 unless Congress takes urgent action to pass the Telehealth Moderniztion Act of 2024.
Before COVID, Medicare provided limited coverage for telehealth and mainly limited it to rural patients. It required them to go to a local hospital or clinic to interact with a specialist until early 2020. At the beginning of the COVID-19 pandemic, Medicare greatly expanded coverage to include patients anywhere, allowing them to access specialty care from home. Expanded services also included physical and occupational therapy, emergency department visits, and nursing facility care via telehealth. This expansion provided care to Medicare’s 64 million enrollees and broadened pre-existing access for 76 million low-income Americans on Medicaid.
It’s not just patients on Medicare/Medicaid who need to worry if this bill isn’t renewed. Private insurers often follow Medicare’s lead regarding what services they will cover.
Congress.gov summarizes the H.R. 7623 Telehealth Modernization Act of 2024 as follows: “This bill modifies requirements relating to coverage of telehealth services under Medicare.
Specifically, the bill permanently extends certain flexibilities that were initially authorized during the public health emergency relating to COVID-19. Among other things, the bill allows (1) rural health clinics and federally qualified health centers to serve as the distant site (i.e., the location of the health care practitioner); (2) the home of a beneficiary to serve as the originating site (i.e., the location of the beneficiary) for all services (rather than for only certain services); and (3) all types of practitioners to furnish telehealth services, as determined by the Centers for Medicare & Medicaid Services.”
Why Does Telehealth Matter?
Being able to access medical remotely has been a huge boon to many, particularly in rural areas or those who are disabled.
Jessica Offir, PhD, is a disabled health care advocate and social psychologist for whom telemedicine is a priority issue. She observed that a stumbling block to the renewal of the bill is that “insurance companies didn't want to pay the same amounts as they were for in-person care, but providers have been insisting on it.” She added, “Trump is also wanting to reduce Medicare & Medicaid payouts, and this is one way to make that happen, as telehealth greatly increased the healthcare access of the elderly and disabled. Take away access, and payments decrease. The only entities who benefit are insurers.”
My own family are ardent supporters of access to telemedicine. We live in western Maryland, a three-hour drive to the university hospitals in Washington/Baltimore. I’m unable to drive that far, so increasingly rely on remote services, particularly for specialties that are poorly represented in our town. If telemedicine services are cut, I will be unable to access some specialties I need. Someone drives me twice a year for in-person examinations. These increasingly feel hazardous to my health for two reasons—one is the worsening traffic and trucking on the interstate. The other is that while my family still recognizes that the COVID-19 pandemic has not ended, our providers have not. They have stopped masking and even turned off HEPA filters in exam areas and waiting rooms, leaving them abandoned and useless. I take an Aranet CO2 monitor with me everywhere and try to educate people. On one recent visit, the CO2 level went from 600 ppm when I entered the exam room, to 1704 ppm before I left! That’s a level that can make you sleepy and show poorer judgment. I explained to the physician that each breath that he took had 3.4% rebreathed air from someone else, per SN Rudnick and Don Milton’s study, popularized by David Elfstrom’s reference table. That caught his attention and recognition of his potential risk of a Covid or other respiratory tract infection.
My experience is not unique. A recent article found that more than 17 percent of older Medicare beneficiaries similarly report difficulty traveling to doctor’s offices. Those over 65 averaged about 17 contact days that year for ambulatory care. That rose to 30 contact days per year for the 14 percent of patients with ten or more chronic illnesses—a considerable time and energy burden.
Another study of cancer patients found (73.8%) rated their first telemedicine visit as good as or better than an in-person visit, and 4606 (18.9%) rated it superior. In another striking example, those who received care through telehealth with peer assistance were almost seven times more likely to be treated for hepatitis C and four times more likely to achieve viral clearance after six months.
One bit of good news is that on November 15, the U.S. Drug Enforcement Administration (DEA) and the Department of Health and Human Services (HHS) announced they will extend telemedicine flexibilities through 2025. This is an important win for access to medication in end-of-life care. More than 40,000 comments were submitted to the DEA.
Paying for telehealth is a major concern now, although there has been bipartisan support for the bill. A House Republican staffer explained that “Medicare beneficiaries are on a cliff, losing tele services after December 31 2024.” Congress is negotiating how long another extension could look like and where the funding will come from, with the two parties not yet in agreement.
There have been higher per-person costs where more telehealth is used. On the other hand, telemedicine might improve patient compliance with medications and reduce costly emergency room visits.
One can argue about relative costs, but the bottom line is that there are people behind these numbers—largely disabled, elderly and rural. There are some concerns about ensuring quality of care, but that appears to be minor.
The Action Network is encouraging people to write their Congressional representatives to urge them to pass this Telehealth Modernization Act before the end of the year. It’s the only chance of saving it. With the news of planned slashes to government spending, there is no time to waste.
As Offir reminds us, “Once again, the people who will be most harmed are the vulnerable populations that can least afford to be.”
You can contact your House representatives here, and Senators here.
Please contact your Congresspeople about this one. It's vital.
You can send an email via ResistBot here:
#telehealth#this is important#everyone can benefit#it's done so much good#write your congressperson#full article text
899 notes
·
View notes
Text
Suicide Prevention Strategies in Mental Health Care

Amidst wars in the eastern hemisphere and central part of this world, conflicts against each other have claimed a lot of lives.
But do you know, apart from wars and homicide combined, what claims most lives in a calendar year?
Well, since you’re reading this article, you probably would’ve guessed it right. According to the World Health Organisation, suicides take away the lives of 800000 individuals every year. Interestingly, a person who dies committing suicide tries to attempt it almost 20 times.
The aftermath of suicide is devastating. Some families are torn apart, communities are shaken to their core and there are individuals who suffer their loved one’s loss for their entire life. The atrocities, sufferings, and other factors might have blurred the line between life and death, but the value of life is simply priceless.
But there is hope beyond the tunnel. Every suicide is preventable. All that one needs is a hand of empathy. That is the reason why even most governments across the globe do not allow ‘euthanasia,’ even to those who might have lost all hope in life.
Furthermore, the rising cases of mental illness are widening the gaps between prevention and cause.
But as they say, ‘every black cloud has a silver lining,’ there is also one saving life with effective suicide prevention strategies, especially in mental health care.
In this blog, let’s have a look at some of the suicide prevention strategies in mental health that might help you or someone you know save their life. So let's be the hope people search for their entire lives and let’s get started!
Access & Delivery of Suicide Care
It has been observed that people before committing suicide tend to seek help but access to that help often comes from long. By streamlining care delivery and appropriate insurance coverage of mental health conditions can really make a difference.
Furthermore, it has been observed that the suicide rate in rural areas of the United States is almost twice as high as in the urban population. This can be the change, since the arrival of telehealth care delivery, provider availability in underserved areas has increased.
Along with that, independent initiatives create safer suicide care through appropriate changes.
Teach Coping & Problem-solving Skills
Suicide grows over the years due to several reasons and in mental conditions it is often due to the lack of social-emotional support. The initiation of this can be done in schools and by teaching the kids while they are young how to cope with suicide. Along with that, helping patients with problem-solving skills makes them emotionally stronger and also helps in further phases of their lives.
Supporting social-emotional learning programs can be a good way to start for someone who might find it hard to come up with a depleting mental condition. Parenting also plays a crucial role in this and investing in their family relationships can make a huge difference in helping children in being socially and emotionally stable.
Identify & Support People at Risk
There is very common perception that people with suicidal tendencies are hard to identify, but it is actually quite the contrary. All we as fellow humans need to be a little more conscious. Being observant of the people around you and rather than reacting to their crisis responding to it can go a long way in keeping those people alive and in your life.
Along with that, if you identify someone who can commit suicide, plan in advance for their safety and create a follow-up after you know that they have attempted. However, you need to be more cautious and a little proactive after someone has attempted to take their life, provide them with therapies and if possible even go with them for a session or two just to make them comfortable and to be sure.
Create Protective Environment
Living in this materialistic world, we might not notice it but we are constantly surrounded by lethal objects that could be used for killing. Whether it is office space, home, or even the very vehicle that you’re driving to school or work every day. Here it is important to create a protective environment, where access to lethal means is out of sight.
Also, create a healthy organisation with policies and culture where everyone proactively participates and helps people who are at high risk of suicide. Also, it is found that alcohol and substance abuse are some of the most common habits found in people who commit suicide. Helping people reduce this through the use of community-based policies and practices can go a long way in saving probably a lot of lives.
Lessen Harms & Prevent Future Risk
Once you know, someone has tried to take their own life or is trying to intervene, small talk can help make them change their mind. And once you make them comfortable report and message about suicide safely. This would not only lessen the harm but also prevent any future attempts of the person trying to commit suicide.
An Everyone’s Initiative
One of the major reasons for suicide has been finances and that has been seen across age groups and the world. By reducing this a drastic change in the suicide rate can be brought. Governments and families need to work towards improving household financial security and plan to stabilise housing policies to make it all work.
Conclusion
Taking care of our physical and mental health is equally important. Since one complements the other it also helps a person live, love, and laugh. Furthermore, suicide is avoidable, especially in the cases of people suffering from mental conditions. Help is needed but more than help, we need to be more human first. So, next time you see someone struggling with their mental health and always complaining about their lives, help them, you might just help them save their lives and the lives of others that they care about.
Join the Movement for Change with IMPAAKT!
0 notes
Text
How Much Does Therapy Cost in India: Affordable & Accessible Mental Health Care

Mental health care is becoming increasingly vital, and many people are now seeking therapy as a way to improve their overall well-being. One common question that arises is: How much does therapy cost in India? The good news is that therapy in India is generally very affordable, with a variety of options available to suit different budgets and needs.
Understanding the Cost Factors
Therapy costs in India depend on several factors. Here are some key points to consider:
Therapist’s Qualifications: Highly experienced or specialized therapists may charge more, while new practitioners might offer more affordable rates.
Type of Therapy: Different therapy methods such as Cognitive Behavioral Therapy (CBT), psychoanalysis, or counseling sessions can vary in price.
Session Duration: Standard sessions typically last 45–60 minutes, but some therapists may offer shorter or extended sessions based on your needs.
Location: Therapy costs can differ between metropolitan cities like Mumbai, Delhi, or Bangalore and smaller towns or rural areas.
Mode of Therapy: In-person sessions might be a bit more expensive due to overheads, while online therapy is often more cost-effective and accessible.
Average Cost Breakdown
While prices can vary, here’s a rough breakdown of what you might expect:
In-Person Therapy:
In metro cities, individual sessions can range from ₹800 to ₹2,500 per session.
In smaller cities, rates might range from ₹500 to ₹1,500.
Online Therapy:
Many online platforms offer therapy sessions starting at around ₹500 per session, with some premium services costing up to ₹2,000.
Sliding Scale Options:
Some therapists offer sliding scale fees based on income, ensuring that therapy remains accessible for those on a tight budget.
Special Packages:
Many mental health clinics and online platforms provide package deals for multiple sessions, which can help reduce the overall cost.
Affordable Options for Everyone
1. Government and NGO Initiatives
Several state-run initiatives and non-governmental organizations in India provide mental health services at subsidized rates or even for free. These services are designed to make mental health care accessible to everyone, regardless of income.
2. Online Therapy Platforms
With the rise of telehealth, online therapy has become a popular choice. These platforms not only offer flexible scheduling but also lower costs due to reduced overheads. They’re a great option if you’re looking for quality care without breaking the bank.
3. Community Clinics and University Programs
Many community clinics and educational institutions offer counseling services provided by trainee therapists under supervision. These sessions are often offered at a fraction of the cost of traditional therapy.
Why Investing in Therapy is Worth It
Investing in your mental health can lead to significant long-term benefits, including:
Improved Emotional Resilience: Therapy can help you manage stress, anxiety, and depression effectively.
Better Relationships: Learning coping mechanisms and communication strategies enhances personal and professional relationships.
Enhanced Quality of Life: With better mental health, you’re more likely to enjoy life’s daily moments and pursue your goals.
Making the Right Choice for Your Mental Health
When considering therapy, remember that cost is only one aspect. Look for a therapist or service that resonates with your personal needs and goals. Affordable does not mean low quality—many therapists in India provide excellent care at competitive prices.
By exploring the various options—from government programs and community clinics to online therapy platforms—you can find the right support without feeling burdened by high costs. Your mental well-being is a worthy investment, and the affordability of therapy in India is a step toward making quality care accessible to all.
How much does therapy cost in india?
Taking the first step towards therapy can be life-changing. If you’re feeling overwhelmed or simply need someone to talk to, explore these affordable options and prioritize your mental health today.
Contact us at +91 98047 91047 or
Let Lyfsmile help you rediscover joy and peace in your life.
#AffordableTherapy#AccessibleMentalHealth#TherapyForAll#LowCostTherapy#InvestInYourself#MentalWellness#SelfCare
0 notes