#prevention from COVID-19 infection
Explore tagged Tumblr posts
Text
youtube
Call : +917997101303 | Whatsapp : https://wa.me/917997101505 | Website : https://fidicus.com
ఈ జాగ్రత్తలు పాటిస్తే మీకు HIV ఉన్నా ఏం కాదు | Precautions for HIV Patients Treatment Cure Medicine
"Learn the essential precautions for HIV patients to maintain health and prevent transmission. In this video, we cover key tips like regular medical check-ups, staying on antiretroviral therapy (ART), safe practices to avoid infections, balanced nutrition, and mental health support. We also discuss ways to protect others through safe behaviors. Stay informed and empowered with these practical steps for better living with HIV."
Dr. Bharadwaz | HIV AIDS | Health & Fitness | Homeopathy, Medicine & Surgery | Clinical Research
#HIVPrecautions #HIVAwareness #HealthTips #HIVSupport #LivingWithHIV
#DrBharadwaz #Helseform #Fidicus #Clingenious
#ClingeniousHealth #HelseformFitness #FidicusHomeopathy #ClingeniousResearch
#FidicusHIV #HIV #AIDS #HumanImmunodeficiencyViruses #AcquiredImmuneDeficiencySyndrome
#Treatment #Cure #Prevent #Relieve #Medicine #Vaccine
#AlternativeTherapy #AdjuvantTherapy #AlternativeMedicine #AlternativeSystem
Specialty Clinic Fidicus HIV highest success with homeopathy Improve Wellness | Increase Longevity | Addresses Questions
#hiv patients#covid-19 precautions for pregnant patients#precautions for planning pregnancy with hiv#precautions for aids#hiv#precautions#hiv patients life#universal precautions against hiv#hiv infection#precautions for not spreading from one person to another#hiv prevention#hiv aids#universal precautions#universal precautions excellent#hiv preacuation#importance of screening and diagnosis for hiv#standard precautions#best universal precautions#Youtube
0 notes
Text
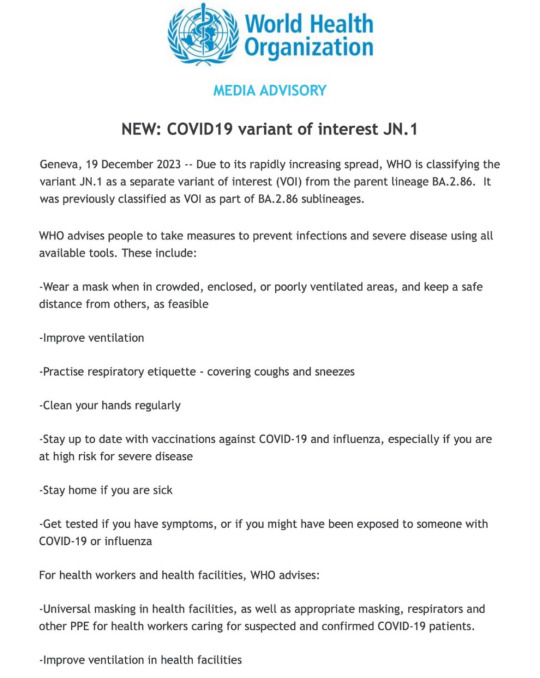
World Health Organization
MEDIA ADVISORY
NEW: COVID19 variant of interest JN.1
Geneva, 19 December 2023 -- Due to its rapidly increasing spread, WHO is classifying the variant JN.1 as a separate variant of interest (VOl) from the parent lineage BA.2.86. It was previously classified as VOl as part of BA.2.86 sublineages.
WHO advises people to take measures to prevent infections and severe disease using all available tools. These include:
-Wear a mask when in crowded, enclosed, or poorly ventilated areas, and keep a safe distance from others, as feasible
-Improve ventilation
-Practise respiratory etiquette - covering coughs and sneezes
-Clean your hands regularly
-Stay up to date with vaccinations against COVID-19 and influenza, especially if you are at high risk for severe disease
-Stay home if you are sick
-Get tested if you have symptoms, or if you might have been exposed to someone with COVID-19 or influenza
For health workers and health facilities, WHO advises:
-Universal masking in health facilities, as well as appropriate masking, respirators and other PPE for health workers caring for suspected and confirmed COVID-19 patients.
-Improve ventilation in health facilities
Image also has alt text embedded.
#WHO#health advisory#December 2023#pandemic is not over#covid#rsv#flu#please wear a mask#wear a mask#long covid#masks#ppe#n95 masks
16K notes
·
View notes
Text
CDC Recommends Multi-layered Protection Against COVID-19 as it recognises SARS-CoV-2 is a Year-round Threat
Published July 4, 2024
The US Center for Disease Control now recommends immunization, hand hygiene, clean air, isolation, treatment, face masks, social distancing and testing to prevent and protect against COVID-19 and tells the public there is no sign of SARS-CoV-2 becoming a winter virus.
In this update published on 3 July, the CDC’s National Center for Immunization and Respiratory Diseases warns the public that COVID-19 is likely to remain a year-round threat. This new official advice is at odds with the recommendations of some vocal scientists, who, without evidence, still push the line that COVID-19 will simply attenuate or weaken over time to join the many causes of the common cold, only really affects the vulnerable, or that it will become a winter bug.
The CDC’s new position is a welcome recognition of reality and an acknowledgement that those who expected SARS-CoV-2 to settle into a winter virus pattern were wrong. The advice to adopt multi-layered protection is perhaps a tacit admission that COVID-19 is taking more of a toll on public health than many people expected.
In a study recently published in Science, Peluso et al. provide compelling evidence for two potential contributors to Long Covid: persistent SARS-CoV-2 and aberrant T cell activation, both of which can be found for up to two years after acute infection.
A recent review published in Medical Review sets out the spectrum of disease pathology with COVID-19 and Long Covid and gives some clues about why we’re seeing an increase in long-term sickness and in work disability around the world.
Our recommendation remains the same, take whatever steps you can to protect you and yours from COVID-19. You can find our advice here, or download the US Center for Disease Control’s easy to follow graphic on multi-layered protection.
#covid isn't over#covid 19#covid#pandemic#wear a mask#public health#mask up#sars cov 2#coronavirus#wear a respirator#still coviding#cdc#covid-19#covid conscious#covid cautious
4K notes
·
View notes
Text
This year’s flu shot will be missing a strain of influenza it’s protected against for more than a decade.
That’s because there have been no confirmed flu cases caused by the Influenza B/Yamagata lineage since spring 2020. And the Food and Drug Administration decided this year that the strain now poses little to no threat to human health.
Scientists have concluded that widespread physical distancing and masking practiced during the early days of COVID-19 appear to have pushed B/Yamagata into oblivion.
This surprised many who study influenza, as it would be the first documented instance of a virus going extinct due to changes in human behavior, said Dr. Rebecca Wurtz, an infectious disease physician and epidemiologist at the University of Minnesota School of Public Health.
“It is such an interesting and unique story,” Wurtz said, adding that if it were not for COVID, B/Yamagata would still be circulating.
One reason COVID mitigation efforts were so effective at eliminating B/Yamagata is there was already a fair amount of immunity in the population against this strain of flu, which was also circulating at a lower level, said Dr. Kawsar Talaat, an infectious disease physician at Johns Hopkins Bloomberg School of Public Health.
In contrast, SARS-CoV-2 was a brand new virus that no one had encountered before; therefore, masking and isolation only slowed its transmission, but did not stop it.
The absence of B/Yamagata won’t change the experience of getting this year’s flu shot, which the Centers for Disease Control and Prevention recommends to everyone over 6 months old. And unvaccinated people are no less likely to get the flu, as B/Victoria and two influenza A lineages are still circulating widely and making people sick. Talaat said the disappearance of B/Yamagata doesn’t appear to have lessened the overall burden of flu, noting that the level of illness that can be attributed to any strain varies from year to year.
The CDC estimates that between 12,000 and 51,000 people die every year from influenza.
However, the manufacturing process is simplified now that the vaccine is trivalent — designed to protect against three flu viruses — instead of quadrivalent, protecting against four. That change allows more doses to be produced, said Talaat.
Ultimately, the costs of continuing to include protection against B/Yamagata in the flu shot outweigh its benefits, said Talaat.
"If you include a strain for which you don't think anybody's going to get infected into a vaccine, there are some potential risks and no potential benefits," she said. "Even though the risks might be infinitesimal, the benefits are also infinitesimal."
Scientists and public health experts have discussed for the past couple years whether to pull B/Yamagata from the flu vaccine or wait for a possible reemergence, said Kevin R. McCarthy, an assistant professor at the University of Pittsburgh's Center for Vaccine Research. But McCarthy agrees that continuing to vaccinate people against B/Yamagata does not benefit public health.
Additionally, there is a slight chance of B/Yamagata accidentally infecting the workers who manufacture the flu vaccine. The viruses, grown in eggs, are inactivated before being put into the shots: You cannot get influenza from the flu shot. But worker exposure to live B/Yamagata might occur before it's rendered harmless.
That hypothetically could lead to a reintroduction of a virus that populations have waning immunity to because B/Yamagata is no longer making people sick. While that risk is very low, McCarthy said it doesn’t make sense to produce thousands of gallons of a likely extinct virus.
It is possible that B/Yamagata continues to exist in pockets of the world that have less comprehensive flu surveillance. However, scientists aren’t worried that it is hiding in animals because humans are the only host population for B lineage flu viruses.
Scientists determined that B/Yamagata disappeared in a relatively short period of time, and this in and of itself is a success, said McCarthy. That required collaboration and data sharing from people all over the world, including countries that the U.S. has more tenuous diplomatic relationships with, like China and Russia.
“I think the fact that we can do that shows that we can get some things right,” he said.
Sarah Boden is an independent health and science journalist based in Pittsburgh.
#op#links#npr#covid#flu#influenza#public health#vaccines#flu vaccine#flu shot#flu season#b/yamagata#influenza virus#influenza b#influenza b/yamagata#masking#wear a mask#mask up#infectious diseases#disease prevention#infectious disease#illness#get vaccinated#get vaxxed#covid prevention#covid conscious#covid cautious#wear a respirator#covid realistic#viral infection
2K notes
·
View notes
Text
Long Covid Justice on COVID and LONG COVID from the mask ban teach-in
COVID/SARS-CoV-2 basics
It is NOT seasonal, like the flu is.
Spreads through air, like smoke.
The 6 feet apart rule is no longer great prevention advice.
Handwashing is a great hygiene practice, but transmission via surfaces is unlikely.
Vaccines do NOT prevent transmission. They reduce symptoms and severity for some.
You can transmit [COVID] while completely asymptomatic. Around half of transmission is as asymptomatic or presymptomatic. Everyone's immune system is different.
Being indoors increases risk of transmission, but you can still get it in crowded outdoor spaces.
What is Long Covid?
Long Covid is a set of health issues after someone has COVID-19
New health issues, ongoing issues, or worsening of previous symptoms and conditions.
It is a biological disease that affects hundreds of millions of people globally. It is a mass disabling condition and crisis.
It can cause significant disability and can be fatal.
Anyone can develop it, and up to 10% of people with COVID will.
Severity of initial infection doesn't correlate to potential to develop Long COVID.
It can be very hard to get a diagnosis and proper treatment or care for Long COVID.
Every time you get COVID infection, you increase your chances of developing Long COVID.
How do we prevent Long COVID? Layers of protection
Masking.
Air filtration.
Ventilation.
Vaccines.
Testing (right now Aug 2024, rapid tests are only about 20% reliable. Try to test two times in 24-48 hours).
Nasal sprays before and after exposure. (little data on these being effective against COVID but some are choosing to use them until more research comes out)
Mouthwashes with CPC (Cetylpyridinium Chloride) before and after exposure. (Must be used for at least 60 seconds)
2K notes
·
View notes
Text
In photos of 2023’s World Economic Forum- or Davos as it is commonly called, after the Swiss resort town where it annually occurs- you might not notice the HEPA filters. They’re in the background, unobtrusive and unremarked upon, quietly cleansing the air of viruses and bacteria. You wouldn’t know- not unless you asked- that every attendee was PCR tested before entering the forum, or that in the case of a positive test, access was automatically, electronically, revoked. And if you happened to get a glimpse of the strange blue lights overhead, you could reasonably assume that their glow was simply a modern aesthetic choice, not the calming buzz of cutting edge Far UVC technology- demonstrated to kill microbes in the air.
It’s hard to square this information with the public narrative about COVID, isn’t it? President Biden has called the pandemic “over”. The New York Times recently claimed that “the risk of Covid is similar to that of the flu” in an article about “hold outs” that are annoyingly refusing to accept continual reinfection as their “new normal”. Yet, this week the richest people in the world are taking common sense, easy- but strict- precautions to ensure they don’t catch Covid-19 at Davos.
These common sense, easy precautions include high-quality ventiliation, use of Far UVC-lighting technology, and PCR testing. You’ll also see some masks at Davos, but generally, the testing + air filtration protocol seems to be effective at preventing the kind of super-spreader events most of us are now accustomed to attending.
It seems unlikely to me that a New York Times reporter will follow the super-rich around like David Attenborough on safari, the way one of their employees did when they profiled middle-class maskers last month. I doubt they will write “family members and friends can get a little exasperated by the hyper-concern” about the assembled Prime Ministers, Presidents and CEOs in Switzerland. After all, these are important people. The kind of people who merit high-quality ventilation. The kind of people who deserve accurate tests.
Why is the media so hellbent on portraying simple, scientifically proven measures like high-quality ventilation as ridiculous and unnecessary as hundreds of people continue to die daily here in the US?
Why is the public accepting a “new normal” where we are expected to get infected over and over and over again, at work events with zero precautions, on airplanes with no masks, and at social dinners trying to approximate our 2019 normal?
We deserve better. We deserve to be #DavosSafe as the hashtag going around on twitter puts it. Your children deserve to be treated with the care that world leaders are treating each other. Your family deserves to be protected from the disease which is still- unlike the flu- the third leading cause of death in the US. We don’t deserve to be shoved back into poorly ventilated workplaces while our politicians and press assure us that only crazy people would demand to breathe clean air.
Clean water and clean food are rights we fought for; we have regulatory bodies that ensure we aren’t exposed to pathogens via our water supply nor our food. In 1854, John Snow famously conducted his Broad Street Pump study in London and demonstrated that cholera was water-bourne; however, it took decades for our public policy to catch up with our scientific knowledge.
A public health case study published by the NBCI describes the years that followed:
The first use of chlorine as a disinfectant for water facilities was in 1897 in England. The first use of this method for municipal water facilities in the United States was in Jersey City, New Jersey, and Chicago, Illinois, in 1915. Other cities followed and the use of chlorination as standard treatment for water disinfection rapidly grew. During the 20th century, death rates from waterborne diseases decreased significantly, and although other additional factors contributed to the general improvements in health (such as sanitation, improved quality of life, and nutrition), the improvement of water quality was, without doubt, a major reason.
Forty-three years passed from the initial demonstration that pathogens were being spread via water, and public action and regulation to halt disease.
Can you imagine, in the 1890s, being somebody who argued against cleaning the water?
Can you imagine, in those years of plentiful cholera, calling the people who demanded shit-free water “hold outs”?
One thing COVID realists are accused of is being “doomsayers” and “fearmongers,” so let me share a dose of optimism about the future with you. When we choose- whenever we choose- to get COVID under control, there’s an exciting new world awaiting us. One, not only without constant COVID reinfection, but where our kids can grow up free of colds, flus, RSV, and many other common bugs. And no, contrary to what you may have heard, staying healthy (shockingly enough) is not bad for children!
Once we choose to institute ventilation standards and introduce new technologies like Far UVC lighting- and embrace masking as an easy, kind, and useful tool to control outbreaks- we can bring every nasty airborne pathogen under control the way we did cholera. We didn’t have the science before; now we do. (I mean that quite literally; I can’t recommend enough the linked Wired article cataloguing the long journey to establishing that Covid is, indeed, airborne).
We face a stark choice; down one road, the one with zero infrastructure upgrades, no air quality regulations, and Covid safety only for those who can afford it, you and your family will get Covid this year. You will get Covid next year. You will continue to get Covid over and over and over again, as the health problems - like cardiac damage, viral persistance, and immune system dysfunction- continue to build up. (The billionaires, of course, will not).
Down the other road, we quite simply treat ourselves the way Davos would. We engage with what the science is telling us and we build a safer, better world for our kids. We embrace the lessons this pandemic is teaching us, and let go of things we now know are harming people. We stop clinging desperately to the idea that 2019 will come back if we just get the virus one more time, and we come together to achieve what we’ve been told is impossible: elimination.
The economic elite thrive on our divisiveness and blame casting. They don’t mind that we’re calling each other names, engaging in racial stereotyping, or leaving disabled people to die, so long as we keep their machine running. But we can choose to stop throwing blame at each other, and direct it where it belongs: at the powerful people who’ve left us to suffer, at the politicians who are whipping people into a frenzy over masks instead of over our millions of dead, at the talking heads on TV that work so hard to convince us: you want to get sick. It’s better than being a *weirdo* or a *hold out*.
We needn’t wait 43 years to redirect our energies. France and Belgium have already introduced new air quality standards, and DIY projects to build Corsi-Rosenthal boxes for schools and healthcare settings have popped up around the country. We have the science, we have the technology. All we need now is the political will and the solidarity to truly end the pandemic- the kind of solidarity the super rich always show with one another.
The billionaires at Davos don’t accept continual Covid reinfection. They demand better. It’s time we demand better too.
8K notes
·
View notes
Text
Updated vaccines against Covid-19 are coming, just as hospitalizations and deaths due to the virus are steadily ticking up again.
Today, the US Food and Drug Administration authorized new mRNA booster shots from Moderna and Pfizer, and a panel of outside experts that advises the Centers for Disease Control and Prevention voted to recommend the shots to everyone in the United States ages 6 months and older. Once Centers for Disease Control and Prevention director Mandy Cohen signs off on the recommendations and the vaccines are shipped, people can start getting the boosters.
The recommendation is projected to prevent about 400,000 hospitalizations and 40,000 deaths over the next two years, according to data presented at the meeting by CDC epidemiologist Megan Wallace.
This year’s mRNA vaccines are different from the 2022 booster in a key way. Last year’s shot was a bivalent vaccine, meaning it covered two variants: the original one that emerged in China in 2019, plus the Omicron subvariant BA.5, which was circulating during much of 2022. This fall’s booster drops the original variant, which is no longer circulating and is unlikely to return. It targets just the Omicron subvariant XBB.1.5, which was dominant throughout much of 2023.
Pfizer and Moderna’s vaccines work by introducing a tiny piece of genetic material called messenger RNA, or mRNA, that carries instructions for making SARS-CoV-2’s characteristic spike protein. Once it is injected, cells in the body use those instructions to temporarily make the spike protein. The immune system recognizes the protein as foreign and generates antibodies against it. Those antibodies stick around so that if they encounter that foreign invader again, they will mount a response against it.
Since the start of the Covid-19 pandemic, the virus has acquired new mutations in its spike protein and elsewhere. These mutations result in new variants and subvariants that diverge from the original virus. When enough mutations accumulate, these new versions can more easily evade the antibodies created by previous vaccine doses or infections.
The constantly evolving nature of the virus is the reason health regulators decided last year to update the original mRNA vaccines, which were designed against the version of the virus that first appeared in 2019. This year, once again, the virus has changed enough to warrant an updated booster.
In June, an advisory committee to the FDA recommended that this fall’s booster be a monovalent vaccine—targeting only the then-dominant XBB.1.5 subvariant.
At that meeting, committee members reviewed evidence suggesting that the inclusion of the original variant may hamper the booster’s effectiveness against newer offshoots. “The previous bivalent vaccine contained the ancestral spike and thus skewed immune responses to the old spike,” says David Ho, a professor of microbiology at Columbia University whose research, which is not yet peer-reviewed, was among the evidence the FDA panel reviewed. “This is what we call immunological imprinting, and it results in lack of immune responses to the new spike.” He thinks taking out the old variant should optimize the immune response.
But over the past few months, even newer Omicron offshoots have arrived. Currently, EG.5.1, or Eris, is the dominant one in the United States, United Kingdom, and China. Meanwhile, a variant called BA.2.86, or Pirola, has been detected in several countries. Pirola has raised alarm bells because it has more than 30 new mutations compared to XBB.1.5.
Even though the new boosters were formulated against XBB.1.5, they’re still expected to provide protection against these new variants. “The reason is, while antibodies are important in protection against mild disease, the critical part of the immune response that’s important for protecting against severe disease is T cells,” says Paul Offit, a professor of vaccinology at the University of Pennsylvania and member of the FDA’s vaccine advisory committee.
These cells are a different part of the immune response. Unlike antibodies, which neutralize a pathogen by preventing it from infecting cells, T cells work by eliminating the cells that have already been invaded and boosting creation of more antibodies. Both the Moderna and Pfizer-BioNTech Covid vaccines produce long-lasting T cells in addition to antibodies.
It’s why, Offit says, when the Omicron wave hit in late 2021 and peaked in January 2022, the US didn’t see a dramatic increase in hospitalizations and deaths even as cases rose significantly: People’s T cells kicked into gear, even when their antibodies didn’t recognize the Omicron variant.
“In some ways,” says Offit, when it comes to vaccine booster development, “it almost doesn’t matter what we pick to target” because the coronavirus has yet to evolve away from T cell recognition. “Everything works.”
Scientists think T cells are able to protect against severe Covid because they’re recognizing parts of the virus that have remained unchanged throughout the pandemic. “I suspect that as we continue to vaccinate, there are some conserved regions [of the virus],” says Jacqueline Miller, Moderna’s head of infectious diseases. “So even with the accumulation of mutations, we’re still building on previous immunity.”
People who have hybrid immunity—that is, have had a Covid infection and have also been vaccinated—seem to have the best immune responses to new variants, she says, which suggests that previous exposure shapes and improves immune responses to new variants. Preliminary studies show that antibodies generated by previous infections and vaccinations should be capable of neutralizing Pirola.
Earlier this month, Moderna issued a press release saying that clinical trial data showed that its updated booster generated a strong immune response against Pirola, as well as the more prevalent Eris variant.
In a statement to WIRED, Pfizer spokesperson Jerica Pitts said the company continues to closely monitor emerging variants and conduct tests of its updated monovalent booster against them. Data presented at Tuesday’s CDC meeting showed that Pfizer-BioNTech’s updated booster elicited a strong neutralizing antibody response against both Eris and Pirola.
The FDA expects that Covid-19 vaccines will continue to be updated on an annual basis, unless a completely new variant emerges that requires a different approach. “We will always be a little behind the virus,” says Ho. “In this instance, we won’t suffer too much, but that might not be the case going forward. Surveillance is imperative.”
813 notes
·
View notes
Text
Some recent COVID-19 news
Growing Concern for back to school as data shows rising COVID cases in B.C.
A grassroots group of health professionals are calling for British Columbia to reinstate mask mandates in schools and hospitals to prevent a repeat “tripledemic” of COVID-19, RSV and influenza infections that pushed the province’s hospitals to the brink last fall.
And with data showing rising COVID-19 cases in B.C. and two new viral subvariants on the horizon, Protect Our Province B.C. says the province should act sooner rather than later.
The group is composed of more than a dozen doctors, nurses, researchers, teachers and professionals who advocate for evidence-based pandemic policies.
“We know from last year kids and schools were hit hard and if the goal is to keep kids learning in school we need to do what we can to prevent virus spread this fall,” said Dr. Lyne Filiatrault, a retired emergency room physician in Vancouver and a member of the group.
COVID response confounds SARS expert
As COVID-19 surges globally, a leading infectious disease specialist is confounded by the lack of pandemic mitigation measures in Ontario.
Q: What is your advice for people who want to stay safe this fall?
Dr. Dick Zoutman: “One is to be informed. I do recommend Dr. Tara Moriarty’s website — COVID19resources.ca,” Zoutman said. “We owe her a large debt.”
Second, when the latest COVID-19 vaccine is available, “get it,” he recommended.
Third, “buy N95 respirators and make sure you have plenty and have one with you all the time. And when you go into an indoor public space — be it a hospital, a bank, a grocery store, school — put it on. The best ones are the ones that go around your head, because they’re tighter.”
Fourth, antigen rapid tests must be made widely available. “If you have any symptoms, you need to test and isolate yourself.”
Finally, avoid indoor public places this fall, he said. “I haven’t eaten in a restaurant in almost four years, and I don’t intend to.”
428 notes
·
View notes
Text
What is immunocompromisation?
Being immunocompromised means you have a weaker immune system than most people. There are two main ways people become immunocompromised
1. Medical Conditions
Certain medical conditions cause your immune system to be weaker. Some examples include:
Immunodeficiencies- A category of conditions causing a lower number of or lower efficacy of immune cells. This category is divided into two subcategories: primary immunodeficiency and secondary immunodeficiency. Primary immunodeficiency is a subcategory consisting of hundreds of different conditions all causing a lower number of immune cells. Secondary immunodeficiency is a smaller category consisting of conditions where a person lacks immune cells due to other causes such as malnutrition.
HIV/AIDS
Some cancers
2. Medications
There are two main types of medications that result in being immunocompromised: Immunosuppressants and chemotherapy
Immunosuppressive medications- Immunosuppressive medications are medications designed to suppress your immune response. These can work in many different ways with some targeting a broad range of immune cells and others being highly specific. These medications are often used for organ transplant recipients and people with moderate-severe autoimmune diseases. Some medications in this category include: organ transplant medications, biologics, and high dose corticosteroids
Chemotherapy- Chemotherapy often comes with the effect of preventing new fast-dividing cells from being produced. This is why hair loss is such a common side effect of chemotherapy. Immune cells are fast dividing and therefore frequently are unable to be produced while on chemotherapy
The effects of immunocompromisation
Immunocompromisation has a large range of effects depending on the reason someone is immunocompromised. The most common effects are an increased susceptibility to illness and cancers. Increased susceptibility to illness can look like:
Frequent illnesses
Illnesses that are more severe than they would be for other people
Recurrent infections
Infections that don't respond to medication
Delayed response to infection
Infections that last longer than usual
Some people are more susceptible to certain types of infections. For example anifrolumab, a biologic used for lupus, makes people more susceptible to herpes zoster and respiratory tract infections while prednisone, a corticosteroid, increases risk of infection across the board. This occurs due to different causes of immunocompromisation affecting different immune cells with different roles in preventing and responding to infection.
Grades of severity
Recently the term "moderately and severely immunocompromised" has been used in covid-19 resources. Certain factors are considered to make someone moderately or severely immunocompromised, these include:
Advanced or untreated HIV infection
Moderate or severe primary immunodeficiencies
Hematologic malignancies
Active treatment for solid tumors or hematologic malignancies
Immunosuppressant medications used for solid organ or islet transplants
CAR-T cell therapy or hematopoietic stem cell transplantation
Treatment with alkylating agents, antimetabolites, high-dose corticosteroids, chemotherapeutic agents, TNF blockers, and other biologic agents that are immunosuppressive or immunomodulatory
What immunocompromisation is not
It's worth noting that getting sick frequently or getting seriously sick from illnesses that are usually mild is a warning sign for being immunocompromised but does not inherently make you immunocompromised. Some people are just more susceptible to illness without being immunocompromised.
Having minimal response to an infection that is usually more serious is a sign of a strong immune system, not a weak one.
Being immunocompromised is also not the same as being high risk for serious infection. All immunocompromised people are high risk but not all high risk people are immunocompromised. Immunocompromisation is specifically when someone is high risk because their immune system is weak. Particularly in regards to covid, there are many conditions that make you higher risk that do not involve a weak immune system.
Autoimmune diseases do not automatically make you immunocompromised. Something being a disorder of the immune system does not mean that you are immunocompromised because immunocompromised means a weaker immune system not a malfunctioning immune system.
#someone in my notes was claiming fibromyalgia makes you immunocompromised#heres some info about what being immunocompromised actually is#chronic illness#chronically ill#cripple punk#cripplepunk#physical disability#physically disabled#immunocompromised#immunocompromisation
164 notes
·
View notes
Text

Some colorized bits from my recent free printable zine WHY WE MASK: It's Not "Just A Cold"! I purposefully made the whole thing b&w to make printing as cheap as possible, but it's fun to add color especially to the snot-splosions.
HEY COMICS FRIENDS going to SPX or other cons this weekend - MASK UP, EAT OUTDOORS, and REST if you start feeling run down. COVID-19 levels are BAD bad right now (it's currently the worst September out of the whole pandemic) and the government does not have our backs. This virus causes YEARS worth of horrible vascular, neurological, and immune system damage, and each infection raises your chances of gaining fun new disabilities that could prevent you ever making comics again.

I strongly advice cancelling festivals, cons, indoor dining, anything involving crowds indoors OR outdoors, etc. But I know people depend on income from cons, so: PACK MASKS, NASAL SPRAY, and CPC MOUTHWASH and actually use them! If you develop any COVID-19 symptoms (headaches, dizziness, nausea, stomach pain, diarrhea, sore throat, sore joints, etc) don't assume it's "just a cold". Stay in your dang hotel room and REST! You can TRY to "push through" to keep tabling but you are NOT gonna like the long-term results (aka Long COVID).

I care about all you comics people and I want you to enjoy many more decades of making and sharing and reading comics with each other. If you're feeling sick at a show this weekend and don't know what to do, drop me a line! No judgements. Take care of yourself and each other out there and remember, no one can rest your body for you but you.
(Image Descriptions are in the Alt Text. Also please feel free to print my zine and hand it out if you do go)co
#indie comics#spx 2024#covid safety#covid isnt over#sci art#sciart#graphic medicine#science illustration#covid is airborne#long covid#disability justice#disability community#queer comics#lgbtq comics#comics convention#mask up#public health#we keep us safe#workers rights#comics art#con crud#covid resources
58 notes
·
View notes
Text
"Long COVID has destroyed my life
I would love nothing more than to “finally ignore COVID,” as the headline to Dr. Ashish Jha’s July 31 op-ed reads (“With a few basic steps, most of us can finally ignore COVID”). As a healthy, vaccinated, and recently boosted 35-year-old, I did what he said: I ignored COVID-19 on a weekend trip with friends in September 2022. But the infection I got as a result has all but destroyed my life.
A week after my infection, I began to experience intense fatigue, overwhelming headaches, and cognitive challenges that continue to this day. These symptoms are debilitating: I can no longer work, socialize, or travel. My finances are dire. And if I am unable to avoid another infection, my condition may deteriorate even further.
Jha wrote of long COVID “treatments” being promising. Perhaps he could clarify what treatments he is referring to, because my doctors say that there are no approved treatments for long COVID.
A recent study funded by the NIH’s RECOVER initiative showed that 10 percent of adults infected with COVID still have symptoms six months later, even with vaccination. By downplaying the prevalence and debilitating outcomes of even moderate long COVID, Jha is signing thousands of people up to the misery and despair with which I live every day.
Ezra J. Spier
Oakland, Calif.
Another view from infectious disease doctors
As infectious disease doctors, we disagree with Dr. Jha’s contention that it is time to ignore COVID-19.
Yes, being vaccinated and taking Paxlovid thankfully decrease the risk of severe disease. But only 43 percent of people age 65 and over and only 17 percent of all Americans had received an updated COVID vaccination by May 2023, and access to Paxlovid treatment is inequitable by race and insurance status.
Long-term complications of COVID can be devastating, including after second infections.
More than half a million Americans have died since the summer of 2021, when sufficient vaccine doses were available: COVID death rates in the United States continue to be double those of Canada. Termination of free tests and “commercialization” of medications as implemented by the federal government will only widen our country’s grisly COVID-related health disparities.
Inevitably, ignoring COVID leads to ignoring the slow-motion epidemic of long COVID. Standing up against such neglect, leaders like Boston Mayor Michelle Wu and Governor Maura Healey can promote meaningful measures to protect our communities: air purification in all schools and public spaces; free COVID-preventive masks (KN95 or N95, not surgical masks); tests, vaccines, and Paxlovid for all who cannot afford to buy them; and concern for and support of long COVID victims.
Dr. Julia Koehler
Boston
Dr. Regina LaRocque
Wellesley
We remain vulnerable to long COVID
Ashish Jha’s position as former White House COVID-19 Response Coordinator is a conflict of interest masquerading as a qualification for his op-ed. Researchers who study long COVID stated in a recent paper in Nature Reviews Immunology that “the oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable.” Rapid tests, which are less accurate with recent strains while PCR tests are less available, and low death rates give a false sense of security.
I agree that despite progress, more buildings need the air filtration and ventilation that would make public life safer. But Jha omits our vulnerability to long COVID after even mild infections, its devastating effects, and higher death rates for hospital-acquired COVID-19, combined with a lack of collective protection in health care settings with unmasked, untested people who prefer to ignore COVID-19.
Aside from advocating vaccines, he describes an everyone-for-themselves approach, not mentioning responsibility to protect others or access to essentials.
Jha dines in a restaurant with his friends while patients even in leading cancer hospitals are forced into Russian roulette, thanks to this approach.
Kathryn Nichols
Cambridge
Vigilance is necessary to prevent long COVID
While I understand the desire to promote optimism amid the ongoing pandemic, I am deeply concerned about the potential consequences of downplaying the importance of COVID precautions and the significant risk of long COVID. As a person living with long COVID for the last 16 months despite being vaccinated and boosted, I have experienced post-exertional malaise, fatigue, headaches, joint and muscle pain, cognitive dysfunction, and more symptoms that have continued to today. I have tried numerous medicines, supplements, and even participated in a clinical trial, only to find limited relief from the persistent effects of this virus.
Such a stance overlooks the reality that millions more people could end up with long COVID if we fail to remain vigilant in our efforts to combat the virus. Long COVID is a devastating consequence of this virus, and we cannot rely solely on vaccinations to end the pandemic. Even with widespread vaccination, the risk of contracting long COVID remains high. A recent study funded by the NIH’s RECOVER initiative showed that 10 percent of adults infected with COVID still have symptoms six months later. Minimizing the significance of long COVID not only neglects the suffering of long-haulers but also risks undermining public health efforts to control the spread of the virus.
By raising awareness about the risk of long COVID, media outlets can play a pivotal role in educating the public and promoting continued vigilance. Responsible reporting on the enduring impact of long COVID can serve as a reminder that the pandemic is far from over and that we must remain committed to taking necessary precautions to protect ourselves and others. Highlighting the struggles of long COVID survivors and the lack of proven treatments can spur further research and medical advancements in addressing this condition. Empathy and support for those living with long COVID are essential in paving the way for better understanding, compassionate care, and better health outcomes for everyone as COVID rates increase again this summer.
Travis Hardy
Norwalk, Conn.
Link https://www.bostonglobe.com/2023/08/05/opinion/cant-ignore-long-covid-jha/
406 notes
·
View notes
Text
Also preserved on our archive
By Anthony Robledo
The side effects of newly discovered COVID-19 strain XEC might not be as severe, but is part of the more contagious variant class, experts say.
The Centers for Disease Control and Prevention (CDC) defines XEC as recombinant or hybrid of the strains KS.1.1 and KP.3.3., both from the Omicron family that became the predominant strain in the U.S. late December 2022.
The variant, which first appeared in Berlin in late June, has increasingly seen hundreds of cases in Germany, France, Denmark and Netherlands, according to a report by Australia-based data integration specialist Mike Honey.
XEC has also been reported in at least 25 U.S. states though there could be more as genetic testing is not done on every positive test, RTI International epidemiologist Joëlla W. Adams said.
"We often use what happens in Europe as a good indication of what might happen here," Adams told USA TODAY Friday. "Whenever we're entering into a season where we have multiple viruses occurring at the same time, like we're entering into flu season, that obviously complicates things."
What is the XEC variant? New COVID strain XEC is a recombinant strain of two variants in the Omicron family: KS.1.1 and KP.3.3.
The hybrid strain was first reported in Berlin late June but has spread across Europe, North America and Asia with the countries Germany, France, the Netherlands and Denmark leading cases.
Is the XEC variant more contagious? While there's no indication the XEC strain will increase the severity of virus, it could potentially become a dominant strain as Omicron variants are more contagious. However, current available COVID-19 vaccines and booster shots are particularly protective against XEC as it is a hybrid of two Omicron strains.
"These strains do have the advantage in the fact that they are more transmissible compared to other families, and so the vaccines that are currently being offered were not based off of the XEC variant, but they are related," Adams said.
Like other respiratory infections, COVID-19 and its recent Omicron variants will increasingly spread during the fall and winter seasons as students return to classes, kids spend more time inside and people visit family for the holidays, according to Adams.
How can we protect ourselves from XEC and other variants? The CDC continues to monitor the emergence of variants in the population, according to spokesperson Rosa Norman.
"At this time, we anticipate that COVID-19 treatments and vaccines will continue to work against all circulating variants," Norman said in a statement to USA TODAY. "CDC will continue to monitor the effectiveness of treatment and vaccines against circulating variants."
The CDC recommends that everyone ages 6 months and older, with some exceptions, receive an updated 2024-2025 COVID-19 vaccine to protect against the virus, regardless whether or not you have previously been vaccinated or infected.
Norman urged Americans to monitor the agency's COVID Data Tracker for updates to new variants.
KP.3.1.1:This dominant COVID-19 variant accounts for over 50% of cases, new CDC data shows
What is the dominant strain of COVID in the US? COVID-19 variant KP.3.1.1 is currently the dominant strain accounting for more than half of positive infections in the U.S. according to recent CDC projections.
Between Sept. 1 and Sept. 14, 52.7% of positive infections were of the KP.3.1.1 strain, followed by KP.2.3 at 12.2%, according to the agency's Nowcast data tracker, which displays COVID-19 estimates and projections for two-week periods.
KP.3.1.1 first became the dominant strain in the two-week period, starting on July 21st and ending on August 3rd.
"The KP.3.1.1 variant is very similar to other circulating variants in the United States. All current lineages are descendants of JN.1, which emerged in late 2023," Norman previously told USA TODAY.
COVID XEC symptoms There is no indication that the XEC variant comes with its own unique symptoms.
The CDC continues to outline the basic COVID-19 symptoms, which can appear between two to 14 days after exposure to the virus and can range from mild to severe.
These are some of the symptoms of COVID-19:
Fever or chills Cough Shortness of breath or difficulty breathing Fatigue Muscle or body aches Headache Loss of taste or smell Sore throat Congestion or runny nose Nausea or vomiting Diarrhea
The CDC said you should seek medical attention if you have the following symptoms:
Trouble breathing Persistent pain or pressure in the chest New confusion Inability to wake or stay awake Pale, gray or blue-colored skin, lips, or nail beds
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
2K notes
·
View notes
Text
You might be forgiven for thinking it’s been a very quiet few months for the Covid-19 pandemic. Besides the rollout of new boosters, the coronavirus has largely slipped out of the headlines. But the virus is on the move. Viral levels in wastewater are similar to what they were during the first two waves of the pandemic. Recent coverage of the so-called Pirola variant, which is acknowledged to have “an alarming number of mutations,” led with the headline “Yes, There’s a New Covid Variant. No, You Shouldn’t Panic.”
Even if you haven’t heard much about the new strain of the coronavirus, being told not to panic might induce déjà vu. In late 2021, as the Omicron variant was making its way to the United States, Anthony Fauci told the public that it was “nothing to panic about” and that “we should not be freaking out.” Ashish Jha, the Biden administration’s former Covid czar, also cautioned against undue alarm over Omicron BA.1, claiming that there was “absolutely no reason to panic.” This is a telling claim, given what was to follow—the six weeks of the Omicron BA.1 wave led to hundreds of thousands of deaths in a matter of weeks, a mortality event unprecedented in the history of the republic.
Indeed, experts have been offering the public advice about how to feel about Covid-19 since January 2020, when New York Times columnist Farhad Manjoo opined, “Panic will hurt us far more than it’ll help.” That same week, Zeke Emanuel—a former health adviser to the Obama administration, latterly an adviser to the Biden administration—said Americans should “stop panicking and being hysterical.… We are having a little too much [sic] histrionics about this.”
This concern about public panic has been a leitmotif of the Covid-19 pandemic, even earning itself a name (“elite panic”) among some scholars. But if there’s one thing we’ve learned, three and a half years into the current crisis, it’s that—contrary to what the movies taught us—pandemics don’t automatically spawn terror-stricken stampedes in the streets. Media and public health coverage have a strong hand in shaping public response and can—under the wrong circumstances—promote indifference, incaution, and even apathy. A very visible example of this was the sharp drop in the number of people masking after the CDC revised its guidelines in 2021, recommending that masking was not necessary for the vaccinated (from 90 percent in May to 53 percent in September).
As that example suggests, emphasizing the message “don’t panic” puts the cart before the horse unless tangible measures are being taken to prevent panic-worthy outcomes. And indeed, these repeated assurances against panic have arguably also preempted a more vigorous and urgent public health response—as well as perversely increasing public acceptance of the risks posed by coronavirus infection and the unchecked transmission of the virus. This “moral calm”—a sort of manufactured consent—impedes risk mitigation by promoting the underestimation of a threat. Soothing public messaging during disasters can often lead to an increased death toll: Tragically, false reassurance contributed to mortality in both the attacks on the World Trade Center and the sinking of the Titanic.
But at a deeper level, this emphasis on public sentiment has contributed to confusion about the meaning of the term “pandemic.” A pandemic is an epidemiological term, and the meaning is quite specific—pandemics are global and unpredictable in their trajectory; endemic diseases are local and predictable. Despite the end of the Public Health Emergency in May, Covid-19 remains a pandemic, by definition. Yet some experts and public figures have uncritically advanced the idea that if the public appears to be tired, bored, or noncompliant with public health measures, then the pandemic must be over.
But pandemics are impervious to ratings; they cannot be canceled or publicly shamed. History is replete with examples of pandemics that blazed for decades, sometimes smoldering for years before flaring up again into catastrophe. The Black Death (1346–1353 AD), the Antonine Plague (165–180 AD), and the Plague of Justinian (541–549 AD), pandemics all, lacked the quick resolution of the 1918 influenza pandemic. A pandemic cannot tell when the news cycle has moved on.
Yet this misperception—that pandemics can be ended by human fiat—has had remarkable staying power during the current crisis. In November 2021, the former Obama administration official Juliette Kayyem claimed that the pandemic response needed to be ended politically, with Americans getting “nudged into the recovery phase” by officials. It is fortunate that Kayyem’s words were not heeded—the Omicron wave arrived in the US just weeks after her article ran—but her basic premise has informed Biden’s pandemic policy ever since.
Perhaps even less responsibly, the physician Steven Phillips has called for “new courageous ‘accept exposure’ policies”—asserting that incautious behavior by Americans would be the true signal of the end of the pandemic. In an essay for Time this January, Phillips wrote: “Here’s my proposed definition: the country will not fully emerge from the Covid-19 pandemic until most people in our diverse nation accept the risk and consequences of exposure to a ubiquitous SARS-CoV-2, the virus that causes Covid-19.”
This claim—that more disease risk and contagion means the end of a disease event—runs contrary to the science. Many have claimed that widespread SARS-CoV-2 infections will lead to increasingly mild disease that poses fewer concerns for an increasingly vaccinated (or previously infected) population. In fact, more disease spread means faster evolution for SARS-CoV-2, and greater risks for public health. As we (A.C. and collaborators) and others have pointed out, rapid evolution creates the risk of novel variants with unpredictable severity. It also threatens the means that we have to prevent and treat Covid-19: monoclonal antibody treatments no longer work, Paxlovid is showing signs of viral resistance, and booster strategy is complicated by viral evolution of resistance to vaccines.
But these efforts to manage and direct public feelings are not just more magical thinking; they are specifically intended to promote a return to pre-pandemic patterns of work and consumption. This motive was articulated explicitly in a McKinsey white paper from March 2022, which put forward the invented concept of “economic endemicity”—defined as occurring when “epidemiology substantially decouples from economic activity.” The “Urgency of Normal” movement similarly used an emotional message (that an “urgent return to fully normal life and schooling” is needed to “protect” children) to advocate for the near-total abandonment of disease containment measures. But in the absence of disease control measures, a rebound of economic activity can only lead to a rebound of disease. (This outcome was predicted by a team that was led by one of the authors [A.C.] in the spring of 2021.)
A pandemic is a public health crisis, not a public relations crisis. Conflating the spread of a disease with the way people feel about responding to that spread is deeply illogical—yet a great deal of the Biden administration’s management of Covid-19 has rested on this confusion. Joe Biden amplified this mistaken perspective last September when he noted that the pandemic was “over”—and then backed that claim by stating, “If you notice, no one’s wearing masks. Everybody seems to be in pretty good shape.” The presence or absence of health behaviors reveals little about a threat to health itself, of course—and a decline in mask use has been shaped, in part, by the Biden administration’s waning support for masking.
Separately, long Covid poses an ongoing threat both at an individual and a public health level. If our increasingly relaxed attitude toward public health measures and the relatively unchecked spread of the virus continue, most people will get Covid at least once a year; one in five infections leads to long Covid. Although it’s not talked about a lot, anyone can get long Covid; vaccines reduce this risk, but only modestly. This math gets really ugly.
The situation we are in today was predictable. It was predictable that the virus would rapidly evolve to evade the immune system, that natural immunity would wane quickly and unevenly in the population, that a vaccine-only strategy would not be sufficient to control widespread Covid-19 transmission through herd immunity, and that reopening too quickly would lead to a variant-driven rebound. All of these unfortunate outcomes were predicted in peer-reviewed literature in 2020–21 by a team led by one of the authors (A.C.), even though the soothing public messaging at the time called it very differently.
As should now be very clear, we cannot manifest our way to a good outcome. Concrete interventions are required—including improvements in air quality and other measures aimed at limiting spread in public buildings, more research into vaccine boosting strategy, and investments in next-generation prophylactics and treatments. Rather than damping down panic, public health messaging needs to discuss risks honestly and focus on reducing spread. Despite messages to the contrary, our situation remains unstable, because the virus continues to evolve rapidly, and vaccines alone cannot slow this evolution.
In the early months of the pandemic, many in the media drew parallels between the public’s response to Covid-19 and the well-known “stages of grief”: denial, bargaining, anger, depression, and acceptance. The current situation with Covid-19 calls for solutions, not a grieving process that should be hustled along to the final stage of acceptance.
844 notes
·
View notes
Text
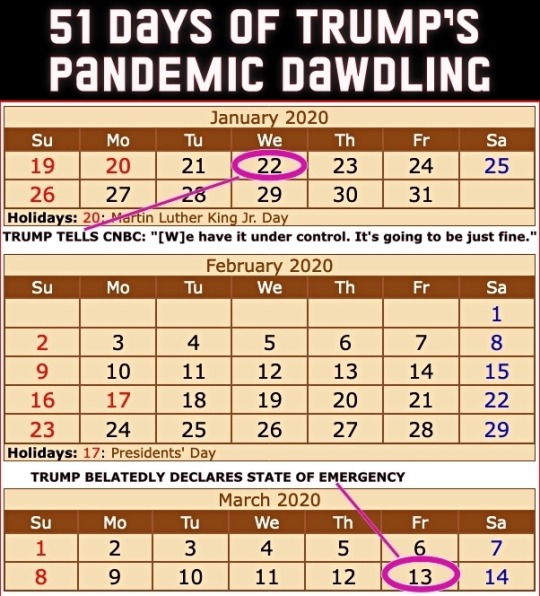
Four years ago today (March 13th), then President Donald Trump got around to declaring a national state of emergency for the COVID-19 pandemic. The administration had been downplaying the danger to the United States for 51 days since the first US infection was confirmed on January 22nd.
From an ABC News article dated 25 February 2020...
CDC warns Americans of 'significant disruption' from coronavirus
Until now, health officials said they'd hoped to prevent community spread in the United States. But following community transmissions in Italy, Iran and South Korea, health officials believe the virus may not be able to be contained at the border and that Americans should prepare for a "significant disruption." This comes in contrast to statements from the Trump administration. Acting Department of Homeland Security Secretary Chad Wolf said Tuesday the threat to the United States from coronavirus "remains low," despite the White House seeking $1.25 billion in emergency funding to combat the virus. Larry Kudlow, director of the National Economic Council, told CNBC’s Kelly Evans on “The Exchange” Tuesday evening, "We have contained the virus very well here in the U.S." [ ... ] House Speaker Nancy Pelosi called the request "long overdue and completely inadequate to the scale of this emergency." She also accused President Trump of leaving "critical positions in charge of managing pandemics at the National Security Council and the Department of Homeland Security vacant." "The president's most recent budget called for slashing funding for the Centers for Disease Control, which is on the front lines of this emergency. And now, he is compounding our vulnerabilities by seeking to ransack funds still needed to keep Ebola in check," Pelosi said in a statement Tuesday morning. "Our state and local governments need serious funding to be ready to respond effectively to any outbreak in the United States. The president should not be raiding money that Congress has appropriated for other life-or-death public health priorities." She added that lawmakers in the House of Representatives "will swiftly advance a strong, strategic funding package that fully addresses the scale and seriousness of this public health crisis." Senate Minority Leader Chuck Schumer also called the Trump administration's request "too little too late." "That President Trump is trying to steal funds dedicated to fight Ebola -- which is still considered an epidemic in the Democratic Republic of the Congo -- is indicative of his towering incompetence and further proof that he and his administration aren't taking the coronavirus crisis as seriously as they need to be," Schumer said in a statement.
A reminder that Trump had been leaving many positions vacant – part of a Republican strategy to undermine the federal government.
Here's a picture from that ABC piece from a nearly empty restaurant in San Francisco's Chinatown. The screen displays a Trump tweet still downplaying COVID-19 with him seeming more concerned about the effect of the Dow Jones on his re-election bid.
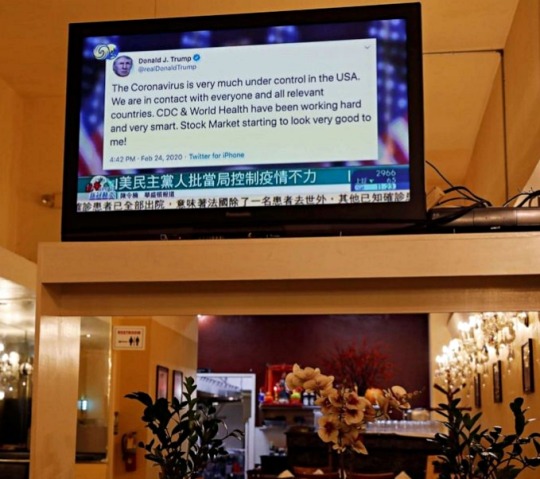
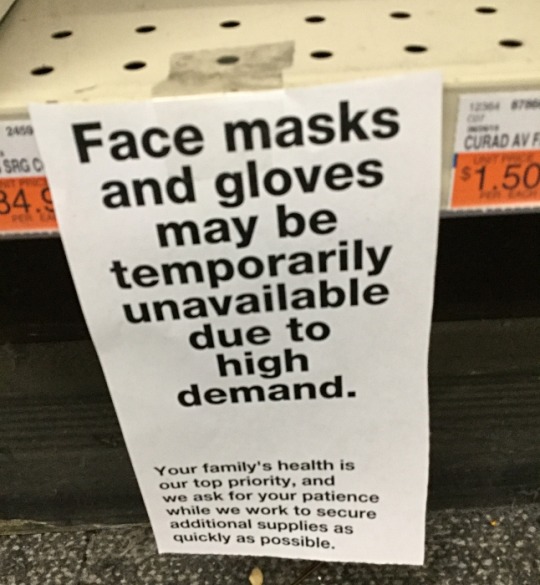
People were not buying Trump's claims but they were buying PPE.
I took this picture at CVS on February 26th that year.
The stock market which Trump in his February tweet claimed looked "very good" was tanking on March 12th – the day before his state of emergency declaration.

Trump succeeded in sending the US economy into recession much faster than George W. Bush did at the end of his term – quite a feat!. (As an aside, every recession in the US since 1981 has been triggered by Republican presidents.)
Of course Trump never stopped trying to downplay the pandemic nor did he ever take responsibility for it. The US ended up with the highest per capita death rate of any technologically advanced country.
Precious time was lost while Trump dawdled. Orange on this map indicates COVID infections while red indicates COVID deaths. At the time Trump declared a state of emergency, the virus had already spread to 49 states.

The United States could have done far better and it certainly had the tools to do so.
The Obama administration had limited the number of US cases of Ebola to under one dozen during that pandemic in the 2010s. Based on their success, they compiled a guide on how the federal government could limit future pandemics.
Obama team left pandemic playbook for Trump administration, officials confirm
Of course Trump ignored it.
Unlike those boxes of nuclear secrets in Trump's bathroom, the Obama pandemic limitation document is not classified. Anybody can read it – even if Trump didn't. This copy comes from the Stanford University Libraries.
TOWARDS EPIDEMIC PREDICTION: FEDERAL EFFORTS AND OPPORTUNITIES IN OUTBREAK MODELING
Feel free to share this post with anybody who still feels nostalgic about the Trump White House years!
#covid-19#coronavirus#pandemic#public health#donald trump#trump's incompetent response to the pandemic#covid state of emergency#2020#trump recession#51 days of trump pandemic dawdling#obama pandemic playbook#2010s ebola outbreak#nostalgia for trump administration#republicans#election 2024#vote blue no matter who
113 notes
·
View notes
Text
In the U.K., the Health Security Agency recently raised its threat level to 4 out of 6, the stage immediately before large-scale human outbreaks. In Europe, countries are proactively vaccinating dairy and poultry workers against infection, with 15 nations already securing a total of 40 million doses through the European Commission. In the United States, despite having a stockpile of those vaccines, we are not distributing them, instead focusing on standing up voluntary supplies of seasonal flu vaccines to frontline workers. (The hope is that this will prevent animal infections of human flu that might aid in the further mutation of H5N1.) The Centers for Disease Control and Prevention has cited the low number of cases to justify its inaction, but it has also moved remarkably slowly to promote the kind of widespread surveillance testing that could actually identify cases. Only recently has the agency begun to mobilize real funding for a testing push, after a period of months in which various federal groups batted around responsibility and ultimate authority like a hot potato. And as was the case early in the Covid-19 pandemic, the C.D.C.’s preferred test for bird flu “has issues.” Three months into the outbreak, only 45 people had even been tested; six weeks later, the total number of people tested had grown only to “230+.” [...] Most farms aren’t supplying N95 masks, goggles or aprons to protect workers, either, and when Amy Maxmen of KFF News surveyed farm workers to ask why they weren’t getting tested, “no one had heard of bird flu, never mind gotten P.P.E. or offers of tests,” she reported. “One said they don’t get much from their employers, not even water. If they call in sick, they worry about getting fired.” Last month, a crew was deployed to slow the spread of the disease by killing every last chicken of 1.78 million on a large Colorado farm where H5N1 had broken out and six of the workers contracted the virus, partly because the gear they’d been provided was hard to use in the punishing 104-degree heat. In June, Robert Redfield, former director of the C.D.C., echoed many epidemiologists in predicting that “it’s not a question of if, it’s more of a question of when we will have a bird flu pandemic.” In July, Brown’s Jennifer Nuzzo warned that the steady beat of new cases “screams at us that this virus is not going away.” Tulio de Oliveira, a bioinformatician who studies global disease surveillance, marveled that the American effort to track the spread of the disease was absolutely amateurish and the country’s apparent indifference “unbelievable.”
59 notes
·
View notes
Note
I'm seeing information about the Novavax being formulated for the previous variant and the Moderna and Pfizer being for a more recent one. Is this true and if so, why are so many people trying to get the Novavax?
Hi, glad you asked! Here's a few posts on this:
Graphic (albeit from Novavax, no 3rd-party trials) showing broad neutralization:
Another, thread explaining the above. Particularly:
"Ultimately as the antigenic distance is very close for all major circulating variants, all vaccine options should be very good, and provide good protection against infection and severe disease (even when compared with infection-acquired/natural immunity)."
One more, from NPR: https://www.npr.org/sections/shots-health-news/2024/08/22/nx-s1-5082372/updated-covid-vaccines-fda-approved
The Pfizer-BioNTech and Moderna ... now target the KP.2 variant ... The Novavax vaccine, which is based on an older technology, targets an earlier strain of the virus called JN.1. As many of us know by now, the virus continues evolving to better evade our immune defense, which means regularly updating the vaccines to keep up with the latest strain. It turns out the KP.2 and JN.1 variants have already been overtaken by newer variants. Because those are also descendants of omicron, the hope is that the new vaccines are close enough matches that they can still boost immunity and protect people in the coming months – ideally reducing the chances of a big winter wave. “The vaccine is not intended to be perfect. It’s not going to absolutely prevent COVID-19," Dr. Peter Marks from the FDA told NPR in an interview. "But if we can prevent people from getting serious cases that end up in emergency rooms, hospitals or worse — dead — that’s what we’re trying to do with these vaccines.”
There's a couple of other points I do not have sources for right now; if anyone would like to reblog and add some or correct this, please do!:
I've read that in the past, for example, flu vaccine efficacy was not necessarily dampened when the vax targeted a "parent". They are in the same lineage, so efficacy should be good.
Analogy (albeit imperfect): using a net vs a spear.
Of course, without more data, we don't know. I would wager that people who choose Novavax nowadays may also be informed on #Layered Protection and prioritize physical barriers (N95 masking) as the first line of defense, with vaccine as secondary bonus, since any of them have a non-negligible % of breakthroughs at this point.
It was different in 2021 when they were first released and showed high efficacy; ~3% breakthrough, if that. Now, I would not in any case rely on Pfizer or Moderna alone, so there's not much of a reason to suffer their ill effects for days.
But bodies are all different. Some people tolerate them well. Some have no other choice. As always, get the one you can, that works for you!
#covid#novavax#vaccines#commentary/opinion#data#why novavax#2024#get vaccinated#get boosted#layers of protection
48 notes
·
View notes