#osseous-lesion
Explore tagged Tumblr posts
Text

tried my hand at @mintybagels DTIYS! Their color composition is literally so good it's fucking insane
#art#my art#my art 2024#osseous-lesion#fanart#digital art#tma#tma fanart#the magnus archives#the magnus archives fanart#jonathan sims#jonathan sims fanart#artists on tumblr#this is like the first think I've been interested in drawing and posting in ages
100 notes
·
View notes
Text
Gusher phenomenon and Ménière disease. An enigmatic Case report by Bonifacio F. MD in Journal of Clinical Case Reports MedicaI Images and Health Sciences
Abstract
During stapedotomies or cochlear implant placement, cerebrospinal fluid gusher was described. The recognized causes result from abnormal communication between perilymphatic space and subarachnoid space. Our clinical case describes a patient with Ménière disease that presented a gusher phenomenon during surgery. A dubious and controversial case report.
Key words: Otogenic vertigo, Ménière disease, endolymphatic hydrops, perilymph, Cerebrospinal Fluid
INTRODUCTION
The gusher phenomenon happens more frequently during stapes surgery and cochlear implant placement. Violent perilymph leakage starts during platinotomy or electrode placement and must be plugged in order not to cause sensorineural deafness. The stapes surgery is not practicable; instead, the positioning of cochlear implants is possible after the cleansing of cochleostomy; furthermore, other cases of uncontrolled perilymph leakage are described in the literature after temporal bone fracture.1,2,3This phenomenon is due to abnormal communication between perilymphatic and subarachnoid spaces.4 The connection is produced by anatomical alterations such as internal auditory canal bone fistula or the cochlear and vestibular aqueduct enlargement.5,6 Mondini cochlear malformation is a cochlear gyrus reduction in the osseous and membranous labyrinth; the cochlea does not finish its development during the seventh week of gestation. Cochlea dysplasia is often associated with fistulas between a labyrinth and the subarachnoid spaces (modiolus fistula).7,8
The cochlear aqueduct allows communication between the cochlear perilymphatic space and the cerebellar subarachnoid fossa. This structure plays a role in perilymphatic, endolymphatic, and cerebrospinal fluid flow. The fluid flow rate is a function of the fourth power of duct radius, therefore a minimal change of cochlear aqueduct radius is responsible for a change in the inner ear hydrodynamics.9 To avoid the high risk of hearing loss due to cerebrospinal fluid (CSF) gusher, a proper diagnostic procedure is required before this type of surgery.
Case presentation
The 81-year-old patient reports vestibular symptoms for about 30 years with objective vertigo lasting about an hour with fullness and tinnitus referable to the left ear.
Serial audiometric examinations showed a fluctuating sensorineural hearing loss in the left ear, ranging from low to medium frequencies (Fig. 1).
Tympanometry produces a type A graft and absent stapedius reflexes. In two different hospitals, Ménière disease (MD) diagnosis was made. Cranial CT excludes malformations of the inner ear: enlargement cochlear aqueduct (ECA), enlargement vestibular aqueduct (EVA), Mondini Malformation, third-window lesion, ear semicircular canal fistula (Fig.2). Also in our hospital, after excluding other pathologies with vestibular symptomatology, definite Meniere disease of the left ear was confirmed following the Classification Committee of the Bárány Society.10,11
After ten years, audiometric examinations showed severe left pantonal sensorineural hearing loss (Fig.1). The patient describes the last vertigo from 2001 until January 2018, during a more violent crisis recurrence, with objective vertigo lasting 6-7 hours accompanied by nausea and vomiting. The first medical line (betahistine, diuretics, dexamethasone) failed to treat vertigo. Left transcanal labyrinthectomy has been performed considering untreatable vertigos, patient’s age, and severe hearing loss.12
During the intervention, the authors proceeded to tympanic cavity exploration. The middle ear appeared free from inflammatory disease and windows perilymphatic fistulas; therefore, with a microscopic vision, two windows ossification was identified. During the opening of the oval window, unpredictable high-pressure liquid leakage happened with a diagnosis of the perilymphatic gusher. The next step was to put a fragment of the temporal muscle and temporal fascia on the oval window and the round window until we verified the absence of perilymph.
DISCUSSION
The perilymphatic gusher was described in stapes surgery and cochlear implant placement. Otosclerosis result in bilateral mixed or conductive hearing loss with absent stapedial reflexes; only a few times high-resolution CT scan or an MRI is required for the inner ear studies, therefore is difficult to suspect possible gusher events.
The inner ear should be studied with radiology before surgery to avoid the risk of hearing loss.
A cranial CT scan can highlight cochlear and vestibular aqueduct enlargement, the Mondini malformation, and other forms of inner ear hypoplasia, but not allow inner ear canal fistulas.13 Several studies also argue that an enlarged vestibular aqueduct is not necessarily associated with the gusher phenomenon.14 However, there seems to be a more significant correlation with the enlargement of the cochlear aqueduct.13,15
Other studies show that an oblique plane CT scan can diagnose bone dehiscence between the basal gyrus of the cochlea and the inner ear canal.16,4 Preoperative CT scans do not necessarily investigate subtle inner ear malformations.
A retrospective study on preoperative CTs revealed that a negative result from the wrong collection in the inner ear could be associated with false negatives.17 A correct diagnosis is essential to avoid the gusher phenomenon, but a CT scan does not always help the surgeon. This study is the first reported case of a perilymphatic gusher in a patient suffering from vertigo. CSF leakage has never been described in a patient with Meniere Disease.
Among Meniere's disease therapies, there isn't a window opening. Labyrinthectomy can be used as the last step of MD treatment, but no cases of CSF gusher have been described during transcanal labyrinthectomy. More data is needed in the literature to answer these doubts.
Based on the data collected, the authors formulate the following hypotheses to explain the clinical case:
Prominent endolymphatic hydrops could be the cause of a gusher phenomenon
MD in vertigo absence if unilateral can mimic otosclerosis.
The patient could be affected by MD and an unrecognized inner ear malformation.
The MD diagnosis could be incorrect because of a malformation of the inner ear that could create a diagnostic picture similar to MD.
Conclusion
Internal ear abnormalities can cause no-standard communication between perilymphatic and subarachnoid space; these anomalies may remain unknown. Can Meniere's disease be considered endolymphatic hypertension?
Conflicts of Interest and Source of Funding:
The authors declare no conflict of interests or external fundings.
Financial Support/Conflict of Interest: None
#Otogenic vertigo#Ménière disease#endolymphatic hydrops#perilymph#Cerebrospinal Fluid#jcrmhs#Journal of Clinical Case Reports MedicaI Images and Health Sciences
3 notes
·
View notes
Text
Confess and be hanged
Kathy Griffin's elbow (Other congenital malformations of hair)
Dave Navarro's forehead (Subluxation of lens, unspecified eye)
Jessica Biel's eye (Other hammer toe(s) (acquired), left foot)
James Franco's fist (Solitary bone cyst, left ulna and radius)
Simon Doonan's thigh (Malignant neoplasm of left orbit)
Carson Palmer's head (School (private) (public) (state) as the place of occurrence of the external cause)
Pitbull's eye (Chondrolysis, hip)
Kevin Federline's eye (Osseous and subluxation stenosis of intervertebral foramina of abdomen and other regions)
Tate Donovan's thigh (Chronic myeloid leukemia, BCR/ABL-positive, in remission)
Ryan Gosling's arm (Pedal cycle passenger injured in collision with fixed or stationary object in traffic accident)
Sean Combs's neck (Mixed pediculosis and phthiriasis)
Katharine McPhee's chin (Calcific tendinitis, right lower leg)
Katrina Bowden's back (Kernicterus, unspecified)
Balthazar Getty's hair (Toxic effect of contact with other venomous marine animals, assault)
Elizabeth Taylor's ear (Displaced trimalleolar fracture of left lower leg)
Kelsey Grammer's eye (Major laceration of left kidney)
Kerry Diamond's neck (Scrotal transposition)
Jason Lee's wrist (Papyraceous fetus, first trimester)
Josh Holloway's upper arm (Activity, swimming)
Desiree Hartsock's ear (Swimmer's ear, left ear)
Jared Leto's eyebrow (Pathological fracture, right hand)
Rumer Willis's eye (Lesion of plantar nerve)
Ramona Singer's arm (Other specified injury of intrinsic muscle and tendon at ankle and foot level, left foot)
Emily VanCamp's calf (Nicotine dependence, cigarettes, with withdrawal)
Jane Krakowski's fist (Other unilateral secondary osteoarthritis of hip)
Vince Vaughn's lower leg (Unspecified complication following infusion and therapeutic injection)
Olivia Palermo's shoulder (Laceration without foreign body of right back wall of thorax with penetration into thoracic cavity)
Russell Brand's wrist (Malignant neoplasm of left orbit)
Jackson Rathbone's belly (Primary cyst of pars plana, unspecified eye)
Garth Brooks's eyebrow (Nondisplaced fracture of anterior process of left calcaneus)
Adrian Grenier's nose (Military operations involving flamethrower, civilian)
Jesse Tyler Ferguson's hair (Retinal hemorrhage, left eye)
Martin Lawrence's ankle (Hemorrhagic disease of newborn)
Spencer Pratt's neck (Perforated corneal ulcer, unspecified eye)
Ashley Hebert's bottom (Major laceration of left kidney)
Hugh Jackman's bottom (Laceration of radial artery at wrist and hand level of left arm)
Paris Hilton's chin (Preterm labor without delivery, unspecified trimester)
Simon Cowell's arm (Contusion of small intestine)
Tila Tequila's cheek (Other superficial bite of hand of unspecified hand)
Jennifer Grey's toe (Injury of quadriceps muscle, fascia and tendon)
Brody Jenner's hip (Laceration without foreign body of back wall of thorax without penetration into thoracic cavity)
Ciara's hair (Diffuse cystic mastopathy of unspecified breast)
Molly Sims's chin (Urticaria due to cold and heat)
Luke Bryan's buttocks (Urticaria due to cold and heat)
Richard Gere's breast (Endometriosis of pelvic peritoneum)
Jensen Ackles's calf (Other ulcerative colitis with intestinal obstruction)
Teresa Giudice's head (Laceration of extensor muscle, fascia and tendon of left middle finger at forearm level)
Stavros Niarchos III's ear (Striatonigral degeneration)
Winona Ryder's thumb (Acute embolism and thrombosis of right femoral vein)
Scott Disick's forearm (Extranodal NK/T-cell lymphoma, nasal type)
3 notes
·
View notes
Note
credit your pfp, you’re not helping anyone by saying “pfp isn’t by me”
...*deep intake* YES, I KNOW. I'm sorry, but my friend sent the post to me. in MY HASTE, I real quick said, "hey, lemme just put 'not mine' because I'm not an ART STEALER." wow, I'm "not helping anyone" sorry I didn't take the time out of my already busy schedule to search a bunch of posts to find it. but I did, just for you. the artists name is @osseous-lesion
sorry for being rude. I'm just in a bad mood already. my day hasn't really been that great.
5 notes
·
View notes
Text
@osseous-lesion
I can’t believe there are people who haven’t seen this video. Now is the time to watch!
22K notes
·
View notes
Text
Disease Of Bone Manifested In The Jaws And Fibro-Osseous Lesions
0 notes
Text
Disease Of Bone Manifested In The Jaws And Fibro-Osseous Lesions
0 notes
Text
"Bad news about my knee" the text read.
Took me a few to remember that my sister's knee has been really bothering her for months since the trip to Parris Island and she had mentioned seeing a doctor about it.
"oh no! Not surgery!" I replied. It's not even been a year since she had to have a kidney removed due to Renal Cancer.
"Lesion on the bone, because of where it's located it's most likely cancer."
Dafuq.
I let that word just sit there in my text messages for a bit. I was at work I needed a sec.
Knee cancer? Was that even a thing? I've never heard of knee cancer.
A quick Google told me why, that's because it's called bone cancer.
Well fuck. That sounded a lot worse than knee cancer.
Kim sent over a picture of the MRI results . There were filled with medical jargon like marrow replacing osseous leison and indicative of metastasis.
2.3cm by 2.3 cm by 3.0 cm
It's that big? I mean in the cancer world?
Metastasis? Did they think this was from her kidney cancer? If it went to her knee where else did it go?
Google is not your friend at a time like this.
After like 10 frantic minutes of searching online I was scared and I still had not responded to my sister.
"burn that. I don't like what it says" I texted back.
"We know nothing until a full body scan and biopsy"
Kim replied with, "they want me to visit an oncologist immediately, they said every day matters."
At reading this, I locked my computer and went outside. I googled life expectancy of bone cancer and read 6 to 48 months.
And I cried.
I messaged my sister between sobs. I told her that was terrifying and it wasn't fair, she's been through enough.
That dropping a bomb on you like that and making you just wait for any real answers, or even a plan was like torture.
I tried to go the whole it might be benign route, but that doctor's findings seemed pretty clear they don't think it was likely.
So we just have to wait and worry. Will I lose my sister in a matter of months?
Unthinkable. No!
So i just sat there and cried until I was sure I could return to my desk more or less put together.
1 note
·
View note
Text
Disease Of Bone Manifested In The Jaws And Fibro-Osseous Lesions
0 notes
Text

I redesigned Alastor again because I can't help myself lmao
I've gotten into historical fashion again since I took a class on it this last fall semester, so I worked that into the design a bit more. The coat is a little too fitted for the 20s or 30s, but I think a fitted look is nicer on him lol. I also stuck with giving him more dear features in his face because I think it's fun :) I've been seeing people make his antlers little radio tower-looking things and I'm literally in love with that idea, so that's thrown in there too. A lot of the microphones I was looking at that were used for radio shows in the 20s were circular, so that's why I changed Alastor's staff, but I didn't think a pentagram would make a ton of sense because that's Lucifer's symbol. I also wanted to stray away from Vodou or voodoo imagery because the way it shows up in the show isn't the most respectful. I think his powers make more sense as something Lovecraftian based, but I was kind of iffy about even doing that because Lovecraft was a racist shitbag and his works cannot be separated from that with how ingrained it was in his writing. Personally, I think the Lovecraftian mythos has kind of evolved past what H.P. Lovecraft wrote, and he's kind of forgotten in a lot of media that spawns from or takes inspiration from his work, which is great and that's how it should be. Anyway, Alastor's staff is the Necronomicon symbol, and the rest of the symbols are either radio symbols or Lovecraftian god symbols. I gave him a little spade on his tale because I think his staff in the show kind of looks like a spade, and that's a little asexual symbol, so I thought it was a fun thing to tack on there Last thing I thought would be fun was if the color literally drained from him as he got panicked or angry. I've seen a lot of black and white Alastor designs, and I'm in love with them all, so I wanted to incorporate that a little bit.
Anyway, this was just a conglomerate of a bunch of ideas and passing thoughts lol
#art#my art#my art 2024#digital art#fanart#hazbin hotel#alastor#hazbin alastor#alastor hazbin hotel#hazbin hotel fanart#alastor fanart#alastor redesign#osseous-lesion#Oh! Another random thing about his staff#I feel like he 'd be able to change it's shape for show or whatever#like when he does a little dance number it might turn into a more typical cane for the aesthetic#or if he doesn't want it out he could make it turn into a lapel pin#idk#I also like a lot of headcanons that both his power and his voice either come from the staff or are kind of focused through it
43 notes
·
View notes
Text
Medical Knowledge
500 MOST COMMONs...
1. Most common aortic branch involved in Takayasu arteritis : Left subclavian
2. Most common cause of respiratory distress in newborn : Transient tachypnea of the newborn
3. Most common location to see Asbestosis sequale : Posterior lower lobes.
4. Most common karyotype / chromosomal abnormality in USA : Down’s syndrome
5. Most common osseous lymphoma, primary and secondary : Diffuse large B-cell lymphoma
6. Most common primary malignant orbital tumor in childhood : Rhabdomyosarcoma
7. Most common type of fluid collection in scrotum : Hydrocele
8. Most common type of liposarcoma to affect children : Myxoid liposarcoma
9. Most common abdominal emergency of early childhood : Intussusception.
10. Most common acetabular fracture : Posterior acetabulum.
11. Most common affected bowel segment in TB : Ileocecal area.
12. Most common affected joint in gout : First MTP.
13. Most common AIDS-related neoplasm : Kaposi Sarcoma
14. Most common allergic aspergillosis syndrome : Allergic bronchopulmonary aspergillosis.
15. Most common anatomic variant of pancreas : Pancreas divisum
16. Most common anomalous course of RCA : Interarterial
17. Most common appearance of Legionella at the peak of the disease : Bilateral airspace consolidation.
18. Most common assoc. w/ Fx of great toe distal phalanx with physeal involvement :Osteomyelitis.
19. Most common associated anomaly with coarctation : Bicuspid valve.
20. Most common association of PAPVR : Sinus venosus type ASD.
21. Most common association with small left colon syndrome : Maternal DM
22. Most common bacterial cause of mesenteric adenitis : Yersinia enterocolitica.
23. Most common benign cardiac rhythm abnormality : PAC
24. Most common benign cartilage-containing tumor : Osteochondroma
25. Most common benign growth of the skeleton : Osteochondroma
26. Most common benign hepatic lesion : Hemangioma
27. Most common benign hepatic tumor during fist 6 mo. of life : Infantile Hemangioendothelioma
28. Most common benign intraconal tumor of the orbit in adults : Cavernous hemangiomas.
29. Most common benign masses caused by asbestos exposure : Atelectatic Asbestos Pseudotumor
30. Most common benign mesenchymal tumor of kidney : AML
31. Most common benign mucosal tumor of the esophagus : Papilloma
32. Most common benign nasopharyngeal tumor : Juvenile angiofibroma.
33. Most common benign orbital tumor in childhood : Dermoid Cyst of Orbit
34. Most common benign ovarian neoplasm in young and middle-aged women (<45 years) :Mature teratoma
35. Most common benign radiation-induced tumor of the musculoskeletal system : Osteochondroma
36. Most common benign rib lesion in an adult : Fibrous dysplasia.
37. Most common benign soft-tissue tumor of the foot : Plantar fibromatosis
38. Most common benign soft-tissue tumor of vascular origin : Hemangioma
39. Most common benign solid tumor in women of childbearing age : Fibroadenoma
40. Most common benign testicular mass : Simple cyst
41. Most common benign tumor of spleen : Hemangioma
42. Most common benign tumor of the larynx : Squamous papilloma
43. Most common benign tumor of the lung : Hamartoma
44. Most common benign tumor of the small bowel : GIST
45. Most common benign vascular gastric tumor : Glomus tumor of stomach.
46. Most common bilateral testicular tumor : Lymphoma
47. Most common biliary complication s/p lap. cholecystectomy : Bile duct leak from cystic duct stump.
48. Most common biliary complication s/p liver transplantation : Obstruction/stenosis at anastomosis.
49. Most common bladder neoplasm in children younger than 10 years : Rhabdomyosarcoma
50. Most common bone to develop an osteochondroma : Femur (tibia second most common)
51. Most common brain anomaly on prenatal sonograms : Isolated Mild Ventriculomegaly
52. Most common breast tumor under age 25 years : Fibroadenoma
53. Most common cardiac manifestation of Systemic Lupus Erythematous : Pericarditis
54. Most common cardiac tumor in children : Rhabdomyoma.
55. Most common cardiac valvular tumor : Papillary fibroelastoma
56. Most common carpal dislocation : Transscaphoid perilunate dislocation.
57. Most common causative organism of acute pyogenic meningitis in adults : Strep. pneumoniae
58. Most common causative organism of neonatal pyogenic meningitis : E. coli
59. Most common cause for failure of dialysis graft : Fibrointimal hyperplasia : venous outflow stenosis.
60. Most common cause for late failure in lung transplant patient : Bronchiolitis obliterans
61. Most common cause for pulmonary edema : Left-sided heart disease
62. Most common cause non iatrogenic cause of small bowel obstruction : Hernia
63. Most common cause of a large choroid plexus cyst : Trisomy 18.
64. Most common cause of a large pleural fluid collection in the newborn period : Chylothorax
65. Most common cause of acute renal failure in children requiring dialysis : HUS
66. Most common cause of acute testicular pain in postpubertal male : Acute epididymitis
67. Most common cause of acute testicular pain in prepubertal male : Torsion
68. Most common cause of AIDS cholangiopathy : Cryptosporidium
69. Most common cause of an echogenic renal mass in a 3-month-old : Mesoblastic nephroma.
70. Most common cause of an intraorbital mass lesion in adult : Pseudotumor of Orbit
71. Most common cause of AS in Western world : Degenerative disease
72. Most common cause of bilateral breast edema : CHF.
73. Most common cause of bilateral echogenic renal cortex : Chronic glomerulonephritis.
74. Most common cause of biliary obstruction : Choledocholithiasis
75. Most common cause of bleeding between menstrual cycles : Endometrial hyperplasia.
76. Most common cause of bronchopneumonia : Staphylococcal
77. Most common cause of cancer deaths in males and females : Bronchogenic Carcinoma
78. Most common cause of cause of infectious esophagitis : Candida Esophagitis
79. Most common cause of cavitary (necrotic) pneumonia in a child : Strep pneum.
80. Most common cause of Charcot joints : Diabetes mellitus
81. Most common cause of CHF in a child : ALCAPA / aberrant left coronary artery
82. Most common cause of CHF in a neonate : Hypoplastic Left Heart.
83. Most common cause of chronic hydronephrosis in renal transplant : UV anastomosis stricture.
84. Most common cause of colonic obstruction in adults : Malignancy
85. Most common cause of colonic obstruction in the infant : Meconium plug syndrome in CF patients
86. Most common cause of colovesical fistula : Diverticulitis
87. Most common cause of congenital CNS infection : CMV.
88. Most common cause of congenital duodenal obstruction : Duodenal atresia.
89. Most common cause of congenital sensorineural hearing loss : Giant vestibular aqueduct syndrome
90. Most common cause of cord ischemia : Thromboembolic disease
91. Most common cause of coronary artery aneurysm in USA : Atherosclerosis
92. Most common cause of coronary artery aneurysm Worldwide : Kawasaki
93. Most common cause of cyanosis in a child : Tetralogy of Fallot
94. Most common cause of cyanosis n newborn Transposition of great vessels
95. Most common cause of death in a severe pelvic fracture : Hemorrhage.
96. Most common cause of death in Ataxia –Telangiectasia : Respiratory failure.
97. Most common cause of death in Jeune syndrome : Respiratory failure
98. Most common cause of drop mets : Medulloblastoma
99. Most common cause of dwarfism : Achondroplasia
100. Most common cause of echogenic renal pyramids in children : Furosemide
101. Most common cause of ejaculatory duct obstruction : Mullerian duct cyst ?
102. Most common cause of endometriosis in girls <16 years of age : Obstructive müllerian duct anomalies
103. Most common cause of end-stage renal disease : Diabetic Nephropathy
104. Most common cause of epididymitis in males aged 15 to 35 years : Sexually transmitted diseases
105. Most common cause of esophageal rupture : Iatrogenic
106. Most common cause of exocrine pancreatic insufficiency in patients <30 years of age : CF
107. Most common cause of facial hemipalsy : Bell palsy
108. Most common cause of false-positive V/Q scan for acute PE : Previous pulmonary embolism
109. Most common cause of fungal infection in AIDS patients : Cryptococcosis
110. Most common cause of gastrocolic fistula : Gastric ulcer.
111. Most common cause of heart failure in patients with COPD : Atherosclerotic heart disease
112. Most common cause of hemifacial spasticity is vertebrobasilar dolichoectasia.
113. Most common cause of hepatic calcifications : Infection
114. Most common cause of hydronephrosis in the newborn male : Ureteropelvic junction
115. Most common cause of hyperreflexive bladder : Spinal cord trauma
116. Most common cause of increased nuchal thickness : Downs syndrome
117. Most common cause of interstitial and airspace edema : CHF
118. Most common cause of intradiaphragmatic cyst :Extralobar sequestration
119. Most common cause of intraventricular hemorrhage :Disruption of the subependymal veins
120. Most common cause of intussusception in children >6 years : Lymphoma
121. Most common cause of large spherical pancreatic calcifications in children : Hereditary pancreatitis
122. Most common cause of left atrial dilatation : Mitral regurgitation.
123. Most common cause of leukokoria : Retinoblastoma.
124. Most common cause of liver metastasis : Colon.
125. Most common cause of lower extremity venous valve dysfunction : DVT.
126. Most common cause of lower GI bleeding : Diverticulosis.
127. Most common cause of malignancy of men in the world -- Bronchogenic Carcinoma
128. Most common cause of maternal peripartum death : Amniotic fluid embolism
129. Most common cause of membranous croup : Staph. Aureus.
130. Most common cause of microcolon: Meconium ileus.
131. Most common cause of mortality in ulcerative colitis : Toxic megacolon.
132. Most common cause of necrolytic migrating erythema : Glucagonoma
133. Most common cause of neonatal nasal obstruction : Choanal atresia.
134. Most common cause of Neonatal Pneumonia : Group B streptococcus.
135. Most common cause of neonatal respiratory distress in full term/postmature infants – Meconium aspiration
136. Most common cause of nephrocalcinosis in adults : Primary hyperparathyroidism
137. Most common cause of non-immune hydrops in USA : Cardiac anomaly
138. Most common cause of optic nerve enlargement : Optic nerve glioma
139. Most common cause of orbital calcifications : Retinoblastoma
140. Most common cause of orbital infection : Paranasal sinusitis
141. Most common cause of osteoblastic bone metastases in an adult female : Breast cancer
142. Most common cause of osteoblastic bone metastases in an adult male : Prostate cancer
143. Most common cause of osteolytic bone metastases in a child : Neuroblastoma
144. Most common cause of osteolytic bone metastases in an adult female : Breast cancer
145. Most common cause of osteolytic bone metastases in an adult male : Lung cancer
146. Most common cause of Osteomyelitis of spine : Penetrating direct trauma
147. Most common cause of pancreatic lipomatosis in children : CF
148. Most common cause of pleural eosinophilia : Air in the pleural space
149. Most common cause of pneumoperitoneum : Ruptured duodenal ulcer.
150. Most common cause of postpartum fever : Endometritis.
151. Most common cause of pseudomyxoma peritonei : Appendiceal mucinous adenocarcinoma
152. Most common cause of pseudoureterocele : Bladder tumor
153. Most common cause of pulmonary hypoplasia : Diaphragmatic hernia
154. Most common cause of pulmonary tumor embolus : Gastric carcinoma
155. Most common cause of recurrent hip disloc. s/p hip arthroplasty : Acetabular component malposition
156. Most common cause of reflux in child w/ non-duplicated collecting system: Short intramural ureter.
157. Most common cause of renal vein thrombosis in adults : Nephrotic syndrome
158. Most common cause of restrictive cardiomyopathy : Amyloid
159. Most common cause of round pneumonia in children : Streptococcus.
160. Most common cause of round pneumonia in children : Streptococcus
161. Most common cause of small bowel obstruction : Adhesions
162. Most common cause of squamous cell ca. in the renal pelvis : Chronic Infected stag horn calculus
163. Most common cause of stridor in neonate and young infant : Laryngomalacia
164. Most common cause of sudden cardiac death among young people Hypertrophic cardiomyopathy (HCM)
165. Most common cause of SVC syndrome : Bronchogenic carcinoma
166. Most common cause of testicular swelling : Hydrocele
167. Most common cause of the pulmonary-renal syndrome : Microscopic polyangitis.
168. Most common cause of the stripe sign on V/Q scan : COPD
169. Most common cause of thoracic outlet syndrome : Scalene anticus.
170. Most common cause of toxic mega colon : Pseudomembranous colitis.
171. Most common cause of tree in bud appearance on CT : Bronchiolitis
172. Most common cause of tricuspid stenosis : Rheumatic heart disease
173. Most common cause of unilateral diaphragmatic paralysis : Malignant invasion
174. Most common cause of unilateral nonperfused lung on V/Q scan : Bronchogenic carcinoma
175. Most common cause of unilateral pulmonary edema : Prolonged unilateral dependent positioning
176. Most common cause of urinary obstruction in boys : posterior urethral valves
177. Most common cause of valvular heart disease in the United States : Degenerative
178. Most common cause of vascular ring : Double arch.
179. Most common cause of vertebra plana in children : EG
180. Most common cause requiring bronchial artery embolization : CF
181. Most common cause worldwide for cholangiocarcinoma : Clonorchis sinensis infestation
182. Most common cerebellar neoplasm in children : Medulloblastoma
183. Most common cerebral mass lesion in AIDS : Toxoplasmosis
184. Most common chest radiograph finding seen in pts with an acute PE : Atelectasis
185. Most common chest x-ray abnormality in the ICU : Atelectasis
186. Most common child abuse facture : Diaphyseal fracture,
187. Most common collagen disorder for a pleural effusion : SLE
188. Most common colonic polyp : Hyperplastic polyp
189. Most common colonic site for lymphoma : Cecum
190. Most common complication of ERCP : Pancreatitis
191. Most common complication of popliteal artery aneurysm : Distal ischemia (thrombosis/embolism)
192. Most common complication with IVC filters : DVT.
193. Most common component of mixed germ cell tumors : Embryonal Cell Carcinoma
194. Most common congenital abnormality of GI tract : Meckel’s diverticulum
195. Most common congenital anomaly of CNS in live births : Myelomeningocele
196. Most common congenital defect of CNS : Anencephaly.
197. Most common congenital head and neck cyst in a child : Thornwaldt cyst
198. Most common congenital heart disease : Bicuspid aortic valve.
199. Most common congenital intracranial tumor : Epidermoid or inclusion cyst
200. Most common congenital lesion of bile ducts : Choledochal Cyst
201. Most common congenital skeletal dysplasia : Achondroplasia.
202. Most common congenital solid tumor in the newborn : Sacrococcygeal Teratoma (1:40K live births)
203. Most common cranial nerve affected by a pituitary macroadenoma : CN VI.
204. Most common cranial nerve to be affected with schwannoma : VIII
205. Most common craniofacial malformation : Facial Clefting
206. Most common crystalline arthropathy : CPPD
207. Most common CT finding in bowel ischemia : Bowel wall thickening.
208. Most common cyanotic congenital heart malformation beyond neonatal period : TOF
209. Most common cyst of the jaw : Radicular cyst = Periapical cyst
210. Most common cystic lesion of prostate : Cystic degeneration of BPH
211. Most common cystic tumor of pancreas : Mucinous cystic neoplasm
212. Most common diffuse breast disorder : Fibrocystic disease of breast.
213. Most common diffuse gray matter degenerative disease : Alzheimer’s
214. Most common dislocated auditory ossicle longitudinal temporal bone fracture : Incus
215. Most common dislocation in adult : Glenohumeral.
216. Most common dislocation in child : Elbow.
217. Most common epididymal neoplasm : Adenomatoid tumor
218. Most common estrogenic ovarian tumor : Granulosa Cell Tumor
219. Most common etiology for chronic temporal lobe epilepsy : Ganglioglioma
220. Most common etiology for multiple small gastric polyps : Hyperplastic polyps.
221. Most common etiology for osteomyelitis : Staphylococcus aureus.
222. Most common etiology of bilaterally enlarged, hyperechoic kidneys in newborn infant : ARPKD.
223. Most common etiology of mesenteric adenitis : Viral
224. Most common etiology of pneumomediastinum : Alveolar rupture.
225. Most common etiology of rickets : Vitamin D deficiency.
226. Most common extra-adrenal site of pheochromocytoma : Organ of Zuckerkandl.
227. Most common extraaxial neoplasm of CNS : Meningioma
228. Most common extragonadal site of primary germ cell tumors : Anterior mediastinum.
229. Most common extrapulmonary site of tuberculosis : Urinary tract
230. Most common fetal cardiac anomaly seen on 4 chamber view US : AV canal defect (aka ECD)
231. Most common fibromatosis in childhood : Infantile Myofibromatosis
232. Most common finding of a tubal pregnancy seen on US images Adnexal mass separate from ovary
233. Most common finding of contralateral kidney in MCKD : Reflux
234. Most common fluid collection seen in transplant patients : Lymphoceles.
235. Most common form of aortic stenosis : Valvular
236. Most common form of carpal instability : DISI
237. Most common form of emphysema in alpha-1 antitrypsin deficiency : Panlobular emphysema
238. Most common form of emphysema in nonsmokers : Panlobular emphysema
239. Most common form of emphysema in smokers : Centrilobular emphysema
240. Most common form of hypertrophic cardiomyopathy : Asymmetric involvement of the interventricular septum
241. Most common form of skeletal dysplasia : Acquired skeletal dysplasia.
242. Most common form of systemic vasculitis in adults : Giant cell (temporal) arteritis
243. Most common fracture of forearm : Colles
244. Most common functional tumors of the ovary : Sex cord–stromal tumors
245. Most common fungal infection in AIDS : Cryptococcus.
246. Most common genitourinary organ affected by neurofibromas : Urinary bladder
247. Most common germ cell tumor associated with excessive hCG production :Choriocarcinoma.
248. Most common germ cell tumor associated with excessive hCG production after choriocarcinoma : Dysgerminoma.
249. Most common GI neoplasm : Adenoma
250. Most common GI tract location for primary extranodal lymphoma : Stomach, usually NHL type.
251. Most common glial tumor in adults : Ependymoma
252. Most common glial tumor in NF 1 : JPA.
253. Most common glial tumor with microcalcifications : Oligodendroglioma
254. Most common gynecologic neoplasm : Uterine Leiomyoma
255. Most common hereditary hypercoagulable condition : Factor V Leiden
256. Most common hereditary leukodystrophy : Metachromatic leukodystrophy
257. Most common histologic type of bronchogenic carcinoma associated with cavitation : Squamous
258. Most common histologic type of bronchogenic carcinoma associated with pancoast tumor : Squamous
259. Most common histologic type of bronchogenic carcinoma associated with pleural effusion : Adenocarcinoma
260. Most common histologic type of lung cancer associated with asbestosis exposure : BAC
261. Most common histologic type of primary cutaneous lymphoma :T-cell lymphoma
262. Most common ILD to be found in association with collagen vascular disease : NSIP
263. Most common indication for percutaneous vertebroplasty : Osteoporosis.
264. Most common infection to cause cerebellar hypoplasia & migration anomalies : CMV
265. Most common infratentorial neoplasm in an adult : Metastases
266. Most common inherited disease among Caucasian Americans : CF
267. Most common internal enhancement pattern in DCIS with non mass like enhancement : Clumped enhancement
268. Most common intracranial for site of teratomas : Pineal region.
269. Most common intracranial presentation of TB : Tuberculous meningitis.
270. Most common intramedullary spinal neoplasm in adults : Ependymoma of Spinal Cord
271. Most common intramedullary tumor in children : Astrocytoma
272. Most common intramedullary tumor of adults : Ependymoma.
273. Most common intraocular neoplasm in childhood : Retinoblastoma
274. Most common intraorbital tumors found in adults : Cavernous hemangiomas.
275. Most common intrathoracic fetal anomaly : Congenital diaphragmatic Hernia
276. Most common intrathoracic foregut cyst : Bronchogenic Cyst
277. Most common intrauterine CNS infection : CMV
278. Most common intravascular venous tumor : Leiomyosarcoma of IVC
279. Most common in-utero renal tumor : Mesoblastic nephroma.
280. Most common invasive gynecologic malignancy : Endometrial malignancy
281. Most common islet cell tumor in MEN 1 : Gastrinoma
282. Most common islet cell tumor of the pancreas : Insulinoma.
283. Most common joint involved in synovial osteochondromatosis : Knee
284. Most common lesion to cause expansion of paranasal sinus : Mucocele
285. Most common lethal bone dysplasia : Osteogenesis imperfecta type II ?
286. Most common liver tumor after metastases : Hemangioma
287. Most common lobe affected in bronchial atresia : Left upper lobe.
288. Most common location for a cephalhematoma : Parietal
289. Most common location for a gastric diverticulum : Posterior wall of the gastric fundus.
290. Most common location for a pilocytic astrocytoma : Cerebellum
291. Most common location for a solitary myeloma of the bone : Thoracolumbar spine
292. Most common location for a synovial sarcoma : Knee
293. Most common location for a Tarlov cyst : Posterior rootlets of S2 + S3
294. Most common location for abdominal sarcoid involvement : Stomach
295. Most common location for atelectatic asbestos pseudotumor : Posteromedial & -lateral basal region of lower lobes
296. Most common location for chordomas : Sacral spine.
297. Most common location for gallbladder perforation : Fundus
298. Most common location for Sclerosing Osteomyelitis of Garré (sterile Osteomyelitis) : Mandible
299. Most common location for typhlitis : Cecum.
300. Most common location for well-differentiated liposarcoma : Thigh
301. Most common location in biliary tree for cholangiocarcinoma : Upper third/perihilar region.
302. Most common location in the spine for an osteochondroma : Cervical (C2) followed by thoracic T8
303. Most common location of a meningioma in the spine : Thoracic spinal cord
304. Most common location of a periurethral diverticulum in a female : Posterolateral.
305. Most common location of an ectopic pregnancy : Ampullary region of the fallopian tube.
306. Most common location of benign and malignant masses in breast : Upper outer quadrant
307. Most common location of bronchogenic carcinoma : Right upper lobe
308. Most common location of coarctation : Postductal beyond the origin of the left subclavian artery.
309. Most common location of coronary calcifications : LAD.
310. Most common location of DAI : Frontotemporal gray–white matter junction.
311. Most common location of GIST : Stomach.
312. Most common location of GU obstruction in a neonatal male : Ureteropelvic junction.
313. Most common location of intracranial dissection : Vertebral arteries.
314. Most common location of intraorbital abscess : Subperiosteal space on medial wall.
315. Most common location of intraventricular meningioma : Atrium of the lateral ventricle.
316. Most common location of oligodendroglioma : Frontal lobe.
317. Most common location of pleomorphic xanthoastrocytoma : Temporal lobes.
318. Most common location of pulmonary sequestration : Posterior medial lower.
319. Most common location of PVNS : Knee.
320. Most common location of sarcoidosis in spinal cord : Cervical.
321. Most common location of the biliary embryonal Rhabdomyosarcoma : CBD
322. Most common location of triquetral fracture is dorsal avulsion
323. Most common location to find a lithopedion : Adnexae
324. Most common location to see intravertebral vacuum phenomenon (Kümmell Disease) : Thoracolumbar junction
325. Most common lung infection in HIV: Bacterial pneumonia
326. Most common lung mass : Granuloma
327. Most common lysosomal storage disorder : Gaucher’s disease
328. Most common malformation associated with callosal agenesis : Dandy-Walker malformation.
329. Most common malignancy of childhood : Leukemia.
330. Most common malignancy of parotid gland in adult : Mucoepidermoid carcinoma.
331. Most common malignant abdominal neoplasm in children 1–8 years old : Wilms Tumor.
332. Most common malignant bone tumor in children : Ewings
333. Most common malignant cause of bilateral global renal enlargement : Lymphoma.
334. Most common malignant neoplasm of diaphragm : Fibrosarcoma.
335. Most common malignant neoplasm of the spleen : Lymphoma.
336. Most common malignant ovarian neoplasm : Serous adenocarcinoma.
337. Most common malignant ovarian neoplasm : Serous cystadenocarcinoma.
338. Most common malignant primary bone tumor in young adults + children : Osteosarcoma
339. Most common malignant radiation-induced tumor of the musculoskeletal system : MFH
340. Most common malignant sex cord–stromal tumor : Granulosa cell tumor
341. Most common malignant testicular neoplasm : Nonseminomatous germ cell tumors
342. Most common malignant tumor affecting ribs of children + adolescents : Ewings Sarcoma
343. Most common malignant tumor of the abdomen in patients with NF1 Malignant peripheral nerve sheath tumor
344. Most common malignant tumor of the duodenum : Adenocarcinoma.
345. Most common malignant tumor of the heart : Angiosarcoma
346. Most common malignant tumor of the small bowel : Carcinoid
347. Most common mammographic finding in DCIS : Microcalcifications
348. Most common mammographic finding in Infiltrating/Invasive Lobular Carcinoma : Architectural distortion.
349. Most common manifestation of asbestosis exposure : Pleural plaques
350. Most common manifestation of asbestos-related pleural disease : Pleural effusion
351. Most common manifestation of blunt chest trauma : Pulmonary contusion
352. Most common mass lesion of the cerebellopontine angle after acoustic schwannoma : Meningioma
353. Most common mediastinal germ cell tumor : Seminoma.
354. Most common mediastinal mass in a child between the ages of 6 & 12 years old : Lymphoma
355. Most common mediastinal neurogenic tumor : Schwannoma
356. Most common mesenchymal origin neoplasm of GI tract : GIST
357. Most common metabolic liver disease in children : Hepatic cirrhosis in homozygous alpha-1 Antitrypsin
Deficiency
358. Most common metastases to the spleen : Breast carcinoma
359. Most common metastasis to the heart : Melanoma
360. Most common metastatic cause of linitis plastica : Breast carcinoma
361. Most common metatarsal to have a stress fracture : Second metatarsal.
362. Most common missed type of breast cancer on mammography : Infiltrating/Invasive Lobular Carcinoma.
363. Most common mitral valve abnormality in the Western world : Non-rheumatic mitral valve disease.
364. Most common monodermal teratoma : Struma ovarii.
365. Most common motor neuron disease : ALS.
366. Most common MR imaging finding in DCIS : Non-masslike enhancement.
367. Most common mycotic pneumonia in an AIDS patient : Cryptococcus.
368. Most common natural outcome of the VSD : Spontaneous complete closure.
369. Most common neonatal cyanotic congenital heart malformation : TGV
370. Most common neonatal lesion of adrenal gland : Nontraumatic Adrenal Hemorrhage.
371. Most common neoplasm of conus medullaris : Myxopapillary Ependymoma of Spinal Cord.
372. Most common neoplasm of internal auditory canal / cerebellopontine angle : Vestibular Schwannoma.
373. Most common neoplasm of the gastrointestinal tract in patients with NF1: Neurofibromas.
374. Most common nerve to be involved in tarsal tunnel syndrome : Posterior tibial nerve.
375. Most common nonepidemic meningoencephalitis in immunocompetent individuals in US : Herpes Encephalitis.
376. Most common nonepithelial malignant bladder tumor : Leiomyosarcoma.
377. Most common nonepithelial tumor in the colon : Lipoma.
378. Most common nonepithelial tumor of the bladder : Leiomyoma.
379. Most common nonglial primary tumors of the central nervous system : Meningiomas.
380. Most common nonlymphoproliferative primary malignant tumor of the spine in adults : Chordoma.
381. Most common nonlymphoproliferative primary malignant tumor of the spine in children : PNET.
382. Most common nontraumatic cause of acute limp in a child : Toxic synovitis.
383. Most common non-traumatic cause of facial nerve paralysis & hearing loss : CPA tumor.
384. Most common odontogenic mass : Odontoma= odontogenic hamartomatous malformation.
385. Most common of all alimentary tract duplications : Small Bowel Duplication Cyst.
386. Most common of cerebral vascular malformation : DVA.
387. Most common opportunistic infection in AIDS : Toxoplasmosis.
388. Most common organism involved in pancreatic abscess : E. Coli.
389. Most common organism of acute pyogenic meningitis in infants & children : N. meningitides.
390. Most common origin of cystic artery : Right hepatic artery.
391. Most common osteochondrodysplasia : Hereditary Multiple Exostoses
392. Most common ovarian neoplasm : Dermoid aka dermoid cyst = Mature cystic teratoma
393. Most common ovarian tumor-related morbidity : Bowel obstruction
394. Most common pancreatic abnormality in adult pt's with CF : Complete fatty replacement
395. Most common paraneoplastic disease associated with thymoma : Myasthenia gravis
396. Most common parasitic infection involving CNS in developing countries : Cysticercosis
397. Most common parotid disease in children : Mumps parotitis.
398. Most common pattern of bronchial arteries : Two left & one right bronchial artery
399. Most common pattern of enhancement at DE MR cardiac imaging : Patchy midwall enhancement with multiple
foci
400. Most common pattern of hepatic involvement of secondary lymphoma : Diffuse infiltrative
401. Most common pattern of spread in Gallbladder Carcinoma : Direct spread.
402. Most common pediatric glioma : JPA
403. Most common pediatric tumor causing isosexual precocious puberty in a girl : Granulosa cell tumor
404. Most common phakomatoses : NF1
405. Most common pineal tumor : Pineal Germinoma
406. Most common predisposing cause to develop pneumothorax during percutaneous lung biopsy : COPD
407. Most common predisposing disorder of secondary spontaneous pneumothorax : COPD
408. Most common pregnancy-related mortality in the first trimester Ectopic pregnancy
409. Most common presentation for idiopathic pulmonary fibrosis : Dyspnea
410. Most common presentation in stuck twin syndrome : Monochorionic diamniotic
411. Most common presentation of bronchoalveolar cell carcinoma (BAC) : Solitary pulmonary nodule.
412. Most common presentation of GIST on cross sectional imaging : Cystic areas of necrosis.
413. Most common presentation of mesoblastic nephroma : Palpable mass at birth.
414. Most common presentation of neurocysticercosis : Seizures.
415. Most common presenting symptom of Osler Weber Rendu : Hemoptysis.
416. Most common primary benign mesenteric tumor : Desmoid.
417. Most common primary brain tumor : GBM.
418. Most common primary cardiac tumors in adults : Myxomas.
419. Most common primary cerebellar mass in an adult : Hemangioblastoma
420. Most common primary demyelinating disease : MS
421. Most common primary female urethral malignancy : Squamous cell carcinoma
422. Most common primary hepatic neoplasm in infants & children <5 years old : Hepatoblastoma
423. Most common primary intraocular neoplasm in adult Caucasian : Uveal Melanoma
424. Most common primary lung tumor under age 16 : Bronchial Adenoma
425. Most common primary malignant rib tumor : Chondrosarcoma
426. Most common primary malignant sacral tumor : Sacrococcygeal Chordoma
427. Most common primary malignant soft-tissue tumor of late adult life : Soft-tissue MFH
428. Most common primary neoplasm of the spleen : Cavernous hemangioma
429. Most common primary neoplasms of the anterior superior mediastinum Thymomas.
430. Most common primary posterior mediastinal neoplasms :Neurogenic tumors
431. Most common primary tumor of the diaphragm : Lipoma
432. Most common radiation-induced CNS tumor : Meningioma
433. Most common reason for cardiac transplantation : Dilated cardiomyopathy
434. Most common recognized CNS manifestation of VHL disease : Hemangioblastoma of CNS
435. Most common relevant finding on cavogram for IVC filter placement : Circumaortic left renal vein.
436. Most common renal fusion anomaly : Horseshoe kidney
437. Most common renal mass in a 3 months old infant : Mesoblastic nephroma
438. Most common respiratory cause of cold agglutinin production : Mycoplasma pneumonia
439. Most common retinal infection in AIDS : Toxoplasmosis
440. Most common right cardiophrenic angle mass : Epicardial fat-pad/lipoma
441. Most common segment involved in tracheobronchial injury : Right lower lobe bronchus.
442. Most common sex cord-stromal cell tumor : Ovarian Fibroma
443. Most common sign of failing dialysis graft : Increased venous pressures
444. Most common sign of tuberous sclerosis : Myoclonic seizures
445. Most common single cause of breast lumps in females between 35 to 55 years of age : Breast cyst
446. Most common site for an intracardiac papillary fibroelastoma : Aortic valve.
447. Most common site for aneurysm in the chest : Descending thoracic aorta.
448. Most common site for cardiac myxoma : Left atrium
449. Most common site for intra cardiac thrombus formation : Atrial appendage.
450. Most common site for optic melanoma metastases : Liver.
451. Most common site for penetrating aortic ulcers : Descending thoracic aorta
452. Most common site of abdominal involvement in Hodgkins disease : Spleen
453. Most common site of aortic dissection : Prox. Desc. Thoracic aorta near ductus lig. attachment
454. Most common site of biliary tract injury caused by blunt abdominal trauma : Gallbladder
455. Most common site of monostotic fibrous dysplasia : Ribs
456. Most common site of rupture of sinus of Valsalva aneurysm : RV followed by RA.
457. Most common solid extracranial tumor of childhood : Neuroblastoma
458. Most common spermatic cord tumor : Lipoma
459. Most common spinal cord segment of lymphoma of spinal cord : Cervical
460. Most common spinal cord tumor : Ependymoma
461. Most common spinal location for cord astrocytoma : Thoracic
462. Most common spinal location for cord ependymoma : Cervical
463. Most common subcortical degenerative disease : Parkinson’s
464. Most common subglottic soft-tissue upper resp. tract obstructing mass in neonates : Subglottic Hemangioma
465. Most common submucosal tumor in colon : Lipoma
466. Most common subtype of NHL involving the esophagus : Diffuse large B-cell lymphoma
467. Most common subtype of renal cell carcinoma : Clear cell adenocarcinomas
468. Most common suprasellar mass : Craniopharyngioma
469. Most common syndromic islet cell tumor : Insulinoma
470. Most common systemic allergic hypersensitivity-related acute small-vessel vasculitis in children : HSP
471. Most common systemic fungal infection in immunocompromised patients : Candidiasis Of Liver
472. Most common tarsal bone to get fractured : Calcaneus
473. Most common tarsal coalition : Talocalcaneal
474. Most common testicular tumor in a young boy : Yolk sac tumor
475. Most common tibial plateau fractures : Lateral tibial plateau (Schatzker classification type I–III)
476. Most common trigonal intraventricular mass in adulthood : Meningioma
477. Most common tumor of adenohypophysis : Pituitary Adenoma
478. Most common tumor of genitourinary tract : Metachronous TCC
479. Most common tumor of the appendix : Carcinoid
480. Most common tumor of the esophagus : Leiomyomas
481. Most common tumor of the minor salivary glands : Adenoid Cystic Carcinoma
482. Most common type of abdominal wall hernia : Inguinal hernia
483. Most common type of ASD : Ostium secundum
484. Most common type of brain hernaition : anterior / uncal transtentorial
485. Most common type of brain herniation : Subfalcine herniation
486. Most common type of C2 fractures : Type 2
487. Most common type of cancer to arise from a thyroglossal duct cyst : Papillary carcinoma
488. Most common type of cardiomyopathy : Dilated cardiomyopathy
489. Most common type of choledochal cyst : fusiform dilatation of the extrahepatic duct Type 1c
490. Most common type of congenital internal hernia : Left paraduodenal hernia
491. Most common type of encephalocele in SE Asia: Sincipital Encephalocele
492. Most common type of encephalocele in US : Occipital Encephalocele
493. Most common type of endoleak in the abdominal aorta : Type II endoleak
494. Most common type of endoleak in the thoracic aorta : Type I endoleak
495. Most common type of fracture of the proximal 5th metatarsal bone : Peroneus brevis avulsion fracture.
496. Most common type of gallbladder inflammation : Chronic cholecystitis
497. Most common type of internal hernia : Postoperative, transmesenteric hernias.
498. Most common type of intrapulmonary involvement of Hodgkins disease : Bronchovascular form.
499. Most common type of liver abscess : Pyogenic Liver Abscess
500. Most common type of lymphoma involving the head and neck region : Diffuse large B-cell lymphoma

1 note
·
View note
Text
Chondroblastoma of the Medial Malleolus: A Very Rare Case with Radiopathological Correlation

Chondroblastoma of the Medial Malleolus: A Very Rare Case with Radiopathological Correlation in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006057.php
Chondroblastoma is an uncommon osseous neoplasm. It accounts for less than 1% of all bone tumors. Tumors of the medial malleolus are rare, and even rarer is the chondrogenic tumors of the medial malleolus [1]. The most common anatomical site involved by this tumor is the proximal humerus, followed by the distal femur, proximal femur, proximal tibia, talus and innominate bone, in descending order. The typical radiological finding is an eccentric osteolytic lesion, frequently accompanied by a thin sclerotic rim [2,3]. The male to female ratio is greater than 2:1, with peak incidence at age of 16 years. The proximal tibia is the most common location; but there is near even distribution of cases between the proximal tibia, proximal humerus, proximal femur, and distal femur [4-6]. Malignant transformation in chondroblastoma has been described in only a few cases [7]. Patients usually present with pain and swelling, particularly if a pathological fracture is present [8]. Chondroblastoma is usually treated by simple curettage with bone grafting [4,9].
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#Biomedical Journal Articles#Bio-psychological Medicine#Journals on Vaccination#journal of biomedical sciences research review#biomedical journal impact factor
0 notes
Text
What Is Osteosarcoma? What Kinds of Symptoms Does It Cause?

Osteosarcoma is a type of bone cancer that can occur in people of any age. But it is generally more commonly found in adolescents and young adults who are starting to go through puberty. It’s not usually diagnosed until after the patient has already developed symptoms.
What causes osteosarcoma?
Some rare types of cancers cause bone breaks, or osteosarcomas. This makes up about 2% of all cancer diagnoses each year.[1] The major risk factors for this type of cancer are being exposed to high levels of radiation, having a family history of osteosarcoma, and having endocrine-disrupting hormones (like some birth control pills) taken by patients with osteosarcoma. If you are at a higher risk of developing osteosarcoma than others, there may be several warning signs you should watch out for before the disease becomes worse. Treatment involves changing your lifestyle and getting regular checkups with a doctor.
How do I tell if my child has osteosarcoma? One of the first signs a child may have osteosarcoma is a broken arm, leg, or hip. Your child may also complain about pain in his or her jaw or bone in his legs. Children who have these symptoms often receive an “open surgery.
What is the average survival time for children with osteosarcoma?
The survival time for children with osteosarcoma is only 20 months, compared with around two years for those without disease, according to Jain Dhanalakshmi MD, author of 'Osteosarcoma in Young Adults'. For this reason, doctors sometimes call osteosarcomas "young adult disease." There is also little information available about how long children with osteosarcoma will live. However, when treatment is given, it usually lasts from 5 to 10 years, depending on the stage and type of treatment. A recent study found the median overall survival was 10 years in children treated successfully.[2]
What types does osteosarcoma affect?
Osteosarcomas affect bone and soft tissue. They include both primary (involving the whole bone) and secondary (involving one section of the bone) lesions. Secondary lesions are usually found later in life, and are most frequently observed in older adults. These include fractures caused by a fall or sports injury. Primary lesions, however, usually involve only one part of the bone (such as a femur), but they can occur anywhere in the body, including in your spine. Other examples of primary tumors that can form in the spine include rhabdomyosarcoma, chondrosarcoma, osseous angiosarcoma, and chondroglioma.[citation needed] According to the National Cancer Institute, osteosarcoma occurs at five times more frequently in females than males, and it can appear in various forms, including primary or metastatic. The age group most likely to develop osteosarcoma includes teenagers and young adults and includes individuals who are overweight or obese. Most cases also occur during adolescence, and childhood is rarely associated with the development of osteosarcoma. Secondary bone cancers caused by osteosarcomas, such as osteoblastic sarcoma and osteoblastic hyperplasia, represent only 8% to 18% of the total number of new cancers in adults. [3] People with osteosarcoma are at increased risk of contracting certain types of leukemia, multiple myeloma, and other cancers. An increase in the incidence of osteosarcomas over the past decade has been attributed in part to the increasing age of menarche. In fact, women are now at increased risk of osteosarcoma than men. And because osteosarcoma tends to occur earlier in the growth spurt in girls compared with boys, early diagnosis becomes a key component to managing its impact on the overall health of these teenagers.
What symptoms does osteosarcoma cause?
There are three main features to look for in teenagers and young adults who have osteosarcoma. First, they often complain about pain. Second, if they have a fracture, pain is accompanied by bruising and swelling, often accompanied by fever. Third, this might not get better in a few weeks. Sometimes, the patients will start complaining about unusual weight loss. This can be followed by sudden death within days. Also, in older patients, bone metastases are observed. Osteosarcoma can progress over time to lead to massive destruction of bone or even to cause bone cancer. As a result, you should contact our medical team right away if you notice something out of the ordinary.
What kind of drugs can help with osteosarcoma?
Chemotherapy is still used to treat cancer-related bone disorders. While chemotherapy may not entirely cure osteosarcoma, it helps manage the progression and increases survival rates. Unfortunately, this is usually not possible for every patient. Therefore, while surgery may not completely solve your child's problem, proper medical care and good nutrition can help ensure your child remains healthy long enough for surgery. Since chemotherapy cannot target what causes the disease, it is important to consider the possibility that chemotherapy is contributing to the formation of more cancer cells. If so, you should stop taking this drug and discuss surgery with your insurance provider. Another option is hormone therapy, which improves the production of thyroid hormones. Hormones like estrogen help regulate the bones and muscles so they don't become brittle or calcified; hence, they're useful in preventing osteosarcoma. You might also want to try using a topical corticosteroid for painful and tender areas like the thighs and pelvis. Corticosteroids are relatively safe. Unlike chemotherapy, topical corticosteroids tend to be safer because they don't affect the immune system as much as chemotherapy does. If this doesn't work, you can use radioactive iodine for additional protection against bone damage.
What happens after surgery?
Surgery is one way to combat osteosarcoma. After surgery to remove the tumor, your baby will experience many healing processes that will leave him or her feeling normal again. Depending on the type of the tumor, the recovery period can range from a few days to approximately 6 months to a year. Recovery time may depend on the size of the tumor and the general health of the patient. To reduce postoperative pain, your partner can administer narcotic drugs to help relieve pain by blocking receptors that may be involved in inflammation. For some patients, pain relievers given in small doses may be helpful. In addition, depending on how severe your osteosarcoma symptoms are, you may need to take medications to control pain before returning home. Medications include aspirin, acetaminophen, ibuprofen, and naproxen.
What does surgery mean?
Surgeries can treat various problems, including cancers of the heart and lungs. Any operation will require anesthesia, which can be provided by local or general anesthetic agents. Anesthesia can also be administered via intravenous (IV) lines with oxygen support. Because surgery involves removing part or all of the body, it's best to speak with your surgeon about all the potential consequences and talk to them in advance about whether you want to proceed with undergoing surgery. Before surgical procedures, it's advisable to check your blood pressure. Many patients report improved mental status and reduction of anxiety symptoms after an anesthesia procedure. However, if you experience vomiting or excessive bleeding after surgery, seek emergency medical attention immediately. Also, you should monitor your skin color and the amount of fluid in your body. The last thing you want to worry about when you get back home is sagging skin. Make sure to drink lots of fluids and eat a balanced diet. For most patients, minor surgery is typically able to be reversed after a couple of days, whereas complicated or advanced complications require a longer term of follow-up care. For example, surgery is often recommended for patients with conditions like diabetes. Doctors also perform surgeries regularly to stabilize joints or restore movement after injuries such as strokes. A large variety of options are available for treating osteosarcoma. Whether this process can successfully be reversed depends on how well you handle postoperative side effects. Pain management is another concern for patients with osteosarcoma. If your surgery involves incision, pain medication, or anti-inflammatory drugs, make sure you don't experience postoperative discomfort. When you return home following surgery, you'll want to keep yourself hydrated. Excessive thirst is usually the result of dehydration rather than decreased electrolytes in the body. Drinking plenty of fresh water can help replenish lost minerals after surgery, so be careful about drinking. Finally, it's important to remember that although your body will recover immediately following surgery, you may not feel as completely healed immediately. Some pain medication will take some time to pass into your bloodstream. Always continue to take pain relief medications, especially when you notice increased signs of joint pain.
What are the treatment and prognosis for osteosarcoma?
Once your child is stable, you should discuss the treatment plan with your healthcare provider. Usually, surgery is a safe, effective, and reliable option for treating osteosarcoma. At least half of all patients in the United States have had their tumor successfully removed in the early stages, usually within 1 year. However, surgeons may recommend different treatments, depending on the location of the tumor and overall health of the patient. For example, some children are good candidates for radiotherapy or cry
Conclusion
Osteosarcoma is a type of bone cancer that can occur in people of any age, but is most common in teenagers and young adults. It is a very aggressive form of cancer that can spread quickly to other parts of the body. Symptoms of osteosarcoma include pain in the affected bone, swelling, and fatigue. If you experience any of these symptoms, it's important to see a doctor right away so that you can begin treatment as soon as possible.
0 notes
Text

@theblackdragon-studios @immabethehero @foooxobsessedperson @aspiringcandleartist @osseous-lesion
Who wants to do a cute fall picrew with me? 🥺
🍁🍂 Link here 🍁🍂

Tagging: @wyvernslovecake @averysmolbear @oxygenbefore1775 @humanitys-strongest-bamf @chaotic-on-main @youre-ackermine @mobolanz @bita-bita @satorizz @marleysfinest @nube55 @stoned-eren and anyone who would like to join! :)
441 notes
·
View notes
Text
Back Pain Issues- Causes and Treatments

Back pain is one of the most common problems that have been faced in the present in the age group of 18 and above. The age group was previously considered to be above 40 years. It has been observed that the gravity of back pain fluctuates with respect to its various types.
Types of Back pain and their causes
Somatic Back Pain: under this particular category of somatic back pain, chronic back pain and Fibromyalgia has been taken under consideration. This kind of back pain is generally caused by day-to-day tension and stress. It has been observed in mothers mostly who struggle with young children every day. Moreover, high work pressure and working in shifts is also held responsible for somatic back pain. Sore muscles lead to this kind of back pain.
Osseous Back pain: under this kind of back pain, the most serious one is known as Sciatica or Lumbar Radiculopathy. It has been observed that it is a kind of pain that takes place from the section of the sciatic nerve from the lower back to the tail bone and to the legs. It causes swelling of calf muscles in many cases. It mostly occurs between the age group of 18-35 and seen more in males. It is caused by strain in the back muscle caused due to pregnancy, Spondylolisthesis, and Lumbar spinal stenosis.
Referral Back Pain: Referral pain is caused by various issues regarding organs placed in the back of the human body. It has been observed it Is caused mostly by pregnancy and kidney issues. It is most likely to remain for a longer period of time, and its severity depends on the severity of the organ issues
Back pain that is caused by nerve lesion: Under this kind of back pain, myofascial pain syndrome is observed. It is mostly caused by spinal lesions. Weakness and numbness are felt, along with difficulty in maintaining motor skills.
Treatment of Types of Back pain
Somatic Back Pain: Fibromyalgia and chronic back pain is treatable and are cured with anti-inflammatory drugs, which are non-steroidal. For example, Ibuprofen or Motrin, acetaminophen or Tylenol, and naproxen or Naprosyn. However, in most cases, somatic back pain is cured by itself with time and exercise. Only in case of excessive pain medication is prescribed.
Osseous Back pain: it has been observed that this kind of back pain is self-treated in most cases with the help of various exercises and yoga. The treatment of these kinds of back pain is done with nutrition in order to repair the strain. Medication is often prescribed in case of excessive pain. Neurologists and orthopedists are the medical professionals who take up the treatment for this kind of back pain.
Referral Back Pain: this type of back pain is mostly cured with the cure of the lower back issues. In case of excessive pain, non-surgical methods are taken under consideration, like axial low back pain.
Back pain that is caused by nerve lesion: for the treatment of this kind of pain, NSAIDs are the most frequent methods used. Moreover, staying active and proper rest can be added to its treatment.
4 notes
·
View notes
Photo
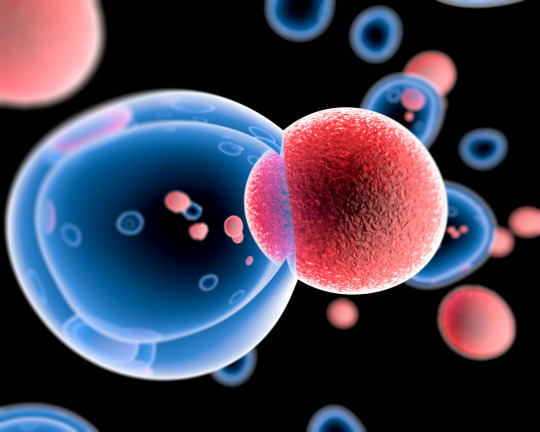
Stem Cell Therapy

Stem cells are the foundation for every organ and tissue in your body. They are the body's raw materials — cells from which all other cells with specialized functions are generated. There are many different types of stem cells that come from different places in the body or are formed at different times in our lives. These include embryonic stem cells that exist only at the earliest stages of development and various types of tissue-specific (or adult) stem cells that appear during fetal development and remain in our bodies throughout life.
Cell therapy involves grafting cells to restore the function of a tissue or organ. The aim is to provide long-term care to the patient through a single injection of therapeutic cells. These cells are obtained from pluripotent (can give all types of cells) or multipotent (can give a limited number of cell types) from the patient himself or from a donor. Under the right conditions in the body or a laboratory, stem cells divide to form more cells called daughter cells. Researchers now know how to differentiate pluripotent cells into several cell types.
People who might benefit from stem cell therapies include those with spinal cord injuries, type 1 diabetes, Parkinson's disease, amyotrophic lateral sclerosis, Alzheimer's disease, heart disease, stroke, burns, cancer and osteoarthritis.
The most used Multipotent stem cells, present throughout the body within the adipose, bone marrow, organ support tissues, but also from bones, cartilage, muscles ... These stem cells are particularly easy to take from adipose tissue or bone marrow. They can give rise to cartilaginous cells (chondrocytes), Osseous (ostheoblasts), fatty (adipocytes), muscle fibers (myocytes), cardiomyocytes ... They also secrete growth factors favorable to the surrounding cells and are sometimes used exclusively for this property. They also produce anti-inflammatory factors, which lead to local immunosuppression and promote the function of cells regulating immunity. These properties limit local inflammation and protect, a priori, against transplant rejection.
Other multipotent cells can be used in cell therapy, such as skin stem cells. The stem cells of the eye make it possible to repair lesions of the cornea. Hematopoietic stem cells from the bone marrow are the source of all blood cells: in the case of hematological cancer, they make it possible to rebuild a stock of healthy blood cells after chemotherapy. Umbilical cord blood contains immune-naive hematopoietic stem cells, and therefore very well tolerated in the event of a transplant. Cord blood is used to treat malignant hemopathies such as leukemia or lymphoma, or genetic diseases like Fanconi anemia. It offers a serious alternative to bone marrow transplantation in the absence of a compatible donor. However, the number of therapeutic cells recovered by cord is low. When therapeutic stem cells are taken from someone other than the patient, they are said to be allogeneic. Their use can pose problems of immune tolerance.
Stem cell therapy, also known as regenerative medicine, promotes the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. It is the next chapter in organ transplantation and uses cells instead of donor organs, which are limited in supply.
The indications for cell therapy are endless and the promise is real in many areas. Clinical fields such as that of neurodegenerative diseases (Parkinson's or Alzheimer's diseases) or muscular degenerations (Duchenne muscular dystrophy) could be concerned if the researchers manage to produce different subtypes of neurons in large quantities and skeletal muscle cells. And how not to also imagine the possibility of producing blood cells, including platelet, in unlimited quantity, to cover the blood needs of hospitals? All assumptions are now allowed.
Stem cell researchers are making great advances in understanding normal development, figuring out what goes wrong in disease and developing and testing potential treatments to help patients. They still have much to learn, however, about how stem cells work in the body and their capacity for healing. Safe and effective treatments for most diseases, conditions and injuries are in the future.
There is certain information you should look into if you are considering a stem cell treatment, including a detailed description of the treatment and the science that supports it, the expected outcome and the risks. It is important to discuss any research or information you gather with your primary care physician and other trusted members of your healthcare team in deciding what is right for you.
CLINICS & DOCTORS LIST
Kristin Comella. PhD | Stem Cell | U.S. Stem Cell, Inc., 13794 NW4th Street, Suite 212 Sunrise, FL 33325
Regenerative Medicine Institute, Vincent Giampapa MD, F.A.C.S. Plastic Reconstructive Surgeon | Stem Cell | 89 Valley Rd, Montclair, NJ, 07042 USA
Advanced Orthopedic Specialists | Stem Cell | Genoa Business Park Drive 2305, Brighton, 48114 Michigan USA
Anatara Medicine & San Francisco Stem Cell | Stem Cell | 1700 California Street, Suite 520, San Francisco, CA 94109 USA
Beatriz Palma-Zevallos, SA-C Cosmetic Surgeon | Stem Cell | 118 S Pendleton St, Easley, SC, USA
Caring Medical & Rehabilitation Services – Chicagoland Office | Stem Cell | North Lake Street. Oak Park 715 Grayslake, 60030 Illinois USA
Darrow Stem Cell Institute | Stem Cell | Wilshere Boulevard 11645, Los Angeles, CA 90025 USA
Jonathan Landow, MD | Stem Cell | 420 Jericho Tpke, Jericho, NY 11753 USA
Manhattan Integrtive Medicine | Stem Cell | 330 West 58th Street, Suite 610, New York, NY 10019 USA
Pangenics Regenerative Center | Stem Cell | 3599 University Blvd, Suite 603, Jacksonville, FL 32218 USA
South Florida Bone Marrow / Stem Cell Transplant Institute, | Stem Cell | Ste 600 10301, Boynton Beach, FL 33437 USA
Stem Cell Carolina | Stem Cell | 7928 Counsel Place, #116 Matthews, NC 28105 USA
Charm – Center for Healing and Regenerative Medicine | Stem Cell | Ranch Road 2222 10815, Austin, TX &8730 USA
UCLA-UCI Alpha Stem Cell Clinic | Stem Cell | University of California Irvine, 845 Health Sciences Road, 1001 Gross Hall Irvine, CA 92697-1705 USA
U.S. STEM CELL, Inc, | Stem Cell | 1560 Sawgrass Corporate Parkway, 4th Floor, FL 33323 USA
U.S. STEM-CELL CLINIC, Michelle Parlo, PA-C Physician Assistant, Beatriz Palma-Zevallos, SA-C Cosmetic Surgeon, Antonio E. Blanco, MD | Stem Cell | 1290 Weston Road, Suite 203A, Weston, FL 33326 USA
INTERNATIONAL CLINICS & DOCTORS LIST
COSTA RICA
REGENERATIVE MEDICINE INSTITUTE, Vincent Giampapa, MD, F.A.C.S. Victor Urzola MD, Estaban Urzola MDS, Richard D. Striano D.C., RMSK, | Stem Cell | Avenida Escazu, Torre Lexus 3rd Floor San Jose, Costa Rica 101017
STEM CELLS TRANSPLANT INSTITUTE, Leslie Mesen MD | Stem Cell | Hospital Cima,Medical Tower II, Office 618, San Rafael, Escazú, San José, Costa Rica
CROATIA
ST. CATHERINE SPECIALITY HOSPITAL - STEM CELL | Stem Cell | Bračak 8, Bračak, 49210 Krapinsko-Zagorska Zupanija, Croatia
INDIA
KOKILABEN DHIRUBHAI AMBANI HOSPITAL | Stem Cell | Swaminarayan Complex Surat, 395001 Gujarat India
JAPAN
OMOTESANDO HELENE CLINIC | Stem Cell | 5-9-15 Minami Aoyama Minato-Ku, Minato, 107-0052 Tokyo Japan
MEXICO
STEM CELL THERAPY TIJUANA MEXICO, Hospital Angeles Tijuana | Stem Cell | Paseo de los Heroes 10999 – 309, Zona Urbana Rio Tijuana, 22010 Tijuana, B.C. Mexico
PROGENCELL – STEM CELL THERAPIES | Stem Cell | Medical clinic, Tijuana, Baja California, Mexico – In Plaza Comercial Pavillion
WORLD STEM CELL CLINIC | Stem Cell | Cancun, Quintana Roo, Mexico
PANAMA
STEM CELL INSTITUTE | Stem Cell | BICSA Financial Tower 63rd Floor, Calle Aquilino de la Guardia, Panama City, Panama
SOUTH AFRICA
THE MELROSE AESTHETIC CENTRE | Stem Cell | 3rd Floor, Medical Centre, Melrose Arch Johannesburg, 2196 Gauteng South Africa
THAILAND
STEMCELLS21| Stem Cell | Soi Ruam 3 Bangkok, 10330 Bangkok Thailand
UK
UK STEM CELLFOUNDATION | Stem Cell | 21 Albermarle Street, London, W1S4BS UK
MEDICA STEM CELLS | Stem Cell | 27 George Street, Marylebone, London, W1U3QA UK
UKRAINE
ILAYA MEDICAL STEM CELL CLINIC, R. Sulik MD & Neurologist | Stem Cell | Ivana Kramskogo Street 9, 03115 Kiev, Ukraine
ABLOU SREM CELL CLINIC | Stem Cell | Voznesens’kyy uzviz 23B, Kyiv – 02000, Ukraine
5 notes
·
View notes