#nonalcoholic fatty liver disease
Explore tagged Tumblr posts
Text
8 Symptoms of Nonalcoholic Fatty Liver | What You Need To Know
#nonalcoholic fatty liver disease#reverse fatty liver#fatty liver disease diet#fatty liver#video#weight loss#lose weight#fatty liver disease
0 notes
Text
I just wanna share a little win today 🥺
It's going to be under the break, though, because there is talk of weight and fat loss. I'm going to try to add correct tags for blocking but if I miss any please feel free to let me know.
So, back in May, I went to the doctor thinking that I would leave with a scheduled gallbladder removal surgery. Instead, I walked away with news of a more complicated-to-resolve condition, Non-Alcoholic Fatty Liver Disease (NAFLD).
I had been on metformin for about a month due to recently discovered insulin resistance that I have likely been struggling with since I was very young, based on symptoms. I've been overweight since I was probably around 5ish.
I had been having symptoms that I believed were a bad gallbladder, my body reacting to the pregnancy hormones that had just dropped, since late February. By May, I was struggling to eat, struggling to stay hydrated, and I was scared. But that was the earliest I could be seen by any doctor.
Since that visit, I've adopted a diet similar to the Mediterranean diet. I don't eat more than 12g of added sugar most days. I don't have more than an oz of dairy. I can't eat almost any of my autism-safe foods because 99% of them were ultra-processed and finding adequate substitutes has been complicated. But I am still eating, and I am doing my best to exercise more than I had been (which was mainly zero, because I was severely depressed).
Well, I did some low-level research so that I could give myself a goal to reach; bc 'lose weight' on its own is discouraging. My wife and I joined a health program that gives you 24/7 access to a health coach and a specialist and they are great at motivating. And, today, I've surpassed my goal of losing 3% of my body fat (by a lot, actually, I don't weigh every day because it stresses me out). This should mean, hopefully, that my liver is now healing itself again because I was in early stages of the disease.
I was nervous about how quickly I'm losing weight at first, but my doctors are not concerned and the combination of meds I'm on facilitate weight loss at least x3, plus I've cut out almost all added sugar, so I'm trying to not be too worried unless the doctors tell me to be. Therefore, if folks comment here, I would very much appreciate not being told I'm losing weight too quickly. I know it's fast. And I am always worried about it in the back of my mind because I know it can also cause problems, but I'm here today to celebrate achieving something I have been fighting for, for the last couple months, and I was told I needed to lose 30lbs this year.

#weight loss#nafld#nonalcoholic fatty liver disease#diet#diet changes#weight loss diet#ed warning#rapid weight loss#metformin
1 note
·
View note
Text
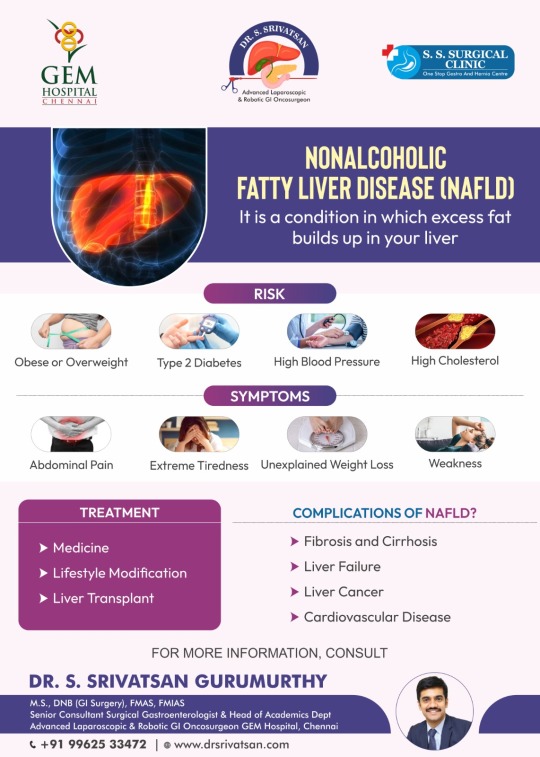
NAFLD: Take Control of Your Liver Health
Learn about Nonalcoholic Fatty Liver Disease (NAFLD), its risks including obesity, type 2 diabetes, and high blood pressure, symptoms like abdominal pain and extreme tiredness, treatment options, complications such as fibrosis and liver cancer, and more. Consult for further details.Consult Today!!!
For more information
Dr. S. Srivatsan Gurumurthy
Senior Consultant Surgical Gastroenterologist & Head of Academics Department and Advanced Laparoscopic & Robotic GI Oncosurgeon
Call: +91 +91 99625 33472
#NAFLD#Nonalcoholic Fatty Liver Disease#Liver Cancer Surgeon in Chennai#Liver Diseases Treatment in Chennai#Liver Transplant Surgery in Chennai
0 notes
Text




#Outlive#peter attia#bill gifford#nonalcoholic fatty liver disease#NAFLD#NASH#alzheimers#cancer#cardiovascular disease#type 2 diabetes#glucose metrics#cirrhosis#liver#inflammation#ALT#obesity#hyperlipidemia#cholesterol#high cholesterol#rising ALT levels#longevity#health#overweight
1 note
·
View note
Text
Understanding Fatty Liver: From AFLD to NAFLD
Your liver is your body's powerhouse, filtering toxins, processing nutrients, and keeping everything running smoothly. But what happens when fat starts to accumulate in this vital organ? It leads to a disease known as fatty liver disease. In this blog, we'll delve into the world of fatty liver, exploring what it is, the different types (including AFLD and NAFLD), and, most importantly, how to treat fatty liver.
What is Fatty Liver?
Your liver is an organ responsible for over 500 bodily functions. One of its key jobs is storing fat, but when too much accumulates, it can lead to fatty liver disease.
Fatty liver disorder means a conditon in which excess fat builds up in your liver cells. It can happen for various reasons. Fatty liver often doesn't cause immediate problems, however, if left untreated, it can progress to serious liver diseases and symptoms, such as liver inflammation and even cirrhosis.
Types of Fatty Liver
There are two main categories of fatty liver disease, differentiated by the root cause of the fat accumulation:
Alcoholic Fatty Liver Disease (AFLD)
As the name implies, alcoholic fatty liver disease is directly linked to excessive alcohol consumption. Heavy drinking over a prolonged period can damage your liver cells. The liver, struggling to keep up with the constant assault of alcohol, starts to malfunction and become inflamed, allowing fat to accumulate and wreak havoc on its delicate processes.
Nonalcoholic Fatty Liver Disease (NAFLD)
Nonalcoholic fatty liver disease is the more prevalent type of fatty liver disease, affecting individuals who don't necessarily consume excessive alcohol. The exact cause of NAFLD remains under investigation, but research suggests a strong link to factors like insulin resistance, obesity, and genetics.
How Do You Treat Fatty Liver?
There's no magic bullet for fatty liver, but a multi-pronged approach can effectively manage the condition and even reverse the fat buildup. Here's a look at some key strategies:
Weight Loss: Shedding even a modest body weight can significantly improve your liver health, whether or not you are diagnosed with nonalcoholic fatty liver. Aim for gradual, sustainable weight loss through healthy eating and exercise.
Dietary Changes: Embrace a balanced diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats to keep your liver happy.
Exercise: Regular physical activity helps burn fat and improve insulin sensitivity. Patients diagnosed with alcoholic and nonalcoholic fatty liver diseases are advised to aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Limit Alcohol: If you have AFLD, abstaining from alcohol is crucial. Even for nonalcoholic fatty liver disease (NAFLD), moderation or complete abstinence is recommended.
Manage Underlying Conditions: If you have diabetes, high cholesterol, or other health conditions contributing to a fatty liver, work with your doctor to manage them effectively with medications.
Conclusion
Alcoholic and nonalcoholic fatty liver diseases are problematic but manageable. Now that you understand the disease and the potential treatments, you know you can take action to improve your liver health. To simplify your journey and get personalised guidance on fatty liver treatments, explore digital healthcare apps that offer resources and support through health monitoring, dietary consultations, and more.
#nonalcoholic fatty liver#fatty liver condition#fatty liver disorder#liver diseases and symptoms#how to treat fatty liver
0 notes
Text
A REGULATED NERVOUS SYSTEM = SUCCESS
This is list of some of the diseases and conditions a women can get due to chronic stress. I have said it before, messing with someone’s nervous system is a form of abuse because it not only deliberately disrupts your mental and emotional stability, it can cause long term harm to your health!!!!
Cardiovascular disease
Hypertension
Stroke
Diabetes
Obesity
Depression
Anxiety disorders
Gastrointestinal disorders (IBS, ulcers)
Autoimmune diseases (lupus, rheumatoid arthritis)
Thyroid disorders (hyperthyroidism, hypothyroidism)
Infertility
Menstrual irregularities
Osteoporosis
Chronic fatigue syndrome
Sleep disorders (insomnia)
Migraine and tension headaches
Fibromyalgia
Alzheimer’s disease and cognitive decline
Eating disorders
Chronic pain disorders
Endometriosis
Polycystic ovary syndrome (PCOS)
Heart arrhythmias
Metabolic syndrome
Adrenal fatigue
Hair loss (telogen effluvium, alopecia)
Chronic inflammation
Eczema and psoriasis
Acne and other skin disorders
Urinary incontinence
Osteoarthritis
Temporomandibular joint disorder (TMJ)
Chronic pelvic pain
Sexual dysfunction
Nonalcoholic fatty liver disease (NAFLD)
Weakened immune system (leading to frequent infections)
Vision problems (stress related blurred vision)
Hearing loss or tinnitus
Substance use disorders
Increased risk of cancer (breast, ovarian)
Hormone imbalances
Gallbladder disease
Hyperprolactinemia
Chronic kidney disease
156 notes
·
View notes
Text
NASH is now called MASH
metabolic dysfunction-associated steatohepatitis (MASH), formerly known as nonalcoholic steatohepatitis (NASH), which has long been recognized as “the hepatic manifestation of metabolic syndrome.”
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a chronic liver disease that occurs when fat builds up in the liver in people who don't drink much or no alcohol. It was previously known as non-alcoholic fatty liver disease (NAFLD)
3 notes
·
View notes
Text
Nonalcoholic fatty liver disease is definitely one of those things you don't want to Google without adding "haes" to the search...
Truly "you should just lose weight" everywhere... You got any other song and dance? No?
Damn I wonder if weight cycling (you know, the thing that happens to like, almost everyone who persistently tries to lose weight) is like. Bad for the liver...
3 notes
·
View notes
Text
Mélovin Health Update: What We Know So Far (11/13/2023)
Okay so normally I'd just reblog the last post I made, but after trawling through countless news/tabloids sites, Reddit, and the cesspool that is Twitter and sorting through the various information available, it seemed more important to make a separate post entirely so people could see.
HERE IS WHAT HAS HAPPENED/WHAT WE KNOW:
-Mel has been diagnosed with a serious illness.
-I cannot *personally* confirm for sure what illness, HOWEVER, most sources are reporting that it is steatohepatitis, a liver condition, sometimes also known as "Nonalcoholic Fatty Liver Disease"
-In essence: this is essentially an inflammation of the liver caused by fat cells building up in said liver, not brought on by drinking alcohol.
-It is considered a metabolic disorder. There are several potential causes, most of which are tied to type 2 diabetes and obesity complications, hormone imbalances such as with the thyroid, but it can also just be bad luck of the genetic draw.
-This is NOT the same condition as viral hepatitis (aka Hepatitis C, etc.) I mention this specifically because some sites are incorrectly reporting this claim and people are already using that misinformation as ammo to be homophobic and claim that he got this condition as a result of his "orientation". Do not do this. Do not be these people.
-Is it terminal or is it incurable? Well, that's the muddied part of this. Even Mel used the term 'terminal' in his Instagram post about this, however many sources seem to point to 'incurable' as a more accurate term. It could be that the words are very similar in Ukrainian and thus the confusion there.
-Note that steatohepatitis *is* incurable, however it *may* or *may not* be terminal/fatal. We don't know how long he's had it, if there was liver damage already present before his being officially diagnosed, and to what extent. The main complications that can lead to death if no treatment is administered are cirrhosis and scarring, even liver cancer, which the only treatment at that point would be a full liver transplant. Without treatment, expectancy is anywhere between 3-5 years in severe cases, or 10-15 in lesser ones. Again, this is not proof of anything yet, this is only the general knowledge I have gained from researching this condition.
-This diagnosis came about as a result of bloodwork when he intended to get some kind of cosmetic procedure.
-(Before anyone asks what cosmetic surgery was he getting - that I don't know, and I don't think anyone else does either. He hasn't said, and cosmetic is a very broad term and can range from anything like traditionally thought-of plastic surgeries to something less intensive like a mole removal or getting his teeth worked on. Personally I think he's too young to be getting cosmetic work done, but that's not important right now.)
-He is seeking/undergoing treatment and currently resting and recovering at home with his family.
-His Instagram is currently private to non-followers, probably to prevent harassment. I have downloaded the video regarding this apparent diagnosis announcement and will try to upload it.
-He is still apparently on the longlist for competing in Vidbir, as announced by Suspilne.
-It is not known if this will impact the release of his newest song or further music going forward.
= o = o = o = o = o = o =
If more develops, I will try to let you all know. Right now, please just try to be supportive, don't harass him or his friends/family for more info (he will no doubt tell us when he is ready), and don't spread wild misinformation. We can only imagine what he must be going through right now. Even if this ends up not being nearly as bad as it sounds, getting a lifelong illness diagnosis is not easy for anyone to handle.
5 notes
·
View notes
Text
2 notes
·
View notes
Text
I suddenly remembered that I also got diagnosed with nonalcoholic fatty liver disease when I had the ultrasound for my gallbladder back in February. And how I've only gained weight since upping the dose of my antidepressant. And how I know I need to be healthier but idk where to start and I'm just so overwhelmed I don't do anything 🙃🙃🙃🙃🙃
#personal#venting#my mom has type 2 diabetes and I know I need to be healthier but omfg. I'm so tired and overwhelmed by it all.#guess I'll just cry at my desk instead
3 notes
·
View notes
Text
I want to try this before returning to FedEx in the winter. It’s really difficult to fast while working there.
2 notes
·
View notes
Text
I technically have a liver disease (nonalcoholic fatty liver) and like, it’s something that’s reasonably easy to “treat” in the sense that it calls for lifestyle changes like more exercise and eating more healthily. But holy shit I’m so stressed about it because I didn’t have great lifestyle habits last year and this year has been a struggle and like I’m trying to get on track with that but I’m crazy paranoid that it’s already too late and I’ve already done irreparable damage to my liver and I’m going to have significant health problems imminently. I know it’s probably just my health anxiety being triggered since that’s the one form of anxiety that’s hard for me to manage but I can’t help it.
Logically I know I’m probably not at a severe point yet because sure I’m overweight and I don’t do a lot of exercise but I don’t drink basically ever, and I’m not experiencing noticeable symptoms that I can’t attribute to anything else…like I’m tired because I don’t have a good sleep routine, I have some isolated yellowish spots on my skin that I can’t be confident aren’t bruises or from something else, my eyes look normal….there’s one symptom that’s been concerning but it’s kinda gross so I’m not going there. But basically there’s only one, maybe two signs that I’m getting worse. And I’m already noticing an improvement in the more gross symptom after a only a few days of one specific change, so…
ugh. On the one hand being very aware of my body is good because it means I’ll probably notice if something’s genuinely wrong. But fuck I hate feeling scared all the time. It’s hard to focus on being in the moment and just making changes now. And I’m scared I’m gonna fall off the wagon again like I have in the past even though I’m in a better place than I was back then
1 note
·
View note
Text
Thanks for the reply. I certainly did NOT miss the point of the call out, I reblogged it because I agree with the same premise that adding to food doesn't take away from what you will have eaten. People should enjoy what they eat.
Along those same lines, I just don't agree with the vitriol about the keto diet and wanted to point out that being being keto doesn't make a person "fucking stupid" nor necessirly unhealthy. My concern was that the distate of the "fucking stupid" person may be justified but their diet got tagged also as "fucking stupid". And then expanding that tag of "fucking stupid" to everyone following a keto diet, Which is not fair. There are plenty of "fucking stupid" Unhealthy Non-Keto people out there, too! :D
I never claimed keto could not aggravate the condition of someone with an already damaged liver or comprimised health. I've seen that study and that lady had litany of health issues and a medication list as long as a scarf that didn't start only when she decided to change her diet. Thus, in her, it did correlate with negative markers of health. And Yes, Correlation and Causation and what not. I totally agree. Yet, then, asking me to prove something "doesn't cause" something else is some sort of fallacy, I am sure. isn't that Burden of Proof? Either such a relationship does not exist or the evidence in support of it is insufficient. And the evidence is certainly INsufficient to claim that a ketonic diet "does cause" *deadly* liver disease in a non-diseased liver. (Unlike how we can clearly see that smoking can cause damage in a healthy lung, but a person who never smokes can also develop lung cancer for other reasons that would also be aggravated if they started smoking...)
Meanwhile, I can also point to a March 2020 study that showed evidence of a ketogenic diet being an effective treatment for hepatic steatosis, aka Non Alcoholid Fatty Liver Disease in people who already had a damaged liver. It led to an improvement in all the markers concerning NAFLD , and not just one but 10 people were observed. That is Evidence of a Positive Claim, in general.
My Point was Keto doesn't cause deadly liver disease. Just becuz some guy was "fucking stupid" and also Keto, don't throw everyone else Keto to the fire. Keep Him in his stupid little box where he belongs, and the rest of us can agree to Enjoy Our Food and Let Others Enjoy Theirs. Cheers.
Reference Study:

159K notes
·
View notes
Text
How to Improve Gut Health for Diabetics
Researchers have studied the interaction between gut health and the role it plays in the development of diabetes. Ten types of bacteria were discovered to be associated with lowering fluctuating blood sugar levels.

So, it makes sense to increase the number of these bacteria to influence sugar levels in diabetic patients.
In this post, we will highlight how gut health affects diabetic symptoms.
Is diabetes related to gut health?
The simple answer is yes. Diabetes is the leading cause of gastroparesis, a condition in which food remains in the stomach for too long. It is also responsible for a host of other diseases, such as diabetic enteropathy, nonalcoholic fatty liver disease, nerve issues in the esophagus, cirrhosis of the liver (scarring of the liver), and hepatitis C (Infection of the liver).
Let’s discuss how diabetes can cause some of these diseases:
Gastroparesis
The vagus nerve is a major nerve in the gastrointestinal tract (GIT), and it signals the muscles to push food from the stomach to the small intestine. Diabetes is known to damage nerves due to the excess sugar content in the body. When this nerve is damaged, the food you eat slows down or stops moving on its way to the small intestine. This condition is known as gastroparesis, and it is more common in women than in men. Some symptoms of this condition include feeling full after a few bites of food, bloating or discomfort after a meal, upper stomach ache, and nausea.
Diabetic Enteropathy
Enteropathy is a disease of the intestine, and it can be a follow-up to gastroparesis. If you’ve had diabetes for a long time, you’re likely to have issues with your small intestine, colon, or rectum. A slowing down of food processing in the body leads to constipation and can be a breeding ground for unhealthy bacteria. This can lead to diarrhea, a common symptom of enteropathy. Diabetic enteropathy might also be characterized by stool leaking from your rectum or an inability to control bowel movements, which will get worse after you eat.
Nonalcoholic fatty liver disease
You are at risk of nonalcoholic fatty liver disease if you have diabetes. This condition is characterized by a buildup of fatty tissues around the liver and can be similar to liver damage in people given to alcoholism. This condition makes it harder to control diabetes as the liver is responsible for processing insulin. Many patients with this condition do not have direct symptoms but experience tiredness or notice tenderness in the right upper side of the stomach.
How to know if I have an unhealthy gut
When your gut functions properly, your body can metabolize food and provide you with energy from the foods you eat, boosting your mood and protecting you from diseases.
An unhealthy gut is marked by a number of signs like:
Fatigue
If you experience chronic fatigue, you may have imbalances in your gut. A study showed that people who experienced fatigue suffered from irritable bowel syndrome (IBS), a condition affecting nearly 70 million Americans.
Insomnia
An unhealthy gut can be the reason why you find it hard to sleep. The majority of the body’s serotonin, which affects mood and sleep, is produced in the gut. An unhealthy gut consists of an overgrowth of bacteria or an inflammation in the gut, which affects your sleep as well.
Food cravings
Eating sugary foods can result in the growth of bad bacteria in the gut. These bad bacteria feed on sugar and can cause extreme sugar cravings. High amounts of sugar, especially high fructose, can cause inflammation and put you at risk of other diseases.
Skin irritations
Your skin reflects your gut health. Excess bad bacteria in your gut throws off your body’s pH levels, resulting in skin issues like eczema, acne, and psoriasis.
Migraines
Studies suggest that people with regular headaches are more likely to have gastrointestinal diseases as a root cause. An unhealthy gut may suffer inflammation, which results in dehydration and is a direct cause of headaches.
Best foods for better gut health
Your gut is full of microbes that favorably or unfavorably influence your gut health. Some of them were passed to you through your mother at birth, but a majority of them come from what you eat.
Here are some foods that can give you a more flourishing guy health:
Eat more plants
Dr Tamara Freuman, a nutritionist who specializes in digestive disorders, confirms that a diet rich in plant fiber can influence microbiome diversity in the gut. Plants are rich in fiber, a good source of good bacteria. Fermentable fibers are more advantageous as they support the growth of gut microbiomes while reducing unfavourable bacteria and reversing diabetic symptoms. Such fibers can be found in oats, beans, cashews, and yams.
Unsaturated fats
Replacing saturated fats with unsaturated fats not only improves your heart health but your gut health as well. Unsaturated fats protect your gut from microbes that cause insulin resistance. Steaks high in saturated fats contain a compound called endotoxin, which causes inflammation and damages insulin receptors. Trade foods high in saturated fats like beef, lamb, pork, cheese, and butter with unsaturated fat sources like nuts, olives, avocados, and seeds.
Nuts
Nuts are rich in fiber and unsaturated fats and can prevent diseases with a special substance called polyphenols. These polyphenols also feed gut bacteria in the large intestine. In a 2018 study, it was discovered that people who ate up to 1½ounces of walnuts per day for eight weeks increased the number of good gut bacteria. These bacteria also produce byproducts like butyrate, which nourishes the large intestine and helps it fight off diseases. Butyrate is also capable of fighting off colon cancer.
Low-fructose fruits
If you’re prone to bloating or gas, consider reducing your fructose intake or fruit sugar. This form of sugar is present in apples, pears, and mangoes. Fruits like berries, bananas, and some citrus fruits have low fructose and are less likely to produce gas. Bananas are rich in fiber and contain inulin, a substance that stimulates the growth of good bacteria.
FAQs
Does probiotics reduce diabetes?
Probiotics may help reduce blood sugar and even improve gut health. However, you should consult your doctor before taking them, especially if you are already taking medication for diabetes.
What supplements help diabetes?
Vitamin D, chromium, magnesium, berberine, and even Cinnamon supplements can help lower blood sugar and improve diabetic conditions.
Wrapping up
Gut health can directly affect diabetic conditions, and patients can alleviate their symptoms by making diet changes. Diets rich in fiber, unsaturated fats, and low fructose are better ways of managing diabetes and even putting you on the path to recovery.
If you notice any signs of an unhealthy gut, especially if you are diabetic or pre-diabetic, speak to a medical professional and take steps to restore your good gut bacteria.
Source: https://cashnowforteststrips.com/how-to-improve-gut-health-for-diabetics/
0 notes