#neurofibromatosis type 2
Explore tagged Tumblr posts
Text

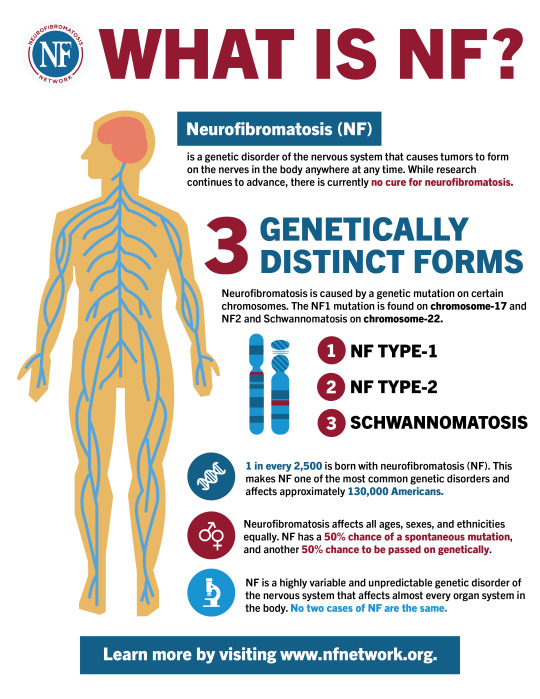
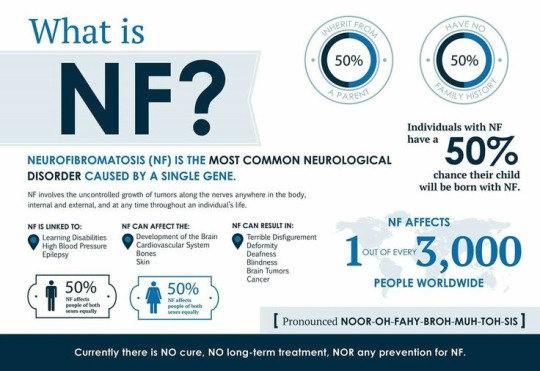
May is Neurofibromatosis (NF) awareness month
NF is a set of 3 complex genetic condition that causes benign tumours to grow on the body.
NF 1 is the most common effecting around 1 in 2500 (AU). It causes benign tumours known as neurofibromas, café-au-lait marks. These benign tumours can appear anywhere from the spinal cord, optic nerve, neck, arms, stomach etc. It can also cause learning disability’s. NF 1 extremely variable condition with some being able to live their life unaffected and others it could debilitating and in some cases life threatening.
NF 2 affects approximately 1 in every 25,000-40,000 people (AU). It is characterised by d by the development of tumours called vestibular schwannomas on the 8th cranial nerve. It can also lead to begin tumours on the brain and spinal cord.
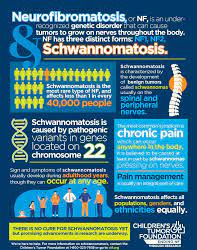
Schwannomatosis is the rarest form of neurofibromatosis and has only recently been identified as a separate condition. It affects less than 1 in every 40,000 people and causes the development of tumours called schwannomas to form on nerves on the spine and other peripheral nerves.
I have NF1.
Information from
#neurofibromatosis#nf#nf1#nf2#schwannomatosis#children’s tumor foundation#awereness#may is NF awerness month#neurofibromatosis type 1#neurofibromatosis type 2
24 notes
·
View notes
Text
When your disability isn't classified as a disability because it can affects people in different various ways. When people with it will have almost no effects and all while others are extremely affected. When it can be both visible and invisible at the same time. When your disability can also lead to things such as an increased chance of being neurodivergent, mental health issues, physically disabilities, learning disabilities, non-cancerous tumors, cancerous tumors but people with the same condition can not be affected at all or if so very limited. But you also don't know how it may effect you since you don't know what it would be like without it.
It is really confusing.
Welcome to Neurofibromatosis
"low support needs disabled people are often not believed to have a disability at all and therefore struggle to get accommodations."
"high support needs disabled people's accommodations are often seen as 'too much' and therefore are not met."
"neurodivergent people's needs are often dismissed because nothing is physically wrong with them."
"physically disabled people people often cannot physically access buildings and people refuse to do anything about it."
"invisibly disabled people are seen as lazy by society."
"visibly disabled people are ostracized from society."
IT'S ALMOST LIKE THERE'S NO SUCH THING AS A SOCIALLY ACCEPTABLE DISABILITY
#this is mainly type 1 but also can be the same thing for type 2 and schwannomatosis#like for me i struggle with learning#sorry for my mini rant#nf1#neurofibromatosistype1#neurofibromatosis#neurofibromatosis type 2#neurofibromatosis awareness#nf2#schwannomatosis#adhd#like idk
36K notes
·
View notes
Text
Meet the makeup wizard who transformed Sebastian Stan into ‘A Different Man’

By Josh Rottenberg
At the tender age of 5, Mike Marino saw “The Elephant Man” for the first time and his life was forever changed. When David Lynch’s haunting and heartbreaking story of the disfigured John Merrick would air on HBO in the early 1980s, Marino found himself horrified but unable to look away, sparking a fascination with prosthetics that would eventually lead him to becoming one of Hollywood’s top makeup artists.
“I was so afraid of it, but little did I know how beautiful that story was and how much of an imprint it would leave on my brain and soul,” says Marino, 47, who earned consecutive Oscar nominations in 2022 and 2023 for his makeup work on “Coming 2 America” and “The Batman,” the latter starring a totally transformed Colin Farrell. “If it wasn’t for that film, I wouldn’t be doing what I’m doing.”
But for actor, TV presenter and disability rights advocate Adam Pearson, Lynch’s film took on a more painful role in his life. Growing up in England with neurofibromatosis type 1, a rare genetic disorder that causes tumors to grow on his face, Pearson was often taunted by classmates who cruelly called him “Elephant Man” and other names. As he got older, he saw how movies routinely depicted people with disfigurements as freaks, villains or victims, stripping away their humanity. “There’s an element of laziness to it,” says Pearson, 39. “How do we show this character is evil? Let’s slap a scar on them.”
Now, through a twist of fate, the lives of Marino and Pearson have intersected on a very different project: the darkly funny, mind-bending psychological thriller “A Different Man.” Directed by Aaron Schimberg, the A24 film stars Sebastian Stan as Edward, a shy, disfigured actor working in New York City who undergoes an experimental procedure to transform his appearance, only to find himself losing the role he was born to play — himself — to a cheerful, outgoing man named Oswald with his same facial deformity, played by Pearson. Renate Reinsve (“The Worst Person in the World”) co-stars as a playwright whose latest work brings Edward’s identity crisis to a head.

“A Different Man,” which The Times called “a self-deconstructing meta-pretzel of a dark comedy” following its debut at this year’s Sundance Film Festival, tackles complex themes of identity, beauty and disability with a blend of Charlie Kaufman-esque surrealism and David Cronenbergian body horror. Along with Stan’s performance, Marino’s meticulously crafted prosthetics are key to bringing Edward and his inner agonies to life, reflecting the deeper emotional anguish of a man trying to escape his own skin.
“The movie portrays how the shell of who we are should not dictate our spirit and our personality,” Marino says. “I think it’s a very important film, much like ‘The Elephant Man’ was.”
When Schimberg first wrote the script, inspired by his own struggles with a cleft palate and his experience working with Pearson on his 2019 satire “Chained for Life,” he initially had no idea how he would actually pull off the film’s demanding prosthetics work. “I was sort of blissfully ignorant,” says Schimberg. “After Sebastian came aboard, we started cobbling the film together very quickly. It was only about a month before shooting that I realized this film was going to completely fall apart if we didn’t get this right. It was very down to the wire.”
Signing on as an executive producer for the film, Stan asked around about makeup artists in the New York area who could handle such a difficult job under that kind of time pressure. One answer consistently came back: “Literally everyone, hands down, was like, ‘You’ve got to get Marino,’ ” the actor recalls.

Though he was already busy with a job on “The Marvelous Mrs. Maisel,” Marino, who has done his share of more fantastical creatures, leapt at the challenge of re-creating a real-life disfigurement like Pearson’s. “I’m fascinated with people that have something going on with their skin because it’s just the most interesting, artistic, natural thing,” Marino says. “For me, there’s an amazing beauty to how Adam looks. This was not about a scary face or a monstrous person. I don’t like to do things like that with no soul or purpose.”
Marino’s passion for makeup and prosthetics took root early in life, inspired by industry legends like Dick Smith (“The Exorcist”) and Rick Baker (“An American Werewolf in London”). Growing up in New York, Marino started honing his skills as a preteen by practicing on his friends with latex, foam and various chemicals, destroying his bedroom rug in the process, to the chagrin of his parents. While still in high school, he mailed his portfolio to Smith and received encouragement and advice by phone from the makeup legend, who won an Oscar in 1985 for “Amadeus” and earned an honorary Academy Award for his life’s work in 2012. “Once he acknowledged me, it was like, OK, this is serious. There was no stopping me.”

After cutting his teeth on “Saturday Night Live” and “Buffy the Vampire Slayer,” Marino broke into film with the 2007 psychological thriller “Anamorph” and quickly became known for his versatility, seamlessly switching between fantasy creatures and more subtle, realistic applications. His work on Darren Aronofsky’s “Black Swan” amplified the film’s psychological horror, while on Martin Scorsese’s “The Irishman,” he enhanced the film’s digital de-aging of Robert De Niro and Al Pacino with carefully crafted prosthetics.
Outside of film, Marino created the Weeknd’s plastic-surgery-gone-wrong look for the singer’s “Save Your Tears” video. “It’s all problems to solve,” Marino says. “There is no playbook.”
Diving into “A Different Man,” Marino used photographs and 3D scans of Pearson’s face, which has undergone some 40 surgeries over the years, as the basis for a multi-piece silicone prosthetic that would work with Stan’s features. “There was no way I could completely replicate Adam’s exact proportions,” he says. “I had to make some aesthetic choices.”
While the makeup work in “The Elephant Man” benefited from that film’s grainy black-and-white cinematography, the prosthetics in “A Different Man” had to withstand more unforgiving scrutiny. To put his Edward face to the test, Stan would walk from Marino’s makeup chair to the set through the streets of New York and crowds of strangers, giving him tremendous insight into how people treat those who look different.
“I went to my old coffee shop and the same barista who’d served me for years couldn’t identify me,” Stan recalls. “I got to really feel people’s reactions in real time. There were people who couldn’t even look at me, other people were staring and sometimes you’d get a bigger reaction, like, ‘Oh s—, it’s the Elephant Man!’ As Adam puts it, you feel like public property.”
Pearson, who shares his character’s sunny gregariousness, encouraged Stan to think about it like he does with his own experience as a movie star. “I was like, ‘You don’t know the level of invasion I get with people pointing, staring and taking photos, but you do understand a very similar thing from this angle, so lean into that heavily,’ ” he says. “ ‘And if it makes you uncomfortable, lean into it further.’ ”
While wearing the prosthetics, Stan could only see out of one eye and had limited hearing in one ear, challenges that helped further inform his performance as a man who has learned to shy away from potential threats and insults. “Edward is a character that has had to endure a lot of emotional abuse and probably some physical abuse, so he is probably always on his left foot a little bit in case something happens,” Stan says.
As Edward’s face changes following his radical treatment, Marino made additional prosthetics showing the transition, including an “extremely soft, mushy version” that, in a particularly Cronenbergian scene, Stan could pull off in chunks.

Colin Farrell as Oswald Cobblepot in “The Batman,” work for which Marino was Oscar-nominated. (Warner Bros. Pictures)
Marino’s talent for transforming stars is on full display in Farrell’s hulking, thuggish look as the Penguin in 2022’s “The Batman” and the new HBO spinoff series. “When Colin saw the sculpture I made, ideas started exploding,” Marino says. “Once we did a makeup test, it was magical — he knew how to speak, how to walk and he was already the guy.”
Marino, who is preparing to make his directorial debut based on a script he wrote set in the 1980s (“It’s deliberately not effects-heavy,” he hints), has lost none of his passion for the transformative power of latex and silicone since the days he was obsessively poring through issues of Cinefex magazine as a teenager. “If you think of Michelangelo showing beauty 500 years ago in painting and sculpture, I’m still showing that same beauty but in this new hyper-realistic way, in silicone,” says Marino, who named his makeup effects studio Prosthetic Renaissance. “It’s a very unique art. It’s like moving sculptures and paintings all at once.”
As for Pearson, if he were offered an experimental treatment to change his face, like in “A Different Man,” he says he wouldn’t take it. Despite the challenges it has brought him, Pearson believes his face has shaped the life he leads today.
“I joke with my friends that my disability does a lot of heavy lifting for my appalling personality,” he says with a laugh. “Everyone thinks it’s hard to go from non-disabled to disabled but I think the other way around would be even harder. The path we walk and the struggles we go through make us who we are and they’re inseparable from one another.”
17 notes
·
View notes
Text
Is it a pimple, insect bit, a random lump or fibroma…
A follow up Autobiography
Is this a fibroma I feel underneath my skin or is nothing there and I'm just being paranoid?: An NF Autobiography
#nf#nf1#nf2#neurofibromatosis#neurofibromatosis type 1#neurofibromatosis type 2#schwannomatosis#genetic disorders
29 notes
·
View notes
Text
Neurofibromatosis Type 2 Treatment Market Size in the 7MM was approximately USD 60 million in 2023, estimated DelveInsight
http://dlvr.it/TDh7wT
0 notes
Text
As with surgery, there are now many newer and emerging radiation technologies, tools, and techniques, including radiosurgery (also called stereotactic radiosurgery) and proton beam therapy.
According to each patient’s unique demands, the treatment strategy may combine surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. There are now better brain tumour diagnostic tools, surgical methods, and treatment choices because to developments in medical technology and research.
Types of Brain Tumor
1. Primary– Our brain is where primary brain tumours start. They can arise from your nerve cells, brain cells, meninges, the membranes that surround your brain, and glands like the pituitary and pineal. Primary tumours can be malignant or benign. Gliomas and meningiomas are the most prevalent kinds of brain tumours in adults.
2. Gliomas– Gliomas are tumors that develop from glial cells. These cells normally support the structure of your central nervous system, provide nutrition to your central nervous system, clean cellular waste, break down dead neurons
3. Meningioma– Meningioma is the most common primary brain tumor, accounting for more than 30% of all brain tumors. Meningiomas originate in the meninges, the outer three layers of tissue that cover and protect the brain just under the skull. Women are diagnosed with meningiomas more often than men
4. Neurofibroma– Neurofibromas are benign tumours that can develop on any part of the body’s nerves and are often painless. These fleshy, soft growths can occasionally form on the spinal cord, cranial nerves, or the brain. Neurofibromatosis type 1 (NF1) is a hereditary condition characterised by many neurofibromas as one of its symptoms.
5. Giant Cell Tumor– Named for their extremely large cells, giant cell tumors are rare bone tumors that usually affect the leg and arm bones. They may also be found in the skull. Most giant cell tumors are benign and occur in patients between 20 and 40 years of age.
6. Osteoma– Osteomas are benign bone tumours that typically appear on the base of the skull and the bones of the face. These slowly expanding tumours typically don’t manifest any symptoms. Large osteomas, however, may result in issues with breathing, vision, or hearing if they develop in specific regions of the brain.
Medications After Brain Tumor Surgery in India
There are several medicines that are helpful for reducing the symptoms of brain tumors. There are some of the medications are clinically tested and recommended by several physicians. They are:
Conclusion
Brain tumors are increasing on a large scale worldwide. Malignant tumors can be life-threatening. Whether benign or malignant, treatment depends on the specifics of the tumor. There are several treatment initiatives that are to be considered for a brain tumor patient. Treatment such as different medications, targeted surgery, chemotherapy, immunotherapy and others are really helpful in treating these patients.
1 note
·
View note
Text
Acoustic neuroma

Overview
Acoustic neuroma, also known as vestibular schwannoma, is a noncancerous tumor that develops on the main nerve that leads from the inner ear to the brain. This nerve is called the vestibulocochlear nerve, and it is responsible for transmitting sound and balance information from the inner ear to the brain. Acoustic neuromas are rare, and they typically grow slowly over a period of years. They are usually benign, meaning they do not spread to other parts of the body, but they can still cause problems if they grow large enough to press against nearby structures in the brain. Symptoms of acoustic neuroma can include hearing loss, tinnitus (ringing in the ears), dizziness or loss of balance, facial numbness or tingling, and headaches. The severity of symptoms can vary depending on the size and location of the tumor. Diagnosis of acoustic neuroma typically involves a combination of hearing tests, imaging studies such as magnetic resonance imaging (MRI), and a physical exam. Treatment options may include surgery to remove the tumor, radiation therapy, or observation with regular monitoring. While acoustic neuromas are not typically life-threatening, they can have a significant impact on a person's quality of life. Early diagnosis and treatment can help to minimize the risk of complications and improve outcomes.
Symptoms
Symptoms of acoustic neuroma can vary depending on the size and location of the tumor. Some common symptoms may include: - Hearing loss, usually affecting only one ear - Tinnitus (ringing, buzzing, or other noises in the ear) - Vertigo or dizziness, which may be mild or severe - Loss of balance or coordination - Headaches, which may be severe or persistent - Facial numbness or tingling, especially on one side of the face - Weakness or paralysis of the facial muscles, which can affect facial expression or make it difficult to close the eye or control drooling - Difficulty swallowing or speaking - Increased pressure within the skull, which can cause symptoms such as vomiting, confusion, or altered consciousness. It's important to note that not everyone with an acoustic neuroma will experience all of these symptoms, and some people may not have any symptoms at all. If you experience any of these symptoms, especially if they are persistent or severe, it's important to see a healthcare provider for evaluation and diagnosis.
When to see a doctor
If you experience any of the symptoms associated with an acoustic neuroma, it's important to see a doctor for evaluation and diagnosis. Some specific situations that may warrant a visit to the doctor include: - Unexplained hearing loss, especially if it affects only one ear - Persistent or worsening tinnitus (ringing, buzzing, or other noises in the ear) - Vertigo or dizziness that interferes with daily activities or is accompanied by other symptoms - Facial numbness or weakness, especially if it affects only one side of the face - Difficulty swallowing or speaking - Persistent headaches, especially if they are severe or accompanied by other symptoms. It's also a good idea to see a doctor if you have a family history of acoustic neuroma or if you have been diagnosed with a condition that increases your risk of developing this type of tumor, such as neurofibromatosis type 2. Early diagnosis and treatment can help to minimize the risk of complications and improve outcomes, so it's important to seek medical attention if you experience any of these symptoms.
Causes
The exact cause of acoustic neuroma is not known, but it is believed to develop when a type of cell called a Schwann cell begins to grow and divide abnormally on the vestibulocochlear nerve. The reason why this occurs is not fully understood, but some possible factors that may increase the risk of developing an acoustic neuroma include: - Neurofibromatosis type 2 (NF2): This is a rare genetic disorder that increases the risk of developing acoustic neuroma as well as other tumors. - Exposure to high levels of radiation: Exposure to ionizing radiation, such as that used in radiation therapy for other types of cancer, has been linked to an increased risk of developing acoustic neuroma. - Age: Acoustic neuromas are more common in people over the age of 60, although they can occur at any age. - Gender: Acoustic neuromas are slightly more common in women than in men. - Family history: While most cases of acoustic neuroma are not inherited, having a close relative with the condition may increase the risk of developing it. - Environmental factors: Some studies have suggested that exposure to certain chemicals or toxins may increase the risk of developing acoustic neuroma, but more research is needed to confirm this. It's important to note that many people with acoustic neuroma do not have any known risk factors, and the condition can occur in anyone. If you are concerned about your risk of developing acoustic neuroma, talk to your healthcare provider for more information.
Risk factors
There are several risk factors that may increase the likelihood of developing an acoustic neuroma. These include: - Neurofibromatosis type 2 (NF2): This rare genetic disorder increases the risk of developing acoustic neuroma as well as other types of tumors. - Age: Acoustic neuromas are more commonly diagnosed in people over the age of 60, although they can occur at any age. - Gender: Women are slightly more likely than men to develop an acoustic neuroma. - Family history: While most cases of acoustic neuroma are not inherited, having a close relative with the condition may increase the risk of developing it. - Exposure to high levels of radiation: Exposure to ionizing radiation, such as radiation therapy for other types of cancer, has been linked to an increased risk of developing acoustic neuroma. - Environmental factors: Some studies have suggested that exposure to certain chemicals or toxins may increase the risk of developing acoustic neuroma, but more research is needed to confirm this. It's important to note that many people with acoustic neuroma do not have any known risk factors, and the condition can occur in anyone. If you are concerned about your risk of developing acoustic neuroma, talk to your healthcare provider for more information.
Complications
Complications associated with acoustic neuroma can vary depending on the size and location of the tumor, as well as the specific nerves or structures it affects. Some potential complications of acoustic neuroma may include: - Hearing loss: Acoustic neuroma can cause hearing loss, which may be permanent or temporary depending on the extent of the damage. - Balance problems: Acoustic neuroma can affect the vestibular nerve, which plays a key role in maintaining balance, leading to problems with balance and coordination. - Facial weakness or paralysis: If the facial nerve is affected by the tumor, it can lead to weakness or paralysis of the facial muscles on one side of the face. - Difficulty swallowing or speaking: If the tumor grows to a large size or presses on certain nerves, it can cause difficulty swallowing or speaking. - Increased pressure within the skull: Large acoustic neuromas can cause increased pressure within the skull, which can lead to headaches, vomiting, confusion, and other symptoms. - Surgery complications: Surgery to remove an acoustic neuroma carries some risks, such as infection, bleeding, and damage to surrounding nerves or structures. It's important to note that not everyone with an acoustic neuroma will experience complications, and some people may have very mild symptoms that do not require treatment. However, it's important to seek medical attention if you experience any symptoms associated with acoustic neuroma, as early diagnosis and treatment can help to minimize the risk of complications and improve outcomes. Read the full article
#Acousticneuroma#activities#balanceproblems#benigntumor#care#Causes#diagnosis#eartumor#full#health#hearing#hearingloss#men#risk#skullbasesurgery#style#symptoms#tinnitus#Treatment#vestibularschwannoma#women
0 notes
Text
NF AWARENESS DAY
Today Neurofibromatosis (NF) Awareness Day.
NF is a group of complex genetic conditions that cause tumours to form on the nerves throughout the body.
NF includes Neurofibromatosis type 1 (NF1), Neurofibromatosis Type 2 and Schwannomatosis.

#neurofibromatosis awareness#nf1#neurofibromatosis type 1#neurofibromatosis type 2#neurofibromatosis#schwannomatosis#awareness#nf awareness
4 notes
·
View notes
Text
OK, so eye doctor. I have temporary prism glasses I'm to try out for the next two months. If I need to change the prism, they will do it at that appointment. Once we figure out the best prism, they'll also check my glasses to make sure my prescription is up to date since glasses can be expensive even BEFORE they add the prism. Was not expecting this, but a bonus, the prism glasses really reduced the amount of GET tinnitus I hear. My head was pretty quiet. Yeah, it Was still there, but quieter. I have the beginnings of two teeny tiny cateracts, but the optical nerve is very healthy. My eyes are all dialated. Hubby and I were there for 3 hours! And did a bunch of testing, They measured my periferary vision and took pictures of my eyeball! We had to wake up at 6 am to get there! Yearly detailed visits to keep an eye on optic health, back in 2 months to check the prism. The temporary is like a phone screen protector, so if it bothers me, I can peel it off and try a new one next time so we can figure out what works best for me. They had a bunch they tried out on me, we picked out what was the best at the time, now to see how it works in the real world. But first a nap. And maybe when I wake up, my eyes won't be too dialated to use the computer or go outside.
2 notes
·
View notes
Photo

NF-2 is not even neurofibromatosis! The name is a misnomer. The peripheral nerve sheath tumors these pts develop are not neurofibromas, they are actually schwannomas. But we still call this NF-2. It’s a different gene. NF2 gene is called “Merlin.” Loss of function mutation of Merlin—>upregulated Ras/MAPK and PI3K/Akt/mTOR pathways—>tissue proliferation. NF2 doesn’t have café-au-lait spots. The schwannomas can occur on vestibular nerves—>hearing loss; tumors can develop in the meninges/ependymal cells/astrocytes. They already have 1 hit (the gene is mutated); a 2nd hit—>tumor formation.
1 note
·
View note
Text
Sooo I possibly get my results for my ultrasound tomorrow... That means that I find out if the new lump that has grown is either a thyroid problem or another neurofibroma or a cancer. Like, I know that if it was BAD bad, then I would probably be contacted much faster but...If it's a rare cancer (which the cancers associated with NF normally are) then it would take many groups of people to find some kind of diagnosis. And many people mean A LOT OF TIME. If it is cancer, then I know it will probably be MPNST or some kind of soft tissue cancer, but still...those cancers are horrible, and from what I've seen, the chemo is worse. In a way, though...If it IS cancer, then at least I would have an answer. I would have an answer and I could get it cured. Idk. Being sixteen (in six days!!) means that you're incredibly insecure as fuck. Having a plexiforma on your neck/face is also bad. And possibly having cancer??? AHAHAH That mixed in with GAD, insomnia, some sort of depression/dissociation disorder, and being a queer trans person? Even better! the world fuckin hates me sometimes.
#neurofibromatosis#neurofibromatosis type one#neurofibromatosis type 2#MPNST#cancer#illness#chronically ill#queer#transgender#FTM#femaletomale#femaletosickmale
2 notes
·
View notes
Text
Introducing the NFCord!!
Happy NF awareness month everyone!! I’ve decided to celebrate by creating a server for people with NF, be it NF1 or NF2!! This is a server to meet, connect with, and get to know others with NF, since we seem to be so few and far between and it can be rough feeling alone and like you don’t have a community.
Join here!!
Please note that this server is ONLY for people with NF!! Make sure to read the rules and post an intro!! Also, feel free to (please) spread this, even if you don’t have NF!!
24 notes
·
View notes
Text
⚠️MUTUAL AID REQUEST⚠️
Hi friends, this is an update to my last mutual aid request for my friend Hyde. You can read it in full detail here, but to summarize: Hyde is severely disabled and chronically ill with Neurofibromatosis type-1 and severe scoliosis, requiring 1-2 surgeries or other treatments every year to keep him stable, and he is in need of money for medical equipment and to receive care outside of the country.
Since the last update, Hyde’s health has significantly worsened, to which he is now considered an incomplete paraplegic and has surgery to fuse his entire spine in the coming days. He has also experienced several falls, and is developing fullbody numbness from the torso down and bladder issues.
Because of the fact that his mother is also disabled and they don’t have a car, Hyde needs help in order to cover the cost of transportation for future treatments. He also needs money to help cover new medical equipment that he will need due to his current health condition, including ramps, bracing equipment, and arm crutches.
It would mean a lot to the both of us if you could donate, or at least share. $10USD is equivalent to $16NZD, so even a small amount can go a long way.
You can donate to him through these links:
Kofi @ Vampire
Give a Little @ Hydeyfund
Goal 1: $9,000 (Basic wheelchair)
Goal 2: $18,000 (Power assist and modifications)
Goal 3: $24,000+ (Motorized and all terrain wheels)
Currently: 13% of $18,000 goal
62 notes
·
View notes
Text
I haven't been able to sleep past few nights. Too much emotion. There's currently too much uncertainty of what's going to happen with my current life due to my medical condition. Kubler Ross talked about the stages of grieving but I feel they can be applied to different time in our lives. At the moment I haven't gone through any of them. I do have moments of sadness that can last hours, moments when I just cry and at times which I wasn't here to have to go through this. Life has thrown at me many obstacles as a child, diagnosed with (Neurofibromatosis type 1) NF at the age of 6 months and having to go to specialist, doctors, hospitals, being a genui pig etc. Currently 36 and will be 37 next month. It's been a long a hard battle and I am tired. On June 6th I had bladder surgery to remove tumors from my bladder wall (Malignant Neoplasm of the bladder wall) unfortunately my surgery failed. Last night I found out this doctor has a pending law suit for malpractice. I am currently on a waiting list to be seen by a new specialist; a urologist that specializes in cancer patients in regards the the bladder as well as prostate, etc. I am hoping to be seen in 2 weeks or less given my current diagnosis. What's been going on in my mind is why have I had to go through so much since I was a baby. Where or what did I do wrong? I'm not a perfect person, I will admit I have my flaws and make mistakes daily and perhaps have even hurt people. It's never been with malicious intent or any type of agenda. I am upset at the universe and basically the spontaneous mutation that occurred as I was still in my mother's womb. I still haven't told my mom or sister. Given that my sister is an emergency ER trauma Nurse Practitioner (NP) pretty much a doctor for those that may be unfamiliar with that term. My emotions lately have been of uncertainty, should I try chemotherapy, immunotherapy, is it even worth going through. Part of me does want to move on and live a comfortable life and ultimately overcome this. The other side of me doesn't want to try chemo or other treatment options and just succumb. I feel that I am simply just one of those lucky people that become cursed . To me it's the only logical way I can explain this to others and what I believe. This new urologist Dr Bruce specializes in robotics and cancer at Loma Linda University Hospital one of the best here in California.
Having NF and Bladder cancer is pretty much the worst scenario. I am not sure how well I will take the treatments that are required, if it will spread or it turns out to be all well in the end. What ever time I have left on this earth 🌎 I want to be able to be a good person to my friends, love ones and people in general. I hope they have good memories of me. In the meantime I'm hoping to get back into my photography and art in general. #cancer #malignantneoplasmofthebladder #chronicillness #neurofibromatosis

8 notes
·
View notes
Note
Someday, your body will fail you in a way you might not expect ... // This. My body "failed me" 10 yrs when I was diagnosed w/ a disease called Neurofibromatosis Type 2. It causes me to grow benign tumors mostly around my brain, down my spine, but they can grow on other nerves, too. I've had a whirlwind of emotions since & the last thing a person should project onto me is I'm infertile because I'm now "too old" to have a child. What a horrible thing to say to a woman who wants to carry a baby.
I hesitate to even say "failed" about someone's body. Our bodies do a lot of things, but if you're still alive, it's not really "failing" you. It's just doing something else that might not always be so great...I don't know...I've been in a lot of medical facilities lately, when they'll let me in with my sister for her cancer treatments, and it's shocking the number of young women I've seen going to get chemotherapy. Some young men, too.
We're all here. We're all alive. We're all experiencing this moment together. We should just appreciate each other and our time on this Earth, and that we're all sharing this moment at the same exact time.
It's a beautiful thing, and we shouldn't just discard one another so easily. I wish you peace, happiness, and the best things.

10 notes
·
View notes
Note
Can I ask why you’re having brain surgery? I’m new to your blog and I’m interested!! I love your blog btw and ur gorgeous!! 💕 good luck :)
Hi! I have a pretty rareish genetic disorder called neurofibromatosis type 2, that causes tumors to grow on my nerves. I’ve had 11 surgeries now over the last few years, and most of them have been on my head/brain. I’m having a brain tumor removed tomorrow (My 3rd tumor surgery) and having an auditory brain stem implant put in. So if this works, I’ll have sort of robotic ear, which sounds nifty.
23 notes
·
View notes