#liver transplant survival rate
Explore tagged Tumblr posts
Text
In the world of medical innovation, Dr. Vivek Vij is a famous surgeon.
Renowned for elevating liver transplant survival rate, Dr. Vivek Vij is a famous surgeon at the forefront of medical innovation. With expertise that spans decades, he has transformed the landscape of liver transplant surgery in India. Dr. Vij's commitment to affordable healthcare ensures that liver transplant surgery costs in India remain accessible, providing hope to countless patients in need. Trust in his expertise for life-changing liver transplants.
0 notes
Text

Amanita phalloides, the deadliest mushroom of the world
Commonly known as "death cap" internationally, this mushroom of European origin occurs now in all countries with temperate climate zones worldwide. It is particularly abundant in northern, central and eastern Europe, including Germany, where it forms an ectomycorrhiza symbiosis with broad leaf tree species.
Its similarity to edible mushroom species such as the straw mushroom and the white Caesar make it particularly dangerous. It may also be confused with the cultivated mushroom and the field or meadow mushroom, although clear distinguishing features exist.
Its deadly poison are heat-stable polycyclic oligopeptides of the amatoxin group with a lethal dose of about 0.1 mg per kg of body weight. This is equivalent to 20 to 40 grams of mushroom for an adult and 1 to 2 grams for children. The poison survives cooking, freezing and drying.
Amatoxins are highly efficient inhibitors of the RNA polymerase and disrupt gene expression in human cells. This causes nausea, vomiting and severe diarrhea about 8 to 12 hours after ingestion. At this time, the toxin has already distributed throughout the whole body and enriched in the liver, so any attempt to bind the toxin in the digestive tract is inefficient. The disruption of gene expression in the liver causes the liver cells to die and the liver to dissolve. Blood coagulation is severely disturbed, leading to severe interior bleeding. Hepathic encephalopathy leading to coma is the final cause of death and occurs six to ten days after ingestion.
Early stages or a mild poisoning is treated with Silymarin, an extract from the milk thistle, which inhibits the uptake of amatoxins into the liver cells. The ultimate cure for severe cases of amatoxin poisoning is a liver transplant. Due to these therapies, the death rate of cases of Amanita poisoning has been reduced from almost 100 % to 10 to 15 %. Early diagnosis and quick action are the prerequisites for a poisitive outcome.
Mushroom hunters in Europe usually know to distinguish the death cap from edible fungi, so cases among Europeans are rare. Immigrants, however, have more frequently suffered from Amanita poisonings. Many of the victims of the last decade came from Syria, where the death cap is unknown in many regions. In the USA, immigrants from south east Asia are frequent victims of Amanita poisoning. In Australia, signs warn mushroom hunters to abstain from their leisure activity in areas where Amanita phalloides has been introduced.
55 notes
·
View notes
Text

The death cap mushroom (Amanita phalloides) is one of the most toxic and deadly mushrooms in the world. It’s responsible for the majority of fatal mushroom poisonings, as it contains potent toxins called amatoxins that are highly resistant to heat and enzymes, meaning they remain toxic even after cooking.
Characteristics of the Death Cap
Appearance:
Cap: It has a pale green to olive-brown, smooth cap that can be mistaken for other edible mushrooms. The cap is usually 5–15 cm in diameter, with a somewhat sticky surface when wet.
Gills: The gills beneath the cap are white and free (not attached to the stalk).
Stalk: The stalk is white or pale, with a swollen base that may have a cup-like structure (volva).
Spore Print: The spore print of the death cap is white.
Habitat:
It is most commonly found in temperate regions, particularly in Europe and North America, often growing in association with hardwood trees like oak, chestnut, and pine.
It thrives in moist environments, typically appearing in late summer or fall.
Toxicity and Symptoms of Poisoning
Death cap mushrooms contain several toxic compounds, with amatoxins being the most lethal. These toxins inhibit RNA polymerase II, a critical enzyme in protein synthesis, leading to cell death—especially in the liver and kidneys.
Poisoning Stages:
Latency Period (6-12 hours): After ingestion, there is a deceptive phase with no symptoms, which can lull people into a false sense of security.
Gastrointestinal Phase (12-24 hours): Violent abdominal pain, vomiting, and diarrhea occur, leading to dehydration and electrolyte imbalance.
Apparent Recovery (1-2 days): Symptoms seem to improve, but this is an illusion. Meanwhile, liver and kidney damage is worsening internally.
Liver/Kidney Failure (3-5 days): If untreated, the liver and kidneys begin to fail, leading to coma and potentially death.
Treatment
Immediate medical attention is critical. Hospital treatment often involves:
Activated Charcoal: Administered to absorb any remaining toxins.
Intravenous fluids: To manage dehydration.
Liver Transplant: In severe cases, patients may require a liver transplant to survive.
Unfortunately, even with aggressive treatment, the death rate for death cap mushroom poisoning can range from 10–30%.
Edibility Confusion
One of the most dangerous aspects of the death cap is its resemblance to edible mushrooms. It can easily be confused with mushrooms like the paddy straw mushroom (Volvariella volvacea) and the caesar’s mushroom (Amanita caesarea), particularly in its early stages of growth.
Cultural Impact and History
Death caps have a long and infamous history:
In ancient Rome, they were believed to have been used in political assassinations, notably in the death of Emperor Claudius.
Poisonings continue to occur worldwide, often involving foragers who mistake the death cap for an edible mushroom, particularly in areas where foraging is common.
Conclusion
The death cap mushroom is a highly toxic species that requires caution and awareness. It highlights the importance of proper identification and knowledge for those who forage mushrooms.
Get yourself my art works to add to your collection of mushrooms:


#ainight#handmade#art#mushroomcore#artists on tumblr#mushroom art#artists of tumblr#mushrooms#stay vigilant#tumblr#artists of threadless#threadless#death cap#poisonous mushrooms#poison#dead#deadly#mushroom love#mushrooms that can kill you
9 notes
·
View notes
Text
It's very cute that Mr. Mega thinks his refusal to read our leaks means anything. We'll continue sharing them, and people will continue reading them. But here, for you, Mr. Curt Mega, we have provided the medical report from John's time in the hospital after the ten days of sleeplessness he spoke of. Thank us later!
Mount Sinai Hospital Treatment Report: Johnathan S. MacNamara
Date of Admission: September 9, 2012
Date of Discharge: November 17, 2012
The patient was admitted to the Emergency Room at 6:24 AM, 09/05/12 and evaluated to be in critical condition almost immediately. He exhibited signs of septic shock, including: lung failure, kidney failure, liver failure, a blood pressure of 68/43 mm Hg, and a heart rate of 134 BPM. In addition, he showed signs of infection stemming from an abdominal laceration approximately 30 inches in length and on average approximately 2 inches deep. The exhibited signs included: seizures, a consistent 105° F fever, swelling around the wound, pus in and around the wound, and human fecal matter smeared across the abdominal region. The lattermost sign was not so much a symptom as an obvious cause.
The patient's wounds were immediately cleaned with heavy disinfectants and a tracheostomy was preformed. He was attached to a mechanical ventilator and the blood-oxygen levels slowly stabilized. Patient was admitted to the ICU for further treatment at 7:36 PM, 09/05/12. Injuries upon admission were mapped as follows:
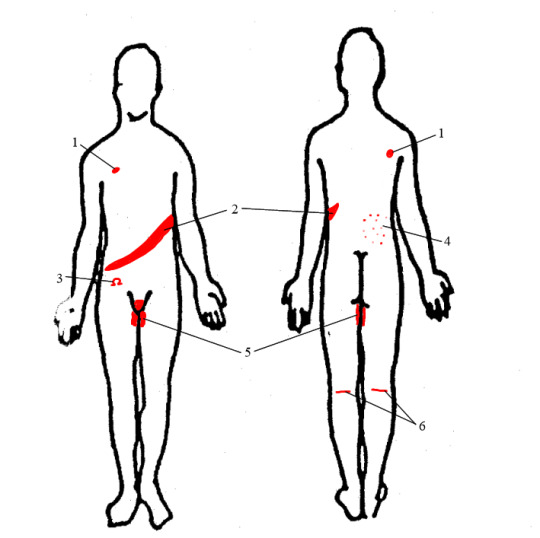
1. Bullet entry and exit through right deltoid. 2. Large laceration across midsection. Shows signs of heavy bacterial and viral infection. 3. Second-degree burn in the shape of greek letter omega. 4. Electric burns on lower right back. Presumably from high-voltage taser or cattle prod. 5. Intense electric burns in genital and inner-thigh areas. 6. Hamstrings lacerated. Presumably to constrict movement of legs.
Upon admission to the ICU, the patient was administered a standard dose of penicillin. There had been no signs of consciousness since arrival to the hospital, however the patient did appear to be in a survivable state. Within the unit, he was attached to a dialysis machine and given a steady IV of saline solution and another one that contained water-soluble vitamins and nutrients. Once the infection showed no further sign of spreading, the patient was given an emergency liver transplant. This occurred on 09/06/12.
The transplant succeeded, and the liver immediately began to filter blood and further cleared the infection. The decision was made to keep the patient on the dialysis machine until the infection and subsequent sepsis was cleared, and after a partial recovery from the first transplant occurred.
After 57 hours of total unconsciousness and unresponsiveness, the patient was declared to be in a coma caused by toxic-metabolic encephalopathy. He was assumed to wake up within the month.
The tracheostomy ventilator was removed on 09/23/12 and replaced with a laryngoscopic ventilator. This was changed once more on 10/03/12 when it was replaced with a mask ventilator.
The genital burns required a skin graft, but otherwise healed normally without infection or complications.
At 1:58 PM on 10/09/12, the patient began to react to outside stimuli. He moved when touched and made audible responses to pain. Over the next few days, he began to react to auditory and olfactory stimuli in addition to touch-based reactions increasing in consistency. By 10/12/12, the patient could follow simple commands and had managed to open his eyes a few times.
On 10/15/12 at approximately 12:30 AM, the patient awoke in a frenzied state. He attempted to rip out IVs and pulled off the ventilation mask and appeared to be unaware of where he was. It took excessive physical force, but he was eventually restrained and slowly calmed. He fell back asleep soon after, but showed greater signs of healing by that point. The next afternoon, he gave an official record of what happened to him, which provided a more accurate method of how to treat him. He consented to a kidney transplant and went into surgery on 10/18/12.
There were no complications during the surgery, and the donor was the wife of the patient, Rosalind M. Schaffer. She didn't suffer any complications from the donation either.
After the surgery, he was moved from the ICU and into the recovery wing with a private room.
The patient was dosed on standard pain medication over recovery, and showed no infectious flare-ups over recovery. He was monitored for lasting impacts of his wounds or disease, and had gained a noticeable tremor in both his hands. He underwent physical therapy while in the hospital's care, allowing him to regain full motion in his legs and to lessen his hand tremors.
The patient was discharged at 8:14 PM on 11/17/12 with a clean bill of health and prescribed a pain medication for as long as needed. It was also recommended that the patient stop smoking, as his lungs had previously failed once and it could be a major risk factor. The patient obviously did not follow the advice, as he was seen smoking a cigarette the second he left hospital grounds.
3 notes
·
View notes
Text
Jess Watches // Sun 12 May // Day 228 Synopses & Favourite Scenes & Poll
The Resident (with mum) 3x10 Whistleblower (mid season break)
On Devon's last day as an intern, he and Conrad are faced with a moral dilemma over a suicidal patient who is in need of a liver transplant. When Bell discovers that Cain is keeping braindead patients alive in order to boost his survival rates and add to Red Rock's profits, he decides to take matters into his own hands. Meanwhile, Adaku goes into early labor, causing a strain on her heart and Mina is left in doubt over how to best handle her care.
You just knew Conrad wasn't gonna make it to the end of his shift without being caught. Red Rock pounced. Hopefully Conrad's dad helps defeat them. How smug they were to demote Bell, but him being more focused on making sure Kit gets to keep her job. And I hope Adaku and baby are ok.
Star Trek: Prodigy 1x14 Crossroads
When the crew attempts to secure transport to the Federation, they unwittingly cross paths with the Vice Admiral who is hunting them.
I like that Starfleet aren't clean cut 'good guys'. They seem to be thriving on the power afforded to them by the Federation and the story is building effectively to show how dangerous that can be.
Amphibia 1x12 Civil Wart / Hop-Popular
Anne exposes Wartwood to a teen romance film, and the town is split on the movie's love triangle. / After losing his stand, Hop Pop decides to run for mayor of Wartwood.
Shipping wars are serious business in Wartwood. Sequel Plot Twist: the boys are in love too! I had a good giggle at the end with not-so-subtle references to fandom culture. / And being a theatre major, Hop Pop would be a marvellous mayor.
3 notes
·
View notes
Text
The targeting practices make this so much worse. I was diagnosed with liver disease a few years ago and eventually got on the transplant list, so during that I was googling a lot of medications and symptoms and survival rates. Apparently the algorithms associate liver with alcohol and I started getting alcohol ads constantly. What if I was an alcoholic? Who's blamed if someone goes back to an addiction because of those constant reminders?


114K notes
·
View notes
Text
Best Hospital for Liver Transplant in LB Nagar, Hyderabad
The Institute of Hepatology and Liver Transplantation at Kamineni Hospitals has been at the forefront in providing comprehensive, holistic healthcare to patients with advanced liver and pancreato-biliary disorders. We have been caring for patients with difficult and complex liver and pancreato-biliary disease, with a strong emphasis on prevention as much as treatment of such diseases.
A combination of internationally and locally trained doctors with extensive experience, a multidisciplinary team approach to patient care and state-of-the-art infrastructure, has enabled us to deliver excellent results that meet national benchmarks and achieve unparalleled patient satisfaction.
Our team includes Hepatologists, HPB surgeons, Transplant Anesthetists and Intensivists. The core team is supported by a host of allied specialities including interventional radiology, pathology, specialized nursing, physiotherapy, transplant coordinators and nutritionists. We have state-of-the-art infrastructure dedicated to liver transplantation including operation theatres, ICUs and wards.
We at Kamineni Hospitals are at the forefront of the management of such patients. Our trained medical and allied personnel strive towards the betterment of such patients using up-to-date treatment protocols and the latest advancements in the field of liver failure. We are equipped with a rapid response state-of-the-art dedicated Liver Intensive Care Unit with an International Ambulance Facility for transporting seriously ill patients for urgent liver transplants and other advanced liver disease treatment.
Kamineni Hospitals is one of the leading liver transplant facilities with state-of-the-art infrastructure and the best team of transplant surgeons, hepatologists, anaesthetists, and ICU staff, providing the most comprehensive and advanced liver care for adults and children of all ages. Currently, the success rate is over 95%, with a 10-year survival rate close to 80%, which is on par with major transplant centres worldwide. Our dedicated staff will provide the best possible experience to the patients from the moment they step into our premises all the way from OPD consultation, diagnosis, counselling, and treatment plan to post-treatment care, ensuring that you are given the utmost care at every stage.
#best hepatologist in hyderabad#best hematology hospital in hyderabad#liver transplant hospital in hyderabad#best hospital for liver transplant in hyderabad
0 notes
Text
Liver Cirrhosis Unveiled: A Complete Guide to Diagnosis and Treatment

Liver cirrhosis is a condition that often goes unnoticed until it starts affecting your daily life. It's a slow and progressive disease where healthy liver tissue is replaced with scar tissue, preventing the liver from working properly. This guide will walk you through what liver cirrhosis is, its symptoms, causes, how it’s diagnosed, and available treatments—so you can take the right steps for better liver health.
Whether you or a loved one are showing signs of liver trouble, understanding cirrhosis is the first step toward managing it better.
What Is Liver Cirrhosis?
Your liver is one of the most important organs in your body. It helps in digesting food, filtering toxins, storing energy, and supporting your immune system. But when the liver is damaged repeatedly—due to conditions like hepatitis, alcohol use, or fatty liver—the healthy cells are replaced by scar tissue.
This scarring, also called fibrosis, gradually spreads, affecting liver function. Once the liver becomes severely scarred, it leads to cirrhosis.
What Causes Liver Cirrhosis?
Several different conditions can lead to cirrhosis. Here are the most common causes:
Chronic Alcohol Use: Drinking heavily over time can damage the liver and cause cirrhosis.
Hepatitis B and C Infections: These viruses cause inflammation that leads to long-term liver damage.
Non-Alcoholic Fatty Liver Disease (NAFLD): Caused by obesity, diabetes, and poor diet, this is becoming a leading cause of liver cirrhosis worldwide.
Autoimmune Hepatitis: The body’s immune system mistakenly attacks liver cells.
Genetic Diseases: Conditions like hemochromatosis (iron buildup) or Wilson’s disease (copper buildup) can harm the liver over time.
Bile Duct Diseases: Blockages or inflammation in the bile ducts (such as primary biliary cholangitis) can also lead to cirrhosis.
Common Symptoms of Cirrhosis
Cirrhosis often develops slowly and may not show symptoms at first. As the disease progresses, you may notice:
Fatigue and weakness
Yellowing of the skin and eyes (jaundice)
Swelling in the legs, ankles, or belly (edema and ascites)
Loss of appetite or weight loss
Nausea or vomiting
Easy bruising or bleeding
Confusion or memory problems (hepatic encephalopathy)
Itchy skin
Spider-like blood vessels on the skin
If you're experiencing any of these symptoms, especially with a history of liver issues, it’s important to consult a specialist.
Diagnosis: How Is Cirrhosis Detected?
Cirrhosis can often be diagnosed with a mix of physical exams, medical history, blood tests, and imaging. Here’s what doctors might use:
Blood Tests: These check liver enzymes, clotting factors, and signs of liver function or damage.
Ultrasound or CT Scans: These images help doctors see liver size, shape, and scarring.
Fibroscan: A special scan that measures liver stiffness, often used to assess the level of scarring.
Liver Biopsy: A small tissue sample taken to confirm diagnosis and stage the disease.
Early diagnosis can significantly improve treatment outcomes. The earlier you find the problem, the easier it is to manage.
Treatment Options: Managing Cirrhosis
While scar tissue in the liver cannot be completely reversed, treatment focuses on stopping further damage, managing symptoms, and treating the underlying cause.
1. Lifestyle Changes
Stop Drinking Alcohol: Even small amounts can worsen cirrhosis.
Healthy Diet: Low-sodium, liver-friendly diets help reduce swelling and prevent complications.
Exercise Regularly: Helps manage weight and reduce fatty liver.
2. Medications
Doctors may prescribe medicines to treat hepatitis, reduce liver inflammation, or manage complications like fluid buildup and confusion.
3. Monitoring and Screening
Regular checkups, liver function tests, and screenings for liver cancer are critical.
Early detection of liver-related cancers or bleeding risks helps improve survival rates.
4. Advanced Treatments
Liver Transplant: In advanced cirrhosis, a liver transplant may be the only long-term solution. Not everyone qualifies, but it offers new hope for those with life-threatening liver failure.
Complications You Should Know
Cirrhosis can lead to serious health problems if not managed properly:
Portal Hypertension: Increased pressure in liver veins can lead to bleeding or varices.
Ascites: Fluid accumulation in the abdomen.
Hepatic Encephalopathy: Confusion and forgetfulness due to toxin buildup.
Infections: Increased risk due to a weakened immune system.
Liver Cancer: People with cirrhosis are at a higher risk of liver cancer.
Living with Cirrhosis: Tips for a Healthier Life
Here are a few practical things you can do every day:
Follow your doctor’s advice closely.
Take medications exactly as prescribed.
Avoid pain relievers like ibuprofen unless approved.
Eat fresh, liver-friendly foods like fruits, vegetables, and whole grains.
Avoid raw seafood, which can contain harmful bacteria.
Get vaccinated against hepatitis A and B.
When to See a Specialist
If you have ongoing fatigue, swelling, yellowing of the skin, or persistent stomach issues, don’t ignore it. Liver disease often progresses silently. For expert advice and care, many people trust the top 10 gastroenterologist in Surat who specialize in diagnosing and treating liver and digestive conditions.
Conclusion
Cirrhosis is a serious yet manageable condition. With early diagnosis, the right lifestyle choices, and medical care, you can live a fulfilling life while protecting your liver. Remember, your liver does a lot for your body—treating it kindly is one of the best investments you can make in your long-term health.
If you or someone you love is at risk, don’t wait. Reach out to a trusted gastroenterologist in Surat and take the first step toward better liver health today.
#gut health#health#digestion#digestivehealth#stomach problems#gastrologist#digestive health#healthylifestyle#digestive problems#stomach health#liver health#liver cirrhosis#liver tips#liver care
0 notes
Text
Liver Transplant for Children: Special Considerations and Outcomes
When it comes to treating severe liver conditions in children, a pediatric liver transplant can be a life-saving option. While the procedure shares many similarities with adult transplants, it also involves unique challenges and considerations. If you’re seeking a trusted pediatric liver transplant doctor in Ahmedabad, understanding the process, care standards, and outcomes can help you make informed decisions for your child.
What Is a Pediatric Liver Transplant?
A pediatric liver transplant is a surgical procedure in which a diseased or failing liver in a child is replaced with a healthy liver from a donor. The donor may be a deceased individual or a living person (often a parent or close relative) willing to donate a part of their liver.
This procedure is often recommended for children suffering from:
Biliary atresia
Acute liver failure
Metabolic liver diseases
Autoimmune hepatitis
Genetic liver disorders
Special Considerations in Pediatric Liver Transplants
Children are not just “small adults” — their anatomy, immune system, and response to surgery differ significantly. Hence, pediatric liver transplants require:
Specialized Expertise: A skilled pediatric liver transplant doctor in Ahmedabad understands the complexities of pediatric cases, from matching donor organs to managing immunosuppressive therapy post-transplant.
Age-Appropriate Care: From infants to adolescents, each age group needs a tailored medical approach, including anesthesia, medication dosing, and psychological support.
Long-Term Monitoring: Children require lifelong follow-up to monitor organ function, manage potential complications, and ensure proper growth and development.
Multidisciplinary Support: Successful outcomes often involve a team of specialists including hepatologists, pediatric surgeons, nutritionists, and psychologists.
Outcomes and Success Rates
Thanks to advancements in surgical techniques and post-operative care, pediatric liver transplant success rates have significantly improved. Most children go on to lead healthy, active lives with minimal restrictions. Early diagnosis, timely surgery, and expert follow-up care contribute to long-term survival and quality of life.
Why Choose Dr. Divakar Jain?
If you are searching for an experienced and compassionate pediatric liver transplant doctor in Ahmedabad, Dr. Divakar Jain stands out as a trusted name. With years of experience in treating complex liver conditions in both children and adults, Dr. Jain combines clinical excellence with a patient-first approach.
At drdivakarjain.com, families can access comprehensive information, expert consultation, and state-of-the-art treatment options for liver transplants in Ahmedabad.
Final Thoughts
A pediatric liver transplant is a complex journey, but with the right medical team, the outcome can be incredibly positive. Always consult with a specialized pediatric liver transplant doctor in Ahmedabad to evaluate the best options for your child’s condition. Early intervention and expert care can make all the difference.
0 notes
Text
Best Liver Transplant Surgeon in delhi NCR - Dr. Giriraj Singh Bora
Best Liver Transplant Surgeon in Delhi NCR | Dr. Giriraj Singh Bora
🩺 Best Liver Transplant Surgeon in Delhi NCR – Meet the Expert Saving Lives
Looking for the best liver transplant surgeon in Delhi NCR? Learn about Dr. Giriraj Singh Bora, his experience, success rates, and why patients trust him for advanced liver transplants.
🏥 Why Choosing the Right Liver Transplant Surgeon Is Crucial
A liver transplant is a life-saving procedure, and selecting the right surgeon plays a major role in its success. In the Delhi NCR region, patients seek not just experience, but compassion, precision, and a strong post-operative care system. That’s why many choose Dr. Giriraj Singh Bora, recognized as one of the best liver transplant surgeons in Delhi NCR.
👨⚕️ Dr. Giriraj Singh Bora – Leading Liver Transplant Surgeon in Delhi NCR
With over [X] years of experience in hepatobiliary surgery and more than [Y] successful liver transplants, Dr. Giriraj Singh Bora stands out in the field. His commitment to patient care, use of advanced techniques, and leadership in liver transplant teams across top hospitals in Delhi NCR make him a trusted choice.
Credentials:
MBBS, MS, MCh (Hepatobiliary Surgery)
Fellowship in Liver Transplantation (From [Institute/Hospital])
Member of [Liver Transplant Society, Indian Medical Council, etc.]
✅ Why Patients Choose Dr. Giriraj Singh Bora for Liver Transplants
Here’s what sets Dr. Giriraj Singh Bora apart from other liver transplant surgeons in Delhi NCR:
🔬 Advanced Technology: 3D laparoscopic and robotic-assisted transplants
🧠 Multidisciplinary Team: Collaboration with anesthetists, hepatologists & ICU experts
💬 Clear Communication: Transparent consultation & expectations
💯 High Success Rate: Over [Z]% survival rate among patients
🕒 24/7 Post-Surgery Support
💡 When Should You Consult a Liver Transplant Surgeon?
If you or a loved one is facing any of the following, it’s time to consult the best:
End-stage liver disease
Chronic liver failure due to hepatitis B or C
Cirrhosis caused by alcohol, fatty liver disease
Liver cancer in its early stages
📍 Liver Transplant in Delhi NCR – What to Expect
At our Liver Transplant Institute in Delhi NCR:
Pre-Transplant Assessment: Full body and liver evaluation
Donor Compatibility Testing: Living or deceased donor
Surgical Procedure: Performed at a state-of-the-art hospital
Post-Op Care: 24/7 monitoring and follow-up for 12 months
“Thanks to Dr. Giriraj Singh Bora, my life turned around. His skill and compassion made all the difference.” — Rajesh P., Delhi NCR
📲 Book Your Consultation with the Best Liver Transplant Surgeon in Delhi NCR
If you're searching for the top liver transplant expert in Delhi NCR, Dr. Giriraj Singh Bora is here to help. With compassionate care, world-class facilities, and unmatched surgical precision, your journey to recovery starts here.
📅 Schedule an Appointment Today 📞 Call: +91 96431 41912 🌐 Visit: https://livertransplantinstitute.com
Blogger:- https://livertransplantinstitute.blogspot.com/2025/05/best-liver-transplant-surgeon-in-delhi.html
1 note
·
View note
Text
Best Liver Transplant Surgeons in Coimbatore

When it comes to liver transplant surgeons in Coimbatore, Dr. Anand Vijai stands out as a pioneering expert in hepatobiliary and liver transplantation procedures. With years of specialized experience, cutting-edge surgical techniques, and a patient-first approach, he has transformed the lives of countless individuals suffering from end-stage liver disease, liver cirrhosis, and liver cancer. Dr. Anand Vijai is renowned for his expertise in minimally invasive liver transplants, robotic-assisted surgery, and laparoscopic procedures, ensuring faster recovery and reduced complications. If you or a loved one requires a liver transplant, Dr. Anand Vijai provides world-class care, high success rates, and long-term patient support.
Why Choose Dr. Anand Vijai as Your Liver Transplant Surgeon in Coimbatore ?
Extensive Experience in Liver Transplantation — Dr. Anand Vijai is a highly qualified and internationally trained liver transplant surgeon, specializing in complex hepatobiliary procedures. His in-depth knowledge and hands-on experience in liver transplant surgery have contributed to his reputation as a leading transplant expert surgeon in Tamil Nadu.
High Success Rates and Patient-Centric Care — Personalized treatment plans tailored to each patient’s condition , Minimally invasive techniques for faster recovery and reduced post-operative pain , Comprehensive pre- and post-transplant care to ensure long-term success.
Advanced Surgical Techniques — Dr. Anand Vijai is at the forefront of liver transplant innovation, offering Laparoscopic liver transplant surgery for minimal scarring and quicker recovery,Robotic-assisted liver transplantation, enhancing precision and reducing surgical risks,3D imaging and navigation technology for enhanced accuracy during surgery.
Dedicated Multidisciplinary Team — Dr. Anand Vijai works with a highly experienced team, including hepatologists, transplant specialists, anesthetists, and critical care experts, ensuring a smooth and successful liver transplant journey for patients.

Types of Liver Transplants
Dr. Anand Vijai specializes in various liver transplant procedures, catering to different patient needs:
Living Donor Liver Transplant (LDLT): A healthy donor donates a portion of their liver to the recipient.
Deceased Donor Liver Transplant (DDLT):The liver is sourced from a brain-dead donor.
Split Liver Transplant: A single liver is divided and transplanted into two different patients.
ABO-Incompatible Liver Transplant: Transplants performed even with blood group mismatches.
Pre-Operative Evaluation and Preparation
Comprehensive liver function tests and imaging.
Donor-recipient compatibility assessment.
Nutritional and lifestyle guidance for optimal transplant outcomes.
Post-Operative Care & Long-Term Management
Regular monitoring and immunosuppressive therapy to prevent organ rejection.
Customized rehabilitation programs for faster recovery.
Lifelong follow-up care to ensure sustained health and transplant success.
Understanding Liver Diseases & When to Consider a Transplant
Liver transplantation is often recommended for patients suffering from severe liver diseases, including:
Cirrhosis-(caused by alcohol, hepatitis B/C, fatty liver disease, or autoimmune disorders).
Liver cancer (Hepatocellular carcinoma — HCC)
Genetic liver disorders such as Wilson’s disease and Hemochromatosis.
Acute liver failure due to toxins, infections, or drug-induced damage.
When is a liver transplant necessary ?
When conventional treatments fail to manage liver disease.
In cases of severe jaundice, ascites, or hepatic encephalopathy.
If liver function deteriorates to a point where survival is at risk without a transplant.
conclusion
Dr. Anand Vijai stands as one of the most trusted and accomplished liver transplant surgeons in Coimbatore, combining exceptional surgical expertise with compassionate, patient-centered care. With advanced training in liver transplantation and minimally invasive robotic liver surgery, he has transformed the lives of countless patients suffering from complex liver diseases. His commitment to clinical excellence, use of cutting-edge technology, and personalized treatment approach make him a leading choice for liver care in South India. For those seeking world-class liver transplant solutions with integrity and empathy, Dr. Anand Vijai is the name to trust. for more info follow the ref link :https://shorturl.at/QGmxi
0 notes
Text
Insurance Discrimination The number of people who need a liver transplant is currently far greater than the number of donor livers available. Unfortunately, this can lead to discrimination by insurance companies against alcoholics who they believe have caused their own ill health and are, therefore, less deserving of the liver than other individuals. However, medical principles should guide treatment procedures not prejudice. Alcoholics should have the same access to health care as anyone else. The discrimination against alcoholics occurs because insurance companies fail to recognize the disease nature of addiction. According to the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine, "Alcoholism is a primary, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations." This definition recognizes alcoholism as a disease, i.e., as an involuntary disability and accepts a genetic vulnerability in some people. Thus, to discriminate against alcoholics because of the belief that they have some sort of moral defect defies medically accepted evidence that suggests otherwise. Ignorance always seems to the largest driver of prejudice. Insurance companies also mistakenly believe that alcoholics will be less likely to benefit from a liver transplant than other patients. However, researchers have proved that discrimination against alcoholics in liver transplant programs is unjustified. They have found no major differences in survival or organ rejection rates between liver transplants of cirrhosis patients and those with other liver diseases. Thus, liver transplantation is just as justified for alcoholic cirrhosis as it is for other factors leading to liver damage. The denial of a liver transplant to an alcoholic represents an undesired shift from humanitarian ethics to utilitarian ethics. Humanitarian ethics state that the well being of the individual is central. Today, insurance companies are asking doctors and patients to accept a new utilitarian ethic where the well being of others prevails over the well being of the patient. The doctor judges the quality and the sense of whether a patient is a burden or useful to society, etc. In the past, medical ethics had been based on the notion that all men's lives had equal value. But now, utilitarianism maintains that this can no longer be maintained as available resources can't keep up with demand. Discrimination by insurance companies should never prevent Americans from receiving the benefits that they have paid for. Not only is it unfair to the alcoholic, but it holds broader implications that are disturbing. If society tolerates discrimination against alcoholics, then what's next? Once discrimination against alcoholics becomes common practice, acceptance for discrimination against the elderly, minorities or physically handicapped people could easily follow suit. In a profit-driven health care system, society simply cannot rely on the faith in the goodness of human nature or the ability of the American democratic system to protect the weak. Instead, society requires strong laws that prevent any form of discrimination in medical treatment. Bibliography Alcoholics Discriminated Against in Liver Transplant Programs." 03 Sept. 1999. Join Together. 09 Dec.2003. Alcoholism." Infoplease.com. 09 Dec. 2003. http://www.infoplease.com/ce6/sci/A0803142.html. Gunning, Karel F. "Why Not Euthanasia." Oregon Right to Life. 08 Dec. 2003. http://www.ortl.org/suicide/euthanasia_gunning.htm. Alcoholics Discriminated Against in Liver Transplant Programs." 03 Sept. 1999. Join Together. 09 Dec.2003. http://www.jointogether.org/sa/news/summaries/reader Alcoholism." Infoplease.com. 09 Dec. 2003. http://www.infoplease.com/ce6/sci/A0803142.html. Alcoholics Discriminated Against in Liver Transplant Programs." 03 Sept. 1999. Join Together. 09 Dec.2003. Gunning, Karel F. "Why Not Euthanasia." Oregon Right to Life. 08 Dec. 2003. http://www.ortl.org/suicide/euthanasia_gunning.htm. Read the full article
0 notes
Text
Liver Cancer Treatment in India: Advanced Medical Care & Treatment Options
Understanding Liver Cancer and Its Impact
Liver cancer is a life-threatening disease that affects thousands of people worldwide. It occurs when malignant cells develop in the liver, leading to serious health complications. India has emerged as a preferred destination for liver cancer treatment due to its advanced medical technology, experienced oncologists, and world-class healthcare infrastructure.
Why Choose Liver Cancer Treatment in India?
India has made significant strides in oncology and hepatology, making it one of the best places for liver cancer treatment in India. The country is home to highly qualified cancer specialists, cutting-edge surgical techniques, and comprehensive treatment plans. Many leading hospitals in India provide personalized cancer care, ensuring better survival rates and improved quality of life for patients.
Types of Liver Cancer Treated in India
Liver cancer is primarily categorized into two types:
Hepatocellular Carcinoma (HCC): The most common type, affecting the main liver cells (hepatocytes).
Cholangiocarcinoma (Bile Duct Cancer): Affects the bile ducts inside and outside the liver. Other types include fibrolamellar carcinoma and angiosarcoma, which are rarer but require specialized care.
Best Liver Cancer Treatment in India
Liver cancer treatment depends on the stage of the disease, patient health, and available treatment options. India offers a range of therapies, including:
1. Liver Surgery (Hepatectomy)
For patients with localized liver cancer, surgical resection or partial hepatectomy can remove the affected portion of the liver. India’s leading cancer hospitals use minimally invasive laparoscopic techniques, ensuring faster recovery.
2. Liver Transplantation
In advanced cases, a liver transplant may be necessary. India has some of the best transplant centers with high success rates, offering both cadaveric and living donor liver transplants.
3. Targeted Therapy
This innovative treatment uses drugs to target specific cancer cells without affecting healthy tissues. Medications like Sorafenib are widely used in liver cancer treatment in India.
4. Immunotherapy
Immunotherapy boosts the body's immune system to fight cancer. This approach is increasingly being used in India to treat advanced liver cancer cases.
5. Chemotherapy
Chemotherapy is often used when surgery is not an option. It can be administered orally or intravenously to slow cancer growth and alleviate symptoms.
6. Radiation Therapy
High-energy beams are used to destroy cancer cells, often recommended for patients who are not eligible for surgery. Advanced techniques like Stereotactic Body Radiation Therapy (SBRT) are available in India.
7. Radiofrequency Ablation (RFA) and Microwave Ablation (MWA)
Minimally invasive techniques like RFA and MWA use heat to destroy cancer cells, making them effective for patients with early-stage liver cancer.
Top Hospitals for Liver Cancer Treatment in India
India has numerous hospitals specializing in oncology and hepatology, equipped with modern technology and a multidisciplinary team of experts. Some of the leading hospitals include:
RPS Hospitals
AIIMS, New Delhi
Tata Memorial Hospital, Mumbai
Apollo Hospitals
Fortis Healthcare
Medanta - The Medicity
Factors to Consider When Choosing a Hospital for Liver Cancer Treatment in India
When selecting a hospital for liver cancer care, consider the following:
Expertise of oncologists and hepatologists
Availability of advanced treatment options
Accreditation and international standards
Success rates of surgeries and treatments
Post-treatment care and rehabilitation facilities
Lifestyle Changes to Support Liver Cancer Treatment
Apart from medical intervention, lifestyle changes play a crucial role in liver cancer management. Patients are advised to:
Follow a healthy diet rich in fruits, vegetables, and lean proteins.
Avoid alcohol and tobacco to prevent further liver damage.
Maintain a healthy weight and stay physically active.
Take prescribed medications and attend regular follow-up appointments.
Conclusion
India has established itself as a hub for liver cancer treatment, offering high-quality medical care at internationally accredited hospitals. With advanced therapies, experienced specialists, and holistic cancer care, patients can receive effective treatment tailored to their needs.

If you or a loved one is seeking liver cancer treatment in India, RPS Hospitals provides world-class oncology services with a patient-centric approach.
0 notes
Text
The Future of Healthcare in Maval: Pawana Hospital’s Vision for Innovation
Healthcare is rapidly evolving, with new technologies, treatments, and patient care models transforming the way hospitals operate. At Pawana Hospital, we are not just keeping up with these advancements—we are leading the way in bringing world-class healthcare to the Maval region.
With 27 years of excellence, we are committed to continuous innovation, ensuring that our patients receive the best possible care, right here in their hometown. But what does the future of healthcare in Maval look like? Let’s explore Pawana Hospital’s vision for innovation and how we plan to shape the next era of medical care.

1. Expanding Super-Specialty Care in Maval 🏥✨
As the largest healthcare provider in the region, Pawana Hospital is on a mission to expand and strengthen super-specialty services.
🔹 Cardiac Care Advancements – Expanding heart surgeries, electrophysiology, and heart failure management. 🔹 Oncology (Cancer Care) Services – Establishing comprehensive cancer diagnosis, treatment & chemotherapy. 🔹 Advanced Neurology & Neurosurgery – Introducing stroke rehabilitation & robotic-assisted neurosurgery. 🔹 Transplant Programs – Expanding into kidney, liver, and corneal transplants.
💡 The Impact: ✅ Maval residents will no longer need to travel to metros for specialized treatments. ✅ Access to world-class super-specialty care closer to home. ✅ Faster diagnosis and treatment, leading to better patient outcomes.
2. Integrating AI & Digital Healthcare Solutions 🤖💻
Artificial Intelligence (AI) and digital healthcare are redefining patient care, making diagnosis and treatment more efficient, accurate, and personalized.
🛑 Upcoming Digital Innovations at Pawana Hospital: ✅ AI-Based Radiology & Imaging – Faster, more accurate MRI, CT scan & X-ray analysis. ✅ Telemedicine & Online Consultations – Enabling patients to consult specialists remotely. ✅ Electronic Medical Records (EMR) – Streamlining patient data for faster & safer treatment decisions. ✅ AI-Driven Predictive Healthcare – Identifying early warning signs for conditions like heart disease and diabetes.
💡 The Impact: ✅ Quicker and more precise diagnosis, reducing treatment delays. ✅ Easier access to specialist doctors, even for those in remote areas. ✅ Less paperwork, more efficiency, and seamless patient experience.
3. Strengthening Emergency & Trauma Care 🚑🔬
Pawana Hospital is committed to enhancing emergency response with:
🛑 Next-Generation Trauma & Critical Care: ✅ AI-Assisted Emergency Triage – Faster identification of critical cases. ✅ Advanced Life-Saving Equipment – High-tech ventilators, ECMO (extracorporeal membrane oxygenation) for severe heart and lung failure. ✅ Rapid Stroke & Heart Attack Response Units – Reducing critical response time with on-the-go care. ✅ Enhanced NICU & Neonatal Transport Services – Providing life-saving care for premature and critical newborns.
💡 The Impact: ✅ Golden hour treatment for accident & stroke patients, improving survival rates. ✅ Advanced neonatal emergency care, ensuring better newborn survival. ✅ Quicker, more effective emergency treatments, saving more lives.
4. Robotics & Minimally Invasive Surgery 🤖🔪
The future of surgery lies in precision, minimal invasion, and faster recovery. Pawana Hospital is gearing up to bring:
🛑 Revolutionary Surgical Innovations: ✅ Robotic-Assisted Surgeries – More precision, minimal scars, faster recovery. ✅ Laparoscopic & Endoscopic Surgeries – Painless & quicker operations. ✅ 3D Printing for Customized Implants – Better fit, better function for orthopedic & reconstructive surgeries.
💡 The Impact: ✅ Shorter hospital stays, reduced pain, and quicker recovery. ✅ Better outcomes for complex surgeries (spine, orthopedic, cancer). ✅ More accurate and personalized treatment plans.
5. Holistic & Preventive Healthcare Approach 🏃♂️🌱
Prevention is better than cure, and Pawana Hospital is investing in community-driven healthcare:
🛑 Upcoming Preventive & Holistic Health Programs: ✅ Chronic Disease Management Clinics – Focus on diabetes, hypertension & heart health. ✅ Regular Free Health Camps – Early screening for cancer, kidney, and eye diseases. ✅ Nutrition & Lifestyle Clinics – Educating Maval residents on diet, fitness & mental wellness. ✅ Corporate Wellness Programs – Partnering with businesses to ensure employee well-being.
💡 The Impact: ✅ Early detection & prevention of major diseases, reducing long-term health risks. ✅ Better health awareness & education, leading to healthier communities. ✅ Empowering individuals with knowledge about self-care & disease prevention.
6. Sustainable & Eco-Friendly Healthcare 🌱🏥
Healthcare should not just heal people—it should protect the planet too. Pawana Hospital is committed to:
🛑 Green & Sustainable Hospital Practices: ✅ Solar-Powered Energy Solutions – Reducing the hospital’s carbon footprint. ✅ Zero Waste Medical Recycling – Safe disposal & recycling of medical waste. ✅ Rainwater Harvesting & Water Recycling – Sustainable water usage for hospital operations. ✅ Paperless Hospital System – Digital documentation to minimize paper waste.
💡 The Impact: ✅ A healthier environment for patients & staff. ✅ Lower operational costs, making healthcare more affordable. ✅ Contribution to Maval’s ecological well-being.
Conclusion: A Healthier Future for Maval Starts Here
Pawana Hospital is not just a healthcare provider—it is a pioneer of medical innovation in Maval.
🏥 Our vision is clear: ✅ Cutting-edge medical technology integrated with compassionate care. ✅ Affordable, accessible, and ethical healthcare for all. ✅ A stronger, healthier Maval region through prevention & innovation.
🔹 The future of healthcare in Maval is bright, and Pawana Hospital is leading the way.
📍 Looking for advanced, world-class healthcare close to home? Visit Pawana Hospital today!
0 notes
Text
Meet the Leading Oncologists in Dubai: Experts Who Are Changing Lives
Cancer is a battle that requires expertise, innovation, and compassion. Dubai has become a global center for advanced cancer treatment, boasting some of the most skilled oncologists in the world. Whether you need specialized care for colorectal, liver, or pediatric cancer, Dubai’s top oncologists are at the forefront of medical breakthroughs, changing lives every day.
In this article, we introduce some of the leading oncologists in Dubai, their contributions to cancer care, and why patients from around the world trust them for their treatment.
The Role of Oncologists in Dubai’s Advanced Cancer Care
Dubai’s oncologists specialize in a variety of cancer treatments, offering world-class services in both diagnosis and management. Their expertise spans across various fields, including:
Colorectal Oncology in UAE: Focusing on colon and rectal cancers, specialists in this field use cutting-edge surgical techniques and targeted therapies.
Liver Oncology Surgery in Dubai: Experts in hepatobiliary cancers offer minimally invasive procedures and liver transplants.
Pediatric Oncology Dubai: Dedicated specialists treat childhood cancers with a multidisciplinary approach to ensure better outcomes.
These subspecialties are crucial in providing personalized treatment plans that cater to each patient’s needs.
Pioneering Oncologists in Dubai: Changing the Landscape of Cancer Treatment
1. Experts in Colorectal Oncology: Precision in Surgical Excellence
Colorectal cancer is one of the most common cancers worldwide, and Dubai’s oncologists have developed innovative surgical and non-surgical approaches to treat it.
Patients seeking colorectal oncology in UAE benefit from state-of-the-art robotic-assisted surgeries, immunotherapy, and minimally invasive techniques that improve recovery rates.
2. Leaders in Liver Oncology Surgery: Revolutionizing Treatments
Liver cancer requires precise and complex surgical interventions, often involving liver transplants or partial liver resections. Liver oncology surgery in Dubai has witnessed a transformation with the use of 3D imaging for pre-surgical planning and targeted radiotherapy to preserve healthy tissues.
3. Pediatric Oncology: Giving Children a Fighting Chance
Children diagnosed with cancer need specialized care that balances aggressive treatment with long-term wellness. Pediatric oncology Dubai is led by compassionate specialists who employ personalized chemotherapy, radiation therapy, and innovative drug trials to improve survival rates while minimizing long-term side effects.
4. The Best Oncologists in the UAE: A Multidisciplinary Approach
The best oncologists in UAE adopt a team-based approach to cancer care. A single patient may receive treatment from medical oncologists, radiation oncologists, and surgical oncologists to ensure the best possible outcome. This integrated strategy enhances the success of treatments by combining expertise across various specialties.
Cutting-Edge Cancer Treatments Available in Dubai
The advancements in cancer treatment available in Dubai make it one of the most sought-after destinations for oncology care. Some of the most revolutionary treatments include:
1. Immunotherapy and Targeted Therapy
Dubai’s oncologists utilize personalized medicine, which tailors treatments based on a patient’s genetic profile. Immunotherapy has proven highly effective for certain cancers, boosting the body's natural defenses to fight malignant cells.
2. Robotic and Minimally Invasive Surgeries
Innovations in robotic-assisted surgeries have significantly improved precision, reducing recovery time and minimizing complications. These methods are frequently used in colorectal oncology in UAE and liver oncology surgery in Dubai.
3. Advanced Radiation Therapy
Modern radiation therapy techniques, such as proton therapy and intensity-modulated radiation therapy (IMRT), allow for high-dose radiation to be delivered with pinpoint accuracy, sparing healthy tissues.
Why Dubai is a Global Destination for Cancer Treatment
Dubai has positioned itself as a leading medical tourism hub, attracting patients from across the globe. Here’s why:
State-of-the-Art Medical Facilities: World-class hospitals equipped with the latest technologies.
Internationally Accredited Specialists: Many oncologists in Dubai have trained in prestigious medical institutions worldwide.
Holistic and Patient-Centric Care: A focus on both physical treatment and emotional well-being.
Access to Clinical Trials: Cutting-edge research and experimental treatments give patients additional options beyond conventional therapy.
For anyone seeking expert oncology care, Dubai’s best oncologists provide a comprehensive range of services tailored to individual patient needs.
Conclusion: Choosing the Right Oncologist in Dubai
Selecting the right oncologist in Dubai is a crucial decision that can influence treatment success and overall recovery. Whether you're looking for expertise in colorectal oncology in UAE, liver oncology surgery in Dubai, or pediatric oncology Dubai, Dubai offers world-class specialists dedicated to delivering the best cancer care.
To ensure the best possible treatment, take time to research credentials, hospital facilities, and patient reviews. The best oncologists in UAE are changing lives through their expertise, innovation, and compassionate approach to care.
If you or a loved one needs top-tier cancer treatment, Dubai stands as a beacon of hope, offering some of the most advanced and effective oncology care in the world.
Source : https://cancercarespecialtiesmena.blogspot.com/2025/03/meet-leading-oncologists-in-dubai.html
#oncologist in dubai#Colorectal Oncology in UAE#Liver Oncology Surgery In Dubai#Best Oncologist In UAE
0 notes
Text
Effective Liver Cirrhosis Treatment: Best Options for Managing Liver Cirrhosis
Understanding Liver Cirrhosis Treatment
Liver cirrhosis is a progressive disease where healthy liver tissue is replaced with scar tissue, leading to liver dysfunction. It is primarily caused by chronic liver diseases such as hepatitis B, hepatitis C, and long-term alcohol consumption. Effective liver cirrhosis treatment focuses on slowing disease progression, managing complications, and improving the patient’s quality of life.
Cirrhosis develops gradually and often goes unnoticed until significant liver damage has occurred. That is why early detection and proper liver cirrhosis treatment are essential to prevent severe complications and improve survival rates. Common causes include:
Chronic viral hepatitis (Hepatitis B & C)
Alcoholic liver disease
Non-alcoholic fatty liver disease (NAFLD)
Autoimmune liver diseases
Genetic disorders such as Wilson’s disease
Symptoms of liver cirrhosis may include:
Fatigue and weakness
Loss of appetite
Jaundice (yellowing of the skin and eyes)
Swelling in the legs and abdomen
Easy bruising and bleeding
Confusion or difficulty concentrating (hepatic encephalopathy)
Nausea and vomiting
Unintentional weight loss
Medical Liver Cirrhosis Treatment Options
1. Medications for Liver Cirrhosis
Medications play a crucial role in liver cirrhosis treatment, particularly in managing symptoms and preventing further liver damage. Doctors may prescribe:
Antiviral drugs: To treat hepatitis-related cirrhosis.
Diuretics: To reduce fluid retention.
Beta-blockers: To prevent bleeding from varices.
Lactulose: To manage hepatic encephalopathy.
Vitamin and mineral supplements: To prevent deficiencies due to poor liver function.
Immunosuppressants: For autoimmune liver disease.
Statins: To manage cholesterol levels in patients with NAFLD-related cirrhosis.
2. Lifestyle Changes and Dietary Modifications
A healthy lifestyle and balanced diet are essential for managing cirrhosis. Key recommendations include:
Avoid alcohol consumption completely to prevent further liver damage.
Follow a low-sodium diet to reduce fluid buildup.
Maintain a healthy weight to prevent fatty liver disease.
Increase protein intake to support liver function.
Stay hydrated to aid liver detoxification.
Consume antioxidant-rich foods to help reduce oxidative stress on the liver.
Limit processed foods and refined sugars to avoid fat accumulation in the liver.
3. Treatment for Cirrhosis Complications
Liver cirrhosis can lead to serious complications like ascites, variceal bleeding, and liver cancer. Specific treatments include:
Endoscopic procedures: To treat esophageal varices and prevent bleeding.
Paracentesis: To remove excess fluid from the abdomen.
Liver transplantation: The only curative option for end-stage liver cirrhosis.
Antibiotics: To prevent infections common in cirrhotic patients.
Bile acid medications: To improve bile flow and reduce liver stress.
Advanced Liver Cirrhosis Treatment Techniques
1. Minimally Invasive Procedures
For patients with severe cirrhosis, advanced procedures can help alleviate symptoms. These include:
Transjugular Intrahepatic Portosystemic Shunt (TIPS): A procedure to relieve portal hypertension and prevent variceal bleeding.
Radiofrequency Ablation (RFA): To treat early-stage liver cancer in cirrhotic patients.
Percutaneous Ethanol Injection (PEI): To shrink small liver tumors.
Balloon-occluded Retrograde Transvenous Obliteration (BRTO): To manage gastric varices.
2. Stem Cell Therapy and Regenerative Medicine
Research into stem cell therapy shows promising results in liver regeneration. Clinical trials are exploring the effectiveness of using stem cells to repair damaged liver tissue. Stem cell treatment aims to replace damaged liver cells and restore liver function in cirrhotic patients.
3. Liver Transplantation: The Last Resort
A liver transplant is considered when liver cirrhosis progresses to liver failure. In this procedure, the diseased liver is replaced with a healthy donor liver. Patients on transplant lists must meet specific eligibility criteria and receive post-transplant care to ensure success.
Prevention and Early Detection of Liver Cirrhosis
While liver cirrhosis is irreversible, early detection and preventive measures can slow its progression. Important steps include:
Routine liver function tests for individuals at risk.
Vaccination against hepatitis B to prevent viral infections.
Avoiding excessive alcohol intake to protect liver health.
Managing metabolic conditions like diabetes and obesity to reduce NAFLD risk.
Regular ultrasound screenings to monitor liver health.
Managing stress levels to reduce the impact of inflammation on liver function.
Consulting a hepatologist regularly for expert liver health advice.
Conclusion: Seeking the Right Liver Cirrhosis Treatment
Managing liver cirrhosis treatment requires a comprehensive approach, including medication, lifestyle changes, and in severe cases, liver transplantation. Early diagnosis and timely intervention can improve outcomes and enhance quality of life. By following a proper treatment plan, patients can manage symptoms effectively and reduce the risk of severe complications.
If you or a loved one is suffering from liver cirrhosis, consult a specialist for a personalized treatment plan. Taking proactive steps toward liver health can make a significant difference in long-term well-being.

For expert liver care and the best treatment options, reach out to Chennai Liver Foundation, a trusted name in liver health.
0 notes