#lads ekg
Explore tagged Tumblr posts
Note
Helloooo your blog is a liver saver for lore enthusiast like me! You know, although infold hadn't release much info on certain crucial aspect in the game but I was wondering what's your take or theory on how Protocore Syndrome works? Is it just another name for a Heart failure Disease or something more? Would love to read more of your fanon idea on it! And thank you for creating this amazing wiki blog! 💕💕💕
Ayyyy lore enthusiasts gang~ And of course! Thank you for reading! Sorry this took SO long to reply to. Had to do some major studying for this one lol.

I want to start off by saying that medical knowledge is not my area of expertise, so this is purely a layman's best interpretation based on everything I could learn at Google University 🤣 I managed to decipher her electrocardiogram (ECG/EKG) report results. But as for what irl diagnosis those results indicate, I simply lack the expertise required to deduce that answer. Even though I couldn't answer the second part of your question (believe me, I tried so hard 😭), I hope this post is still useful to you! To any medical or med school folk out there, now is your time to shine and save the day (pls 🙏).
How Protocore Syndrome Works?
The basic in-game description of Protocore Syndrome is very rudimentary and doesn't really give us a lot to go off of. But here's what we know:
Protocore Syndrome: From the "Deepspace Messages" section of the in-game Spacepedia resource, we learn that it is a unique disease caused by Protocores. There are different types, and they harm the human body in various ways. Currently, the known types are A, E, and Y
Type Y Protocore Syndrome: From the description given in the World Underneath story "No Morning", we learn that it is a heart syndrome that involves that hides in various organs and systems, with a long latency period, and slow progression. By the time it's detected, it's often too late. There is currently no known cure.
Still digging for concrete information to confirm the protaganist's diagnosis, but the story seems to infer she has Protocore Syndrome. (If you have any screenshots or resources that definitively identify her condition, pls dm me and I'll credit you).
From Zayne's statements during her chapter 1 appointment, we learn that she has Protocore fragments in her heart. He goes on to specify the following symptoms:
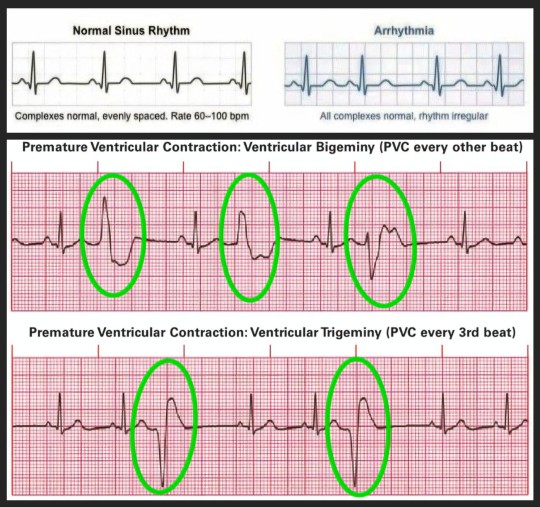
Heart arrhythmia
Premature ventricular contractions (PVCs)
Heart murmurs
The game shows us glimpses of her medical paperwork too. We are shown her ECG report and summary. After covering her report, I'll explain some potential discrepancies (emphasis on "potential" since I'm nowhere near an expert lol).
ECG Basics:
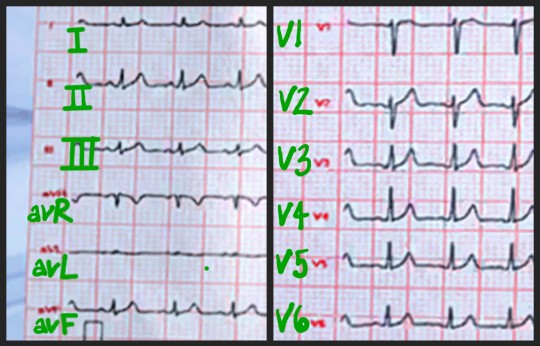
We're going to get a little technical here. But I think we'll get the most value from the analysis once we understand what we're looking at. The ECG shown in-game is a standard 12-lead report, producing 12 individual strips.
Leads:
There are the six limb leads: I, II, III, aVR (augmented vector right), aVL (augmented vector left), and aVF (augmented vector foot).
Then, there are the six chest leads: V1, V2, V3, V4, V5, and V6.
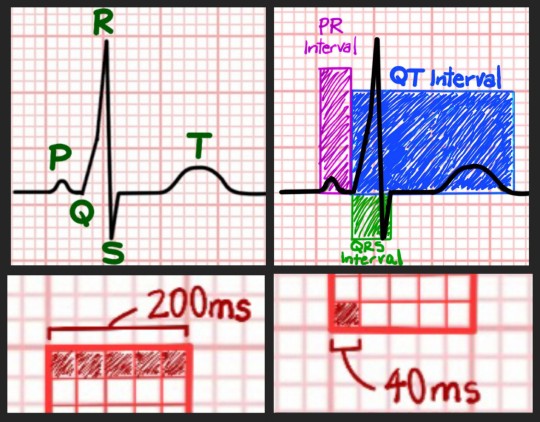
Intervals & Waves:
For the report details to make more sense, here's a quick reference to aid in the interpretation of different waves, wave interval, gain settings, and speed settings.
And, based on the gain and speed settings detailed below, each small square on her chart represent 40 milliseconds (ms) and each large squares represents 200 ms.
ECG Report Analysis:
Gain, Speed, and Heart Rate:
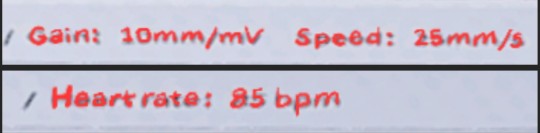
Gain: 10 mm/mV
Gain is a setting on an ECG machine that controls the size of an ECG trace. The standard gain setting is 10mm/mV, meaning that 10 mm on the screen represents 1 millivolt (mV) of voltage. It appears that Akso Hospital's ECG adheres to this standard.
Speed: 25 mm/s
Speed is the paper speed setting on an ECG machine. So, the Akso Hospital's ECG machine is set to 25 mm/s (meaning that each small square on the chart represents 0.04 seconds).
Heart rate: 85 bpm
Pretty self-explanatoty, but this measures how many times her heart beats within one minute. For women, a normal resting heart rate is considered 60-100 bpm, and hers is within this range.
PR Interval: 138 ms
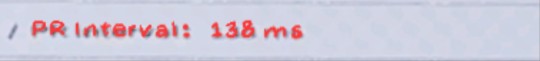
The PR Interval (or PQ Interval) is the distance between the start of the P wave and the start of the QRS complex. A normal PR Interval is between 120 - 200 ms. Since hers is 138 ms, she falls within the normal range.
QT & QTC Intervals:
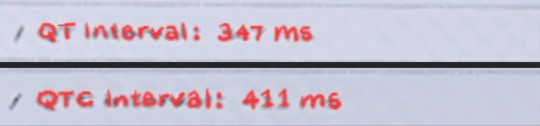
QT Interval: 347 ms
The QT Interval is the time between the start of the QRS segment and the end of the T wave. It measures the electrical activity of the heart's ventricles. For a heart rate of 85 bpm, a normal QT Interval would generally be 380 ms or less. So, hers is normal.
QTC Interval: 411 ms
The QTC Interval is the corrected QT interval (thats what the "c" is for). It represents the time it takes the heart's ventricles to contract and relax. It is calculated by adjusting the QT interval for heart rate. A normal QTC interval for women is usually less than 460 ms. Since hers is 411 ms, she's within the normal range.
P, T, and QRS Wave Axes:
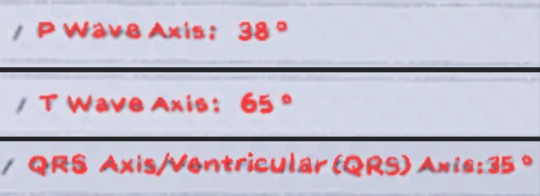
P Wave Axis: 38°
The P wave axis tells us the net direction of the P wave. A normal P wave axis is usually between 0° and 75°. Since hers is 38°, it falls within the normal range.
T Wave Axis: 65°
The T wave tells us the net direction of the T wave. A normal P wave axis is usually between 15° and 75°. Since hers is 65°, it is within the normal range.
QRS Axis: 35°
The QRS Axis tells us the average direction of electrical activity in the heart during ventricular depolarization. A normal adult QRS axis is between -30° and 90°. Since hers is 35°, she falls within the normal range.
SV1 and RV5:
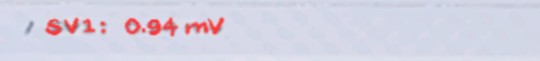
SV1: 0.94 mV
SV1 represents the voltage of the S wave from the V1 lead. It is used to detect ventricular hypertrophy. A normal SV1 is considered to be less than 2.5 mV and hers is within this range.
RV5: 0.85 mV
The RV5 represents the voltage of the R wave from the V5 lead. It is used to measure electrical activity in the left ventricle. An RV5 reading is considered normal if it is less than 3.5 mV and hers is within this range.
QRS Interval: 71 ms
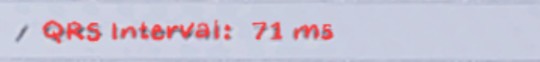
The QRS Interval the interval between the start of the Q wave and the end of the S wave. Represents the time it takes for electrical impulses to spread through the ventricles. A normal QRS Interval is 70-100 ms. Since hers is 71 ms, she's within the normal range.
Potential Discrepancies:
Okay. So, I thought it was a bit strange that all of her ECG readings were within the normal ranges. But I genuinely don't know if a patient can be diagnosed with an irl heart condition despite having an ECG that appears normal. Maybe its a diagnosis determined by other criteria we aren't shown?
Additionally, I looked up ECG strip examples of both cardiac arrhythmias and premature ventricular contractions (PVCs). And comparing them with her charts, I don't see indications of those symptoms in there.
#love and deepspace#lads#tysm <3#thanks for the ask!#ilysmmmm#lads protocore syndrome#love and deepspace protocore syndrome#lads random facts#love and deepspace random facts#random facts mc#love and deepspace mc#lads mc#random facts the protaganist#random facts protaganist#love and deepspace the protaganist#lads the protaganist#lads ecg#love and deepspace ecg#lads ekg#love and deepspace ekg#lads akso hospital#love and deepspace akso hospital#akso hospital
25 notes
·
View notes
Text
dear diary today was a rough day and not because work was hard but because it was just a lot ;;; let’s see where do i start
1. started the day by placing an impella in a patient that should have had a chest tube placed two days ago due to some bad pleural effusions. at this point he was decompensating and had coded twice so he needed the impella to give his heart a break. they also did an ekg which showed he was having a stemi! nice. we opened the rca, lad, and om1, and also found out he had some bad aortic stenosis. he was real sensitive as we were going in with the swan ganz to get pressures and actually went into vfib but we shocked him out of it :-) he seemed to be doing okay when we left so i hope he’s still doing well
the real kicker though was at the end of that case. we’ve got a nurse in orientation that has the knowledge but zero critical thinking skills and a bad attitude, so she was in the case with me and her preceptor. once we finished the case she asked me to waste some remaining sedation with her and return the meds we pulled from the med cart. for procedures that are high risk we pull out emergency drugs such as epinephrine, atropine, neo, etc. we didn’t end up using any for this case but the patient was still on the table so i told the nurse to wait until the patient left before putting the meds up. she wanted to put them up so that, in her words, her preceptor “wouldn’t yell at her.” i said “we may need these later, you never know what’ll happen once you pull the patient back into their bed, let’s put everything up once we’re truly finished” because patients like that can crash in a heartbeat and often times it’s when you’re trying to move them. like, this was a sick ass patient— intubated, almost maxed out on levo, had coded twice before, vfib arrested on our table— it’s common sense you’d keep that stuff available. and, her preceptor wouldn’t have yelled at her because the case wasn’t finished and would have said the same thing i did. sure enough, as we’re pulling the patient from the table to the bed, his waveform on the impella tanks and his map drops into the 30s, and his heart rate dropped from 130s to 60s. we move him back to the table and call the dr in to assess because we were worried we dislodged the impella during transfer. at this point, we’re seconds away from doing cpr - we’re bolusing levo, troubleshooting the impella, everything. his heart rate keeps dropping so the dr tells us to give epi. but….the nurse went behind my back and returned all the emergency meds we needed…. so instead of having it at the ready, i had to pull it from the omnicell. luckily we keep our drugs in the room so we don’t have to go far to get them but that is the *exact* reason why we don’t put the meds up until the patient is gone. in situations like that you don’t have time to unlock the omnicell, search for the patient, search for the drug, and pull it out. it’s just basic common sense and what’s best for the patient. and stuff like that we keep trying to teach her but it’s not clicking and she just doesn’t seem interested. and her background in critical care isn’t apparent at all. so that’s just an ongoing frustration but telling her point blank that we need to keep the meds out but then i see her returning them a few minutes later pissed me off.
2. got called to IR for a vascath and we had just gotten the patient on the table when the doc comes in and starts putting his sterile gown on. as in to start the procedure. mind you he had to leave early so he wanted to get it finished but we hadn’t gotten anything set up. i had barely gotten his info in the ultrasound and x-ray and hadn’t gotten consent and this dr wants to start??? no. not to mention he wasn’t on the monitor??? luckily he was stable but that was not cool. and then the dr has the audacity to correct me and say “this should have been done before we started” THEN he starts to yell because we didn’t move the table when he wanted us to? omg if i wasn’t already pissed off and was in a mood to argue i would have said something. because how dare you expect us to have everything prepared for you ~just how you like it~ when you don’t give us the time to set up. so inappropriate. this is the same dr that says the cath lab team is too incompetent to do anything more complex than a vas or permacath. which is such an insult to us because we’re the only cath lab in the city that does peripheral procedures like venograms and aortagrams, and does antiemobolization procedures for pe’s and dvt’s. aka procedures that are often done in IR….
1 note
·
View note
Text
Sugar Bear
The needle pierced stubbornly, reminding Josef of some other prick he’d met before. The ‘prick’ in his arm had been more courteous, but he still thought about calling that other lad up and maybe trying him out for a drink once…, if, this was all over. Josef, for sure, would appreciate that moon-lit beau of a man compared to the intern currently fumbling through his medical records, double-checking the footnotes the resident doctor would no-doubt quiz him on later. It was his acne that really held him back, Josef thought, otherwise he could do well on a Friday night at Jo’s. ‘Aren’t you like 25?’ he thought.
Beep. Beep.
The EKG machine droned on the same as it had for the 2 weeks he had been arrested to the hospital bed, his own body turning against him. He had fair warning over the years, and the medication helped. Unfortunately it was still in the trial run, and he wasn’t sure if fate had given him the placebo or not. ‘Just my luck to get the motherfucker that hates workin’. Making another mental note to call the lad, Josef sighed, deeply. It was the loudest thing in the room, followed by the machine and the rustling of papers.
“Okayyyy… Mr. Royce?” the intern questioned.
“Guilty,” Josef replied, saluting the newbie doc with a wave of his hand from his diminishing hip.
“Right on, okay sooo…” He trailed off. ‘Bonus points for being cute,’ Josef thought.
“It seems the targeted therapy didn’t quite pan out as well as we had hoped,” the Intern continued, putting emphasis on the word hoped only. ”The targets in your liver unfortunately did not respond to the treatment, and the Gemcitabine doesn’t seem to be having a strong effect anymore either.”
‘Bummer’, Josef thought.
“We can continue attempting to limit the spread as much as we can, but the cancer has already reached your lymph nodes, and we’re running out of effective treatment. At this point in time we may have to consider transitioning to hospice care to help alleviate any symptoms and pain, go over any end-of-life treatments with loved ones, begin getting your affairs in order…” The intern waved his hand in the air unintentionally dismissive, the entire time his eyes glued to the pages. Contained in those sheets, the science spoke of no miracles. The intern was very aware of that. “Etcetera.” He raised his head to meet Josef’s. ”The choice is ultimately up to you. I am very sorry.” He then bowed his head, holding his papers in his hand and taking them to his waist, one fist over the other, a move no doubt practiced in the mirror likely before he entered the room. Josef was appalled.
“Did you literally just bow your head? Is this your first time throwing the ‘you’re dying’ bomb or something?”
“Well no-,”
“I’m just kidding, doc. I gave my last doctor a bunch of shit too. He was an asshole though.”
“Doctor Lund?” Josef continued the joke and nodded. “Ha! He’d get a kick out of that.” The intern looked at his papers, seemingly pleased. I may be dying but I still got it, Josef thought.
“Anyways, I did want to mention that we do have one more alternative, if you would like to continue treatment.” All business, this guy. Josef nodded, a sign to continue which wasted minimum effort. “There is a new drug being developed which is seeing higher than average success rates in animal trials. They just opened trials for human treatment, and I think it could potentially be a good match, you do qualify.” He checked his papers again. “The biggest issue is, of course, there is no guarantee.”
Josef thought for a moment and then responded. ”So basically it could prolong my life a little, but I’ll probably just be sick the entire time, and there’s a high probability I’ll die anyways?”
“There are no guarantees, unfortunately.”
“I’m gonna need the opinion of my trusty advisor then if you don’t mind.”
“Sure sure! I completely understand, I can give you some time.”
“No need, she’s right outside.” Josef cupped his hands and pointed his mouth at the door.
“HEY SUGAR BEAR, BABY, COME IN HERE FOR A MINUTE.”
There was an audible scratching at the door as the doctor turned and stared perplexed. The door opened, and a tiny hand waved through the door, announcing her welcome. This was followed promptly by a tiny head, and the young girl walked timidly into view. Her grandfather behind her opened the door wide enough for her to slip in, then waved them away as he awkwardly dismissed himself from view. No doubt they were both eavesdropping.
The doctor stared at the young girl, then looked at Josef. “Your advisor I’m assuming?”
Josef nodded. It was easy to nod, just a shake of the head.
“My daughter.” Josef motioned to the tiny creature and the girl ran up to his bed with both arms raised. Once she got to his side she realized her father wouldn’t be much help in getting her up, instead backing up two steps to run and hop her upper half onto the bed. Josef moaned quite playfully and the young girl gingerly clambered up to his chest, where she pushed herself onto his ear and whispered into it. Josef nodded again, and the girl carefully placed herself on his hip.
“There you go. Anyways, can you explain what you just said to me again, doc?”
The doctor cautiously glanced at the girl as if she secretly held the cure for cancer herself. “You- do you want me to explain to her what I just said?’”
“You’re the doctor.”
“Mr. Royce, I’m not sure what you want me to do here.”
Two hazel eyes that seemed to encompass an entire third of the child’s face peered at the doctor. Mouth slightly open, the child didn’t seem to have much of a response either.
“Doc, I want you to meet Sugar Bear. That’s her name.”
“Hi… Sugar Bear.” The Intern cautiously waved with a quick motion of his wrist.
“Go ahead Doc, she’s smart.” Josef kissed his daughter’s head. The little girl laid back onto his chest, keeping her head level and continuing to look at the doctor. She waved back, a bit more enthusiastically.
“Ummm…… Sugar Bear?”
The Girl nodded.
“Um.” Josef urged the doctor with another nod. “Alright so…” The intern was caught off guard, he quickly realized he had never had to explain death and probabilities to a child before, that was always the parent’s job. He had been trained about counseling patients of course, however he avoided pediatricy as much as possible, as children were often gross, whiny, hyperactive goblins. The little goblin before him seemed pretty interested in what he had to say however. The intern sighed. Josef was loving it.
“So Sugar Bear, I have some bad news. Your dad, umm, is very sick, very very sick. He’s been fighting the cancer, the thing hurting him and making him sick, for a very long time.” The intern used his counseling skills as best he could, keeping eye contact with the tame child. It blinked ever so slowly, mouth slightly hung open to maximize oxygen intake. She looked maybe four years old. “Its- it’s getting pretty hard to keep the fight going and umm… sw-sweetie I don’t think this is a fight that your dad can keep trying to win.” Her eyes furrowed, a child trying to understand what it already sort of knew.
Another nod from dad. “Say it doc.”
“…. So, umm, your dad and I were talking and well, uuh, he has two choices.” The intern held his fingers up for visual representation. “He can still keep fighting,” he curled his middle finger and kept the pointer straight, “and we can try one more thing.” Sugar bear’s expressions never changed, except for her eyebrows, which moved slightly with the end of each sentence, as if she was recounting what she heard in her head. She briefly glanced at the doctor’s pointed finger, counted one with her mouth, then concentrated again at the man in the lab coat who was helping her daddy. “The problem is, is that your daddy is already hurting a lot, and this could be a really long-.”
The intern, who realized he had stooped in order to be level with the child, stood up and waved his hands. “Mr. Royce I’m sorry but I need to ask, this is, this decision is entirely based on you and you alone. I, I can see why you’d like,” he gestured towards the girl,” Sugar B- her, this kid, involved, but I don’t see the need to explain to your daughter about this until you decide, otherwise I think this is a lot of pressure. She can’t decide for you.”
“Ha!” Josef countered almost immediately.
“Mr. Royce please take this seriousl-.”
“To hell she can’t.” The girl turned to look at her father.
“Excuse me, Mr. Royce, I don’t mean to tell you how to,” a broad gesture, “‘parent’, I’m just not sure how to explain,” and another gesture,” to your daughter how she can weigh in on your treatment. How old is she anyways?”
Sugar bear played with her hands, firmly tucked into her father’s lap as he stared amused towards the intern.
He pulled a lock of hair from her eyes. “You gotta give her more credit, doc, kids in general,” Josef stated. He turned to look up at the doctor, now employing his counseling skills he learned as a parent and social worker.
The intern sighed. Josef continued.
“Cover your ears bubbie.”
The girl did so.
“Listen Doc, I don’t want to tell you how to,” Josef gestured with only one hand, the other tucked around Sugar Bear, “‘doctor’, but it’s my right to discuss these things with my family. You see that old man out there? That’s her grandfather from her mom’s side. ‘Sugar’ here is a copy of her mom, basically, and it was her wish before SHE died that I get custody of her. Not her actual father, fucking drunk he is, or her actual grandfather, ME.” Josef pointed at himself. Sugar turned to look at the finger, counted one, then turned back. She kept her hands in place.
The intern stood silent.
“She was my best friend. This girl is her mirror-fucking-image, I swear to god. I can’t even tell you about the legal battle I went through, it was hell. I raised her before she was even speaking, I’m her goddamned father. I didn’t even want kids.” Josef again looked at Sugar Bear. “You don’t understand ’til you have them. No doctor, this doesn’t affect me, I don’t give a shit. I’m old and greying, I did my thing already.” He hugged her with both arms. She lay back into his chest. “You need to tell this girl and it needs to come from you because pretty soon she’s going to lose her grandfather too. She’s going to go through a world of hurt and she’s going to have to endure some of it alone, and she needs to know that she can go to fuckheads like you and handle shit like an adult because she’s gonna grow up so fucking fast and I don’t think the world is ready for her, but she can be good and goddamned ready for it. So you fucking tell her, and explain it as best as you can, to the best of your ability please.”
The intern wavered for a second, abashed. A few seconds passed before he responded, “but what can she do about it?”
“Have you tried actually asking her?”
The intern did not understand. He looked at the girl.
Josef tugged at her sleeve and she relaxed her hands, head resting still on his chest. She was watching the screen on the television, hardly aware of the conversation that was just had.
“Ms. Bear?”
She turned as if to say ‘Oh me?’
“… I was trying to tell you earlier that your dad… he might pass away soon.”
Confusion from the girl.
“He, he’s going to heaven, with your mom.”
Sugar bear gasped and covered her mouth. Josef hugged her tightly and she turned to him and hugged his neck . “Noo daddyyy,” was heard very subtly behind him.
“It’s okay baby,” Josef rocked her gently, allowing her a moment to process. After a second he brought her forward and pointed to the doctor. Wiping her eyes, she turned back to the doctor with a grimace, breathed in deeply, and tried to steady herself.
“I’ve been teaching her that,” Josef stated with a smile.
The intern couldn’t help but chuckle. He truly believed the man before him had led a good life, the way he humbly seemed to accept death.
“Nice job man… Hey Sugar Bear?” The girl nodded in between shuddered breaths. She uttered a whine, but managed her breathing. “Hey hey, it’s okay. I wanted to let you know, there’s still something we could do.” The girl was wiping her eyes, but now her full attention turned to the doctor. “ We can still try to save him, but it might hurt your dad even more. He’s already hurting a lot, so you might not like what you see if we do try, and there’s a good chance that he might not make it either way.” The girl uttered another sob. Josef comforted her as best he could. “The other thing we could do…. the other thing we could do is try to make him as comfortable as we can until his last breath.”
The girl wiped her eyes and muttered “Conftable?” in between deep breaths, trying to master the sobs that randomly escaped her.
“Yes… We can try to make sure he doesn’t hurt so much. That way you can see him happy and quiet while he waits to… see your mommy again.” The intern had a hard time keeping his tears in now. They were bold faced lies, but close enough to the truth for a child. “Your dad said he wanted you to say what we should do. Your daddy thinks you’re pretty smart.” The intern smiled.
‘Cute,’ Josef thought, followed immediately by ‘Ya I have faith.’
“Conftable.” Sugar bear said it again, this time to herself, one hand rubbing her right eye. There were no more tears, but it was comforting. Josef held her other hand. “The other one.. hurts? Hurts him?” She put her hand to Josef’s face, and Josef took her scent in, adoring her smell and committing it to memory for the thousandth time.
“Yes… Yes it hurts, but it could help him too. We just don’t know.”
“Mmm,” She whined, “does it hurt a lot?”
“It could. He might not be too happy if you see him and, well, we just don’t know sweetie we’re trying the best we can.”
A moment passed by, the fate of the world being mulled over by a pre-schooler before nap-time. She lay back down on her father’s chest. She could feel his heartbeat still, at least.
“I want daddy to be happy.”
“You.. you want him to be happy?
She put her thumb in her mouth and vigorously shook her head up and down. Her father nodded approvingly.
“Yeah baby, that’s what I want too.”
The intern had no words. So, he followed his script. More patients to see.
“Okay, umm well, great, well,” he wiped his eyes, “Umm, Mr. Royce.” The intern bowed his head again. “I will… discuss the treatment plan with your pharmacist and uh, we’ll see about what options we have, that way maybe we can discuss transitioning to in-home treatment, so we can make you as… comfortable as we can.” He smiled at the man sitting with his daughter and wondered.
“Thanks, doc.” Josef winked.
The intern turned to leave, but he caught himself catching a glimpse towards Sugar Bear, who had begun falling asleep with her hand by her face, eardrum placed firmly over her dad’s chest.
“Don’t worry about her, she’ll get a good inheritance.” Josef touched his thumb and forefinger together and rubbed them back and forth. “So will the old man. Sorry for calling you a fuckhead by the way. Do me a favor will ya, grab me my phone from the counter please? I gotta schedule a date.”>
0 notes
Photo



The left main coronary artery bifurcates into the left anterior descending artery and the left circumflex artery. If there is a blockage involving the left main coronary artery, all myocardium downstream would be affected and you would likely see ECG changes involving V1–V6, I, and aVL. Osteopathic examination demonstrates Chapman points in the 2nd and 3rd intercostal spaces, which is suggestive of myocardial dysfunction in this patient. Chapman points in the 2nd intercostal space may also represent dysfunction in the thyroid gland, esophagus, or bronchi. Chapman points in the 3rd intercostal space may also represent dysfunction in the upper lung or upper extremities.
Bottom Line: Because the left anterior descending coronary artery provides blood to the anteroseptal portion of the heart, a blockage would likely result in ST-segment elevations involving leads V1–V4.
COMBANK Insight: The anatomy of the coronary arteries is a hot topic because it gives test writers a chance to test anatomy and cardiology with the same clinical case. The left anterior descending artery is the most common artery associated with myocardial infarctions.
3 notes
·
View notes
Text
Random E! Thoughts: S4E22 - 905-Wild
Of all the Season 4 episodes, THIS is the one with the original intro and good picture quality? Oh for fuck’s sake.
I mean, don’t get me wrong, I kinda like this one - It’s not necessarily a great E! episode (on account of being very little E!), but it’s pretty entertaining TV nonetheless - but Season 4 has so many incredible episodes in piss-poor quality... yeah.
I really like the credits for the Show That Wasn’t, I gotta admit.
Do you ever wonder who the hell signed those people playing some of the victims and families? oh boy, that kid and her grandpa.
Johnny and Roy working on a goat, looking as determined and serious as they ever have.
Would they... would they be able to get a reading through all that fur, though?
The lads, sending that EKG without first explaining that that’s a goat.
The looks Johnny and Roy share as Johnny has to tell them that that’s a goat.
I love how it’s Morton who starts caving first on treating that goat.
Dix inadvertently calling Kel out on the whole “not treating the goat” thing
Dix also fetching the goat, no matter what Kel says
Joe and Mike being on Dix’s side pretty much instantly
Kel telling Joe to shut up
“quiet as a mouse” [...] “let’s go, mouse”
The entire goat operation and how tense it is
Johnny, silent, until Roy remarks upon it
Morton, standing up to Kel being an asshole
Johnny, finally cracking and saying something after all
The lads both being startled when the HT goes up - but Roy barely flinches while Johnny practically jumps.
It always feels so odd when the camera cuts to Johnny and Roy in this episode, and the scene after the goat’s okay is no different - especially because the contrast between the animal control guys and our lads really stands out here - the animal control guys are touched, but each on their own, while pretty much the first thing Roy does is to look over at Johnny.
(not to mention how bafflingly close to each other they’ve been standing this entire time, lol. Hardly even registers by now.)
One person out of the two medical teams clearly did manage to pick up a phone. My money’s on Joe or Dix.
10 notes
·
View notes
Photo
Story time! The start of this story has a bit of a theme song, because i just always think of this: www.youtube.com/watch?v=uyGSe7… Sad and awful as it looks, this actually has a majorly happy ending! Major thank you to my friend Sumi-Sprite for collaging this for me! -------------------------------------------------------------------------------------------------------- When Walter is 22, he goes on a very dangerous mission with Lance. While they wait for backup (which Lance is willing to accept most of the time now on account of personal growth), the duo storms a chemical lab, where the "final battle" takes place. I don't have a lot of details worked out, but long story short, they succeed in their mission (with several casualties as a result of what comes next), but fire and blow-outs in the lab lead to a very terrifying situation. The men find themselves in a space with only one oxygen mask for emergencies. Lance forces Walter to wear it, but even after being taught compromise, the latter is very stubborn. As Lance begins to lose consciousness from being stuck inhaling smoke and various chemicals, Walter takes advantage of this. He shoots him in the neck with his own tranquilizer (a familiar scene, no?), and as Lance is passing out, Walter gives him the mask instead. Lance passes out from the tranquilizer, and Walter slowly begins to suffocate until he too, is rendered unconscious. Lance wakes up in the medical bay at the H.T.U.V. Delirious but suddenly remembering the mission, he starts to panic and call out for Walter. Not a few moments later, the younger of them reveals he's in a bed right beside Lance's, groggy with an oxygen mask strapped to his face, an IV in his arm and an EKG hooked up to him, but he's smiling and reaching out for Lance. Lance takes the boy's hand firmly and says "You scared me." Walter answers with "You scared me first...!" He sleepily explains that backup came and rescued them and brought them back to the agency, where they've apparently only been for a short while. In better shape than Walter on account of the latter's sacrifice, Lance gets up and lays beside him, jokingly threatening a "quadruple fire" if he ever does something like that again. Walter very softly smiles and says "I'm not sorry." When Marcy eventually shows up to visit them after hearing the news, she finds them laying there in the bed together and jokingly asks if she's interrupting something. "Nope, just two grown men cuddling after they almost died, nothin' to see here," answers Lance in a similar tone. Marcy informs them that most of their targets were saved and are in custody (some of them being in the hospital), but a few of them died from the fire and chemical blast. Walter is sad to hear it, but accepting of it, and glad that not every life was lost. About an hour or two later, he's stable enough to be off of the oxygen and other attachments. With all the smoke and chemical inhalation, the medical staff advises giving Walter a bronchoscopy to check for potential damage to his lungs. Such a procedure often only requires conscious sedation with a numbing of the nose and throat, but when they get him to the operating room, Walter panics at the thought of being awake while having a scope down his throat; after having nearly suffocated to death just hours ago, the thought of being awake and the fear of suffocating again is too much to bear (even though he would be fine). So instead, they decide to give him a general anesthesia and put him under for the procedure. It's just safer for everyone this way. When it's over and he's beginning to wake from the anesthesia, Walter is wheeled back to his room on the bed, and is happy to see Marcy and Lance waiting for him. But anesthesia is a funny thing, and as he's wheeled in, he's singing the Disclaimer Song in a very loopy fashion. Once settled, he chooses not to finish the song. This conversation ensues: ------- "Lance: You're not gonna finish the song? Walter: *mildly sassy* Ffffhhh, youknooww... I sing...ALLLL the tiiime, anndiiiffinishh all of them, anndd it'ssfuunn, buut... Whyy issitt aalwaayys me...? Why'd's WalterrBeckkett onlyy siing??? YOUU finishth'sonng... Lance: *"well shit" face* Wow, all right then, I'll finish the song. ♫Don't try this at home, if you do, you might--♫ Ey, aren't you gonna sing? Walter: ...Mmm givinng youaheadd starrtt..." ------- He joins in eventually. There is a lot of talking about various things, and lots of Marcy and Lance laughing to themselves at the rambling and singing. Oh yes, more singing. Lots of singing. Lance records some of the rambling, including an entire conversation that begins with Walter casually asking if they'll have to "take his lungs out." After being told no, that he's perfectly fine, he says it would be hard to breathe without lungs, and then regales his company with the thought of the lungs being replaced with balloons. Specifically, the left one would be blue, and the right one would be red. Why? He doesn't know, it's not his call, apparently. At the thought of them popping if he took too deep a breath, a laughing fit on Walter's part ensues. A little while later, this conversation happens: --- "Walter: Whenn I'mmbetterr, 'm gonna drriiveyou'round in the e-tron... Lance: You wanna drive me around? Walter: Yeaaah... Ohh, waait... Imight craash... Lance: Naaahhh, i think it'd be worth the risk. You can drive the car. Walter: Buutt youuloove that carr... Lance: Yeah, well... I love you more. Walter: Hmm..... Whaat...? Lance: *softly* I said I love you, Walter." --- Lance has told him this before, but in his drugged up state, the blatant expression of love swiftly turns the tide of the mood from funny to pitiful. Walter bursts into tears and tells Lance he loves him, too. And Marcy. And Killian, and Joy, and Lovey and Jeff and Crazy Eyes, and Terrance even though he ignores him, and August (OC) and Ramsey (OC [sorta]) and Shannon (OC) and that he thinks it's mean that people nickname Joy "Joyless," all while bawling his poor eyes out. Endeared, Marcy and Lance try to calm him down. But Walter reveals that he hasn't forgotten his conversation with Lance when they first woke up in that room together. He says he's sorry for scaring Lance, that he just didn't want him to die because he "doesn't want to be alone again," but that he understands Lance has the same fear and he just couldn't win. Somewhere in the rambling mess of emotions, he mentions fear of Lance "dying like his mother." Basically, every subconscious or pushed-down negative thought and feeling he's had since the mission comes blubbering out in a heap of drunken tears and sadness. Seeing how very real his distress is, his company is quick to try and ease his mind and offer him comfort. Walter asks if Lance really is going to fire him again, to which Lance says no. He then asks if Lance is mad at him, which earns another "no." Lance says no one is mad at him, that he just needs to close his eyes and try to take a nap. After a few minutes of quietly crying to himself with his eyes closed, Walter comes to a terrifying conclusion... What if he never stops crying?! Of course, Lance almost bursts out laughing, but a death glare from Marcy forces him to keep it to himself, lest he risk further upsetting Walter. It may sound ridiculous, but for someone who's been anesthetized, every feeling is very real. Marcy comforts him, tells him no, he's not going to cry forever. It's not long before the tears slow down. They don't stop, but they slow down. [fun fact: crying is reported in 40% of patients who wake from anesthesia, be it for a presented reason or for no reason at all. Very little is known about why this occurs, though it's suspected that the stress and fear from whatever they had to be put out for manifests itself in that drugged-up state. This is referred to as "the boo-hoos."] But it's late, and Marcy must go home. She and Lance talk off to the side, and the lady gives her man a kiss to remember her by for the evening.~ After Marcy's departure, Lance decides that after everything they've been through and with how upset Walter's been, he will sleep in the bed with him. He reclines him, crawls in, and holds him tight until morning. Walter wakes up around 1 in the morning, mildly confused, but Lance tells him to go back to sleep. Happy that Lance stayed with him and choosing not to question this unexpected all-night cuddling party, he submits without a word. By morning, everything is fine, and the anesthesia has worn off. Before the lad can even put his clothes on, Lance just HAS to show him the video he took of him while he was all loopy. Walter is embarrassed and cringes through it, but also laughs at some parts. It's a happy ending. "Okay but for real, don't ever do that again." "No promises." ----------------------------------------------------------------------------------- ------------------------------------------------------------------- ----------------------------------------------- This movie is something else. Lance, Walter and Killian have all experienced trauma and loss, but in different ways. Walter and Killian are the extremes; one copes with loss through love, wanting desperately to let people in and let others know they aren't alone. Killian has no way to cope, and expresses his pain through hatred and a desperate longing to make the one who hurt him feel what he's felt, and then end it all in his own death. Lance is right in the middle. He has acquaintances, he talks to people, he cares, but he holds everyone at arm's length. He pretends everything is fine, he acts cold and aloof, "too cool" for playing on a team or working with others. But really, it's a fear of letting others in, because life could take it all away again. He still bears a lot of empathy, but also exercises carelessness on criminals. He and Killian are not so different, but with Walter's help, both men learn to open up (we can see Killian's expression for redemption in his final scene in the movie, we know he was a little touched that Walter saved him. Also consider, Killian didn't know Walter survived that fall at the time). So now that they're partners and each have someone in their lives to love -- multiple people now, in fact, it means feeling desperation to keep them close. It means taking a bigger risk, it means work. After everything they've been through, no, Lance is not ashamed to hug and hold and love on his little nerdy white gay son. He's not afraid of intimacy anymore, no matter the form. He'll take what he can get, because tomorrow is never a promise. Would you die for the ones you love...?
#Spies in Disguise#Walter Beckett#Lance Sterling#Marcy Kappel#Unus Annus#kind of#i mean i meme their song all the time#disclaimer song
152 notes
·
View notes
Photo

Oh man. Just beware that I have some embarrassingly strong opinions on medical notes. I was (and still am) one obsessive motherfucker when it concerns patients under my care... probably, at times, at the expense of my mental health. So...
We’ll start with your general hospital H&P
As a medical student, however your attending wanted your note written was always the correct answer. That applies to a lesser degree during residency. You’ll generally figure out the people who have strong opinions because, without fail, they will tell you. In those situations, again, the correct answer is whatever your attending says is correct is correct.
The biggest tip I can give is to develop a mental template for everything. I wrote every H&P during residency in a very specific format. It had a couple of advantages: (1) I never left something important out, and (2) it sped up my ability to churn out H&Ps. Now that template had slight variations depending on which service I was on because, as you probably already have realized, different things are important to different subspecialties. In the beginning, it may be near impossible to put together a mental template just because you’re still learning to differentiate the signal from the noise. Everyone is. I will say that my notes now, as an April first year fellow, are much better and more succinct than my notes were as a July first year fellow. That is perfectly ok to adapt things as you learn more and more. So my basic template for a hospital admission was this:
------------------------------------------
HISTORY OF PRESENT ILLNESS
------------------------------------------
A minimalistic one-liner that should tell you, in broad strokes, what you need to know to start formulating a differential diagnosis.
Mr. Smith is a 58 YOM with PMHx significant for [only RELEVANT co-morbidities] who presented by ambulance to the ED for shortness of breath of three days duration.
Next, this is where you break out your mnemonic of choice to describe the patient’s chief complaint. Was onset acute vs slowly progressive? What was his baseline respiratory status and how does it compare to now? Is it continuous or does it only happen when he’s moving? Does he have any pertinent associated symptoms? What makes his sob better or worse? Has this happened to him before? Pertinent negatives to rule out other possible causes of the patient’s chief complaints.
Patient reports his shortness of breath started two days ago and has slowly worsened. At baseline, he is able to ambulate without limitation but is now having difficultly walking more than from room-to-room in his home. While he initially only had symptoms with exertion, he now has symptoms at rest. Sitting in an upright position improves his shortness of breath and lying flat worsens his symptoms. He endorses worsening orthopnea, PND, and lower extremity edema. No fevers, chills, localized symptoms of infection, or sick contacts. No associated cough. No chest pain or anginal equivalents. No personal or family history of blood clots. Reports he was hospitalized two years ago for similar symptoms that required IV diuretics.
Next, I went into the objectives obtained in the ED. What were the patient’s vitals on presentation? What pertinent abnormalities were noted on labs? Imaging? If there were any consults, what was recommended? What treatment was provided in the ED?
In the ED, patient was afebrile, normotensive, but tachycardic to the 120s and initially satting 85% on room air. He was placed on 4L supplemental O2 with improvement. Labs were significant for acute on chronic elevated creatinine, a minimally elevated troponin, and severely elevated BNP. EKG showed sinus tachycardia. CXR showed bilateral pulmonary edema. Cardiology was consulted in the ED and felt his elevated troponin was due to demand ischemia rather than true ACS. Patient received 80 mg IV lasix and was admitted to the gen med service for further care.
------------------------------------------
ASSESSMENT
------------------------------------------
Now a few lines that succinctly presents the case, from beginning to planned end. My goal was always to present a quick overview of the patient’s treatment course.
Mr. Smith is a 58 YOM with NSTEMI s/p DES to the LAD and HFrEF 2/2 ischemic cardiomyopathy who presented to the ED with shortness of breath with a new oxygen requirement and was found to have a HFrEF exacerbation. Treatment course was complicated by a brief transfer to the step-down unit for BIPAP support following admission. He has since been treated with aggressive IV diuresis with improved respiratory status and was transferred back to the floor. He is now maintaining appropriate oxygen saturations on room air. Plan for discharge in 2-3 days following conversion to PO lasix.
------------------------------------------
PLAN
------------------------------------------
These are pretty straightforward. I usually presented off of this part of my note and included things that helped me keep track of my patient’s pertinent history and recent results. For this guy, that would mean knowing this guy’s last EF by echo and when his PCI was performed.
#Acute hypoxic respiratory failure 2/2 HFrEF exacerbation.
-Presented to ED with shortness of breath and new O2 requirement
-Hx of NSTEMI s/p DES to the LAD in Oct 2018
-Baseline EKG with sinus tachycardia. No change compared to prior.
-Last echo in Jan 2019 with EF = 30%; echo 4/8/20 showed EF 15% and WMA of the left apex
-Dry weight 70 kg; patient currently above dry weight at 78 kg
PLAN
-Lasix 40 mg IV; goal net negative 1L
-Follow-up on BID BMP; replete lytes as needed
-Arrange outpatient visit with heart failure clinic
If anyone is interested, especially the new ‘terns or med studs, I can do some additional posts on note writing tips. Outpatient notes are also definitely a completely different ballgame and thus approach.
#medblr#pgy-dinosaur#COVID19-Fest 2020#medical school#internal medicine#residency#internal medicine is the BEST medicine
61 notes
·
View notes
Text
going to get an ekg lads :/
9 notes
·
View notes
Text
Vocivore, Ltd. (16 of ?)
A OUAT WINTER WHUMP FIC
Also on FFN and AO3 (still need to update there!) (ListerofTardis)
Tagging @ouatwinterwhump, @killian-whump, @cocohook38, @killianjonesownsmyheart1, and @courtorderedcake <3
***THE MOST WONDERFUL COVER ART BY COCOHOOK38 HERE!!!!!******
****ALSO!!!!!!!!!!!!Chapter 12 animation and art that will absolutely astound you!!! THANK YOU MY WONDERFUL COCONUT FRIEND!!!!!!!!!!*************
Present (Wednesday, continued)...
Jones sat alone in the hospital cafeteria, nursing an overly sweet sports drink and wondering at the liveliness of the place at 3:00 in the afternoon. It wasn’t as if the population size of Storybrooke would explain it; nor would the rather pathetic selection of entrees on offer. He could only conclude that the majority of customers were family members of the slaves captured that morning, come to check on their loved ones and only now getting a chance for a lunch break. It certainly wouldn’t be the slaves themselves; Whale would have them tucked away for observation and whatever experimental therapies he was devising for their life-threatening condition.
The detective was quickly discovering the inconvenience of having injuries to the undersides of both forearms. He could not rest either on the table in the normal fashion, for that placed pressure directly on the cuts. Neither could he rotate the wrist without pulling on the stitches, which were now beginning to make themselves known in a prickly, itchy sort of way as the anesthetic wore off. Jones sighed, regretting his decision to postpone the pickup of his prescriptions from the pharmacy. The sudden, fierce ache in his chest added another check to the “Pick Up Now” column. He glanced irritably at his phone lying on the table next to his drink. He had wanted it easily accessible in case Emma called, but it had been at least half an hour since she’d dismissed him, and nothing.
When he looked up, he was startled to see David coming through the door, flanked by his wife and son and looking a bit worse for wear. But he had new clothes on and one arm in a sling; it appeared as if he’d been released to go home. As Snow and Neal headed into line, Jones caught David’s eye with a comradely nod, and the prince smiled wearily and headed in his direction.
“Mind a little company?” asked David as he neared. Jones gave him a lopsided grin and shook his head.
“Be my guest.” He waved at the three empty seats, and David lowered himself carefully into the one across from him. David let out a low, rueful groan, adjusted his sling arm, and winced; Jones’ own injuries twinged in sympathy. “I’m relieved to see you traveling under your own power, mate.”
“Same,” said David, a little sheepishly. “Sorry for leaving you to fend for yourself back there.”
“Not your fault,” Jones assured him. “Who’d have guessed it would take a whole score of slaves to commit simple arson?”
Snow White appeared around the corner and hurried over with a bottle of juice and a package of cookies. She gave a hasty but kind greeting to Jones as she unscrewed the lid, then set both items in front of her husband, saying,
“I’d better go make sure Neal isn’t trying to order one of every dessert in there.”
She dashed off. David took a swig of juice and gestured at the cookies.
“Help yourself; it’s all that sounded good to me at the moment.”
“Standard blood donor fare?” Jones suggested, and David laughed.
“Maybe that’s it.” He picked up the cookies, carefully brought the packaging to his immobilized arm, and pulled lightly. The effort’s only accomplishment was to bring a pronounced grimace of pain to his face, and he immediately gave up. Jones leaned in slightly, impish grin in place.
“May I make a suggestion?”
“I’m not sure a hospital’s the best place to look for a hook lying around,” David teased, though the detective could still see lines of pain around his eyes.
“Think simpler, mate.” Jones reached for the package, wincing a little himself as his sternum spasmed a sullen protest. He pulled the cookies closer, flashed a wink, and said simply, “Teeth.”
Deftly, he gripped the plastic with his incisors and tore it open, managing not to dump the contents all over himself. Then he returned the snack to his friend. David smiled wryly and accepted, grumbling,
“Good thing I’ve just been dosed with antibiotics. Protection against pirate slobber.”
“No need to worry, David: I’ve hardly kissed anyone today.”
The friendly banter was helping to take both of their minds off of their pain, the stress of the morning, and their worries, at least for a short moment. But the mood was all too fleeting, and as Jones glanced again at his phone, David must have sensed his mild concern.
“You, uh… heard anything about Killian?”
The detective quickly filled him in on the current situation, concluding with his intention to call Emma if he hadn't heard from her within the next few minutes. David nodded his approval. He swallowed a mouthful of cookie, looking thoughtful, then said,
“I kinda don’t know what to think.”
“About what?”
“Well… him. He’s gotta be pretty badly brainwashed if he isn’t immediately giving up intel on Hope, but… if he is…”
“Then why aren’t either of us dead?” Jones finished the thought. “I’ve been wondering the same.”
“I mean, you know how he thinks, how he fights… is it possible he missed both times? Or was too weak to finish us off?”
Jones considered this as if he hadn’t been mulling it over for hours already. “I… suppose it's possible, yeah. With the neurological symptoms especially.”
David seemed to find that answer satisfactory and gave a one-shouldered shrug. “Guess we should just be grateful, then.”
But Jones remained uneasy. There were a hundred ways to kill a man, and he knew them all. Many did not require much power or finesse. Yet Killian had aimed for places almost guaranteed to be survivable.
Head suddenly spinning, Jones rubbed at his eyes, careful not to brush against the impressive swelling on his cheek. His bed sounded irresistibly appealing at that moment. As Snow and Neal made their way to the table, both carrying trays laden with mediocre food, Jones reached for his phone. To the backdrop of Neal’s incessant chatter, he dialed Emma, wearing a politely distant smile.
“She’s not picking up,” he finally reported. “Could be she’s fallen asleep as well.”
He gritted his teeth and stood, stiff muscles and sore places hampering easy movement. “I’ll go check on them; she’ll likely be peeved if she sleeps through the only opportunity she has of speaking to him.”
“Let us know how it goes,” David requested.
“Aye, of course. Enjoy your meal.”
“Later, Killian!” chirped Neal, and Jones gave a stiff wave farewell.
“Alice is looking forward to having you aboard the next cruise, lad. She says it’s been exceedingly helpful to have a proper junior crewman along.”
Neal bounced in his seat, excited at the reminder, and Jones smiled fondly. With a nod, he retrieved his sugar water and set off toward his counterpart’s room.
*****
Emma was sleeping, all right.
In Killian’s bed.
With his equipment attached to her, and no sign of him anywhere in the vicinity.
Momentarily stunned by the sight, Jones shook himself and strode to the bed, calling,
“Emma? Are you all right?”
The sheriff stirred slightly at the sound of her name. Not quite sure what had taken place, Jones opted for caution and pressed the nurse call button as he searched her face and arms for any sign of trauma. “Emma?”
Emma groaned quietly and reached for her face. She pulled a deep, slow breath, groggy and disoriented. With a grunt, she rubbed her eyes open. They fixed on Jones and immediately filled with confusion. “Killian? What happened?”
“I don’t know.”
She struggled to her elbows and winced. Jones put a hand on her shoulder.
“Take it slow.”
Emma glanced down at the EKG leads snaking beneath her shirt, at first with massive confusion. But then something clicked, and she sat bolt upright, cursing. Jones took a step back at her vehemence. She wasted no time tearing the sensors off, which set the machines to aggravating beeps of warning.
“Emma, where’s Killian? Did he…?”
He honestly did not need to ask. It was fairly obvious: ground floor private room, easy access to the window, and his unconscious wife left in his place. Still, it seemed an unbelievable circumstance.
A nurse came trotting in, but stopped dead in her tracks as she tried to reconcile the confusing scene. Frustrated and frantic, Emma tore the blood pressure cuff from her arm and practically spiked it into the mattress beside her.
“Uh… Mr. Jones?” inquired the nurse, but the wrong Jones ignored her. Emma had swung her legs over the edge of the bed, evidently about to race off to do gods-knew-what in order to retrieve her wayward husband.
“Were you struck on the head?” Jones asked bluntly, moving to prevent her standing up. “Maybe you should--”
“I’m fine,” snapped Emma. “Get out of my way.”
Without waiting, she surged to her feet, and Jones had to scramble backwards to avoid a collision. Emma pushed past the bemused nurse on her way to the window, swearing the whole way there.
“What’s going on here?” demanded the nurse. “What was she doing in your bed? And what are you doing out of it?”
Jones sighed and prepared to explain himself again, but Emma beat him to it. She turned from the window.
“He’s not my husband. My husband’s gone, dammit.”
“He’s… gone? You… think he went out the window?” The nurse was clearly considering whether to call Security, Dr. Whale, or both.
“He’s gone,” confirmed Emma. Without further ado, she slid the window open and prepared to hurtle through.
“Ma’am, I can’t let you--”
Emma flashed her badge at the nurse, who blinked once and changed her tune. Slightly.
“Sheriff, I can’t let you--”
Jones moved toward the window, adding his own protests to the nurse’s. “Emma, wait; let’s call Henry, or Regina, or--”
Halfway outside, Emma fixed them both with such a dangerous look that they froze in mid-sentence. “I’m going after him. Go home, Jones. You can’t help me right now.”
She wriggled easily the rest of the way through, dropped to the ground into some bushes, and was gone. Jones sighed, reaching for his phone. She didn’t expressly forbid him to call for backup…
Still quite nonplussed, the nurse turned back to Jones, taking in his clothed state but also his readily apparent injures. She frowned at him.
“Are you sure you’re not Killian Jones?”
#ouat fanfiction#wish realm killian#david nolan#emma swan#detective charming#hospital#pain#injuries#escape#Vocivore ltd#queued
15 notes
·
View notes
Text
Proposed Acute Coronary Syndrome (ACS) Chest Pain Pathway Using Quantitative FMTVDM Nuclear Imaging
Short Communication
There are an estimated 8 to 10 million emergency room visits each year for the evaluation and treatment of acute coronary syndrome; i.e. ischemic coronary artery disease; with potential consequential damage to the heart muscle itself (infarction). The standard diagnostic evaluation has routinely included a series of tests looking for evidence of concurrent tissue injury happening at the time of evaluation. This includes a standard 12-lead (perhaps more depending upon specific clinical acumen and equipment) electrocardiogram (ECG) looking for evidence of ST elevations of greater than 1 mm in two or more contiguous leads or in some instances V4 alone for distal LAD disease. Additional information is occasionally gleaned by reciprocal changes. To compare changes over time, patients routinely undergo more than one ECG. In addition to the use of ECGs (also called EKGs to prevent confusion with the term EEG), looking for membrane conduction and ion transport abnormalities caused by damaged myocyte and conduction tissue resulting from insufficient coronary blood flow for the needs of the tissue, clinicians also routinely obtain a series of blood tests looking for enzymes and proteins which have been released from the myocytes themselves. The sequence with which these “cardiac enzymes” appear in the blood are directly related to the fact that ischemic membrane damage will initially result in the leakage of smaller molecules followed by progressively larger molecules. The classic sequence of released molecules is consequently, based upon our current level of knowledge, myoglobin, creatine kinase (CK), Troponin I (TnI) and Troponin T (TnT), serum glutamicoxaloacetic transaminase (SGOT) which is also known as aspartate aminotransferase (AST) and finally lactate dehydrogenase (LDH).
Read More about this article: https://irispublishers.com/acrci/fulltext/proposed-acute-coronary-syndrome-acs-chest-pain-pathway-using-quantitative-fmtvdm-nuclear-imaging.ID.000525.php
Read More about Iris Publishers Google scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=d1PdB38AAAAJ&cstart=20&pagesize=80&authuser=1&citation_for_view=d1PdB38AAAAJ:qxL8FJ1GzNcC
1 note
·
View note
Text
Juniper Publishers-Open Access Journal of Case Studies

5-Fluorouracil (5-FU)-Induced STEMI
Authored by Moamen Al Zoubi
Abstract
Treatment of solid tumor malignancies involves the use of toxic chemotherapeutic agents with potentially life threatening complications and requires vigilance on the part of the physician in promptly recognizing potential adverse effects. We describe a 39 year-old Korean male with history of poorly differentiated gastric adenocarcinoma, who presented with chest pain and shortness of breath 12 hours after completing the first 5-FU cycle. His ECG showed inferior-posterior STEMI. Troponin peaked at 39. He was started on nitroglycerin and heparin drip. His emergent angiography revealed diffusely ectatic coronary arteries. Intracoronary nitroglycerin injection resulted in almost complete resolution of stenosis. He was discharged on aspirin, clopidogrel, atorvastatin, isosorbide mononitrate and amlodipine. It was decided to avoid treatment with 5-FU for his gastric cancer in the future.
Case Presentation
A 39 year-old Korean male with history of poorly differentiated gastric adenocarcinoma, stage IIA (pT2N0M0) status post total gastrectomy and distal esophagectomy who completed the first 5-FU cycle 12 hours prior the presentation to our hospital for chest pain and shortness of breath with one hour duration. He received 5-FU as a continuous IV infusion for 46 hours. Chest pain was substernal, pressure-like, and constant and associated with diaphoresis. ECG showed inferior-posterior STEMI (Figure 1).
Patient was started on nitroglycerin and heparin drip. A limited echocardiography revealed an ejection fraction of 45-50% with severe hypokinesis of the basal and mid infero-lateral myocardium. He was taken emergently to the catheterization lab for coronary angiography where he was found to have diffusely ectatic coronary arteries (Figure 2). The distal RCA was found to have a focal area with 50-60% stenosis without any evidence of thrombus, which was thought to be the culprit lesion based on the EKG and echocardiographic findings. After intracoronary nitroglycerin injection there was almost complete resolution of stenosis with significant improvement in the filling of the RCA distal segments. Post angiography, patient was continued on nitroglycerin with complete resolution of symptoms and repeated ECG 3 hours later showed almost complete resolution of ST elevation (Figure 3). Troponin peaked at 39. He was also found to have an intermediate lesion in the proximal LAD that was assessed 3 days later with a Lexiscan stress test which was negative for ischemia or infarct areas. Given diffuse coronary ectasia, he was evaluated for collagen vascular disease or Kawasaki disease but workup was negative and he did not meet criteria for complete or incomplete Kawasaki. He was discharged on aspirin 81mg once daily, clopidogrel 75mg once daily, atorvastatin 40mg once daily, isosorbide mononitrate 60mg every morning, and amlodipine 10mg once daily. It was decided to avoid treatment with 5-FU for his gastric cancer in the future.
Discussion
Cardiotoxicities have been reported from the use of 5-FU including acute coronary syndrome, vasospastic angina, coronary thrombosis and dissection, malignant arrhythmias, cardiomyopathy, and sudden cardiac death [1-7]. However, 5-FU has a proven therapeutic benefit and remains an important component of first line adjuvant chemotherapeutic regimens in the management of gastrointestinal malignancies. Hence, careful consideration should be given before discontinuing 5-FU at the cost of decreased therapeutic efficacy of chemotherapy in survival outcomes.
5-FU and its oral prodrug capecitabine are widely used in chemotherapeutic regimens in the treatment of gastrointestinal malignancies. Cardiotoxicities are infrequent but important side effects and may necessitate discontinuation of these medications. Reported incidence of symptomatic cardiotoxicities occur from 1 to 19 percent of patients treated with 5-fluorouracil with severe cardiac events including MI, cardiogenic shock, sudden cardiac death occurring in about 2% of treated patients [8]. Cardiotoxicity was most common during the first cycle of 5-FU chemotherapy [9]. ECG abnormalities during 5-FU administration suggest myocardial ischemia as a plausible mechanism behind most of its cardiotoxic effects [10]. Concept of vasospasm leading to myocardial ischemia has been suggested, since coronary angiography usually failed to show coronary artery stenosis with 5-FU cardiotoxicity [11- 17] although coronary artery vasospasm was observed during coronary angiography in rare cases [18-20].
Several suppositions of 5-FU related coronary vasospasm have been proposed. One theory of 5-FU related coronary vasospasm is higher level of endothelin-1 (ET-1) in 5-FU treated patients. ET-1 is a potent vasoconstrictor produced predominantly by endothelial cells [21,22] But under pathophysiological conditions, production of ET-1 is stimulated in several different cells, including vascular smooth muscle cells, cardiac myocytes, cardiac fibroblasts, macrophages, and leukocytes [21-25]. One study showed higher ET-1 level in patients experiencing 5-FU cardiotoxicity during 5-FU treatment than those without cardiotoxicity [26]. This study also showed higher plasma levels of ET-1 in 5-FU treated patients compared with those receiving non-5-FU chemotherapy [26].
Another theory of 5-FU related coronary vasospasm is protein kinase-C (PK-C) mediated vasoconstriction of vascular smooth muscle. Mosseri et al. [4] used ring of aorta from rabbits exposed to different concentrations of 5-FU and pretreated with PK-C inhibitor and observed for vasoconstriction. The result indicated that 5-FU causes direct, endothelin-independent vasoconstriction of vascular smooth muscle in vitro, this vasomotor response involves activation of PK-C, and this response is independent of vasoactive cell membrane receptors, phosphoinositide turnover, or activation of the cyclooxygenase pathway [4].
Coronary artery ectasia predisposes to complications including coronary artery thrombosis, embolism, and vasospasm [27,28]. Contraintuitive to medical reasoning that ectactic vessels are less capable of spasm due to medial damage, ectatic vessels are actually prone to increased risk for spasm. This was elegantly demonstrated by Bove and Vilestra in a provocation experiment with ergonovine which showed augmented 65 to 93% maximal narrowing of ectactic coronary vessels in the study patients compared to 40% maximal reduction in luminal diameter in normal controls [29]. This narrowing was later shown by computer analysis to occur adjacent to the ectactic portions of the coronary vessel and not in the ectactic portions per se [30]. Sorrell et al. [31] suggested a mechanism linking chronic increased local nitric oxide(NO) production to the development of coronary ectasia, which was later supported by experiments documenting locally increased acetylcholine concentrations from downstream inducible NO synthase (iNOS) pathway stimulation [32]. It may be suggested that the local effects of 5-FU, in our patient, may have provoked the ectactic coronary vessels to go into coronary spasm via increased inhibition of a commonly linked hyperactive iNOS pathway.
Increased vasomotor tone due to inhibition of endothelial NO synthases and endothelium-independent vasoconstriction via protein kinase C pathway potentially explains coronary spasm effects of 5-FU [18]. Traditional cardiac risk factors may increase the risk of cardiac side effects and create diagnostic dilemmas. However, isolated case reports and clinical reviews on patients with 5-FU associated cardiac side effects with no known prior heart disease point towards a true causative cardiotoxic potential of 5-FU [8,10]. Cardiac and renal comorbidities, continuous prolonged duration infusion schedules, concomitant cisplatin treatment are potential risk factors for 5-FU associated cardiotoxicity [1,3,6,8]. There are several case reports which showed vasodilator therapies such as calcium channel blocker and nitrate resulted in resolution of chest pain or normalization of ECG changes [33-37]. Prophylactic calcium channel blockers therapy was successful in one case to prevent recurrence of 5-FU-induced variant angina [36].
Our patient presented within 72 hours of his first cycle administration of 5-FU; upto 70% of the side effects have been noted to occur within the first three days of the first cycle of 5-FU [6]. Diagnosis rests on prompt assessment of chest pain with ECG, cardiac troponins and further angiographic studies if there exists high likelihood for coronary artery thrombosis. Therapy with nitrates and CCBs and discontinuation of 5-FU infusion can result in prompt symptom resolution [38-40]. Currently, there exists insufficient evidence to suggest rechallenges with 5-FU but may be considered if there exist no reasonable alternative therapies in the setting of antivasospastic therapy prophylaxis, close clinical monitoring during infusions and with alternate schedule administrations [3,6,38].
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#juniper publishers contact info#juniper publishers journals#Critical Care Medicine#Gastroenterology#Immunology#Microbiology#Otolaryngology#Pediatrics
0 notes
Text
A pt came in with a saddle PE. She had HTN and mild R heart strain, so interventional radiology decided not to remove the thrombus but to keep her on heparin gtt for now. From the intern's note:
#saddle PE #elevated d-dimer CTA from Anna Jacques consistent with saddle PE involving both pulmonary arteries and RV to LV ratio 0.9 suggesting some mild R heart strain. EKG with no ST elevation, LAD. Troponins less than 0.03, probnp 598, d-dimer 17151, and lactic 2.7. Upon transfer to PRH, troponins 15.2, probnp 617, and hypertensive 188/90. IR consulted upon transfer.
- IR consulted, per Dr. Nortin, based on hemodynamic stability and minimal R heart strain, conservative management with heparin gtt at this time with no indication for thrombectomy - stable on 2L NC - continue heparin gtt - continue ASA 81mg daily - trend troponins - trend proBNP for further RHS evaluation - EKG prn - telemetry - PT/OT - protonix ppx
2 notes
·
View notes
Text
Missed an entire week of work lads!
Work week Sunday-Thursday to clarify
Saturday going into Sunday, stomach cramps, feverish, pukey- called out Sunday obviously. Slept a large part of day.
Monday still exhausted, chest pains increasingly noticeable, coughing
Tuesday emotionally exhausted and physically fatigued, chest pain, cough
Wednesday chest pains even worse- called nurse hotline, told to go urgent care. EKG and 2 chest X-rays. 7 vials of blood drawn. Saline and Ativan IV.
Told not to work Thursday by urgent care doctor and to follow up with my GP as soon as they had an open slot.
So I’ll be seeing doctor on Tuesday
I have never once missed a whole week of work due to illness. Being in your 30s at an increasingly stressful job is ~so fun~
0 notes
Text
Safety and Efficacy of Transbrachial Access for Coronary Procedures: Case Report and Review of Literature | Iris publishers

Authored by Mehssani Z*
Introduction
Trans radial approach (TRA) has gained popularity over the trans femoral access (TFA) and has become the default option for coronary procedures around the world, as it has less bleeding access site complications and it is associated with a lower degree of adverse clinical events rate. However, in some situations, the trans radial arterial access could be unsuccessful. We present a case of a 66 years old man with history of aortobifemoral bypass surgery admitted in our department for an ACS and neither TFA nor TRA access were possible.
Case Report
We describe a case of a 66 years old male, with an aortoiliac occlusive disease who was admitted to the vascular surgery unit for aortobifemoral bypass surgery. He had a significant medical history of hypertension, diabetes and an extensive smoking. Pre-operative CAD screening including stress test was normal. The day following the vascular surgery, the patient suffered from severe angina with EKG abnormalities and troponin elevation. He was diagnosed with a non-ST-segment elevation myocardial infarction (NSTEMI). He was forthwith referred to our department for an angiogram to assess for coronary artery disease that may require revascularisation therapy. In the Cath Lab, the radial artery pulse was non palpable due to the thick arterial wall and a low flow state, puncture and cannulation on both radial arterial sides were challenging. In addition, the transfemoral access was not feasible knowing that the patient has just undergone an artobifemoral graft surgery one day ago (Figures 1&2).
To overcome this technical problem, the right brachial artery as an alternative vascular access has been attempted. 1 ml of lidocaine was injected into the subcutaneous tissues overlying the right brachial artery (Figure 3).
A Terumo needle dedicated to radial access was used and a 6F sheath (Terumo interventional system) was pushed easily over an hydrophilic wire and inserted for diagnostic purpose and ad-hoc intervention depending on needs, the intra-arterial nitroglycerine usually used in TRA access to prevent spasm was not administered, and 3000 UI of unfractionned heparin was injected into the sheath sidearm. Judkin’s left and right catheters were successfully advanced into the ascending aorta enabling left main and right coronary engagement and angiography without any difficulties in catheter manipulation during the procedure.
Severe CAD was diagnosed with left main disease, mid LAD stenosis , severe obtuse marginal stenosis and a severe calcified lesion of the RCA ostium. CABG was proposed in order to perform complete revascularisation. After the procedure, the sheath was removed and hemostasis was done by digital compression for 15 min. The puncture site was bandaged and a hard support has been placed under the arm to limit movements of the elbow, with very close monitoring during the first 6 hours.
Discussion
Trans radial arterial approach (TRA) coronary angiogram reduces vascular complications compared with trans femoral approach (TFA). However, the mechanism and predictors of TRA failure access have not been well characterized (Congenital radial artery atrophy/hypoplasia, tortuous configurations, radioulnar loop and abnormal origin of the radial artery; damage to the radial artery and loss of pulse). Many interventional cardiologists considered that switching to the TBA is outdated and risky access. It has been demonstrated significantly higher rate of vascular and neurological complications than other access in previous studies [1]. Nevertheless, with additional care by using smaller sized catheters, an adequate anticoagulation regimen proper methods for achievement of haemostasis as well as a close and careful observation afterward, Newcomers are trying to overcome this mindset and make the TBA approach possible when the TRA fails [2].
Sabbah et al [3] studied 4955 cases undergoing coronary revascularization. Respectively, 22 %, 57 % and 21 % cases were divided into TBA, TRA, and TFA groups. Results showed that forearm artery access in TBA and TRA groups was associated with higher procedural success compared with TFA group . Compared with TRA group, TFA group had higher rate of MACE and inhospital cardiac death, and also higher incidence of major access site hematoma. TBA and TFA groups had higher rate of access site pseudoaneurysm. Gan et al [1] studied 5110 cases undergoing coronary procedures. Of these, 180 and 121 cases were enrolled to TBA and TFA groups, respectively.
Results showed TBA group had a slighter lower incidence of major complications compared with TFA group without significant difference even in minor complications. There was no incidence of brachial artery thrombosis and no puncture-related neurological dysfunction in TBA group.
Conclusion
Our case alongside cited studies above provides evidence that the brachial approach has to be considered as an efficient alternative to the femoral approach for coronary angiogram and interventional procedures when radial access is unsuccessful.
Read More...Full Text
For More articles in Archives of Clinical Case Studies please click on: https://irispublishers.com/accs/
To Read More : Iris Publishers Linkedin
0 notes
Text
Lots of Listens in 2020
As I winnow things down to my Top 20 and, ultimately, AOTY, I’ve come up with quite a few great records that didn’t quite make it into the top echelon...
All Fell Silent - An Autumn For Crippled Children These Dutch practitioners of black-gaze have moved even further into the the “gaze’ side of things by pushing their drums (machine) even further into the background -- sometimes threatening to become ambient music.
10 Years Gone - Deafheaven Speaking of “black-gaze,” this live shit rules. All the hits form all their records with enough rawness and grit to drive the whole thing home.
An Offering - Deterior Apparently this is one dude from Columbus OH. Its fantastic blackened post-metal with plenty of crusty sludge to gum up the proceedings.
Lincoln Hall 2020 - Facs Another live album. This time from Chicago’s ultimate purveyors of fugue-state. A well curated collection of songs from their three records performed with their characteristic aggression/ennui.
Sawtooth EKG - Flust Ex-Twelves singer, Michael Groome, churns out a sultry album of Depeche Mode-inspired make-out tunes. It’s the 80s all over again and I feel fine.
Revisionist - June of 44 The actual title is Revisionist: Adaptations & Future Histories In The Time Of Love And Survival -- ha! It’s remixes and rerecordings of some of the venerable post-rock outfit’s later material. While it doesn’t really hang together as an album, its nice to hear these versions and experimentations. Reminds me of their In The Fishtank record, now that I come to think of it...
Boss Chill - Killer Tame Brendan McGinn is probably best known as the frontman of Lincoln NE’s emo wunderkinds, Her Flyaway Manner. Here, under his beat-maker moniker, he creates inventive and addicting trip-hop than clearly owes a debt to Ninja Tune or Mo Wax.
s/t - Luxor Beam These London lads seem intent on trying to recreate Revolution Summer emotional hardcore. They sorta miss the mark, but by adding noise-rock and post-hardcore elements, they come up with something at least as interesting.
Itch - Mammock Weirdo, mutant noise-rock from Greece. They, mercifully, often stray from the Jesus Lizard-template and veer into math-jazz territory of folks like Oxbow.
Zero Zero Zero - Mogwai Mogwai continue their triumph over movie soundtracks. Here for a show about drug trafficking. It’s got all the somber-yet-catchy piano riffs that we’ve come to expect, but also a fair bit of synthy swells and kraut-rock rhythms. I watched the first episode on Amazon Prime and fell asleep...
Ghosts V-VI - Nine Inch Nails Trent continues his Ghosts series which, I guess, is just song sketch pads that he may or may not go back to later. V reminds me a whole lot of side two of Bowie’s Low and VI sounds like the soundtrack to demented horror movie.
Demo - Rijeka Some cool textural screamo (by way of hardcore) that, while not earth shattering, is extremely satisfying and visceral. Not sure why a band from France names themselves after a city in Croatia...
s/t - Seaxes There can be no doubt that this band hails from Chicago. The ghost of local noise-rock giants hover over this EP like a spectre. Cool shit though, with nods to both The Jesus Lizard and US Maple without ever really aping either of them.
Three Gates Dub - Tara Bulba British dude doing trippy dub shit in the style of Bill Laswell. More of this please.
The Twilight Device - Theta Beach Ambient swells and drones -- the soundtrack to a non-existent movie. Turns out it’s the perfect soundtrack to white knuckling it on country roads in a blinding snow storm.
Now Wait For Last Year - Things Falling Apart Yet another live record (this time on the radio). The long-running post-rock band leans into the “post” with two songs running 19 and 13 minutes. FULL DISCLOSURE (lol): included in the download is a remix I did for Adama under my Bell & Circuit moniker.
Another Life - Twin Siblings Ex-New Cowboy Builders and current Sugar Horse guitarist, Jake Healy, continues to spellbind with his solo project. Less dark than previous outings, here he delves into dubby kraut-rock, Eno-esque swirls, and Cabaret Voltaire-style electro.
0 notes
Text
ABIM: Cardiology
ABIM syllabus can be found here Let me know if you find any errors Sources: UWorld, MKSAP 16/17, Rizk Review Course, Louisville Lectures, Knowmedge (free version)
Hypertension
Essential Hypertension: lifestyle modification first - >140/90 = thiazide only (ACEi if DM) - >160/100 = thiazide + __ (two drugs) Renal Hypertension: - woman with flank bruits, flash pulmonary edema - increased renin and aldosterone - treat with ACEi Coarctation of the aorta: - high arm BP, low LE BP; radiofemoral pulse delay, cold extremities, PVD-like cramping symptoms - AS murmur (early systolic murmur @ RUSB) - figure “3″ on CXR, posterior rib notching - if symptomatic, Tx with balloon dilation Hypertensive urgency: >180/120 Hypertensive emergency: urgency with end organ damage; Tx: IV Hydralazine Undifferentiated hypertension: - PCC (catecholamines) - Cushings (decreased K, metabolic alkalosis, hirsuitism) - Hyperaldosterone (decreased K, increased aldosterone:renin), etc
Pericardial disease
Acute Pericarditis: - within ~42hours post-MI; may have increased troponin - Tx with high dose ASA (NOT NSAIDs, NOT steroids) vs. Dressler: weeks to months after MI associated with fever, leukocytosis, pleuritic chest pain; Tx NSAID if >1mo from PCI/CABG Pericardial effusion: can be associated with malignancy - continue ASA or DAPT - leave it alone if asymptomatic Constrictive pericarditis: calcification on CXR (pathogmnomonic) - loud S3 (pericardial knock) and rub - ECHO shows swinging ventricular septum (NOT seen in restrictive CM) --> if indeterminate results: get hemodynamic catheterization - associated with liver disease and cirrhosis with ascites*, increased JVD but normal CVP - Tx with supportive IVF and vasopressor s--> pericardiectomy *if ascites present: ascites protein >2.5, SAAG >1.1 (vs. cirrhosis: ascites protein <2.5, SAAG >1.1)
Ischemic heart disease
Stable angina pectoris: - goals: BP <140/90, A1c <7%, LDL <100 - Tx: ASA + statin + beta blocker + ACEi if EF <35% (or if they have CAD equivalent) + Diltiazem or Verapamil to keep HR 55-60 Acute coronary syndrome: PCI within 90 minutes > tpa within 30 minutes and then transfer to PCI hospital anyway. - PCI after 4 hours of continued pain + STE - tPA contraindications: CVA within 3 mo, brain cancer, major surgery within 3 weeks, BP>180/110, >10minutes CPR, pregnant - when to do CABG: left main >50%, LAD and prox Cx >70%, 3 vessel disease MI complications: acute hypotension, heart failure symptoms - VSD: palpable thrill --> obtain TTE; Tx: nitroprusside, pressors --> OR - acute MR / pap muscle rupture: acute pulmonary edema (may have holosystolic murmur) - free wall rupture: death Coronary vasospasm associated with migraine headaches; Tx with CCB Heart failure from ischemic cardiomyopathy: *FYI: Metoprolol = okay even in COPD patients *FYI: decreased cardiac output in heart failure may improve with afterload reduction with Nitroprusside (may counterintuitively raise BP) - NYHA III-IV: Spironolactone decreases mortality - NYHA III-IV in AA patients: Hydralazine + Nitrates - ICD if EF <35% after 3 months of failed maximal medical therapy - BiV if NYHA III-IV with QRS>120 or NYHA II with QRS >150 - heart transplant if decreased vO2max Pacemaker settings prior to surgery: change ICD settings to asynchronous pacing and disable shock
Dysrhythmias and conduction defects
*FYI: reperfusion arrhythmias after MI don’t need anti-arrhythmic treatment - WPW: decreased PR with slurred up broad QRS (delta wave); AVOID BB/CCB/Digoxin (may induce VFib); acute Tx with procainamide (*mnemonic: proCANUSamide treats WOLFf-parkinson-white) OR if unstable: cardiovert; ultimate Tx: ablation *be suspicious of WPW in Afib with broad/unusual QRS Bradyarrhythmias: Tx: atropine Tachyarrhythmias: Valsalva, BB (Metoprolol or Verapamil), CCB 1. Regular rhythm: - Sinus tach (>100bpm) - AVNRT (p waves buried in QRS, but otherwise regular): Tx: adenosine - AVRT: decreased RP interval - Atrial tach: increased RP interval 2. Irregular rhythm: - Afib: warfarin for CHA2DS2-VASC >1; for pre-op: hold warfarin and DON’T bridge - Aflutter: Tx: ablation > medication - MAT: >3 p waves Other: - VTach: wide QRS (”tombstone”); Tx: BB, Lidocaine, Amio, shock - Torsades: Tx Magnesium
Congenital heart disease in adults:
Atrial septal defect: fixed split S2 (mnemonic: “split ASs” (a butt has a crack in it so it’s split into two cheeks)), EKG shows RAD with partial RBBB - often discovered with pregnancy - close if symptomatic (orthodeoxia/platypnea) or RA/RV hypertrophy Patent foramen ovale: don’t worry about it. Start ASA if cryptogenic stroke. Bicuspid aortic valve: very young patient with syncope and weird systolic or diastolic murmur (can be either, but most often associated with AS); evaluate for dilated aortic arch PDA: continuous machinery murmur; pulmonary HTN and LE cyanosis (vs ToF cyanosis which has cyanosis of all extremities) VSD: loud holosystolic murmur that obscures S2 with palpable thrill --> may also develop pulm HTN, R to L shunt, AR (blowing decrescendo diastolic murmur) or TR (holosystolic murmur that radiates to liver) Pulmonary regurg: decrescendo diastolic murmur at LSB that increases with inspiration, may present with parasternal heave, associated with Tetralogy of Fallot repair
Valvular heart disease
* see Heart Sounds post for more detailed valve disease facts *if mechanical heart valve, even if pregnant, DO NOT STOP WARFARIN (and aspirin). Aortic stenosis: - systolic crescendo decrescendo murmur at RUSB that radiates to the carotids, - decreases with Valsalva, increases with squatting - pulsus parvus et tardus (delayed carotid upstroke) - preload dependent state (DO NOT GIVE NTG) - severe <1cm or mean TV gradient > 50mmHg = Tx with valve REPLACE, otherwise Tx with diuretics and ACEi Aortic regurgitation: - blowing decrescendo diastolic murmur that radiates to the apex - associated with Marfans, aortic dissection, Syphilis/aortic aneurysm - chronic Tx with ACEi, Nifedipine - acute Tx: valve REPLACE with nitroprusside, IV diuretics and dobutamine/milrinone for support Mitral regurg: - associated with chordae rupture after MI --> acute pulmonary edema/cardiogenic shock - Tx: nitroprusside, diuretic, BB, ACEi +/- dobutamine/milrinone if hypotensive - Surgical Tx: REPAIR > replace (unless hypotensive) Mitral stenosis: - rumbling diastolic murmur with RHF symptoms - often noted in pregnancy, associated with Rheumatic Fever - Tx: BB, CCB --> if <1cm^2 or <1.5cm^2 with exercise limitation or gradient >5-10 or pregnant: valvotomy. *NOT a surgical candidate if there’s MVR. Tricuspid regurg: holosystolic murmurat LUSB that radiates to the liver Pulmonary regurg: decrescendo diastolic murmur at LSB that increases with inspiration, may present with parasternal heave, associated with Tetralogy of Fallot repair Prosthetic valve: if suspected dysfunction, go straight to TEE - choose bioprosthetic valve if patient has high bleeding risk (mechanical valves need AC) - mechanical mitral valve INR 2.5-3.5 (all other goal including aortic valve = 2-3) - all need 81mg ASA
Heart pressures: “nickels, quarters, dimes” RA --> RV --> PA --> wedge/LA: 5 --> 25/5 --> 25/10 --> 10mmHg
Myocardial disease
Heart failure with preserved ejection fraction: candesartan decreases hospitalization (not mortality) Myocarditis: elevated trops --> cardiogenic shock, arrhythmias --> Tx: supportive care + HF treatment Hypertrophic cardiomyopathy: Autosomal Dominant (AD), LVH + LAE with deep inverted T waves in V3-V6 - have carotid bisfiriens pulsus , murmur that increases with valsalva and decreases with squatting and prolonged handgrip - at risk patients 12-18yo: f/u TTE Q12-18 mo; >18yo, Q5 years - all HCM patients need genetic counseling - avoid strenuous exercises; Tx: BB/CCB +/- disopyramide --> surgical myomectomy/septal ablation --> fail/not candidate: ICD placement Restrictive cardiomyopathy: amyloid (neuro, ocular, liver symptoms), sarcoid (Dx: MRI with gadolinium), XRT, anthracycline, hemochromatosis (cardiomyopathy with transaminitis) Dilated cardiomyopathy: acute myocarditis, EtOH, cocaine/amphetamine (avoid BB; Tx with CCB), GCA Peripartum CM: LVEF 45% 1mo pre- to 5 mo post-delivery; Tx with early delivery and HF Tx (make sure to hold ACE/ARB/Statins until AFTER delivery given teratogenicity) Takotsubo: apical ballooning; Tx BB Heart transplant: - symptoms <1 year: rejection --> Dx with endomyo bx - symptoms > 1 year: vasculopathy --> Dx with angiography
Cardiac tumors: atrial myxoma needs to be surgically removed
Endocarditis
Endocarditis: - FROM JANE - Tx Abx 4-6 weeks - suspect abscess when there is increased PR interval/conduction delays Endocarditis prophylaxis: dental only (with gingival involvement) with Amoxicillin or Clindamycin for h/o cardiac transplant, prosthetic valve, or previous bacterial endocarditis
Vascular disease
Carotid artery disease: if pacemaker, LBBB or structural heart issues --> chemical nuclear perfusion scan Thoracic aortic aneurysm: - type A: repair vs - type B: monitor with TEE (as below) and Tx with BB, Nitroprusside - <3.5cm: Q3-5 year US *counsel against pregnancy if >4cm - root <4.5cm: Q1 year US - >4.5cm: Q6mo US - >5-5.5cm or >1cm/year: repair Abdominal aortic aneurysm: *screen male 65-75yo smoker with US - Dx acute aortic dissection with MRA or CT (NOT US); Tx with BB - Surgery if >5.5cm or >0.5cm/year or symptomatic; monitor Q6mo PAD: - ABI<0.9 - PAD - ABI>1.4 suggests DM or calcification = false normal --> get toe:brachial index - Tx: supervised exercise > Cilostazol (Cilostazol is CI in HF, EF <40%) SVC: associated with coarctation; facial/neck vessel plethora
Syncope
*be sure to r/o (1) exertional syncope from AS/HCM, (2) PE --> pulmonary HTN, (3) arrhythmia (no prodrome) Neurocardiogenic / vasovagal syncope: ECG only; can send home if it’s obvious Situational syncope: can occur after elderly person eats; can get tilt table testing if recurrent/high risk of injury Postural hypotension: associated with orthostatic secondary to hypovolemia, drugs or autonomic dysfunction (DM, Parkinsons plus); Dx: carotid massage
Preoperative consultation
*FYI: stop warfarin 5 days prior to surgery and bridge with Heparin after INR 1.5 only if at high risk (h/o clots, mechanical valve) --> resume AC within 24 hours *FYI: if recent PCI, delay elective procedure 4-6 weeks after BMS or 1 year after DES; if urgent procedure, continue DAPT throughout if within the minimum time limit. If beyond minimum time limit for BMS, but still within 1 year, hold Plavix 5 days before and continue ASA. *FYI: okay to go to surgery if BP <180/110 No testing required: >4METS, low risk Sx (endoscopy, superficial, breast, ambulatory procedure) Testing indicated: MI w/n 30 days, acute HF, arrhythmia, severe valve disease, vascular surgery
Lipid disorder = #1 risk factor for future MI
- goal: keep LDL <100 or <70 if CAD + other risk factor
Other
- Eisenmenger cyanosis is NOT improved with O2 supplementation (so don’t bother giving it to them) - Tamponade triad: (1) JVP, (2) distant heart sounds, (3) hypotension, ((4) tachycardia); will also have pulsus paradoxus (>8-10mmHg difference between inspiration and expiration), Kussmaul (increased CVP/JVD with inpsiration), right atrial collapse - Aortic atheroemboli: cholesterol embolus/Hollenhorst plaque (bright cholesterol in retinal artery) --> transient vision loss, digital gangrene, livedo reticularis or CVA/AKI following invasive coronary procedure; Dx: biopsy - Subclavian steal: UE PAD --> dizzy with arm use; Dx: bilateral UE BP’s (difference of 15mmHg) - a sudden rise in end tidal CO2 is the earliest indicator of ROSC during CPR
29 notes
·
View notes