#ivf embryo transfer
Explore tagged Tumblr posts
Text
youtube
Dr Arati R Rao on The day of your Embryo Transfer procedure
0 notes
Text

Frozen Blastocyst Transfer: Understanding Embryo Transfer Process at Indira IVF
Frozen Blastocyst Transfer: Blastocyst embryo transfer process in women infertility treatment. Understand the importance of IVF embryo transfer at Indira IVF. For more details, visit!
0 notes
Text
सरोगेसी यानी भ्रूण स्थानांतरण तकनीक (Embryo Transfer Technology) से हुआ देश के पहले मारवाड़ी घोड़े का जन्म
मारवाड़ी नस्ल के घोड़ों की संख्या में होगा इज़ाफा
देश में घोड़ों की संख्या में पिछले कुछ सालों में बहुत कमी आई है। इसीलिए वैज्ञानिक घोड़ों, खासकर देसी नस्ल के घोड़ों की संख्या बढ़ाने की दिशा में लगातार काम कर रहे हैं। इसी कड़ी में उन्हें भ्रूण स्थानांतरण तकनीक से एक बड़ी सफ़लता मिली है।

सरोगेसी यानी भ्रूण स्थानांतरण तकनीक (Embryo transfer technology) अच्छी नस्ल के जानवरों के संरक्षण के लिए एक वरदान बनकर आई है। अब इसका प्रयोग घोड़ों पर भी किया जा रहा है। देसी नस्ल के घोड़ों की संख्या पिछले कुछ सालों से लगातार कम होती जा रही है। ऐसे में उनके सरंक्षण के लिए वैज्ञानिक नई नई तकनीकों का इस्तेमाल कर रहे हैं।
वैज्ञानिकों ने बहुत ही ख़ास मारवाड़ी नस्ल के घोड़ों (Marwari Horse) की संख्या बढ़ाने के लिए एक सफ़ल प्रयोग किया। उन्होंने इंसानों की तरह ही घोड़ी में Embryo transfer technology यानी भ्रूण स्थानांतरण तकनीक का इस्तेमाल किया जिससे देश के पहले मारवाड़ी घोड़े का जन्म हुआ। इस तकनीक की सफलता ने भविष्य में घोड़ों की संख्या बढ़ाने के लिए एक नई राह दिखाई है।

सरोगेसी के बारे में तो आप सभी जानते ही हैं। जब कोई महिला गर्भधारण नहीं कर पाती है, तो उसके अंडों को दूसरी महिला के गर्भ में प्रत्यारोपित कर दिया जाता है। वो दूसरी महिला सरोगेट मदर कहलाती है। इसी तरह की तकनीक का इस्तेमाल अब घोड़ों की संख्या बढ़ाने के लिए किया जा रहा है। ICAR-राष्ट्रीय अश्व अनुसंधान संस्थान के बीकानेर स्थित इक्वाइन प्रोडक्शन कैंपस (Equine Production Campus) में पहली बार मारवाड़ी नस्ल की घोड़ी में भ्रूण स्था��ंरण तकनीक का प्रयोग किया गया।
यानी एक घोड़ी के एग्स को फर्टिलाइज़ करके सरोगेट मां (घोड़ी) में स्थानांतरित किया गया। इससे देश के पहले मारवाड़ी घोड़े के बच्चे का जन्म हुआ, जिसका नाम रखा गया ‘राज-प्रथमा’। इस तकनीक में ब्लास्टोसिस्ट चरण (गर्भाधान के 7.5 दिन बाद) में एक निषेचित भ्रूण यानी फर्टिलाइज़्ड एम्ब्रो को एक घोड़ी से लेकर सरोगेट मां में स्थानांतरित कर दिया गया।
और पढ़ें......
0 notes
Text
Well, the doctor confirmed what I knew two weeks ago. I'm not pregnant.
At least I can stop taking the damn meds that were making me sick for a day. Starting tomorrow it's daily shots to try for another egg harvest.
I don't really have much hope for this round either. Given just how unprofessional the doctors are, if there were any other ivf option less than three hours away I would do it. But after this round I'm calling it quits. And submitting a stack of complaints.
#Ivf#IVF in Japan#Unprofessional Japanese doctors#The doctor actually tried to argue that a sixty seven percent embryo transfer failure rate wasn't that bad compared to the rest of Japan#Kinda tells you how bad it is in Japan
6 notes
·
View notes
Text


By Dina Fine Maron
January 24, 2024
Scientists have cleared a significant hurdle in the years-long effort to save Africa’s northern white rhinoceros from extinction with the first-ever rhino pregnancy using in vitro fertilization.
The lab-assisted pregnancy, which researchers will announce today, involved implanting a southern white rhino embryo in a surrogate mother named Curra.
The advance provides the essential “proof of concept” that this strategy could help other rhinos, says Jan Stejskal of the BioRescue project, the international group of scientists leading this research.
Curra died just a couple months into her 16-month pregnancy from an unrelated bacterial infection, Stejskal says.
However, the successful embryo transfer and early stages of pregnancy pave the way for next applying the technique to the critically endangered northern white rhino.
The process was documented exclusively by National Geographic for an upcoming Explorer special currently slated to air in 2025 on Nat Geo and Disney+.
BioRescue expects to soon implant a northern white rhino embryo into a southern white rhino surrogate mother.
The two subspecies are similar enough, according to the researchers, that the embryo will be likely to develop.
Eventually, this approach may also help other critically endangered rhinos, including the Asian Javan rhinoceros and the Sumatran rhinoceros, which each now number under 100 individuals, Stejskal says.
But the northern white rhino’s current situation is the most pressing by far.
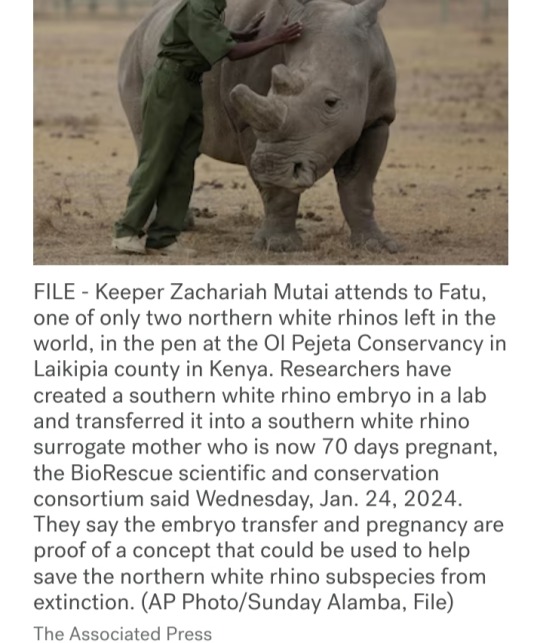
There are no males left, and the only two remaining animals are both elderly females that live under armed guard on a reserve in a 700-acre enclosure in Kenya called Ol Pejeta Conservancy.
The boxy-jawed animals once roamed across central Africa, but in recent decades, their numbers have plummeted due to the overwhelming international demand for their horn, a substance used for unproved medicinal applications and carvings.
Made from the same substance as fingernails, rhino horn is in demand from all species, yet the northern white rhino has been particularly hard-hit.
"These rhinos look prehistoric, and they had survived for millions of years, but they couldn’t survive us,” says Ami Vitale, a National Geographic Explorer and photographer who has been documenting scientists’ efforts to help the animals since 2009.
“If there is some hope of recovery within the northern white rhino gene pool — even though it’s a substantially smaller sample of what there was — we haven’t lost them,” says conservation ecologist David Balfour, who chairs the International Union for the Conservation of Nature’s African rhino specialist group.
Blueprints for rhino babies

To stave off the animal’s disappearance, BioRescue has used preserved sperm from northern white rhinos and eggs removed from the younger of the two remaining females.
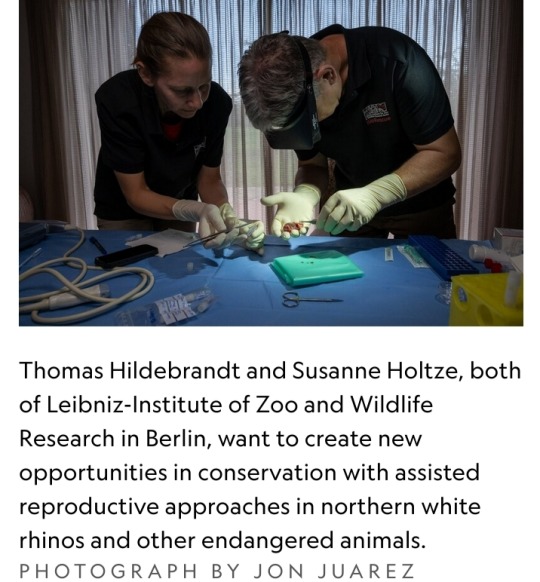
So far, they’ve created about 30 preserved embryos, says Thomas Hildebrandt, the head scientist of BioRescue and an expert in wildlife reproduction based at the Leibniz-Institute of Zoo and Wildlife Research in Berlin.
Eventually, the team plans to reintroduce northern white rhinos into the wild within their range countries.
“That’d be fantastic, but really, really far from now—decades from now,” says Stejskal.
Worldwide, there are five species of rhinoceros, and many are in trouble.
Across all of Africa, there are now only about 23,000 of the animals, and almost 17,000 of them are southern whites.
Then there are more than 6,000 black rhinos, which are slightly smaller animals whose three subspecies are critically endangered.
In Asia, beyond the critically endangered Javan and Sumatran rhinos, there’s also the greater one-horned rhino, whose numbers are increasing and currently are estimated to be around 2,000.
The BioRescue effort has experienced many setbacks, and even though the team now has frozen embryos, the clock is ticking.
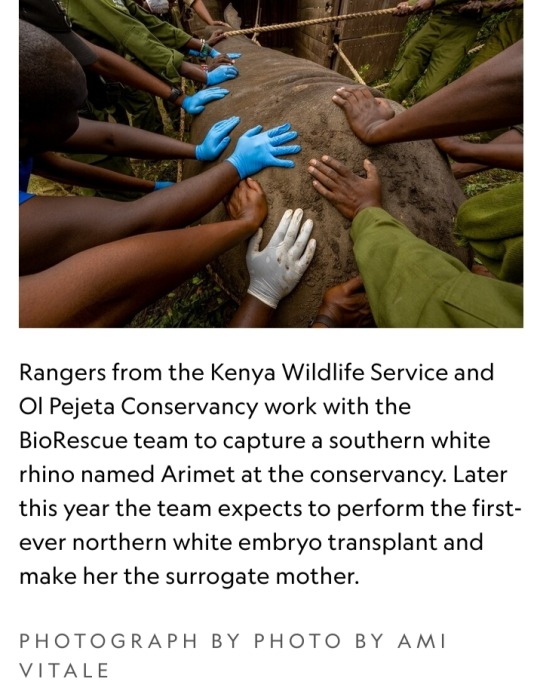
The researchers intend to use southern white rhinos as surrogate moms for the northern white rhino embryos.
However, scientists want any northern white rhino calves to meet and learn from others of their kind, which means they need to be born before the two remaining females die.
“These animals learn behaviors — they don’t have them genetically hard-wired,” says Balfour, who’s not involved with the BioRescue work.
But birthing new animals in time will be a challenge.
“We’re really skating on the edge of what’s possible,” he says, “but it’s worth trying.”
Najin, the older female, will be 35 this year, and Fatu will be 24.
The animals, which were born in a zoo in the Czech Republic, are expected to live to about 40, says Stejskal, who also serves as director of international projects at the Safari Park Dvůr Králové, the zoo where the animals lived until they were brought to Kenya in 2009.
Impregnating a rhino
The next phase of BioRescue’s plan involves implanting one of their limited number of northern white rhino embryos into a southern white rhino surrogate mother — which the group plans to do within the next six months, Stejskal says.
They’ve identified the next surrogate mother and set up precautions to protect her from bacterial infections, including a new enclosure and protocols about disinfecting workers’ boots.
But now, they must wait until the female rhino is in estrus — the period when the animal is ready to mate — to implant the egg.
To identify that prime fertile time, they can’t readily perform regular ultrasounds at the conservancy as they might do in a zoo.
Instead, they have enlisted a rhino bull that has been sterilized to act as a “teaser” for the female, Hildebrandt says, adding that they must wait a few months to make sure that their recently sterilized male is truly free of residual sperm.
Once the animals are brought together, their couplings will alert conservancy staff that the timing is right for reproductive success.
The sex act is also important because it sets off an essential chain of events in the female’s body that boosts the chances of success when they surgically implant the embryo about a week later.
"There’s little chance the conservancy staff will miss the act. White rhinos typically mate for 90 minutes," Hildebrandt says.
What’s more, while mounted on the females, the males often use their temporary height to reach tasty plant snacks that are generally out of reach.
Boosting genetic diversity
With so few northern white rhinos left, their genetic viability may seem uncertain.
But the BioRescue team points to southern white rhinos, whose numbers likely dropped to less than 100, and perhaps even as few as 20, due to hunting in the late 1800s.
Government protections and intense conservation strategies allowed them to bounce back, and now there are almost 17,000.
“They have sufficient diversity to cope with a wide range of conditions,” says Balfour.
Researchers don’t know exactly how many southern white rhinos existed a century ago, he says, but it’s clear that the animals came back from an incredibly low population count and that they now appear healthy.
Beyond their small collection of embryos, the BioRescue team hopes to expand the northern white rhino’s gene pool by drawing from an unconventional source — skin cells extracted from preserved tissue samples that are currently stored at zoos.
They aim to use stem cell techniques to reengineer those cells and develop them into sex cells, building off similar work in lab mice.
According to their plan, those lab-engineered sex cells would then be combined with natural sperm and eggs to make embryos, and from there, the embryos would be implanted into southern white rhino surrogate mothers.
Such stem cell reprogramming work has previously led to healthy offspring in lab mice, Hildebrandt says, but rhinos aren’t as well-studied and understood as mice, making this work significantly challenging.
A global effort
The northern white rhino revitalization venture has cost millions of dollars, supported by a range of public and private donors, including the German Federal Ministry of Education and Research.
Other partners on the effort include the Leibniz Institute for Zoo and Wildlife Research, the Czech Republic’s Safari Park, Kenya Wildlife Service, Ol Pejeta Conservancy, and also Katsuhiko Hayashi, a professor of genome biology at Osaka University in Japan who conducted the mouse stem cell research.
Building upon Hayashi’s stem cell techniques could ultimately bring the northern white rhino gene pool up to 12 animals — including eggs from eight females and the semen of four bulls, according to Stejskal.
An alternative approach to making more babies, like crossbreeding northern and southern white rhinos, would mean the resulting calves wouldn’t be genetically pure northern white rhinos, Hildebrandt notes.
The two subspecies look quite similar, but the northern version has subtle physical differences, including hairier ears and feet that are better suited to its swampy habitat.
The two animals also have different genes that may provide disease resiliency or other benefits, Hildebrandt says.
There are unknown potential differences in behavior and ecological impact when populating the area with southern white rhinos or cross-bred animals.
"The northern white rhino is on the brink of extinction really only due to human greed,” Stejskal says.
“We are in a situation where saving them is at our fingertips, so I think we have a responsibility to try.”
🩶🦏🩶
#northern white rhinoceros#rhino embryo transfer#in vitro fertilization#IVF#southern white rhinoceros#critically endangered animals#National Geographic#BioRescue#rhino horn#International Union for the Conservation of Nature#African rhino specialist group#Thomas Hildebrandt#German Federal Ministry of Education and Research#Leibniz Institute for Zoo and Wildlife Research#Kenya Wildlife Service#Ol Pejeta Conservancy#Katsuhiko Hayashi#genome biology#IVF rhino pregnancy
10 notes
·
View notes
Text
youtube
New Artist Fertility Journey Vlog is posted. I talk about prepping for my Frozen Embryo Transfer and the results.
9 notes
·
View notes
Text
Gay men and the wealthy are no longer content to exploit one woman now exploiting two at the same is becoming trendy
Why have one baby when you can have 2? People are paying $500,000 to hire 2 surrogates at once and have 'twiblings'
By Kelsey Vlamis Jul 16, 2024, 3:04 PM EDT
Some people are hiring two surrogates at the same time to carry their babies.
Concurrent surrogacy can be complicated and costly, with prices reaching up to $500,000 or more.
Many people who do it are in their 40s and trying to build out their family quickly.
Bill Houghton still vividly remembers the moment he met his son.
He was sitting in the hospital waiting room, right outside the birthing room, when a nurse appeared carrying a little green bundle.
"I just held him in my arms and just started crying. It was so overwhelming. My husband was like, 'Oh my God, I can't believe that this is it. We're a family,'" Houghton told Business Insider. "This is my son."
Just one week later, Houghton and his husband would have the same experience all over again when their second child, another son, was delivered.
"And it has been like that ever since," he said. "To this day, I still look at them and I think, 'Oh my God, these are my sons.' My father had sons. I never thought that I would have a son."
Houghton and his husband opted to become parents via concurrent surrogacy — a process in which two surrogates are hired to carry two babies at the same, or overlapping, time.
The resulting children can be born anywhere from one week apart, like Houghton's, to nine months apart, and have been referred to by some people in the industry as "tandem siblings" or "twiblings."
Surrogacy agencies told BI that concurrent surrogacy journeys are not uncommon, with some saying it's a rising trend in a growing industry that was valued at $14 billion in 2022 by Global Market Insights and has attracted the investments of private equity firms.
All kinds of people — couples or singles, straight or gay, young or old — have opted to build out their family two at a time via concurrent surrogacy. But there is one thing that most parents of twiblings have in common: the ability to afford them.
While Houghton hired surrogates abroad, couples who choose to go through US-based agencies can easily spend $300,000 to half a million dollars or more on concurrent surrogates, according to five surrogacy agencies that spoke to BI.
"It is a luxury, absolutely," Brooke Kimbrough, cofounder and CEO of Roots Surrogacy, told BI. "Most American families don't have $200,000 in cash to go through surrogacy generally, and then $400,000-plus in cash to be able to go through that twice at the same time."
Still, the use of concurrent surrogates could grow as surrogacy generally grows in the US, in part because celebrities like Kim Kardashian and Chrissy Teigen have started opening up about using surrogates, as well as depictions in film and TV that have made the practice more mainstream. Teigen was even pregnant at the same time as her surrogate.
Surrogacy is also becoming increasingly relevant as more and more people are opting to have kids and start building their families later in life.

Chrissy Teigen and John Legend have opened up about using a surrogate. Dimitrios Kambouris/Getty Images for Sports Illustrated Swimsuit
Concurrent surrogacy can help build a family quickly
Concurrent journeys typically look like regular surrogacy journeys, just times two. Gestational surrogacy, when IVF is used to place a fertilized embryo into a surrogate, is the most common form of surrogacy in the US today. Parents can use their own egg and sperm or that of donors.
Like many gay couples, Houghton and his husband each used their sperm for one of the babies, as well as the same egg donor, so their sons are technically half brothers.
While there has been increased awareness around what some call "social surrogacy" — using a surrogate when it's not medically or biologically necessary — the majority of people who conceive via surrogacy do so because they have to.
"Typically, when people come to us, they've been through a lot. This is not their plan A, it's often not plan B, maybe it's plan C," Kim Bergman, a psychologist and senior partner at Growing Generations, told BI. "They've had a lot of disappointment, and they've had a lot of trials and tribulations."
Many hopeful parents are in their 40s and are simply eager to build their families, the agencies said. A surrogacy journey can easily take one and a half to two years, so for intended parents who know they want multiple kids, concurrent surrogates can be appealing.
Certainly, some people who opt for concurrent surrogates do not fit the definition of medically necessary, at least according to the standards laid out by the American Society for Reproductive Medicine (ASRM).
Some people have mental health reasons or a fear of giving birth. Others are actors or brain surgeons who spend 12 hours a day on their feet and who can't get pregnant and continue to do their jobs. All the surrogacy agencies BI spoke with said it's essentially never the case that someone opts for surrogacy simply for vanity reasons.
David Sher, founder and CEO of Elite IVF, told BI they've helped coordinate surrogates for celebrities, politicians, and people in demanding careers like finance or tech. He said he currently has a client who serves on the cabinet of a Western country and is trying to have a baby via surrogate in part due to her demanding schedule.
Sher said he thinks concurrent surrogacy has long been an option for intended parents but that there does seem to be an uptick in people who are opting to do it.
Part of the reason for that could be because fewer and fewer agencies are willing to do double embryo transfers, which were previously more common and could result in a twin pregnancy. The ASRM recommends against them, as twin pregnancies come with heightened risks for both the surrogate and the babies. So concurrent surrogacy is a safer option for intended parents who want to have two kids at the same time or in close succession.
Costly and complicated
Though it's viewed as a safer option, concurrent surrogacy is controversial. The ASRM guidelines actually recommend against concurrent surrogacy, as well as against social, or not medically necessary, surrogacy. But all five surrogacy agencies that BI spoke to will facilitate concurrent surrogacies.
The agencies said they've seen many concurrent surrogacy journeys be successful and that a lot of care and prior planning goes into making them happen.
"It's not taken lightly," Bergman said, adding that concurrent journeys are rarely chosen by 30-year-olds who have plenty of time to build their families, though that does occasionally happen.
Surrogacy, in general, is expensive — commonly ranging from $150,000 to $250,000 for one child. The costs go toward surrogate compensation, agency fees, legal fees for contracts, and clinical bills.
The agencies BI spoke with said a concurrent surrogacy journey would essentially cost twice that. Meaning there's no two-for-one special.
But cost isn't the only factor to consider. Perhaps the primary drawback to pursuing concurrent surrogacy (that is, besides the high price tag) is the logistics of it.
All the agencies emphasized that concurrent surrogacy should only be pursued with full transparency and the fully informed consent of every person involved. That means matching intended parents to surrogates who are fully aware and OK with the fact that they will not be the only surrogate.

Gestational surrogacy, in which a fertilized embryo is implanted in a surrogate, is most common in the US. Jay L. Clendenin/for The Washington Post/Getty Images
There's also tons of planning and talking through hypotheticals. Are the surrogates based in the same area? Can the parents attend both births? Are we staggering expected delivery times enough? What's the plan if one surrogate gets pregnant on the first try but the other doesn't?
There's also a psychological aspect. Will both surrogates feel fully supported? How will one feel if she doesn't get pregnant right away and the other does?
"All of these conversations are front-loaded. Anytime in the conversation, the surrogate can say, 'I'm not comfortable doing this,'" Bergman said, adding that sometimes, after thinking through the logistics, some parents will change their minds and plan to space the deliveries out further than they initially wanted, like to six or nine months.
Most agencies recommended staggering the planned deliveries by at least three months. But at the end of the day, parents need to be ready for the timeline to not go exactly as planned.
Houghton and his husband had actually planned to have their babies six weeks apart, but when one of the babies was born five weeks premature, they ended up with birthdays one week apart.
Concurrent surrogacy may not be for everyone — even if you can afford it
Although the cost of concurrent surrogacy makes it prohibitive for most people, that could change in the future as more and more companies expand their fertility benefits.
There are also more nonprofits popping up that will provide grants or partial funds to people who want to build their families via surrogacy but may not have the means to.
Jarret Zafran, founder and executive director at Brownstone Surrogacy, told BI that it's not necessarily only the ultrawealthy who pursue concurrent surrogacy. He said he currently has clients who are lifelong educators on the older side who are getting ready to start the surrogacy process. They recently asked about what it would look like for them to do a concurrent journey.
"I guess it is still a luxury in the sense that most Americans would not even be in a financial position to afford it the first time," Zafran, who also had a child with his husband through surrogacy, said. "But for them, this is not a frivolous decision, and they're scraping together every single little penny that they have, all of their savings, their retirement funds, and I get it."
By using surrogates abroad over a decade ago, Houghton and his husband, who are based in Spain, spent much less on their concurrent surrogates than they would have in the US. But he's still not totally sure why they chose to do concurrent journeys rather than space the children out a bit more.
"We just liked the idea of having two kids that were about the same age that would sort of grow up together," he said, adding, "I didn't realize at the time the challenges that would come with having two kids."
In reality, he said having the two boys grow up so close together in age, not twins but in the same class in school, ended up leading to a lot of conflict and constant competition as they were growing up. He said it has gotten better now that the boys are facing their teen years and developing their own identities.
Still, if he could do it over again, he thinks he would stagger them more.
"They're unbelievable young men, and I'm so proud of everything about them," he said. "But having the two together has been a challenge."
Have a news tip or a story to share about concurrent surrogacy? Contact this reporter at [email protected].
If a brain surgeon or politician can't do their job while pregnant have they thought about how kids in general will impact their job? What if their kid wakes them up the night before surgery because they got of had a nightmare? Are they counting on a reliable spouse or a nanny to take care to the unpleasant parts of parenting.
Finally at the very end of the article they address how being born so close together impacts kids. We're they really surprised that there was a lot of competition? And they article just touched on how one of the twins was born 5 weeks premature. That means at one week old the dudes in charge of its care were focused on its twibling. Considering that surrogacy pregnancies are more likely to have complications do the parents consider how they will care for one baby while another baby is in the hospital longer than expected?
#anti surrogacy#Twibling#Surrogacy exploits women#Twibling Surrogacy exploits two women at the same time#Babies are not commodities#If people want to build their families quickly why can't they just have one then adopt one?#Half a million dollars spent on having bio offspring when so many kids are up for adoption#concurrent surrogacy#tandem siblings#Surrogacy is an industry that was valued at $14 billion in 2022 by Global Market insights#The dude in this article choose foreign surrogates both times#Using foreign surrogates leads to the human trafficking of infants#Being in a same sex relationship is not infertility#Waiting too long to have kids is not infertility#social surrogacy" — using a surrogate when it's not medically or biologically necessary#Surrogacy is never necessary it just means the reproductive purchasers never considered adoption#American Society for Reproductive Medicine (ASRM)#If people have jobs too demanding to go through pregnancy how they hell are they going to raise the kid?#fewer and fewer agencies are willing to do double embryo transfers which were previously more common and could result in twin pregnancy#All the questions about feelings were about how will the reproductive purchasers balance two pregnancies at the same time#Not about how being born so close together will impact two half siblings#Brownstone Surrogacy#Elite IVF#Roots Surrogacy#Growing Generations
5 notes
·
View notes
Text
What is IVF?
In recent decades, advancements in medical science have revolutionized the field of reproductive medicine, providing hope and opportunities for couples struggling with infertility. One such groundbreaking technique is In Vitro Fertilization (IVF). In this blog post, we will delve into the intricacies of IVF treatment, exploring what it is, how it works, and the potential it holds for those seeking to build a family.
What is IVF?
In Vitro Fertilization, commonly known as IVF, is a fertility treatment that involves the fertilization of an egg with sperm outside the human body. The process begins by extracting eggs from a woman's ovaries and fertilizing them with sperm in a laboratory dish. Once fertilization occurs, the resulting embryos are then implanted in the woman's uterus with the hope of establishing a successful pregnancy.
Understanding the IVF Process
Ovulation Induction: The first step in IVF involves stimulating the ovaries to produce multiple eggs. Fertility medications are administered to enhance egg production, monitored through ultrasound and blood tests.
Egg Retrieval: Once the eggs are mature, a minor surgical procedure known as egg retrieval is performed. A thin needle is inserted through the vaginal wall to collect the eggs from the ovaries.
Fertilization: The collected eggs are then combined with sperm in a controlled environment, allowing fertilization to occur. This step is closely monitored to ensure the formation of healthy embryos.
Embryo Culture: The fertilized eggs, now embryos, are cultured and monitored for several days. The healthcare team assesses their quality before selecting the most viable embryos for transfer.
Embryo Transfer: In the final step, one or more selected embryos are transferred into the woman's uterus. This is a relatively simple and painless procedure that aims to establish a successful pregnancy.
Success Rates and Considerations
IVF success rates vary depending on several factors, including the age of the woman, the cause of infertility, and the quality of the embryos. While some individuals achieve pregnancy in the first cycle, others may require multiple attempts. It's essential to approach IVF with realistic expectations and to consult with healthcare professionals to understand individual circumstances.
Challenges and Emotional Aspects
Embarking on an IVF journey can be emotionally challenging for couples. The process involves physical, emotional, and financial commitments, and individuals may experience a range of emotions, from hope and excitement to disappointment and stress. Support from loved ones and mental health professionals can play a crucial role in helping individuals navigate these challenges.
Conclusion
In Vitro Fertilization has emerged as a beacon of hope for many couples facing infertility challenges.
Schedule a Consultation with Dr. Sonal Lathi Today If you are considering IVF treatment, Dr. Sonal Lathi is the perfect choice for you. She is a leading expert in IVF, and she is committed to helping couples achieve their parenthood dreams.
#IVF#fertility treatment#reproductive health#in vitro fertilization#family building#infertility#assisted reproductive technology#egg retrieval#embryo transfer#pregnancy journey#parenting hope#medical advancements#healthcare#women's health#parenthood#emotional wellness#support network#family building options#fertility awareness#IVF success#embryo quality#hopeful beginnings#modern medicine#couples' journey#future of reproductive medicine#life through IVF
2 notes
·
View notes
Text
IVF Treatment: Pros and Cons of Multiple Embryo Transfer
IVF (in vitro fertilization) is a form of assisted reproductive technology that involves retrieving eggs from a woman's ovaries and fertilizing them with sperm in a laboratory. The fertilized eggs (embryos) are then transferred to the woman's uterus to establish a pregnancy. Multiple embryo transfer is a technique used in IVF where more than one embryo is transferred to increase the chances of pregnancy. In this blog, we will discuss the pros and cons of multiple embryo transfer in IVF treatment.
Multiple embryo transfer is a complex issue and requires a thorough understanding of the risks and benefits. As such, it is important for couples considering IVF to have an open discussion with their fertility specialist about the pros and cons of multiple embryo transfer. This will help them make an informed decision about the number of embryos to transfer during IVF treatment.
What is IVF Treatment?
IVF is a fertility treatment in which eggs are extracted from a woman's ovaries and fertilized with sperm in a laboratory. The resulting embryos are then transferred into the woman's uterus in hopes of achieving a pregnancy. IVF treatment is often recommended for couples who have been trying to conceive for a long time with no success, have a history of infertility, or have certain medical conditions that make it difficult to conceive naturally.
Multiple Embryo Transfer in IVF Treatment
Multiple embryo transfer in IVF treatment refers to the transfer of more than one embryo into the woman's uterus during the IVF cycle. This is usually done to increase the chances of a successful pregnancy, especially for couples who have had unsuccessful IVF cycles in the past. However, the decision to transfer multiple embryos should be carefully considered, as it can lead to multiple pregnancies, which come with their own set of risks.
The Pros of Multiple Embryo Transfer:
Increased Chances of Pregnancy
One of the main advantages of multiple embryo transfer in IVF treatment is the increased chances of achieving a pregnancy. Since not all embryos that are transferred will result in a successful pregnancy, transferring more embryos increases the chances of at least one embryo implanting and developing into a fetus. This is particularly beneficial for couples who have had unsuccessful IVF cycles in the past and are looking to increase their chances of success.
Reduced Need for Repeat Cycles
Another advantage of multiple embryo transfer is that it reduces the need for repeat IVF cycles. Since transferring more embryos increases the chances of achieving a pregnancy, couples are less likely to need to undergo additional IVF cycles, which can be time-consuming, emotionally draining, and expensive.
No need for freezing and storage
When only one embryo is transferred during IVF treatment, any additional embryos are frozen and stored for future use. This can be expensive and may not be feasible for some couples. With multiple embryo transfer, there is no need for freezing and storage, which can simplify the process and reduce costs.
Reduced cost and time
Another advantage of multiple embryo transfer is that it can reduce the cost and time of IVF treatment. Since multiple embryos are transferred, there is no need for repeated IVF cycles, which can be expensive and time-consuming. Additionally, the cost of IVF treatment can be a significant barrier for some couples, and multiple embryo transfer can be a cost-effective option.
Cost-Effective
Transferring multiple embryos can also be cost-effective for couples undergoing IVF treatment. Since each cycle of IVF can be expensive, transferring more embryos in a single cycle can reduce the overall cost of treatment by reducing the need for repeat cycles.
The Cons of Multiple Embryo Transfer:
Higher Risk of Multiple Pregnancy
One of the main disadvantages of multiple embryo transfer is the higher risk of multiple pregnancy. Multiple pregnancy occurs when more than one fetus develops in the uterus, and it is a major risk associated with IVF treatment. Multiple pregnancies can increase the risk of complications such as premature birth, low birth weight, and other health problems for both the mother and the babies.
Increased Risk of Premature Birth and Low Birth Weight
Multiple pregnancy also increases the risk of premature birth and low birth weight. Premature birth can result in a range of health problems for the babies, such as developmental delays, vision and hearing problems, and respiratory distress syndrome. Low birth weight, which is common in multiple pregnancies, can also lead to a range of health problems, including developmental delays, infections, and neurological problems.
Emotional and Physical Stress
Multiple embryo transfer can also be emotionally and physically stressful for couples undergoing IVF treatment. The process can be emotionally draining, and the uncertainty of whether or not the transfer will be successful can take a toll on the mental health of both partners. Physically, multiple embryo transfer can lead to discomfort, bloating, and other side effects that can make the IVF process even more challenging.
The Ethical Debate Surrounding Multiple Embryo Transfer
The use of multiple embryo transfer in IVF treatment has sparked a heated ethical debate in the medical community. While the practice can increase the chances of a successful pregnancy, it also carries significant risks for both the mother and the babies. Additionally, transferring multiple embryos can lead to unused embryos, which raises questions about what should be done with these embryos.
Alternatives to Multiple Embryo Transfer
For couples who are concerned about the risks of multiple embryo transfer, there are alternatives available. One option is to transfer a single embryo during IVF treatment, which can reduce the risk of multiple pregnancy while still providing a chance for a successful pregnancy. Another option is to freeze unused embryos for future use, which can reduce the need for repeat IVF cycles and increase the chances of success in the future.
Ethical concerns
Multiple embryo transfer raises ethical concerns, particularly around the number of embryos to transfer. Transferring too many embryos can increase the risk of multiple pregnancies, while transferring too few embryos can reduce the chances of pregnancy. Additionally, couples may be faced with difficult decisions around selective reduction, which involves reducing the number of fetuses in a multiple pregnancy to improve the chances of a healthy pregnancy.
Mitigating the Risks of Multiple Embryo Transfer:
A. Elective single embryo transfer (eSET)
One way to mitigate the risks of multiple embryo transfer is to consider elective single embryo transfer (eSET). eSET involves transferring only one embryo during IVF treatment, which can reduce the risk of multiple pregnancies. eSET is particularly recommended for couples who have a good chance of success with IVF treatment and who are at risk of multiple pregnancies.
B. Embryo screening
Another way to mitigate the risks of multiple embryo transfer is to consider embryo screening. Embryo screening involves testing the embryos for genetic abnormalities before transfer. This can help identify the healthiest embryos for transfer and reduce the risk of multiple pregnancies.
C. Counselling and support
Couples considering multiple embryo transfer should receive counselling and support to help them make an informed decision. This includes discussing the risks and benefits of multiple embryo transfer, as well as the emotional and financial implications of caring for multiple babies. Couples may also benefit from support groups and counselling services to help them cope with the stress and emotional challenges of IVF treatment.
https://healthtrip.com/
#https://healthtrip.com/#https://healthtrip.com/blog/ivf-treatment-pros-cons-multiple-embryo-transfer
2 notes
·
View notes
Text
Top 5 Misconceptions About IVF Treatments: What You Need to Know

In today's world, in vitro fertilization (IVF) is a popular fertility treatment that has helped millions of couples and individuals realize their dreams of parenthood. However, with its growing popularity comes a plethora of misconceptions and myths that often cloud the understanding of this advanced reproductive technology. For those considering IVF, it's essential to separate fact from fiction. In this article, we’ll debunk the top 5 misconceptions about IVF treatments and give you a clearer picture of what to expect. Whether you’re just starting your fertility journey or exploring your options, Yellow IVF is here to guide you.
Misconception 1: IVF Guarantees Pregnancy
One of the most common misconceptions is that IVF guarantees a successful pregnancy. While IVF has revolutionized fertility treatments and improved success rates significantly, it does not guarantee pregnancy. IVF is a complex process that involves several stages, including ovarian stimulation, egg retrieval, fertilization, and embryo transfer. Each stage can pose potential challenges that may impact the outcome.
The Truth
IVF success rates vary based on several factors, including a woman's age, the cause of infertility, and the quality of the embryos. While IVF increases the chances of pregnancy, it’s important to remember that no fertility treatment can guarantee success. According to studies, women under 35 have a success rate of around 50%, while women over 40 may experience lower success rates. However, each case is unique, and IVF can be customized to improve the chances of a successful pregnancy.
Misconception 2: IVF Is Only for Older Women
Another misconception is that IVF is only a solution for older women who are struggling to conceive naturally. While age is a significant factor in fertility, IVF is not exclusive to women over 35. In fact, IVF can be a viable solution for younger women and even men who are experiencing infertility issues, regardless of their age.
The Truth
Infertility can affect anyone, and IVF is not limited by age. Younger women with conditions such as blocked fallopian tubes, endometriosis, or polycystic ovary syndrome (PCOS) may benefit from IVF. Additionally, IVF can be used by men with low sperm count or motility issues. In many cases, couples or individuals choose IVF when other fertility treatments, such as medications or intrauterine insemination (IUI), have not been successful.
Misconception 3: IVF Is Too Expensive for Most People
Cost is often cited as a reason why people shy away from considering IVF. Many assume that IVF treatments are prohibitively expensive and out of reach for the average person. While IVF can be costly, there are several options available to make it more affordable.
The Truth
While IVF can be a significant financial investment, there are many ways to manage the cost. Clinics like Yellow IVF offer flexible payment plans, financing options, and insurance coverage that may help offset the expenses. Additionally, the cost of IVF can vary based on the clinic, location, and the specific treatments required. Some couples also explore grants, scholarships, and crowdfunding as potential resources to support their fertility journey.
It’s essential to discuss all your options with your fertility clinic to find a plan that works for you. With the right financial guidance, IVF can be accessible to many people.
Misconception 4: IVF Increases the Chances of Multiple Births
Many people believe that IVF always results in twins or triplets. This misconception likely stems from the early days of IVF when multiple embryos were often transferred to increase the chances of pregnancy. However, modern advancements in IVF technology have changed the approach to embryo transfer, significantly reducing the chances of multiple births.
The Truth
Advances in embryo selection and transfer techniques have allowed fertility specialists to improve the chances of a successful pregnancy with the transfer of a single embryo. Single embryo transfer (SET) has become a common practice, reducing the risk of multiple births. While there is still a possibility of twins or triplets, the goal of IVF today is to achieve a healthy singleton pregnancy.
At Yellow IVF, we prioritize the health and safety of both the mother and baby, offering personalized treatment plans that minimize the risk of complications associated with multiple births.
Misconception 5: IVF Is Only for Couples
Another widespread misconception is that IVF is only for couples experiencing infertility. However, IVF is also a viable option for single women, LGBTQ+ individuals, and couples who are looking to build a family. IVF has expanded beyond traditional family structures to accommodate various fertility needs.
The Truth
IVF can be used by a wide range of individuals, including single women who want to preserve their fertility, same-sex couples who require donor eggs or sperm, and individuals with medical conditions that affect their fertility. Yellow IVF offers a welcoming and inclusive environment for all patients, providing customized treatment plans that align with each individual's family-building goals.
Whether you’re a single woman looking to freeze your eggs or a same-sex couple seeking fertility assistance, IVF can provide the necessary tools and support for starting or growing your family.
Conclusion
IVF is a powerful and advanced fertility treatment that has helped countless individuals and couples achieve their dreams of parenthood. While there are many misconceptions surrounding IVF, it’s important to educate yourself on the facts. At Yellow IVF, we strive to provide compassionate care and expert guidance to help you navigate your fertility journey. By dispelling common myths and understanding the realities of IVF, you can make informed decisions and feel confident in your path to parenthood.
If you’re considering IVF or looking for more information, contact Yellow IVF today to schedule a consultation with our experienced fertility specialists. We're here to support you every step of the way.
Content Source - https://yellowivf.blogspot.com/2025/02/top-5-misconceptions-about-ivf.html
#IVF myths and facts#Misconceptions about IVF treatments#IVF success rate#Is IVF expensive?#Fertility treatments for couples#IVF single embryo transfer#IVF for single women#IVF for LGBTQ+ couples#IVF fertility treatment guide#IVF pregnancy myths#Yellow IVF clinic#IVF for infertility issues#IVF financial options#IVF multiple birth risks#Yellow IVF
0 notes
Text
Embryo Freezing & Transfer Procedure for In Vitro Fertilization –Best Fertility Center in Bargarh, Odisha

In vitro fertilization (IVF) has revolutionized fertility treatments, offering hope to couples struggling to conceive. Among the many breakthroughs in assisted reproductive technologies, embryo freezing and transfer procedures have emerged as pivotal steps to maximize success rates and provide flexibility. At the Advanced Fertility Center in Bargarh, Odisha, we are proud to provide cutting-edge solutions that prioritize patient care and success.
What is Embryo Freezing?
Embryo freezing, or cryopreservation, involves preserving embryos at sub-zero temperatures for future use. After a successful IVF cycle, any healthy embryos that are not immediately transferred to the uterus can be frozen. These embryos can then be thawed and transferred in subsequent cycles, eliminating the need for repeated egg retrieval procedures.
Benefits of Embryo Freezing:
Increased Flexibility: Couples can choose the best timing for embryo transfer, considering physical and emotional readiness.
Higher Success Rates: Frozen embryos have shown comparable or even better implantation rates compared to fresh transfers.
Reduced Costs: Using frozen embryos for subsequent cycles is more cost-effective than undergoing a new IVF cycle.
Fertility Preservation: Women undergoing treatments like chemotherapy can freeze embryos for future use.
The Embryo Freezing Process
Ovarian Stimulation: Women undergo hormonal treatments to stimulate the ovaries to produce multiple eggs.
Egg Retrieval: Mature eggs are retrieved in a minimally invasive procedure.
Fertilization: The eggs are fertilized with sperm in the laboratory to create embryos.
Embryo Assessment: The resulting embryos are monitored for quality and development.
Cryopreservation: Viable embryos are frozen using a process called vitrification, which prevents ice crystal formation and ensures high survival rates.
Embryo Transfer Procedure
The embryo transfer is a straightforward and painless procedure that involves placing the embryo into the uterus. Here’s how it works:
Preparation: The uterine lining is prepared using hormonal treatments to ensure it is receptive to the embryo.
Thawing the Embryo: Frozen embryos are carefully thawed, with survival rates exceeding 90% in most cases.
Transfer: Using a thin catheter, the embryo is gently placed into the uterus under ultrasound guidance. The process typically takes only a few minutes.
Post-Transfer Care: Patients are advised to rest and avoid strenuous activities for a short period. Pregnancy tests are conducted after two weeks to confirm implantation.
Why Choose IVF Advanced Fertility Center in Bargarh, Odisha?
At our center, we are committed to providing personalized care, leveraging state-of-the-art technology, and ensuring emotional support throughout the journey. Here are some reasons why couples choose us:
Experienced Team: Our fertility specialists and embryologists have years of expertise in handling complex cases.
Advanced Technology: We use the latest cryopreservation techniques, ensuring high embryo survival rates.
Comprehensive Care: From consultation to post-transfer support, we are with you every step of the way.
Affordable Treatments: Our center offers world-class fertility services at cost-effective rates.
Conclusion
Embryo freezing and transfer procedures have transformed the landscape of fertility treatments, offering hope and flexibility to countless couples. At the IVF Advanced Fertility Center in Bargarh, Odisha, we strive to make parenthood dreams a reality with compassionate care and advanced technology.
If you’re considering IVF or want to learn more about embryo freezing and transfer, contact us today. Let us help you take the next step in your fertility journey.
#IVF Advanced Fertility Center#ivf hospital#ivf treatment#ivfsuccess#ivf center in odisha#ivfcenter#test tube baby treatment#ivf#test tube center#Embryo Transfer Procedure#Embryo Freezing Process#Embryo freezing#cryopreservation
0 notes
Text

Frozen Blastocyst Transfer: Understanding IVF Embryo Transfer at Indira IVF
Frozen Blastocyst Transfer: Understand blastocyst and it's process in women infertiliy. Learn about importance of IVF embryo transfer at Indira IVF.
0 notes
Text
SCI IVF Hospital: The Best Altruistic Surrogacy Centre in Delhi
Altruistic surrogacy has emerged as a ray of hope for many couples struggling with infertility, offering them a chance to experience the joy of parenthood. In Delhi, SCI IVF Hospital has established itself as the best altruistic surrogacy centre, combining advanced medical technology, a compassionate approach, and adherence to ethical standards.
Understanding Altruistic Surrogacy in Delhi
Altruistic surrogacy is a legally regulated process in which a surrogate mother carries a baby for intending parents without financial compensation, except for medical and essential living expenses. This method ensures ethical practices and mutual respect among all parties involved.
Delhi has become a hub for altruistic surrogacy due to its adherence to India’s Surrogacy (Regulation) Act, 2021, which ensures transparency, fairness, and legal safeguards. SCI IVF Hospital leads the way in providing professional and empathetic care throughout the surrogacy journey.
Why Choose SCI IVF Hospital?
SCI IVF Hospital is a pioneer in offering altruistic surrogacy in Delhi, helping numerous families achieve their parenthood dreams.
1. Renowned Expertise:
Led by Dr. Shivani Sachdev Gour, a highly experienced fertility specialist, SCI IVF Hospital has a proven track record of successful surrogacy cases. The dedicated team of doctors, embryologists, and counselors ensures a smooth process for both the intended parents and the surrogate.
2. State-of-the-Art Facilities:
SCI IVF Hospital is equipped with cutting-edge technology for IVF, embryo transfer, and other fertility treatments, ensuring the highest success rates.
3. Ethical and Transparent Practices:
As the best altruistic surrogacy centre in Delhi, SCI IVF Hospital strictly follows legal and ethical guidelines, offering clear communication and support at every stage.
4. Comprehensive Support Services:
From selecting a surrogate to legal documentation, medical care, and emotional support, SCI IVF Hospital provides a holistic approach to surrogacy, ensuring a seamless experience for all parties involved.
Affordable Altruistic Surrogacy Treatment Cost in Delhi
One of the key concerns for intending parents is the cost of surrogacy. At SCI IVF Hospital, the altruistic surrogacy treatment cost in Delhi is designed to be transparent and affordable while maintaining the highest standards of care.
What Influences the Cost?
Medical procedures like IVF and embryo transfer.
Essential medical care and living expenses for the surrogate.
Legal documentation and counseling fees.
SCI IVF Hospital ensures that every aspect of the treatment is optimized for cost-effectiveness, making it accessible for families across the globe.
Your Journey to Parenthood Starts Here
For couples dreaming of starting a family, SCI IVF Hospital offers a perfect blend of expertise, empathy, and excellence in surrogacy care.
Contact SCI IVF Hospital today to learn more about how altruistic surrogacy in Delhi can help you realize your dream of parenthood.
0 notes
Text
Understanding the stages of IVF implantation can give you clarity during your fertility journey.
#ivf#ivf procedure#ivfjourney#ivf treatment#ivf specialist#ivf babies#ivf hospital#fertility#fertilitytreatment#fertilitycentre#infertility#healthylifestyle#embryo#embryo transfer#ivf implantation#implantation#in vitro fertilization
0 notes
Text

Single Embryo Transfer (SET) vs. Multiple Embryo Transfer: Risks and Benefits
During the IVF process, multiple eggs are harvested and fertilized, leading to the development of viable embryos, which are transferred to the uterus. In your IVF process, you need the mots critical decision for yourself whether you need to opt for single embryo transfer (SET) or multiple embryo transfer (MET). This article will provide you with information about the distinction between each approach, as both are associated with different risks and benefits. Your choice will directly impact the outcome of the IVF cycle and the long-term health of both the child and mother. Read more
1 note
·
View note
Text
Hey there beautiful people!
Today's been a day. My hubbys parents are coming to visit this week for a few days and we were suppose to be getting the house ready starting today. We started with washing the puppies and I definitely did too much. I'm having some cramping pains and my legs hurt like I pulled a bunch of muscles. I also have been feeling super nauseous all day. I told hubby that whatever gets done gets done and if there's an issue I'll handle it. Like he's been so great with taking on a lot more work than he normally does. I had this huge plan of all the things that need to get done and now I only have 2 days to get it done so yeah. It's not all going to get done. He agrees that I overdid it and was basically like "you need to rest" so resting I shall do. I also have work Monday-Wednesday, Friday so I really need to make sure I'm taking it easy. We get to see our little Embie again on Thursday so we have 4 days to wait.
ttf
Take Care of Yourself, Love yourself
0 notes