#improving vaccination and treatment
Explore tagged Tumblr posts
Text
Understanding the Crucial Role of Regular Health Check-ups for Optimal Wellness
Regular health check-ups refer to the routine medical examinations or tests that are conducted to assess an individual’s overall health status. These check-ups are crucial as they help in early detection and prevention of potential health issues. They can include various tests such as blood tests, physical examinations, screenings, and consultations with doctors. The importance of regular health…

View On WordPress
#early detection of diseases#improving lifespan#keeping a check on body weight#maintaining a healthy lifestyle#managing stress#monitoring blood pressure#preventing complications of existing health conditions#prevention of illnesses#reducing healthcare costs#Regular monitoring of health#tracking progress of a treatment#updating vaccinations
0 notes
Text
I can think of a hundred things we could do to improve our collective health a hundred fold more than replacing sugar with a slightly different sugar that breaks down to be the same sugar in our bodies.
Free cancer screenings.
Eliminating food deserts.
Free vaccines.
Free birth control.
Drug treatment.
Naloxone to anyone who wants it.
Okay, I am too tired to do one hundred. But I'm sure I could.
1K notes
·
View notes
Text
"Engineers at the University of Pennsylvania have made a critical breakthrough that promises better outcomes for pregnancies threatened with pre-eclampsia, a condition that arises due to insufficient blood flow to the placenta, resulting in high maternal blood pressure and restricted blood flow to the fetus.
Pre-eclampsia is one of the leading causes of stillbirths and prematurity worldwide, and it occurs in 3 to 5% of pregnancies. Without a cure, options for these patients only treat symptoms, such as taking blood pressure medication, being on bed rest, or delivering prematurely—regardless of the viability of their baby.
Making a decision to treat pre-eclampsia in any manner can be a moral conundrum, to balance many personal health decisions with long-standing impacts—and for Kelsey Swingle, a doctoral student in the UPenn bioengineering lab, these options are not enough.
In previous research, she conducted a successful proof-of-concept study that examined a library of lipid nanoparticles (LNPs)—which are the delivery molecules that helped get the mRNA of the COVID vaccine into cells—and their ability to reach the placenta in pregnant mice.
In her latest study, published in Nature, Swingle examined 98 different LNPs and their ability to get to the placenta and decrease high blood pressure and increase vasodilation in pre-eclamptic pregnant mice.
Her work shows that the best LNP for the job was one that resulted in more than 100-fold greater mRNA delivery to the placenta in pregnant mice than an FDA-approved LNP formulation.
The drug worked.
“Our LNP was able to deliver an mRNA therapeutic that reduced maternal blood pressure through the end of gestation and improved fetal health and blood circulation in the placenta,” says Swingle.
“Additionally, at birth we saw an increase in litter weight of the pups, which indicates a healthy mom and healthy babies. I am very excited about this work and its current stage because it could offer a real treatment for pre-eclampsia in human patients in the very near future.”
While further developing this cure for pre-eclampsia and getting it to the market for human use is on the horizon for the research team, Swingle had to start from scratch to make this work possible. She first had to lay the groundwork to run experiments using pregnant mice and determine how to induce pre-eclampsia in this animal model, processes that are not as well studied.
But, by laying this groundwork, Swingle’s work has not only identified an avenue for curing pre-eclampsia, it also opens doors for research on LNP-mRNA therapeutics addressing other reproductive health challenges...
As Swingle thinks ahead for next steps in her research, which was funded by the National Institutes of Health and the National Science Foundation, she will also collaborate to further optimize the LNP to deliver the mRNA even more efficiently, as well as understanding the mechanisms of how it gets to the placenta, a question still not fully answered.
They are already in talks about creating a spin-off company and want to work on bringing this LNP-mRNA therapeutic to clinical trials and the market.
Swingle, who is currently finishing up her Ph.D. research, has not only successfully led this new series of studies advancing pre-eclampsia treatment at Penn, she has also inspired other early career researchers in the field as she continues to thrive while bringing women’s health into the spotlight."
-via Good News Network, December 15, 2024
1K notes
·
View notes
Text
Listen that billboard pissed me off so I'm gonna put my Unicef pin on my fandom hat for a second and take a page from @911actually 's book (their fundraisers for fallen and disabled firefighters/their families can be found here).
Our beloved fire dad died from Crimean Congo Hemorrhagic Fever, which currently has no approved vaccine. It's part of a list of illnesses as long as my arm from which hundreds of thousands of people die every year without so much as a headline in the Western world.
I think it would be a missed opportunity to not call attention (and funds) to finding cures and improving the delivery of treatments/therapies/vaccines for these illnesses. So with that in mind here's some fundraising links:
The End Fund: These guys fill in the atrocious gaps in funding for delivering Neglected Tropical Disease treatments. While USAID is under consistent attack, its more important than ever to help these organizations keep the lights on and save lives.
Gavi : Full disclosure, I wrote my masters thesis on this organization and I'm here to tell you, our global vaccine delivery system is *terrifyingly* dependent on billionaires. Bill Gates is just shy of 70 and currently his foundation accounts for over a third of the investments in these types of global health initiatives. We need large grassroots funding and we need to start building these practices right the fuck now. We cannot count on the benevolent billionaire (which is an oxymoron but I digress) to sustain the most important global health infrastructure we have.
WHO: They've developed the action plan for CCHF which you can read here if you're interested. They don't have any CCHF specific fundraisers that I can find at the moment, however, one thing you learn is building the research and delivery infrastructure for combatting one disease has positive spillover effects for fighting other ones too <3.
Feel free to reblog with more links if you find them!!
298 notes
·
View notes
Note
My mom has gone full on Youtube Woo "natural cures" and I have no idea how to get through to her. Literally sitting at home in front of the tv playing video after video of pseudoscientific bunk and lapping it up... She's diabetic and a cancer survivor and I fear she's gonna do irreparable damage in her forays into the deep end...
Do you have any tips on reaching folks that are in this deep?
Regular reinforcement of evidence-based medicine as kind as you can make it whenever it comes up.
"Oh I heard about this coffee enema thing..." "There's not really any evidence to back that up, mom, and besides, it sounds pretty unpleasant."
"Oh I heard about how nightshades are poison" "That book doesn't have a lot of great evidence, plus here are the kinds of micronutrients that you can get from nightshades, they're important in your diet."
"Oh I'm not sure about vaccines anymore, the new ones are so scary" "Mom, I'm so glad you got me vaccinated, I think about how kids younger than me are at risk of measles and other issues because of vaccine hesitancy and I worry so much for them, I think you made the right decision when I was a kid and I'm grateful for it."
"Oh, but fluoride in the water can cause IQ losses in young children," "Mom, those studies aren't in areas where fluoride is added, they're in areas where it's naturally high and are way, way above what gets added here, plus look at you and me, we have been drinking fluoridated water and we're both smart."
IDK, it's miserable. Basically you go on natural news and learn about all the lies, then spend twenty times as much time learning about the debunkings for all the lies and then try to be nice when you tell them they're wrong.
Since your mom has had previous successful treatment from allopathic doctors call back to that; "but mom I'm so glad they were able to take care of your cancer - I know it was hard but I think you might not have survived if you hadn't trusted your doctors." "but mom, look at how much the medical science on diabetes has improved in your lifetime; i'm glad it's easier to manage now than it was when you were younger, and that there are better treatments being developed all the time; I don't think they're hiding things from us otherwise they'd still treat diabetes and cancer like they did in the 50s, and things are so much better than that."
Just. Try to be nice. Try not to attack her. Try to keep it light and offer cheerful arguments before changing the subject.
You don't want her to get defensive, you want her to consider you to be someone she can ask for information who won't make fun of her and doesn't think she's stupid.
Anyway. Life with my mother in law has been fun recently. She watched a youtube video and decided she must have gone into ketosis after fasting for twelve hours so she ordered a bunch of protein strips and I'm cooking for her a few times a week to guarantee that she's eating something other than canned chili beans.
So. You know. I feel you.
452 notes
·
View notes
Text
Why I'm Enthusiastic About Kamala Harris



I've seen so much negative talk about Trump and we all agree with that, but I want to highlight what I like most about Kamala Harris and why I'm actively enthusiastic and excited about voting for her:
She is pro-abortion rights and pro- comprehensive sex ed
She would appoint good Supreme Court Justices.
She respects people with a diverse range of political views and would include some voices from both progressive and conservative perspectives in her administration.
She is unambiguously pro-LGBTQ rights, including not just on gay rights but also trans rights.
She would represent continuity with the Biden administration, an administration that I think has done a good job on most issues.
On the issue of Palestine/Israel/Gaza (where I am most critical of Biden), I think Harris is a significant improvement over Biden, and also offers the better path of the only two viable candidates, towards ending the genocide. She has spoken out against the civilian deaths and she has snubbed Netanyahu which is a huge plus in my book.
She has shown a willingness to change her views, such as how she moved from being opposed to decriminalizing sex work in 2008, to being supportive of it in 2019, and being initially skeptical of marijuana legalization in 2010, but coming to support it in 2015. I like a candidate who can change their views, but more importantly, she is changing in a direction I like.
She would be good on the economy; she opposes tariffs, and would continue the Biden administration policies which have led to economic prosperity.
She has a solid and fairly diverse track record of experience, working as attorney general for the largest state, then senator for that state, then VP.
She has worked to combat over-incarceration and cruel treatment of people in prison, doing things like reducing mandatory minimum sentences and working to reduce recidivism, opposing solitary confinement, ending private prisons, and ending cash bail. She has also pledged to use the president's clemency powers to release a lot of people who have been imprisoned unjustly or given unfairly harsh sentences.
She has a concrete plan to enact immigration reform that would adequately fund the processing of asylum applications and fix the backlog of immigrants at the border. And the plan has broad bipartisan support.
On top of this she also has already done some things to address the root causes of migration in Latin America, particularly people fleeing Guatemala, Honduras, and El Salvador
She is pro-net-neutrality.
She supports universal healthcare, but also has concrete recommendations for how to improve the current status quo.
She is pro-science, including on issues like climate change, COVID, vaccinations, and health and nutrition. Her mom was a scientist!
She is pro-Ukraine, wanting to keep Russia out of Ukraine and ensure Ukraine wins their war of defense and maintains their independence.
She is across-the-board better on women's issues, not just reproductive rights but also sexual violence and domestic violence, workplace equality and the pay gap, and women's issues in Latin America (which is related to the immigration pressure I mentioned above.)
She generally takes stances on foreign policy I agree with, being skeptical of leaders (Putin, Orban, Netanyahu) I want us to be skeptical of, and working with and looking up to the ones I want us to work with and look up to (Olaf Scholz, Emmanuel Macron). She already has a working relationship with many of these leaders too, and has a reputation of being both personable and tough, just what I'd want.
She's smart, well-educated, and surrounded with smart, well-educated, and wise people. Her campaign is stable and well-run, and I trust her to put together a team of competent advisors and run this country competently, probably even more so than Biden has done, and Biden has done a pretty decent job, exceeding my expectations even.
Harris also has an impressive list of endorsements. I can't possibly be comprehensive here, but it includes people as diverse as the most progressive Democrat Lawmakers (Bernie Sanders and AOC), some of the most conservative former GOP legislators (Jeff Flake, Liz Cheney), and over 100 former GOP staffers including a disturbing number of insiders from the Trump administration. This is telling! You don't see this sort of whistleblowing and defection from within the Biden administration.
The fact that Harris has racked up endorsements from people spanning the whole political spectrum from solid-right to solid-left and everything in between, impresses me. This is the sign of someone who is going to be good at getting people to work together, someone who will listen to a wide range of viewpoints and develop better policy and take better courses of action as a result. It's what I always want in a president.
In some elections I have been frustrated that I'm voting for a "lesser of two evils" but this time around I actually feel actively enthusiastic about Harris. I am excited to vote tomorrow and excited to finally be done with this election, and I am cautiously optimistic that it is going to turn out really well.
I encourage everyone to vote and make sure to make sure everyone close to you is also voting!
272 notes
·
View notes
Text
also preserved on our archive
by Rowan Walrath
Public and private funding is lacking, scrambling opportunities to develop treatments
In brief Long COVID is a difficult therapeutic area to work in. It’s a scientifically challenging condition, but perhaps more critically, few want to fund new treatments. Private investors, Big Pharma, and government agencies alike see long COVID as too risky as long as its underlying mechanisms are so poorly understood. This dynamic has hampered the few biotechnology and pharmaceutical companies trying to develop new medicines. The lack of funding has frustrated people with long COVID, who have few options available to them. And crucially, it has snarled research and development, cutting drug development short.
When COVID-19 hit, the biotechnology company Aim ImmunoTech was developing a drug for myalgic encephalomyelitis/chronic fatigue syndrome, better known as ME/CFS. As more people came down with COVID-19, some began to describe lingering problems that sounded a lot like ME/CFS. In many cases, people who got sick simply never seemed to get better. In others, they recovered completely—or thought they had—only to be waylaid by new problems: fatigue that wouldn’t go away with any amount of rest, brain fog that got in the way of normal conversations, a sudden tendency toward dizziness and fainting, or all the above.
There was a clear overlap between the condition, which patients began calling long COVID, and ME/CFS. People with ME/CFS have a deep, debilitating fatigue. They cannot tolerate much, if any, exercise; walking up a slight incline can mean days of recovery. Those with the most severe cases are bedbound.
Aim’s leaders set out to test whether the company’s drug, Ampligen, which is approved for ME/CFS in Argentina but not yet in the US, might be a good fit for treating long COVID. They started with a tiny study, just 4 people. When most of those participants responded well, they scaled up to 80. While initial data were mixed, people taking Ampligen were generally able to walk farther in a 6 min walk test than those who took a placebo, indicating improvement in baseline fatigue. The company is now making plans for a follow-on study in long COVID.
Aim’s motivation for testing Ampligen in long COVID was twofold. Executives believed they could help people with the condition, given the significant overlap in symptoms with ME/CFS. But they also, plainly, thought there’d be money. They were wrong.
“When we first went out to do this study in long COVID, there was money from . . . RECOVER,” Aim scientific officer Chris McAleer says, referring to Researching COVID to Enhance Recovery (RECOVER), the National Institutes of Health’s $1.7 billion initiative to fund projects investigating causes of, and potential treatments for, long COVID. McAleer says Aim attempted to get RECOVER funds, “believing that we had a therapeutic for these individuals, and we get nothing.”
Instead of funding novel medicines like Ampligen, the NIH has directed most of its RECOVER resources to observational studies designed to learn more about the condition, not treat it. Only last year did the agency begin to fund clinical trials for long COVID treatments, and those investigate the repurposing of approved drugs. What RECOVER is not doing is funding new compounds.
RECOVER is the only federal funding mechanism aimed at long COVID research. Other initiatives, like the $5 billion Project NextGen and the $577 million Antiviral Drug Discovery (AViDD) Centers for Pathogens of Pandemic Concern, put grant money toward next-generation vaccines, monoclonal antibodies, and antivirals for COVID-19. They stop short of testing those compounds as long COVID treatments.
Private funding is even harder to come by. Large pharmaceutical companies have mostly stayed away from the condition. (Some RECOVER trials are testing Pfizer’s COVID-19 antiviral Paxlovid, but a Pfizer spokesperson confirms that Pfizer is not sponsoring those studies.) Most investors have also avoided long COVID: a senior analyst on PitchBook’s biotech team, which tracks industry financing closely, says he isn’t aware of any investment in the space.
“What you need is innovation on this front that’s not driven by profit motive, but impact on global human health,” says Sumit Chanda, an immunologist and microbiologist at Scripps Research who coleads one of the AViDD centers. “We could have been filling in the gaps for things like long COVID, where pharma doesn’t see that there’s a billion-dollar market.”
The few biotech companies that are developing potential treatments for long COVID, including Aim, are usually funding those efforts out of their own balance sheets. Experts warn that such a pattern is not sustainable. At least four companies that were developing long COVID treatments have shut down because of an apparent lack of finances. Others are evaluating a shift away from long COVID.
“It is seen by the industry and by investors as a shot in the dark,” says Radu Pislariu, cofounder and CEO of Laurent Pharmaceuticals, a start-up that’s developing an antiviral and anti-inflammatory for long COVID. “What I know is that nobody wants to hear about COVID. When you say the name COVID, it’s bad . . ., but long COVID is not going anywhere, because COVID-19 is endemic. It will stay. At some point, everyone will realize that we have to do more for it.”
‘Time and patience and money’ Much of the hesitancy to make new medicines stems from the evasive nature of long COVID itself. The condition is multisystemic, affecting the brain, heart, endocrine network, immune system, reproductive organs, and gastrointestinal tract. While researchers are finding increasing evidence for some of the disease’s mechanisms, like viral persistence, immune dysregulation, and mitochondrial dysfunction, they might not uncover a one-size-fits-all treatment.
“Until we have a better understanding of the underlying mechanisms of long COVID, I think physicians are doing the best they can with the information they have and the guidance that is available to them,” says Ian Simon, director of the US Department of Health and Human Services’ Office of Long COVID Research and Practice. The research taking place now will eventually guide new therapeutic development, he says.
Meanwhile, time marches on.
By the end of 2023, more than 409 million people worldwide had long COVID, according to a recent review coauthored by two cofounders of the Patient-Led Research Collaborative (PLRC) and several prominent long COVID researchers (Nat. Med. 2024; DOI: 10.1038/s41591-024-03173-6). Most of those 409 million contracted COVID-19 and then long COVID after vaccines and antivirals became available. That fact undercuts the notion that the condition results only from severe cases of COVID-19 contracted before those interventions existed. (Vaccination and treatment with antivirals do correlate with a lower incidence of long COVID but don’t prevent it outright.)
“There is that narrative that long COVID is over,” says Hannah Davis, cofounder of the PLRC and a coauthor of the review, who has had long COVID since 2020. “I think that’s fairly obviously not true.”
The few biotech companies that have taken matters into their own hands, like Aim, are often reduced to small study sizes with limited time frames because they can’t get outside funding.
InflammX Therapeutics, a Florida-based ophthalmology firm headed by former Bausch & Lomb executive Brian Levy, started testing an anti-inflammatory drug candidate called Xiflam after Levy’s daughter came down with long COVID. Xiflam is designed to close connexin 43 (Cx43) hemichannels when they become pathological. The hemichannels, which form in cell membranes, would otherwise allow intracellular adenosine triphosphate (ATP) to escape and signal the NLRP3 inflammasome to crank up its activity, causing pain and inflammation.
InflammX originally conceived of Xiflam as a treatment for inflammation in various eye disorders, but after Levy familiarized himself with the literature on long COVID, he figured the compound might be useful for people like his daughter.
InflammX set up a small Phase 2a study at a site just outside Boston. The trial will enroll just 20 participants, including Levy’s daughter and InflammX’s chief operating and financial officer, David Pool, who also has long COVID. The study is set up such that participants don’t know if they’re taking Xiflam or a placebo.
Levy says the company tried to communicate with NIH RECOVER staff multiple times but never heard back. “We couldn’t wait,” he says.
Larger firms are similarly disconnected from US federal efforts. COVID-19 vaccine maker Moderna appointed a vice president of long COVID last year. Bishoy Rizkalla now oversees a small team studying how the company’s messenger RNA shots could mitigate problems caused by new and latent viruses, including SARS-CoV-2. But Rizkalla says Moderna has no federally funded projects in long COVID.
Federal bureaucracy has slowed down research in other ways. When long COVID appeared, Tonix Pharmaceuticals was developing a possible drug called TNX-102 SL to treat fibromyalgia. The two conditions look similar: they’re painful, fatiguing, and multisystemic, and fibromyalgia can crop up after a viral infection.
But it wasn’t easy to design a study to test the compound in long COVID. Among other issues, the US Food and Drug Administration initially insisted that participants have a positive COVID-19 test confirmed by a laboratory, like a polymerase chain reaction test, to be included in the study. At-home diagnostics wouldn’t count.
“We spent a huge amount of money, and we couldn’t enroll people who had lab-confirmed COVID because no one was going to labs to confirm their COVID,” cofounder and CEO Seth Lederman says. “We just ran out of time and patience and money, frankly.”
Tonix had planned to enroll 450 participants. The company ultimately enrolled only 63. The study failed to meet its primary end point of reducing pain intensity, a result Lederman attributes to the smaller-than-expected sample size.
TNX-102 SL trended toward improvements in fatigue and other areas, like sleep quality and cognitive function, but Tonix is moving away from developing the compound as a long COVID treatment and focusing on developing it for fibromyalgia. If it’s approved, Lederman hopes that physicians will prescribe it to people who meet the clinical criteria for fibromyalgia regardless of whether their condition stems from COVID-19.
“I’m not saying we’re not going to do another study in long COVID, but for the short term, it’s deemphasized,” Lederman says.
Abandoned attempts Without more public or private investment, it’s unclear how research can proceed. The small corner of the private sector that has endeavored to take on long COVID is slowly becoming a graveyard.
Axcella Therapeutics made a big gamble in late 2022. The company pivoted from trying to treat nonalcoholic steatohepatitis, a liver disease, to addressing chronic fatigue in people with long COVID. In doing so, Axcella reoriented itself exclusively around long COVID, laying off most of its staff and abandoning other research activities. People in a 41-person Phase 2a trial of the drug candidate, AXA1125, showed improvement in fatigue scores based on a clinical questionnaire (eClinicalMedicine 2023, DOI: 10.1016/j.eclinm.2023.101946), but Axcella shut down before it could get its planned 300-person follow-on study up and running.
The fate of AXA1125 may be to gather dust. Axcella’s former executives have moved on to other pursuits. Erstwhile chief medical officer Margaret Koziel, once a champion of AXA1125, says by email that she is “not up to date on current research on long COVID.” Staff at the University of Oxford, which ran the Phase 2a study, were not able to procure information about the planned Phase 2b/3 trial. A spokesperson for Flagship Pioneering, the venture firm that founded Axcella in 2011, declined to comment to C&EN.
Other firms have met similar ends. Ampio Pharmaceuticals dissolved in August after completing only a Phase 1 study to evaluate an inhaled medication called Ampion in people with long COVID who have breathing issues. Biotech firm SolAeroMed shut down before even starting a trial of its bronchodilating medicine for people with long COVID. “Unfortunately we were unable to attract funding to support our clinical work for COVID,” CEO John Dennis says by email.
Another biotech company, Aerium Therapeutics, did manage to get just enough of its monoclonal antibody AER002 manufactured and in the hands of researchers at the University of California, San Francisco, before it ended operations. The researchers are now testing AER002 in a Phase 2 trial with people with long COVID. Michael Peluso, an infectious disease clinician and researcher at UCSF and principal investigator of the trial, says that while AER002 may not advance without a company behind it, the study could be valuable for validating long COVID’s mechanisms of disease and providing a proof of concept for monoclonal antibody treatment more generally.
“[Aerium] put a lot of effort into making sure that the study would not be impacted,” Peluso says. “Regardless of the results of this study, doing a follow-up study now that we’ve kind of learned the mechanics of it with modern monoclonals would be really, really interesting.”
‘A squandered opportunity’ In 2022, the NIH’s National Institute of Allergy and Infectious Diseases (NIAID) put about $577 million toward nine research centers that would discover and develop antivirals for various pathogens. Called the Antiviral Drug Discovery (AViDD) Centers for Pathogens of Pandemic Concern, the centers were initially imagined as 5-year projects, enough time to ready multiple candidates for preclinical development. The NIH allocated money for the first 3 years and promised more funds to come later.
The prospect excited John Chodera, a computational chemist at the Memorial Sloan Kettering Cancer Center and a principal investigator at an AViDD center called the AI-Driven Structure-Enabled Antiviral Platform. Chodera figured that if his team were able to develop a potent antiviral for SARS-CoV-2, it could potentially be used to treat long COVID as well. A predominant theory is that reservoirs of hidden virus in the body cause ongoing symptoms.
But Chodera says NIAID told him and other AViDD investigators that establishing long COVID models was out of scope. And last year, Congress clawed back unspent COVID-19 pandemic relief funds, including the pool of money intended for the AViDD centers’ last 2 years. Lawmakers were supposed to come through with additional funding, Chodera says, but it never materialized. All nine AViDD centers will run out of money come May 2025.
“When we do start to understand what the molecular targets for long COVID are going to be, it’d be very easy to pivot and train our fire on those targets,” says Chanda from Scripps’s AViDD center. “The problem is that it took us probably 2 years to get everything up and going. If you cut the funding after 3 years, we basically have to dismantle it. We don’t have an opportunity to say, ‘Hey, look, this is what we’ve done. We can now take this and train our fire on X, Y, and Z.’ ”
Researchers at multiple AViDD centers confirm that the NIH has offered a 1-year, no-cost extension, but it doesn’t come with additional funds. They now find themselves in the same position as many academic labs: seeking grant money to keep their projects going.
Worse, they say, is that applying for other grants will likely mean splitting up research teams, thus undoing the network effect that these centers were supposed to provide.
“Now what we’ve got is a bunch of half bridges with nowhere to fund the continuation of that work,” says Nathaniel Moorman, cofounder and scientific adviser of the Rapidly Emerging Antiviral Drug Development Initiative, which houses an AViDD center at the University of North Carolina at Chapel Hill.
“This was a squandered opportunity, not just for pandemic preparedness but to tackle these unmet needs that are being neglected by biotech and pharma,” Chanda says.
Viral persistence Ann Kwong has been here before. The virologist was among the first industry scientists trying to develop antivirals for hepatitis C virus (HCV) back in the 1990s. Kwong led an antiviral discovery team at the Schering-Plough Research Institute for 6 years. In 1997, Vertex Pharmaceuticals recruited her to lead its new virology group.
Kwong and her team at Vertex developed a number of antivirals for HCV, HIV, and influenza viruses; one was the HCV protease inhibitor telaprevir. She recalls that a major challenge for the HCV antivirals was that scientists didn’t know where in the body the virus was hiding. Kwong says she had to fight to develop an antiviral that targeted the liver since it hadn’t yet been confirmed that HCV primarily resides there. People with chronic hepatitis C would in many cases eventually develop liver failure or cancer, but they presented with other issues too, like brain fog, fatigue, and inflammation.
She sees the same dynamic playing out in long COVID.
“This reminds me of HIV days and HCV days,” Kwong says. “This idea that pharma doesn’t want to work on this because we don’t know things about SARS-CoV-2 and long COVID is bullshit.”
Since January, Kwong has been cooking up something new. She’s approaching long COVID the way she did chronic hepatitis C: treating it as a chronic infection, through a start-up called Persistence Bio. Persistence is still in stealth; its name reflects its mission to create antivirals that can reach hidden reservoirs of persistent SARS-CoV-2, which many researchers believe to be a cause of long COVID.
“Long COVID is really interesting because there’s so many different symptoms,” Kwong says. “As a virologist, I am not surprised, because it’s an amazing virus. It infects every tissue in your body. . . . All the autopsy studies show that it’s in your brain. It’s in your gut. It’s in your lungs. It’s in your heart. To me, all the different symptoms are indicative of where the virus has gone when it infected you.”
Kwong has experienced some of these symptoms firsthand. She contracted COVID-19 while flying home to Massachusetts from Germany in 2020. For about a year afterward, she’d get caught off guard by sudden bouts of fatigue, bending over to catch her breath as she walked around the horse farm where she lives, her legs aching. Those symptoms went away with time and luck, but another round of symptoms roared to life this spring, including what Kwong describes as “partial blackouts.”
Kwong hasn’t been formally diagnosed with long COVID, but she says she “strongly suspects” she has it. Others among Persistence’s team of about 25 also have the condition.
“Long COVID patients have been involved with the founding of our company, and we work closely with them and know how awful the condition can be,” Kwong says. “It is a big motivator for our team.”
Persistence is in the process of fundraising. Kwong says she’s in conversations with private investors, but she and her cofounders are hoping to get public funding too.
On Sept. 23, the NIH is convening a 3-day workshop to review what RECOVER has accomplished and plan the next phase of the initiative. Crucially, that phase will include additional clinical trials. RECOVER’s $1.7 billion in funding includes a recent award of $515 million over the next 4 years. It’s not out of the question that this time, industry players might be invited to the table. Tonix Pharmaceuticals’ Lederman and Aim ImmunoTech’s McAleer will both speak during the workshop.
The US Senate Committee on Appropriations explicitly directed the NIH during an Aug. 1 meeting to prioritize research to understand, diagnose, and treat long COVID. It also recommended that Congress put $1.5 billion toward the Advanced Research Projects Agency for Health (ARPA-H), which often partners with industry players. The committee instructed ARPA-H to invest in “high-risk, high-reward research . . . focused on drug trials, development of biomarkers, and research that includes long COVID associated conditions.” Also last month, Sen. Bernie Sanders (I-VT) introduced the Long COVID Research Moonshot Act, which would give the NIH $1 billion a year for a decade to treat and monitor patients.
It’s these kinds of mechanisms that might make a difference for long COVID drug development.
“What I’ve seen a lot is pharma being hesitant to get involved,” says Lisa McCorkell, a cofounder of the PLRC and a coauthor of the recent long COVID review. “Maybe they’ll invest if NIH also matches their investment or something like that. Having those public-private partnerships is really, at this stage, what will propel us forward.”
Chemical & Engineering News ISSN 0009-2347 Copyright © 2024 American Chemical Society
#mask up#covid#pandemic#wear a mask#covid 19#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid#covid conscious#covid is not over#wear a fucking mask
149 notes
·
View notes
Note
“This woman prayed and her cancer was cured”
“That miracle only happened to one person, it’s way too small, is God asleep at the wheel or something?”
“Thousands of people saw another miracle”
“Well, that was probably mass hysteria”
What would be a hypothetical miracle which you would accept?
approximately ten million people die of cancer each year, so prayer appears to be an ineffective intervention in general and we don't see a significant difference in remissions between Catholic or Protestant or Muslim or Hindu patients as far as I'm aware, but we have seen dramatic improvements in outcomes for some cancers due to our understanding of the condition and development of new treatments, suggesting that scientific research saves lives and prayer does not (reinforced during the covid pandemic with the creation of new RNA vaccines while many religious leaders were still urging people to meet communally and give the virus to each other and trust in god).
far more people have seen UFOs than Catholic miracles and I believe these can be analysed in a similar manner.
there are so many miracles that would actually be convincing! but if they were observed and confirmed then they wouldn't be miracles would they, the key aspect of a miracle is that it needs to be a rumour, improbable, unverifiable, something that demands faith without evidence, to confirm a belief already strongly held; a real miracle would convince me, but ironically wouldn't be very interesting to the religious (NASA putting Jesus in the wind tunnel to see how he manages to ascend through the air without being torn apart by aerodynamic forces).
56 notes
·
View notes
Text
100 Inventions by Women
LIFE-SAVING/MEDICAL/GLOBAL IMPACT:
Artificial Heart Valve – Nina Starr Braunwald
Stem Cell Isolation from Bone Marrow – Ann Tsukamoto
Chemotherapy Drug Research – Gertrude Elion
Antifungal Antibiotic (Nystatin) – Rachel Fuller Brown & Elizabeth Lee Hazen
Apgar Score (Newborn Health Assessment) – Virginia Apgar
Vaccination Distribution Logistics – Sara Josephine Baker
Hand-Held Laser Device for Cataracts – Patricia Bath
Portable Life-Saving Heart Monitor – Dr. Helen Brooke Taussig
Medical Mask Design – Ellen Ochoa
Dental Filling Techniques – Lucy Hobbs Taylor
Radiation Treatment Research – Cécile Vogt
Ultrasound Advancements – Denise Grey
Biodegradable Sanitary Pads – Arunachalam Muruganantham (with women-led testing teams)
First Computer Algorithm – Ada Lovelace
COBOL Programming Language – Grace Hopper
Computer Compiler – Grace Hopper
FORTRAN/FORUMAC Language Development – Jean E. Sammet
Caller ID and Call Waiting – Dr. Shirley Ann Jackson
Voice over Internet Protocol (VoIP) – Marian Croak
Wireless Transmission Technology – Hedy Lamarr
Polaroid Camera Chemistry / Digital Projection Optics – Edith Clarke
Jet Propulsion Systems Work – Yvonne Brill
Infrared Astronomy Tech – Nancy Roman
Astronomical Data Archiving – Henrietta Swan Leavitt
Nuclear Physics Research Tools – Chien-Shiung Wu
Protein Folding Software – Eleanor Dodson
Global Network for Earthquake Detection – Inge Lehmann
Earthquake Resistant Structures – Edith Clarke
Water Distillation Device – Maria Telkes
Portable Water Filtration Devices – Theresa Dankovich
Solar Thermal Storage System – Maria Telkes
Solar-Powered House – Mária Telkes
Solar Cooker Advancements – Barbara Kerr
Microbiome Research – Maria Gloria Dominguez-Bello
Marine Navigation System – Ida Hyde
Anti-Malarial Drug Work – Tu Youyou
Digital Payment Security Algorithms – Radia Perlman
Wireless Transmitters for Aviation – Harriet Quimby
Contributions to Touchscreen Tech – Dr. Annette V. Simmonds
Robotic Surgery Systems – Paula Hammond
Battery-Powered Baby Stroller – Ann Moore
Smart Textile Sensor Fabric – Leah Buechley
Voice-Activated Devices – Kimberly Bryant
Artificial Limb Enhancements – Aimee Mullins
Crash Test Dummies for Women – Astrid Linder
Shark Repellent – Julia Child
3D Illusionary Display Tech – Valerie Thomas
Biodegradable Plastics – Julia F. Carney
Ink Chemistry for Inkjet Printers – Margaret Wu
Computerised Telephone Switching – Erna Hoover
Word Processor Innovations – Evelyn Berezin
Braille Printer Software – Carol Shaw
⸻
HOUSEHOLD & SAFETY INNOVATIONS:
Home Security System – Marie Van Brittan Brown
Fire Escape – Anna Connelly
Life Raft – Maria Beasley
Windshield Wiper – Mary Anderson
Car Heater – Margaret Wilcox
Toilet Paper Holder – Mary Beatrice Davidson Kenner
Foot-Pedal Trash Can – Lillian Moller Gilbreth
Retractable Dog Leash – Mary A. Delaney
Disposable Diaper Cover – Marion Donovan
Disposable Glove Design – Kathryn Croft
Ice Cream Maker – Nancy Johnson
Electric Refrigerator Improvements – Florence Parpart
Fold-Out Bed – Sarah E. Goode
Flat-Bottomed Paper Bag Machine – Margaret Knight
Square-Bottomed Paper Bag – Margaret Knight
Street-Cleaning Machine – Florence Parpart
Improved Ironing Board – Sarah Boone
Underwater Telescope – Sarah Mather
Clothes Wringer – Ellene Alice Bailey
Coffee Filter – Melitta Bentz
Scotchgard (Fabric Protector) – Patsy Sherman
Liquid Paper (Correction Fluid) – Bette Nesmith Graham
Leak-Proof Diapers – Valerie Hunter Gordon
FOOD/CONVENIENCE/CULTURAL IMPACT:
Chocolate Chip Cookie – Ruth Graves Wakefield
Monopoly (The Landlord’s Game) – Elizabeth Magie
Snugli Baby Carrier – Ann Moore
Barrel-Style Curling Iron – Theora Stephens
Natural Hair Product Line – Madame C.J. Walker
Virtual Reality Journalism – Nonny de la Peña
Digital Camera Sensor Contributions – Edith Clarke
Textile Color Processing – Beulah Henry
Ice Cream Freezer – Nancy Johnson
Spray-On Skin (ReCell) – Fiona Wood
Langmuir-Blodgett Film – Katharine Burr Blodgett
Fish & Marine Signal Flares – Martha Coston
Windshield Washer System – Charlotte Bridgwood
Smart Clothing / Sensor Integration – Leah Buechley
Fibre Optic Pressure Sensors – Mary Lou Jepsen
#women#inventions#technology#world#history#invented#creations#healthcare#home#education#science#feminism#feminist
56 notes
·
View notes
Text

Article
The number of children dying under five years of age declined by two thirds over the past two decades in Southern Asia, according to new mortality estimates released by UNICEF, the World Health Organization (WHO), the United Nations Population Division and the World Bank Group. Southern Asia includes nine countries: Afghanistan, Bangladesh, Bhutan, India, Iran, Maldives, Nepal, Pakistan, and Sri Lanka.
The report reveals that the number of child deaths under 5 years of age decreased from 5 million in 1990 to 1.3 million in 2022. The report also shows that Southern Asia’s under five mortality rate, or the probability that a child would die before five years of age, reduced by 72 per cent since 1990, and 62 per cent since 2000.
“We have made heartening progress to save millions of children’s lives since 1990. These aren’t just numbers on a page – these are children’s lives saved, sons and daughters, brothers and sisters. This success is largely due to investments in trained health workers, improvements in newborn care, treatment of childhood illnesses and vaccinations for children against deadly diseases,” said Sanjay Wijesekera, UNICEF Regional Director for Southern Asia. “This progress shows us that change is possible. These lives saved are testament to the engagement and will of governments, local organizations, health care professionals such as skilled birth attendants, parents, and families to save the most vulnerable children.” ...
Despite this progress, however, much more needs to be done...
The report also reveals that progress among countries is uneven. Three countries (Iran, Sri Lanka and Maldives) have achieved the SDG 2030 target for under five child mortality reduction and four are on track to meet the target (India, Bangladesh, Bhutan and Nepal). For example, Bangladesh’s neonatal mortality rate decreased from 66 deaths per 1,000 live births in 1990, to 17 deaths per 1,000 live births in 2022.
However, in Pakistan and Afghanistan, urgent action is required to accelerate their annual rates of reduction substantially to meet 2030 targets...
“We call on governments across the region to invest in simple solutions such as having trained birth attendants at every birth, ensuring that all newborns have essential care, better care of small and sick newborn babies, medicines, clean water, electricity, and vaccines to save lives. Every child has the right to healthcare.”
-via UNICEF, March 14, 2024
#children#cw infant death#cw child death#neonatal#public health#south asia#asia#iran#sri lank#maldives#india#bangladesh#bhutan#nepal#pakistan#afghanistan#medical news#children's rights#infant mortality#unicef#good news#hope
252 notes
·
View notes
Text
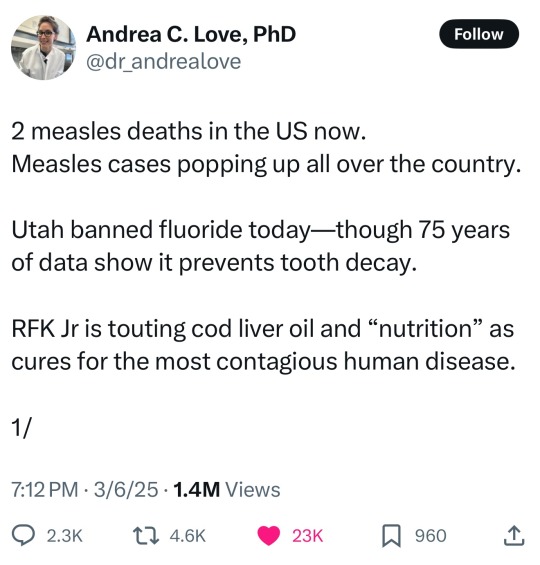
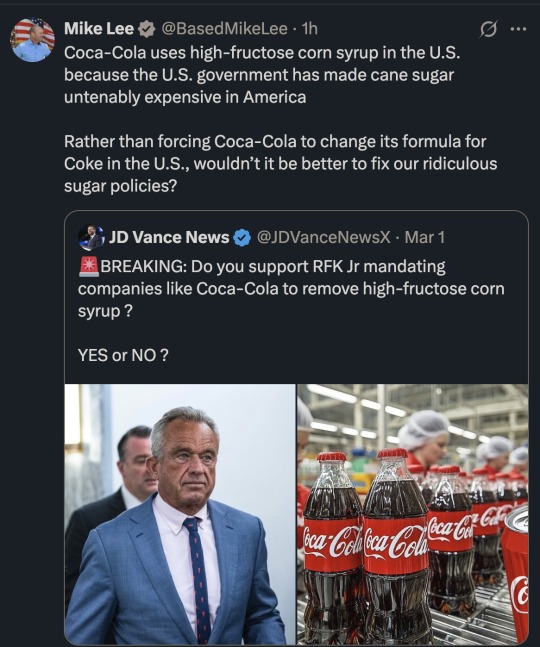
Everyone wants to be healthier. MAHA and RFK Jr will make people sicker—and poorer.
Make America Healthy Again, MAHA, claims it wants to improve American health, but MAHA actually opposes every single public health intervention and scientific innovation that improves health.
RFK Jr. and MAHA’s positions, rhetoric, and policy goals extend beyond anti-vaccine activism. The common theme: all of them will worsen people’s health. RFK Jr. and MAHA have shown, time and again, that they do not care about improving people’s health, only lining their pockets.
An anti-vaccine cult can’t call itself pro-health.
MAHA claims they want to tackle “chronic disease” yet ignore what this even means.
All organisms die—of something. Humans used to die prematurely because of acute causes. In 1900, US life expectancy was 47 years old and the leading causes of death were pneumonia, tuberculosis, and acute gastroenteritis (caused by food- and water-borne pathogens).
30.4% of all deaths in the United States in 1900 were in children younger than 5. Today, 0.75% of all deaths in the US are in children under 5.
Sit with that HUGE improvement. We are saving children’s lives because of scientific research, innovation, and medical developments.
We have eliminated the leading causes of death in 1900 from even being a blip on the radar in the US because of vaccines, sterilization, antimicrobials (antibiotics, antiparasitics, disinfectants), pasteurization, and hygiene measures (food hygiene, sexual hygiene, water treatment, plumbing, hand washing, etc).
People in the 1900s didn’t contend with chronic diseases because they were dying well before those chronic diseases would develop.
Today, leading causes of death are chronic: heart disease, cancers, and stroke top the list. MAHA claims this is cause for alarm: that there is a “chronic disease epidemic” — yet fail to understand that chronic diseases replaced acute illnesses as leading causes of death BECAUSE of the public health interventions they demonize.
👉🏿 https://news.immunologic.org/p/everyone-wants-better-health-rfk
#politics#maha#rfk jr#antivaxxers#republicans#freedom sores#measles#childhood illnesses#preventable illnesses#preventable diseases#freedom fries
74 notes
·
View notes
Text
The Best News of Last Week
🦾 - High-Five for Bionic Hand
1. Houston-area school district announces free breakfast and lunch for students

Pasadena ISD students will be getting free breakfast and lunch for the 2023-24 school year, per an announcement on the district's social media pages.
The 2023-24 free lunch program is thanks to a Community Eligibility Provision grant the district applied for last year. The CEP, which is distributed by the Department of Agriculture, is specially geared toward providing free meals for low-income students.
2. Dolphin and her baby rescued after being trapped in pond for 2 years
youtube
A pair of dolphins that spent nearly two years stuck in a Louisiana pond system are back at sea thanks to the help of several agencies and volunteers.
According to the Audubon Nature Institute, wildlife observers believe the mother dolphin and her baby were pushed into the pond system near Grand Isle, Louisiana, during Hurricane Ida in late August 2021.
3. Studies show that putting solar panels over waterways could boost clean energy and conserve water. The first U.S. pilot project is getting underway in California.

Some 8,000 miles of federally owned canals snake across the United States, channeling water to replenish crops, fuel hydropower plants and supply drinking water to rural communities. In the future, these narrow waterways could serve an additional role: as hubs of solar energy generation.
4. Gene therapy eyedrops restored a boy's sight. Similar treatments could help millions

Antonio was born with dystrophic epidermolysis bullosa, a rare genetic condition that causes blisters all over his body and in his eyes. But his skin improved when he joined a clinical trial to test the world’s first topical gene therapy.
The same therapy was applied to his eyes. Antonio, who’s been legally blind for much of his 14 years, can see again.
5. Scientists develop game-changing vaccine against Lyme disease ticks!

A major step in battling Lyme disease and other dangerous tick-borne viruses may have been taken as researchers announced they have developed a vaccine against the ticks themselves.
Rather than combatting the effects of the bacteria or microbe that causes Lyme disease, the vaccine targets the microbiota of the tick, according to a paper published in the journal Microbiota on Monday.
6. HIV Transmission Virtually Eliminated in Inner Sydney, Australia

Sydney may be the first city in the world to end AIDS as a public health threat by 2030. Inner Sydney has reduced new HIV acquisitions by 88%, meaning it may be the first locality in the world to reach the UN target to end AIDS as a public health threat by 2030
7. New bionic hand allows amputees to control each finger with unprecedented accuracy

In a world first, surgeons and engineers have developed a new bionic hand that allows users with arm amputations to effortlessly control each finger as though it was their own body.
Successful testing of the bionic hand has already been conducted on a patient who lost his arm above the elbow.
----
That's it for this week :)
This newsletter will always be free. If you liked this post you can support me with a small kofi donation:
Support this newsletter ❤️
Also don’t forget to reblog.
897 notes
·
View notes
Text
❗ HELP ME SAVE MY KITTEN ❗
updates about this post:
The diagnosis was confirmed. Léia suffers from a serious infectious disease called Panleukopenia. The treatment consists of serum therapy, probiotics and intravenous antibiotics, monitoring her appetite and checking her antibodies until she recovers and gets the necessary vaccine to return home so we can continue monitoring her. As a result, she remains hospitalized, but has been transferred to the infected animals area. This has generated another cost. She needed other tests, specific foods and special care and will need it until her health improves. We will not give up on her life. We are fighting with all our strength, and we count on the help and may God touch the hearts of everyone who can strengthen us in this difficult time. The disease is curable, all we need is intensive and correct treatment.
We are counting on the recovery and healing of our Princess Leia 🤍
tips and donations at ko-fi (or if you prefer sent me paypal at: [email protected])
EDIT 16/03 i appreciate so much all the help and kind gesture. unfortunately, she was a warrior but the disease was too aggressive. i may have lost her on earth but she's taking care of me up above. just like her sister i also lost last week...
thank you all from the bottom of my broken heart 💗
58 notes
·
View notes
Text
Things Biden and the Democrats did, this week #22
June 7-14 2024
Vice-President Harris announced that the Consumer Financial Protection Bureau is moving to remove medical debt for people's credit score. This move will improve the credit rating of 15 million Americans. Millions of Americans struggling with debt from medical expenses can't get approved for a loan for a car, to start a small business or buy a home. The new rule will improve credit scores by an average of 20 points and lead to 22,000 additional mortgages being approved every year. This comes on top of efforts by the Biden Administration to buy up and forgive medical debt. Through money in the American Rescue Plan $7 billion dollars of medical debt will be forgiven by the end of 2026. To date state and local governments have used ARP funds to buy up and forgive the debt of 3 million Americans and counting.
The EPA, Department of Agriculture, and FDA announced a joint "National Strategy for Reducing Food Loss and Waste and Recycling Organics". The Strategy aimed to cut food waste by 50% by 2030. Currently 24% of municipal solid waste in landfills is food waste, and food waste accounts for 58% of methane emissions from landfills roughly the green house gas emissions of 60 coal-fired power plants every year. This connects to $200 million the EPA already has invested in recycling, the largest investment in recycling by the federal government in 30 years. The average American family loses $1,500 ever year in spoiled food, and the strategy through better labeling, packaging, and education hopes to save people money and reduce hunger as well as the environmental impact.
President Biden signed with Ukrainian President Zelenskyy a ten-year US-Ukraine Security Agreement. The Agreement is aimed at helping Ukraine win the war against Russia, as well as help Ukraine meet the standards it will have to be ready for EU and NATO memberships. President Biden also spearheaded efforts at the G7 meeting to secure $50 billion for Ukraine from the 7 top economic nations.
HHS announced $500 million for the development of new non-injection vaccines against Covid. The money is part of Project NextGen a $5 billion program to accelerate and streamline new Covid vaccines and treatments. The investment announced this week will support a clinical trial of 10,000 people testing a vaccine in pill form. It's also supporting two vaccines administered as nasal sprays that are in earlier stages of development. The government hopes that break throughs in non-needle based vaccines for Covid might be applied to other vaccinations thus making vaccines more widely available and more easily administered.
Secretary of State Antony Blinken announced $404 million in additional humanitarian assistance for Palestinians in Gaza, the West Bank and the region. This brings the total invested by the Biden administration in the Palestinians to $1.8 billion since taking office, over $600 million since the war started in October 2023. The money will focus on safe drinking water, health care, protection, education, shelter, and psychosocial support.
The Department of the Interior announced $142 million for drought resilience and boosting water supplies. The funding will provide about 40,000 acre-feet of annual recycled water, enough to support more than 160,000 people a year. It's funding water recycling programs in California, Hawaii, Kansas, Nevada and Texas. It's also supporting 4 water desalination projects in Southern California. Desalination is proving to be an important tool used by countries with limited freshwater.
President Biden took the lead at the G7 on the Partnership for Global Infrastructure and Investment. The PGI is a global program to connect the developing world to investment in its infrastructure from the G7 nations. So far the US has invested $40 billion into the program with a goal of $200 billion by 2027. The G7 overall plans on $600 billion by 2027. There has been heavy investment in the Lobito Corridor, an economic zone that runs from Angola, through the Democratic Republic of Congo, to Zambia, the PGI has helped connect the 3 nations by rail allowing land locked Zambia and largely landlocked DRC access Angolan ports. The PGI also is investing in a $900 million solar farm in Angola. The PGI got a $5 billion dollar investment from Microsoft aimed at expanding digital access in Kenya, Indonesia, and Malaysia. The PGI's bold vision is to connect Africa and the Indian Ocean region economically through rail and transportation link as well as boost greener economic growth in the developing world and bring developing nations on-line.
#Thanks Biden#Joe Biden#us politics#american politics#Medical debt#debt forgiveness#climate change#food waste#Covid#covid vaccine#Gaza#water resources#global development#Africa#developing countries
185 notes
·
View notes
Text
What do GPs do?
For the past few years, there's been a constant undercurrent of hostility towards the medical field in mainstream media, particularly GPs. Especially from certain conservative former doctors who write in to the Torygraph.
One of the charges levelled against GPs is that they are purpotedly ruining the NHS by not working enough hours. They need to be making more time for appointments and are all shirking.
How do GPs work?
GP work is measured in sessions, defined by the BMA as a 4h 10 minute time slot. 3 hours of this is meant to be clinical time, with some admin time for tasks - meant to be at least and hour. Typically, a whole day will involve a session in the morning and a session in the afternoon.
What do GPs do? The BMA breaks it down here. I also find articles by GPs can be useful for explaining. When not talking to patients, we are sending referrals or liaising with specialists about their care. We are checking blood test results and other investigations that were carried out by the practice, and then informing patients. We are filling prescriptions- each time a patient asks for their prescription to be refilled, a doctor or pharmacist is checking the order and whether it is safe to give, abd whether we are monitiring blood tests and keeping the patient safe. We are reading letters from specialists and actioning their recommendations.
However, in reality, multiple surveys reveal that GPs spend significantly more time working than what they are directly paid for. Whilst a 6 session GP should be spending around 24 hours at work, it's closer to 38 hours on average. GPs report spending up to 40% of their working time on admin - much of it being unpaid time outside of the hours they are contractually hired for. I and most GPs I know routinely stay late at work in order to make sure patient care is completed. We're in before 9am and leave between 7 or 8pm.
Add to that that many might have further responsibilities, especially if they are a partner in the practice.
Funnily enough, full time in general practice is considered to be 8 sessions. That's 4 long days. Gone are the days when anyone would consider a 5 day working week for GPs, because the workload is increasingly intense and sessions generate more paperwork than they used to.
Demand Is Increasing
GPs may be moving towards working less sessions, but that's because our work is getting more complex. As patients live longer, with more complicated combinations of illnesses and treatments, and we exist in a society that has progressively defunded social care and benefits, and impoverished our most vulnerable patients, there are more calls on our time abd attention than ever before. Stripped hospital services are increasingly rejecting our referrals, often inappropriately and against actual guidelines. Services are being pushed onto GPs via shared care agreements that would once have been handled by specialist teams in clinic. Services that we heavily rely on to serve our patients are sometimes defunded or disappear as contracts end or are transferred to new providers. Long wait lists lead to exasperated patients repeatedly seeing their GPs to manage issues that can't be managed well in the community.
There's a narrative in the media that appointments are impossible to get, but in reality, nationally GP surgeries are providing more appointments per month than they did before the pandemic. For example, 25.7 million appointments (excluding Covid vaccinations) were delivered by GP practices in December 2023, an increase of 9% compared to pre-pandemic. Practices are trying to find how to offer more appointments on a budget and how to improve access and find alterantive ways to serve patients; for example online forms, so that phone lines are freed up for vulnerable patients. Many practices are also offering longer appointments as many patients have complex needs.
Let's talk Pay
People also assume GPs are rich, but that's not really the case, especially given most of us wrent working full time. Average pay for a session is somewhere between 10k and 12k a year for each session a week that you work, depending on things like seniority and location. So for example, a 5 session GP earning 10k per session can expect to earn 50k a year. That's barely above the London average salary of 44k for a job that requires medical school, often an additional bachelor's degree and then at least 5 years of postgraduate training at minimum. That's more comfortable than a lot of vulnerable people, but it's nowhere near what most people think. Even if someone is paid higher per session and working more sessions, the average is still closer to 80 or 90k for salaried GP roles.
I've found figures that suggest the average GP salary is just over 100k, but that includes people doing separate private work or being partners, where in reality these are different roles that are paid differently. Partners are effectively shareholders in the practice. Locum or private work is much more lucrative and needs to be considered separately from a standard salaried role.
Some Partners may be earning £100k-150 in a good year, but that will be after working a LOT of overtime outside of their clinics, abd is in line with hospital specialists. The proportion of GPs earning more than that are miniscule. And honestly, if someone is working a ton of extra hours with their local LMC or med school or deanery, or doing a ton of locum work in evenings and weekends, I'm happy for them to be earning more money than me. Extra work and hours should be rewarded.
The Gender Aspect
I think we need to address the fact that complaining about doctors choosing to work less than what is defined as full time, often goes hand in hand with people complaining about women having the temerity to work in medicine. Apparently we're devaluing the profession by making it too female, going part time and having children. Why us ut that nobidy cares about whether men are going less than full time to look after their kids, and whether fathers are missing out on their children's upbringing?
As women, many of us are still facing sexism in our working lives. Whilst still having to deal with the fact that even uf we earn more and work longer hours than our menfolk, we usually end up doing the majority of the childcare and housework. Women in medicine are more likely to go less than full time because we are more likely to feel compelled to take on unpaid labour at home. Like our non medical sisters.
For reference, the full time nursing week in the NHS is 37.5h - with some variation between 36-40h depending on where you work. Working part time would benefit nurses, too. The nursing workforce is mostly women, and yet there's not the same outrage about their working hours or going less than full time, because women being nurses is expected. People don't seem to care about nurses' working conditions or the stresses they are under, and honestly most articles ignore the financial stresses or difficulties of most NHS workers because they are normally focused on doctors as a resource that they want to exploit maximally.
We aren't out there trying to police what hours other professions work - or at least, we shouldn't be. So why does the public feel entitled to dictate what hours doctors should be working? It's not like people are being paid for hours they aren't working!
#dxlives#dx lives#nhs#healthcare#gp#general practice#been meaning to get back into rabting#long post#gp pay#medicine#med student#junior doctor
71 notes
·
View notes
Text
Yes, there's hope in the fight against Long Covid.
Hope doesn't come in the form of natural immunity or subpar vaccines rolled out after waves of illness have already peaked. It comes in the form of clean indoor air, widespread masking, and better treatments. In that vein, the NIH is finally launching a new batch of clinical trials focused on Long Covid, five total, dedicated to different aspects of the condition. Institutes like Mount Sinai are running clinical trials on repurposed HIV drugs. So is HealthBio, a startup working on immune diseases. (They're testing maraviroc and atorvastatin.) Post-Viral Trials News is sharing updates as they roll in. Of course, the NIH and FDA need steady pressure to make sure they're funding trials that focus on a range of options. Given the urgency of the crisis, we should be doing far more. As Harvard economist David Cutler has said on developing treatments for Long Covid, "There is no amount that's overdoing it." We're talking about a $16 trillion crisis.
We're talking about an urgent need for dozens of expedited clinical trials for drugs that already exist, which have shown effectiveness in preventing and treating Long Covid in its various incarnations. We're talking about making those drugs accessible right now for off-label use, so that Covid survivors can finally get the help they need.
Long Covid is an emergency.
We're going to talk about prescription treatments first, and then supplements and extracts you can find yourself. Up front, you can try services like RTHM and CURE ID that aim to connect patients with treatments without endless waits. (I'm not endorsing them. I'm just telling you they exist.)
Let's dig in.
Healthcare largely abandoned monoclonal antibodies during the first Omicron wave, but some of them remain effective in higher doses as postviral therapies. We've also found new ones. For example: A study in Nature offers 5B8 as a therapy for fibrinogen, a protein in your body that binds to the Covid spike protein during infection. Afterward, that protein starts to behave differently, "forming pro-inflammatory blood clots" that lead to cardiac and brain dysfunction, especially in young patients with mild infections. It also suppresses your natural killer cells, weakening your immune system. So, damaged fibrinogen is the culprit behind a lot of the "mysterious" health problems we're seeing.
As the authors show, "fibrin-targeting immunotherapy may represent a therapeutic intervention for patients with acute Covid-19 and Long Covid." The monoclonal antibody 5B8 "provides protection...without adverse effects." The sooner you get it, the better it works.
A 2024 study in the American Journal of Emergency Medicine also found that the monoclonal antibody regeneron helped Long Covid survivors recover. Researchers "expressed surprise at the swift and comprehensive improvements observed in the patients," adding that "regardless of the duration of their Long Covid experience, significant progress was noted within a mere 5 days of receiving the Regeneron treatment." It might work because it helps your immune system eliminate residual amounts of virus or viral fragments, or it might replace damaged antibodies that attack your cells.
A 2022 study found that another monoclonal antibody, Sotrovimab, helped survivors with persistent viral loads after initial infection who were still reporting fatigue, chest pain, and trouble breathing months after infection. As the researchers note, the patients showed "rapid improvement of symptoms and inflammation markers as well as negative swabs."
Yet another 2022 study in Clinical Infectious Diseases found that a monoclonal antibody treatment called Leronlimab could help Long Covid patients recover by boosting their immune system in cases where Covid downregulated it, causing a drop in their CCR5 levels, a receptor found on a range of cells that fight pathogens, including your CD4 lymphocytes.
The Long Covid Action Project is also developing a list of drugs that desperately need clinical trials and faster deployment. They stress the need for monoclonal antibodies and antivirals like pemivibart, azvudine, ensitrelvir (Xocova), and sofosbuvir. They'll be releasing a full list later this year.
So while these monoclonal antibodies might not save your life during early infection, they can help your recovery.
There should be more clinical trials and off-label use.
Interferon treatments, specifically Interferon-Lambda, have shown the potential to help with immune system problems and cognitive deficits (caused by brain inflammation) after Covid infections.
Also:
A 2022 study in Frontiers in Immunology found that high doses of immunoglobulin have shown "a significant to remarkable clinical benefit" in treating a full range of brain, heart, and lung problems in Long Covid patients. A major 2023 study in Frontiers in Neuroscience confirmed that immunoglobulin lead to significant improvement in neurological problems. As researchers in a third study on immunoglobulins and Long Covid state, we already use this therapy to treat a variety of chronic inflammatory diseases, as well as flu, HIV, and measles. (The NIH has included immunoglobulins in their new clinical trials.)
HIV drugs have also shown promise for helping Long Covid patients. A 2023 study in Clinical Infectious Diseases found that Tenofovir reduced someone's Covid risk regardless of whether they had HIV. A range of studies have supported the use of Tenofovir, Darunavir Ethanolate, and Azvudine for Covid. As we noted earlier, clinical trials are currently testing HIV drugs for Long Covid.
Another study in Antiviral Research found that cobicistat, used to boost HIV antivirals, also fights Covid and leads to a significant reduction in overall risk. The researchers found that higher doses work better. They also found that higher doses work better for ritonavir, one of the key components of Paxlovid. By the way, ritonavir has been used in HIV treatments since the mid-1990s.
The research on repurposed HIV drugs points to the potential of many antiretroviral therapy (ART) medications for Long Covid, given that viral persistence plays a large role in most cases.
When you consider that Paxlovid itself contains an HIV antiviral, it sounds a little less extreme to compare Covid to HIV and discuss repurposing existing drugs.
Finally, studies have shown that molnupiravir and metformin have shown effectiveness against Covid. In particular, a 2024 study in Clinical Infectious Diseases found that metformin prescribed in the early stages of a Covid infection led to a 41 percent drop in Long Covid risk.
Other research has revealed that sometimes it takes a combination of these drugs to help patients recover. In a 2022 study in Clinical Infectious Diseases, researchers used nanopore technology to identify the specific variants patients were infected with and select the most effective treatments for that variant. In one case, a Long Covid patient with severe Paxlovid rebound only got better after doctors prescribed Paxlovid again and added remdesivir. Nobody had thought to try that yet.
It worked.
These are the drugs that demand renewed attention and clinical trials, given that most research on Long Covid points to ongoing infection, viral persistence, and the disruption of your immune system, which could mean a downregulated or weakened immune system or an overactive one. We especially need clinical trials that match drugs with specific conditions.
Specialists are going to decide the right dose for prescription drugs. Generally, the research indicates that if a standard dose doesn't work, a higher dose might as long as it doesn't trigger side effects. A combination of drugs can work when a single drug fails.
What can you do if you don't have access to these drugs?
This:
A major 2023 study in Cells found that eriodictyol, a flavonoid extracted from yerba santa, can help with the brain inflammation caused by Covid infections that leads to cognitive deficits and fatigue. Researchers have found that at least part of the "brain fog" from Long Covid happens when the virus triggers immune cells to attack the brain. Eriodictyol can also be derived from citrus fruits, tomatoes, and grapes. As the authors explain, a range of flavonoids "have been reported to prevent neuroinflammation, provide neuroprotection, and reduce cognitive dysfunction, especially brain fog."
The authors of the Cell study list flavanoids liposomal luteolin, oleuropein, and sulforaphane as all beneficial for recovering brain function. They identify formulas called BrainGain and FibroProtek containing flavonoids that helped Long Covid patients with severe brain fog in previous studies. Those contain luteolin. They ultimately recommend ViralProtek, which combines several flavonoids, "alone or together" with eriodictyol.
These formulas aren't just managing symptoms. According to the studies, they're helping you clear viral remnants and rehabilitate your immune system. They inhibit your microglia and mast cells, immune cells that often drive the brain inflammation behind Long Covid cognitive problems.
What else?
A 2022 study in Molecules found promise in nattokinase, "a popular traditional Japanese food made from soybeans fermented by Bacillus subtilis var." Not so coincidentally, nattokinase also "decreases the plasma levels of fibrinogen," the same protein that drives thrombosis in Long Covid patients and indeed "has drawn central attention in thrombolytic drug studies," as well as tumor treatment. It also inhibits the replication of bovine herpes virus. Clinical trials have found no adverse effects from eating natto. In this particular study, the researchers found that nattokinase degrades the Covid spike protein, inhibiting infection. As they conclude, "nattokinase and natto extracts have potential effects on the inhibition of SAS-cOv-2 host cell entry."
Martha Eckey describes natto extracts in more detail here, along with benefits, recommended dosage, and possible side effects. Respondents to her survey reported the best results when they took Solaray's natto extract along with serrapeptase, an enzyme and commonly used drug in Japan and Europe that helps your body break down proteins. A large number of patients reported improvement after taking the natto-serra combination, often within a week or two. Many of them also benefited from adding lumbrokinase, an enzyme shown to facilitate healing.
Like natto, lumbrokinase breaks down fibrin. We're seeing a theme here. Any kind of treatment that breaks down fibrin, whether it's a monoclonal antibody or an enzyme, helps after a Covid infection.
Take a look for yourself:

Eckey discusses cromolyn for brain inflammation and neurological issues, and some people have said it helps with other problems. She also wrote this great post about protecting kids from Long Covid.
A lot of it also applies to adults.
Another surprising study in Viruses from 2021 found that grapeseed extract (V. vinifera) contained dozens of flavonoid compounds that inhibited viral replication, including for Covid. The researchers used concentrations from 500 μg/ml down to 10 μg/ml.
Studies have even found that taurine supplements can do a lot to reduce your Covid risks, including Long Covid. A 2024 study in PLoS One found that the amino acid can serve as both a biomarker and a target for treatment in Long Covid. As they write, taurine has already "shown benefits such as reducing depressive behavior, improving memory, and mitigating age-related issues by addressing cellular senescence, chronic inflammation, DNA damage, and mitochondrial dysfunction." It can play "a potential protective role" in "alleviating the burdens of PCC." If that weren't enough, "taurine supplementation has demonstrated diverse therapeutic properties, including anti-oxidation, anti-aging, antiepileptic, cytoprotective, and cardioprotective effects in many diseases." Yes, even taurine from energy drinks. (And I guess it's a good thing I drink them.)
A standard diet contains about 40-400 mg of taurine per day. Medical use often starts at 6 grams a day.
There's a reason why many of these treatments don't get the attention they deserve, and Timothy Ferriss of all people describes it very well in the opening to The 4-Hour Body. As he learns from talking with a wide range of doctors and medical researchers, the industry frowns on any kind of treatment that doesn't look or feel "elite" enough. There's not a lot of incentive for major research on supplements or cheap, widely available drugs because they're just not cool enough, even if they work. For drug makers, it can't just work. It also has to generate enough profit.
That's what happens when you privatize medicine.
As a society, we have to overcome that. This shortcoming isn't going to help us address the myriad public health challenges of the future.
It's a little ironic that the catchphrase "do your own research," once levied against anti-vaxxers, is now used to insult Long Covid survivors and advocates who are trying desperately to find treatments. The difference is that we're not rejecting medicines.
We're simply not getting them.
This article can't replace a doctor or a nutritionist, but it offers a comprehensive starting point for anyone who needs it. You can do more digging and confirm what's here. You could also just make a list of all the things discussed here and take them to someone you trust, and go from there.
It's crucial for us to develop a range of treatments and therapies for Covid that go beyond the mainstream reliance on Paxlovid and vaccines, conveniently dominated by a single pharmaceutical company.
It won't last forever.
In fact, research has shown that Paxlovid leads increasingly to rebound infections in which "the virus can return unimpeded by the drug, bringing the risk of disease and even death."
That's the part left out by corporate media. Rebound doesn't simply mean another round of Paxlovid. It means decreased effectiveness.
It means evasion.
Just like our mediocre vaccines, Covid is developing resistance to Paxlovid. According to an article in Nature, researchers around the world are now quietly racing to develop alternatives. No doubt, viral evolution offers one of the unspoken reasons why many of us find it so hard to access the drug now. The elites are terrified of losing the thing that enables their denial and wishful thinking.
Here's what one researcher said:
“This type of approach helped to improve HIV drugs, and we think it’s a good way to improve antivirals against SARS-CoV-2,” says Sho Iketani, PhD, assistant professor of medical sciences at Columbia University’s Vagelos College of Physicians and Surgeons and Aaron Diamond AIDS Research Center, who co-led the research..."
Western countries are well behind the curve on these fronts. Japan now offers a drug called Xocova (ensitrelvir), arguably more effective than Paxlovid, and it's been sitting in the FDA approval queue for about a year. China approved HIV antivirals for Long Covid back in 2022. While some healthcare workers in Europe and North America know about combining and repurposing drugs, many of them are still busy pretending Covid is over.
It's time for government agencies to pull their heads out of the sand and do their jobs. If there had been more urgency over the last four years, and less favoritism toward one or two drug giants, we would already have these treatments deployed. As things stand, we need leaders to not only run these long overdue clinical trials but also prepare to scale up production considerably, while making sure that everyone has access, not just those with platinum insurance plans. We could already be doing that for emergency off-label use now. Why aren't we?
Although it's infuriating and demoralizing it took us so long to get here, it's encouraging to know that teams of scientists around the world have been working on this crisis and producing results. We just need the gates unlocked.
There's no time to waste.
Let's get moving.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator
135 notes
·
View notes