#ibd disease treatment
Explore tagged Tumblr posts
Text
Best Gastroenterologist in Pune - Dr. Vikrant Kale
If you are looking for the best gastroenterologist in Pune? Dr. Vikrant Kale is a practicing consultant Gastroenterologist, Hepatologist, and Interventional Endoscopist with experience of more than 17 years. At present, he is the Director & Head of the Department of Medical Gastroenterology at the Kaizen Gastro Care Clinic, PCMC, Pune. He has expertise in managing various GI disorders (which include intestine, liver, gallbladder, and pancreas) at a very advanced level.
#Gastroenterologist#Liver Specialist#Stomach Specialist#Interventional Endoscopist#Crohn's and Colitis Specialist#Crohn's Disease treatment#IBD Disease treatment#Ulcerative Disease Treatment
0 notes
Text
Understanding IBD and IBS: Symptoms, Diagnosis, and Management
Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) are two distinct gastrointestinal disorders that, despite sharing similar symptoms, differ significantly in their causes, diagnostic approaches, and treatment strategies. IBD encompasses chronic inflammatory conditions like Crohn's disease and ulcerative colitis, which cause visible inflammation and damage to the gastrointestinal tract. In contrast, IBS is a functional disorder characterized by symptoms such as abdominal pain, bloating, and altered bowel habits without any detectable inflammation or structural abnormalities. For expert advice and treatment, it’s best to visit an experienced IBD IBS specialist in Hyderabad like Dr. N Subrahmaneswara Babu, one of the top medical and surgical gastroenterologists in Hyderabad at Apollo Hospitals and EVOKE Clinics.
Symptoms and Diagnosis
IBD symptoms often include persistent diarrhea, abdominal pain, weight loss, fatigue, and blood in the stool. Diagnosis typically involves a combination of blood tests, stool tests, endoscopic procedures, and imaging studies to assess inflammation and rule out other conditions. IBS, on the other hand, presents with recurrent abdominal discomfort, bloating, and changes in bowel habits, such as constipation or diarrhea. Diagnosis is primarily based on symptom patterns and the exclusion of other gastrointestinal diseases, as there are no specific tests to confirm IBS.
Management Strategies
Managing IBD often requires a comprehensive approach, including anti-inflammatory medications, immunosuppressants, biological therapies, and sometimes surgical interventions to remove damaged portions of the digestive tract. Lifestyle modifications, such as dietary changes and stress management, also play a crucial role. For IBS, treatment focuses on symptom relief through dietary adjustments (like a low FODMAP diet), fiber supplementation, antispasmodic medications, and psychological therapies to address stress and anxiety, which can exacerbate symptoms.
Expert Care in Hyderabad
For individuals seeking specialized care in Hyderabad, Dr. N. S. Babu stands out as a leading Surgical Gastroenterologist with over 15 years of experience in treating complex gastrointestinal conditions, including IBD and IBS. His expertise in advanced laparoscopic and robotic surgeries ensures comprehensive care for patients requiring surgical intervention. Dr. Babu's practice at Hills Gastrocare is dedicated to providing personalized treatment plans tailored to each patient's unique needs.
#Best gastroenterologist in Hyderabad#IBS treatment in Hyderabad#IBD specialist doctor in Hyderabad#Top GI surgeon in Hyderabad#Laparoscopic gastro surgeon Hyderabad#Gastro hospital in Hyderabad#Best digestive disorder doctor in Hyderabad#Crohn’s disease treatment in Hyderabad#Ulcerative colitis specialist in Hyderabad#Gastroenterology clinic in Secunderabad#IBS and IBD difference#Best surgeon for stomach problems in Hyderabad#Dr. N.S. Babu gastroenterologist reviews#Advanced IBD treatment in Hyderabad#Laparoscopic surgery hospital in Hyderabad.
0 notes
Text
Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain.
Peptic ulcers include:
Gastric ulcers that occur on the inside of the stomach
Duodenal ulcers that occur on the inside of the upper portion of your small intestine (duodenum)
The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
#Liver Disease Treatment in Navi Mumbai#Best Gastroenterologist in Navi Mumbai#Stomach Specialist in Navi Mumbai#Gastro Specialist in Navi Mumbai#Best Piles Doctor in Navi Mumbai#Peptic ulcer disease treatment doctor in Navi Mumbai#Crohn Disease specialist in Navi Mumbai#IBS Specialist in Navi Mumbai#IBD Specialist in Navi Mumbai#Ulcerative colitis specialist in Navi Mumbai
0 notes
Text

Inflammatory Bowel Disease (IBD) Treatment in Ahmedabad
Manage IBD with care and precision under expert guidance. Dr. Jigar Patel offers diagnosis and treatment for both Crohn’s disease and ulcerative colitis. Services: Colonoscopy, medication plans, symptom monitoring, flare-up management
#IBD Treatment#Crohn’s Disease#Ulcerative Colitis#GI Specialist#Colonoscopy#Intestinal Inflammation#Digestive Doctor#Gut Disorders#Ahmedabad GI#Bowel Health
0 notes
Text
Living with inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis can be difficult. Crohn’s disease and ulcerative colitis are chronic inflammatory conditions that affect the gastrointestinal tract. While medical management is the first line of treatment, some patients may need surgical intervention to manage severe symptoms, complications, or medication resistance.
#IBD treatment#IBD specialist#Ulcerative colitis specialist#Crohn's Disease Treatment#Gastroenterologist#Stomach Specialist
0 notes
Text
youtube
#Ulcerative colitis#immune cell infiltration#small molecule compounds#chronic inflammation#gut health#immune response#inflammatory bowel disease#mucosal healing#colon inflammation#autoimmune diseases#precision medicine#targeted therapies#immunotherapy#microbiome and health#novel treatments#drug development#patient outcomes#UC research#clinical innovation#IBD treatment.#Youtube
0 notes
Text
#Inflammatory Bowel Disease symptoms#when to see a gastroenterologist#IBD diagnosis#Dr. Vatsal Mehta#best gastroenterologist Ahmedabad#gastroenterologist Ahmedabad#IBD treatment#gastroenterologist
0 notes
Text
Charting Your Course: A Deep Dive into Personalized Treatment Plans for IBD
Living with Inflammatory Bowel Disease (IBD) can feel like navigating a stormy sea without a map. The unpredictable flares, the persistent discomfort, the emotional toll – it’s a journey that demands resilience and a tailored approach. In this in-depth guide, we’ll embark on an exploration of IBD, unravel the complexities of personalized treatment plans, and equip you with the knowledge and tools…
0 notes
Text
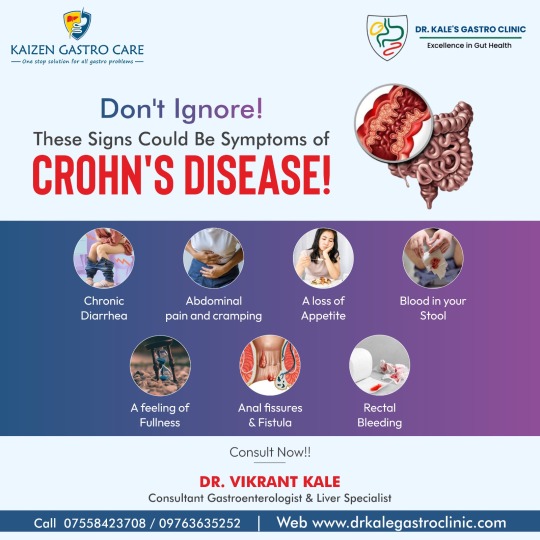
If you're experiencing any of the symptoms of #CrohnsDisease, OR If you have symptoms that aren't going away, feel free to Consult the experienced #IBD specialist, Dr. Vikrant Kale, and get expert advice today.
Early diagnosis and treatment are essential for managing Crohn's disease and improving your quality of life.
#Crohn's Disease Treatment#Crohn's Disease specialist#IBD specialist#IBD treatment#Gastroenterologist
0 notes
Text
#Liver Disease Treatment in Navi Mumbai#Best Gastroenterologist in Navi Mumbai#Stomach Specialist in Navi Mumbai#Liver Disease Treatment in Mulund#Best Gastroenterologist in mulund#Stomach Specialist in Mulund#Liver Disease Treatment in chembur#Best Gastroenterologist in chembur#Stomach Specialist in chembur#Peptic ulcer disease treatment doctor in Navi Mumbai#IBS Specialist in Navi Mumbai#Crohn Disease specialist in chembur#IBD Specialist in chembur#Ulcerative colitis specialist in Mulund#Best Piles Doctor in mulund.#Constipation treatment in mumbai#Constipation treatment in Navi Mumbai#Best doctor for loose motions in mumbai#Best doctor for loose motions in Navi mumbai
0 notes
Text
It took me nearly 15 years to get my endometriosis diagnosis and comprehensive treatment, but I recognize I’m super privileged in being able to access care where I live from one of the top doctors in endometriosis research(specifically endometriosis in adolescents, but his research spans all age groups). I want to share some of the things I learned, along with study sources he linked me to, so others can advocate to their providers for the care they need. So without further ado:
✨ What I Wish I Knew About Endometriosis 15 Years Ago ✨
No amount of pain is “normal”
Don’t get gaslit into thinking “everyone” who has periods goes through pain. Seek treatment - you deserve better.
Diagnosis/treatment is kinda a pain, even with a doc who takes you seriously
The general course of action for diagnosis/treatment will be attempt treatment through OTC painkillers (Tylenol, Midol, etc), attempt at least 1-2 forms of hormonal birth control(typically oral contraceptive/birth control pill or the ring/patch/shot), then decide with your doctor whether to pursue either further hormone treatments, such as GnRH(which suppress estrogen/can help stop progression of endo) or an IUD, and/or surgical intervention where they go in and find/remove the existing lesions.
Surgery for me took a couple hours, and I had an IUD placed during the operation(at recommendation of my doc). Full recovery was around 2 weeks. Its worth noting right now you can technically only be diagnosed through surgery.
You may have to mix-and-match to find the right solution.
Only 33% of people with endometriosis in a recent controlled study saw significant improvement by IUD alone, as compared to IUD with supplementary hormonal treatment(like oral birth control or hormone inhibitors). Source: https://www.sciencedirect.com/science/article/abs/pii/S1083318812002379
Some options may actually make it worse. Keep an eye on your symptoms.
Studies show that estrogen based treatments can potentially exacerbate endometriosis and promote endometrial growth, so treatments without estrogen or with specific types of estrogen are more recommended. Source: https://pmc.ncbi.nlm.nih.gov/articles/PMC5683134/
Its Got Hella Comorbidities
Fibromyalgia, scoliosis, arthritis, thyroid disease, migraines, chronic fatigue, and bowel disease(IBS, crohn’s, celiac, etc), and more are all potential associations/comorbitities. It’s also worth noting that having any of these in your family history may also put you at higher risk for endo. As my doc said - you’re not guaranteed to get all, or even any, of these, but they’re things to keep an eye out for. Sources:
IBS: https://pmc.ncbi.nlm.nih.gov/articles/PMC9357916/
IBD/Crohns: https://pubmed.ncbi.nlm.nih.gov/32629225/
Celiac: https://pubmed.ncbi.nlm.nih.gov/24992792/
Thyroid: https://pmc.ncbi.nlm.nih.gov/articles/PMC10234359/
Migraine: https://pubmed.ncbi.nlm.nih.gov/38436302/
Painful Bladder Syndrome: https://pmc.ncbi.nlm.nih.gov/articles/PMC3015716/
EDS: https://www.sciencedirect.com/science/article/abs/pii/S0002937824001637
Arthritis: https://pubmed.ncbi.nlm.nih.gov/35258592/
Scoliosis: https://pubmed.ncbi.nlm.nih.gov/9238674/
TMJ: https://pmc.ncbi.nlm.nih.gov/articles/PMC10144081/
Kidney Stones: https://pmc.ncbi.nlm.nih.gov/articles/PMC9108729/
POTS: https://pmc.ncbi.nlm.nih.gov/articles/PMC3413773/
Fibromyalgia: https://pubmed.ncbi.nlm.nih.gov/30682223/
Chronic Fatigue: https://pmc.ncbi.nlm.nih.gov/articles/PMC6537603/
Sjogren’s Syndrome: https://pubmed.ncbi.nlm.nih.gov/39083399/
Bonus Advice
No published studies exist showing any increase/decrease of symptoms between usage of different menstrual products. Do whatever makes you most comfortable!
For OTC pain management, Tylenol or Aleve may be your best bets over Advil, based on their anti-inflammatory nature.
He also recommended probiotics pretty heavily, since digestive issues(ie bad period poops) are super common. Any with >10Bn active cultures are good!
(Disclaimer: I am not a doctor, just someone that learned a lot and wants to share)
490 notes
·
View notes
Text
Piles, also known as hemorrhoids, are swollen veins in the lower rectum and anus that cause pain, itching, and discomfort. This condition affects a significant number of individuals, often due to factors like a sedentary lifestyle, unhealthy diet, chronic constipation, or even genetic predisposition. If you’re dealing with painful or persistent piles, finding the right specialist is crucial for effective treatment and long-term relief. Dr. Vasudev, known as the best piles doctor in Mulund, is dedicated to offering compassionate, expert care for this common yet often distressing condition.
#Liver Disease Treatment in Mumbai#Best Gastroenterologist in Mumbai#Stomach Specialist in Mumbai#Gastro Specialist in Mumbai#Best Piles Doctor in Mumbai#Peptic Ulcer Disease Treatment Doctor in Mumbai#Crohn Disease Specialist in Mumbai#IBS Specialist in Mumbai#IBD Specialist in Mumbai#Ulcerative colitis Specialist in Mumbai#Liver Disease Treatment in Navi Mumbai#Best Gastroenterologist in Navi Mumbai#Stomach Specialist in Navi Mumbai#Gastro Specialist in Navi Mumbai#Best Piles Doctor in Navi Mumbai#Peptic ulcer disease treatment doctor in Navi Mumbai#Crohn Disease specialist in Navi Mumbai#IBS Specialist in Navi Mumbai#IBD Specialist in Navi Mumbai#Ulcerative colitis specialist in Navi Mumbai#Liver Disease Treatment in chembur#Best Gastroenterologist in chembur#Stomach Specialist in chembur#Gastro Specialist in chembur#Best Piles Doctor in chembur#Peptic ulcer disease treatment doctor in chembur#Crohn Disease specialist in chembur#IBS Specialist in chembur#IBD Specialist in chembur#Ulcerative colitis specialist in Chembur
0 notes
Text

IBD Treatment in Ahmedabad- Dr. Jigar Patel
Dr. Jigar Patel provides specialized treatment for Inflammatory Bowel Disease (IBD) in Ahmedabad, offering expert care to manage and improve digestive health.
#IBD Treatment Ahmedabad#Inflammatory Bowel Disease Care#Dr. Jigar Patel IBD Specialist#Ulcerative Colitis Treatment Ahmedabad#Crohn’s Disease Specialist Gujarat#Digestive Health Expert Ahmedabad#Advanced IBD Solutions Gujarat#Trusted Gastroenterologist Ahmedabad#Chronic Bowel Disorder Treatment#Personalized IBD Care Solutions
0 notes
Text
4/10/25: entire body has been achy, feeling an all over malaise and gross feeling. my joints have been aching no matter which ones. moving around too much is painful. eating hurts no matter what the food or drink is. my intestines hurt in specific spots on the lower & upper left hand side and lower right hand side and hurt more when anything passes through the affected areas. i'm tired and can't stay awake sometimes. it's hard to eat and drink enough. i've been very dehydrated. abdomen hurts no matter whether or sit, stand or lay down. i can find less painful angles but at this point everything hurts. food is a total gamble, i have no idea if its going to hurt my intestines or not.
that's the worst part, is the pain in centered in my intestines, which is why people don't want to take it seriously. it's in the "gross" part of my GI system. nausea isn't really that big of a problem for me. i'm having issues relating to going to the bathroom, and that's a huge issue. i was told i had IBS 3 years ago and put on IBS meds and told how to treat IBS. my condition has worsened steadily over that time. none of it has helped. IBS is a bunch of very serious health conditions that can really ruin someone's quality of life and health in general. however, i am not experiencing IBS, i'm experiencing IBD.
crohn's disease falls under an umbrella of GI & autoimmune health disorders called inflammatory bowel diseases. this is NOT the same as IBS- that is irritable bowel syndrome. IBS can be very painful, disabling and serious in its own right, but that is simply just not what i am experiencing. IBS and IBD are not the same health conditions, they are caused by very different methods of action and affect people in different ways. they are not the same and it's exhausting to receive incorrect treatment that doesn't work because of ignorance on the behalf of a medical provider. my physical therapist is also a licensed nutritionist and told me that my symptoms match up with crohn's disease and what i'm dealing with makes a lot of sense. i'm hoping that if i need to, he can help advocate for me in some manner or another.
i get to talk to a GI specialist tomorrow. after months of waiting. she observed the elevated fecal calprotectin levels as well as other issues like inflammation in my small intestine. this person isn't completely unaware of what's happening. let's hope and pray and this person gets the job done. i'm so tired of doing little else than sleeping because i'm so tired from my body struggling to get any nutrients out of what i manage to put inside of it. i can barely sit up at my chair to write this. wish me luck.
135 notes
·
View notes
Text

a couple people coincidentally reblogged my rare disease day post from [last year] so. here's how that's been going. (some of this is repeat info if you click the link)
I have mast cell activation syndrome (or MCAS), an immune disorder in which my signaling cells are way too jumpy and can trigger all kinds of symptoms (up to and including anaphylaxis) in response to seemingly harmless stimuli. this is distinct from allergies as whether or not I react to a trigger can change from day to day based on how many other triggers are present, and the chemical mediators released cover a broader spectrum than just the IgE release in a classical allergic reaction. plus oftentimes symptoms are a mix of episodic and chronic, rather than being acute episodes like allergies.
triggers can be commonly understood things like certain food ingredients or scent chemicals, but can also include things like hormone fluctuations, physical or mental exertion, and the sun. I have reacted to ginger, laundry detergent, and a natural gas furnace, for example. I also do a lot worse in summer because it is both sunny and warm, and I always have to be very careful how much energy I use up or I might trigger anaphylaxis.
it's common for people with MCAS to have some level of symptoms all their life, that go unnoticed or dismissed until some precipitating event causes a substantial downturn in their condition. for me it was mono, but other infections (especially covid) and significant stressful events have also been anecdotally reported to precipitate downturns if I recall correctly, or simply being uncontrolled enough for long enough can also snowball.
diagnostic criteria for MCAS were first proposed in 2010, so the true rarity is still very up in the air. (personally I believe a lot of common wastebin diagnoses (ibd, fibro, cfs/me, etc) should be scrutinized very carefully as potential "specialty silos" of MCAS, especially given how often they tend to travel together.)
firstline treatments for MCAS include cheap medications available over the counter like loratadine, aspirin, and famotidine. my condition has become severe enough that I'm currently on third-line treatment (omalizumab injections), which does finally seem to be getting me somewhere. (this is, of course, in addition to still taking all of the first- and second-line treatments. I take 24 units of 13 medications in a given day, it's a lot to keep track of. to the point where I'm not actually sure I've counted it correctly :v then there's my monthly injections and my emergency medications on top of that.)
(those injections btw? can cost thousands of dollars even with insurance. thankfully I'm able to use the company's assistance program, so I don't pay anything out of pocket. for that one.)
being sick is never fun, but if you have a disease perceived as rare it introduces a ton of new complications. (which get even more complicated when the disease is legit super rare!) it took me a long time to figure out what was wrong with me, and I had to do it almost entirely by myself, because doctors simply don't have the knowledge. they're not taught to look for it and there's no simple reliable test. but by yammering about it, it might make someone else's slog a tiny bit shorter <3
#kirby#needles#long post#rare disease day#mcas#mast cell activation syndrome#ask to tag#daily kirby#my art#digital#hal laboratory#nintendo
95 notes
·
View notes
Text
It's endometriosis awareness month! Here's some general knowledge on my condition, as misinformation is constantly spread about it.
Endometriosis is a disease affecting 1 in 10 people with uteruses. A tissue similar to the endometrial lining, of period blood, grows and sheds on the outside of the uterus. As the menstrual cycle comes, the blood has nowhere to go. This causes intense pain and irritation to surrounding organs. It is one of the most painful diseases recorded.
Endometriosis was first discovered in 1860, though it was recognized in the Hippocratic Corpus around 4,000 years ago. Treatments have varied through the years, starting out with bloodletting, leeches, hanging upside down, exorcisms, genital mutilation, and chemical douches. During the Middle ages, the perception of chronic pelvic pain shifted from a recognized condition to something caused by hysteria, promiscuity, or it was made up. In the hayday of Hippocratic practice, Endometriosis was more common than it is today, likely due to the inaccessibility of diagnosis compared to 4,000 years ago. Somehow.
Today, treatments include birth control, surgery, hysterectomy, and pain relief. There is no cure.
It takes an average of 7-12 years for someone to receive a diagnosis.
Anyone can get endometriosis, including cis men
A hysterectomy is not a cure, as endometriosis will continue to grow and spread to other organs
The pain one experiences due to endometriosis does not correlate with staging. Staging reveals how extensive endometriosis lesions are, not pain. Someone with stage 1 could experience excruciating pain, while someone with stage 4 and frozen pelvis can experience no pain.
Endometriosis lesions are not endometrial lining. The tissue is similar, but not the same. Thus, no one actually knows what endometriosis actually is.
It is only diagnosable through laparoscopic surgery. It can be detected via imaging such as ultrasound or MRI, but more often than not, it isn't seen. You can have completely clear tests up until your surgery and still have even the higher stages of Endo (like me!) (this one was for all you undiagnosed people, you're not crazy!)
Endometriosis is comorbid with many things, including pelvic floor dysfunction, adenomyosis, vulvodynia, uterine cancer and fibroids, ovarian cancer, many autoimmune and inflammatory conditions (rheumatoid arthritis, MS, IBD), and cardiovascular disease.
I've provided links in each point and I deeply encourage you to read my sources, whether you have endo or not. Not enough people understand endometriosis so a lot of us who deal with it don't get grace or compassion, be it in our work lives, relationships, friendships, or family. People with endo, happy endometriosis awareness month.
#endometriosis#endo#endometriosis awareness#chronic illness#disability#cripple punk#chronic pain#chronically ill#disability awareness#cpunk#endometriosis awareness month
110 notes
·
View notes