#i don’t THINK I have a fever and no other gi symptoms yet so like. i’m trying to tell myself to chill and just ignore it
Explore tagged Tumblr posts
Text
the problem with chronic illness. and compounded by constantly hearing “your labs are normal” while feeling like trash. is that when something new happens you have no perspective whatsoever on whether it’s serious or just needs ignored until it goes away. it’s great stuff.
#kit talks#like. i’ve frequently thru adulthood had sharp pains in lower right abdomen#but it has not happened much since the hysterectomy and i always assumed before it was just the endo#but it’s here again today. has popped up a couple times over the last couple months#along with increased gas#and today it’s hm. very very stabby#but i can’t tell if i should be panicking or not bc my knee and hip are fucked up and it may be radiating from my hip#or it could just be gas too. like if i hit the panic button and it’s gas that’s embarassing af#i don’t THINK I have a fever and no other gi symptoms yet so like. i’m trying to tell myself to chill and just ignore it#god i hate new mystery pains. fuck I guess it could be an ovary doing something fucky too#GOD. GOD
2 notes
·
View notes
Text
Moonlight Yearnings (1/2)
AO3 Version
Chapters: 1 | 2
Relationship: Reader/Jae-Ha
Wordcount: 2.0k
Tags: Reader is Yona AU, Mating Cycles/In Heat, Pining, Dirty Thoughts, Dirty Talk, Falling In Love, Breeding kink
Summary: Jae-Ha thinks that he’s dying. He might not actually be dying, but who is to argue semantics when it feels as though fire itself licks hungrily at his skin with every moment of existence? When hot blades of steel sink through his mind with every inhale of air?
He’s as close to death as can be without literally taking his final breath, but he's about to realize who will quell his boiling blood--the very person that caused the reaction in the first place without anyone realizing it.
You.
-
Everything is on fire . From the air that he breathes to the very skin on his body, Jae-Ha feels as if he’s submerged into a pool of lava. It comes on too quickly to be a fever and it’s not nearly as debilitating–there’s no other symptoms that would lead him to thinking that he’s sick–but he would be an utter fool to consider himself entirely healthy.
Even Yoon can’t seem to find an answer, only offering the dragon a cursory look-over and a constant pinch of his brows tight over his eyes. It’s not a look that the green dragon trusted. If the young genius of a boy couldn’t gather the faintest idea of what ailed him, then did he truly have any chance to figure it out on his own?
Suffice to say, there was little else that Jae-Ha had than simply treating the symptoms that he could and ignoring the rest–and that alone was hell.
Though he could treat the tension, the body aches and even the uncomfortable churning of his stomach, there was absolutely nothing to ease the heat burning him to the core. It clung to him like a heatwave–it felt worse than even the days he had spent out at sea with Gi-Gan and her crew, when the days were smoldering and sweat dripped down his skin. Even then he could seek comfort in the shade of the mast or even slip below deck if there was little to do.
But now?
Jae-Ha thinks that he’s dying. He might not actually be dying, but who is to argue semantics when it feels as though fire itself licks hungrily at his skin with every moment of existence? When hot blades of steel sink through his mind with every inhale of air?
So truly, he’s as close to death as can be without literally taking his final breath.
---
“I swear, Jae-Ha, I have no idea what’s causing this.”
Yoon sighs, rolling up the cloth mat of tools and herbs in a relinquishing of effort. He’s tried everything twice over in stubborn attempts to help bring the man any relief from his symptoms, but absolutely nothing seems to work. No tea, no supplement, no medicine of any type that does more than curtail what always comes back in a matter of hours.
“As far as I know you’re healthy, just…”
He trails off into silence. Jae-Ha sighs after a few moments and pinches his fingers over the bridge of his nose; at least he’s gotten better at hiding the little nuances of discomfort that plague his body. A few days ago had him seething at the end of his mental restraint, but now he’s able to take most waves of searing heat in stride even as it all but rolls through his body like scorching lava.
“Don’t worry about it then,” he says at last, moving to his feet so sharply that he doesn’t miss the way Yuun flinches back from him. “Better to let it run its course than to keep using up what few medicinal resources we have right now.”
“But aren’t you in pain?”
Jae-Ha considers himself for a moment. Each breath is even, as easy to take in as any other, but yet each inhale feels like he’s pulling smoke into his lungs, the scent branding his thoughts so deeply that he can’t think about anything other than the sensations that plague his body. But where is it coming from?
“No,” he finally lies, brushing off both concern and a lock of hair that had fallen over his eyes.
It takes every ounce of his willpower to push down the ache that wrenches deep in his stomach, but the dragon warrior manages to hold a steady gaze as he turns back to Yuun. He offers the young man a simple wave in greatful farewell mere moments before his legs send him up into the sky above.
By the time Yuun can think to say anything, Jae-Ha is already too high up to hear him.
---
When something starts to seem off about Jae-Ha, you feel it more than you see it. The green dragon warrior was normally so casual and freespoken, but over the last few days you notice more and more that he’s distanced himself considerably from not only his fellow warriors, but also from Hak, Yuun, and even yourself.
While the others didn’t seem to notice the subtle differences, you could feel it like a knife slicing across your consciousness. Something was different . Something was wrong . Instinct started as a little whisper in the back of your thoughts, but has grown into a dull roar, calling you to action to find out what was troubling your green dragon warrior so deeply. Could he be feeling burdened by joining you and the others, leaving behind all of those people in Awa that had been like family to him?
Could he...even be feeling….hateful towards you?
No. Absolutely not. You had given great care to give each and every one of the warriors a choice. While each of them were compelled to follow you as heir to the Kouka kingdom, you did not want that to usurp their freedom as individuals.
But perhaps Jae-Ha did not feel the same, and his continued distance only furthered the worry gnawing at your mind until you simply couldn’t take it anymore--you had to talk to him. If he was truly feeling homesick and under the duress of his dragon blood forcing him alongside you, then you would do anything in your power to alleviate his woes and allow him safe return to the Water Clan’s territory.
With a mind made up and too stubborn for second thoughts, you decide to talk to the green dragon warrior the next chance that you get.
---
The treeline seems to always be within reach for the green dragon warrior, an easy avenue of escape when things get to be too much for him to bear.
Too much noise. Too many smells. Too many people.
Though he likes a bit of solid ground beneath his feet in some form, Jae-Ha always seems to find a suitable tree branch to sit himself upon with ease, high enough that he can’t be noticed from the ground, and out of the leaves enough so that he can stare up into the starlit night sky.
The stars, they looked especially beautiful above him. He might even describe them as peaceful, in any other circumstance. A sea of glittering dots within a sea of ever-expansive darkness, not quite unlike the lanterns of ships bedding down for the night as the last echoes of sunlight fade away on the horizon.
With the young Yuun’s words still bouncing around inside of his skull, Jae-Ha reserved himself to the unfamiliar waves of fire ravaging his body and soul alike. He certainly didn’t feel healthy, despite the boy’s assurance of the contrary. He knew no poison, drug or food that could cause such symptoms--if nothing else, they reminded him greatly of what one Awa pirate had described Nadai withdrawal to feel like.
Withdrawal.
Jae-Ha’s entire body shivered at the thought of the word. It’s implications meant more than he wanted to think about. Wanted to admit, even if it was to himself. After all, there was perhaps one important change in his life that could be the cause for the burning in his veins.
A certain person whose presence he can’t seem to get out of his thoughts no matter how hard he tries. A person who, whether he realized it or not, he had been avoiding since the waves of hot agony began.
You.
The person who had become his master, who had earned his trust and admiration, who had made his blood boil with the utmost sense of passion and loyalty and adoration-
And just like that, another wave overtakes the man without warning, always starting like a wildfire from the very center of his chest before wrapping itself around his limbs and mind. Hot. Smoldering. It’s every bit as agonizing as what he thinks withdrawal to be and every bit as yielding in how it can reach into the depth of his soul and rip out the most stupid things.
The way his heartbeat skips when he sees you smile. The way his lips tremble when he wonders what yours might feel like against his, pressing deep and passionate beneath the tender light of a full moon.
The fire continues to sink into Jae-Ha’s bones as he entertains the rampaging fantasy.
A night like this would really be a good one for that, wouldn’t it? A smile breaks across the man’s face as he, smothered in a cold sweat and his heart racing so fast that it hurts, stares up at the moon shining bright above his head. Mocking him? Enticing him? Jae-Ha can’t say for certain which, but there’s a certain masochism to the notion that every little perverse thought of you, that special person, seems only to kindle the fire ever hotter.
Would you want the green dragon to take you gently? Roughly? Would you tempt him openly with fluttering lashes and gentle words, or would you take your pleasure from him while he plays the ever-loyal servant? The thought of being made to serve anyone makes his stomach churn and his jaw clench, but you?
You’re the exception. To a lot of things.
Jae-Ha thinks about how he first met you in Awa. Though you were with so little experience outside of being the heir to the Kouka kingdom, you showcased an immeasurable amount of courage above and beyond what he would have ever expected to find in his would-be master. Years of tall tales and assumptions had built up a very distasteful and sturdy portrait for what the crimson dragon king would be like in his return--powerful and unyielding, forcing his will on the four dragon warriors without so much as a care for their use beyond tools for war and bloodshed.
And with one single glance of his eyes into yours, one touch of your gentle hand upon his fevered forehead after his dragon blood’s enticement, that very portrait shattered into a million imperceivable pieces.
He would follow no other person with as much loyalty as he would for you. He would fight for nobody else, protect nobody else, long for nobody else-
The breeze picks up, pulling Jae-Ha out of his thoughts and leading him to the sudden realization that he was...no longer in pain. While the heat still laced through every vein of his body, the warrior couldn't find anything more than a dull ache echoing from his chest and legs. It even seemed to grow smaller by the second, fading away until only the heat itself remained fervent, his blood still boiling with emotions that he only then became aware were buried by it the entire time--denied, rejected, ignored.
Lust swept over him, twisting around the fiery heat in a tightly-braided cord which bound his limbs frozen and kept him still where he sat, as if unable to even breathe for a few terrifying heartbeats. Before Jae-Ha could stop it, the duo of sensations welled within his belly, coming to blossom with one aching, terrifying gasp of air.
Realization was all too quick to follow, now that he could recognize the emotions swirling around his soul. This heat, this agonizing torture that filled his veins in a way he could scarcely describe--was it a yearning to be with the new crimson ruler?
And not just to be with you, but to have you in ways that only instincts could understand, buried somewhere deep in Jae-Ha’s mind. Instincts to protect, to mark, to breed .
Instincts of a dragon. Unmistakable.
And that is when Jae-Ha, in his moment of carnal paralysis, finally realized that he could hear your voice calling to him from far below the branches. Your sweet voice, soft and worried and edging on fearful, calling his name in such a beautiful, breathtaking way that could make the very moon above bristle with jealousy.
Calling for him.
Calling for the green dragon.
Jae-Ha, Jae-Ha, Jae-Ha.
It was an impossible cry for the man to ignore.
#yona of the dawn#akayona#akatsuki no yona#jae ha#jaeha#lemon#lemon readerinsert#writing#readerinsert#reader is yona au#who!! wants some dragon heats babey!!#chapter#moonlight yearnings chapter#lemon writing
49 notes
·
View notes
Photo

QUARANZINE #14
QUARANZINE #14: Rachel Herman. Rachel was diagnosed as a presumptive positive for COVID-19 after a test for Influenza A and B turned up negative. She's been fighting the virus for just over two weeks. Yesterday she posted this long message on Facebook about her experience so far and I asked her about publishing it in QUARANZINE. She had been thinking about reaching out to me, so we were both on the same page. The text is very long for the format I adhere to so the type is quite small, unfortunately. Here it is in its entirety: Dear friends,
This is the week many of us will get sick. Social distancing is working, but most cities waited too long to declare shelter-in-place orders and many others have yet to. So, we will see spikes in confirmed cases within the next week or so. I want you all to be armed with pragmatic and useful information if this happens to you or someone you care about.
I am on Day 14 of what was diagnosed as a presumptive positive for COVID-19 after a test for Influenza A and B turned up negative. (I am still waiting for my COVID-19 results.) I’ve had a relatively mild case, and I’m on the mend. My congestion is clearing up, I can breathe deeply again, and going up and down the stairs doesn’t make me winded. My energy and appetite are coming back though I still have had a fever of 100+ for 14 straight days. Most of us will get a mild case. 40-70% of us will get it, but so much of the media frenzy right now is focused on things that were important last week and yesterday (every day feels a year these days, though, to be fair). I have seen shockingly few articles or helpful testimonials advising how best to treat ourselves at home, and, trust me, I’ve been looking. So much of the information we’re focused on now is preventing transmission, but there is woefully little on what to do IF and WHEN we get sick.
Being waylaid during the time that so many folks have been still frantically trying to avoid getting sick has offered me a strange bubble of calm and insight. I’m grateful for that because the fear out there is palpable. I would like for this to be an offering to assuage at least some panic. That is my hope anyway.
The CDC and the WHO have labored and lengthy instructions on how to prevent transmission to someone else in the household or orders to quarantine. This creates a new problem for us as caregivers. A potentially critically ill person separated from everyone else drastically reduces a caregiver’s ability to monitor, replenish fluids, and generally take care of the person who is sick. On top of that, these two trusted sources offer only the most basic (honestly, negligible) recommendations for treating symptoms: sleep, keep hydrated, and take Tylenol (or the generic acetaminophen). This kind of bare bones advice is, well, skeletal. We all want to know how best to take care of ourselves and each other so that we can avoid having to go to the hospital. We want to be able to recuperate at home because we want to prevent putting a strain on the system and, face it, the idea of going to the hospital in this scenario is downright daunting. The better we know how to nurse ourselves back to health, the better our odds are healing well in our own beds.
So, I wanted to share what I’ve learned.
Caveat emptors/disclaimers because I’m making this public and shareable: This is based on my own personal, lived experience. I am not a doctor, so this does not replace or supplant solid medical advice from a professional you trust. I have had relatively mild symptoms but still a longish case. I am one of the freakish 5% who has had never-ending nasal congestion that went into my upper respiratory tract, but I somehow avoided the dreaded cough. YMMV (your mileage may vary). I have no underlying health concerns, I’m 52, a non-smoker, and fortunate. I have a comfortable apartment to myself, and I was able to spend $500 to stock up on essentials before the lockdown and before I got sick. (For the love of all that is holy, I swear I did not stockpile anything, especially TP. Stocking up is simply incredibly expensive. I dwindled my account down to almost my last dollar, since I’m adjunct faculty at two local universities and don’t make a whole lot.) Still, that is more than so many of us are able to do, and I am grateful for all that I have. What follows goes a bit beyond common sense, because this virus is unlike anything I’ve experienced before, even though to be clear, this is certainly a far cry from the sickest I’ve ever been. I hope it can be a boon to friends and strangers alike.
Here are the things I did that helped:
WHILE YOU ARE WELL
1) Start taking your temperature in the morning and at night so that you have a baseline.
One of the first signs of the virus can be a low-grade fever, though this virus does present in different ways. Full disclosure: I was one of those people who had to go to 3 different drugstores on Wed Mar 11 looking for a thermometer amid decimated shelves.
2) Before you get sick, change your diet.
Stop eating and drinking things that will make it harder to fight off the virus. Mellow out on the processed foods, dairy, and sugar (alcohol and gluten are in this category too, sorry).
Increase your intake of immune-boosting foods like green vegetables, fish and other omega-threes, garlic, ginger, and citrus. You don’t have to give in to the whole elderberry craze (though it does taste pretty good). Replace coffee with chaga, a fungal immune booster that you can brew into a strong, soothing tea, for a few weeks.
If you think these dietary recommendations are extreme, consider that you are in a temporary but dire situation where everything else around us is collapsing. Change your eating habits this month, even if it’s just a little for a little while.
3) SLEEP at least 8 hours a night. (I know, I wake up at 4am in a blind panic too. But, still, try.)
4) Make a pot of soup NOW while you are healthy or at the first sign of any symptoms.
This is especially important if you are sheltering in place alone. When/if you get sick, trust me, you won’t have energy to cook. You will barely want to eat anything anyway. But you will force yourself to have two bowls of it every day, and it will help. The pot should be big enough so that you can eat from it for a week. Make your favorite broth-based recipe: chicken, vegetable, or bone. Bone is most healing, obviously. Avoid dairy and noodles because these ingredients increase congestion and inflammation. Freeze it if you don’t have any symptoms at this point, so you will be able to thaw it when you start to feel oogy.
WHEN YOU GET SICK
1) At the first sign of fatigue, a tickle in your throat, aches, or a fever, go to bed and stay there. SLEEP. Don’t try to keep working. Your body needs to heal, and it can do that most effectively when you are sleeping.
Early symptoms reportedly vary. Some have aches and fever, scratchy throat, and chest tightness with a dry cough. Headaches, sneezing + nasal congestion, shortness of breath, nausea, and diarrhea have all been reported. I woke up on Mar 14 with a headache, body aches, congestion, and a fever of 101. My fever spiked to 102.5 on Day 2, and I’ve had a fever of 100+ every day since along with body aches, nasal congestion (my nose opened up like an actual running faucet on day 5), chest tightness and upper respiratory congestion, exhaustion, lack of appetite, and some lower GI distress (though not full-on diarrhea, everything just felt labored and different and, sincere apologies for the vivid image I’m about to put in your head, my poop seemed to be covered in a gauzy cloud). The two aberrations from most commonly reported symptoms: I have only had a negligible cough, and I never had a sore throat. My baseline temp leading up to getting sick was 99, but I am usually a straight-up 98.6 kind of person.
I had a dinner party the Monday before I got sick, and a friend who helped me in the kitchen came down with the same thing at the same time. My friend has asthma and has had a much harder time of things. But we are both on the road to recovery, in large part because we have been sharing what we’ve learned, checking in with each other, and doing some intense jobs taking care of ourselves while in isolation. (No one else from the dinner party has gotten sick to date.)
2) DRINK WATER, every 15 minutes when you are awake. Every time you wake up or roll over, drink. It should be room temperature, not cold. Cold liquids exacerbate the illness.
3) Drink WARM liquids like herbal tea and broth. Hot liquids keep everything in your system moving. Make soothing, healing, and warming remedies out of whatever inexpensive supplies you already have available.
4) In the giant void of an antiviral treatment that works on COVID-19, I have turned/returned to plant medicine, and it has helped me a lot.
My cousin, who is taking a Chinese medicine course in Singapore right now, sent me directions on how to make a ginger and licorice root decoction that was used throughout China during the Hubei lockdown. It’s easy to make. You bake the licorice in molasses, and then you boil the licorice root and the ginger for an hour. The ginger licorice decoction has really helped my friend who also got sick at the same time I did.
Making tea from Chaga – an Alaskan mushroom – has been so incredibly helpful. I’ve made a large pot of it every day, reserving the chaga and re-steeping over and over again for the past two weeks. Was it the chaga or the fact that I was drinking a gallon of warm soothing liquid daily, ladling out a mugful every couple of hours, that helped me get better? I’ll go with a little of both.
Other natural antiviral immune boosters that might help include vitamin C, C60, and olive leaf extract, oregano oil, and Manuka honey. Since stores are closed and Amazon has stopped shipping, we have to make do with what we already have. Make a tea with citrus peels and cloves and sliced ginger, if that’s is in your fridge.
5) The word on the street is to manage fever with Tylenol or acetaminophen or paracetamol, which are supposed to be more suited to treating respiratory illness than other alternatives. Frankly, I have been taking acetaminophen as sparingly as possible to avoid putting strain on my other organs. Cool compresses work too.
Some people are saying NOT to take Advil and its generic ibuprofen, as they have anecdotally said to propel otherwise healthy people to hospitals for oxygen. There is a lot of noise and confusion in this debate, and I’m going to sidestep this thorny conversation for our purposes.
6) Zinc lozenges and elderberry syrup help with a scratchy throat and cough. A friend of mine prone to bronchitis recommended Myrtol, a German cough syrup made from natural ingredients, including elderberry. If you have a pharma protocol in place for managing a persistent, chronic cough, you are probably already on it.
7) The fatigue is real. It also becomes really hard to think clearly. That’s why it’s so important to have soup and tea and other supportive supplies ready ahead of time.8) When you think you are getting better the first three or four times, STAY IN BED.
The arc of this virus is really rollercoaster-y: up and down and up and down. After the initial alarm passes, (and it is alarming at first because you don’t know which way it’s going to go and that seizing up can make everything feel worse), I was able to focus on getting better, calmly. I made it through the first scary fever spikes, but right when I thought I was feeling better, I would get knocked down again. There were critical junctures around days 3, 5, and 7 where I was certain I’d turned a corner, and, well, yesterday.
I’d get up and do dishes, take out the trash, take my dog for a walk around the neighborhood (face covered), and try to get some work done (end of quarter grades were due at both my schools and my departments have been preparing like mad to take our classes online in the spring). Then I would feel hot and light-headed again, taking my temp only to see it had sprung back up to 101.5. You will feel better and want to get back up and do things only to get knocked right back down. The moment I ease up on drinking water and tea constantly, I start to feel horrible again.
Remember: YOU ARE ESSENTIALLY PREVENTING YOURSELF FROM DEVELOPING FULL-BLOWN VIRAL PNEUMONIA. I would say the new mantra needs to be SLEEP + DRINK WATER. Start now, to the extent that you can. Please resist the urge to get up and do things. Rest. Do your Zoom meetings from bed with a virtual office background, if you absolutely have to be on a call. But, truly, you shouldn’t because this is the time to sleep sleep sleep and binge watch The Good Place (my choice for existential dystopian laughs/insert whatever makes your socks go up and down). For the past few days, my temp has been normal in the morning only to spring back up to 100+ if I try to do too much (e.g. read: ANYTHING). When I let myself sleep, my temp goes back down.
9) A humidifier has helped. Some recommend running a hot shower and sitting in your own makeshift bathroom sauna. Steam eucalyptus or rosemary, if you have any, and inhale deeply. I just made a homemade vaporub with a base of coconut oil and a few drops each of clove, thyme, rosemary, and peppermint oil. It is wonderful.
10) My breathing never got dangerously shallow. But this virus can potentially fill your upper and lower respiratory tracts with mucous until you feel like you are drowning. A physical therapist wrote with life-saving advice about the importance of Postural Draining, a method of draining mucous from the lungs using gravity and percussion. It involves physically moving your body so that you tilt your lungs and bronchial tubes upside down and then firmly clap the back or chest. This allows the mucous to flow up out of the lungs along with deep, prolonged exhales. Then you can cough it the rest of the way out. You can do postural draining alone or have someone perform it on you. Google postural draining diagrams – there are different for positions for each of the five lobes of your lungs. Do these exercises for 3-5 minutes a day before you get too sick. You can get into position in a chair or laying over a yoga ball, bean bag, or pillows for support.
Failing steps 1-10, if you have difficulty breathing or your temperature spikes beyond what you and your doctor are comfortable with (I’ve heard different numbers), please go to the ER immediately. Some of you will develop dramatic and dangerous symptoms quickly. Please do not wait to seek care if your lungs are struggling beyond what you can manage at home. My advice is geared to keeping as many of us comfortable for as long as it takes to heal, but that obviously is only going to go so far for those who suffer from chronic conditions, are older, or are immunosuppressed. If you have a finger oximeter, and are able to monitor your oxygen levels numerically, then you will know when you have to go to the hospital. But very few of us have those, and they are way sold out.
THE OTHER SIDE
Healing from even a mild case (and mine IS mild) takes about two weeks to a month.
As my dad would day, take it easy. It is unclear how immunity works with COVID-19. Some have said that there was a patient in Japan who tested positive a second time. There is speculation that this, in fact, was a relapse and not re-infection. We need more time to learn about the virus. In the meantime, please give yourselves time to heal.
We don’t know how long immunity lasts, and we don’t know about immunity to slightly different mutated strains even if we have recovered from one of them. I do hope that we get to develop a fair amount of herd immunity in the next year, but, again, there is a lot to learn. We will obviously still need to protect our vulnerable populations, and our society will continue to bend and contort itself around the virus.
But I hope to be in a position to assist when others get sick. I will happily help you to the best of my abilities. Looking to a future I can hardly conceive at the moment, I anticipate learning more about plant medicine. Scientists will develop new antivirals, retrovirals, and vaccines. I look forward to donating plasma as part of a treatment for those who get sick in the future, whenever that near-distant moment may be.
And thank you, friends. I am good. I have everything I need. My inner circle is incredible (I love you, mom!). I have been quarantined since developing symptoms and went out for a half hour only to get tested (thank you, Howard Brown for your invaluable service). No one else I spent time with beforehand has gotten sick (except my one friend whose illness coincided with mine, and they are also struggling a bit today with the ups and downs. Please hold them in your thoughts).
May you and your loved ones stay healthy. Or, more to the point, may we all get well and stay well. Sending love to all corners.– Rachel Herman
#QUARANZINE#Rachel Herman#Public Collectors#Marc Fischer#Zines#RISO#Publications#covid-19#coronavirus
45 notes
·
View notes
Note
Hi c: I remember a post, I think it was from you, about long covid and getting it? Was that you? A friend of mine is struggling and I was wondering if you had any advice about what she can do :< Thank you!!
Oh no, I hope your friend feels better soon! That might have been me, I think I posted about it here a few times and there have definitely been twitter threads.
Standard disclaimer stuff: I am not a doctor. What I found helped me might not help someone else. Long covid is kind of fucked up to deal with because it seems to hit everyone in different ways, in different areas, and months later something that wasn't a problem before can suddenly become one. The long haul groups talk about it as something that feels like it moves around the body, like a total shit gremlin.
The thing that helped me the most initially was joining the facebook groups with other people figuring shit out. This was back April/May for me but they're still very active and full of people sharing resources.
Survivor Corps is I think the big one and they've been the ones reaching out to media and doctors to try to gain some recognition with the medical community initially (as far as I know, all kind of a blur tbh). There's also a long covid group here, and if your friend searches for like, long covid + the country they're in there are usually more local/regional ones for resources closer to home too.
Because we don't really know what specific mechanism is triggering a lot of the long covid stuff yet, most of us are just treating symptoms. Some people have been diagnosed with mast cell activation syndrome (MCAS) and I don't know diddly squat about that but it might be something for your friend to look into. My whole thing has been inflammation and my immune system basically attacking itself because immune systems are both very complex and compellingly fucking stupid. Not to victim blame the immune system or anything.
What helped me depended on what was going wrong at the time, obv, but it means it's a long list.
This is just going to be a brain dump, sorry.
- I never had pneumonia. Mine started in my throat, probably damaged my vocal chords, but never turned into pneumonia. I still had shortness of breath, pressure in my chest, and my oxygen levels dropped. I could breathe but with great difficulty and described it to the EMTs as "breathing is like work." It took all of my energy and focus to breathe in enough. If you are that this point, ever, like, literally fucking ever, call an ambulance.
- Tylenol for a fever.
- Blood thinners if necessary, I never had any but we know now that a lot of problems are blood clot-related. Tbqh my blood is more thin now than anything but I always had anemia and some sort of “your blood is too small actually?” problem and we don’t know why. I just bleed a lot and bruise easier now.
- If they try to tell you it's anxiety or in your head or you're not that bed, tell them to go fuck themselves and go to the hospital. Get tested if you can. A lot of the problems long haulers ran into was that we got sick before tests were available, or we were talked into staying home by the emergency workers, and we never got tested. This opens the doors for doctors to tell you it's all in your head, psychological, anxiety, allergies, etc. Just. Go when you first feel sick if at all possible. Get tested before it turns into long covid.
- I was not sure in the beginning what "shortness of breath" or "pressure" actually felt like, and it made me delay calling for an ambulance for a few days as well. For me, it felt like there was an elastic band of pressure around my lungs. I couldn't fully inhale. My diaphragm was fucked in ways I still don't understand. My lungs also felt heavy, like there was a weight on them or like my lungs themselves were too stiff to inhale. That all counts as pressure/tightness/shortness of breath. So does air hunger, or feeling like you want to be swallowing air.
- I know I'm being super obvious but seriously shortly before I got sicker, I hit up twitter to ask what "pressure" was supposed to feel like because I couldn't tell if what I had "counted."
- Breathing: lying on my stomach with my chest propped up by pillow, in bed helped. So did pursed lip breathing: here.
- I was prescribed salbutamol initially, which did help with the worst of the wheezing and opened up some of my lungs so I could breathe easier. When I went to the ER again a couple months later, they gave me like 5x the usual dose and sent me home.
- I'm also taking Flovent/fluticasone twice a day for asthma maintenance.
- Histamines are a problem for a lot of people. Some develop a histamine intolerance, which can be helped by eating a low histamine diet.
- Antihistamines helped me the most. I was taking Allegra-D daily. Pepcid AC also helps, because it targets a different kind of histamine. There was such a run on Pepcid when this started that it was actually impossible to find in my area and I had to order some online.
- I was recently prescribed Singulair and it has been life-changing this past week or so. As far as I know it's not really an antihistamine but blocks/inhibits a particular receptor involved in inflammation that comes into play when allergies do.
- Electrolytes. I don't know why, but my electrolytes are permanently fucked and too low now. If I don't go through like a litre of gatorade a day (or whatever, pick your brand of supplements), I am even more tired and brain foggy than usual. Helps a lot.
- Inflammation is a major problem all around. Sometimes I go for the naproxen or advil and it will help any really major acute flare-up now (like, I can feel when my gallbladder is getting inflamed and about to spasm and I can cut it off sort of), but mostly it's also daily maintenance. I take cucurmin and black pepper daily.
- Other supplements: vitamins A & D, a multivitamin, NAC.
- CBD oil. This worked wonders for me for a lot of the side-effects of covid, costochondritis and shingles pain especially.
- Diet. I mentioned the low histamine one above. Other people have had some success with a low inflammation diet. Some folks also have so many GI problems that they basically ate chicken and rice and slowly reintroduced foods to see what would trigger something. I appear to get super fucked by nightshades now, e.g. Alcohol is an absolute no. I had to cut caffeine for months because of my heart. (No caffeine/alcohol/red meat was my doctor's first and best advice for heart stuff at the time.)
- Speaking of the heart stuff, if your friend is dealing with that: electrolytes again. I have pedialyte freezies that I would suck on whenever heart palpitations started and it helped calm it down some. My heart was so, so fucked for months that whenever I ate or stood up or sat down it would hit like 140bpm and I had to spend an hour moving as little as possible or I'd just about pass out. There are a LOT of long-haulers now dealing with POTS and I can't really speak to what helps that in particular but if your heart is messing up at all: call a doctor. I still don't know how damaged my heart is from all of this because doctors and wait lists, etc. Get a jump on that.
- Insomnia was absolutely the worst I’ve ever had and I’ve had lifelong, “I’m awake for three days wee” insomnia. The Singulair knocks me right out at night, so that's a bonus, but there has not been a single night since getting sick where I didn't have to take something to help me sleep. I was on Zopiclone before getting sick, at least, but seriously talk to someone about insomnia if necessary. The sleep deprivation alone was making so many things worse.
- Brain fog? Brain fog. I don't have any or many answers for this. My short-term memory is wrecked and usually I'll remember something 2 weeks later, so I live my life on a 2-week lag now.
- Related to brain fog, fatigue. Don't fuck with it. Do not. Chronic Fatigue and Myalgic encephalomyelitis are both brought up often with long covid. I am dealing with it but don't know what to say about it yet because I haven't had a single doctor give a shit thus far. I've spoken to a relative who's an occupational therapist about it and her most helpful advice was about "energy envelopes," which is basically spoon theory. If you feel tired: stop. If you don't, or if you try to push through, we relapse hard and fast and you can pay for one day of walking 10 minutes too long with weeks of being stuck in bed. It's miserable. It will take longer to get back to normal. Some of us can exercise and feel amazing after; others are exercise intolerant and it wrecks them. (I feel best after like, 10 minutes of walking and sunshine right now, which is after months and months of being bedridden.)
- Treat mental exertion the same as physical. Doctors told me to drink Gatorade after mental work because it's still work, and it has helped a lot for whatever reason. It also helps to work on one thing at a time, take a break, switch gears, take a break, etc. I can't multitask anymore anyway.
- Eliminate whatever stressors you can. Stress will make everything worse.
- It comes and goes. Every relapse was a bit shorter and a bit easier for me, so that now when I fuck up it's like 2-3 days instead of weeks, but it's a rollercoaster.
- It can be random as hell. For about two months my gallbladder just decided to up and die, basically, and we were talking about having it removed. And then it was fine. Hasn't bugged me again lately. I know I said it's symptom management, but it's also like... symptom chasing and trying to figure out what's happening every time the sun rises. This is also exhausting. Everything is exhausting.
- Brain shit. Some of us have serious trouble reading. Sentences swim together. Letters wouldn't turn into words. I took this as a Challenge and started reading children's books and then Animorphs again, like... slowly, as much as I could do without pushing it, and it's still not perfect or great but it was an okay place to start. Honestly the hardest part was the embarrassment and going from a PhD program to reading kids books, but. Do what you have to. Do what you can.
- Sticky notes and labelling things around the house so I could see them when I needed them. I am not fucking around when I say brain fog. I can open the fridge, know I have milk, know it is in the door, and literally not see it to find it. I will put the cream in the dishwasher. I will spin in circles in the kitchen remembering and forgetting and remembering why I’m there again. Sticky notes. Also: journals, index cards, write literally everything down if you need to remember something. Put it somewhere obvious. I like writing on the bathroom mirror for the important shit. (Don’t use lipstick.)
- Unsurprisingly, a lot of us are struggling with anxiety and depression. Don't let doctors get it backward: it's not anxiety making us sick, it's being sick and ignored and fighting to be helped that's making our mental health worse. So many doctors tell us it's all in our head. I did not move across the country because I was too sick to take care of myself because of ~allergies~ or ~anxiety.~ Fuck off.
- So, so many people report that they relapse whenever they menstruate so if your friend is in that group, they might want to prepare to feel like fucking trash every 4 weeks no matter what they do. I don’t have any advice on this one, I’m sorry. There are a lot of people discussing it in the FB groups, though, and those are searchable for symptoms.
- So... a tl;dr list of things that might help: anti-inflammatory diets, anti-histamine diets, pepcid AC, allegra or other allergy meds, vitamin A/D/E, multivitamins, electrolytes and gatorade, albuterol, fluticasone, zopiclone (or anything that helps with sleep), CBD oil, singulair, anti-nausea meds (buscopan), muscle relaxants (spasming gallbladder). Rest, so much rest, do not fuck with The Rest if you can help it. I also encourage just getting high and edibles as much as you can because it sure helped me chill out big time and I think was a big factor in my recovery, at least as far as helping me calm down and helping my heart were concerned.
- The actual most helpful part outside of what to take or do was other people. Friends would go out and get me things when I could not, including like, cat food deliveries and all. I had co-workers ready to step in to take over my work on days I could not. I had friends calling doctors because I was too tired to fight them or self-advocate. I don't think it's an exaggeration to say they helped save my idiot life this year. Literally. It's a lot to ask of anyone but it's also that level of support that some of us need, and there shouldn't be any shame in it. (I still feel bad about it anyway but what are you gonna do.)
Depending on where you live, some places are setting up long-haul covid clinics to help people. Reports are mixed: some demand you had a positive test even if you were sick before tests were available. Some people are getting a lot of help regardless. Some are being sent home and told not to come back anyway. It’s kind of a gamble right now but either way, there’s at least some medical recognition making headway now so my fingers are crossed.
Anyway you basically sound like a good bean and your friend is lucky to have you asking around. I have absolutely forgotten something at some point in here because, well, brain fog and no memory, but if you have any questions or want something clarified please just ask. Stay safe!
2 notes
·
View notes
Note
glad to know you are mostly recovered from covid! if i may ask, could you describe how where your symptoms or at what pace you got them? the information i've got from both medical / govermental sources in my country is contradictory at times. also, what would you recommend drinking if i found myself to be with covid?
first off: WATER!!! drink water!!! I mean you can probably drink whatever as long as it’s moderately healthy and you’re staying hydrated (my drink of choice while sick is red gatorade. it has to be red or it doesn’t work though) but water is always a safe bet
also I’m happy to share my experience, just know that (1) I am not a doctor, just a professional Sick Person and (2) I never officially got tested thanks to a shortage of coronavirus tests in my area, but I’m pretty damn sure my symptoms were aligned with covid-19, so take that as you will
the first thing I noticed was a sore throat... but I have sore throats allll the time because of my other health issues, so I didn’t think much of it. I did start to notice my sore throat was getting better (from a previous mystery illness that knocked me out for a few days, and which I initially thought was strep but was probably just a bad cold) before suddenly getting bad again. I also had a day where my sore throat was especially pronounced and I had that Really Tired Feeling you get when you’re sick. I guess we can call that day one, but at this point I definitely didn’t think I had corona
that night I noticed some chest tightness, which I initially wrote off as an anxiety attack (and considering my extremely anxious personality and the fact that we were battening down the hatches for a pandemic, that seemed like a fair assumption) but using my inhaler didn’t help--in fact, it made the pain worse! but it did pass eventually, more or less, and I forgot about it
(side note here that if you think you have corona, do NOT use your albuterol inhaler or any kind of steroid inhaler unless you’re having a legit asthma attack with wheezing and all the works. using your inhaler can make the corona symptoms worse, but obviously if you need to use it then it’s important to keep using it. consult your doctor. also another similar note: if you think you have it, stay away from most NSAIDs if you can, as those can also make things worse. tylenol is okay though as long as you’re careful about the dosage--not as a corona thing, you just always need to be careful with tylenol dosage. and it’ll help keep your fever down, which is important!)
then over the next day or two I noticed the chest pain flare-ups but wrote those off as well. they were short-lived and mainly seemed to happen at night, but the inhaler always made them worse. around this time I also started experiencing some general GI upset for a few days (not to get too into that...), but I have a very touchy digestive track and was taking antibiotics at the same for other unrelated reasons, so I was like “well it’s probably nothing” but was starting to get worried.
then about five days later, the chest tightness really made itself present. like, it lasted all day and was constant. I was concerned but not immediately freaking out, and it was really windy that day so I kind of chalked it up to allergies, but as a very allergic person I’ve never had chest tightness like that from allergies (and my other allergic symptoms have improved considerably since I started allergy shots, so it would be weird to have a new symptom crop up out of nowhere like that).
then the next day, and the next day, the tightness wasn’t going away. this was clearly not allergies. I started to seriously think about corona tests, and I even called my primary care doctor, but she was extremely dismissive (all she did was call in a prescription for an old allergy drug that never even worked for me in the first place) and it was downright impossible to get tested. I was freaked out, but not entirely sure.
it’s about day seven at this point, and the chest tightness is in full swing. when I first wake up, the pain isn’t really present, but after about an hour of wakefulness my chest starts to get tight, congested, and kind of has that rattle-y feeling when it’s full of mucus and crap from the postnasal drip. not much congestion otherwise, but I’m so hopped up on antihistamines at all times that I don’t really get congested in general. the best way I can describe the chest tightness is that it feels like when I exert myself and my asthma makes my chest seize up and it’s hard to catch my breath (aka every single PE class I was ever forced to take as a kid), but my inhaler doesn’t do shit. my throat is still hurting pretty bad too and I feel vaguely fevery, but I don’t have a working thermometer at home. overall I just feel shitty, like that feeling you have when you know you’re sick (and I get sick a lot so I’m pretty well-versed in that lol). for quarantine purposes, this is the day I’ve been counting as the “first day” of having obvious corona symptoms, but it was really predated by the things I described above.
several days pass like this, I keep trying to get tested and call all sorts of places but it’s all dead ends. I also develop a slight cough, which mostly comes in bursts or when I speak/eat. by day twelve I manage to get a primary care appointment, and they do an EKG to make sure it’s not cardiac pain (the EKG came back fine) and a throat swab to see if it’s something bacterial (it’s not). they do confirm I’m running a slight fever, although my body temperature is usually so low that even a fever of 99 is high for me. my primary care doc basically tells me to fuck off and stay home, which I was already planning on doing. she also didn’t even wear a mask or gloves to look into my throat, despite the fact that all the other nurses in the practice were wearing masks and gloves when they interacted with patients... so I’m not exactly full of confidence in her judgement here.
the night of day thirteen, the day after seeing my doctor, I have a night where I can’t sleep because my airway feels restricted (both in my chest and my actual throat being swollen from pain). I used my inhaler, like a fool, and when the inhaler didn’t help the first time I tried using it two more times. big mistake! I ended up lying awake gasping for air, taking huge gulps just to feel like I was getting the teeniest bit of oxygen, and feeling stabbing pain when I took these deep breaths. I was too afraid to sleep and almost made my girlfriend drive me to the ER but I hate going to the ER so instead I just tried to calm down until I got exhausted enough to fall asleep around dawn. I also kept alternating between sweating buckets and shivering to death, no matter how I kept adjusting the temperature and my blankets, so I assume I was having a crazy fever that night.
the next day, roughly day fourteen, I decided to suck it up and go to the ER to get a chest x-ray. they said my x-ray looked fine, which was encouraging (hopefully no permanent lung damage there), and they took a flu swab and a strep swab just to rule those out (both negative, of course). at least two other people were there with me in the ER complaining of similar symptoms, but they didn’t have any tests for us so the doctor just told me to go home, act as if I had it, and keep taking tylenol and drinking water. this doctor is also the one who told me to stop using my inhaler--and the fact that my inhaler kept making the pain worse is one of the things that really tips me off here that I probably had it.
things are pretty much uneventful for the next week: still having a tight chest, a fever that seems to come and go, sore throat, cough. no more crazy attacks like that one night.
by day nineteen (yesterday) I start to notice a bit of improvement in my chest pain. it’s not gone, but it’s not as bad and I’ll have slight reprieves from the tightness. today is day twenty (more or less, my numbers are a little rough here) and I actually felt okay most of the day. by the evening the tightness returned and I’m still coughing every now and then, but far less often. I think the fever is gone and my throat doesn’t hurt too bad, either! I’m well past the point of being contagious, so I actually went to the grocery store today and got a few things. I’m not totally out of the woods yet, but I think (knock on fucking wood) the worst has passed.
anyway, I hope my anecdote is helpful for you, and I hope you stay safe and healthy!
18 notes
·
View notes
Text
6 / 28 / 2020 ENTRY TWO

It is a little ridiculous the way things work out sometimes in life. Ridiculous as in… uncalled for, extensive, unnecessary, crazy. I have always been in perfect health. There was that one time I had cat-scratch fever when I was a kid but other than that I never had any issues, never broke any bones. We thought my chest pain way back in 2015 was just leftover remnants of grief, because my mom had a similar pain ever since we lost my sisters a few years before. I was told it was anxiety, figured that my stress as work was considered just that, along with eating too much pizza and called it a day. It no longer started to make sense a year and a half later when the pain increased during my most mellow of moments and all I felt like doing was napping. Sure, every college student loves a good nap, but that just wasn’t how I rolled. Naps were for the weak, I could get so much done in the time of a nap. Yet I always felt like I needed one.
Low and behold, we gave up trying to reason with it and just decided to go to the doctor and ask about it again. Oh, and maybe run some tests just in case. All the basic ones. If we need to do more then we’ll figure it out. We didn’t need to. The last test that came back showed that I was positive for a local happenstance called Lyme Disease. I got the call while I was driving on my way to work in Bangor. I kind of freaked out. Called my mom afterwards and cried over the phone a bit shaken up, mostly because I didn’t know what it meant. I use to think that I overreacted because most of the time a little thing like a brief disease from a tick was just a handful of days worth of pills and you’re done. I wasn’t done. In fact, we screwed up. I took those antibiotics and, without realizing it, woke up the rest of the disease inside of me that was dormant for years. I was down for the count. Well, not really, not yet.
A lot of doctors don’t understand Lyme. They just don’t. My pediatrician didn’t. My mom didn’t, not that she was a doctor but a master researcher. We tried so many things for 10 months. Crazy things. Ridiculous things. Almost more ridiculous than the disease itself can be. Almost. Essential oils, salt and vitamin C, cannabis, GI health supplement program. Nothing worked. Nothing made anything better. I got worse actually. In the fall, I went to the ER twice because of extreme stomach pain but no one could tell what was wrong. That was because you can’t really see an over abundance of bad intestine bacteria with ultrasounds or a CT scan. My mother, a master researcher as I must repeat, got me in as one of the first patients of a new Lyme clinic in the town over in December of 2017. This doctor, let me tell you, is my favorite man on earth.
I didn’t go back to college that spring. Finally I was down for the count. Treatment sucks. It really sucks. The way herxing works is that you take your medicine and slowly increase it over time. When you increase it, all your symptoms increase by tenfold for a short while, killing off the Lyme bacteria quicker than your body can process the toxins their death releases. In the end, you feel worse in order to feel better. Herxing isn’t meant to last long. You have your period of misery and you’re suppose to feel better than you did after the herx than before it. Not only that, but I had to change my entire diet due to small intestine bacterial overgrowth from that absolutely ridiculous pyramid scheme health program. I’m still bitter about it. I’ll probably always be. Had to drop so much money on an antibiotic that was literally sent from God Himself. I did get better.
I went back to college in the fall of 2018, ready to take everything back on. Keep on keeping on really. I was always cautious of not doing too much otherwise I’ll get knocked down again. But here’s the thing about New England. We have old buildings. Old buildings include this lovely stuff called mold that can make one’s life miserable if your immune system is already compromised. I was feeling great, better than I had for awhile, but the longer I was back at college the worse I started to feel. I had to go home in the spring, finish my schooling and rest. Graduation consisted of so many tears but I’m glad I pushed through. Glad it was over though I was sad.
It was officially time to get to work. Heal from mold exposure, heal from Lyme, and take my life back from this disease that just kept hanging on. Doctor and I hit the ground running this past winter. Once I finished the protocols from mold detox we increased everything else so that I could be free quicker, sooner, and more efficiently. It was rough but in the end it was so worth it. In April, I started taking my physical well being back into my own hands. Exercising consistently for the first time in three years. Bread, sugar, coffee have returned to my diet. As of now I have been free of all Lyme supplements for two months. Aside from my sprained foot... I have been healthy and able to work consistently without struggle.
Now there’s a lot of things I’ve learned in this time. I can’t tell you the amount of times I went up to the altar at church, at camp, at college for healing. Going to a Pentecostal college where they preach healing with the laying on of hands and that all you need is to have faith that God can do it... truly gives you the right environment. I read books. Memorized verses. But in the times where it was really bad, I was confused as to why God didn’t or wouldn’t heal me. I still don’t quite understand why He didn’t heal me during those other times and I could have received my Bachelor’s without problem, where my dad could have saved money instead of going into debt. But God works in mysterious ways and if there is ever a more true statement... I honestly doubt it.
Lean on Him. Lean on Him even if you don’t get it. Lean on Him even if you think you know the better way and everything is crashing around you. There is no other force that is more stable than Him. I vented to Him often. I know we’re suppose to have reverence for God and respect and fear, which I do have all those things, but sometimes there would be a day where I just had it and told God how I really felt. Even when I yelled at Him, He still comforted me. There’s a peace that passes all understanding, literally. And it’s because of this experience with Lyme that I learned new ways to trust Him, to be guided by Him and to listen to Him. To find hope in hopeless, suffocating places. So maybe there were a few reasons why I wasn’t healed on the spot, who knows but God?
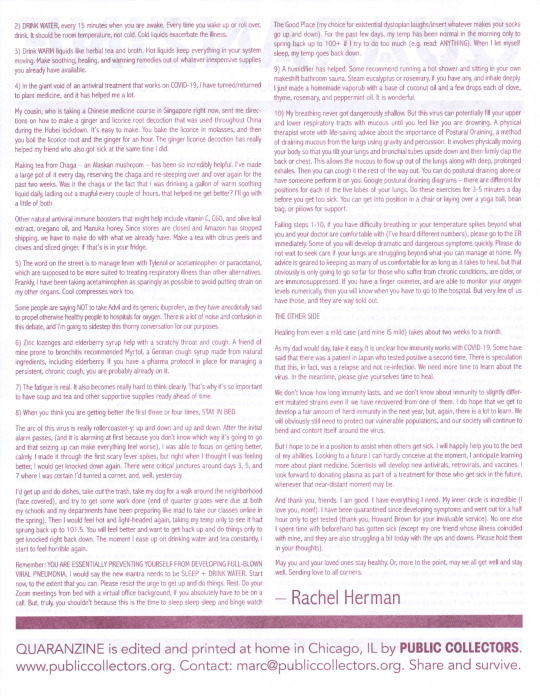
The other week I put the box away. The box I found in the school’s “blessing room” of free stuff that I stored my supplements. The l leftovers and the medical papers all went inside and I put it up in my closet. I did it on the anniversary of Bailey’s, my sister’s, death. Right now I think it means a bit more than what I currently understand. Okay God. I’m ready for what’s next.
--Amberthyst
1 note
·
View note
Text
hi yes hello i am alive
big boring update ahead, tl;dr: i’m okay!
so last night after the scary temperature jump i decided to give the meds a chance to bring it down before i went and racked up some medical bills and fortunately it did start to come down after that
i stayed up for a little bit and kept an eye on things and when my temperature seemed to stabilize around 98-97 degrees i went to bed and seemed to do okay
for most of today i was fine apart from still not a great appetite for the first part of the day and absolute lack of energy for the whole day (but that’s pretty typical with my myasthenia and fevers, it just...wipes me the absolute fuck out. every trip i’ve made up and down the stairs today has felt like climbing a fucking mountain, it’s great)
i’d read something online because i was curious why i mostly seemed to deal with this shit at night and apparently there’s something about your cortisol levels being down at night and therefore your white blood cells just kinda go nuts and that’s what can sometimes bring a lot of symptoms and shit to the surface, especially since in the case of a fever that’s the body trying to like...burn shit out of you and i thought maybe that was total bullshit, but i asked my mom who’s been a nurse for like...ever and she said that checks, because several times she’d have patients who would be fine all during the day but would just go to hell health-wise at night, so there’s that
that being that case, i took some more tylenol as it rolled around to evening and i’m glad i did because i checked my temperature around that time and it was 99.1 so i think it was already trying to creep back up
as for what it is, i still don’t know and part of why i’m so hesitant to go see another doctor is because i really only have the one symptom. i’m pretty sure the appetite thing and the weakness is because of the fever. i’m not having any congestive symptoms or GI symptoms. i guess the only thing i haven’t had done or checked off is blood tests but...it’s not like you can just say, “here, take my blood and figure out what’s wrong with me!” they need to know general ballpark of what to test for to know what to order and i can only give so much blood. the next step would be scans and x-rays and shit and that’s when you start getting into the EXPENSE and...being that i’m not having any pain that’s going along with this i just...don’t want to go there just yet. i had the lower back pain before all of this shit started and i still don’t know what that was, but it’s been gone for days now so it was either a tiny kidney stone that just bothered me for a little bit and passed or maybe it was pinched nerve pain all along. who can never be sure when you’ve got scoliosis and shitty little kidneys full of shitty little stones
that being said, i took to google again because i just wanted to see like...are there any illnesses that are just fever that comes and goes?
i think sometimes the flu can start out that way, where it’s just a fever in the beginning and then gradually other symptoms start to appear, but this is like...day three and i still don’t have any and not that i’m particularly keen for flu symptoms to show up, but...you’d think they’d be here by now is all
i did find, however, something called roseola ?? i’d never heard of it before and from what i can tell primarily kids get it, but it’s possible for all ages to get it.
it’s a viral thing where you have a high fever for several days and then when the fever is finally done you break out into a rash and that goes away on its own and so i’m just kind of curious like...maybe in another day or two if i’m going to suddenly see a rash show up and that might be my answer then
as best as i can tell, too, the treatment for it is exactly what i’ve been doing just...rest, drink lots of fluid, take tylenol to keep the fever down, rinse and repeat
and it would make sense too because like...i go around to a lot of different schools and see a lot of different little kids. i know on mondays alone i see about 175 sooooooooooooooo there’s that
also, my mom reminded me i wasn’t able to get all my MMR vaccines when i was little because i had a seizure after the first one (not something that is common, i was just a very sick child, please vaccinate your fucking kids) so that is also a very, very good reason i think i might wanna make a career change Very Soon
so yeah, that’s what i’ve got so far so i guess in the mean time i’m just going to stay on top of taking Tylenol in the evenings for the next two days probably and then see maybe if a rash shows up if nothing else new appears in the mean time. I’m hoping my strength will return soon because although i don’t have to teach tomorrow (thank fuck) i do tuesday, wednesday, and thursday so it’d really be nice to like...walk without needing to immediately sit down and rest for five minutes after? or stand for prolonged periods of time? i dunno, body, you think it over and let me know what you decide.
oh, also i got nicely baked because i figured i fuckin’ deserved it and would ya know it, i suddenly had an appetite again ?!
i literally went from taking two hours to eat a bowl of soup this afternoon to basically devouring a big plate of queso and hot sauce covered tators tots with a side of skillet cooked vegetarian buffalo wings like...thanks, bud.
...get it? bud? euhuhuhuhuhuh

4 notes
·
View notes
Text
Here’s the thing about pain management
I’m a chronically ill person with several chronic conditions and chronic pain. I have AS, Endo, as well as frequent headaches, GI issues, and joint pain that have yet to be diagnosed. Keep in mind that all of this has set in within the last year or so and, before that, I was quite healthy besides having PMDD. Pain management was not a part of my life like it is now.
As soon as you say “I’m in pain” or “I have chronic pain,” everyone has suggestions to fix it. They mean well. Some people even know what they’re talking about and have good suggestions. I just want to bring some attention to how difficult and complicated it can be to implement some very simple techniques. Keep in mind that I try to utilize all of these methods, but sometimes I’m not able to or they’re completely ineffective.
1. Get more sleep - This is a suggestion that I’ve taken completely to heart since my chronic fatigue has set in. More sleep is not an option. Unfortunately, as a student, getting all the sleep I need is nearly impossible. My body sometimes demands a ridiculous amount of sleep that makes it impossible to complete assignments and other tasks. I often have to decide: Do I want to sleep more and maybe feel a bit better, or complete this urgent responsibility and deal with the consequences?
2. Exercise - Because I have AS, I have to exercise. However, I only have around eight hours of energy per day to do everything I need to do before I crash. Exercise requires a lot of energy that sometimes needs to be devoted to dishes, homework, shopping, or taking a shower. My other symptoms also interfere with my ability to exercise. Have you ever tried to do yoga with a splitting headache, a fever, eye irritation, nausea, body aches, and back pain?
3. Medication - Of course I take medication. I take birth control to stop my periods for my endometriosis. Sometimes I have to take anti-inflammatories for my AS. The problem is that these medications do just enough good with just enough side effects that I can’t justify taking anything stronger. I can’t take NSAIDs all the time, even though they would help with pain, because that causes awful liver and kidney issues. NSAIDs also make me very tired so even if I take them, I’m practically useless for the rest of the day. Short-term side effects include dehydration, nausea, and constipation. Even the strongest NSAID doses don’t take care of the pain that much but the only other option is to either take VERY strong painkillers (highly addictive and very bad for long-term use) or biologics (which essentially weaken my immune system and increase my risk of cancer).
4. A change in diet - Oh I love some good fruits and vegetables. I can’t eat them as often as I’d like because of the expense (my medications cost quite a bit) and also because cooking and washing dishes can be physically painful for me. Stooping and scrubbing especially is murder on my back and can trigger a flare. Also, when I’m very nauseous from my endo or cocktail of NSAIDs I have to take sometimes, something very acidic like an orange or strawberry is murder on my stomach. I eat more canned soup and bread than I would like. (Btw, I’ve been tested for celiac and I don’t have it so leave me and my saltines alone)
5. Using CBD - I do use it but only sparingly because of the expense. During bad months when I’ve splurged and bought enough to truly help, I’ve spent around $100 buying stuff I need for just 3-4 weeks. That’s way too much.
6. Heat / cold therapy - I take a LOT of hot baths and use a lot of icy hot. My heating pad is my best friend. This can help with more muscular or surface-level pain but it doesn’t do much for my very deep pain in the joint capsules in my spine and it does nothing for my other symptoms like nausea or inflamed/dry eyes.
7. Massage therapy - Massages are wonderful but I’m not made of money. Insurance will not cover them so every massage costs well over $60 and relief is only temporary because it doesn’t address the underlying causes of my pain.
8. Essential oils - I’m not going to lie. I have a diffuser because essential oils just smell so nice. Has eucalyptus oil stopped my spine from trying to fuse together? Ehhhh not yet. I only use them for morale.
9. Mindfulness meditation - Yeah when people suggest this I’m inclined to think that they understand my pain as all in my head. It’s not. I have the blood work to prove it. Meditation can help me accept the pain that I’m experiencing and feel it with less panic but it doesn’t lessen the pain. I’m sorry but deep breathing doesn’t fix it.
10. Supplements - I’ve tried this before with far-fetched hopes that my body would perform slightly better with more folic acid. My problems are not caused by any nutritional deficiency so supplements don’t really help me. In fact, my gut is so sensitive that throwing an iron capsule in there can make me feel incredibly sick. I’m still experimenting with some supplements but I have no hope that they’re going to mitigate pain. I just want thicker hair, y’all.
11. Kratom - I’ve tried it and I think I may be slightly allergic. When I take a little, I feel no effect and when I take a lot, I still feel no effect except a very angry stomach.
12. Steroids, botox, and every other injection you’ve heard of - these are legitimately helpful for some conditions but not mine. When people suggest really specific and off-the-wall things either a) they have personal experience with this treatment for whatever reason and think it might help or b) they read an article about how someone got a shot of a miracle drug and never had another headache again. It’s almost always B.
13. Surgery - Never once has an actual medical professional suggested that I need surgery. I currently don’t. This one always comes from people who think the answer to a serious ailment is to go under the knife. I can see where they get this but no.
14. “Toughening up” - *Sigh* THIS IS NOT A SOLUTION TO ANYTHING. To a certain extent, everyone with chronic pain is implementing this strategy, but we all know that it takes a toll. Sometimes I have the option of continuing to do an activity even though it causes pain. Choosing this option almost always ends quite badly. Unless you can give me the next two days to recover, if I say I have to stop, I have to stop. Trust me. I’ve done the whole “just push through” thing enough times to know when I’m not going to be able to walk the next day.
Let’s imagine that I adopt every strategy at my disposal to cope with pain. Let’s imagine that I do an hour of PT every day, that I “eat clean,” take the strongest meds I can (even when they incapacitate other functions), get massages every week, meditate all the time, and sleep ten hours every day. If I do all of that, I might decrease my pain slightly but I’ll still have incurable illnesses causing more pain. Can you even imagine how much time and money it would take to lower my pain even a little? Pain management is important, of course, but it can’t be a full-time job and it certainly can’t be my life.
I kind of just need others to reach the same realization that I did: that I’m sick, I’m in pain, and this is the way things are now. I need help and I need to keep seeking treatment, but ultimately, I have very little control over the pain. I just have to try and manage it.
2 notes
·
View notes
Text
HEALTH UPDATE because I have been having some fun. TMI, etc.
So on the 24th of october, I had a really nasty attack of a particular pain that I’d had a few times before, but this time it sent me to the emergency room. It hit at about 1am; thankfully, my housemate was around to drive me in. We were there until 7 the next morning. Nothing much happened; we all kind of expected appendicitis at first, but it wasn’t really behaving like one, I didn’t have a high fever (or any fever - yet), and the timeline didn’t make sense, so they took some blood and just kind of observed me until I could move again, and decided it was safe to send me home.
The next several days were shitty. I was dealing with lingering pain and also a low-grade fever that has been messing with me on and off for a couple months, but has now been definitively linked to this pain. I went to my gp for an ultrasound ordered by the ER, and there they found a THING on my right ovary. This THING is believed to be a cyst, although exactly what type of cyst cannot be determined without surgery. The first report said it looked like one of two things: a dermoid cyst or an endometrioma. A second opinion from the ob/gyn they referred me to is that it’s unlikely to be the first one, much more likely an endometrioma given - oh right! - my history of excruciating periods, inflammation, disordered bleeding that drove me to get an IUD to make it stop, GI involvement, et fucking cetera it would be surprising if I don’t have endometriosis, honestly. It would explain a lot.
(I’m actually disappointed that it’s not a dermoid cyst. Dermoids are a type of teratoma, which, if you’re gross like me, you know frequently have teeth in them, and I wanted to ask my eventual surgeon to keep them for me. Like. Call me a disgusting medical goblin, but I wanted a little glass jar of teeth from the time my ovary bit me so hard I needed surgery. I was looking forward to the ovary dentata jokes. Oh, well.)
Endometriosis is not a fun thing to have at all. There are still a couple other possible things my THING could be, none of which anyone thinks is cancer, which of course would be the ultimate worst case scenario. But the prospect of an incurable, creeping disorder that debilitates and scars and can itself lead to cancer is hard enough to deal with. Cysts can also fuck you up in a number of ways; other than pain, which is draining my energy and making everything harder, I have a whole host of recurring symptoms that suggest this THING is leaking. But there’s nothing to be done unless it ruptures and becomes an emergency surgery instead of a scheduled one. Cool.
(Another side note: the low-grade fevers in particular have been wild because it’s only a difference of, like, 1.4 degrees {I normally run low. Like a possum}, but suddenly I’ll be all chatty and energetic, flushed and agitated, until it goes away, and then I’m exhausted. I mention this because it’s the one thing that online friends might notice - I’m here and then GONE, and back again at weird intervals.)
For right now, I’m just trying not freak out too much about having a growth the size of a ping pong ball hanging off an organ smaller than a grape while I wait for surgery. At the moment, it’s set for January 4th.
I think that’s about it. Thanks for reading; I can see myself being very anxious about this by January, and it makes me feel better knowing that people I like know why.
#gyn symptoms/discussion tw#not catastrophic news so don't worry; just not very pleasant news either#I may regret being so chatty tonight
5 notes
·
View notes
Text
— By Occupy Democrats | May 5, 2020

"I am a Covid ICU nurse in New York City, and yesterday, like many other days lately, I couldn’t fix my patient. Sure, that happens all the time in the ICU. It definitely wasn’t the first time. It certainly won’t be the last. What makes this patient noteworthy? A few things, actually. He was infected with Covid 19, and he lost his battle with Covid 19. He was only 23 years old.
I was destroyed by his clinical course in a way that has only happened a few times in my nursing career. It wasn’t his presentation. I’ve seen that before. It wasn’t his complications. I’ve seen that too.
It was the grief. It was his parents. The grief I witnessed yesterday, was grief that I haven’t allowed myself to recognize since this runaway train got rolling here in early March. I could sense it. It was lingering in the periphery of my mind, but yesterday something in me gave way, and that grief rushed in.
I think I was struck by a lot of emotions and realities yesterday. Emotions that have been brewing for weeks, and realities that I have been stifling because I had to in order to do my job effectively. My therapist tells me weekly via facetime that it’s impossible to process trauma when the trauma is still occurring. It just keeps building.
I get home from work, take my trusty companion Apollo immediately out to pee, he’s been home for 14 hours at a time. I have to keep my dog walker safe. No one can come into my apartment.
I’ve already been very sick from my work exposure, and I’m heavily exposed every day that I work since I returned after being 72 hours afebrile, the new standard for healthcare workers. That was after a week of running a fever of 104 even with Tylenol around the clock, but thankfully without respiratory symptoms. I was lucky.
Like every other healthcare worker on the planet right now, I strip inside the door, throw all the scrubs in the wash, bleach wipe all of my every day carry supplies, shoes and work bag stay at the bottom of the stairs.
You see, there’s a descending level of Covid contamination as you ascend the stairs just inside my apartment door. Work bag and shoes stay at the bottom. Dog walking shoes next step up, then dog leash, then running shoes.
I dodge my excited and doofy German shepherd, who is bringing me every toy he has to play with, and I go and scald myself for 20 minutes in a hot shower. Washing off the germs, metaphorically washing off the weight of the day.
We play fetch after the shower. Once he’s tired, I lay on the floor with him, holding him tight, until I’m ready to get up and eat, but sometimes I just go straight to bed.
Quite honestly, I’m so tired of the death. With three days off from what has been two months of literal hell on earth as a Covid ICU nurse in NYC, I’m having an evening glass of wine, and munching on the twizzlers my dear aunt sent me from Upstate NY, while my dog is bouncing off the walls because I still don’t have the energy to run every day with him.
Is it the residual effects of the virus? Is it just general exhaustion from working three days in a row? Regardless, the thoughts are finally bleeding out of my mind and into a medium that I’m not sure could possibly convey the reality of this experience.
There’s been a significant change in how we approach the critically ill covid-infected patients on a number of different levels over the last two months. We’re learning about the virus. We’re following trends and patterns. We are researching as we are treating.
The reality is, the people who get sick later in this pandemic will have a better chance for survival. Yet, every day working feels like Groundhog Day. All of the patients have developed the same issues. This 23-year-old kid walked around for a week silently hypoxic and silently dying. By the time he got to us, it was already far too late.
First pneumonia, then Acute Respiratory Distress Syndrome (ARDS), essentially lung failure. Then kidney failure from global hypoxia and the medications we were giving in the beginning, desperately trying to find something that works. Then learning that it doesn’t work, it’s doing more harm than good in the critical care Covid population.
Dialysis for the kidneys. They are so sick that your normal three-times weekly dialysis schedule is too harsh on their body. They’re too unstable. So, we, the ICU nurses, run the dialysis slowly and continuously.
They are all obstructing their bowels from the ever-changing array of medications, as we ran out of some medications completely during our surge. We had to substitute alternatives, narcotics, sedatives, and paralytics, medications we’re heavily sedating and treating their pain with, in an effort to help them tolerate barbaric ventilator settings.
Barbaric ventilator settings while lying them on their bellies because their lungs are so damaged that we have to flip them onto their bellies in an effort to perfuse the functioning lung tissue and ventilate the damaged lung tissue. Ventilator pressure settings that are so high that some of their lungs are being blown out completely in an effort to give them enough oxygen, because lung-protective ventilation measures aren’t working for these patients.
Lungs that are perfused with blood that doesn’t even have adequate oxygen carrying capacity because of how this virus attacks.
Blood that clots. And bleeds. And clots. And bleeds. Everything in their bodies is deranged. Treat the clots with continuous anticoagulation. Stop the anticoagulation when they bleed.
GI bleeds, brain bleeds, pulmonary emboli, strokes. The brain bleeds will likely die. The GI bleeds get blood transfusions and interventions.
Restart the anticoagulation when they clot their continuous or intermittent dialysis filters, rendering them unusable, because we’re trying not to let them die slowly from renal failure. We are constantly making impossible treatment decisions in the critical care pandemic population.
A lot of people have asked me what it’s like here. I truly don’t have adequate descriptors in my vocabulary, try as I might, so I’ll defer to the metaphor of fire.
We are attempting to put out one fire, while three more are cropping up. Then we find out a week or two later that we unknowingly threw gasoline on one fire, because there’s still so much we don’t know about this virus.
Then suddenly there’s no water to fight the fire with. We’re running around holding ice cubes in an effort to put out an inferno. Oh yeah, and the entire time you’ve been in this burning building, you barely have what you need to protect yourself.
The protection you’re using, the guidelines governing that protection, evolved with the surge. One-time use N95? That’s the prior standard, and after what we’ve been through, that’s honestly hysterical. As we were surging here, the CDC revised their guidelines, because the PPE shortage was so critical.
Use anything, they said. Use whatever you have for as long as you can, and improvise what you don’t have.
As we’re discussing medication and viral research, starting clinical trials, talking treatment options in morning rounds for your patient with the team of doctors and clinical pharmacists, suddenly, surprise! Your patient developed a mucous plug in his breathing tube.
Yes, that vital, precious tube that’s connected to the ventilator that’s breathing for them. It’s completely plugged. Blocked. No oxygen or carbon dioxide in or out. It’s a critical emergency.
Even with nebulizer treatments, once we finally had the closed-delivery systems we needed to administer these medications and keep ourselves safe, they’re still plugging. We cannot even routinely suction unless we absolutely have to because suctioning steals all of the positive pressure that’s keeping them alive from the ventilator circuit. One routine suction pass down the breathing tube could kill someone, or leave their body and vital organs hypoxic for hours after.
Well, now they’re plugged. We are then faced with a choice. Both choices place the respiratory therapists, nurses, and doctors at extremely high risk for aerosolized exposure.
We could exchange the breathing tube, but that could take too long, the patient may die in the 2-3 minutes we need to assemble the supplies and manpower needed, and it’s one of the highest-risk procedures for our providers that we could possibly carry out.
Or we could use the clamps that have been the best addition to my every day carry nursing arsenal. You yell for help, you’re alone in the room. Your friends and coworkers, respiratory therapists, doctors, are all rushing to get their PPE on and get into the room to help.
You move around the room cluttered with machines and life sustaining therapies to set up what you need to stave off death. You move deliberately, and you move FAST. The patient is decompensating in the now-familiar and coordinated effort to intervene.
Attach the ambu bag to wall oxygen. Turn it all the way up. Where’s the PEEP valve? God, someone go grab me the PEEP valve off the ambu bag in room 11 next door. We ran out of those a month ago, too. It’s all covid anyway, all of it is covid. Risk cross-contamination or risk imminent death for your patient, risk extreme viral load exposure for you and your coworkers, and most certain death for your patient if you intervene without a PEEP valve.
You clamp the breathing tube, tight. The respiratory therapist shuts off the ventilator, because that side of the circuit can aerosolize and spray virus too if you leave it blasting air after you disconnect. Open the circuit. Respiratory therapy attaches the ambu bag. You unclamp. Bag, bag, bag. Clear the plug. The patient’s oxygen saturation is 23% with a PERFECT waveform. Their heart rate is slowing. Their blood pressure is tanking. Max all your drips, then watch and wait while this patient takes 3 hours to recover to a measly oxygen saturation of 82%, the best you’ll get from them all shift. These patients have no pulmonary reserve.
All of our choices to intervene in this situation risk our own health and safety. In the beginning we were more cautious with ourselves. We don’t want to get sick. We don’t want to be a patient in our own ICU. We’ve cared for our own staff in our ICUs. We don’t want to die. Now? I’ve already been sick. I am so, so tired of the constant death that is the ICU, that personally, I will do anything as long as I have my weeks old N95 and face shield on, just to keep someone alive.
I’ve realized that for many of these patients in the ICU, it won’t matter what I do. It won’t matter how hard I work, though I’ll still work like a crazy person all day, aggressively advocate for my patients in the same way.
My coworkers will go without meals, even though they’re being donated and delivered by people who love and support you. Generous people are helping to keep local restaurants afloat. We can always take the meal home for dinner, or I can devour a slice of pizza as I walk out to my truck parked on the pier, a walk I look forward to every day, because it gives me about eight minutes of silence. To process. To reflect.
I’ll chug a Gatorade when I start feeling lightheaded and I’m seeing stars, immediately after I just pushed an amp of bicarb on a patient and I know I have at least five minutes of a stable blood pressure to step out of the unit, take off my mask and actually breathe.
Every dedicated staff member is working tirelessly to help. The now-closed dental clinic staff has been trained to work in the respiratory lab to run our arterial blood gases, so that the absolutely incredible respiratory therapists who we so desperately need can take care of the patients with us.
Nurses in procedural areas that were closed have been repurposed to work as runners. To run for supplies while the primary nurse is in an isolation room trying to stabilize a patient without the supplies they need, runners to run for blood transfusions.
Physical therapists, occupational therapists, speech and language pathologists being repurposed to be part of the proning teams that helps the nurses turn patients onto their backs and bellies amidst a tangled web of critical lines and tubes, where one small error could mean death for the patient, and exposure for all staff.
Anesthesiologists and residents are managing airways and lines when carrying out these massive patient position changes. Surgical residents are all over the hospital just to put in the critical invasive lines we need in all of our patients.
The travel nurses who rushed into this burning building to help us are easing a healthcare system. The first travel nurse I met came all the way from Texas. Others terminated their steady employment to enlist with a travel agency to help us. Every day there are more travelers arriving.
A nurse from LA came to me after she found out I was part of the home staff, in my home unit, where this all first started in my hospital what feels like a lifetime ago, and said, “I came here for you. For all of the nurses. Because I couldn’t imagine working the way you guys were working for how long you were working like that”. During our surge and peak in the ICU, we were 1:3 ratios with three patients who normally would be a 1:1 assignment. And they were all trying to die at the same time. We were having to choose which patients we were rushing to because we couldn’t help them all at the same time.
The overhead pages for emergencies throughout the hospital rang out and echoed endlessly. Every minute, another rapid response call. Another anesthesia page for an intubation. Another cardiopulmonary arrest. A hospital bursting at the seams with death. Refrigerated trailers being filled.
First it was our normal white body bags. Then orange disaster bags. Then blue tarp bags. We ran out of those too. Now, black bags.
The heartbreakingly unique part of this pandemic, is that these patients are so alone. We are here, but they are suffering alone, with no familiar face or voice. They are dying alone, surrounded by strangers crying into their own masks, trying not to let our precious N95 get wet, trying not to touch our faces with contaminated hands.
Their families are home, waiting for the phone call with their daily update. Some of their loved ones are also sick and quarantined at home.
Can you even IMAGINE? Your husband or wife, mother or father. Sibling. Your child. You drop your loved one off at the emergency department entrance, and you never, ever see them alive again.
Families are home, getting phone calls every day that they’re getting worse. Or maybe they’re getting better. Unfortunately, the ICU in what has quickly become the global epicenter for this pandemic is not a happy place. We are mostly purgatory where I work, so this snapshot may be more morbid than most.
These people are saying goodbye to their loved ones, while they’re still walking and talking, and then maybe a week or two later, they’re just gone. It’s like they disappeared into thin air.
That level of grief is absolutely astounding to me, and that’s coming from a person who knows grief. It changes you immeasurably.
But this grief? This pandemic grief? It’s inconceivable. These families will suffer horribly, every day for the rest of their lives. They might not even be able to bury their loved one. God, if they can’t afford a funeral with an economic shut-down, their loved one will be buried in a mass grave on Hart Island with thousands of others like them. What grave will they have to visit on birthdays and holidays?
Yesterday, I was preparing for a bedside endoscopy procedure to secure a catastrophic GI bleed in this 23-year-old patient.
It was a bleed that required a massive transfusion protocol where the blood bank releases coolers of uncrossmatched O negative blood in an emergency, an overhead page that, ironically, I heard as I was getting into the elevator to head to the fourth floor for my shift yesterday morning; a massive transfusion protocol that I found out I would own as a primary nurse, as I desperately squeezed liters of IV fluids into this patient until we got the cooler full of blood products, and then pumped this patient full of units of blood until we could intervene with endoscopy.
Before the procedure, I stopped everything I was doing that wasn’t life-sustaining. I stopped gathering supplies to start and assist with the procedure.
I told the doctors that I would not do a required “time-out” procedure until I got my phone out, and I facetimed this kid’s mom because I didn’t think he would survive the bedside procedure.
She cried. She wailed. She begged her son to open his eyes, to breathe. She begged me to help her. Ayudame. Ayudame. She begged me to help him. She sang to him. She told him he was strong. She told him how much she loved him. I listened to her heart breaking in real time while she talked to her son, while she saw his swollen face, her baby boy, dying before her eyes through a phone.
Later in the day, after the procedure, his mom and dad came to the hospital. He survived the securement of the bleed, but he was still getting worse no matter what we did. He’s going to die. And against policy, we fought to get them up to see their son.
We found them masks and gowns that we’re still rationing in the hospital, and we let his parents see him, hold him. We let them be with their son.
Like every other nurse would do in the ICU here, I bounced around the room, moving mom from one side of the bed to the other and back again, so I could do what I needed to do, setting up my continuous dialysis machine, with the ONE filter that supply sent up for my use to initiate dialysis therapy. This spaceship-like machine, finicky as all hell, and I had one shot to prime this machine successfully to start dialysis therapy to try to slowly correct the metabolic acidosis that was just ONE of the problems that was killing him as his systolic blood pressure lingered in the 70s, despite maxing all of my blood pressure mediations.
Continuous dialysis started. You press start and hold your breath. You’re not removing any fluid, just filtering the blood, but even the tiniest of fluid shifts in this patient could kill him. But you have no choice.
His vital signs started to look concerning. I could feel the dread in the pit of my stomach, this was going south very quickly. Another nurse and the patient’s father had to physically drag this mother out of the room so we could fill the room with the brains and eyes and hands that would keep this boy alive for another hour.
She wailed in the hallway. Nurses in the next unit down the hall heard her cries through two sets of closed fire doors. We worked furiously to stabilize him for the next four hours.
Twenty minutes before the end of my shift last night, I sat with the attending physician and the parents in a quiet and deserted family waiting room outside the unit. I told his mother that no matter what I do, I cannot fix this. I have maximized everything I have, every tool and medicine at my disposal to save her son. I can’t save her son.
The doctor explained that no matter what we do, his body is failing him. No matter what we do, her son will die. They realized that no matter how hard they pray, no matter how much they want to tear down walls, no matter how many times his mother begs and pleads, “take me instead, I would rather die myself than lose my son”, we cannot save him.
We stayed while she screamed. We stayed until she finally let go of her vice grip on my hands, her body trembling uncontrollably, as she dissolved into her grief, in the arms of her husband.
This is ONE patient. One patient, in one ICU, in one hospital, in one city, in one country, on a planet being ravaged by a virus.
This is the tiniest, devastating snapshot of one patient and one family and their unimaginable grief. Yet, the weight is enormous.
The world should feel that weight too. Because this grief, this heartbreak is everywhere in many forms. Every person on this planet is grieving the loss of something.
Whether that’s freedom or autonomy sacrificed for the greater good. Whether that’s a paycheck or a business, or their livelihood, or maybe they’re grieving the loss of a loved one while still fighting to earn a paycheck, or waiting for government financial relief that they don’t know for certain will come. Maybe they’re a high school senior who will never get to have the graduation they dreamed of. Maybe they’re a college senior, who won’t get to have their senior game they so looked forward to. Maybe they’re afraid that the government is encroaching on their constitutional rights. Maybe it’s their first pregnancy, and it’s nothing like they imagined because of the terrifying world surrounding them.
Or maybe they lost a loved one, maybe someone they love is sick, and they can’t go see them, because there are no visitors allowed and they’re an essential worker. Maybe all they can see of someone they love is a random facetime call in the middle of the day from an area code and a number they don’t know.
Everyone is grieving. We’ve heard plenty of the public’s grief.
I don’t blame anyone for how they’re coping with that grief, even if it frustrates the ever-living hell out of me as I drown in death every day at work. It’s all valid. Everyone’s grief is different, but it doesn’t change the discomfort, the despair on various levels. We are at the bottom of Maslow’s hierarchy of needs. Basic survival, physiological and safety needs. I’ve been here before. I know this feeling. How we survive is how we survive.
Now that I’ve had the time to reflect and write, now that I’ve let the walls down in my mind to let the grief flood in, now that I’ve seen this grief for what feels like the thousandth time since the first week of March as a nurse in a Covid ICU in New York City, it’s time you heard our side. This is devastating. This is our reality. This is our grief."
— Jeannine Nicole
0 notes
Text
Roundup of my mentions of EIAn
I'm seeing a new immunologist today, so I'm trying to prepare for the appointment. Especially since she seems to be one of the ones who barely "believes in" MCAS, and certainly not without high tryptase, which I've never tested above normal on before. But it seems like for some people she's still good at treating the symptoms, even if she calls it different things. So I'm trying to list out all my symptoms. But, naturally, my brain feels dead today, and it's hard to think of stuff. Therefore, I'm trying to gather things I've said about it online recently, and I figured I'd just do that here so that I wont lose it next time I need to reference this! Exercise Induced Anaphylaxis:
“ A year after my #MCAS diagnosis and a month after my long suspected Exercise Induced Anaphylaxis diagnosis, I finally got my first epi pens today. And about 7 years after I got my #VCD dx, I finally got a speech therapy referral! I spent most of this month in a terrible flare so I'll try whatever at this point. 😱 “
Facebook post in a Dysautonomia Group
(Oct 2019)
Does anyone know the WHY, biologically (not just "bc that's what dysautonomia does," but specifics!) that often when I stand up for too long, like today when shopping, instead of normal presyncope where the head symptoms predominate, I'll just start overheating, and then it feels like my post-eating reactions sometimes, where it'll feel like all my blood is rushing to my guts and they are liquifying most uncomfortably. When I sit down, it's significantly better.
I get the blood pooling in the legs, gravity and all, but why does it sometimes seem to pool in my guts just from being upright?!
This has happened ever since I can remember, in fact as a teen I associated it with libraries, as if go and stand around for ages looking at books, and would always get such angry guts. My lightheaded regular presyncope seems to have developed in my early 20s, but this one has been around a lot longer longer.

“ I got my free lifetime access pass to national parks system today! Such a great program! ❤️❤️I almost felt bad for it, as it's such a great deal, until a 3 minute walk on a path to a waterfall (that a 2 year old was walking himself), which has an accessible trail that was still in progress of being made, made my lungs burn to the point of almost throwing up. So, nm, I don't feel bad for getting a free pass to places I can really only enjoy via the car (which I can't even drive myself). But, I am very grateful for it! If you're an American who has a doctor sign off that you have a lifelong disability of any sort, you can get one of these! “
Exercise-Induced Anaphalaxis test.
(Mar 2019)
Ah, irony. Literally the first time IN MY LIFE I have done cardio and not reacted. ENTIRELY different from my cardiac exercise test last year where all the symptoms started up I started blacking out and it took 15 minutes to be able to leave the table the tech dragged me onto when he had to pull me off the treadmill and not almost puke and over a half hour before I was able to leave the waiting room bc I was flat on the floor, legs up, trying to breath and not puke and get the rest of my body able to move again and perhaps be less tomato-red, sweaty, and scary looking.)
For the first time in my entire life, I did intense cardio (well, only for a minute or two), and didn't react (tho my lungs burned like a mfer and I was still coughing 15+ minutes later, which does always happen too, but none of the other things did, like tanking BP and skyrocketing HR, extreme gi upset, throat swelling, blacking out.. Not even Flushing which happens first and to an absurd degree (in gym classes my level of redness would always scare my gym teachers)
MCAS hates cleaning
(Feb 2019)
me: *cleans in a flurry of bodily movement* mast cells: ALERT! ALERT! IS THIS AN ALL OUT BODY INVASION THREATENING YOUR VERY LIFE??? ALL HANDS ON DECK!!! *releases like, all 200 mediators* me: um, no, it's okay, I'm just making the bed and tidying and taking out the trash???? This isn't even cardio!! I am literally barely doing more than just walking!! mast cells/body: *turns face tomato red and burns like i have a horrible fever* *circulatory system forgets how to push blood up against gravity* *heart flutters at full speed* *body overheats* *lungs burn, throat burns* *gets out of breath* *starts to sweat* *gets pre-pre-syncope-y* me: um okay fine. this is fine, sure. *has to sit every 3 minutes so it doesn't progress further (GI revolt & throat swelling would be up next)* *is unable to do all the things*😒😩
Exercise Induced Anaphalaxis during a super mild bike ride this morning. SIGH
(Dec 2018)
1.2 mile bike ride to the place where we've been dropping the mice we catch in our house reminded me that I'm still a total mess. By the time we got there I had just started coughing and feeling like my lungs were goopy (first step in my exercise-induced anaphalaxis when it's a slow-build)
We were there like 20 minutes, I thought I was mostly okay so we started on the .8mile ride to the coffee shop I'm currently at.... My eyes didn't register an incline in the street at all but my body sure AF did. Within 3 minutes my lungs were ON FIRE... I have a very visual brain and so I had this mental image of someone holding a lighter up to the cillia of my lungs and burning it all off. It hurt a lot. The coughing started again and my ..idk, neck area? got all tingly like it does before I throw up. Breathing was troublesome. I stopped and stood there and my face started feeling hot and sweaty.
I walked the bike slowly only a tiny distance to the top of the 'incline' and glided down, but then it got to a flat part again, and normally that would have been fine, but since my chemical soup hadn't settled down yet it just put me right back in it. We slowly cruised one block to the coffee shop and I was out of breath (it's not quite wheezing but it feels close, just without any wheezing sound) and it was all back with a vengeance.
Facebook Post
(Nov 2018)
Anyway, I'm tentatively excited about this. Because my #1 biggest problem with my MCAS is how severely my body reacts to even the smallest amount of cardio, as in it legit starts anaphalaxis RIGHT AWAY (I rode my bike on a not-even-noticable-unless-youre-me incline last weekend, I stopped several times (less than a mile distance!) and it still started!). The throat swelling in reaction to everyday triggers has mostly been controlled by my new MCAS med regiment (yay!) but it doesn't do anything for the exercise-induced anaphalaxis.
This weekend, though, I was actually reading up on what teeny tiny amount of research *has* been done on exercise-induced anaphalaxis so far, and the one and only treatment they've found that has worked (though not for everyone) has been cromolyn (and the other mcas med that starts with an O-- i forget the name). It is, interestingly, also a medicine that IS used for exercise-induced asthma as well, too (which is what i was diagnosed with starting in elementary school (and the inhalers were unsurprisingly useless) but then an asthma dr in my 20s said I didn't have it..).
But like, what if this works?? What if I can actually.. ride bikes? Go on an actual hike?? DANCE?? (I had to quit dance as a kid bc of health and that still makes me sad..) :-o :-o :-o
She said that a lot of her MCAS patients also have a huge reduction in brain fog with this, too. Not all, but many. Having consistently good brain days is even more unbelievable for me to even think about. But I sure as heck am crossing my fingers.
MCAS is also implicated in my dysautonomia (along with my neck/spine instability and squished spinal cord..), interstitial cystitis and other conditions (mast cells are all over and thus wreck havok all over) so.. who knows what all might get better!
Exercise-Induced Anaphalaxis
(Sep 2018)
Even as a kid, whenever I'd do gym class or try to do anything cardio-y, I would get TOMATO RED, itchy, sweat buckets, struggle to breathe because my throat felt so constricted, have an upset stomach, feel like I was about to pass out, and feel like death in general. As a kid I was diagnosed with exercise-induced asthma. Inhalers never did anything though.
0 notes
Text
A Cannabis Treatment Protocol for Cohn’s Condition. What Helped Me

My experience treating myself with medical cannabis is that it was an accomplishment of experimentation which was both costly and also lengthy, but that's probably the way it need to be. People are not carbon duplicates of each various other and also there is no factor to think that Huge Pharma poisonous substances will certainly affect different people the same way although that is the lie we have been informed.
Likewise, individuals will respond in a different way to various marijuana stress, products as well as dosages as well as the only method to discover something that you recognize will benefit you is to attempt it. I was recommended in the starting to document my treatment progression to aid me figure this out in a well organized means yet I was as well ill and really did not have the psychological, physical or psychological gets to document anything.
The "budtenders" at the marijuana shops played a very minor supportive role by defining one of the most usual uses as well as results in reducing different signs but possibly their best guidance was that "the nose recognizes." When it come to entire blossom marijuana (bud) you are meant to inhale the fragrance of the various pressures as well as the ones that smell the very best to you are the ones you should attempt as well as certainly the ones that scent offending to you are best avoided.
Comparison that sage as well as benign guidance with that said of Large Pharma especially in the case of Crohn's and also other autoimmune and persistent illnesses where we are advised and expected to take Large Pharma toxins that we understand make us really feel even worse.
In my situation, I needed to travel out-of-state to treat lawfully with medical cannabis as well as I had a terrible influenza when I got right here so I began with fresh marijuana juice and Buy CBD Suppositories CBD-oil infused edibles to begin with to make sure that I didn't have to smoke. I likewise did not and still do not delight in the psychoactive "high" of cannabis so I was confident these items would offer me some alleviation without requiring to try the THC products that would certainly make me stoned.
I may've simply been also sick or my illness too major but these items provided me definitely no obvious relief. I next attempted taking a percentage of THC-infused edible in the evening which did not touch my discomfort whatsoever however which aided me rest. That was the first real relief I found as well as I continued looking for something that would certainly knock senseless my complete body joint as well as body pain, fevers and also different deep gut pains as well as intestinal symptoms of my illness. At some point I found that I needed to smoke whole flower marijuana (bud) to get any pain relief at all as well as I tried lots of stress. Indica or indica-dominant hybrid pressures were my preference as sativa pressures gave me the analytical head-high I did not desire.
Smoking indica strains aided substantially with my body as well as joint discomfort and somewhat with my gut as well as GI pain and also signs and symptoms. Finally, I found that vaping concentrates permeated even the inmost gut discomfort and also signs as well as I had ultimately, ultimately found alleviation. I simply "overcame" my previous hostility to being essentially constantly stoned and hunkered down for the long run of recovery myself as well as alleviating my disabling pain.
I kept using the non-psychoactive juice and also CBD items as dietary supplements and concentrated on sampling various items as well as indica strains to treat certain signs and symptoms like nausea and also helping me procedure and digest food.
I began making use of a transdermal substance topically on my abdomen as well as right flank which produced an enjoyable cooling sensation that partially extinguished the burning, bloating, pulling, itching and also various other sensations in my gut and over my liver area. I discovered that smoking throughout dishes aided with my queasiness, disinterest in food as well as "anorexic" kind signs of a Crohn's flare. I took a bite or 2 of food complied with by a bong hit and also maintained it till I didn't wish to eat anymore. I would certainly acquire a small amount of a number of different strains each time as well as attempt them out during meals or before bed.
Although I did not have a cancer diagnosis, I really felt drawn to try the Rick Simpson Oil (RSO) protocol where I slowly worked my means up to consuming 1 gram (1000 mg) of cannabis oil a day or 60 grams in 90 days.
This is a very high dose as well as I don't assume I ever before made it to the full gram a day but I make certain I ingested the full 60 grams of marijuana oil and after that some by spraying a slim line of oil onto a cannabis-infused fool as well as letting it liquify over a hr or so. I did that everyday for possibly 9-12 months. The very last point I did before bed to extinguish my relentless deep intestine pain was to take 30-50mg indica edible (about 3-5x a conventional leisure dosage), take 3 or 4 hits from a joint, regarding 2 attracts from a vape pen having concentrated oil or resin, and I rested well as well as primarily might not feel my digestive tract at all up until I got up in the early morning.
The discomfort alleviation was exquisite however cannabis pain relief is not a numbing kind feeling numb where you don't feel it anymore in any way, or where you are tricked into believing that you are no more sick, or a superhero. It just really feels a lot various and much less aggravatingly relentlessly excruciating than it was before and mentally you remain in a better position to handle any continuing to be feelings also. It's tough to define however it was and is wonderful pain relief.
Also after sleeping very well, I constantly got up sweaty, nauseated, suffering and also drastically bloated so I would certainly take 25mg of a THC/CBD combination edible as soon as I woke up as well as return to rest or simply rest in bed until it started working, typically 30-60 mins. Then I would certainly stand up as well as do whatever jobs I required to perform around your home and also if I needed to drive anywhere I would certainly wait until later in the day when the early morning dose had actually worn off.
Occasionally when it wore off I was too sick to go anywhere so I would certainly just hunch down as well as medicate once more up until I felt far better and try to go out the following day and so on. When I really did not leave my home for a number of months as well as had Amazon.com deliver food and feline litter so I really did not have to bother with being too ill to go out or needing to medicate just to be well adequate to drive.
At some point I discovered that cannabis transdermal spots kept me at a wonderful degree for 24 to 48 hours and also this item was really game-changing for me as I was still comfortably medicated when I awakened in the morning-- this was vital. I likewise did not have to bother with obtaining "also low" otherwise obtaining "expensive" as well as constantly thinking of medicating as well as medicating and so on. Some people use a fifty percent a patch as well as leave it on for two days yet I located I require 2 spots and to alter them every 1 day if I am really sick or every two days if I'm feeling a little much better.
This is the product that has most boosted my lifestyle as it is both low-maintenance and also effective. Contrasted to various other delivery approaches the patches are a relatively reduced dosage and also are absorbed straight into the bloodstream without needing to go through the gut possibly making them excellent for people with conditions of malabsorption like Crohn's. I do not get any recognizable "high" from the spots as well as make use of one 1:1 ratio THC/CBD patch and also one fully CBD patch at the very same time.
I likewise made my very own marijuana suppositories with cocoa butter, coconut oil and cannabis oil. As soon as the patches quit my regularity, digestive tract spasms as well as looseness of the bowels I had the ability to utilize this delivery method and it appeared to function rather well for discomfort alleviation and also sensations of despair without providing me the head-high I really did not want. I made each suppository with about 30mg overall THC as well as made use of a couple of each day for a couple of months.
I discovered that this was additionally an excellent way to use up different concentrates that I had actually attempted that I really did not look after such as where I got numerous doses of a concentrate wholesale that gave me undesirable sativa kind impacts that I really did not desire and also had not been expecting. I just melted the focuses right into the chocolate butter and coconut oil and monitored the complete mg of THC I was putting into the blend to ensure the end product was the dosage I wanted.
I also began a 100% organic and also fermented organic diet plan together with high-grade organic or non-GMO supplements. After regarding a year on the cannabis and after that switching to this diet regimen for 6 months I began to really feel as if I was truly healing rather and not just concealing the pain.
I didn't need to smoke during dishes anymore and I was moderately thinking about food once more. I attempted to consume raw fermented organic foods a minimum of 3 or 4 times a day so I found that kombucha tea in the morning, miso soup in the afternoon and also some sort of raw sauerkraut, pickle (or their juice) throughout the day functioned well. I saw a significant renovation at one factor after I had actually included a fruit and vegetable juice based supplement to my regimen. I have no suggestion if it was actually doing anything but I was feeling progressively much better. I was likewise taking a multivitamin and also numerous probiotic supplements and purchased an infrared heating mat which was supposed to be valuable for discomfort and other things.
I laid on the floor covering for numerous hrs a day usually at night as well as if nothing else it was kicking back as well as helped my body as well as joint discomfort. And although pure CBD products not did anything to soothe my pain at first, once I began feeling better I found that CBD-infused edibles as well as tinctures do take the edge off and I use them sometimes if I am coming to be bewildered with pain and also do not want to be high simply after that. I can additionally handle most of my present discomfort as well as symptoms with edibles and also patches and also currently rarely require to either smoke or vape.
Presently I have actually been overcome paying for supplements or fermented food as well as have been consuming GMO food periodically also. My signs are beginning to find back and I am again fighting with anorexia nervosa, heartburn, bloating, joint discomfort as well as digestion signs and symptoms but thankfully I am still able to obtain discomfort remedy for marijuana.
At first, if Western medication as well as Huge Pharma had supplied me easy discomfort relief with no recovery whatsoever I would have settled for that but Huge Pharma has absolutely nothing in its toolbox that can touch the deep gut as well as various other discomfort of Crohn's disease and which isn't contraindicated for creating even more GI signs.
Now that I have actually experienced true recovery and signs and symptom relief as opposed to simply discomfort relief clearly I wish to have both as well as the natural as well as fermented diet plan combined with supplements and also cannabis seem to work best when utilized together. As my finances have actually been depleted and also my health is once more declining, I do not know what the future will hold for my illness, my therapy or my life.
Obviously, I have likewise found significant discomfort remedy for my 2 embraced felines who constantly rest with me when I remain in serious discomfort as well as their presence has been greatly reassuring. Staying in a gorgeous, serene rural area has possibly aided too, in addition to having left a bad connection and also an uneasy living circumstance in my prior life, prior to I vacated state to legitimately treat with clinical cannabis.
Initially of my cannabis trip I have actually been fended off at the degree of consumerism I now technique in order to regulate my symptoms and get relief from this condition and this blog post is urging consumerist solutions which I do not appreciate. But for any person that desires this details, I want to make it readily available.
Possibly it will certainly conserve someone time, money or energy at the beginning of their very own journey and also they will certainly get relief as swiftly as feasible which for those suffering the gruesome physical impacts of autoimmune condition may be the most effective we can wish for.
What I understand for specific is that Western medicine has absolutely nothing to supply to help me heal or even mask the discomfort, development or crippling signs and symptoms of Crohn's but they will certainly still force me to take their inefficient toxins anyhow if I ultimately need to go to them for help. I will resist that end result with every ounce of my continuing to be stamina and am identified not to let Western medicine once again sink its violent, inept claws right into me and also this terrible illness also they recognize they can't deal with.
0 notes
Text
COVID-19: My family’s experience
On Sunday March 15, my younger sister called me crying. She had temperature of 101OF and a blinding headache, but it was an important day at her job, and she knew her supervisor really needed her help. “Stay home,” I said. “Tell him you’re sick, he’ll understand. Even if there wasn’t an emerging global pandemic, you’re legitimately sick. He’s understanding, this won’t affect your job at all. And call your doctor if the fever sticks around… If it was COVID-19, I would tell you just stay home, but it doesn’t sound like it, maybe you have something bacterial.” The next morning, things were about the same, so she called her doctor’s office and was advised to come in. A nurse wearing a gown, mask, and gloves took throat and nasal swabs. When the doctor came into the exam room, he was dressed similar, and stood at the farthest corner from her. “Well, rapid strep and flu are negative. We don’t test for it, but assume you have COVID-19. Go home and quarantine.”
At that point, believe it or not just three weeks ago, we only believed COVID-19 as a respiratory infection. She called me scared, suddenly afraid she might have a life-threatening illness. “Why would they say, just assume? What does this mean for me?” She lives with my 60-year-old mother, who had been dropping off groceries at her 85-year-old mother since the first reported case. Everyone had been doing their part at social distancing, but was it enough? I reached out to the New York State Department of Health for guidance. “That’s ridiculous,” they told me. “She has no respiratory symptoms, without coughing she can’t spread droplets, and if they considered her a Person Under Investigation, they should have referred her for testing.” Within a week, we would find that every single one of those instructions had become obsolete or been proven incorrect. As the days progressed, she began to vomit excessively, unable to even keep water down. The fever continued. By that point, I began to hear reports from friends and colleagues on the front lines about younger patients presenting with GI or other atypical symptoms, and the daily reports I received from my mother had me more and more concerned. Friday the 20th, I contacted the DOH again. The hold time was 100 minutes. I described her symptoms, and this time they took down her information so they could contact her with a testing site and time, advising that she must come alone so as not to expose anyone else. Saturday evening, my mother called me frantic. After vomiting all day, my sister was too weak to sit up and while she wasn’t disoriented, she was acting euphoric- that’s medical speak for “she knew who she was and where she was but sounded high as a kite”. My concerns about dehydration, lurking in the back of my mind when the vomiting began, started creeping to the forefront. I contacted several urgent cares in her neighborhood, looking for someone who could administer IV fluids and do bloodwork. The answers were all the same: urgent cares aren’t designed for isolation; they aren’t seeing anyone who is suspected COVID-19. Desperate, I reached out to friends who are active EMTs and live closer to her to see if anyone could evaluate her. In full isolation gear, a friend went over to see her. “Look, she’s sick. She’s really sick,” he told me. “Any other time, any other virus, she probably would be hospitalized. But this time, she won’t be. I’ve been in the EDs, they’re overflowing. She’ll wait, and ultimately, she probably won’t get a bed. There’s just too many people sicker than her.”
Nobody slept that night. The next morning, the DOH called to give her an appointment slot the following day at a public park 18 miles away. Going alone wasn’t an option anymore, she could barely sit up let alone drive. So, Monday morning my mother packed her, a blanket, and a bottle of Powerade, into the car and made the trip up to what I now refer to as their “black ops testing experience”. At the entrance to the park, they were stopped by the National Guard, in uniform, with yellow safety vests and surgical masks. “Hold your ID up to the window- DO NOT OPEN YOUR WINDOWS,” the soldier shouted at them. Their appointment was verified, and they were directed to drive up to a testing tent. The nurse at the tent shouted through her mask and the sealed window. “Since you’re here and exposed, you’re getting tested too,” she called out to my mother. “Tilt your heads back, open the window and please, please, don’t cough or sneeze on me.” They had their noses swabbed and were cleared to leave. That was when it started to snow. Can’t make this stuff up. Twice, they pulled over for her to kneel in the slush on the side of the highway and vomit.
Then came the long anxious wait for results. With the amount of testing done daily, I wasn’t surprised at all that the timeline they gave us was behind by a day or two. On Thursday, my mother’s temperature creeped just above normal and she started complaining about ear pain. She called her primary doctor’s office, who gave her a mask and saw her in a tent in their parking lot. Once again, rapid strep and flu are negative. They prescribed antibiotics “just in case.” She asked me what I thought. Well, it’s been three days, maybe give it one more day to see how your viral culture comes back? On Friday afternoon, March 27, the DOH called, they both tested positive. Two weeks of quarantine from the date of testing for anyone in the house, and anyone sick must be symptom free for 72 hours, even if that’s longer than 14 days. Now my brother, the last man standing in the house, who had been picking up the groceries, dropping food off on my grandmother’s doorstep, has become Typhoid Mary (I educated my entire extended family on her life story, side bar, a very relevant reference to the asymptomatic carriers of this virus. Although she probably didn’t wash her hands…. I digress).
By that point, I think I would have been more surprised if they tested negative instead of positive. But my anxiety about my mother skyrocketed. I fretted and checked in with her daily. By sometime around the 30th, my sister was strong enough to care for herself, and by the end of that week she was feeling well. My mother’s temperature climbed, she developed a cough, but luckily, surprisingly, she bounced back faster than my young healthy sister, and seems well on her way to recovery as well. I hear my brother built a firepit in the backyard and repainted the dining room ceiling.
As this global health emergency evolves, I’ve developed a mantra: “We don’t know yet.” As my family’s token healthcare provider, with experience as an EMT as well as laboratory, in the scramble to gather information and understand this health crisis, I’ve repeated to them more times than I can count, “we just don’t know yet.” And perhaps for me that’s the biggest emotional challenge. I’m a healthcare provider, I’m a doer, I’m used to jumping in and caring for my family when they’re in need, and in this era, there’s nothing I can do but monitor and advise from a distance. I’m avidly reading studies as they get published, I’ve given my family crash courses in interpreting data and checking sources to try and make sense of the information overload. (For those interested, if you hear about a “miracle solution”, read the information carefully. Was the study published by a credible medical site/journal, or was it “published” to YouTube or the media? What was the sample size- how many people were in the study? Who was excluded and why? If people got better, what’s the likelihood that they would have recovered without intervention?)
A Note from Michael Werner, MD, Medical Director at Maze Health
In this time of fear and uncertainty, it’s important to share information such as this so we can all better understand the severity of this pandemic and its effects on individuals and our communities. At Maze, we are diligently practicing social distancing by remaining open on a very limited basis. We are seeing existing patients with only a practitioner and one patient in the office at a time and our laboratory remains open for emergency sperm cryopreservation (for patients about to undergo chemotherapy etc.). Simultaneously, we are doing our best to serve our patients via telehealth services. If you need assistance, please contact us. We’re here to help.
The post COVID-19: My family’s experience appeared first on Treating Vaginismus, Low Sex Drive, Hormone Imbalances | Sexual Health Experts.
COVID-19: My family’s experience published first on https://medium.com/@PickupSexDolls
0 notes
Text
COVID-19: My family’s experience
On Sunday March 15, my younger sister called me crying. She had temperature of 101OF and a blinding headache, but it was an important day at her job, and she knew her supervisor really needed her help. “Stay home,” I said. “Tell him you’re sick, he’ll understand. Even if there wasn’t an emerging global pandemic, you’re legitimately sick. He’s understanding, this won’t affect your job at all. And call your doctor if the fever sticks around… If it was COVID-19, I would tell you just stay home, but it doesn’t sound like it, maybe you have something bacterial.” The next morning, things were about the same, so she called her doctor’s office and was advised to come in. A nurse wearing a gown, mask, and gloves took throat and nasal swabs. When the doctor came into the exam room, he was dressed similar, and stood at the farthest corner from her. “Well, rapid strep and flu are negative. We don’t test for it, but assume you have COVID-19. Go home and quarantine.”
At that point, believe it or not just three weeks ago, we only believed COVID-19 as a respiratory infection. She called me scared, suddenly afraid she might have a life-threatening illness. “Why would they say, just assume? What does this mean for me?” She lives with my 60-year-old mother, who had been dropping off groceries at her 85-year-old mother since the first reported case. Everyone had been doing their part at social distancing, but was it enough? I reached out to the New York State Department of Health for guidance. “That’s ridiculous,” they told me. “She has no respiratory symptoms, without coughing she can’t spread droplets, and if they considered her a Person Under Investigation, they should have referred her for testing.” Within a week, we would find that every single one of those instructions had become obsolete or been proven incorrect. As the days progressed, she began to vomit excessively, unable to even keep water down. The fever continued. By that point, I began to hear reports from friends and colleagues on the front lines about younger patients presenting with GI or other atypical symptoms, and the daily reports I received from my mother had me more and more concerned. Friday the 20th, I contacted the DOH again. The hold time was 100 minutes. I described her symptoms, and this time they took down her information so they could contact her with a testing site and time, advising that she must come alone so as not to expose anyone else. Saturday evening, my mother called me frantic. After vomiting all day, my sister was too weak to sit up and while she wasn’t disoriented, she was acting euphoric- that’s medical speak for “she knew who she was and where she was but sounded high as a kite”. My concerns about dehydration, lurking in the back of my mind when the vomiting began, started creeping to the forefront. I contacted several urgent cares in her neighborhood, looking for someone who could administer IV fluids and do bloodwork. The answers were all the same: urgent cares aren’t designed for isolation; they aren’t seeing anyone who is suspected COVID-19. Desperate, I reached out to friends who are active EMTs and live closer to her to see if anyone could evaluate her. In full isolation gear, a friend went over to see her. “Look, she’s sick. She’s really sick,” he told me. “Any other time, any other virus, she probably would be hospitalized. But this time, she won’t be. I’ve been in the EDs, they’re overflowing. She’ll wait, and ultimately, she probably won’t get a bed. There’s just too many people sicker than her.”
Nobody slept that night. The next morning, the DOH called to give her an appointment slot the following day at a public park 18 miles away. Going alone wasn’t an option anymore, she could barely sit up let alone drive. So, Monday morning my mother packed her, a blanket, and a bottle of Powerade, into the car and made the trip up to what I now refer to as their “black ops testing experience”. At the entrance to the park, they were stopped by the National Guard, in uniform, with yellow safety vests and surgical masks. “Hold your ID up to the window- DO NOT OPEN YOUR WINDOWS,” the soldier shouted at them. Their appointment was verified, and they were directed to drive up to a testing tent. The nurse at the tent shouted through her mask and the sealed window. “Since you’re here and exposed, you’re getting tested too,” she called out to my mother. “Tilt your heads back, open the window and please, please, don’t cough or sneeze on me.” They had their noses swabbed and were cleared to leave. That was when it started to snow. Can’t make this stuff up. Twice, they pulled over for her to kneel in the slush on the side of the highway and vomit.
Then came the long anxious wait for results. With the amount of testing done daily, I wasn’t surprised at all that the timeline they gave us was behind by a day or two. On Thursday, my mother’s temperature creeped just above normal and she started complaining about ear pain. She called her primary doctor’s office, who gave her a mask and saw her in a tent in their parking lot. Once again, rapid strep and flu are negative. They prescribed antibiotics “just in case.” She asked me what I thought. Well, it’s been three days, maybe give it one more day to see how your viral culture comes back? On Friday afternoon, March 27, the DOH called, they both tested positive. Two weeks of quarantine from the date of testing for anyone in the house, and anyone sick must be symptom free for 72 hours, even if that’s longer than 14 days. Now my brother, the last man standing in the house, who had been picking up the groceries, dropping food off on my grandmother’s doorstep, has become Typhoid Mary (I educated my entire extended family on her life story, side bar, a very relevant reference to the asymptomatic carriers of this virus. Although she probably didn’t wash her hands…. I digress).
By that point, I think I would have been more surprised if they tested negative instead of positive. But my anxiety about my mother skyrocketed. I fretted and checked in with her daily. By sometime around the 30th, my sister was strong enough to care for herself, and by the end of that week she was feeling well. My mother’s temperature climbed, she developed a cough, but luckily, surprisingly, she bounced back faster than my young healthy sister, and seems well on her way to recovery as well. I hear my brother built a firepit in the backyard and repainted the dining room ceiling.
As this global health emergency evolves, I’ve developed a mantra: “We don’t know yet.” As my family’s token healthcare provider, with experience as an EMT as well as laboratory, in the scramble to gather information and understand this health crisis, I’ve repeated to them more times than I can count, “we just don’t know yet.” And perhaps for me that’s the biggest emotional challenge. I’m a healthcare provider, I’m a doer, I’m used to jumping in and caring for my family when they’re in need, and in this era, there’s nothing I can do but monitor and advise from a distance. I’m avidly reading studies as they get published, I’ve given my family crash courses in interpreting data and checking sources to try and make sense of the information overload. (For those interested, if you hear about a “miracle solution”, read the information carefully. Was the study published by a credible medical site/journal, or was it “published” to YouTube or the media? What was the sample size- how many people were in the study? Who was excluded and why? If people got better, what’s the likelihood that they would have recovered without intervention?)
A Note from Michael Werner, MD, Medical Director at Maze Health
In this time of fear and uncertainty, it’s important to share information such as this so we can all better understand the severity of this pandemic and its effects on individuals and our communities. At Maze, we are diligently practicing social distancing by remaining open on a very limited basis. We are seeing existing patients with only a practitioner and one patient in the office at a time and our laboratory remains open for emergency sperm cryopreservation (for patients about to undergo chemotherapy etc.). Simultaneously, we are doing our best to serve our patients via telehealth services. If you need assistance, please contact us. We’re here to help.
The post COVID-19: My family’s experience appeared first on Treating Vaginismus, Low Sex Drive, Hormone Imbalances | Sexual Health Experts.
COVID-19: My family’s experience published first on https://spanishflyhealth.tumblr.com/
0 notes
Text
Round up of my mentions of MCAS reactions

“ Escape to the mountains for breathable air! I know grass makes my throat swell up and my chest get tight, but but I've not known what my other triggers are. Til recently. I downloaded the weather Channel app on my phone and now it alerts me during Ozone Action/Warning Days, and woops, they match up with my swelling, too. So this weekend I saw that the grass pollen was high AND it was an ozone action day, and tho I hate using the car on such days, my house apparently doesn't protect me from bad air (and I sure as heck can't afford an air purifier) so I just needed to escape. Picture 2 is just outside of Boulder, where I live, and my throat was already swelling up before we made it out of the area. But by the time we got into the mountains, it was calming down again.thank goodness! And TG for accessible overlooks, like in Pics 1 & 3! No hiking required to see prettiness. :) “

“ Whoa there, face. You look like you've been outside in the cold for an hour.. But I haven't left my couch all day! It's hard to get with this annoying portrait filter I can't turn off, but you can see the diff between my face and neck. I usually look much more pallid and anemic! ) I always say I have very little skin involvement with#MCAS (and I've only had hives once in my life) but I wonder how much of that is true and how much is just me not putting two and two together before. Like, my face has felt hot all day, I used to call this "fevering", but I've recently realized it's only my face that's hot and red, so it's prolly MCAS flushing, not a fever at all. Which is interesting that before I had an app for it, the only way I knew I was about to start my period is that I'd get one of these "fevers" for an hour or two the night before! I must be reactive to one of my own gd hormones. 😅😅😅 Yup, sounds like an MCAS thing! As I'm on my period now, (tho I don't think I usually am flushed at this poiny/for this long) and my stomach still feels full of good from yesterday, and who knows what else, but maybe I'm just reacting to a bunch of stuff. My face is redder irl, and I startled myself a few minutes ago when I went to the bathroom and saw my face. I've NEVER seen it this red while just sitting around the house! “

“ Oops I ate an often-trigger food without tacking my Cromolyn first. :( I feel like I have a fever and my belly is angeryyyy. Sighhh. “
MCAS & Cromolyn
(Jan 2019)
#MCAS: where normal food can make you shiver violently while your face blazes and your stomach thinks it's been poisoned.
Woops forgot to take my Cromolyn Sodium before eating. ☹️😷😱☠️
Also, this is what it looks like. Supposed to take 2 viles 4x a day, but I have yet to remember all 4 even once. :-x
Edit 1 hour later: my stomach and face have calmed down, but now my heart rate Is in the 130s as I'm laying here, and I feel like if I open my mouth I'll be like a megaphone and the sound of my speeding, thumping heart would loudly reverberate through the house.. It honest to God feels like my heart has grown wings and is violently trying to escape my chest.

“ Ok you can't really tell here, but my face is rosy. I'm wondering if these random few-hour "fevers" I've always gotten are really jus t flushing? Does your face feel warm and tight and similar to when your fevering when you're flushing from #MCAS? Or Allergies? We are house sitting a doggo, but I'm allergic, and I'm feeling it way more than I have before when we've watched him! Waaah. "I need vogmask, but for my eyes!" Me, earlier. “

“ Wait, what?! I react to freshly cut grass exactly the same in all months. Could it really be from different things?! Although maybe I do react differently. I feel wayyy itchier lately and maybe less swollen sinus cavity & throat, but I've only recent started noticing how itchy I get when I'm walking outside, particularly if I'm sweating even minutely, which could mean it's started up recently, or not. Adhd makes it so hard to keep track of symptoms :( :/ Fwiw, I think the same allergy test that told me I was allergic to grass said mold as well... 🤔 This post brought to you by my overwhelming need to scratch all my skin off. (Also my skin doesn't seem to really turn red til I scratch it, then it gets v angry btw). #allergy #GrassAllergy “

“ Ugh, motility issues are more than just delayed!! My psych had me request a emptying study from my GI to check for RAPID emptying (bc my meds don't work if I eat with them and she needs the results for dose adjustments) but this report is clearly looking only for delayed. Now, I sometimes do experience delayed for a few days a month, but I don't mind it much, it's the rapid that screws with my meds and makes it risky to eat at a restaurant without hanging around a half hour afterwards in case I have to run to the bathroom (in those cases my dysautonomia (and pain) also flares while my stomach is emptying, then I seem to get hit with reactive hypoglycemia or whatever it's called. Ugh.) Nausea is only a small symptom a few times a month, max, yet it is THE symptom on this test. Annoying. As I said day-of, my stomach was behaving that day, so I'm not surprised it was normal, but from the penciled in average emptying time I found, it does suggest that even when it's not acting up, it is a bit faster than normal. “

“Post treadmill stress test dinner. Vegan Pad Thai. It's been almost two hours and my muscles are still goop and I'm still extra shakey. My body did not approve. I'm surprised I made it a whole 5 minutes tho, tbh. “

“ Reverse progression of my chest today. I just now took the first picture. I removed the electrodes 6 hours ago, and boy, my body still wants it to be known that, I guess the gel that was over the round electrode itself, And to a lesser extent, the sticky stuff, was v annoying. When I first took the Holter monitor off, it was really only red on the circle bits, and where I'd been scratching (see pic 3). But then once they were off, I scratched a bunch because OMG, and that left me super red itself (pic 2) now where the sticky bits were seem red too. Is this normal, or allergies or mast cell (I've never been tested for it, but I think I should be) or what. 6 hours seems a long time to still be so red! “
Gastro follow up: Endoscopy, MCAS talk!
(Apr 2018)
During the appointment I told her that I had less rapid gastric emptying than I had been before, but more constipation and fullness-- but especially BLOATING.
I don't think I fully realized how frequently I have the sensation of bloating or stomach discomfort, because, I have noticed, when I experience it, I instinctively... eat... MORE. Especially crappy foods that frequently cause the rapid gastric emptying symptoms. That makes sense, but it's interesting to realize since I was doing it pretty unconsciously! But it hasn't been super helpful lately AND I've gained 10lbs in the last month alone! (after having gained 30+lbs in the ~8 months prior!)
And finally, I told her that I had been reading up on Mast Cell Activation Syndrome/Disease lately and it's fairly likely that I have it, and it seems to have a huge effect on the GI system. Surprisingly, her eyes widened a bit and she said that, in fact, she had just been to a conference this weekend, and they talked about Mast Cells as a cause of Functional GI Disorders! So, she said she will read up more on MCAS & EDS/HSD and how they influence the GI system.
0 notes