#hyposignal
Explore tagged Tumblr posts
Text

Best I can do is The Hyposignal
need a bat signal for McCoy enjoyers....
#star trek#star trek tos#star trek aos#leonard mccoy#bones mccoy#bat signal#bones mccoy bat signal#hyposignal#hypospray signal#youandthe mountains
189 notes
·
View notes
Text
Sub-Clavicular Hibernoma: A Rare Diagnosis of Lipomatous Tumor by Zaïd Boughaleb in Journal of Clinical and Medical Images, Case Reports

Abstract
Lipomatous tumors are the most common soft tissue tumors, including a large variety of benign and malignant lesions. Hibernoma is a benign lipomatous tumor originating from the brown adipose tissue inherited from the fetus. The diagnosis is often incidental, since the large majority are asymptomatic or very slow growing. Differential diagnosis with other lipomatous tumors is often challenging. Hence the diagnostic work-up is large and must be multidisciplinary. Biopsy and large resection with sane margins are the standard of care. We describe a 48-year-old male patient with a history of a painless, mobile, slow growing right sub-clavicular mass apparently evolving for eleven years. This patient underwent ultrasound, mammography, MRI, CT Scan and ultrasound guided large core biopsy at different points in time. We describe this case of a well-documented hibernoma of the sub-clavicular region in line with the current literature.
Keywords: CT scan; hibernoma; lipomatous tumor; MRI; ultrasound.
Introduction
Lipomatous tumors including a large variety of benign and malignant lesions are the most common soft tissue tumors, their prevalence increasing with age [1]. Sometimes, overlapping imaging features can be misleading in diagnosis [2]. Since the distinction between benign and malignant lipomatous tumor is challenging, especially when based on clinical and superficial work-up, the differential diagnosis of lipomatous tumors includes hibernoma [3]. Hibernoma is a rare, heterogeneous, slow growing fatty tumor of good prognosis [1], arising from brown fat precursors, representing approximatively 1% of all tumors derived from lipomatous tissues [1]. Usually, no symptoms are associated except when the enlarging mass impinges on local tissues4. To date a few thousand cases worldwide have been described [1].
Case Presentation
A 48-year-old male patient was referred to our mammography unit with a history of a painless, mobile, slow growing right sub-clavicular mass apparently evolving for eleven years. No skin redness, fever or signs of nerve or vascular compression were related. Previous ultrasound examinations reported a fatty mass with a diagnosis of lipoma (well-differentiated fatty tumor without suspicious radiological signs of malignancy [3]). Mammography showed a radiolucent mass consistent with a lipomatous origin on a targeted modified medio-lateral oblique view [5]. Ultrasound revealed a hyperechoic, homogeneous mass compared to the subcutaneous fatty tissue, measuring 11,5 x 3,6 x 10 cm, with vascular hyperemia on color-doppler ultrasound (Figure 1). MRI examination was performed to assess the precise extent and possible invasion of the underlying tissues. MRI described a mass measuring 10 x 3,9 x 9 cm with hypersignal on T2 sequence (but slightly lower than the subcutaneous fat signal [3]), hyposignal on T1 sequence compared to muscle structure (but slightly higher than subcutaneous fat signal [3]), very low signal on a fat suppression sequence and moderate enhancement on the post-contrast T1 sequence. No invasion of the adjacent soft tissues, muscles or bones was described (Figure 2). A CT scan without contrast media injection recently performed for other reasons showed a pre-pectoral low attenuation mass without involvement of the underlying tissues. In our case, density of the lesion was slightly higher than subcutaneous fat [5]. Eventually, diagnostic large core needle biopsies under ultrasound control were performed yielding the histological diagnosis of adipocytes with a microvacuolar and eosinophilic cytoplasm without signs of mitosis or necrosis. The diagnosis of hibernoma was raised. For aesthetic reasons, this patient was referred to our oncologic plastic surgeon; preoperative laboratory testing reported no evidence of metabolic disorder or infectious component [6]. Surgery showed a mass alongside the pectoral fascia, without muscle or vessel invasion. Histology confirmed the diagnosis of hibernoma.
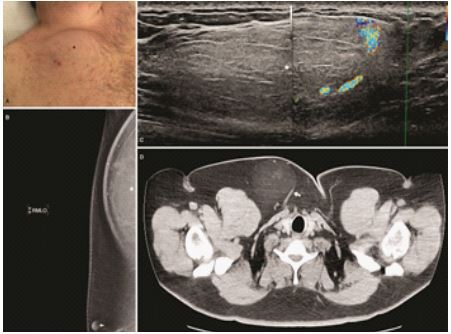
Figure 1: (A) Subclavicular swelling due to the clinical mass (black star). (B) Mediolateral modified oblique mammographic view showing a radiolucent mass (white star), nipple (with arrow). (C) Ultrasound: hyperechoic mass with peripheral vessels on color ultrasound (white star). (D) Axial non-enhanced CT scan showing the mass (white arrow).

Figure 2: (A) T2-weighted axial MRI image revealing a slightly hypointense mass compared to subcutaneous fatty tissue (black star). (B) Axial T1-weighted non-enhanced MRI image with fat suppression: hibernoma undistinguishable from adjacent fatty tissue. (C) Gross macroscopic specimen showing a lipomatous mass. (D) Axial T1-weighted MRI image with fat-suppression post Gadolinium injection demonstrating a slight enhancement of the mass (white arrow).
Discussion
Huge progress has been made since the descriptions by Merkel in 1906 and Gery in 1914 [7, 8]. Brown fat is a particular form of fat found in the hibernating and non-hibernating animals [9]. Representing approximatively 1,6% of all benign lipomatous tumors, hibernomas are very slow growing tumors usually occurring between the age of 20 and 50 years [11, 12]. Average age at diagnosis is 38 years and various gender predominance have been described in the literature. Intraosseous hibernomas are found in older patient [13]. The most common location, as the majority of fat tumors, are neck, shoulder and periscapular regions which are areas with possible remaining brown fat tissue [14]. However, hibernomas can occur anywhere in the body [15]. The clinical manifestations are rare, but might occur as a painless soft tissue mass, with a locoregional irritation or neurovascular compression [16]. Conventional radiography demonstrates a radiolucent mass with no adjacent osseous abnormalities or mineralization [17]. Ultrasound describes a rather uniformly hyperechoic mass [5], with increased vascular flow [17] generally unspecific, like other soft tissue tumors. In our case, the diagnosis of a typical lipoma [5] was ruled out due to vascular hyperemia on color doppler ultrasound. On CT scan, hibernoma presents as a homogenous low-density mass of lipidic composition between the attenuation of subcutaneous fat and skeletal muscle [5]. Contrast enhanced CT scan usually shows variable degree of enhancement [16] and intra-tumoral septas [10]. Diagnosis of hibernoma cannot be excluded based on the lack of intra-tumoral vessels [10]. On MRI, the imaging modality of choice [3], hibernoma shows an hypoT1 and hyperT2 signal because of the fatty component alike our case but differs slightly from the fat signal. On a fat-suppressed sequence, attenuation is similar to fatty tissue. After Gadolinium contrast media injection, enhancement is variable but predominantly present and rather heterogeneous [5]; a common sign are large flow voids indicating fast flowing flood in intratumoral vessels. Internal septation, one of the features of hibernoma [3], was absent in our case. High level of FDG uptake has been described in brown adipose tissue [16], sometimes even higher than liposarcoma [10] but overlapping results [2] prevent clear distinction between both tumors. Four types of hibernomas have been described, based on a histological classification [15]: the typical variant, the most common one like our case, the “myxoid” variant, the “lipoma-like” variant and the “spindle-cell” variant. Differences in imaging characteristics among these different histological subtypes of hibernomas are due to the variable amounts of water and fat content. One study distinguished between “lipoma-like” and “non lipoma-like” hibernoma [18]. Non-lipomatous hibernomas are probably indistinguishable from other liposarcomas [17]. Differential diagnosis of hibernoma is very large and may include benign tumors (lipoma, angiolipoma, hemangioma, hemangiopericytoma, hemangioblastoma, xanthoma, granular cell tumor, adult rhabdomyoma, lipoblastoma…) [16, 19] and malignant tumors (liposarcoma, clear cell sarcoma,…) 5, 10, 16. Clinical and imaging features as previously described may guide the diagnosis, but the histological examination gives the final diagnostic. In the absence of treatment, hibernoma continues to grow and leads to functional or cosmetic consequences 2. Tumor regrowth has been reported with incomplete excision of hibernoma 19. The standard of care of hibernoma is surgical removal with clear margins. Surgical excision is advised to rule out a possible malignant lesion with hibernoma-like differentiation which could be missed by core needle biopsy 1. No risk factor has been described [1]. Multiple lesions in a single patient are possible 21. After resection, the tumor generally does not recur. Since no malignant transformation or metastatic (22) spread have been described in the current literature, hibernoma can be considered as a benign tumor 1 for patients is 20.
In conclusion, the diagnosis of fatty tumors, often challenging especially with rare tumors like hibernomas, should comprise ultrasound, MRI and large core needle biopsies. Since hibernomas are benign tumors with no tendency to recur or metastasize, surgical resection with clear margins is recommended 17.
Declarations
Funding
This work did not benefit from any financial support
Conflict of interest
All authors declare no conflict of interest.
Ethical approval statement
The study has been approved by the Ethical Committee of the institution (76/2021).
Patient consent statement
A written permission to publish has been obtained from the patient.
For more details : https://jcmimagescasereports.org/author-guidelines/
#CT scan#hibernoma#lipomatous tumor#MRI#ultrasound#asymptomatic#sub-clavicular#hyposignal#Subclavicular#mammographic#Zaïd Boughaleb#JCMICR
0 notes
Text
Localization and a Typical Aspect of the Chondromyxoid Fibroma in a Child by Echcikhi M*

Abstract
The chondromyxoid tumor is a primitive benign tumor of cartilaginous differentiation. We report the case of a 10-year-old child presenting with an aggressive form of the tumor that mimics a malignant process, atypical localization at the iliac axis.
Keywords: Fibromy Chondromyxoid; Child; IRM
Introduction
The chondromyxoid tumor is a benign benign tumor, presenting 0.5% of primitive tumors. She is generally interested in the metaphysics of the lungs. The objective of our article is to illustrate an aggressive form of this tumor, atypical localization in a child, highlighting the role of the IRM in its taking charge.
Case Report
Child of 10 years, consulted at the emergency room of the Rabat Children's Hospital for a prolonged and painful tumult of the right iliac fossa, rapidly increasing in volume. The biological balance was normal. The radiography objective showed a mixed lithic and condensing lesion, heterogeneous, of the right iliac artery, inciting the realization of an IRM. The IRM has objectiveed a legal process centered on the right iliac axis (Figure 1), multi-locale, in hyposignal T1, hyerignal heterogeneous T2, reproducing multiple septa stages in hyposignal T2 enhanced by Gadolinium, without restriction in diffusion. It is associated with a compact reaction with respect, without overriding adjacent structures. Absence of infiltration of fat or associated adenopathies. The process was in favor of a more benign origin than a chondrosarcome. The chondromyxoid fibroma was among the evacuated diagnostics, and was histologically confirmed. The surgical excision was indicated. A tumor recurrence was objective by a follow-up IRM after 5 months. It should be noted that tumor recurrence is more voluminous than primitive tumor (Figure 1 d).
(a) After (b) Gadolinium injection, and in sequential T2 in sagittal cup before (c) 5 months after a surgical resection (d) The images show a tumor process centered on the right, multi-locus iliac axis, in hyposignal T1 (a), enhanced by Gadolinium (b). The tumor shows a heterogeneous T2 hyersignal, confirming multiple septa steps in hyposignal T2 (c). It is a compact periodic response with regard to, without overheating of adjunct organs.
Discussion
Chondromyxoid fibrosis generally affects young subjects and manifests itself clinically through pain and tumors. Pathological fractures are common [1]. On standard radiography, at the level of the lungs, one finds an eccentric geographical gap, soufflant the cortical. On the sites where the iliacs are, the tumor is often polycyclic and mixed, associated with a condensation and a bright osseuse. Intra-tumor microcalcifications may be encountered [2]. The IRM is the key exam that can evoke the diagnosis of chondromyxoid fibroma. The myxoid component appears in hyposignal T1, hypersignal T2, and is enhanced by Gadolinium. The IRM also allows the detection of other associated intratumoral components: fibrous, cystic and calcareous [3,4]. Chondromyxoid fibroma is characterized by the absence of intra-medial extension, which allows to differentiate its aggressive form of a chondrosarcoma, the latter being the differential diagnostic principal. In the interest of a meticulous analysis of tumor reports in IRM. Histological confirmation after a biopsy is always indicated [3,4]. The treatment consists of a complete tumor excision with curettage and joint osseux. Note that total resection is not always possible given the frequency of relapses that occur in 25% of cases. The malignant tumor transformation is exceptional [1,2].
Conclusion
The imagery and in particular the IRM play multiple and fundamental roles in taking charge of the chondromyxoid fibroma. The IRM offers a diagnostic orientation, in particular in the case of atypical localization, a precise study of tumor reports guiding surgical treatment, as well as the search for a recurrent postoperative operation.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00151/ https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00151.pdf
0 notes