#hematocrit
Explore tagged Tumblr posts
Text

The Science Manuscripts of S. Sunkavally, p 742.
#stress#consciousness#amoeba#pseudopodia#electrofusion#calcium#increase of size in evolution#memorization#songs#dispassionate women#female beauty#metabolic rate of muscle#free radicals#sweating in exercise#hematocrit
0 notes
Text
Hematocrit micro- centrifuge
Labotronics hematocrit micro-centrifuge is a tabletop unit operating at 12,000 rpm, ideal for determining erythrocyte volume and solution separation. Its precise speed and time control ensures accurate sedimentation, while continuous operation allows rapid processing of samples.

1 note
·
View note
Text
Book PACKED CELL VOLUME (PCV); HEMATOCRIT by Dr. Lal Pathlabs
Book Dr. Lal Pathlabs - PACKED CELL VOLUME (PCV); HEMATOCRIT online for Rs 130 at SecondMedic,with 1+ tests free doctor consultation with every package, Book now.
0 notes
Text
Exploring the Packed Cell Volume (PCV) Test: Procedure, Results, and Clinical Implications
The Packed Cell Volume (PCV) test, also known as hematocrit, is a common diagnostic tool used in medicine to measure the proportion of blood volume occupied by red blood cells (RBCs). This test provides valuable information about a person's overall health and helps in diagnosing various medical conditions. Understanding the PCV test, its significance, and interpretation is essential for both healthcare professionals and patients alike.
What is PCV?
Packed Cell Volume (pcv), and it refers to the volume of red blood cells in a given volume of blood after centrifugation. It is expressed as a percentage of the total blood volume. For example, a PCV of 40% means that 40% of the blood volume consists of red blood cells, while the remaining 60% comprises plasma and other blood components.
Importance of PCV Test:
The PCV test is crucial in assessing the oxygen-carrying capacity of the blood. Red blood cells contain hemoglobin, a protein that binds to oxygen and transports it to various tissues and organs throughout the body. A decrease in PCV indicates anemia, a condition characterized by low levels of hemoglobin or fewer red blood cells. Conversely, an increase in PCV may suggest dehydration or certain medical conditions such as polycythemia vera, a rare blood disorder characterized by the overproduction of red blood cells.
Indications for PCV Test:
Healthcare providers may order a PCV test for various reasons, including:
1. Evaluation of anemia:
A low PCV may indicate different types of anemia, including iron deficiency anemia, vitamin deficiency anemia, or hemolytic anemia.
2. Monitoring of blood disorders:
Patients with blood disorders such as polycythemia vera or thalassemia require regular PCV tests to monitor their condition and response to treatment.
3. Assessment of hydration status:
Dehydration can cause an increase in PCV due to the hemoconcentration of blood.
4. Preoperative assessment:
PCV levels are often checked before surgery to ensure adequate oxygen-carrying capacity and overall health status.
Procedure for PCV Test:
The PCV test is typically performed as part of a complete blood count (CBC). A small sample of blood is drawn from a vein, usually in the arm, using a needle and syringe or through a finger prick. The blood sample is then placed in a special tube and centrifuged at high speed to separate the cellular components from the plasma. The PCV is calculated by measuring the height of the packed red blood cells relative to the total height of the blood column in the tube.
Interpretation of PCV Results:
The interpretation of PCV results depends on various factors, including age, sex, altitude, and underlying health conditions. In general, a PCV within the normal range (usually 40-50% in adults) is considered normal. However, deviations from the normal range may indicate underlying health issues:
1. Low PCV (Anemia):
A PCV below the normal range suggests anemia, which may be caused by factors such as iron deficiency, vitamin deficiencies, blood loss, or underlying medical conditions affecting red blood cell production or lifespan.
2. High PCV (Polycythemia):
An elevated PCV may indicate dehydration, lung disease, smoking, or conditions such as polycythemia vera, where there is an abnormal increase in red blood cell production.
Conclusion:
The PCV test is a valuable tool in the diagnosis and management of various medical conditions, particularly those affecting the blood and oxygen-carrying capacity. Understanding the significance of PCV results and their interpretation is essential for healthcare providers to make accurate diagnoses and formulate appropriate treatment plans. Additionally, patients can benefit from knowing about the PCV test and its implications for their health and well-being. Regular monitoring of PCV levels, along with other relevant tests, can help ensure timely intervention and optimal management of underlying health issues.
0 notes
Text
Understanding Hemogram
A hemogram can tell you a lot about your blood. For instance, red and white blood cells, as well as platelets (also called thrombocytes), will be counted and examined for size, shape, volume, and degree of organization. Specific factors that may affect these parameters include a total number of erythrocyte progenitor stem cells; RBC membrane stiffness; frequency of RBC production; distribution and frequency of phagocytosis (cellular breakdown); distribution and type of leukocytes (white blood cells) in circulation; vitamin deficiencies like folic acid or B12 deficiency. The number of toxic substances such as lead poisoning can also be analyzed from a hemogram.
0 notes
Text
A 12 Day- Old Female Infant Diagnosed with Pelvic Osteomyelitis in the Pediatric Emergency Department by Mehmet Ali Oktay in Journal of Clinical and Medical Images, Case Reports

Abstract
Osteomyelitis (OM) is a bacterial disease that is very rare in newborns and has devastating consequences. Neonatal OM is seen in 1-3 in 1000 babies. We presented a 12-day-old female baby who was brought to the Pediatric Emergency Department (PED). Because she could not move her leg. She did not have fever and septic appearance and had a history of hospitalization in Neonatal Intensive Care Unit; acute phase reactants were high and radiological imaging performed gradually was consistent with OM. Our patient is the youngest patient who was diagnosed with pelvic OM upon admission to the PED. Earlydiagnosis and treatment prevent complications and sequels. Keywords: Osteomyelitis; newborn; pediatric emergency
Introduction
Osteomyelitis often occurs secondary to the hematogenous spread of microorganisms into the blood-rich metaphysis of the developing bone. When left untreated, it leads to complications such as joint destruction and decreased range of motion [1]. Osteomyelitis (OM) of the hip is rare in newborns. Signs and symptoms are quite different compared to older children. This may cause difficulties/delays in diagnosis and permanent disability [2]. Successful management of OM in the neonatal period has been associated with rapid correct diagnosis and adequate correct treatment [2, 3]. The incidence of OM in the pediatric age group is 1/5000 cases. About 50% of pediatric OM cases are under the age of five. The incidence of neonatal OM is 1-3/1000 cases [3]. Although there are studies on patients diagnosed with osteomyelitis while staying in neonatal intensive care unit (NICU) [1, 4, 5], cases diagnosed upon PED (Pediatric Emergency Department) admission are very rare [6]. In this article, the youngest case in literature who went to the PED and was diagnosed with pelvic and acetabulary OM is presented.
Case Report
A 12-day-old girl, born from the first pregnancy of a 28-year-old mother, was admitted to the PED with complaints of restlessness and inability to move her right leg. The day before the application, it was stated by her mother that she did not move her leg, that she was agitated when forced to move, and could not be consoled. The baby did not have a history of fever or trauma, her feeding was good, and her urine and defecation were normal. From her history, it was learned that she was born at 36 weeks and 3 days of gestation and had intrauterine growth retardation compatible with 31 weeks gestational age, and she was born by emergency cesarean section due to preeclampsia. The patient, who was hospitalized in the NICU due to temporary tachypnea of the newborn after birth, was discharged on the sixth postnatal day. During the follow-up in the NICU, umbilical catheterization was not applied to the patient. She had not received antibiotic treatment and no growth was detected in blood cultures taken before discharge.
At her evaluation in the Pediatric Emergency Department triage area, she was a restless baby with a good general appearance. Vital signs; body temperature was 37°C, heart rate was 140/min, respiratory rate was 42/min, pulse oximetry was 98%, and mean arterial pressure was 45 mmHg. There was no pathological finding in the physical examination, and it was observed that the patient's discomfort increased due to the position given to the hip and leg while changing the diaper. While abducting the right thigh from the hip in the supine position, there was limited range of motion compared to the left. No swelling or redness was detected on the joint surface.
Laboratory and radiological examinations were planned for the patient with a preliminary diagnosis of septic arthritis. In laboratory tests: hemoglobin (Hb) 14.6 g/dL, RBC (Erythrocyte) - 3.361 x10.e6/uL, hematocrit (Hct) 40.04%, white blood cell (WBC) 16.82 x10.e3/uL, neutrophil percentage 59.8%, C-reactive protein (CRP) 25.9 mg/L, erythrocyte sedimentation rate (ESR) 51 mm/hr, procalcitonin (PCT) 2.95 ng/mL, IL-6 145.6 pg /mL detected. On direct radiographs of the lower extremity and pelvis, the right femoro-acetabular distance was observed to be increased (Figure 1). Long bone radiographs were normal. In the superficial tissue ultrasound (US) performed for the right hip joint, bilateral hip joints were compared with each other, and no significant effusion was observed on the right side. The patient was consulted to the Orthopedics and Traumatology department with a preliminary diagnosis of septic arthritis. MRI was requested from the patient for the differential diagnosis of septic arthritis.

Figure 1: There is an increase in the right acetofemoral distance compared to the left.
Bilateral hip MR imaging showed “The right femoral head is small and irregular in appearance, and an area of pathological signal change in the right femur proximal metaphysis, medullary bone marrow, and solid periosteal reaction in the lateral proximal section is observed. Widespread edema was observed in the surrounding muscle planes, fascial surface and subcutaneous adipose tissue adjacent to the hip joint. In addition, medullary bone marrow edema was observed in the right acetabulum (osteomyelitis). Areas of pathological signal changes consistent with diffuse edema are observed in the right obturator externus, pectineus, quadriceps muscles, gluteal muscle planes and iliacus muscle (myositis). Minimal free fluid was observed in the right hip joint space. Findings were primarily evaluated as compatible with osteomyelitis and myositis.” (Figure 2).

Figure 2: Osteomyelitis in the proximal metaphysis of the femur
Due to the history of hospitalization in the intensive care unit, the patient was diagnosed with OM secondary to hematogenous spread and, according to the age, to include possible infectious agents, vancomycin (15mg/kg/dosex3), ceftazidime (30 mg/kg/dose x 3), fluconazole loading (12 mg/kg/dose)) and maintenance (6 mg/kg/dose) treatment was started. Blood culture was taken before antibiotic treatment. Our patient, who received antibiotic doses only one day before the operation, was operated on the postnatal 13th day.
The patient was operated by the Orthopedics and Traumatology department and the intra-articular pus was drained. From the material; joint fluid culture, fungal culture, tuberculosis PCR, ARB staining, fungus search was sent. There was no growth in the blood culture, but because of the growth of ceftazidime-resistant Klebsiella pneumoniae in the joint fluid culture, ceftazidime was discontinued and meropenem (20 mg/kg/dosex3) treatment was started. Fluconazole was discontinued on the 8th day because there was no growth in the fungal culture. The patient was discharged with oral trimethoprim-sulfamethoxazole treatment after 25 days of vancomycin and 27 days of meropenem treatment. Trimethoprim-sulfamethoxazole was discontinued 22 days after discharge. The regression of the inflammation was seen in the MRI taken under the control of the outpatient clinic. verbal consent was obtained from the patient's parents for the publication of the article.
Discussion
This case demonstrates the importance of detailed investigation of newborn infants admitted to PED. Although OM in newborns is rare, there are difficulties in diagnosing and treating it. High suspicion is required for early diagnosis and observation of clinical signs is very important.
Risk factors for osteomyelitis in newborns are stated as immature host-defense mechanisms, invasive intervention such as umbilical catheterization. It has been shown that half of the cases diagnosed with neonatal OM have a history of umbilical catheterization. It has been observed that the pregnancy and delivery history of the mother is also important in the development of OM, and maternal complications such as maternal hypertension, preeclampsia, ablatio placentae, infection are present in approximately half of the infants who develop OM [7]. Particular attention should be paid to the evaluation of newborn cases, especially in PEDs where is crowded and the number of patient admissions is high. Newborns are among the patients at risk for PED and require special care. Application complaints and prenatal, natal and postnatal history should be questioned in detail. It was observed that the mother of our case had preeclampsia during pregnancy, but umbilical catheterization was not applied to the baby.
In studies conducted in newborns with neonatal osteomyelitis, the most common sites of involvement were reported as femur, humerus, and tibia, respectively [1, 4, 8]. The pelvis is a rare site of hematogenous disseminated OM for neonates. Pelvic OM constitutes 2.3% of all childhood osteomyelitis cases [3]. Our case also had pelvic (acetabular) OM, which is a rare site of OM involvement. Involvement was also demonstrated in the proximal region of the right femur.
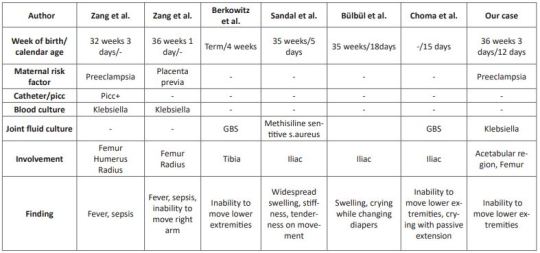
Pelvic OM was defined in three cases at 5, 15, and 18 days in the neonatal period [3, 9, 10]. In the literature, it has been observed that mostly cases hospitalized in the NICU were diagnosed with osteomyelitis [1, 3, 4, 8-10]. As far as we can find in the literature, a 4-week-old case with a diagnosis of distal tibial OM and culture of GBS has been reported, just like our case [6]. Our case is the youngest OM case diagnosed in the emergency department, except for the case in the literature. The clinical features, presentation symptoms, cultures and risk factors of cases diagnosed with neonatal osteomyelitis in the literature are shown in (Table 1)
Table 1: Comparison of cases with neonatal osteomyelitis in the literature.
Clinical symptoms are related to the bone or joint area involved in newborns. Swelling and local inflammation findings are common findings in the neonatal osteomyelitis group. Systemic findings such as fever are seen in fewer of these cases. A highly variable rate of fever was found in 9.1-76.5% of patients with extensive neonatal osteomyelitis. In addition, it has been shown that the WBC count, CRP and ESR levels are high in the cases [1, 4, 8, 11]. In our case, there was no fever, but there were complaints of inability to move her right leg and restlessness. Laboratory parameters were high and consistent with the literature. In cases with osteomyelitis, direct radiographs can guide the correct diagnosis, exclude other diagnostic possibilities, or provide clues for underlying pathological conditions [12]. Soft tissue swelling on plain radiographs can be seen within days of the onset of infection. It can also show periosteal reaction, lytic lesions, joint effusions and destructive bone changes 7-10 days after the onset of infection [13]. US findings begin with nonspecific swelling in the soft tissues adjacent to the bone. US can show thickening and elevation of periosteal and subperiosteal fluid collections as early as 3 days [14]. In a study comparing osteomyelitis groups, it was shown that the diagnostic value of US was statistically higher in the newborn group compared to the other groups, regarding the capacity of detecting subperiosteal abscesses [11]. In our case, however, an increased femoro-acetabular distance was observed on direct X-ray, but no finding was found on US. This supports the view that the primary step in the pediatric emergency department in patients with suspected osteomyelitis should be started with direct X-ray as recommended in the literature.
MR imaging is the most useful imaging technique for evaluating suspected OM, allowing early detection of osteomyelitis and assessment of the extent of involvement and disease activity. MRI is very sensitive in detecting OM 3-5 days after the onset of infection [12]. As seen in our case, it still remains the gold standard. However, we recommend hospitalization in order not to miss the newborn cases because MRI is difficult in emergency conditions.
In infants, osteomyelitis and septic arthritis often coexist. While Staphylococcus aureus is the most common organism causing osteomyelitis at all ages, GBS and Escherichia Coli are important pathogens to be considered in newborns [6]. Culture is found to be negative in 22-50% of the cases [15]. Antibiotics to be used in neonatal OM should be effective against these pathogens [16]. In our case, treatment with antibiotics covering these pathogens was applied and Klebsiella pneumoniae growth was observed in the pus culture.
We think that even with rapid diagnosis and aggressive treatment, there are orthopedic sequelae and inadequate treatment increases the risk of chronic osteoma [16], therefore, in cases who apply to the pediatric emergency department with these complaints, early diagnosis and treatment of neonatal OM should be planned in a timely manner to minimize long-term sequelae.
In conclusion, a detailed anamnesis should be taken and a careful physical examination should be performed in newborns who present to the PED with limited range of motion at joints. Neonatal OM cases mostly consist of cases diagnosed while staying in the NICU. Pelvic involvement is rare and our case is the youngest pelvic OM case diagnosed in the PED.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Osteomyelitis#newborn#pediatric emergency#Pediatric Emergency Department#OM#PED#catheterization#RBC#C-reactive protein#hematocrit#Traumatology#Mehmet Ali Oktay#JCMICR
0 notes
Text
Guess who officially has T levels well within the accepted average range in cis men!!! :3 603 sexy sexy ng/dL of it💪😎
#it was like 200 last time i checked#so where's my beard huh? lol#in other news by other stats seem to be improving which is good#my hematocrit is still a bit high but slightly less high than last time#and everything else is within normal!#yay :3#transition update#ftm
3 notes
·
View notes
Text
headache may be kicking my fucking ass but im determined to donate blood tomorrow if it fucking kills me
#probably will#more likely is that they'll tell me my hematocrit is too low and turn me away#plot twist bitch. im volunteering on friday HAH
7 notes
·
View notes
Text
Hey shoutout to my stint on low-dose T for literally curing my chronic anemia, seemingly indefinitely
#went off of it for complex reasons after a while#have now been off of it for longer than i've been on#and still this is the only time in my life my hematocrit has been in normal range#like aside from the gender stuff#this was worth it#i do think my t baseline is higher now#like a lot of the stuff that should be temporary is just sticking around#and while it can take a while for it to flush#like#what was in my system from injections should have eliminated by now#which leaves only the read that i'm just producing more now#personal#anyway obligatory#if you are going to be weird abt me going on T as a lesbian#kiss my whole ass
1 note
·
View note
Text
https://sparktv.net/read-blog/43040_hematocrit-test-devices-market-analysis-size-share-and-forecast-2031.html
The Hematocrit Test Devices Market in 2023 is US$ 4.7 billion, and is expected to reach US$ 6.34 billion by 2031 at a CAGR of 3.82%.
#Hematocrit Test Devices Market#Hematocrit Test Devices Market Growth#Hematocrit Test Devices Market Size
0 notes
Text
Micro Haematocrit Centrifuge 15.5 kg
Labnics micro haematocrit centrifuge is a digitally controlled device with a 12,000 rpm max speed, 15,800×g RCF, 0-99 min timer, and 24-capillary rotor capacity. It features a compact design with a safety interlock system that prevents lid opening during operation.

0 notes
Text

TSRNOSS, p 715.
#histamine content of spinach#Henrik Ibsen#scorpion#bird species#avian penis#birds#body temperature#prostaglandins#testes#polyunsaturated fatty acids#lipid-water interface#acidity of DNA#awareness of time in infants#dogwood#trees#boiling points of acids#hematocrit#extrusion of the nucleus by the erythrocyte#humming birds#heart size in species
1 note
·
View note
Text
Cell Washing Centrifuge
Labtron Cell washing centrifuge is designed for the efficient washing and separation of cells . The device features speeds of up to 5000 RPM, microprocessor control, an automatic rotor imbalance detection system, and a maximum capacity of 12 tubes of 7 ml each. Features include precise speed control, programmable cycles, high-speed capability, digital interface, robust construction, and safety features.

1 note
·
View note
Text
y’all i think testosterone has cured my iron deficiency
#my hemoglobin is at the top of the range#my hematocrit is high#my rbc count is like at the top#never before seen#p sure my doctor is gonna tell me to stop taking the iron pills#also apparently a symptom of high hemoglobin is easy bruising#and let me fucking tell you#i bruised so fucking bad for this last lab#it’s fucking HUGE#and i didnt even feel her poke me so that’s wack
1 note
·
View note
Text
Blood Card Centrifuge

A blood card centrifuge is a type of centrifuge designed specifically for use with blood cards, which are small, specialized cards used for collecting, transporting, and storing blood samples. These centrifuges are often compact and portable, making them suitable for use in various settings such as clinics, hospitals, or fieldwork.These centrifuges may have features such as adjustable speed and time settings, as well as options for different rotor configurations to accommodate various sample sizes and types of blood cards.
0 notes
Text
Micro Hematocrit Centrifuge

A micro hematocrit centrifuge is a specialized centrifuge designed for the determination of hematocrit levels in blood samples. Hematocrit is the percentage of red blood cells (erythrocytes) in the total volume of blood. This measurement is important in diagnosing various medical conditions such as anemia, polycythemia, dehydration, and other blood-related disorders.
0 notes