#heamodynamics
Explore tagged Tumblr posts
Text
I see what you did there…a (very) brief history of imaging the brain: blood, BOLD and fMRI
A little more #neuro #science #history This time: functional magnetic resonance imaging #fMRI #BOLD #scicomm #writing #blogging #neuroscience #brain
For many patients we can discover – or discount – physical causes of neurological problems ‘in real time’ with a range of imaging and other measurement techniques. Neuroimaging techniques are mainly children of the 20th century, and their development is ongoing in the 21st, but their roots stretch back through the 19th century. For example, photography and its ability to reproduce an enduring…

View On WordPress
#Angelo Mosso#CT#EEG#electrophysiology#epilepsy#fMRI#heamodynamics#Keith Thulborn#MEG#MRI#neuroimaging#neurology#neuroskeptic#neurovascular coupling#PET#Peter Bandettini#Seiji Ogawa#xkcd#Your Brain through...History
1 note
·
View note
Text
The Effectiveness of Esmolol in Attenuating the Arousal Response (Heamodynamic Changes and Bis Index) to Endotracheal Intubation in Patients Undergoing Surgical Procedures-Juniper Publishers
Introduction
Measurement of anaesthetic depth is a challenging task for the anaesthesiologist. Ever since the first modern anaesthetics (ether, chloroform, and nitrous oxide) were used in the 1840, doctors have been searching for a reliable method of measuring the depth of the patient's unconsciousness. Research has indicated that patient's attitude towards undergoing surgery is affected by the possibility of awakening during the procedure. Post-traumatic stress disorder (PTSD) is a common result of awareness episodes. [1,2].
There are several reasons for anesthesiologist’s difficulty in evaluating dosages of anesthetic agents:
The lack of a universally accepted definition of "consciousness".
The complex effects of anesthesia on the human organism.
The increased use of combinations of anesthetic agents rather than single drug.
Changes in the patient's response to anesthesia over the course of the operation.
Age and sex related differences in responsiveness to specific anesthetics.
Large differences among individuals apart from age or sex groupings in regard to sensitivity to anesthesia [3].
A variety of different physiological responses have also been used in attempts to indirectly measure the depth of a patient’s unconsciousness under anaesthesia. Most people use haemodynamic responses- the patient's blood pressure and heart rate as basic guidelines for adjusting the amount of anaesthetic agent delivered to the patient during surgery. Other direct measurements have been based on the movements of the patient's body during surgery, hormonal responses, sweating, eye movement, and the reactivity of the eyes to light [4,5].
In contrast, a technology that would permit independent neurophysiologic monitoring of the central nervous system would provide a direct measure of brain status during anesthesia and sedation, allowing clinicians to finely tune perioperative management and achieve the best possible outcome for each patient. Accurate monitoring and targeting of brain effect, in combination with assessment of clinical signs and traditional monitoring, would permit a more complete approach to adjusting the dosing and mixture of anaesthetic, sedative and analgesic agents.
Indirect methods that allow an observer to assess a person's level of awareness have been used since the early 1970. The earliest and most widely used instrument for evaluating impaired consciousness is the Glasgow Coma One difficultly that has emerged from these attempts at direct measurement is that that they are not good predictors of the likelihood of awareness during surgery or recall of the procedure after surgery.
Another measurement that researchers have explored in their attempts to measure depth of anesthesia directly is the electroencephalogram (EEG). The EEG is a complex recording of the electrical activity of the nerve cells in the brain. In 1931 Berger discovered that brain waves change in amplitude and frequency when a person is asleep or anaesthetized; they slow down, shift to lower frequencies, and become more closely synchronized with another.
Bispectral index
It is a numeric index that directly reflects the activity of cerebral cortex and correlate with level of consciousness. It is the latest system used in anesthesiology to measure the effects of specific anaesthetic drug on the brain and to track changes in patient's level of sedation and hypnosis. In technical terms, the Bispectral index itself is a complex mathematical algorithm that allows a computer inside an anesthesia monitor to analyze data from a patient’s electroencephalogram during surgery. BIS was first developed in early 1990 and has been used since 1997, It is a type of automated direct measurement of the patient's condition in comparison to the Glasgow coma scale or similar scoring systems, which are indirect assessment of sedation [6].
The Bispectral Index (BIS) is a measure of the effects of anesthesia and sedation on the brain, a new "vital sign" that allows clinicians to deliver anesthesia with more precision and to assess and respond more appropriately to a patient’s changing condition during surgery. It is a numeric index that directly reflects the activity of cerebral cortex and correlates with the level of consciousness.
BIS monitoring supports three key elements of anaesthesia are:
Vigilance
Diagnostic decision-making
Therapeutic targeting
Therapeutic targeting is a clear benefit that results from BIS monitoring. Using this new parameter, the clinician can manage patients within the optimal plane of anesthesia effect, reducing the unwanted occurrence of excessive or inadequate anesthetic effect. Clinical investigations of BIS monitoring during anesthesia have consistently demonstrated an average 25% reduction in intra operative anesthetic use and a consistent reduction in the time for emergence from general anesthesia.
The key EEG features identified from the database analysis characterized the full spectrum of anaesthetic induced changes and included:-
Degree of beta or high frequency (14-30 Hz) activation,
Amount of low frequency synchronization,
Presence of nearly suppressed periods within the EEG
The BIS is an empiric, statistically derived measurement. The key hypothesis underlying the development of BIS was that some combination of EEG features (e.g. bispectral, power spectral or other) could be identified and shown to be highly correlated with sedation and hypnosis, regardless of the agent used to produce that clinical state. The BIS was derived by analyzing a large database of EEGs from subjects who had received one or more of the most commonly used hypnotic agents [7,8].
The normal neural EEG activity of higher frequency (alpha and beta rhythms) is converted to slower frequencies (delta and theta rhythms) during deep anaesthesia, due to direct suppression of cortical activity or by depression of pacemaker regulation. It further increases the amplitude of EEG (synchronization) leading to 'burst suppression'. On the other hand arousal characteristically decreases amplitude (desynchronization).
BIS calculates three sub parameters.
1) Burst suppression with two separate algorithms
a. Burst Suppression Ratio (BSR)
b. QUAZI
2) Beta Ratio
3) Synch fast slow
The BSR is the proportion of the suppressed EEG (isoelectric) in an epoch, the Beta ratio is the log ratio of the power in the two empirically divided frequency bands (high and medium frequency ranges) and Synch fast slow is the relative Bispectral power in the 40-70 Hz frequency band. The Bispectral analysis examines the relationship between the sinusoids at the two primary frequencies, f1 and f2, and a modulation component of the frequency f1+f2. The set of these three frequency component is known as triplet.
After processing, a database is created describing the EEG- derived sub parameters and the corresponding clinical state (level of consciousness).
Each parameter has a particular stage of anesthesia where it performs more accurately. The Beta ratio parameter reflects light sedation; Synch fast slow detects surgical levels of anaesthesia, and the burst suppression ratio (BSR) and QUAZI predominate during deep levels of anaesthesia. Multi-variate, statistical models were used to derive the optimum combination of the features, which then was transformed into a linear dimensions scale from 0 to 100 [9].
Prospective clinical trials have demonstrated that maintaining BIS Index values in the range of 40-60 ensures adequate hypnotic effect during general aesthesia while improving the recovery process. During sedation care, BIS Index values >70 may be observed during adequate levels of sedation but may have a greater probability of consciousness and potential for recall.
The BIS Index provides a direct measurement of brain status, not the concentration of a particular drug. For example, BIS Index values decrease during natural sleep as well as during administration of an anaesthetic agent. The decrease produced during the natural process of sleep, however, is not to the degree caused by high doses of propofol, thiopental or volatile anaesthetics. The BIS Index values reflect the reduced cerebral metabolic rate produced by most hypnotics. Using positron emission tomography, a significant correlation between BIS Index values and reduction in whole brain metabolic activity was measured [10].
BIS Index monitoring can allow delivery of anesthesia care that is safer, more precise and more pleasant for the patient. In combination with assessment of clinical signs and traditional monitoring, the BIS monitoring can facilitate balanced hypnotic and analgesic administration with ensuring adequacy of anaesthesia. Various measures to be taken during a sudden increase or decrease of BIS values are as below:-
Responding to sudden BIS increase:
Examine for the presence of artefacts (EMG, electrocautery or high frequency signals).
Ensure that anaesthetic delivery systems are operating properly so that the intended dose of anaesthetic agent is reaching the patient.
Ensure that the anaesthetic dose is sufficient.
Assess the current level of surgical stimulation.
Responding to sudden BIS decrease:
Assess for new pharmacologic changes.
Assess the current level of surgical stimulation.
Consider decrease as possible response to administration of muscle relaxants.
Assess for other potential physiologic changes.
Assess for emergence from anaesthesia [11].
BIS monitoring during endotracheal intubation
During endotracheal intubation, one general goal of the anaesthesia provider is to minimize cardiovascular stimulation, thus preventing resultant hypertension and tachycardia. Several strategies are commonly used to blunt the blood pressure and heart rate response including:
Sufficient dosing of intravenous induction agent (e.g., propofol, thiopental)
Opioid supplementation (e.g., fentanyl) [12]
Administration of intravenous or tracheal lidocaine [13]
Administration of antihypertensive (e.g., esmolol)
Alternative intubation methods (e.g., fiberoptic intubation)
Several studies have examined the BIS responses during endotracheal intubation to better understand the relationship between cortical CNS and cardiovascular responses. Quite often, a transient increase in BIS value (ΔBIS) can be observed following tracheal intubation or other stimulation. Studies have demonstrated that BIS responses do not directly correlate with the change in blood pressure following laryngoscopy and intubation.
Laryngoscopy as well as tracheal intubation is one of the most stressful times in the period of anesthesia for the patient. It is associated with significant changes in the hemodynamics i.e. increase in heart rate and blood pressure as well as an arousal response as quantified by BIS.
Various agents have been used to attenuate these reflexes and reduce hemodynamic changes these include opoids, ɑ2-agonists like clonidine, local anesthetics like lidocaine, adrenergic blocking agents like esmolol and vasodilating agents like sodium nitroprusside and nitroglycerine [14,15].
Several studies have examined the BIS responses during endotracheal intubation to better understand the relationship between cortical CNS and cardiovascular responses. Quite often, a transient increase in BIS value (Δ BIS) can be observed following tracheal intubation or other stimulation. Studies have demonstrated that BIS responses do not directly correlate with the change in blood pressure following laryngoscopy and intubation.
Patients with controlled hypertension have demonstrated an exaggerated blood pressure response, while their BIS response was no different than normotensive individuals. BIS responses to stimulation associated with laryngoscopy and intubation can be markedly attenuated in a dose-dependent fashion.
Esmolol, a short-acting (β1-adrenoceptor antagonist, produces dose-dependent attenuation of the adrenergic response to laryngoscope and orotracheal intubation. However, previous studies assessing the effectiveness of esmolol in blunting the hemodynamic alterations induced by laryngoscope and orotracheal intubation failed to monitor electrical activity of the brain. Only a few studies have evaluated the effect of interaction between β1-adrenoceptor antagonists and anesthetics on BIS. They raised the possibility that esmolol administration may mask inadequate anesthesia.
Our purpose was therefore to determine whether preventing hemodynamic responses with esmolol simultaneously ameliorates arousal reactions as quantified by BIS monitoring during laryngoscope and endotracheal intubation.
Materials and Methods
Materials Required
BIS System Components: The BIS system is comprised of five components
BIS sensor-Capture raw EEG
Patient interface cable (PIC)-Transmit raw EEG signal
Digital signal converter (DSC)-Processes raw EEG and filter artefacts
BIS engine-Analyzes EEG signal and calculate BIS index value
Display monitor-Displays BIS index value and displays additional parameters including SQI, EMG, SR, EEG
BIS Sensor: The BIS sensor is a sophisticated electrode system specifically designed to work with BIS systems. A family of sensors tailored to different clinical applications or different patient sizes are available. After minimal skin preparation, the single-use sensor is placed on the forehead of the patient with a specific orientation over either the left or right hemisphere. Due to advanced electrode technology, it results in low impedance values, allowing reliable capture of raw EEG data and increasing the fidelity of the EEG signal. BIS systems routinely test sensor impedance to ensure acceptable sensor performance during clinical monitoring.
Patient Interface Cable (PIC): The raw EEG is transmitted from the sensor through the patient interface cable to the digital signal converter.
Digital Signal Converter (DSC): The digital signal converter receives, amplifies and digitizes the raw EEG signal for subsequent processing and analysis. In addition, key filters and signal processing steps occur in the DSC to identify and reject certain types of electrical artefact (e.g., electrocautery filters in DSC-XP systems). The digitized EEG data travels through the DSC cable to the BIS engine.
BIS Engine: The BIS engine is heart of the BIS system, contains the microprocessor, which is responsible for rapid signal processing and computation of the BIS Index. Some of the steps involved in the analysis of the EEG include multiple methods of artefact detection and processing. Segments of the EEG that are compromised by the presence of artefact are not included in the calculation of the BIS Index. The BIS Index is made by combining selected EEG features, using the BIS algorithm. All BIS values are updated every second but reflect a smoothing function set at either 15 or 30 seconds to minimize excessive fluctuations.
Display Monitor: All BIS systems are linked to display monitors - either stand-alone BIS monitors or integrated multiparameter monitors. These monitors have an ability to display BIS value, BIS trends and important additional data including:
Signal quality index (SQI)
Electromyogram/High-frequency activity (EMG)
Suppression ratio (SR)
EEG waveforms
Signal quality index (SQI) and electromyogram/high- frequency activity (EMG) may be displayed in graphic or digital mode. Suppression ratio (SR) is also available. The display monitor also coordinates a variety of communication alerts and alarms (Figure 1).
Boyle's Anesthesia Workstation.
Multi-para monitor having pulse oxymeter, NIBP, ECG and BIS
IV infusion set, blood transfusion set
IV Cannula: 18G; 20G, IV extension line
IV Fluids: crystalloids; colloids including normal saline
Disposable syringes: 5ml; 10ml; 50ml
Infusion pump
Suction machine, stethoscope, laryngoscope, ET tubes of different sizes, stop clock.
BIS-QUATRO sensor
Drugs required
Anesthesia drugs
Propofol
Glycopyrolate
Esmolol
Atracurium
Diclofenac sodium
Ondensetron
Neostigmine
Methodology
The study was conducted in the Department of Anesthesiology, S.M.S Medical College and attached group of hospitals, Jaipur with due permission from the institutional ethical committee and review board and after taking written informed consent from the patient
Study design
Prospective Randomized Double blind Hospital based Interventionl study.
Sample size
Total 50 patients were selected and divided into 2 groups of 25 each via chit and box randomization technique.
Inclusion criteria/Exclusion criteria
Every patient was screened a day before surgery after applying inclusion and exclusion criteria
Inclusion criteria
o Patients with ASA grade 1 and 2
o Patients of age group 18 to 55 years of either sex undergoing elective surgery under general anesthesia
o Patients willing to give written and informed consent
Exclusion criteria
Patients refusal
Major organ dysfunction
Patients on medications like hypnotics, narcotic analgesics, α2 agonists, calcium channel blockers, β blockers
Patients with anticipated difficult intubation
Patients incubated after more than 1 attempt or more than 20 seconds
Patients with impaired LFT/RFT
Patients with ASA grade 3,4,5
Deaf and dumb patients
Patients with respiratory, cardiac or neurological disease
Patients having known allergy to anesthetic agents used in study
Psychiatric patients
Groups
The patients were divided into two groups of 25 each according to drugs used
Randomization was done by chit and box method.
Pre-anesthetic check up
All patients were examined on the day before surgery and explained about the anesthetic technique and peri-operative course. Informed consent taken, each patient had a pre anesthetic checkup which includes-
Any significant present/past medical surgical history
History of any previous surgery with significant anesthetic complication
Physical examination
Vital parameters like BP/Pulse/Respiratory rate
Routine investigations like Hb, TLC, DLC, LFT, RFT, ECG,X-ray chest (PA view), FBS/RBS, Platelet count.
Technique
On arrival in the operation theatre, weight, fasting status, consent and PAC was checked. Before anaesthetic induction, electrodes for BIS (BISTM monitor 2000, Aspect Medical System, USA) were placed on the forehead and the baseline BIS value was recorded. The electrodes used were disposable BIS-QUATRO Sensor strips (Aspect Medical System, USA). Baseline parameters [SpO2, Pulse rate (PR), Systolic blood pressure (SBP), Diastolic blood pressure (DBP), baseline BIS were recorded.
a) 2 IV lines with 18/20 G cannula were secured.
b) Ringer lactate drip started through one IV cannula
c) Premedication with Inj. Glycopyrolate (0.005 mg/kg) given 6 minutes before start of Induction of Anesthesia.
d) Inj Diclofenac 1.5 mg/kg infusion started after dilution in 100 ml saline.
e) Test drug Bolus: (Esmolol 1mg/kg or Normal saline) was administered IV slowly over 1 minute in double blind fashion just after premedication.
f) PR, SBP, DBP, SpO2, BIS were recorded after the test drug bolus.
g) Test Drug Infusion: (250μg/kg/min esmolol/normal saline) commenced in a double blind fashion after the test drug bolus.
Esmolol infusion prepared by taking 500mg of esmolol in 50ml syringe. The infusion rate adjusted as per the formula.
Rate (ml/min) = 0.25*body weight (kg)
The placebo group received normal saline infusion over the same time period. The rate of infusion again calculated by the same formula. The infusion rate was adjusted in infusion pump as per the weight of the patient before starting the infusion.
The infusion continued for 14 minutes including the time period for pharmacokinetic stabilization of drug levels in the plasma (5min), the time taken for induction (3min) and intubation (1min) and for 5 minutes after intubation.
PR, SBP, DBP, Spo2, BIS were recorded at 1st, 3rd and 5th minute after start of infusion. All the monitoring and recording were made by yet another anesthesiologist who was blinded to the groups. The patients were preoxygenated for 5min during this period.
Induction
Induction was done 5 minutes after start of test drug infusion and with the ongoing infusion, using inj. propofol 2mg/kg injected slowly over IV over 1 minute, and propofol infusion was started at the rate of 6 mg/kg/hr after induction. After induction, pulse rate, blood pressure, SpO2 and BIS was recorded. followed by inj. Atracurium 0.5mg/kg . Hemodynamic parameters and BIS were recorded after end of Propofol administration (6min from start of infusion). Patient were ventilated with face mask with 100% oxygen for 2 minutes. Hemodynamic measurements and BIS were recorded just before intubation (8 min from start of infusion).
Intubation
Intubation was done with endotracheal tube of appropriate size after direct laryngoscopy. Tube position was confirmed by ETCO2 and auscultation. Hemodynamic measurements and BIS were recorded just after intubation (9 min from start of infusion) and 1, 3 and 5 min after intubation (10, 12, 14 min from start of infusion). The test drug infusion was then stopped 5 min after intubation (14 min from start of infusion).
Maintenance
Anesthesia was maintained with inj. Propofol infused at the rate of 6mg/kg/hr and ventilation was done with 40% O2+ 60% N2O by using Ventilator in Volume control mode with Vt at 8ml/kg and rate adjusted to keep ETCO2 between 32-36. Muscle relaxation was maintained with subsequent doses of atracurium (0.1mg/kg).
Intra operative monitoring
Intra operative monitoring continued and hemodynamic measurements were recorded at 20min, 25min, 30min (from start of infusion) and after every 10min thereafter. Inj. Ondensetron (0.1mg/kg) was given intra operatively. Propofol infusion was stopped just after the laproscope ports were taken out.
Reversal
Reversal was done with inj. Neostigmine (0.05mg/kg) and inj. Glycopyrolate (0.01mg/kg). Hemodynamic measurements and BIS were recorded after giving inj. Neostigmine and inj. Glycopyrolate (Reversal was done after onset of spontaneous respiration).
Extubation
Extubation was done and hemodynamic parameters and BIS were recorded immediately after extubation and 5min after extubation. Any complication such as laryngospasm, bronchospasm or desaturation was recorded and managed according to the standard protocols. Any intra operative complication was recorded and managed accordingly. Patients were shifted to recovery room and any immediate post operative complication e.g. nausea, vomiting, shivering, respiratory depression, sedation, restlessness, hypotention, bradycardia etc. were recorded and managed.
Statistical analysis
Statistical analysis done after applying standard qualitative and quantitative tests (eg student-t-test and chi-square-test).
Review of Literature
Gibbs FA et al. [2] illustrates that the electro-encephalograph records the essential activity of the cortex of the brain, and the pattern of wave form is a constitutional characteristic of the individual. Therefore, abnormalities of rhythm may be of more fundamental significance than clinical manifestations. The three main manifestations of epilepsy (grand mal, petit mal and psychomotor epilepsy) are each accompanied by a distinct pattern of dysrhythmia. The electro-encephalogram record obtained in patients having psychomotor seizures is similar to that seen in most patients diagnosed as having schizophrenia. These records, furthermore, are closely similar to those obtained in the majority of children with psychopathic personalities. On the basis of statistical, therapeutic and electrical evidence, they believe that any relationship between epilepsy and schizophrenia is positive rather than negative.
Sigl JC et al. [4]: The goal of their study was to provide a simplified interpretation of the electroencephalogram (EEG) for a variety of applications, including the diagnosis of neurological disorders and the intra operative monitoring of anaesthetic efficacy and cerebral ischemia. Power spectral analysis, for example, quantifies only power distribution as a function of frequency, ignoring phase information. It also makes the assumption that the signal arises from a linear process, thereby ignoring potential interaction between components of the signal that are manifested as phase coupling, a common phenomenon in signals generated from nonlinear sources such as the central nervous system. Bispectral analysis is a method of signal processing that quantifies the degree of phase coupling between the components of a signal.
Zaugg M, et al. [16] found that peri operative betablockade improve long-term cardiac outcome in non-cardiac surgical patients. A possible mechanism for the reduced risk of peri operative myocardial infarction is the attenuation of the excitotoxic effects of catecholamine surges by beta-blockade. It was hypothesized that beta-blocker-induced alteration of the stress response was responsible for the reported improvements in cardiovascular outcome.
Mayer J, et al. [17] showed the impact of Bispectral index (BlS)-guided general anesthesia on recovery from general anesthesia in different patient population. They designed this study to examine the value of BIS-guided anesthesia in a fasttrack setting where the goal is rapid recovery. Forty-four patients undergoing open colon resection were randomly assigned to receive either BIS-guided (BIS group, n=22) or clinically guided (standard care group, n=22) total IV anesthesia with propofol after placing a thoracic epidural catheter. Duration of post anesthesia care unit stay, time to tracheal extubation, direct drug cost, the incidence of hemodynamic abnormalities, ability of ambulation on the day of surgery, and patient satisfaction with anesthetic management were assessed. They found that in the BIS-guided group, tracheal extubation was achieved significantly earlier (7.6 vs. 15.4min, P<0.01) and the post anesthesia care unit stay was significantly shorter (51 vs. 85min, P<0.01). Total anesthetic drug cost was reduced by 23% and the incidence of hypotension requiring treatment was significantly lower in the BIS group. Early ambulation, patient satisfaction, and incidence of adverse events were not significantly different between the groups. They concluded that BIS-guided IV anesthesia in combination with thoracic epidural analgesia facilitates rapid recovery and reduces the overall cost of care in patients undergoing fast-track colon surgery.
Choi, Seung Ho [18] studied that Activation of the peripheral nerve system by endotracheal intubation is accompanied by an increase in bispectral index (BIS). Esmolol produces a dose-dependent attenuation of the adrenergic response to endotracheal intubation. In this double blind, randomized study, after the induction of anesthesia, patients were mask-ventilated with either sevoflurane or desflurane (end-tidal 1 minimum alveolar concentration) and received normal saline or esmolol (0.5mg/kg) 1 minute before intubation (sevoflurane-control, sevoflurane-esmolol, desflurane-control, and desflurane- esmolol groups, n=20/group). BIS, mean arterial pressure, and heart rate were measured before the induction of anesthesia (awake), before esmolol injection (time point 1), immediately before intubation (time point 0), and every minute for 5 minutes after tracheal intubation (time point 1 to 5). Compared with preintubation, esmolol attenuated the increase in BIS at 1 minute after intubation during sevoflurane anesthesia (5.1% for esmolol and 31.7% for control) but not during desflurane anesthesia (28.6% for esmolol and 30.8% for control). Mean arterial pressure and heart rate increased after intubation in all groups but the changes were greater in the control groups than the esmolol groups. In conclusion, a single dose of esmolol blunted the increase in BIS to tracheal intubation during sevoflurane but not desflurane anesthesia.
Zhong TD, et al. [19] observed esmolol infusion as an adjunct to propofol can affect BIS index, reduce anesthetic dose and decrease emergence time Sixty ASA I-II patients, age 18-35, undergoing uterine dilatation and curettage surgery were randomized into two groups. Before induction, patients in esmolol group (Group E) were received 1 mg/kg esmolol intravenously and followed by esmolol 150 microg x kg(-1) x min(-1) intravenous infusion; patients in group C received normal saline instead of esmolol. Fentanyl (1μg/kg) and propofol (2mg/kg) were used as induction drugs. The change of BIS index, heart rate and MAP during operation; total amount of propofol; time when patients opened eyes and time when patients reached the standard for discharge from hospital were recorded. They observed that BIS and heart rate of Group C at 1,2,3 minute after surgery started, increased significantly compared with the time after induction and those in Group E (P<0.05). The time patients reached the score of discharging from hospital in Group C is longer than that in Group E (P<0.05).
Esmolol combined with propofol administering in minor ambulatory operations can control the increase of BIS index caused by surgical nociceptive stimulus. Meanwhile the combination could reduce the dose of sedatives and decrease anesthesia emergence time.
Observations
Table 1 shows the comparison of the two groups with regard to mean ± S.D. of Pulse Rate in both the groups at various time intervals.
Student's T- test (unpaired) was applied for evaluation of changes in heart rate at different time intervals in each group. Values at different time intervals were compared with baseline value. There is no significant difference between the base line value of the heart rate between the group A group B .In group A after test drug bolus heart rate decreased from base line value 90.4±12.1 to 82.3±8.6 compared with group B in which heart rate increased from base line value 85.2±12.6 to 87.8±13.8. In group A, change compared to baseline value, at 1, 3 and 5 minute after intubation, were +3.0, +5.1and 2.3 respectively, which was maximum change from base line after intubation. At the same time in group B these changes were +27.8+27.5 and 22.9 respectively. On intergroup comparision of changes in heart rate from base line at 1,3,5 minute after intubation statistically highly significant difference was found (p value <0.000). At 14, 20, 25, 30, 40, 50min (from start of infusion) changes in heart rate from base line was compared between group A and B a statistically significant difference (p value<0.05) was found. At reversal and just after extubation changes in heart rate from baseline in both group A and B was compared and it was statistically not significant (p value >0.05) (Table 2) (Figure 2).
This table depicts the comparison of the two groups with regard to mean ± S.D. of SBP (Systolic Blood Pressure) in both the groups at various time intervals (Figure 3 & 4) (Table 3 & 4).
This Table shows the comparison of the two groups with regard to mean change in mean blood pressure ± S.D. from baseline value in both the groups at various time intervals. Student- t- test (unpaired) was applied for evaluation of changes in mean blood pressure at different time intervals in each group. There is no significant difference between the base line values of the mean blood pressure between group A group B (p value 698). Values at different time intervals were compared with baseline value. After test drug bolus mean arterial pressure decreases from base line in group A while in group B it remained same.The change in Mean arterial pressure from base line at 1 ,3, 5 6,and 8 min of infusion were compared and on intergroup comparison statistically highly significant difference were found between group A and B (p value<0.05).In group A change compared to baseline value, at 1 ,3 and 5 minute after intubation, were -4.8,-1.8 and +1.8 respectively. At the same time in group B these changes were +12.0,+7.4, +2.3 respectively. Changes in mean arterial pressure at 1,3and 5 minute of intubation were compared and statistically significant difference was found in between group A and B (p value <.05) (Figure 5 & 6) (Table 5).
Discussion
BIS index offers a direct and accurate method for continuous brain status monitoring and provides a measurement of hypnotic effect of anaesthetic agents. BIS monitoring is not a substitute for clinical judgment. However, using BIS information as a part of assessment we can make more informed decision about the dosing and balance of anaesthetic agents.
Laryngoscopy as well as tracheal intubation is one of the most stressful times in the period of anesthesia for the patient. It is associated with significant changes in the hemodynamics i.e. increase in heart rate and blood pressure as well as an arousal response as quantified by BIS.
Various agents have been used to attenuate these reflexes and reduce hemodynamic changes these include opoids, a2 agonists like clonidine, local anesthetics like lidocaine, adrenergic blocking agents like esmolol and vasodilating agents like sodium nitroprusside and nitroglycerine.
The hemodynamic responses to laryngoscopy and tracheal intubation from reflex sympathetic discharge result from epipharyngeal stimulation. It is logical to select an agent which would prevent or minimize the laryngopharyngeal stimulation by the intubation process or an agent which would block the sympathetic activity associated with it.
Several studies have examined the BIS response during laryngoscopy and endotracheal intubation to better understand the relationship between cortical central nervous system and cardiovascular response. With this background we conducted a prospective randomized double blind study. Our purpose was to determine whether preventing haemodynamic response with esmolol simultaneously ameliorates arousal reaction as quantified by BIS monitoring during laryngosopy and intubation.
Esmolol, a short-acting β1-adrenoceptor antagonist, produces dose-dependent attenuation of the adrenergic response to laryngoscopy and orotracheal intubation [20]. However, previous studies assessing the effectiveness of esmolol in blunting the haemodynamic alterations induced by laryngoscopy and orotracheal intubation failed to monitor electrical activity of the brain. Only a few studies have evaluated the effect of interaction between β1-adrenoceptor antagonists and anaesthetics on BIS. There was no dropout recorded throughout the study. No adverse effects were observed during or after the administration of study drugs.
Selection of patients
This study was carried out on 50 patients aged between 18-55 yrs, of either sex belonging to ASA physical status I or II, posted for a variety of surgical procedures. All the patients were randomly divided into two groups of 25 patients each as below:-
Group A - Received Esmolol 1mg/kg bolus (10ml in volume) then 250μg/kg/min infusion for next 14 minute.
Group B - Received equal amount of saline (10ml in volume). Random sampling made the distribution of the patients in two groups.
To study effectiveness of esmolol in attenuation of arousal response as quantified by Bispectral Index. These groups were compared regarding the changes in and hemodynamic parameter to endotracheal intubation. Any significant side effect of drug used.
Monitoring
Heart rate: The mean value of baseline heart rate was almost similar in two groups (90.4±12.1 in group A and 85.2±12.6 in group B). Just after Test drug bolus the mean heart rate decreased in group A but in contrast it showed an increase in group B. This fall in pulse rate can be attributed to ßl- adrenoceptor blockade effect of esmolol. After start of test drug infusion in group A mean heart rate decreased as compared to baseline value. While in group B heart rate showed an increase. At 1, 3 and 5 minute after intubation heart rate increased in both group A and B but increase was significantly greater in saline group (+27.8,+27.5,+19.9 respectively).While in group A 1, 3minute after intubation a rise +5.1, +2.3 was observed. At 5 minute of intubation mean heart rate stabilized and return below baseline value (86.7±9.0) in group A compared to group B(104.2+7.3 and remained stabilized throughout the surgery. It means that in group A esmolol is more effective for attenuation of tachycardia. And throughout the procedure pulse rate in group A remained below the base line value. It is evident in our study that in esmolol group mean heart rate showed a less rise after intubation and it stabilized early (3 minute after intubation) and remained stable throughout the surgery because of attenuation of adrenergic response to laryngoscoy and intubation by direct cardiac effect of esmolol as noted by Menigaux C et al. [21]. In contrast to group B mean heart rate remained above base line value throughout the study.
Our results are comparable to Menigaux C et al. [21] who noticed similar trends in pulse rate after intubation. Our study also validates the findings of JIANG Yong,_et al. [22] who reported that a single dose of esmolol 1mg/Kg better attenuate heart rate than 0.5 mg/kg given before intubation.
There is a dose-dependent risk of hypotension and bradycardia before laryngoscopy when esmolol is combined with anesthesia induction agents [20]. However, the dose regimen used in our study did not result in any adverse haemodynamic effects. Previous studies of Figueredo [20] and Miller DR, et al. [23] demonstrated decrease in heart rate before laryngosopy .This could be because of use of opioids. We did not use opioids (Table 6)
Systolic Blood pressure: The mean value of baseline systolic blood pressure was almost similar in both groups (125.6±11.3 in group A and 126.8±9.7 in group B). Just after administration of study drug bolus systolic blood pressure decreased in A group while in group B it remained almost same. But the changes were statistically significant between group A and B (p value 0.01). In Esmolol group at 1, 3 and 5 minute of intubation although mean systolic blood pressure increased as compared to preintubation value but it was still lower than baseline value(115.1±7.3, 118.3±8.3, 122.2±7.8 respectively). While in saline group at 1 and 3 minute after intubation mean increase in systolic blood pressure was +10.5 and +6.3 respectively. Which was statistically greater (p value<0.005). At 5 minute of intubation systolic blood pressure stabilized and became almost same as base line value. The rise in systolic blood pressure after intubation was compared between the groups statistically highly significant difference was found (P value<0.005). In our study was effective in controlling pressure response to laryngoscopy as it is evident from above observations .and inubation. Esmolol attenuates hypertensive to intubation as it is evident from above observation.
These results are consistent with the findings of Menigaux C, et al. [21] who observed a significant fall in systolic blood pressure at the same time in their study. The hypotensive effect of esmolol results from a gradual decrease in rennin release [24].
Similar trends were observed by JIANG Yong, et al. [22] who reported that a single dose of esmolol 1mg/Kg better attenuate systolic blood pressure than 0.5 mg/kg given before intubation. Shin H Y, et al. [25] observed that there were significant differences in the mean arterial pressure between control group and other groups (Table 7).
Diastolic blood pressure
As systolic blood pressure, there was no significant difference in baseline value of mean diastolic blood pressure in both groups (79.8±7.6 in group A and 80.9±9.2 in group B). Just after administration of study drug bolus diastolic blood pressure decreased in A group while in group B it increased from base line value. But the change was statistically highly significant between group A and B (p value 0.001). In group A at 1 minute of intubation mean diastolic blood pressure (78.7±6.1) increased as compared to preintubation value but it was still lower than baseline value. While in group B at 1 minute after intubation mean increase in diastolic blood pressure was +12.8. In group A at 3 and 5 minute of intubation mean diastolic blood pressure increased as compared to preintubation value (81.4±8.0 and 84.7±8.4 respectively). While in group B at 3 and 5 minute after intubation mean increase in diastolic blood pressure was +9.4 and +16.4 respectively was observed. Just After intubation diastolic blood pressure increased in both the groups but maximum increase was found in group B than group A. Which was statistically significant (p value 0.000). From the above observation it is evident that esmolol effectively attenuates hypertensive response to laryngoscopy and intubation.
Similar trends were observed by Menigaux C, et al. [21] signifying the advantage of using esmolol in anesthetic regimen.
The observations are consistent with the findings of by Jiang Yong, et al. [22] who reported that a single dose of esmolol 1mg/ Kg better attenuate diastolic blood pressure than 0.5 mg/kg given before intubation. Shin, et al. [25] also noted a significant fall in mean diastolic blood pressure compared to baseline values at all the measurement times (Table 8).
Mean blood pressure
Baseline value of mean blood pressure was similar in both the groups (95.4±8.0 in group A and 96.2±7.2 in group B). Just after administration of study drug bolus mean blood pressure decreased in A group while in group B it remained almost same. But the changes was statistically significant between group A and B (p value 0.001). Then mean blood pressure was recorded till at 1,3,5,6 and 8 minutes of infusion. In esmolol group it remained below base line value while in group B mean blood pressure decreased after induction of anesthesia with propofol (6 minute of infusion). The changes was statistically significant between group A and B. At 1, 3 and 5 minute of intubation mean blood pressure increased in B group from base line value(.+12.0,+7.4.and +2.3 respectively) While in Esmolol group at 1 and 3 minute of intubation mean blood pressure decreased from base line value(-4.8 and-1.8 respectively). The rise in mean blood pressure at 1 and 3 after intubation was compared between the groups statistically highly significant difference was found (P value <0.000). These results were similar to the results of Menigaux C, et al. [21].
The observations are consistent with the findings of by JIANG Yong, et al. [22] who reported that a single dose of esmolol 1mg/ Kg better attenuate hypertensive response to intubation than 0.5 mg/kg. Another study conducted by PF White , et al. [26] use of esmolol alone in combination with nicardipine decreases mean arterial pressure in response to intubation (Table 9).
BIS value
Baseline value of Bispectral index value was almost similar in both groups (94.6±2 in group A and 93.8±2.7 in group B). After induction with propofol (2mg/kg) we started the propofol infusion at dose of 6mg/kg/hr. After 5 minute of induction and start of infusion, BIS value decreased up to range of 25-50 in our study.
The mean BIS value just before intubation was 27.4±7.1 and 28.4±6.4 in group A and group B respectively. The difference between group A and B was statistically not significant. Addition of esmolol to general anesthesia with propofol did not affect BIS value before laryngoscopy. This observation suggests that esmolol does not modify BIS during general anesthesia when substantial sympathetic activation is unlikely. Just after intubation, there was increase in BIS value in both esmolol & saline group but increase in BIS value was greater in group B to (52.6±5.8) than group A (35.3±7.1) On inter group comparison it was statistically highly significant (P value 0.0001). At 1, 3 and 5 min after intubation BIS value increased as compared to preintubation value in both groups. This rise was significantly more in group B. These results indicate that esmolol does not have anaesthetic effect per se and it mainly acts via beta adrenergic blockade, thus it is effective only during period of sympathetic activation as occours during laryngoscopy and intubation. Our results are consistent with a study which reports that esmolol does not alter the propofol blood concentration preventing response to command. The noxious stimulation of layngosopy and inubation increases central catecholamine concentration and esmolol prevents this response by blocking β1 adrenoceptor within the reticular formation.
Our results and previous studies indicate that β1- adrenoceptor antagonist not only block cardiovascular stress response after noxious stimulation(laryngoscopy & intubation) but also increase the anti-nociceptive component of anesthesia as reported by Menigaux C, et al. [22]. In a study conducted by Johanson JW, et al. [27] BIS value significantly suppressed in esmolol group compared to placebo group using similar doses of esmolol . We found that at end of 9 minute of intubation there was statistically significant difference in value of BIS between both the groups.
The observations are consistent with the findings of by Oda Y manner, et al. [28] using esmolol and landiolol. BIS was significantly greater in the placebo group compared to esmolol and landiolol group. However, they use sevoflurane for induction and maintenance instead of using propofol. Autoradiographic studies in the rat hippocampus have reported both β1 and β2 adrenergic receptor expression in the rat hippocampus. Esmolol is a moderate lipophilic drug with ( receptor activity and could be involved in the modulation of central adrenergic activity, although some data seem to dispute whether it crosses the blood-brain barrier [29].
Davidson et al. [30] reported that β adrenergic blocking drug possess analgesic-like properties and was able to attenuate the bispectral index responses to noxious stimuli. However, our results are consistent with two other studies, each of which demonstrated that esmolol can be used as analternative to opioids for maintaining haemodynamic and BIS stability during general anaesthesia. Dose of esmolol was selected in accordance with previous reports in which concomitant use of esmolol with propofol showed a significant reduction of the required dose for anesthesia and a favorable inhibition of the BIS response to tracheal intubation [22,28]. The exact mechanism of this response requires further study.
Esmolol has been shown to control intraoperative nociceptive responses during desfurane anesthesiain a similar way to a compatirative group that received desfurane and an opioid in the anaesthetic regimen obseved by Coloma, et al. [31]. In another study, patients β-blocked with atenolol required less fentanyl and isofurane than unblocked control patients to produce similar BIS values.
Another explanation may be an alteration of the pharmacokinetics of propofol by esmolol. Our finding that BIS values before laryngoscopy were similar in the two groups does not support this theory. Esmolol by attenuating the haemodynamic responses to laryngoscopy and orotracheal intubation may have prevented the increase in cardiac output that would normally lead to redistribution of blood flow with a resultant fall in the effect site concentration of propofol and an increase in BIS [28].
It can be concluded bolus dose of Esmolol then continuous infusion of esmolol provides better control of Bispectral Index responses after orotracheal intubation than a single bolus dose of esmolol [29]. However no side effect like bradycardia, hypotension and bronchospasm observed with esmolol in our study (Table 10).
Summary
After approval of hospital's ethical committee and written informed consent from the patients and attendants, the present study was undertaken in 50 ASA status I and II, of either sex between the age group 18-55 years, scheduled for various surgeries in the department of Anaesthesiology at S.M.S. Medical College & Attached Group of hospital, Jaipur. All patients were thoroughly examined pre-anesthetically based on the history, physical examination, chest x-ray and other laboratory investigations.
All the patients were randomly divided into two groups of 25 patients each as follows:-
Group A- Received Esmolol 1mg/kg (10 ml in volume) then 250μg/kg /min infusion for next 14 minute.
Group B - Received equal amount of saline (10ml in volume).
Random sampling made the distribution of the patients in all groups. Baseline pulse rate, blood pressure, SpO2 and BIS was recorded. After loss of consciousness, positive pressure ventilation using bag-valve-mask apparatus and 100% oxygen was performed. Study drug was administered as previously mentioned. Laryngoscopy and tracheal intubation was performed after induction and administration of study drug. The pulse rate, blood pressure, SpO2 and BIS was recorded at various time interval.
There were no significant difference found in demographic data in both the groups as patients were between 36.6 to 39.96 years of age and 55.3 to 58.8kg of Weight of both sexes.
Baseline pulse rate was almost similar in both groups. But after intubation, a significant increase was found in group B that was greater than group A and it was statistically significant . Pulse rate remained near baseline in esmolol group than Saline group after intubation at different time intervals.
Baseline systolic, diastolic and mean blood pressure were almost similar in both groups. Significant increase was found in group B that was significantly greater than group A. The increase in blood pressure at different intervals after intubation was found lower in Esmolol group than Saline group but it was statistically significant. It suggests that Esmolol has more protective effect than Saline against haemodynamic responses to orotracheal intubation.
Propofol provides BIS value in range of 40-60, after induction and on continuous intravenous infusion at 6mg/ kg/hr.After intubation, there was significant increase found in BIS value in group B than group A and 6 min after stoppage of esmolol infusion there was a statistically significant difference in BIS value in group A and B. It proves that bolus dose of Esmolol then continuous infusion of esmolol provides better control of Bispectral Index responses after orotracheal intubation than a single bolus dose of esmolol.
Propofol intravenous infusion provides better control of Bispectral Index responses after orotracheal intubation.
No significant difference in SpO2 was found in all groups.
Conclusion
From the above study and other mentioned previous studies, it can be concluded that Esmolol provides more protective effect against bispectral index and haemodynamic responses after orotracheal intubation.
Previous studies mentioned that when Esmolol was given in a single bolus dose followed by continuous intravenous infusion, it provides better control on Bispectral index responses after orotracheal intubation but a single bolus dose alone was not found so much effective.
Esmolol effectively blunts the hemodynamic response as well as arousal reaction as quantified by BIS to endotracheal intubation in patients undergoing surgical procedures under general anesthesia and can be safely used at induction of general anesthesia.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Journal of Anesthesia & Intensive Care Medicine please click on: https://juniperpublishers.com/jaicm/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
#Juniper publishers Publons#Juniper Publishers Review#Online Publishers#Juniper Publishers#Open access Journals
0 notes
Text
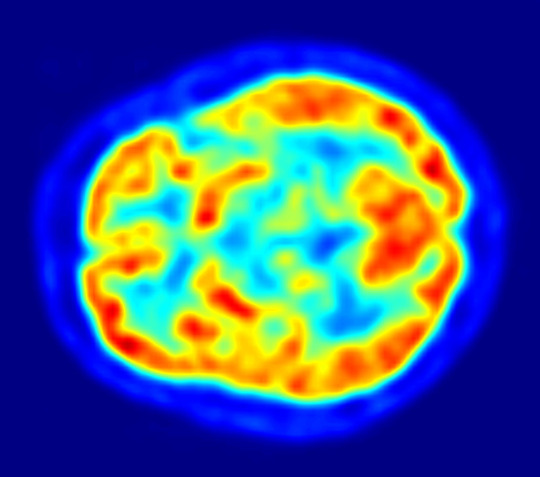
I see what you did there…a (very) brief history of imaging the brain: PET and SPECT
A little more #neuro #science #history on the development of #brain #imaging This time: Positron Emission Tomography (#PET) and SPECT #scicomm #writing #blogging
For many patients we can discover – or discount – physical causes of neurological problems ‘in real time’ with a range of imaging and other measurement techniques. Neuroimaging techniques are mainly children of the 20th century, and their development is ongoing in the 21st, but their roots stretch back through 19th century. For example, photography and its ability to reproduce an enduring…
View On WordPress
#18F-FDG#Alzheimer&039;s Disease#Computed Tomography#epilepsy#heamodynamics#metabolism#neuroimaging#neurology#neuroskeptic#PET#SPECT#Your Brain through...History
0 notes