#health insurance claim rejected
Explore tagged Tumblr posts
Text
Accidental Insurance Claim Got Rejected 😢
Ever thought your accidental insurance would cover everything in case of an accident?
Think again!
In this video, we're sharing a case study of how an individual's health insurance claim was rejected, even though they had the coverage.
You'll learn: ● The common reasons why accidental insurance claims are rejected ● How alcohol consumption can void your accidental insurance coverage ● The importance of staying informed about your insurance policy's terms and conditions
Don't let an unexpected accident turn into a financial burden. Stay safe and stay informed!
Watch now to learn more!
#claim denied#accidental claim denied#term insurance claim denied#health insurance claim denied#health insurance claim rejected#claim rejected#accidental claim rejected#health insurance claim rejection#claim rejection#accidental claim rejection#self-inflicted injury#nidhiverma22#algatesinsurance
0 notes
Text
when i was a homeless 20-year-old i was rejected from multiple housing opportunities because i had 5k in medical debt from going to the ER after getting roofied and sexually assaulted (i was unconscious so calling 911 was not my decision) and UHC denied my insurance claim. so yeah, i'm actually deriving an enormous amount of pleasure from watching health insurance CEOs snivel and hide like the heartless cowards they are. may those who profit from our suffering live in fear of those they seek to deny.
54K notes
·
View notes
Text
Navigating Health Insurance Waiting Periods: A Guide to Claim Success - Insurance Samadhan
Learn how to prevent health insurance claim rejections due to waiting periods. Watch our video for expert advice and secure your claims! Also Visit our website - https://www.insurancesamadhan.com/
0 notes
Text
Is your cashless health insurance claim denied? Know some of the factors that can lead to claim rejection-related issues.
0 notes
Text
That's Right: It's Another Hot Take About That Dead Healthcare CEO
The websites are abuzz with debate on the utilitarian calculus of whether some guy getting shot was a good thing. What are the odds that the assassination will scare the horrible greedy health insurance companies into changing their ways and fixing the system? Is it worth killing someone over? Will the fear of being blasted by some guy with stylishly-engraved bullets put the fat cats in line? Or will their greed win out over their fear, leaving the nightmarish system unchanged?
Well, what if that was totally irrelevant?
You may have seen a graph that looks like this:
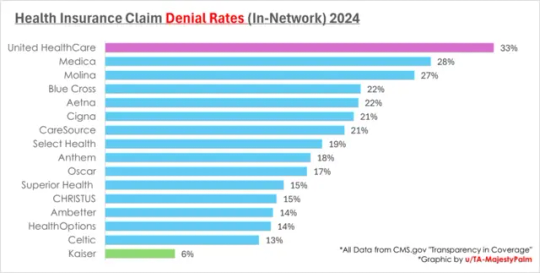
I've seen a few of these going around. These are the rates at which various health insurance companies say "no, you don't get the money" when someone says "hey I need money for this medical thing". UHC, the one whose CEO got shot, is notably really bad in this respect. They've got algorithmic claims denials and all kinds of nasty things that people don't like. All that money they're saving on paying out on claims must be making them rich, right? Let's look at their own financial reports:

Whoa! Big numbers! Six percent looks like a small number, but multiply and they make like thirty billion dollars doing this! That's a lot, right?
Well hang on. They're an insurance company. We can roughly model their profit as the amount people pay them for insurance, minus the amount they have to pay out for claims. Let's look at 2023: simple subtraction, their expenses are $339.2 billion. We simplify other overhead and assume that's all claims. So... that represents those 67% of claims they don't reject. What happens if they approve all the claims?
Multiply: $506.3 billion. They don't have that kind of money. They have $371.6 billion in revenue. So okay- they have to deny some claims. That's pretty normal. But let's pretend they're extremely afraid of assassins now and want to be completely non-greedy: they're okay making zero profit. They make $32.4 billion in profit- how many otherwise-rejected claims can they now afford to approve?
...uh. Well, they can afford to pay out, at most, 73.4% of claims. Still a denial rate of 26.6%, higher than most of their competitors. Not a huge improvement. And in reality, they can't afford to make 0 profit- a company that's making 0 profit is a company investors pull out of immediately, leaving it to collapse, because they can make more money investing in the ones that aren't as afraid of assassins. They've got to at least hover around the same profit margin as their competitors. Which is...

That's average profit margins for the whole US healthcare industry. So, okay, if we match those other companies' profit margins and try to hover around 3-4%... uh. Wait. Hang on. Here's another graph with more recent data on UHC specifically:

Wait, they're still just making that little 3-4% profit margin, even with all these shady automated denials- so how are those other companies doing better on claims? They're obviously not less greedy. They must be making more money somehow, right?
(My guess, sight-unseen, would be that they charge more for their plans, or offer less comprehensive coverage, or use a network of less expensive providers, or other things that make the amount they have to pay out smaller and the amount they're taking in larger. I don't feel like doing a comprehensive consumer review of what every insurance provider's healthcare plans are, but there's always these tradeoffs to make. UHC seems to be offering the tradeoff of "better or cheaper care, on paper" for "but there's a higher risk of getting denied", which is one annoying tradeoff among many.)
Okay But That's Enough Graphs
"Yeah yeah yeah shut up about profit margins and coverage tradeoffs. Is it a good thing that the CEO got shot or not?"
Well, their profit margin at the time he was shot was 3.63%. A company can't survive making 0 or less, so whatever effect fear of assassination has on UHC's greediness, it is going to be no larger than 3.63%.
They may learn the lesson that having their denial rates too high will get them assassinated. Accordingly, they may decrease that metric- by charging higher premiums, kicking expensive doctors out of their network, or reducing their stated coverage. They will not (because they cannot, without ceasing to exist as a company) simply start approving more claims without squeezing their customers elsewhere. They legally cannot do that. No matter how afraid you make the CEOs, you cannot make them afraid to a degree larger than their profit margin.
Well What The Fuck, Then
Like, what, are we supposed to accept that things will literally never get better and that this horrorshow is the best we can hope for? That's some bullshit! If we can't scare the CEOs, who can we scare?
Man I dunno.
Like, for some reason healthcare is stupid expensive! People can't afford to pay for healthcare without insurance- it's like thousands of dollars for basic procedures! Why? Maybe...
Doctors inflate their prices 10x because they know insurance companies will use complicated legal tricks to only pay 10% of the asking price, and this is a constantly escalating price war that serves mainly to fuck over the uninsured
Drug manufacturers and health technology companies fight tooth and nail to maintain monopolies over treatment, so they can charge gazillions to make back the gazillions they had to spend on FDA approval trials
(Trials those same companies lobby to keep necessary because the more money you have to pay for FDA approval, the harder it is for competitors to enter the market since they don't already have the gazillions)
Doctors operate as a cartel and lobby to gatekeep access to medical training so that they can keep doctoring a prestigious and exclusive position, and keep their own salaries high enough to pay their medical school debt and make them rich afterwards- leading to a (profitable) shortage of medical professionals
There is no limit to how expensive things can get but how much people are physically capable of paying, because frequently the alternative to "pay a ridiculous amount for healthcare" is "die", and so healthcare is subject to near-infinitely inelastic demand
Also like a thousand other equally annoying and complicated perverse incentives and stupid situations
This is the human condition: Shit is annoying and complicated and difficult to fix, pretty much 100% of the time forever. A few bullets in some fucko's back isn't really going to make a dent.
(But like, sure, fuck that guy. He probably sucked, as do the hundred other identical suits in line to replace him. Just... don't expect this to help.)
569 notes
·
View notes
Text
My heart goes out to everyone affected by the tragedy of having a health insurance company compromise your life by rejecting your claims.
I am devastated for everyone denied the healthcare they need and deserve because an avaricious middleman industry inserted itself between you and your medical team.
I am significantly less moved by someone experiencing a predictable consequence to leading a life of cruelty and greed.
283 notes
·
View notes
Text
"Cigna tracks every minute that its staff doctors spend deciding whether to pay for health care. Dr. Debby Day said her bosses cared more about being fast than being right: “Deny, deny, deny. That’s how you hit your numbers,” Day said.
...
As ProPublica and The Capitol Forum reported last year, Cigna built a computer program that allowed its medical directors to deny certain claims in bulk. The insurer’s doctors spent an average of just 1.2 seconds on each of those cases.
...
Some of the more astonishing problems that Day spotted have stayed with her. In a case involving a newborn who needed an epilepsy evaluation, Day noticed that a Cigna nurse had listed the mother’s name as the patient, rather than the baby’s. Day fixed that mistake, avoiding what certainly would have been a denial. In another case, a nurse recommended denying payment for an ultrasound of the neck because the treatment wasn’t medically necessary. But the nurse had gotten the body part wrong. It was a hip that was injured, and the imaging was needed. An appeal that landed on Day’s desk involved Cigna’s decision to reject payment for a test because it wasn’t medically necessary for a patient with a sexually transmitted disease. But Day figured out that the patient had toenail fungus, not an STD.
Day said her bosses didn’t want to hear that she was catching errors. By October 2020, Cigna had placed Day on a performance improvement plan that required her to raise her “productivity level” — referring to the score on the dashboard — to at least 70%, which would be a significant jump for her but was slightly below the median for medical directors. The company made the consequences crystal clear: If she failed to successfully complete the plan, she could be terminated."
https://www.propublica.org/article/cigna-medical-director-doctor-patient-preapproval-denials-insurance
601 notes
·
View notes
Text
We are now, what, two three years into the Adderall shortage, and I have been informed by my pharmacy that their next order will arrive during a weekday in November.
Yes, that is how specific the information is.
The amount they will get in November will almost certainly not fill all extant prescriptions, so it will be distributed to whoever calls in and asks for the prescription to be filled on that day.
There is no automated method for informing customers whether the pharmacy has received a shipment, you must call and speak to a pharmacy representative.
This is a very small version of what I assume it must have been like to live in the Soviet Union: Every single decision maker insisting that they are actually operating at 110% efficiency and there are no further improvements that could be made, while meanwhile shortages drag on for literal years and everything grinds to a halt in a bureaucratic mire.
Like, the fact that the way to fix this is to literally call the pharmacy every day and talk to a person means that all of the pharmacists are wasting a tremendous amount of time for, and I cannot stress this enough, literally no reason whatsoever except sheer laziness and apathy on the part of Albertsons management.
In other news, you may remember that after calling four different "Health Homes" that my insurance accepts as PCPs, I got an appointment for 9:40 AM on Christmas Eve. Luckily, they have a telehealth program called "Bridges" which allows you to speak to an RN to get basic health care while you are waiting out the effects of the national Physician shortage that all of our politicians are pretending doesn't exist for some reason.
As best as I can tell, my insurance rejected the claim from the bridges team because they want me to use my Health Home. The one I don't have because they don't have any openings. The one that the bridges team is supposed to cover for until you get establishing care.
I wonder if the people who do health insurance claims ever wonder how many suicides they've caused when they go to bed at night.
66 notes
·
View notes
Text
The real AI fight
Tonight (November 27), I'm appearing at the Toronto Metro Reference Library with Facebook whistleblower Frances Haugen.
On November 29, I'm at NYC's Strand Books with my novel The Lost Cause, a solarpunk tale of hope and danger that Rebecca Solnit called "completely delightful."

Last week's spectacular OpenAI soap-opera hijacked the attention of millions of normal, productive people and nonsensually crammed them full of the fine details of the debate between "Effective Altruism" (doomers) and "Effective Accelerationism" (AKA e/acc), a genuinely absurd debate that was allegedly at the center of the drama.
Very broadly speaking: the Effective Altruists are doomers, who believe that Large Language Models (AKA "spicy autocomplete") will someday become so advanced that it could wake up and annihilate or enslave the human race. To prevent this, we need to employ "AI Safety" – measures that will turn superintelligence into a servant or a partner, nor an adversary.
Contrast this with the Effective Accelerationists, who also believe that LLMs will someday become superintelligences with the potential to annihilate or enslave humanity – but they nevertheless advocate for faster AI development, with fewer "safety" measures, in order to produce an "upward spiral" in the "techno-capital machine."
Once-and-future OpenAI CEO Altman is said to be an accelerationists who was forced out of the company by the Altruists, who were subsequently bested, ousted, and replaced by Larry fucking Summers. This, we're told, is the ideological battle over AI: should cautiously progress our LLMs into superintelligences with safety in mind, or go full speed ahead and trust to market forces to tame and harness the superintelligences to come?
This "AI debate" is pretty stupid, proceeding as it does from the foregone conclusion that adding compute power and data to the next-word-predictor program will eventually create a conscious being, which will then inevitably become a superbeing. This is a proposition akin to the idea that if we keep breeding faster and faster horses, we'll get a locomotive:
https://locusmag.com/2020/07/cory-doctorow-full-employment/
As Molly White writes, this isn't much of a debate. The "two sides" of this debate are as similar as Tweedledee and Tweedledum. Yes, they're arrayed against each other in battle, so furious with each other that they're tearing their hair out. But for people who don't take any of this mystical nonsense about spontaneous consciousness arising from applied statistics seriously, these two sides are nearly indistinguishable, sharing as they do this extremely weird belief. The fact that they've split into warring factions on its particulars is less important than their unified belief in the certain coming of the paperclip-maximizing apocalypse:
https://newsletter.mollywhite.net/p/effective-obfuscation
White points out that there's another, much more distinct side in this AI debate – as different and distant from Dee and Dum as a Beamish Boy and a Jabberwork. This is the side of AI Ethics – the side that worries about "today’s issues of ghost labor, algorithmic bias, and erosion of the rights of artists and others." As White says, shifting the debate to existential risk from a future, hypothetical superintelligence "is incredibly convenient for the powerful individuals and companies who stand to profit from AI."
After all, both sides plan to make money selling AI tools to corporations, whose track record in deploying algorithmic "decision support" systems and other AI-based automation is pretty poor – like the claims-evaluation engine that Cigna uses to deny insurance claims:
https://www.propublica.org/article/cigna-pxdx-medical-health-insurance-rejection-claims
On a graph that plots the various positions on AI, the two groups of weirdos who disagree about how to create the inevitable superintelligence are effectively standing on the same spot, and the people who worry about the actual way that AI harms actual people right now are about a million miles away from that spot.
There's that old programmer joke, "There are 10 kinds of people, those who understand binary and those who don't." But of course, that joke could just as well be, "There are 10 kinds of people, those who understand ternary, those who understand binary, and those who don't understand either":
https://pluralistic.net/2021/12/11/the-ten-types-of-people/
What's more, the joke could be, "there are 10 kinds of people, those who understand hexadecenary, those who understand pentadecenary, those who understand tetradecenary [und so weiter] those who understand ternary, those who understand binary, and those who don't." That is to say, a "polarized" debate often has people who hold positions so far from the ones everyone is talking about that those belligerents' concerns are basically indistinguishable from one another.
The act of identifying these distant positions is a radical opening up of possibilities. Take the indigenous philosopher chief Red Jacket's response to the Christian missionaries who sought permission to proselytize to Red Jacket's people:
https://historymatters.gmu.edu/d/5790/
Red Jacket's whole rebuttal is a superb dunk, but it gets especially interesting where he points to the sectarian differences among Christians as evidence against the missionary's claim to having a single true faith, and in favor of the idea that his own people's traditional faith could be co-equal among Christian doctrines.
The split that White identifies isn't a split about whether AI tools can be useful. Plenty of us AI skeptics are happy to stipulate that there are good uses for AI. For example, I'm 100% in favor of the Human Rights Data Analysis Group using an LLM to classify and extract information from the Innocence Project New Orleans' wrongful conviction case files:
https://hrdag.org/tech-notes/large-language-models-IPNO.html
Automating "extracting officer information from documents – specifically, the officer's name and the role the officer played in the wrongful conviction" was a key step to freeing innocent people from prison, and an LLM allowed HRDAG – a tiny, cash-strapped, excellent nonprofit – to make a giant leap forward in a vital project. I'm a donor to HRDAG and you should donate to them too:
https://hrdag.networkforgood.com/
Good data-analysis is key to addressing many of our thorniest, most pressing problems. As Ben Goldacre recounts in his inaugural Oxford lecture, it is both possible and desirable to build ethical, privacy-preserving systems for analyzing the most sensitive personal data (NHS patient records) that yield scores of solid, ground-breaking medical and scientific insights:
https://www.youtube.com/watch?v=_-eaV8SWdjQ
The difference between this kind of work – HRDAG's exoneration work and Goldacre's medical research – and the approach that OpenAI and its competitors take boils down to how they treat humans. The former treats all humans as worthy of respect and consideration. The latter treats humans as instruments – for profit in the short term, and for creating a hypothetical superintelligence in the (very) long term.
As Terry Pratchett's Granny Weatherwax reminds us, this is the root of all sin: "sin is when you treat people like things":
https://brer-powerofbabel.blogspot.com/2009/02/granny-weatherwax-on-sin-favorite.html
So much of the criticism of AI misses this distinction – instead, this criticism starts by accepting the self-serving marketing claim of the "AI safety" crowd – that their software is on the verge of becoming self-aware, and is thus valuable, a good investment, and a good product to purchase. This is Lee Vinsel's "Criti-Hype": "taking press releases from startups and covering them with hellscapes":
https://sts-news.medium.com/youre-doing-it-wrong-notes-on-criticism-and-technology-hype-18b08b4307e5
Criti-hype and AI were made for each other. Emily M Bender is a tireless cataloger of criti-hypeists, like the newspaper reporters who breathlessly repeat " completely unsubstantiated claims (marketing)…sourced to Altman":
https://dair-community.social/@emilymbender/111464030855880383
Bender, like White, is at pains to point out that the real debate isn't doomers vs accelerationists. That's just "billionaires throwing money at the hope of bringing about the speculative fiction stories they grew up reading – and philosophers and others feeling important by dressing these same silly ideas up in fancy words":
https://dair-community.social/@emilymbender/111464024432217299
All of this is just a distraction from real and important scientific questions about how (and whether) to make automation tools that steer clear of Granny Weatherwax's sin of "treating people like things." Bender – a computational linguist – isn't a reactionary who hates automation for its own sake. On Mystery AI Hype Theater 3000 – the excellent podcast she co-hosts with Alex Hanna – there is a machine-generated transcript:
https://www.buzzsprout.com/2126417
There is a serious, meaty debate to be had about the costs and possibilities of different forms of automation. But the superintelligence true-believers and their criti-hyping critics keep dragging us away from these important questions and into fanciful and pointless discussions of whether and how to appease the godlike computers we will create when we disassemble the solar system and turn it into computronium.
The question of machine intelligence isn't intrinsically unserious. As a materialist, I believe that whatever makes me "me" is the result of the physics and chemistry of processes inside and around my body. My disbelief in the existence of a soul means that I'm prepared to think that it might be possible for something made by humans to replicate something like whatever process makes me "me."
Ironically, the AI doomers and accelerationists claim that they, too, are materialists – and that's why they're so consumed with the idea of machine superintelligence. But it's precisely because I'm a materialist that I understand these hypotheticals about self-aware software are less important and less urgent than the material lives of people today.
It's because I'm a materialist that my primary concerns about AI are things like the climate impact of AI data-centers and the human impact of biased, opaque, incompetent and unfit algorithmic systems – not science fiction-inspired, self-induced panics over the human race being enslaved by our robot overlords.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2023/11/27/10-types-of-people/#taking-up-a-lot-of-space

Image: Cryteria (modified) https://commons.wikimedia.org/wiki/File:HAL9000.svg
CC BY 3.0 https://creativecommons.org/licenses/by/3.0/deed.en
#pluralistic#criti-hype#ai doomers#doomers#eacc#effective acceleration#effective altruism#materialism#ai#10 types of people#data science#llms#large language models#patrick ball#ben goldacre#trusted research environments#science#hrdag#human rights data analysis group#red jacket#religion#emily bender#emily m bender#molly white
289 notes
·
View notes
Text
Those reactions ranged from acerbic jokes (one common quip was "thoughts and prior authorisations", a play on the phrase "thoughts and prayers") to commentary on the number of insurance claims rejected by UnitedHealthcare and other firms.
At the extreme end, critics of the industry pointedly said they had no pity for Thompson. Some even celebrated his death.
The online anger seemed to bridge the political divide.
Animosity was expressed from avowed socialists to right-wing activists suspicious of the so-called "deep state" and corporate power. It also came from ordinary people sharing stories about insurance firms denying their claims for medical treatments.
28 notes
·
View notes
Text
THANK YOU, CLAIMS ADJUSTER!
Do you keep hearing stories about health claims now "mysteriously" being approved and think, nah, it's urban legends? Well, an urban legend just made my life better.
I had a prescription denied a few weeks ago for no discernible reason. It cost the same as the older, but riskier, drug I am now taking, given to me as a stopgap while waiting for approval. I got a 14-page boilerplate rejection letter from my insurer, Molina, saying that I had to "fail" on the first drug first after taking it for at least 30 days (I am just shy of that now, but only because I was taking leftovers of the same drug my husband had). My doc and the pharmacy tried several times to get it through, to no avail. I thought the cause was lost. I was getting ready to call the doc today to get a refill on the old drug and discuss whether it was OK now to say I had failed.
GUESS WHAT JUST SHOWED UP IN MY EMAIL? A notification that the scrip for the new drug has been filled. It's been at least two weeks since the final denial letter.

THANK YOU, CLAIMS ADJUSTER. IT'S A CHRISTMAS MIRACLE!
I should also note, this is the first time in four years on this health plan that I have had anything denied, other than a deductible for genetic testing I needed when I had cancer.
#uhc ceo#claims adjuster#uhc shooter#fuck the insurance companies#healthcare is a human right#protect this man at all costs#cw cancer
23 notes
·
View notes
Text
Chris McGreal at The Guardian:
The killing appeared so well-planned that at first glance many assumed it was a professional hit. The gunman who shot dead Brian Thompson, head of one of the US’s largest health insurance companies, on a New York street before dawn lay in wait with a weapon fitted with a silencer, kept his cool as his gun jammed and made a nimble escape after ensuring that his victim had been fatally struck.
However, within hours, an intense police manhunt turned up a trail of clues and possible mistakes, suggesting that while the killer had taken care to cover his tracks, he also made amateurish missteps that may yet lead to his identification and capture. But millions of Americans were less interested in the mechanics of what New York’s new police commissioner, Jessica Tisch, called “a premeditated, pre-planned, targeted attack” than the possible motive. Despite the fact the killer’s motive remains completely unknown, the death of UnitedHealthcare’s CEO unleashed an eruption of anger from people mistreated, or untreated, by the US’s rapacious medical industry and even a grim schadenfreude from some at Thompson’s death.
Hundreds of thousands of Americans are driven into bankruptcy every year by medical debts, with many of them losing their homes. Thousands die because insurance companies find reasons not to pay for treatment, including UnitedHealthcare, which denies about one-third of claims. Anthony Zenkus, a lecturer at the Columbia School of Social Work, spoke for many in a post on X.
“Today, we mourn the death of United Healthcare CEO Brian Thompson, gunned down.... wait, I’m sorry – today we mourn the deaths of the 68,000 Americans who needlessly die each year so that insurance company execs like Brian Thompson can become multimillionaires,” he wrote.
The revelation that shell casings at the scene were marked with the words “deny” and “defend” and “depose” added weight to speculation that the killer had had a vendetta against UnitedHealthcare, which earned $280bn in revenue last year insuring about 50 million people in the US. Two of the words are used by the industry in policy documents and were included in the title of a 2010 book Delay, Deny, Defend: Why Insurance Companies Don’t Pay Claims and What You Can Do About It.
Thompson was in New York from UnitedHealthcare’s headquarters in Minnesota for an investor conference. The 50-year-old father of two had been appointed the company’s CEO in 2021 and was paid $10m last year after overseeing a sharp rise in profits to $16bn that some critics said came from using artificial intelligence to routinely reject claims. His killer appears to have been well-informed about Thompson’s movements. The assailant apparently knew when his victim was likely to arrive at the New York Hilton Midtown hotel close to Central Park and which entrance he would use. [...]
Thompson was separated from his wife, Paulette, who fueled the speculation that he had been shot by someone with a grudge against UnitedHealthcare in her initial reaction to NBC News. “There had been some threats. Basically, I don’t know, a lack of coverage? I don’t know details. I just know that he said there were some people that had been threatening him,” she said. That there was plenty of public anger at UnitedHealthcare was not a secret.
Earlier this year, protesters from across the country rallied outside the company’s headquarters in Minnesota over its refusal to pay about one-third of claims, according to research by ValuePenguin, more than any other health insurer. Regulators and politicians have accused the company of boosting profits by systematically rejecting care to which people are entitled under their policies or of refusing to meet the full cost and leaving patients in debt. In October, a US Senate committee released a report cataloging how UnitedHealthcare and other companies deny patients care after they have been discharged from hospital following acute operations, even when doctors say they are necessary for a full recovery. The report said that the denials were principally made to drive up profits.
The day before Thompson was killed, the American Society of Anesthesiologists issued a statement condemning another health insurance company, Anthem Blue Cross Blue Shield, for imposing a limit on the amount of time for which it was prepared to pay for patients having surgery to receive anaesthesia. The company reversed its position after the shooting. But Thompson’s death unleashed something more visceral from people who feel helpless in the face of giant medical corporations with the power of life or death. [...] The backlash came not only from patients but doctors who recounted UnitedHealthcare refusing to pay for a child with cancer to receive medicines for the side effects of chemotherapy and questioning the necessity of lifesaving care. The outpouring of anger from within the medical profession at Thompson as representative of the greed of the insurance industry at the cost of lives caused Reddit moderators to delete a thread for the medical community, according to the Daily Beast. The health insurance industry is only one part of a medical system that the Princeton economists Anne Case and Angus Deaton, who won the 2015 Nobel prize for economics, have described as a “Sheriff of Nottingham redistribution” in the fleecing of ordinary Americans to give to rich corporations.
The murder of UnitedHealthcare CEO Brian Thompson has ignited bipartisan rage against the for-profit health insurance industry and its CEOs for their roles in creating unnecessary deaths fueled by delayed and denied claims.
22 notes
·
View notes
Text
Also preserved in our archive
by Hannah Buttle
Editor’s note: This article contains a brief mention of suicidal ideation.
Key points you should know:
There are currently no approved treatments for Long COVID and progress on clinical trials has been slow. Some medications can improve people’s quality of life, but they may not work for everyone.
With few choices, rejected disability claims, financial instability, and little support, some people with the disease have turned to online pharmacies, often based in India, to source potential medications.
Popular choices include medications used to treat conditions like HIV, hepatitis C, and acute COVID-19. Some of these drugs are being tested in upcoming clinical trials for Long COVID.
Buying medications online from unknown sellers can be risky; buyers might not receive the correct medication or even receive something harmful.
However, many people with Long COVID feel their quality of life has declined so severely that these risks are worth taking. With no approved treatments, lack of support, and stigma against the disease, many people with Long COVID are using overseas pharmacies to source medications. Some of these treatments are widely used for other conditions, such as HIV and hepatitis C, but are not approved for use in Long COVID.
“I was in such a desperate situation,” said Rafael, who lives in the U.K. and developed Long COVID in 2021. “I was bedbound, and I was within months of losing my job, which would then mean losing my home. So I didn’t have much to lose.”
Rafael bought several months’ worth of Maraviroc, an HIV drug, from a seller in India via WhatsApp. Soon after taking the Maraviroc, Rafael had a significant improvement in symptoms, although he was taking other medications at the same time.
“If I wasn’t so debilitated by Long COVID, I probably wouldn’t have taken the risk,” Rafael said.
The Sick Times spoke to several people with Long COVID who had used online pharmacies to import medications from abroad. Because importing medication can be illegal in certain circumstances, many sources interviewed for this article asked to be identified by their first name only or by a pseudonym.
Popular choices for people with Long COVID included the acute COVID-19 antiviral Paxlovid, the HIV drugs Maraviroc and Truvada, and the hepatitis C drug Sofosbuvir. Maraviroc and Truvada are currently being evaluated in an upcoming clinical trial at the Cohen Center for Recovery from Complex Chronic Illness, but results are not expected until at least early 2026.
Some people with Long COVID find some relief with off-label medications like low-dose naltrexone, but many told The Sick Times their doctors won’t prescribe these treatments. Even when doctors are willing to consider off-label treatments, health insurance often will not cover them.
Few treatments in sight The slow progress on clinical trials for Long COVID has been a source of frustration for both researchers and patients. The pharmaceutical industry has expressed little interest in finding treatments for the disease. Studies through the RECOVER initiative, launched by the U.S. National Institutes of Health (NIH), have primarily focused on observational approaches, such as asking people with Long COVID to track their symptoms, though the initiative is now planning new trials.
An analysis by The Sick Times found that fewer than a quarter of clinical trials for Long COVID are drug interventions, as of November 2024.
(interactive graph here)
Even when clinical trials take place, there is no guarantee of a “one-size-fits-all” treatment for Long COVID, said Ondine Sherwood, CEO of Long COVID SOS, a charity in the U.K. representing people with the disease. Currently, the available drugs may help only with specific symptoms or may work only for certain subsets of people with Long COVID.
Given the severity of symptoms and widespread government abandonment, it is unsurprising that some people with Long COVID have taken risks to seek relief from their symptoms since the beginning of the pandemic. Past unapproved treatments have included HELP apheresis, an expensive procedure that removes blood from a vein, filters the blood, and returns the filtered blood to the body. Many have also tried triple anticoagulant therapy, in which patients take aspirin, clopidogrel, and a blood thinner like Apixaban to break down small blood clots, called microclots. There is a high bleeding risk associated with triple anticoagulant therapy.
For many people with Long COVID, however, anything that offers a chance of improvement may seem worthwhile. Survey data suggest that the quality of life of someone with Long COVID can be worse than that of someone with stage four cancer. People with Long COVID may also be at a higher risk for suicidal ideation.
Financial insecurity can also drive people with Long COVID to consider experimental treatments, as many are out of work, behind on housing payments, and facing other financial challenges.
Some doctors may be willing to prescribe medications off-label for Long COVID and related conditions, like dysautonomia and mast cell activation syndrome (MCAS). Commonly prescribed drugs include beta-blockers, which lower heart rate, for dysautonomia, or H1 and H2 antihistamines for MCAS.
Dysautonomia drugs can lead to “massive improvement” for some, said Dr. Asad Khan, who worked as a respiratory doctor in the U.K. before developing Long COVID. For example, a beta blocker could bring down a patient’s heart rate while posing a limited risk, he said.
But some off-label treatments could carry higher risks, especially without a doctor’s oversight, said Khan: “You've got people taking anticoagulants and various other drugs that can affect the kidney, and the liver, and can have effects on the nervous system, and nobody's monitoring. The problems could be quite serious, and it could even be fatal.”
However, doing nothing for a patient can also put them in danger, said Khan. For instance, some research indicates that COVID-19 can lead to a higher risk of heart attacks and strokes for years after the infection.
People with Long COVID echoed these concerns. “I worry that, the longer we wait, the higher the destruction in our bodies,” said Lena, from Germany, who has had the disease since 2021.
After a difficult few months of symptoms, Lena decided to buy a generic form of Truvada, an HIV medication, through an online pharmacy. While she was scared, “pure despair” led her to try the medication, she said.
“I was having suicidal ideation,” she said. “If you have to weigh up how I was feeling versus taking an unknown pill, there’s no contest.” Many people with Long COVID who spoke to The Sick Times felt that buying medication online was their only choice.
How online pharmacies work Without a doctor to recommend the correct drug and dosage, many people with Long COVID receive advice from online social media groups. Users share tips on which drugs had worked for them, how to slowly increase the dosage of medications, and which side effects to expect.
Most of those interviewed by The Sick Times reported purchasing drugs without a prescription, either from national online pharmacies or from India via services like IndiaMart, an online marketplace. India is the world's largest exporter of generic pharmaceuticals.
“For me, what helped was a combination of ten days of Paxlovid and Sofosbuvir,” an antiviral drug for hepatitis C, said Tiff, from the U.S., who developed Long COVID in 2020. Tiff had read online about other people finding relief from the disease with these medications. She asked a friend to bring them back from India and had a significant decline in symptoms.
“I felt like I did pre-2020,” she said. “I had energy. I felt wonderful. No [Post-exertional malaise (PEM)] crash, no brain fog, no symptoms, nothing.” Tiff was later reinfected with SARS-C0V-2, and her Long COVID symptoms returned. She once again bought Sofosbuvir and Paxlovid from a seller in India and saw an improvement.
Lower prices offer another incentive to buy medications from abroad. Take Paxlovid, which can cost as much as $1,400 for a five-day course in the U.S., while a generic version from India costs just $103.
Sofia lives in Austria and has Long COVID. “In Austria, it would cost €40,000 for four months of Sofosbuvir,” she said, which “would be unaffordable.”
An anonymous Twitter/X user offered to help Sofia. She sent him €200, and he bought the medication in India and took it back to Europe. Since taking the Sofosbuvir, Sofia said she went from 40% to 60% of her previous level of functioning.
Risks and regulations Generic medications in the U.S., U.K., and Europe are commonly exported from India. But those exported through official channels are often subject to stricter regulatory standards than the medications available to locals. For those who have bought medications online from abroad, confirming the medications are safe can be difficult.
“We don’t have a functional regulatory system in India,” said Dinesh Thakur, a drug-safety advocate and former pharmaceutical executive. Online markets like IndiaMart have no safety guarantee.
“In the best-case scenario, the product may not contain enough of the active ingredient,” he said. “In the worst-case scenario, an injectable may contain endotoxins [harmful substances released by bacteria].”
If buyers from outside India have a bad experience, it would be difficult to hold a foreign company to account, Thakur added.
Nonetheless, many who spoke to The Sick Times felt that, despite the risks involved, they had to try something to relieve their symptoms.
“The symptoms grind you down so much, the risk calculus changes,” said Chris, from the UK, who has had Long COVID since 2020. “There is no help coming, nothing on the horizon.”
The World Health Organization has a checklist for gauging the safety of medicines purchased online. Tips include looking out for unusual activity on your credit card, checking security seals, and ensuring the batch number and expiry date on the package match throughout.
People with Long COVID may also be able to access off-label medications from more reliable sources. For instance, some online clinics may prescribe medications after a consultation. RTHM, a U.S.-based online clinic, offers a prescribing service for certain off-label medications for Long COVID, including low-dose naltrexone, beta-blockers for dysautonomia, and ketotifen for MCAS. In the U.K., those with a confirmed diagnosis of Long COVID or ME can buy low-dose naltrexone through Dicksons Chemist.
Another option for a small number of those with Long COVID is to join a clinical trial — though depending on the trial’s setup, some participants may receive a placebo instead of a drug.
Without the oversight of a pharmacist, taking a DIY approach to medications could also lead to dangerous medication interactions, even when the drugs are high quality. Paxlovid, for example, interacts with many drugs people take for Long COVID. These include ivabradine, some statins, and HIV medications. The University of Liverpool offers a COVID-19 drug interactions checker, which could help those using drugs like Paxlovid.
Regular blood tests could also help monitor for side effects. Truvada and Maraviroc can increase liver enzymes, and patients who take these medications for HIV prevention and HIV are advised to monitor liver enzymes regularly. Rafael, who bought Maraviroc, said he received monthly liver checks while taking the drug. These tests, which individuals can do privately without a GP referral, cost around £50 ($60) in the U.K.
Even if medications are safe, they are not guaranteed to work. People with Long COVID risk spending hundreds to thousands of dollars without success. New drugs could also lead to worse symptoms and significantly worsen a person’s health baseline.
Chris tried several medications, including Maraviroc and blood thinners, but has seen few improvements in symptoms. “You end up becoming your own guinea pig because nothing else is happening,” he said.
“It’s easy to depict people as reckless and not understanding the risks. But that’s not the case at all. Everyone understands the risks —they’re doing it because they’ve got no choice.”
#mask up#public health#wear a mask#pandemic#covid#wear a respirator#still coviding#covid 19#coronavirus#sars cov 2#long covid#covid19#covid conscious#covid is not over
18 notes
·
View notes
Text
Abortion is a top issue in the 2024 election, with a “growing share of voters in swing states now say[ing] abortion is central to their decision this fall,” according to Times/Siena College polls published in August. It is the “single most important issue” for women under 45.
On September 3, Vice President Kamala Harris began a “Fighting for Reproductive Freedom” bus tour in Florida, a state the Democratic Party has lost in the last two presidential elections, but which has abortion on the ballot this year. On November 5, citizens of Florida will be able to vote on an amendment that would restore legal access to abortion “before viability or when necessary to protect a patient’s health, as determined by the patient’s healthcare provider.” Florida currently has a six-week abortion ban, a law signed by Gov. Ron DeSantis in the wake of Dobbs.
The Harris bus tour began about a twenty-minute drive from Mar-a-Lago, the home of the former president who has declared responsibility for the fall of Roe under the Dobbs decision. The decision spawned multiple state abortion bans with severe repercussions upon a woman’s ability in ban states to receive critical or life-saving health care that may necessarily involve an abortion. At the September 10 presidential debate, Harris directly spoke to the post-Roe experiences of women suffering miscarriages and bleeding out in hospital parking lots because they couldn’t get treatment from doctors who were afraid of being prosecuted.
The other presidential candidate, former president Donald Trump, has bragged about overturning Roe v. Wade as a personal achievement of consummate importance. Public opinion polling shows, however, that the majority of Americans support legalized abortion. Moreover, the pro-reproductive rights position has won on abortion-related ballot measures following the Dobbs decision in conservative states like Ohio, Kansas, and Kentucky, and abortion measures are on the ballot this November in key states like Florida, Nevada, Colorado, and Arizona. Trump is now trying to downplay his involvement because the issue of abortion has become an albatross around the neck of the Trump campaign and the Republican Party itself. No wonder, then, in recent comments Trump has stated that abortion policy should be left to the states, and he has been publicly unwilling to endorse a nationwide abortion ban. At the debate, however, he repeatedly refused to answer whether he would veto legislation containing such a ban if it were presented to him as president, rejecting the question as an unlikely hypothetical while claiming he did the country “a great service” by helping overturn Roe.
In the wake of threats to in vitro fertilization (IVF) spurred by the Alabama Supreme Court decision that frozen embryos are children and the corresponding religious view held by some in the anti-abortion movement that a fertilized egg is a full-fledged person, Trump said both that he would mandate insurance companies cover IVF and the federal government would cover it for all Americans in need.
Attempting to persuade women who want their reproductive rights back, he suggested that Florida’s six-week abortion ban is “too short,” stating that he will be “voting that we need more than six weeks.” Later, however, his campaign walked this statement back, indicating that he “has not yet said how he will vote on the ballot initiative in Florida.” Trump attempted to rehabilitate his position on abortion further for his far right, evangelical base by spreading the disinformation that some states allow the legal execution of babies after birth. At the debate, he repeated this false statement, and one of the debate moderators fact-checked him on that. These are just a few examples of the ducking, bobbing, and weaving on abortion that Trump has been doing over the past few weeks.
But Trump’s attempts to obfuscate the abortion policy of his party and his future administration are laid bare by what is stated in the 2024 Republican Party platform and in the 2025 Presidential Transition Project (also known as Project 2025), a detailed blueprint for overhauling the executive branch, published by the Heritage Foundation, which involves at least 140 people who worked in the last Trump administration.
The word “abortion” only appears once in the 28-page Republican Party platform with the statement “[w]e will oppose Late Term Abortion, while supporting mothers and policies that advance Prenatal Care, access to Birth Control, and IVF.” But that statement must be understood in the context of the sentence that immediately precedes it: “We believe that the 14th Amendment to the Constitution of the United States guarantees that no person can be denied Life or Liberty without Due Process, and that the States are, therefore, free to pass Laws protecting those Rights.” By invoking the 14th Amendment to the Constitution in the context of abortion, the platform projects consistency with a religious belief that fertilized eggs, or so-called “unborn children” are full-fledged people deserving all of the rights and protections afforded by the U.S. Constitution. Neither abortion nor IVF, where some embryos may be discarded, is consistent with this “personhood” view. The limited and coded treatment of abortion in the platform is, however, consistent with Trump’s stated belief that the issue is harming the Republican Party and his candidacy with women.
But the Republican Party platform’s concise treatment of abortion should not be separated from Project 2025—a 922-page document replete with instances of the word abortion, along with detailed plans for how a Republican administration should promote “pro-life” policies and, in doing so, further curtail reproductive rights and access to reproductive healthcare.
Project 2025’s explicit anti-abortion positions and goals are summarized in the forward section of the document, which proclaims that “conservatives should gratefully celebrate the greatest pro-family win in a generation: overturning Roe v. Wade, a decision that for five decades made a mockery of our Constitution and facilitated the deaths of tens of millions of unborn children. But the Dobbs decision is just the beginning.”
A national abortion ban emerges as a prominent goal, as the document instructs that “[c]onservatives in the states and in Washington, including in the next conservative Administration, should push as hard as possible to protect the unborn in every jurisdiction in America. In particular, the next conservative President should work with Congress to enact the most robust protections for the unborn that Congress will support . . . .”
Some of the most noteworthy ideas and policies construed to achieve these outcomes presented in the rest of the document include:
A series of actions focused on preventing access to medication abortion nationwide. It is important to recognize that medication abortion accounted for 63% of all abortions in 2023—and that number does not account for pills that were mailed to people in states with an abortion ban, so the overall percentage is likely higher. It can be a particularly useful way to circumvent abortion bans. From the perspective of Project 2025, “[a]bortion pills pose the single greatest threat to unborn children in a post-Roe world.” Accordingly, Project 2025 recommends, among other things, that the FDA “reverse its approval of chemical abortion drugs,” and “stop promoting or approving mail-order abortions.” It also recommends that the DOJ “enforce the Comstock Act,” a law passed in 1873 that would, if read literally, make the mailing of any kind of abortifacient unlawful, effectively resulting in a nationwide ban on medication abortion.
Preventing both HHS and the CDC from treating or promoting abortion as health care. Consistent with this goal, and in furtherance of a “Life Agenda,” Project 2025 states that HHS should be known as the “Department of Life” through “explicitly rejecting the notion that abortion is health care.” Accordingly, Project 2025 recommends that the next Secretary of HHS eliminate the current HHS Reproductive Access Task Force and replace it with “a pro-life task force to ensure that all of the department’s divisions seek to use their authority to promote the life and health of women and their unborn children.” With respect to the CDC, Project 2025 recommends that it “should eliminate programs and projects that do not respect human life and conscious rights and that undermine family formation.” This would include the types of research it chooses to fund.
Preventing any kind of federal funding from supporting abortion care, including helping women travel out of state to receive an abortion. Project 2025 would also prohibit Planned Parenthood or any other abortion provider from receiving Medicaid funds. Two steps recommended in furtherance of this goal are having HHS “[i]ssue guidance reemphasizing that states are free to defund Planned Parenthood in their state Medicaid plans” and “[p]ropose rulemaking to interpret the Medicaid statute to disqualify providers of elective abortion from the Medicaid program.”
In stark contrast, the Democratic Party platform, written when President Biden was still the Democratic candidate for president, has its own section on “Reproductive Freedom” that embraces the idea that abortion is health care. It begins by acknowledging that since the fall of Roe, “more than 20 states have imposed extreme and dangerous abortion bans—many of which include no exception even for rape or incest—that put the health and lives of women in jeopardy, force women to travel hundreds of miles for care, and threaten to criminalize doctors for providing the health care that their patients need and that they are trained to provide.”
The platform looks to the range of actions taken during the Biden-Harris administration as a foundation for continuing efforts to protect reproductive rights and health care. Some of the most notable actions mentioned, which are opposite of the policies promoted by Project 2025, include enabling pharmacies to dispense medication abortion and defending FDA approval of medication abortion in court, expanding reproductive health care for service members and veterans, defending access to emergency abortion care, challenging threats by a Republican attorney general to prosecute those who assist women traveling out of state for abortion care, and assisting states in expanding access under Medicaid for people who travel from states where they are denied access to abortion care.
Going forward, the platform states that Democrats will, among other things, work to restore abortion rights through legislation (assuming a Congress with sufficient Democratic control), protect the right to access IVF, strengthen access to contraception, and continue to support access to medication abortion. The platform also indicates that Democrats will work to repeal the Hyde amendment, which “restricts federally funded abortions under major federal health care programs.”
The contrast between the parties’ platforms and policies is clear. Simply put, the Democratic Party platform explicitly states that “President Biden, Vice President Harris, and Democrats are committed to restoring the reproductive rights Trump ripped away.” As the presidential candidate who has proudly claimed responsibility for the fall of Roe, Trump’s rhetoric resembles the defensive moves of a boxer ducking, bobbing, and weaving to slip an opponent’s punches: he has tried to disavow Project 2025, tried to obfuscate Republican Party positions and plans, and backtracked on some of his positions in an attempt to portray his future administration as “great for women and their reproductive rights.”
20 notes
·
View notes
Text
A lack of empathy does not earn you sympathy.
How many people put thousands of dollars into paying for insurance only to die because their claim is rejected.
Anyone who is okay with this is guilty of causing the death of others.
I will not laugh but I will not cry for him either.
Fuck the health insurance industry.
15 notes
·
View notes