#health care equipment in UK
Explore tagged Tumblr posts
Text
Health Care Equipment UK Ensuring Your Facility Meets Modern Standards
In the UK, the health care equipment sector plays a crucial role in ensuring high-quality medical care. The range of equipment available encompasses everything from diagnostic tools and imaging machines to patient monitoring systems and surgical instruments. As technology advances, the demand for cutting-edge health care equipment has surged, prompting innovations that enhance diagnostic accuracy and patient outcomes.Health care facilities in the UK must navigate a diverse market to select equipment that meets their specific needs. This includes evaluating products based on functionality, reliability, and compliance with regulatory standards. Leading manufacturers and suppliers offer a variety of options, ensuring that hospitals, clinics, and private practices can access the latest technology.
How to Select the Right Health Care Equipment in the UK?
Choosing the right health care equipment in UK involves a thorough evaluation of your facility's needs, the type of equipment required, and budget considerations. Health care equipment UK offers a vast array of products, from basic diagnostic tools to advanced surgical instruments. When selecting equipment, it is essential to consider factors such as the manufacturer's reputation, product reviews, and compliance with UK health regulations. Additionally, understanding the technological advancements and how they align with your specific medical services will help ensure that the equipment meets your operational requirements and enhances patient care.
Key Innovations in Health Care Equipment UK for 2024
The year 2024 has brought several key innovations in health care equipment UK. These advancements include the integration of AI and machine learning in diagnostic tools, which provide more accurate and faster results. Telemedicine equipment has also seen significant upgrades, improving remote consultations and patient monitoring. Innovations in imaging technology, such as high-resolution MRI machines and advanced ultrasound devices, are enhancing diagnostic capabilities. These innovations not only improve patient outcomes but also streamline medical workflows, making the latest health care equipment UK an essential investment for modern medical facilities.
The Role of Health Care Equipment UK in Enhancing Patient Care
Health care equipment UK plays a pivotal role in enhancing patient care by providing accurate diagnostics, effective treatments, and continuous monitoring. High-quality equipment such as advanced imaging machines and patient monitoring systems enables healthcare providers to make informed decisions quickly. The introduction of cutting-edge technology ensures that medical professionals can deliver precise and timely interventions, improving patient outcomes. By investing in the latest health care equipment UK, facilities can maintain high standards of care, reduce errors, and ultimately contribute to better patient experiences and recovery rates.
When Purchasing Health Care Equipment in the UK?
When purchasing health care equipment in the UK, cost considerations are crucial. The initial investment for high-quality equipment can be significant, but it's important to weigh this against long-term benefits such as durability, reliability, and potential savings on maintenance and repairs. Additionally, many suppliers offer financing options or leasing agreements, which can help manage cash flow. Comparing prices from different vendors and considering the total cost of ownership, including installation and training, can help healthcare facilities make informed decisions and ensure they get the best value for their investment in health care equipment UK.
Top Brands and Suppliers of Health Care Equipment UK
Several top brands and suppliers of health care equipment UK are renowned for their quality and innovation. Companies such as Siemens Healthineers, GE Healthcare, and Philips Healthcare offer a range of advanced medical devices and solutions. These brands are known for their commitment to cutting-edge technology and reliability. Working with reputable suppliers ensures that healthcare facilities receive equipment that meets stringent regulatory standards and delivers excellent performance. It's beneficial to explore product reviews, case studies, and customer feedback when choosing suppliers to ensure you invest in the best health care equipment UK.
Health Care Equipment UK Compliance and Regulatory Standards
Compliance with regulatory standards is a key consideration when purchasing health care equipment UK. The Medicines and Healthcare products Regulatory Agency (MHRA) oversees the regulation of medical devices, ensuring they meet safety and efficacy requirements. Healthcare facilities must ensure that their equipment complies with these regulations to avoid potential legal issues and ensure patient safety. Additionally, equipment must meet specific quality standards and undergo regular inspections and certifications. Understanding these compliance requirements is essential for maintaining high standards of care and avoiding potential risks associated with non-compliant health care equipment UK.
The Impact of Technology on Health Care Equipment UK
Technology has a profound impact on health care equipment UK, transforming how medical care is delivered and managed. Advances in digital technology, such as AI, machine learning, and telemedicine, have led to the development of more sophisticated diagnostic and treatment tools. For instance, AI-powered imaging systems can analyze scans with greater accuracy, while telemedicine equipment facilitates remote consultations and monitoring. These technological advancements enhance the efficiency and effectiveness of health care services, leading to improved patient outcomes and more streamlined medical workflows. Embracing the latest technology in health care equipment UK is crucial for staying competitive in the evolving medical landscape.
Conclusion
Health care equipment UK encompasses a broad spectrum of tools and technologies essential for modern medical practice. From selecting the right equipment to understanding innovations and compliance, each aspect plays a crucial role in enhancing patient care and operational efficiency. By staying informed about the latest trends and investing in high-quality equipment, healthcare facilities can ensure they provide the best possible care while navigating the evolving landscape of medical technology. Embracing these advancements and maintaining a focus on quality and compliance will help facilities meet the demands of today’s healthcare environment and improve patient outcomes.
0 notes
Text
Hundreds of women have gone on strike in Scotland as three more councils face claims over equal pay.
Almost 500 workers walked out of their council roles in Falkirk, Renfrewshire and West Dunbartonshire in protest at a pay grading system which they say is outdated and pays women less than comparable male-dominated jobs.
Their action follows a strike by more than 8,000 female carers, caterers and cleaners in Glasgow, in 2018, which resulted in a payout of around £500m from Glasgow council, a bill it is yet to settle fully. It was the biggest equal pay strike in history in the UK.
Workers in similar jobs in Dundee, Perth and Kinross, Angus, Fife and Moray are now in ongoing disputes over equal pay.
The GMB union, which represents many of the women bringing claims, said local authorities across Scotland risk being bankrupted. GMB Scotland secretary Louise Gilmour said Scotland’s councils were approaching equal pay claims “like the Titanic approaching the iceberg”. “Councillors have their heads in the sand and executives have their fingers in their ears, but these equal pay claims will come, will be won and will need to be settled.
“We know local authorities are struggling to make ends meet and we know why. But to suggest women workers are somehow making things worse by asking for money they are owed … is as dishonest as it is disgraceful.”
In England, Birmingham city council last year said it was unable to balance its books due, in part, to equal pay claims. The GMB has ongoing equal pay disputes with a number of other councils including Coventry and Cumberland.
Gilmour called on the Scottish government to create a new specialist body to settle equal pay claims nationwide and enforce payments.
Fiona O’Brien, a home carer in Renfrewshire since 2016 and a GMB rep, said she took strike action “as a last resort because enough is enough”.
“For a long time, we’ve been told: ‘you’ll never go on strike, you care too much, you’ll never stand up for yourselves’,” she said. “But we’ve had enough now – we’ve been taken for granted for too long.”
She said her role is different to what was advertised and more complex than the grade it is paid at, including administering medications, caring for people with dementia and mental illness, using specialist equipment and physically moving people with restricted mobility.
“It’s been inspirational to see us all coming together and standing up for what’s right and fair,” she said. “This could potentially change the road for a lot of people working in care and could also bring more people into the sector.”
In the event of a successful equal pay claim, higher pay grades could be retrospectively applied, allowing workers to claim up to five years of back pay and costing councils millions of pounds, the GMB said.
The union said it expects to see pay reviews in at least a dozen more Scottish local authorities.
A spokesperson for Falkirk Health and Social Care Partnership said: “Falkirk council is committed to upholding equal pay, and continues to engage with GMB. We will seek to minimise disruption for those in need of our care and support at home services.”
A spokesperson for West Dunbartonshire council said: “We are committed to fair pay for home carers and, following a thorough and robust job evaluation process, the pay of a typical home carer has recently risen by at least £2,500 per annum through regrading of the role.”
A Renfrewshire Health and Social Care Partnership spokesperson said: “Negotiations between the Health and Social Care Partnership with all trade unions continue. A further offer was presented to all three trade unions, and Unison and Unite have paused industrial action as they consider this renewed offer. Unfortunately, GMB is continuing with industrial action following a consultative ballot with its members.”
Renfrewshire council did not respond to the Observer’s request for comment.
41 notes
·
View notes
Text
Marking Black History Month and recognising the incredible contributions of the black community, not just this month but every day of the year!
This year’s theme of ‘Reclaiming Narratives’ encourages us to shine a spotlight on the untold stories, the unsung heroes, and the everyday individuals making a big difference.
To celebrate we asked a number of our patronages to highlight some brilliant people whose work is having a lasting impact 👇

Farah Saeed is the Lead Assessment and Resettlement Coordinator at @PassageCharity House. She helps recently homeless individuals transition off the streets into sustainable housing. Nearly 90% move into long-term accommodation with personalised care.

Dwayne Fields is an adventurer, TV presenter, and the UK’s Chief Scout. After seven years as a Scout Ambassador, he now encourages young people from all backgrounds to embrace the outdoors, helping them build self-belief and find role models. As a dedicated volunteer, he also inspires @scouts' 140,000 adult volunteers, motivating others to get involved.

Yasmin Liverpool is a former Great Britain 400m runner and previous beneficiary of @TeamSportsAid support. Since retiring, she has joined the charity’s National Awards Committee and also supports its work in creating more accessible and inclusive talent pathways.

Ama Agbeze MBE has been a trustee of @TeamSportsAid since 2020. The England netball legend, who captained her country to Commonwealth gold in 2018, mentors talented young athletes and supports the delivery of its mental health and wellbeing programme. She also helps guide SportsAid on enhancing its equity, diversity and inclusion work through her role on the Board.

Alero Omaghomi is a Sickle Cell Nurse who supports children with the disease through resources and equipment funded by @NHSCharities Together. She helps sick children stay engaged with their education when they have to spend long periods out of school.

Loveness Scott is the Positive Action Lead at North East Ambulance Service, engaging ethnic minorities to improve understanding of NHS services. She leads lifesaving workshops and supports the recruitment of community ambassadors. Her role is funded by @NHSCharities Together to address health inequalities and promote first aid.

Olivier Nsengimana is the Founder of the Rwanda Wildlife Conservation Association, which helps to protect the endangered Grey Crowned Crane in Rwanda. He trained as a vet and originally worked with gorillas, before founding the RWCA. Olivier was a @tusk_org Award for Conservation finalist in 2016.

Sandra Igwe is the founder and CEO of The Motherhood Group, a leading social enterprise focused on improving maternal health outcomes for Black women in the UK. Sandra also coordinates Black Maternal Mental Health Week UK and organises the annual Black Maternal Health Conference. @MMHAlliance
- The Prince and Princess of Wales
#prince and princess of wales#the prince and princess of wales#kp tweets#kp twitter#prince of wales#princess of wales#prince william#princess catherine#the prince of wales#the princess of wales#19102024#kensingtonroyal#BlackHistoryMonthUK24#british royal family#brf#royalty#british royalty
18 notes
·
View notes
Text
Get ready for some grade-A bullshit
How can they claim that these masks cause "facial ulcers" and "Breathing problems" when miners can wear P100 elastomeric masks underground for 4 to 8 hours at a time with no similar complaints?
Filed under 'ugly' on our archive (we also have a 'good' and a 'bad')
By Jim Reed
There is only “weak evidence” that high-grade face masks better protected health workers than surgical ones in the pandemic, the Covid inquiry has been told.
Prof Susan Hopkins, chief medical adviser at the UK Health Security Agency (UKHSA), said respirator masks – known as FFP3s – may have performed no better than thin surgical masks in real-life situations.
She said there could be “significant harms” from wearing tight-fitting FFP3s, including blisters and breathing difficulties.
“If the evidence was strong that FFP3s really protected people, and we saw a definitive reduction [in infections], they would have been recommended,” she said.
'Life and death' Not all scientists agree on what has become a controversial issue.
The BBC has previously reported on research which appears to show a significant real-world benefit from wearing higher-grade masks on hospital wards.
Throughout the first two years of the pandemic, groups representing doctors, nurses and other health workers repeatedly called for urgent improvements to personal protective equipment (PPE), including the wider use of respirators.
FFP3s are tight-fitting masks with a built-in air filter designed to block out tiny aerosol particles which can carry the virus.
Before they can be used, each wearer must undergo a fit test, to make sure the mask is properly sealed to the face.
For most of the pandemic, national guidance across the whole UK said that healthcare workers should wear basic surgical masks rather than FFP3s, except in intensive care or a small number of medical situations.
The decision was heavily criticised by some staff with the doctors’ union, the BMA, calling it a "matter of life and death".
National guidance on face masks from April 2020 was drawn up by a group of experts from across the United Kingdom known as the IP (Infection Prevention) Cell.
Its membership included representatives from the NHS, government departments and health bodies, including Public Health England (PHE), the organisation replaced by UKHSA in 2021 in a shake-up ordered by then-Health Secretary Matt Hancock.
The inquiry was shown minutes from an IP Cell meeting on 22 December 2020, just after the new Alpha variant of Covid had been detected, which appeared to show disagreement about the use of higher-grade FFP3 masks.
The records quote Dr Colin Brown, now the deputy director of clinical and emerging infections at UKHSA but at the time with PHE, as saying: "Our understanding of aerosol transmission has changed. A precautionary approach to move to FFP3 masks [in all healthcare settings] whilst we are awaiting evidence should be advised."
However, the wider IP Cell decided that no upgrading of the guidance was warranted at the time, and NHS trusts were told to continue to supply staff with standard surgical masks in almost all cases outside intensive care.
It was not until January 2022 that the advice changed, saying that FFP3 respirators "must be worn" by all staff if they are caring for patients with a virus such as Covid, and should be offered to other staff depending on a risk assessment.
By that point, the World Health Organization, and other health bodies, had recognised Covid could be spread in tiny airborne particles over distances longer than 6.5ft (2m), something officials said was impossible at the start of the pandemic.
Prof Hopkins, who served as PHE’s chief Covid adviser before moving across to UKHSA, told the inquiry that FFP3 masks offered a high degree of protection in laboratory studies, but the real-world benefits were less clear-cut.
“Where we looked at it, and repeatedly looked at it and are still looking at it, the evidence is weak that FFP3s protected more than fluid-resistant surgical masks,” she said.
“At the outset, in March 2020, the risks were that we had never asked people to wear FFP3 masks for prolonged periods.
“We saw them get ulcers on their faces and having challenges breathing and challenges in being hydrated.”
'Groupthink' Asked about the December 2020 IP Cell minutes, which suggested PHE was pushing behind-the-scenes for the wider use of respirator masks in healthcare, Prof Hopkins said that was a "really challenging time" in the pandemic with the UK about to enter a third wave of the virus.
“The fact that PHE was giving and airing a different view is an example of [us] not being involved in groupthink,” she said.
The Covid inquiry is currently taking evidence about the impact on the NHS and healthcare systems across all four nations of the UK.
More than 50 witnesses are expected to appear in this third section or "module", which runs until the end of November.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
10 notes
·
View notes
Text
Britain’s lead public health body has a staggering lack of control over billions of pounds of spending, and there is no plan for stockpiling vaccines or personal protective equipment (PPE) for a future pandemic, a damning MPs’ report has found. The public accounts committee was highly critical of the repeated governance and financial failings at the UK Health Security Agency (UKHSA), which was set up with great fanfare under Boris Johnson. Meg Hillier, the committee chair, said it would be “utterly inexcusable” for the government to have failed to make serious preparations for future health emergencies and warned the lack of a plan for stockpiling could leave health workers once again exposed to danger as they were in 2020. The committee lambasted the Department of Health and Social Care (DHSC), which oversees UKHSA, for lacking a strategy for reserves of PPE, vaccines and medicines despite its mandate to protect the country’s health security. The MPs were particularly critical of the decision for it to be led by Prof Dame Jenny Harries, a former deputy chief medical officer for England, saying she was “appointed into a role, as accounting officer and chief executive, of which she had no previous experience”.
[...]
Hillier said it was “completely staggering that an organisation envisaged as a foundation stone of our collective security was established with a leadership hamstrung by a lack of formal governance, and financial controls so poor that billions of pounds in NHS test and trace inventory can no longer be properly accounted for”.
37 notes
·
View notes
Text
youtube
Ten Ways To Improve Health & Wellness Based On Latest Brain Science And Neurotechnologies
These are 10 priorities to consider, if we want to improve health & wellness visit site here based on the latest neuroscience and non-invasive neurotechnology:
Transform the mental health framework, from a constellation of diagnoses such as anxiety, depression, ADHD…to the identification and strengthening of the specific brain circuits ("cells that fire together wire together") that may be deficient. This is what the Research Domain Criteria framework, put forth by the National Institute of Mental Health, is starting to do.
Bring meditative practices to the mainstream, via school-based and corporate programs, and leveraging relatively-inexpensive biometric systems
Coopt pervasive activities, such as playing videogames…but in a way that ensures they have a beneficial effect, such as with cognitive training games specifically designed to prolong cognitive vitality as we age
Offer web-based psychotherapies as first-line interventions for depression and anxiety (and probably insomnia), as recommended by the UK's National Institute for Health and Care Excellence.
Monitor the negative cognitive and emotional side-effects from a variety of medical interventions, to ensure unintentional effects from the cure are not more afflictive than the treated person's original condition. Given that the US Food and Drug Administration just cleared an innovative mobile brain health assessment, what prevents wider use of baseline assessments and active monitoring of cognition as an individual begins a particular treatment program or medication?
Combine pharmacological interventions (bottom-up) with cognitive training (top-down) such as the CogniFit - Bayer partnership for patients with Multiple Sclerosis
Update regulatory frameworks to facilitate safe adoption of consumer-facing neurotechnologies. Start-up Thync just raised $13 million to market transcranial stimulation in 2015, helping users "alter their state of mind." That's not a medical claim per se…but does the technology need to be regulated as a medical device?
Invest more research dollars to fine-tune brain stimulation methods, such as transcranial magnetic stimulation, to enable truly personalized medicine.
Adopt big data research models, such as the newly-announced UCSF Brain Health Registry, to leapfrog the existing small clinical trial model and move us closer towards delivering personalized, integrated brain care.
And, last but certainly not least, promote physical exercise and bilingual education in our schools, and reduce drop-out rates. Improving and enriching our schools is perhaps the most powerful social intervention (and the original non-invasive neurotechnology) to build lifelong brain reserve and delay problems brought by cognitive aging and dementia.
If we want every citizen to adopt more positive lifestyles, especially as we face longer and more demanding lives, it is imperative that we better empower and equip ourselves with the right cognitive and emotional resources and tools. Initiatives such as those above are a significant start to view and treat the human brain as an asset to invest in across the entire human lifespan, and to truly maximize years of healthy, functional and meaningful living.
2 notes
·
View notes
Text

And just like that, it's Day Three of the #TinyCrewBigRaffle Countdown to Christmas Eve. Today brings us to Mermaids one of the two excellent charities chosen for us by Con O'Neill, and the charity with the second highest amount donated ❤️
(Amy is especially moved to see so much money has been donated from outside the UK, and thanks Christina for also choosing to to donate to Mermaids with me for the final two donations.)
Mermaids supports transgender, non-binary and gender-diverse children and young people, as well as their families and professionals involved in their care.
Transgender, non-binary and gender-diverse children and teens need support and understanding, as well as the freedom to explore their gender identity. Whatever the outcome, Mermaids is committed to helping families navigate the challenges they may face.
Mermaids' support… -Reduces isolation and loneliness for transgender, non-binary and gender-diverse children, young people and their families. -Provides families and young people with the tools they need to negotiate education and health services. -Helps young people to cope better with mental and emotional distress, and equips their parents with what they need to offer individual support. -Improves the self-esteem and social skills of children and young people. - Improves awareness, understanding and practices of teachers, GP’s, CAMHS, Social Services and other professionals.
#ofmd#our flag means death#tinycrewbigraffle#pirates#our flag means love#charity#raffle#ofmd s2#ofmd bts#our flag means gay
6 notes
·
View notes
Photo


Queen Camilla’s Patronages
The Royal Osteoporosis Society (President from 01.10.2001)
We’re the Royal Osteoporosis Society – the UK’s largest national charity dedicated to improving bone health and beating osteoporosis. And we’re here for everyone. We equip people with practical information and support to take action on their bone health.Working with healthcare professionals and policy-makers, we’re influencing and shaping policy and practice at every level. We’re driving the research and development of new treatments, to beat osteoporosis together. The charity was established in 1986 and has since grown into a well respected national charity.
In recognition of her tireless work for osteoporosis and her support of the charity, Her Majesty The Queen Consort became President of the Royal Osteoporosis Society in October 2001. Her Majesty first became a supporter of the charity in 1994, when her mother died as a result of osteoporosis, and she later become a patron in 1997.
Her first public speech was made in 2002 at the World Congress on Osteoporosis, hosted by the International Osteoporosis Foundation (IOF) in Lisbon. In this speech, The Duchess explained why fighting osteoporosis is so important to her:
“My family knew nothing about osteoporosis. The local GP was kind and sympathetic but he, like us, was able to do little to alleviate the terrible pain that my mother suffered so stoically. We watched in horror as she quite literally shrank before our eyes. She lost about eight inches in height and became so bent that she was unable to digest her food properly, leaving her with no appetite at all. In her latter years, she could not breathe without oxygen or even totter round her beloved garden on her Zimmer frame. I believe the quality of her life became so dismal and her suffering so unbearable that she just gave up the fight and lost the will to live. As a result of my mother’s death, I became determined to find some way of helping people with osteoporosis from experiencing the same fate and general disregard that she encountered. I was lucky enough to discover, on my doorstep, the National Osteoporosis Society, a relatively new and small charity, piloted by the indomitable Linda Edwards.”
Her poignant words did much to generate a significant amount of press interest in osteoporosis that year and those in attendance at this event used the occasion to urge policy makers across the globe to make the disease a priority for national health care agendas.
During her time as President, Her Majesty has taken an active and very personal interest in raising awareness of our work. Over the years, she has held receptions, attended events, met people living with the condition, and made many impassioned speeches.
In 2007, Her Majesty received the Kohn Foundation Award from Dr Ralph Kohn (later Sir Ralph Kohn) in recognition of her contribution to raising awareness of osteoporosis.
40 notes
·
View notes
Text
A landmark study has uncovered corruption “red flags” in government Covid contracts worth more than £15bn – representing nearly one in every three pounds awarded by the Conservative administration during the pandemic.
The analysis, billed as the most in-depth look yet at public procurement during the crisis, warns that systemic bias, opaque accounting and uncontrolled pricing resulted in vast waste of public funds on testing and personal protective equipment (PPE).
The review of more than 5,000 contracts across 400 public bodies identifies 135 high-risk contracts with a value of £15.3bn where investigation is merited due to the identification of three or more corruption red flags, which include a lack of competition, delays or failure to release information on procurement, and conflicts of interest in the award of contracts. The report by Transparency International UK finds:
At least 28 contracts, worth £4.1bn, went to those with known political connections to the Conservative party. This amounts to almost a tenth of the money spent on the pandemic response.
Fifty-one contracts, worth £4bn, went through the “VIP lane”, a vehicle through which certain suppliers were given priority, of which 24, worth £1.7bn, were referred by politicians from the Conservative party or their offices.
£1bnwas spent on personal protective equipment from 25 VIP-lane suppliers that was later deemed unfit for use. The VIP lane was found to unlawful by a high court judge in a 2022 ruling.
Eight contracts, worth £500m, went to suppliers that were no more than 100 days old.
The UK government awarded more than £30.7bn in high- value contracts without competition – equivalent to almost two-thirds of all Covid contracts by value.
The Department of Health and Social Care wrote off £14.9bn in public money over a two-year period – equivalent to the government’s total spend on personal protective equipment.
In response, a spokesperson for the Conservative party pointed to a National Audit Office report that found that ministers had properly declared their interests.
“Government policy was in no way influenced by the donations the party received – they are entirely separate,” he said.
The Labour chancellor, Rachel Reeves, has said she will appoint a Covid corruption commissioner to examine an estimated £7.6bn worth of Covid-related fraud, with particular focus on the billions wasted on useless PPE.
The National Crime Agency (NCA) is investigating PPE Medpro – a company led by Douglas Barrowman, husband of the Conservative peer Michelle Mone – which was awarded government contracts worth more than £200m. Barrowman and Lady Mone deny any wrongdoing.
But researchers warn of a potential higher cost to the public purse than that acknowledged by Reeves as a result of the previous administration’s widespread and “often unjustifiable” suspension of procurement checks and safeguards.
Of the £1tn-worth of contracts signed in the three years from February 2020, government data shows that £48.1bn was spent in relation to the pandemic, largely on Covid testing and PPE, and a third (32%) of that spending raised serious concerns.
The report, entitled Behind the Masks, acknowledges that there had been a need to act quickly as Covid took grip, but the authors claim there was an unjustifiable disregard for publishing the details of contracts and an unhealthy reliance in government on uncompetitive procurement even as the impact of the crisis on the health system subsided.
Almost two-thirds of all high-value Covid contracts by value lacked competition. A year into the pandemic, UK contracting authorities were still frequently making awards without competition even as countries in the EU such as Italy were reverting to competitive bidding.
It is claimed that the so-called VIP and high-priority lanes – which triaged offers of assistance that came via officials, MPs, members of the Lords and ministerial offices – enabled unqualified politicians to fast-track the reviewing of offers from PPE and testing suppliers – a practice said to be unique to the UK’s pandemic response.
About 2% of all offers – about 500 – went through the VIP lane. Of these, 51 suppliers were successful, representing a 10% success rate, compared with the 0.7% rate on other routes, while the prices paid were on average 80% higher.
The report estimates that Covid contracts boosted some suppliers’ profit margins by as much as 40%.
Of the 135 contracts identified as being high risk, the report’s authors write: “The most common red flags were delayed publication of contracts and those awarded uncompetitively. However, most of these contracts exhibited red flags across multiple areas of risk – including those associated with the supplier profile, the procurement process and the contract outcomes – and often spanning all three. Some contracts displayed as many as eight red flags.”
A Treasury spokesperson said: “The chancellor has been clear that she will not tolerate waste and will appoint a Covid Corruption Commissioner to get back the money that is owed to the British people.
“The commissioner will report directly to the chancellor, working with the secretary of state for health and social care, and their report will be presented to parliament for all members to see.”
The findings have been published on the day that public hearings examining the impact of the pandemic on the healthcare system are due to start. Transparency International UK, as part of the UK Anti-Corruption Coalition, has core participant status in the proceedings.
Joe Powell, a Labour MP and the chair of the all-party parliamentary group on anti-corruption and responsible tax, said: “The scale of money lost to the taxpayer is staggering. Amid a cost of living crisis, it is simply unacceptable that so much money could have been lost to cronyism and human error. Public money must be accountable.
Daniel Bruce, the chief executive of Transparency International UK, said there had been a collapse in the normal checks and balances, and that a slew of changes in procurement was necessary to rebuild confidence in the system.
He said: “The scale of corruption risk in the former government’s approach to spending public money during the years of the Covid pandemic was profound.
“That we find multiple red flags in more than £15bn of contacts – amounting to a third of all such spending – points to more than coincidence or incompetence.
“The Covid procurement response was marked by various points of systemic weakness and political choices that allowed cronyism to thrive, all enabled by woefully inadequate public transparency. As far as we can ascertain, no other country used a system like the UK’s VIP lane in their Covid response.”
4 notes
·
View notes
Text
Wow, a couple of my posts have got popular recently. Hello, new people! I'm an autistic trans man with ADHD, a diverse array of other health issues and disabilities, and no money! 😘 This is a sideblog so you won't get any follows or comments from this url, but I appreciate you for being here. I figure I'd better make a pinned post since a lot of the same things come up frequently in replies and I might save some folks some time:
I'm not in the US. I am from there but I've lived in central Europe for over 15 years now. A lot of stuff is different here. I know a lot of folks reading this blog are in the US or UK and a lot of folks try to make suggestions for some of the troubles I have but 99% of the time it's something that's ubiquitous in the US or UK but straight-up not available here whatsoever. I appreciate the intent, but if you see a really simple, easy solution to a problem I post on here, odds are I've thought of it, I've investigated it, I've tried it, and it's either not available or it doesn't work for me for one reason or another.
Things that aren't available here include air conditioners, box fans, square hepa filters, most dating apps (in fact most apps in general), a lot of streaming services, many types/brands of medication and types of medical equipment that are super common in other countries, Amazon (seriously), Etsy, and a lot of other online shopping sites, a truly incredible number of food and drink items (especially processed or pre-made ones), and most social groups/clubs/events (at least ones accessible to an English speaker). (And much, much more!)
I have a lot of medical issues which I sometimes write about here. I don't necessarily explain everything in every post because that would mean writing a novel every time, but since people keep asking, yes, I know what EDS is, yes, I know what MCAS is, yes, I am investigating these possibilities along with many others with my doctors, but it is an obscenely slow process. This country has a serious lack of specialists in a lot of conditions that are lesser-known or which have only been properly understood in recent years. Overall the medical system here is quite good and I can go to almost any doctor and get almost any of the medications available in this country without paying anything, but that comes at the cost of a language barrier and a lot of outdated diagnostic standards for particular conditions like autism, ADHD, and the aforementioned EDS and MCAS. In short, I'm working on it, but my options are limited and the process is slow.
The disability system is also different here. I know the system in the US is horrific and my heart goes out to everyone struggling to survive in it. Fortunately it is better here. It's a very long, slow process to get approved (mainly because you have to get a pretty significant paper trail first, and the lack of specialists means it can take months to get appointments), but approval is based mostly on the recommendations of doctors, the amount you get is calculated based on your income and how much working capacity you have lost, and it does not carry restrictions on how much money you are allowed to earn or have at any time. I am currently in the process of trying to get some benefits but it is likely to take another year if not longer.
If other stuff starts coming up frequently in comments and replies, I'll add answers here. For now, thanks for reading what I have to share and for the kind words (and kind attempts to help) that many of you have left me. I hope that what I write is helpful to some of you. It's hard to find time and energy to write a lot at the moment, but I will try to post more, since it's clear that a lot of people relate and are looking for more of what I have to share.
Take care of yourselves.
13 notes
·
View notes
Text
Top 10 Colposcopy Clinics in London: Ensuring the Best Care

When it comes to women's health, choosing the right clinic for specialized procedures like colposcopy is crucial. Colposcopy is an essential diagnostic tool for detecting cervical abnormalities, and having it done at a reputable clinic ensures you receive the highest quality care. Here’s a comprehensive guide to the top 10 colposcopy clinics in London, each known for their exceptional services, experienced staff, and patient-focused care.
1. Grosvenor Gardens Healthcare
Location: 7-10 Grosvenor Gardens, Belgravia, SW1W 0DH Website: Grosvenor Gardens Healthcare
Grosvenor Gardens Healthcare provides comprehensive women's health services in a modern facility. The clinic is known for its personalized care and experienced medical professionals.
2. Harley Street Gynaecology
Location: 113-115 Harley Street, Marylebone, W1G 6AP Website: Harley Street Gynaecology
Harley Street Gynaecology offers top-notch colposcopy services with a team of expert gynecologists. The clinic prides itself on providing personalized care in a comfortable and professional setting.
3. The London Clinic
Location: 20 Devonshire Place, Marylebone, W1G 6BW Website: The London Clinic
The London Clinic is renowned for its high standards and comprehensive medical services. With advanced diagnostic technology and expert gynecologists, patients receive precise and compassionate care.
4. Harley Street Clinic
Location: 35 Weymouth Street, Marylebone, W1G 8BJ Website: Harley Street Clinic
Known for its elite medical services, Harley Street Clinic offers personalized treatment plans from top specialists. The clinic is famous for its patient comfort and state-of-the-art facilities.
5. Guy’s and St Thomas’ Hospital
Location: Great Maze Pond, SE1 9RT Website: Guy’s and St Thomas’ Hospital
This esteemed NHS hospital provides extensive women's health services. The colposcopy clinic is staffed by highly skilled professionals and offers comprehensive diagnostic and treatment options.
6. The Portland Hospital
Location: 205-209 Great Portland Street, Marylebone, W1W 5AH Website: The Portland Hospital
Specializing in women’s health and maternity care, The Portland Hospital is part of HCA Healthcare UK. The clinic uses the latest diagnostic tools and offers care from experienced gynecologists.
7. Chelsea and Westminster Hospital
Location: 369 Fulham Road, SW10 9NH Website: Chelsea and Westminster Hospital
Chelsea and Westminster Hospital is dedicated to patient-centered care, delivering excellent clinical outcomes. It features a professional healthcare team and advanced medical technology.
8. University College Hospital (UCH)
Location: 235 Euston Road, NW1 2BU Website: University College Hospital
Part of the University College London Hospitals NHS Foundation Trust, UCH is known for its research-based approach and superior patient care. The colposcopy clinic uses advanced diagnostic tools for effective treatment.
9. Royal Free Hospital
Location: Pond Street, Hampstead, NW3 2QG Website: Royal Free Hospital
Royal Free Hospital emphasizes patient safety and comfort. The gynecology department offers high-quality colposcopy services with advanced equipment and specialized professionals.
10. King’s College Hospital
Location: Denmark Hill, SE5 9RS Website: King’s College Hospital
King’s College Hospital provides comprehensive healthcare services. The colposcopy clinic is known for its supportive environment, experienced gynecologists, and cutting-edge technology.
2 notes
·
View notes
Text
Understanding Hair Transplant Procedures
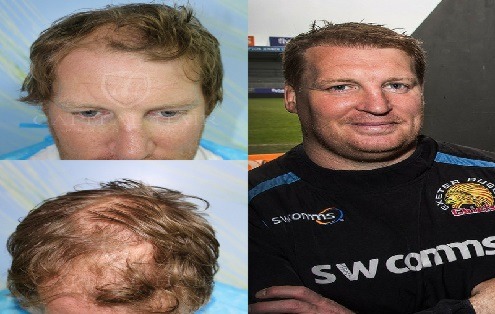
Hair Transplant Costs UK are surgical procedures that involve moving hair follicles from one part of the body (usually the back or sides of the scalp) to areas where hair is thinning or balding. There are two main types of hair transplant procedures:
Follicular Unit Transplantation (FUT):
Also known as the strip method, FUT involves removing a strip of scalp from the donor area and then dissecting it into individual follicular units for transplantation. This method can result in a linear scar at the donor site, which may be a consideration for those who prefer shorter hairstyles. Follicular Unit Extraction (FUE):
In FUE, individual hair follicles are extracted directly from the donor area using a tiny punch tool and then transplanted to the recipient area. FUE is less invasive and leaves minimal scarring, making it a popular choice for many patients. Factors Influencing the Cost of Hair Transplants Several factors can influence the cost of hair transplants in the UK. Understanding these factors can help prospective patients plan and budget for their procedure:
Type of Procedure:
Generally, FUE procedures are more expensive than FUT due to the Clinic Location and Reputation:
Clinics in major cities or those with renowned surgeons may charge higher fees. Reputable clinics with high success rates and experienced surgeons often justify their higher costs with better outcomes and patient satisfaction. Surgeon's Expertise:
Surgeons with extensive experience and specialized training in hair transplantation typically charge more for their services. Patients are advised to prioritize the surgeon’s expertise and track record over cost to ensure the best results. Technology and Techniques Used:
Advanced techniques and equipment, such as robotic FUE systems, can increase the overall cost of the procedure. Innovative methods like Direct Hair Implantation (DHI) or the use of Platelet-Rich Plasma (PRP) therapy as an adjunct treatment may also impact costs. Additional Costs and Considerations Beyond the primary procedure costs, there are several additional expenses and considerations that prospective patients should be aware of: Travel and Accommodation:
For those traveling to a different city or country for their procedure, travel and accommodation costs can add up. It’s important to factor in these expenses, especially if multiple trips are required for consultations and follow-ups. Time Off Work:
Depending on the nature of their job, patients may need to take time off work for recovery. While some can return to work within a few days, others may need up to two weeks, impacting their income during this period. Financing Options and Insurance Hair transplants are generally considered elective cosmetic procedures and are not covered by the NHS or private health insurance. However, several financing options are available:
Payment Plans:
Many clinics offer payment plans that allow patients to spread the cost over several months or years. Interest rates and terms vary, so it’s essential to review these options carefully. Medical Loans:
Specialized medical loans are available for cosmetic procedures, providing another financing option. It’s important to compare interest rates and terms to find the best deal. Credit Cards:
Some patients choose to finance their hair transplant using credit cards, though this can be more expensive due to high-interest rates. Cost Comparison with Other Countries For those considering traveling abroad for their hair transplant, it’s worth comparing costs in different countries. Popular destinations for hair transplants include Turkey, where the procedure can be significantly cheaper than in the UK:
Turkey:
Known for its high-quality clinics and experienced surgeons, hair transplants in Turkey can cost between £1,000 and £3,500. Many clinics offer all-inclusive packages that cover accommodation, airport transfers, and post-operative care. Eastern Europe:
Countries like Hungary and Poland offer competitive prices, ranging from £1,500 to £4,000, with reputable clinics and experienced surgeons. Asia:
India and Thailand are also popular for medical tourism, with hair transplant costs ranging from £1,200 to £3,500. Conclusion The cost of hair transplants in the UK can vary widely based on several factors, including the type of procedure, the number of grafts required, the clinic's location and reputation, and the surgeon's expertise. Additionally, prospective patients should consider pre-operative and post-operative expenses, as well as potential travel and accommodation costs if opting for treatment abroad.
While cost is an important consideration, it should not be the sole factor in deciding where to undergo a hair transplant. The quality of care, the surgeon's experience, and the clinic's reputation are crucial to achieving the desired results and ensuring a safe and successful procedure. By thoroughly researching and understanding the various aspects of hair transplant costs, individuals can make informed decisions and take a significant step towards restoring their hair and confidence.
2 notes
·
View notes
Text
5 minute read
The UK’s controversial two-child benefit limit, which restricts welfare payments to larger families in an attempt to force parents to find work, has failed to increase employment levels – but it has left hundreds of thousands of households in poverty, according to the first study of its kind.
The government introduced the two-child limit in 2017, arguing that removing eligibility for benefits worth £3,000 a year per child for a family’s third and subsequent children would “incentivise” parents to move into work, or work more hours to make up the difference.
However, the study says the policy’s impoverishment of larger low-income households has helped few parents get a job – instead, its “main function” has been to push families further into poverty and damage their mental health.
“We found that, rather than increasing employment, the two-child limit increases poverty and hardship – and that this can actually make it harder for parents to take up work,” said Kitty Stewart, a co-author of the study and an associate professor of social policy at the London School of Economics.
The policy – called the “worst social security policy ever” by one academic expert shortly after its introduction – is now estimated to affect about 1.5 million children, with more than a million of them growing up in poverty. More than half the households affected are working families.
The study says the two-child policy fails to understand how and why parents in larger low-income families prioritise caring roles over work. It underplays many of the costs and complications of moving into work while bringing up young children, such as finding accessible and affordable childcare.
It is scathing about the design of the policy, suggesting it relies on theoretical economic models that assume reductions in benefits would automatically increase labour supply through an “income effect” incentive – an effect evidence shows to be weak or non-existent.
In practice, many parents hit by the limit said they found it harder to enter paid work, because they could no longer afford skills training or to buy equipment for fledgling businesses. Financial difficulties caused by the policy also led to a deterioration in their mental health.
A key lesson, the study says, is that “policymakers need to understand the everyday lives of those in receipt of social security before designing and predicting the effects of welfare reforms. A failure to do so can, in cases like this, preclude the main aims of the policy from being realised, while creating significant harms to affected families.”
The architect of the policy, one of many austerity-era benefit reforms, is the former chancellor George Osborne. He announced it in 2015 amid media hysteria surrounding “benefits broods” – large families supposedly having several children to exploit an allegedly overgenerous welfare system.
The policy was later savaged by Tory former welfare reform minister David Freud, who called it “vicious” and an “excrescence”, and said it should be scrapped. He claimed the policy was forced on a reluctant Department for Work and Pensions (DWP) by the Treasury as the price of introducing universal credit.
Research published last year found the two-child limit – hailed by one minister as a way of teaching low-income families that “children cost money” – has had little impact on restricting family size. Since the policy’s introduction, the fertility rate for third and subsequent children born to poorer families has barely fallen.
A DWP spokesperson said: “We want to help more parents to re-enter and progress in work, and encourage them to consider our childcare offers, which we are boosting to help low-income families.
“The two-child policy asks families on benefits to make the same financial decisions as families supporting themselves solely through work, and there continues to be careful exemptions and safeguards in place within the policy to protect people in the most vulnerable circumstances.”
21 notes
·
View notes
Text
Why Using Buccal Training For Epilepsy Is Important?

Understanding Care Mandatory Training
Understanding care training requirements in the UK is essential for all domiciliary carers. Statutory and mandatory courses cover key subjects to ensure staff members and clients remain safe.
Health and safety training courses cover crucial protocols like risk evaluation, manual handling, fire safety, safeguarding training for care workers to detect abuse as well as local reporting procedures, medication administration training is also a necessity for domiciliary care providers.
Online buccal training for epilepsy wrap training
Buccal training for epilepsy (epilepsy medication administration training) assists healthcare professionals and caregivers to provide effective and safe care to individuals experiencing seizures. The training offers valuable skills that can reduce anxiety and stress as well as enhance quality of life for people living with epilepsy.
Effective training also ensures that care workers and nurses know the correct method of administering buccal midazolam to those experiencing seizures, as incorrect administration can cause it not to be absorbed effectively leading to ineffective or delayed seizure treatment. Individuals with expectations to know about wrap training and other details can feel free to visit here.
As it can be challenging to teach how to administer buccal midazolam successfully without human volunteers, this handheld airway trainer makes training simple and straightforward. With its adjustable jaw, teeth, and tongue features, this device serves as an effective demonstration for how to administer drug therapy into cheek during seizure attacks or other emergency situations.
Paediatric first aid online
Paediatric first aid online training is essential for anyone working with children or infants, including nurses, nannies, au pairs, teachers and parents. This course can save lives when injuries such as choking or cardiac arrest occur and will benefit any profession working directly with children - such as teachers. This course may also benefit their own parents!
This online care mandatory training course covers first aid and CPR for infants and children, as well as using an adrenaline auto-injector in case of an allergic reaction. This course is perfect for teachers, childcare providers, camp counselors, school bus drivers and foster parents. Certification lasts for two years and fulfills OSHA regulations.
CPR AED for the child & infant
CPR and AED training is essential for all care workers, particularly when caring for infants who are more prone to sudden cardiac arrest (SCA). According to the pediatric Chain of Survival guidelines, high-quality CPR should begin immediately rather than waiting until either there is a pulse found or breathing resumes.
Before commencing CPR, ensure the area is free of obstructions and dry. Remove any bulky clothing, place the infant on their back, tap their back several times while speaking loudly to see if they respond; if not, call 911/EMS immediately for assistance.
The Heart saver Pediatric First Aid CPR AED course equips participants to recognize and care for illnesses or injuries in children and infants until professional assistance arrives. Based on current resuscitation science and guidance from the American Heart Association, this course also features hands-on skills sessions as well as teaching how to use an AED.
vimeo
Adult & paediatric first aid
Care workers must complete mandatory training. This may include courses to teach them how to care for elderly individuals as well as how to treat children and infants properly.
These courses cover topics such as first aid, basic life support and infection control for carers. Furthermore, these training programs aim to teach them about providing dignity-in-care while honoring the privacy of those they are caring for.
Paediatric first aid courses are often required for individuals working in industries related to children in the UK, such as nursery staff, child-minders and teachers. Paediatric first aid differs from standard first aid in that its focus lies on treating injuries and illnesses that affect infants and children - such as febrile convulsions, head injuries or choking incidents in young children.
1 note
·
View note
Text
Covid-19: nurses concerned amid summer upsurge - Published Aug 16, 2024
Most nurses are worried about the ongoing impact of Covid-19 on health and care services in the UK amid an apparent summer wave of cases, a Nursing Times poll has found.
In a snap survey of almost 550 nursing professionals, 85% said they had noticed a rise in cases in their workplaces over the last few months.
Six in 10 (61%) said they were worried about how Covid-19 was currently impacting health and social care services.
A bigger proportion – 77% – said they were concerned about how Covid-19 will affect services this coming winter, when pressures generally tend to be higher.
One primary care nurse in England said: “It’s rising and I worry if we don’t become preventative now it could affect our ability to provide a service.”
The survey findings come as the World Health Organization (WHO) warned earlier this month that Covid-19 was “still very much with us” and that cases had been rising globally.
It said new waves of infection had been registered in Europe, as well as the Americas and the Western Pacific.
Available statistics in the UK also point to a potential upward trend in Covid-19 cases over May, June and July.
However, with testing and data collection being much more limited than they were earlier in the pandemic, Nursing Times wanted to ask nursing professionals for their direct experiences.
The survey responses suggested a big variance between organisations in terms of approaches to Covid-19 prevention.
Of the nursing staff who took part in our poll, 61% said there were no longer any specific Covid-19 prevention measures in their workplaces.
For those who did still have some precautions, these varied from testing all patients for Covid-19 before a hospital admission and then weekly, to only testing patients if they have symptoms.
In terms of personal protective equipment (PPE), some said they wore masks for all face-to-face patient contact, others said PPE was only used when dealing with confirmed Covid-19 cases or if they had the virus themselves.
One NHS hospital nurse in Scotland said: “No masks unless you are coming to work with Covid. No precautions if you have no symptoms. It’s quite shocking.”
However, nurses were divided on whether there should be a return of more Covid-19 precautions, although more than half were in favour.
In total, 58% said they would welcome more Covid-19 prevention measures in their workplaces, 19% said they would not welcome them and 22% were unsure.
One hospital nurse from Scotland felt standard infection control procedures, which were in place before Covid-19, were sufficient.
They said: “There is more than enough. Wards get closed if one person has it and they’re not really ill so it feels like overreacting, it causes more disruption.
“Infection control procedures are enough in most cases.”
Finish reading the report at either link!
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#wear a respirator#public health
9 notes
·
View notes
Text
Learn About Yorkie Poo Dog Breeds and Interesting Facts
There is a cute mix breed called the Yorkie Poo that comes from the Yorkshire Terrier and the Poodle. The Yorkie Poo comes from crossing two smart and well-liked dog breeds. It has become a popular pet in many homes and hearts. Their small size and lively personality make them a hit with families, single people, and older people. Even though they are small, they have a lot of personality and charm.

List of things about Yorkie Poo
Looks: Small and tight, with curly or wavy hair.
Smart, playful, and affectionate are some of its traits.
Popularity: Rising quickly because people like it.
The person is friendly, outgoing, and sociable.
10 to 15 years of life.
The color of the coat can be black, white, tan, or gray.
Is the Yorkie Poo dog a mix of different dog breeds or a new breed? The Yorkie Poo is a mix of different dog breeds.
How to keep a Yorkie Poo healthy
Food:
Protein-rich kibble is important for their energy and muscle growth.
Fatty acids, such as Omega-3, help keep their skin and coat healthy.
Calcium: They need it to build strong bones, especially puppies.
The environment:
Safe places: They like to explore, so a safe yard or area is very important.
Comfortable bedding: So they can relax and stay warm.
Interactive toys: To satisfy their need to play and learn.
Take care of them by giving them lots of play and mental stimulation on a regular basis. They love attention and affection.
Brush their fur three times a week to keep it from getting tangled. If you need to, take a bath once a month. They should always wash their face, especially the area around their eyes. Twice a week, check and cut your nails.
How to get ready for life with a Yorkie Poo
Make sure you're ready to commit for a long time.
Yorkie Poos need to be cared for and watched all the time.
Early on, make training and socialization a top priority.
Equipment you need:
Harness and leash that can be adjusted. Good dog bed. Interactive toys.
A lot of diseases:
Patellar luxation: Getting regular check-ups with your vet can help find this problem early.
Dental disease: Getting your teeth cleaned regularly and chewing on good toys can help.
If they have an ear infection, make sure their ears are dry and clean.
Vaccinations: Your Yorkie Poo needs to be vaccinated against rabies, distemper, and hepatitis.
How to get a Yorkie Poo or adopt one
Locations: It's most popular in cities in the US, UK, and Canada.
Prices range from $800 to $1500 on average, depending on the family tree.
Community: There are a lot of Facebook and Instagram groups for people who love Yorkies.
Checklist for adoption:
Health in general: Always check the health in general.
Vaccination status: Make sure they have all of their shots up to date.
Medical history: Make a list of all the health problems you've had in the past.
Knowing the Yorkie Poo's unique traits and needs will help you have a happy and loving relationship with this cute dog breed. Whether you adopt or buy, this little bundle of joy brings is truly unimaginable.
2 notes
·
View notes