#extrapyramidal
Explore tagged Tumblr posts
Text
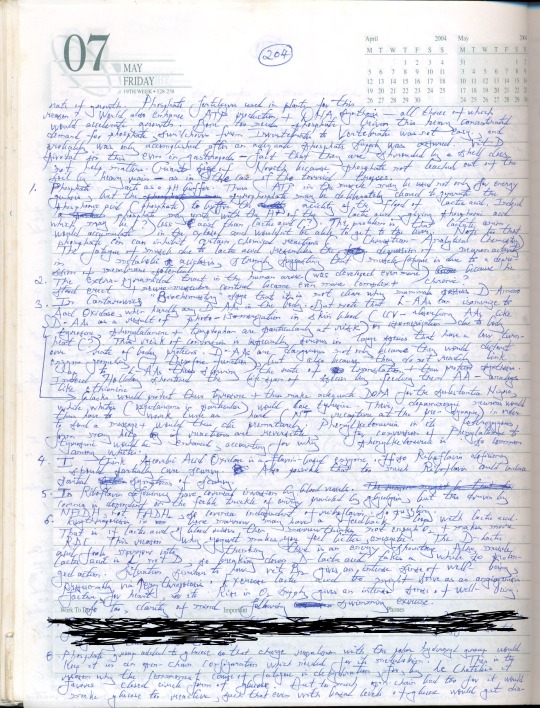
The Science Research Diaries of S. Sunkavally. Page 204.
#phosphate fertilizer#gigantism#gastropods#phosphate#pH buffer#lactic acid#extrapyramidal tract#D-amino acid#D-amino acid oxidase#riboflavin deficiency#ascorbic acid oxidase#NADH#vitamin B12#D-lactic acid#satyendra#theoretical biology#mnauscript#curisve handwriting
0 notes
Text
Understanding Mechanism of Action of Antipsychotic Drugs Medication
Antipsychotic medications work by balancing certain chemicals in the brain called neurotransmitters. The two main neurotransmitters involved in schizophrenia and other psychotic disorders are dopamine and serotonin. All antipsychotic medications act primarily by blocking dopamine receptors in the brain. Specifically, they block dopamine receptors in the mesolimbic pathway, which is the brain system that regulates reward, motivation, and pleasure. By blocking these dopamine receptors, antipsychotics reduce dopamine signaling and the positive symptoms of psychosis, such as hallucinations and delusions. Some antipsychotics may also block serotonin receptors. This helps reduce negative symptoms like social withdrawal and lack of emotion/motivation. The exact mechanism is still being researched, but balancing dopamine and serotonin levels in the brain seems to improve psychotic symptoms. Antipsychotic drugs do not cure schizophrenia or other psychotic disorders but can effectively treat symptoms when taken as prescribed long-term. First-Generation vs Second-Generation Antipsychotic medications are generally classified as either first-generation (typical) or second-generation (atypical). First-generation antipsychotics were the first to be discovered in the 1950s. They are very effective at treating positive symptoms but often cause serious neurological side effects like tremors and muscle rigidity due to their strong dopamine receptor blockade. Second-generation Antipsychotic Drugs were developed in the 1990s to have similar effectiveness against psychosis with reduced neurological side effects. They tend to block serotonin receptors in addition to dopamine receptors. Common second-generation antipsychotics include risperidone, olanzapine, quetiapine, aripiprazole, ziprasidone, and lurasidone. However, second-generation antipsychotics are also associated with metabolic side effects like weight gain, diabetes, and high cholesterol that first-generation antipsychotics rarely cause. Overall, treatment decisions are made on a case-by-case basis depending on individual risk factors, symptoms, and tolerance of side effects. Common Medications Some of the most frequently prescribed antipsychotic drugs include: - Haloperidol (Haldol): A typical first-generation antipsychotic. Very effective for acute psychosis but causes more neurological side effects. - Risperidone (Risperdal): A second-generation antipsychotic used as a first-line treatment. Effective against both positive and negative symptoms with a lower risk of neurological side effects. However, weight gain is common. - Olanzapine (Zyprexa): A second-generation antipsychotic also used as initial treatment. Similar efficacy and side effect profile to risperidone but may cause even more weight gain. - Quetiapine (Seroquel): A second-generation antipsychotic used for both schizophrenia and bipolar disorder. Associated with sedation, dizziness, and increased appetite and weight. - Aripiprazole (Abilify): A second-generation antipsychotic with a unique mechanism of action as a partial dopamine receptor agonist. Associated with less weight gain and metabolic issues compared to other second-generation drugs. - Clozapine (Clozaril): A second-generation antipsychotic reserved for treatment-resistant schizophrenia due to risk of agranulocytosis (low white blood cell count). Very effective but requires regular blood monitoring. Associated with substantial weight gain and other metabolic effects.
Get more insights on Antipsychotic Drugs
Discover the Report for More Insights, Tailored to Your Language
French
German
Italian
Russian
Japanese
Chinese
Korean
Portuguese
Alice Mutum is a seasoned senior content editor at Coherent Market Insights, leveraging extensive expertise gained from her previous role as a content writer. With seven years in content development, Alice masterfully employs SEO best practices and cutting-edge digital marketing strategies to craft high-ranking, impactful content. As an editor, she meticulously ensures flawless grammar and punctuation, precise data accuracy, and perfect alignment with audience needs in every research report. Alice's dedication to excellence and her strategic approach to content make her an invaluable asset in the world of market insights.
(LinkedIn: www.linkedin.com/in/alice-mutum-3b247b137 )

#Antipsychotic Drugs#Schizophrenia#Bipolar Disorder#Psychotic Disorders#Hallucinations#Extrapyramidal Symptoms#Microcontrollers#Sensors#Displays#Connectivity Ics#Power Management Ics
1 note
·
View note
Text
have you tried meditation
if that doesnt work try risperidone
so tired of listening to myself think all the time. just shut the fuck up for a second
#many thoughts head full?#just antagonize the d2 receptors#this post is a joke#please dont take antipsychotics without being evaluated by a psychiatric professional#taking them without a clinical condition that warrants them can lead to parkinsonian extrapyramidal side effects#why am i like this
8K notes
·
View notes
Text
“You may now become who you thought was disposable”: COVID-19 Politics and Ableism - Published July 4, 2024
Unpaywalled link available in the link to our archive! A taste below!
“You may now become who you thought was disposable”: COVID-19 Politics and Ableism Andrea Kitta Journal of American Folklore, Volume 137, Number 545, Summer 2024, pp. 321-330 (Article) Published by American Folklore Society For additional information about this article muse.jhu.edu/article/931461[37.228.238.33] Project MUSE (2024-07-09 12:59 GMT) American Folklore Society
This essay critically examines the intersection of COVID-19, Long COVID, ableism, and health care disparities in the United States, emphasizing the transformative impact of COVID-19 as a mass disabling event with a disproportionate impact on marginalized communities. I also bring an autoethnographic lens to my experi- ence of COVID-19 and Long COVID, underscoring the importance of recognizing the diverse and often untellable experiences of individuals with disabilities and challenging the prevailing ableist perspectives embedded in society. I raise ethical considerations of storytelling in the context of Long COVID and urge researchers to embrace empathy and a more inclusive approach that challenges traditional notions of objectivity and distancing within academic research. I call for a collaborative approach between disability studies and folklore studies, encouraging scholars to interrogate and explore the traditions shaped by experiences of disability.
On December 13, 2020, disability advocate Imani Barbarin created a TikTok where she stated in the caption: “COVID is a mass disabling event. Things will never be the same. Never. You may now become who you thought was disposable” (Barbarin 2020). Barbarin was not overstating what is happening in the United States. In addition to the overwhelming number of US-based COVID-19 deaths (1.07 million as of November 1, 2022, according to the New York Times COVID-19 Tracker [New York Times 2023]), there is also an alarming number of cases of post-acute sequelae SARS-CoV-2 infection (PASC) or, as it’s more commonly known, Long COVID. Long COVID happens in anywhere from 5 percent to 50 percent of COVID-19 infections (although most medical experts agree the rate of Long COVID is somewhere around 20–30 percent of all infections). Long COVID affects women at a 22 percent higher rate than men (Sylvester et al. 2022:1391), and one study of Long COVID listed over 200 symptoms (Davis et al. 2021). The most common symptoms are fatigue, shortness of breath, cough, chest pain, brain fog, sleep disturbances, depression, joint pain, and dysautonomia (a dysfunction of the autonomic nervous system that typically presents as the inability to control temperature, breathing issues, and other things the body normally controls automatically).
Current estimates of those affected by Long COVID in the United States are between twenty and forty million. COVID-19 has also been shown to reactivate other viruses (Gold et al. 2021; Chen et al. 2022; Su et al. 2022), and one current theory is that Long COVID is the result of the COVID-19 virus continually being reactivated in the body (Klein et al. 2022). The latest research out of Yale University shows that COVID-19 cases entail cellular changes to the B and T cells, lower levels of cortisol, and that the virus can reactivate other viruses (Su et al. 2022:891–2). A recent study with more than 154,068 participants showed that “in the post-acute phase of COVID-19, there was increased risk of an array of incident neurologic sequelae including ischemic and hemorrhagic stroke, cognition and memory disorders, peripheral nervous system disorders, episodic disorders (for example, migraine and seizures), extrapyramidal and movement disorders, men tal health disorders, musculoskeletal disorders, sensory disorders, Guillain–Barré syndrome, and encephalitis or encephalopathy” (Xu, Xie, and Al-Aly 2022:2406).
Both COVID-19 and Long COVID exposed inequities in the US health care system, with Black, Indigenous, and people of color (BIPOC) populations dying from COVID-19 at much higher rates than White people at the beginning of the pandemic. Compared to White people, Alaskan Indian or Alaskan Natives died at 2.1 times the rate, Black people at 1.7 times the rate, Hispanic or Latinx people at 1.8 the rate, and Asian Americans at 0.8 times the rate (CDC 2023). According to the Washington Post’s analysis of CDC’s statistics, the rate of White people dying from COVID-19 became equal to the rate of other groups beginning in October 2021, then (except for the Omicron wave) increased, primarily due to White people being unvaccinated. Strangely enough, the equalizing trend wasn’t because death rates dropped for BIPOC people, but rather was due to the rise of the White death rate. Tasleem Padamsee, Assistant Professor at The Ohio State University who researched vaccine use and who is a member of the Ohio Department of Health’s work group on health equity, stated: “Usually, when we say a health disparity is disappearing, what we mean is that . . . the worse-off group is getting better. . . . We don’t usually mean that the group that had a systematic advantage got worse” (quoted in Johnson and Keating 2022).
Additionally, at the time of this writing in Spring 2023, the pandemic has been declared as “over” despite the fact that around 400 people are still dying per day in the United States and that those dying tend to be people with disabilities and the elderly (New York Times 2023). It’s difficult to imagine a situation where 400 deaths a day are deemed acceptable, yet here we are. Many people are desperate to “get back to normal” and seem to care more about going maskless or dining indoors than they do about those who are dying of COVID-19. Those who are unvaccinated and unmasked also seem to not understand (or not care) that the longer they continue on that path, the longer the pandemic will take to dissipate. Simply put, the majority of people do not seem to care about people with disabilities, including those who are immunocompromised, and their increased health risks due to the pandemic.
People with disabilities are an unrecognized health disparity population, and they died at much higher rates during COVID-19 (Krahn, Walker, and Correa-de-Araujo 2015). The National Council on Disability found that 181,000 people with disabilities in long-term care facilities died from COVID-19 in the first year of the pandemic, making up one-third of COVID-19 deaths at that time (National Council of Disabilities 2021). The report is worth quoting at length.
In addition to disproportionate fatalities, key findings of the report include:
People with disabilities faced a high risk of being triaged out of COVID-19 treatment when hospital beds, supplies, and personnel were scarce; were denied the use of their personal ventilator devices after admission to a hospital; and at times, were denied the assistance of critical support persons during hospital stays. Informal and formal Crisis Standards of Care (CSC), pronouncements that guided the provision of scarce health care resources in surge situations, targeted people with certain disabilities for denial of care (National Council of Disabilities 2021).
Students with disabilities were denied necessary educational services and supports during the pandemic and have experienced disruption and regression in their behavioral and educational goals (National Council of Disabilities 2021).
The growing shortage of direct care workers in existence prior to the pandemic became worse during the pandemic. Many such workers, who are women of color earning less than a living wage and lacking health benefits, left their positions for fear of contracting and spreading the virus, leaving people with disabilities and their caregivers without aid and some at risk of losing their independence or being institutionalized (National Council of Disabilities 2021).
Deaf, Hard of Hearing, Deaf-Blind, and Blind persons faced a profound communication gulf as masks became commonplace, making lip-reading impossible and sign language harder (National Council of Disabilities 2021).
#disability justice#disability politics#covid pandemic#covidー19#mask up#covid#pandemic#covid 19#coronavirus#wear a mask#sars cov 2#still coviding#public health#wear a respirator#ableism#covid eugenics
144 notes
·
View notes
Text
My folks and I have been reading some of the literature on COVID/Bipolar I and they seem to suspect — and I’m inclined to agree with them — that what I thought was “long COVID” after my second bout with the virus may have in fact been my first recognizable depressive episode. Most of my symptoms overlapped with the depressive phase of Bipolar I, so disentangling the two is probably impossible in retrospect, but for many many months I was behaving in ways that are completely uncharacteristic of my personality: I was exhausted, unmotivated, and even more inattentive than my ADHD makes me ordinarily; I was uninterested in things that give me great pleasure, like going to shows and creative writing; I had brain fog so bad it was an uphill battle doing things that otherwise come quite easily to me, like communicating verbally and expressing myself with clarity and precision. Gradually these symptoms subsided, and I became even more productive and social than usual, which may very well have been a protracted hypomanic phase. I caught COVID again earlier this year, and by the start of July I was spiraling into full blown mania, prone to intense emotional states like expansive rapturous joy and crying jags at the drop of a hat. Music, theater, and reading fiction felt almost unbearably moving and profound. I was writing like crazy, and pretty soon afterward I was acting crazy, too, with racing thoughts and speech, disturbed sleep, and thoughts/ideas that were growing progressively more disordered and paranoid.
I prefer the term “manic depression,” though some consider it antiquated/offensive, because to me it most accurately describes my experience. But by my 36th birthday my new shrink had diagnosed me with full blown Bipolar I. I’m much better now with several weeks of a mood stabilizer under my belt, and this past weekend we went with the “nuclear option,” I.E. a four-day course of high dose antipsychotics. I was miserable from the extrapyramidal side effects, and had to take Xanax throughout in order to tolerate the akathisia and restless leg syndrome. But thank god, it snapped me right out of it, and knock on wood I’m back to my old self — with a little luck, I’ll have another 15 years symptom-free, or with just low grade hypomanic/depressive states that are so mild as to feel like ordinary, subclinical mood swings.
What I’m struggling with is the feeling that I’ve been handed a label sticker that amounts to crippling disability at best, and an early death sentence at worst. I will probably always have to keep these incredibly powerful drugs with their rotten side effect profile on hand, and may one day need to take them consistently, if I wind up having future severe episodes. To have to choose between Shitty and Shittier over a dangerous brain disease feels like I’ve been dealt the world’s worst genetic hand, and that bums me out a lot. I know it’s not my fault, but seeing the agony I’ve put my parents through is the worst part. Figuring out how to manage this is going to be a lifelong struggle against my own lousy biology, and that sucks. I’m trying to stay optimistic. It’s been really, really hard.
62 notes
·
View notes
Text
This fandom is literally the only good thing that happened this year, but it gave me so much that I would say this was one of the best worst years of my life.
I made my first genuine friends in years, contributed to a fandom for the first time (my Learn Finnish with Käärijä video has 45,2k likes, wtf….), traveled to Berlin, went to gigs and talked to strangers, all because of this fandom.
cw mental health struggles
I survived the constant episodes of hypochondria and intense fear of death, scary extrapyramidal side effects from meds, intrusive thoughts and all the shit that life threw at me. I can’t stress it enough the kind of hell on earth this year was. I have been and will always be mentally ill, I know what it’s like but the things that were happening in my mind and body this year were literal torture.
I think… being here made me feel like a person when I felt like all there is to me are problems. These goofballs, Kä and his crew and Joker Out boys, brought me so much joy. And you guys brought me so much joy.
Thank you for being good to me. Thank you for being a safe place.
#käärijä#joker out#personal#idk if anyone has energy to read another sappy post anymore but I just had to write something
65 notes
·
View notes
Text
New Antipsychotic FDA Approval – Cobenfy
Cobenfy (xanomeline/trospium chloride) has just been approved for schizophrenia treatment in the US. This is huge. It's the first antipsychotic in decades to not target dopamine directly. It's got a much, much better side-effect profile, and it might work for negative and cognitive symptoms.
FOR MORE READING – news report/patient-centred plain language overview: See here.
FOR MORE READING – scientific evidence report: See here (note: the drug is referred to as 'KarXT' in this report).
I couldn't be happier right now. People with psychosis go through so, so much trying to find medications that are both useful and tolerable, and psychiatry has historically neglected psychotic people's needs so, so awfully. (Not to mention how little there is that actually helps with anything other than positive symptoms.) So I'm really, really hoping that with the proof that we can, in fact, make antipsychotics that aren't based on the same old pharmacological things we've tried before. Cobenfy is a muscarinic agonist/antagonist in fixed combination – and it also indirectly regulates dopamine and glutamate. And given that we know both dopamine and NMDA are probably involved in schizophrenia somehow – AND that treating things to do with either is hard – this is so, so, so exciting.
This isn't to say Cobenfy doesn't have side-effects (the most common ones being nausea, constipation, dyspepsia, vomiting, hypertension, dry mouth, and tachycardia. We also know that there is a small risk of extrapyramidal symptoms, and that prolactin-related side-effects do happen, unfortunately). We don't know much about how it affects folks in the long-term, or much about the long-term tardive dyskinesia risk. But even so, it's progress compared to some of the worse antipsychotic side-effects.
Moreover, there is a possibility it might be useful for negative and cognitive symptoms. Holy crap.
I'm really really really excited. I hope this is the start of a shift in psychiatry towards better standards of patient-centred care for psychosis. Y'all have deserved better for far too long – here's hoping this is the start of more ethical, effective treatment.
#antipsychotics#neuroleptics#psychiatry#psychiatric medicine#cobenfy#antipsychotic special interest#antipsychotic drugs#schizophrenia#psychosis#(note: i don't experience psychosis myself. but i do wanna see standards of care for psychosis improve.)#(y'all shouldn't have had to be mistreated so long. i'm really hoping this can be the start of a shift towards more humane treatment)#xanomeline#xanomeline/trospium chloride#important#schizophrenia spectrum#psychotic disorders#KarXT#neurodivergence
8 notes
·
View notes
Text
i am actually going to whine about this publicly
my recent Poisoning Adventure was bc my psych NP (baseline can't be trusted) overdosed me on a new med I never shouldve been on and it caused pretty severe acute extrapyramidal effects (hella muscle spasms, uncontrollable jerking/movements, felt like i was in a fuckin dbz gravity chamber) and METABOLIC ENCEPHALOPATHY!! i couldnt control my body and even tho i knew who i was when it was where i was and why i was there i was also on a completely different realm of existence and it was like, Terrifying Actually!! so even tho im off that med and antidoted and not at risk anymore every time i have any kind of nerve tingling anywhere i start Freaking The Fuck Out. this shit was FOR REAL worse and more harrowing than literally any part of having cancer including the parts where i almost died. was more frightening than having meningitis bc at least i wasnt totally fuckin zooted outta my mind!! ur bitch needs Therapy. wowie!!
anyway ive been struggling w orthostatic hypotension for a hot minute (largely dehydration imo) so i got that rush u get when ur bp tanks and just started cryin like a little bitch babby on account of the Fears. Despite being super tired I am afraid to sleep bc the first bout of extrapyramidal symptoms woke my ass from DEAD SLUMBER
I used to love NPs but nowadays NP schools are clownhouse jokester diploma mills and due to scope creep ushered forth by the capitalist disneyfication of healthcare theyre allowed to practice WAY THE FUCK completely outta bounds. it isnt safe!! chikadee was makin nonstop bonkers med choices for me including putting me on the vers of a medication not even meant to to treat what we were trying to treat and also the correct version had limited success in.. the pediatric population?? babe what?? had to get my pcp involved on that one.
i had issues w nps before on account of all the probs w education and safety (theyre not even required to have 5 minutes of bedside experience outside of clinicals which ultimately are glorified techwork and useless in terms of Actual Nursing Practice (i do think having clinical experience IS Essential and beneficial tho)) but this trash ass dumbshit idiot gave me FRESH TRAUMAS i did NOT need so i have gone from a nonenthusiast to a full on hater. listen we did not go to med school we went to nursing school we should stay in our fucking lane. christ alive!!!!!
i cant fuckin believe this single experience was more traumatizing than actual months of chemotherapy
ALSO I GOT DENIED MEDICAL LEAVE?? WHAT THE FUCK IS UP WITH THAT!!!!!!
#kels talks#miserable medical stuff BEWARE#wah i had a scawy expewience#oh i am also afraid of taking my regular meds now so started taking reduced doses without dr guidance which i know is bad u_u#i see an Actual Doctor in <2wks itll be fine but taking a pill shouldnt give me this much anxiety tch
17 notes
·
View notes
Text
Psychiatry literally be like:
— This will help you with hallucinations.
— What are possible side effects?
— Parkinsonism and extrapyramidal disorders.
— Ok.
— This will help you with parkinsonism and extrapyramidal disorders.
— What are possible side effects?
— ... Hallucinations.
— ... Ok, anyway, I don't have a choice.
[I'm not joking. It's my real story.]
2 notes
·
View notes
Text
for about a year i had a ptsd response to pizza & couldn't eat pizza bc after my overdose i went to the hospital and i said pleeease help me im so hungry but i think i overdosed on my meds because am dizzy asfuck & can't stop frowing up and the doctor was like you're probably just a hysterical woman why don't you take this nausea medicine and try chilling a little? so when i got home i was like hell yeah im medicated its feast time so i ordered pizza and well. you know
& this is funny because last week i was having the worst food poisoning in the history of food poisoning possibly ever and went to the hospital again (mistake) and they gave me an IV that apparently makes 5% of people feel the worst they felt in their lives and as soon as that shit hit my brain i felt the worst i felt in my life and i told the nurse something was very wrong and begged her to help me and she was like ummm you have wrist scars 🤨 you're probably just anxious go home. so i did and i spent the next 24 hours breathing manually & choking on all solids & without one minute of sleep. and when i looked up "(medicine name) restlessness" i found out that yeah 5% of patients get this way and there's an antidote for this reaction (called an extrapyramidal reaction) that works like magic within minutes that the nurse could have easily given me if she hadn't dismissed me as hysterical
anyways i just ate pizza and felt fine about it for the first time in a year so win 👍 but i wish i could have eaten a doctor alive instead❗️
2 notes
·
View notes
Text
I do think that, when we hopefully eventually ban harmful psychiatric drugs, people who are already taking them should be able to choose to be grandfathered in to still be able to take them. Like how people want to progressively raise the smoking age, except linked to specific patient histories.
Idk, you know, maybe at some point we will get rid of all the antipsychotics that are more dangerous than they are helpful! That would be great! But the people who have been on them for years and cope with the side effects and feel their life has been given back to them, well, they can have them still I think. Even if they have horrible extrapyramidal stuff. They can make their own choice -- if they choose to stop ofc they should be aided in titrating off and/or switching to a safer alternative. And, even if they choose to stay on the drug, they should still be entitled to any reparations offered for people who were prescribed the dangerous drug. Its possible to acknowledge you were harmed and treated irresponsibly, but also that you'd make the same choice now and that's okay. And we should also be giving psychotic people money anyway obviously
On a different area of psychiatric drugs completely: Venlafaxine. It could maybe be banned one day for causing people to enter the hell dimension if they attempt to stop taking it, but god damn can you pry it from my cold dead hands
3 notes
·
View notes
Text
okay fuck it if i dont know biology i dont know biology i know what an extrapyramidal system is i bet most random adults on the street do not know that its enough for me.
#wizardspeak#also my biology teacher is so awesome she explains things in a way that i manage to actually remember ill miss her soooo much#will NOT miss the student teachers though
5 notes
·
View notes
Text
Psychopharmacology The British Association of Psychopharmacology (BAP)(n.d.) is a scholarly society and enlisted philanthropy. It advances exploration and instruction in psychopharmacology and related zones, and unites individuals in the educated community, well-being administrations, and industry. Shaped in 1974, it is the biggest such national relationship in Europe, and the second biggest in the world. The website has a lot of different content available that would help me in my coursework. Several articles can be seen in the homepage, which have been published by renowned authors. Videos are also available that would help me in understanding difficult concepts of psychopharmacology. The association has its own journal and publications which are available completely if one becomes a member of the British association. The homepage also presents several tweets by BAP that creates a good impact on the visitor. BAP provides several activities to the members of the website and also includes detailed information for the public so that it's not just the members who benefit from the site, but also the general public. Furthermore, the site provides links and information about new books that can help students and researchers alike. The website also provides information of events and conferences related to psychopharmacology, which gives opportunities to the students to learn and interact more and excel in different topics of pharmacology. Moreover, there are different training and education programs, including Masterclasses that provide training to nurses, pharmacists etc. The website provides a lot of opportunities for the trainees and students thus it has a lot of positive points. Every part of information is given in detail to not only help the people related to psychopharmacology, but also the general public. The vast numbers of articles represent the importance of BAP among the profession. BAP integrates well into the coursework and would not only help in providing ample information, but also opportunities for the emerging pharmacologists. Part II Factors in Treating Depression in the Elderly The video tells that there are several factors that need to be considered in elderly depression. Different medicinal side effects occur because an elderly's brain is damaged, resulting in memory problems, broken bones etc. Extrapyramidal side effects cause gait problems, tremors, muscle spasms, and inner restlessness. Drug issues present that create side effects include: Paxil and Prozac. The presenter provides detailed information about the side effects of elder people suffering from dementia; so it is very relevant and helpful to the coursework; however, I would like to learn more about substitute medicines if the given one has severe side effects (Nickel, 2010). Limits of Pharmacological Treatment The video starts with drug development that mentions RU 4 ME drug that improves judgment of single women about to have sex with eligible seeming men, and Perceptia, which induces euphoric acceptance of hair loss, weight gain, impotence and other natural symptoms of aging; side effects may include verbal seepage. Apart from that, the presenter does not clear anything about the limitations of pharmacological treatment that could be of any use in the coursework. Nickel (2010) talks about psychologists who prescribe medications that will be seen in the future and I would like to learn more about why the psychologists who are not allowed to prescribe medicines in their profession would do so in the future. Specifics in Treating Depression The video talks about antidepressants, including Anergic Depressions in which a combination of Remeron and Ritalin is taken by the patients. Remeron is also used as a sleeping pill for insomnia and helps people go to sleep, but also causes hypertension when the person wakes up. Weight loss is common in the elderly, so Remeron helps them to have the urge of eating and gain weight. Agitated Depressions is another form of depression that can also be treated with Remeron and SSRIs. Psychotic depression is very common and the patient should use AD and anti-psychotics for treatment. Nickel (2010) also gave an example of a personal experience which cleared up a lot of queries regarding psychotic depressions. In this topic, I would also like to learn more about the substitute medicines that can be given if the ones being taken have severe side effects like increased hypertension. Polypharmacy Cascade The video starts with a case study that includes a 78-year-old woman recovering from a hip fracture. She has cognitive impairment, mild high blood pressure and urinary incontinence; her medicinal routine included Ativan 0.5 mg, and Lorazepam 0.5 mg, both of which are the same medicines with different names. The presenter explaining the case gives a clear explanation of how wrong medicinal treatment can cause the pain to get worse instead of being healed (Nickel, 2010). I would like to learn further about how the situation could be avoided in the first hand and the role the psychopharmacology association plays in this regard. Part III Borderline Personality Disorder The distinctive subtypes of borderline personality disorder incorporate schizophrenia, rejection sensitivity, anger, impulsiveness and instability. Nickel (2010) clarifies that the schizophrenic dislikes being within the sight of a specialist, we see a less number of individuals amid the profession looking for treatment. Each subtype is clarified in point of interest alongside cerebrum exercises and treatment impacts of each subtype. The presenter clearly defined the mentioned subtypes, but I would like to learn a detailed description of the treatment of each of them. ADHD The video begins with the chronicled diagnosis of ADHD, which began in 1902 and included imperfections, indications and the finding required for ADHD. The address likewise clears that ADHD is hereditary and can be passed on to children. The pervasiveness rate of ADHD in youngsters is 5 to 7% while in grown-ups it is 4%; among which 20% is gained while 8% is hereditary. The presenter gave an authentic and factual part of the video, which is vital to learn so as to know more about ADHD and I might want to take in more about the Acquired portion of ADHD as it would make me all the clearer about how youngsters can secure ADHD (Nickel, 2010). Depression and Dementia Depression has a great deal of danger variables as it profoundly influences the mind, driving towards dementia. There is an enormous measure of cover amongst dementia and discouragement alongside Parkinson's disease, and Alzheimer's. Depression in later stages can prompt forceful conduct, loss of weight, and physical hallucinations. The illness spreads moderately and takes up to 12 to 14 years until the individual kicks the bucket. The individual influence loses the capacity to nurture himself or herself, and they totally depend on other individuals for each and every thing. The presenter gave a nitty gritty clarification of depression and dementia and would be extremely helpful for the aversion of the turmoil (Nickel, 2010). I would like to know more about how the situation can be recognized at the start so it can be controlled before spreading further. Autism Spectrum Disorders Oxytocin is essential for kids amid work and improves social learning in them. Nickel (2010) presents and contemplates a discussion about Asperger's, and the general population influenced with it is exceptionally clever and can see tones in more passionate ways (Nickel, 2010). I might want to take in more about Nasal infusion, as the study sounded exceptionally intriguing and something that could be examined on additional. Bibliography British Association of Psychopharmacology. (n.d.). Retrieved from Nickel, T. (2010). Factors in Treating Depression in the Elderly.Youtube.com. Retrieved from: https://www.youtube.com/watch?v=_dQfbdLgztQ&index=22&list=PL58291C0D6F73D49D Nickel, T. (2010). Specifics in Treating Depression.Youtube.com. Retrieved from: https://www.youtube.com/watch?v=vPDWjE2iLnQ&index=20&list=PL58291C0D6F73D49D Nickel, T. (2010). Limits of Pharmacology Treatment.Youtube.com. Retrieved from: https://www.youtube.com/watch?v=4rAB54LVywI&index=21&list=PL58291C0D6F73D49D Nickel, T. (2010). Polypharmacy Cascade. Youtube.com. Retrieved from:https://www.youtube.com/watch?v=vncxdR729zc&index=19&list=PL58291C0D6F73D49D Nickel, T. (2010). Depression and Dementia.Youtube.com. Retrieved from: https://www.youtube.com/watch?v=NczlDr8PjM&index=18&list=PL58291C0D6F73D49D Nickel, T. (2010). ADHD.Youtube.com. Retrieved from: https://www.youtube.com/watch?v=6HbercPYv7w&list=PL58291C0D6F73D49D&index=3 Nickel, T. (2010). Autism Spectrum Disorders.Youtube.com. Retrieved from:https://www.youtube.com/watch?v=XI9wloxiGUE&list=PL58291C0D6F73D49D&index=9 Nickel, T. (2010). Borderline Personality Disorder.Youtube.com. Retrieved from:https://www.youtube.com/watch?v=HPuIPDJAysY&index=13&list=PL58291C0D6F73D49D Read the full article
0 notes
Text
need to add everyone having extrapyramidal side effects from their high dose antipsychotics and the washout of dopamine in their brain
0 notes
Text
Une diminution spectaculaire des taux de glutathion chez des patients vivants atteints de la maladie de Parkinson a été observée 🧠⚡️. Cette étude met en lumière un lien potentiel avec la progression de la maladie 🩺🔬. Ces résultats ouvrent la voie à de nouvelles stratégies thérapeutiques pour mieux comprendre et traiter cette pathologie complexe 💡.
A dramatic decrease in glutathione levels has been observed in living patients with Parkinson's disease 🧠⚡️. This study highlights a potential link to disease progression 🩺🔬. These findings pave the way for new therapeutic strategies to better understand and treat this complex condition 💡.
#Parkinson#Glutathion#maladiesieDeParkinson#Santé#Neurodegeneration#RechercheMédicale#Médecine#Traitement#Innovation#Neurologie#Glutathione#ParkinsonsDisease#Health#MedicalResearch#Medicine#Treatment#Neurology
0 notes
Text
Anti Parkisonian Drugs Short And Long Essay Question And Answers
#Pharmacology#PharmaceuticalIndustry#ClinicalPharmacology#DrugsandResearch#Anti Parkisonian Drugs Short And Long Essay Question And Answers
0 notes