#diagnostic criteria for diabetes
Explore tagged Tumblr posts
Text
Everything You Need to Know About Diabetes Tests - A Journey of Uncertainty and Surprises!
Prepare yourself for a roller-coaster ride through the perplexing world of diabetes tests! Embark on this whirlwind tour of different tests, diabetes types, interpreting results, and managing the enigmatic condition. Gain insights to take control of your health in this exhilarating adventure! Introduction to Diabetes Tests – The Enigmatic Puzzle Unveiled! Diabetes, a mysterious metabolic…

View On WordPress
#benefits of diabetes testing#conclusion#continuous glucose monitoring#diabetes educators#diabetes tests#diagnostic criteria for diabetes#fasting plasma glucose test#frequently asked questions#HbA1c test#insulin level test#interpreting test results#Lifestyle Changes#limitations of diabetes testing#managing diabetes#medication adjustments#oral glucose tolerance test#preparing for diabetes tests#random plasma glucose test#understanding diabetes
0 notes
Text
Major medical groups are proposing a change to how doctors diagnose obesity. In Tuesday's issue of The Lancet Diabetes & Endocrinology, 58 international experts across a range of medical specialties and people with lived experience released a report proposing a new definition and diagnostic criteria for clinical obesity. They say the current medical approaches to diagnose obesity don't reliably assess an individual's health. The international Commission on Clinical Obesity which proposed the new definitions called it a nuanced approach. Their report includes 18 diagnostic criteria for clinical obesity in adults and 13 criteria for children and adolescents.
Continue Reading.
157 notes
·
View notes
Text
So ME/CFS (myalgic encephalomyelitis/Chronic Fatigue Syndrome) and fibromyalgia are two syndromes (collections of symptoms often found together, with unknown causative mechanisms) with largely overlapping symptoms. They're currently classified as different diagnoses, but there are plenty of people who aren't convinced that they're actually different things. The biggest diagnostic difference seems to be whether the pain or the fatigue is the biggest problem.
I'm sure there are plenty of people who, like me, couldn't possibly say which of those is ruining my life more. I, like many, fulfill all the diagnostic criteria for both. I have the specific patterns of pain and inflammation characteristic of fibro, but I also have the postural orthostatic problems (Stand Up Feel Real Bad disorder) and extreme fatigue of ME/CFS. There's no test; diagnosis is an inherently subjective thing.
This is just gonna keep being about medical problems, so have a cut.
I also have problems that may be related or may be separate or may be part of the constellation of physical issues associated with ADHD, like loose tendons that lead to terrible core strength and janky joints. So while generally the pain spots for fibromyalgia are considered to have no actual material cause, I am pretty sure that my right hip and shoulder are in fact fucked up, and fibro is just making it experientially worse. I've also got a rib that spends more than half its time in just slightly the wrong goddamn place. I have multiple friends who have hypermobility problems that make mine look like a papercut, but combining them with fibro isn't a lot of fun.
A few months back, at my bestie's prompting and with his help, I started eating keto, which is essentially just restricting carbohydrates so harshly that they represent less than 20% (or less than 10%, this seems to be bioindividual) of your diet, at which point your body begins building energy transport molecules out of fat (ketones) instead of glucose. This has a history of treating several conditions (originally, seizures, but now also diabetes and inflammatory conditions), well before it became popular for weight loss.
It was an experiment. Believe me, I have mixed feelings about the fact that it worked. At first, it worked really, really well. I went from mostly bedbound to up and working full days outside. I've started to hit diminishing returns and having to nap more often, but it's still a radical improvement. I just forget how bad it was too fast. I hate how fast we forget how far we've come.
I haven't talking about it though, because I am so conflicted about restrictive diets as a thing. This started as an experiment, and as an experiment I could sell myself on no apples no potatoes no rice no crackers no no no no etc for a few weeks. After a few weeks I could decide whether it was worth it. And now here we are and it works.
But I've gone through So Much food restriction, starting when Phantom was two and we discovered that gluten fucks us both up. Then the Boy was sensitive to so many things as a baby that I cut out the entire Top Eight allergens (let's see, can I remember? Milk, eggs, peanuts, gluten, corn, soy, uhh....others...) for a year while he was nursing. Once you've cut wheat AND eggs AND corn out there is almost no commercial product you can eat and you have to prepare everything from scratch. With a toddler and a baby. I was literally starving. I used a calorie tracker for a while and found that I was nearly a thousand calories short per day, on average. I could barely think.
It's become a huge depression trigger for me. I tell people that my last major depressive episode was triggered by not being able to eat dairy, and I'm not kidding. I'm struggling with it now, too. Most of the time I'm good, but still, despite medication, I get very low and I just want to be able to fucking eat something tasty and comforting and EASY. I just want...cheese and crackers. A whole piece of fruit. A baked potato. Rice with my stir fry. But then I eat too much fucking watermelon and I can tell the difference in my wellbeing the next day.
Food becomes a minefield. Every meal becomes a struggle. You question every bite, every symptom. At least once a day the whole thing is just too annoying and I decide to just not eat, because fuck it. I dunno if it reaches eating disorder levels, but it's certainly maladaptive. I hate that I've gotten here because what you eat actually DOES matter. it's like the question of how you talk yourself out of anxiety when the world is objectively falling apart.
But I can do the things I love. I owe all this garden progress to not having had a glass of juice or a bowl of pasta in four months. Not to mention the abrupt cessation of all my dermatitis problems, frequent "silent" heartburn, a ton of digestive problems, migraines, most headaches, and more. "Nothing is worth risking depression" but is it though?
I'm holding on to the hope that these changes will allow me to heal. That I'll be able to make long-term progress, as many people say they have, and reintroduce restricted foods gradually. That I'll be able to cement the opportunity diet gave me with regular movement and conditioning and slowly claw my way up the spiral.
But on days when I feel like shit anyway, and I can't have some fucking chips about it....yeah. It's not great.
23 notes
·
View notes
Note
Hello Haitch! Hope you are doing well.
Last year during summer, I was diagnosed with PCOS (i had gotten it checked because i hadnt had my period in like 3 months) and since i was just 17, the doctor asked me to maintain a proper lifestyle and see till November and said that if it wasnt fixed by then, i had to do a checkup again. But i'd gotten my period by august so i never reached out again.
but this year (im 18 now), the last time id gotten my period was in april so it's been 6 months now. im gonna go to the doctor again later this month. but here's the thing— last year, i went to a gyno abroad because women's healthcare isnt the best in my country. but this year, its not possible for me to go abroad right now so im gonna have to work with a gyno from here.
now i have a feeling that theyll put me on pills and while i agree thats the easy way to fix this, im worried itll mess things up for the long run. the lifestyle the first gyno asked me to follow is a little difficult for me to get into since she'd asked me to exercise plenty and im a full time alevel student and it gets hard for me to maintain a proper routine like that. i also struggle with binge eating which i've heard comes with having pcos (im not sure if this is true tho).
so in one hand, i feel like it's easier to just start taking pills but then again it has so many side effects i don't know what to do right now.
Lots to unpack here.
CW/TW: PCOS, medical discussion, endocrine disorders, diabetes, hypothyroidism, weight management, medication management
Firstly, PCOS is often diagnosed based on vague criteria; lots of doctors flippantly diagnose it based on a volume of loose criteria. If you have an increasing number of these criteria, then yes, the chances are you have PCOS. However, it's often erroneously diagnosed without proper diagnostic procedures such as scans, bloods, and a full review of your longer term health history.
That being said, being on the pill doesn't 'cure' PCOS, it can simply manage the symptom of irregular periods. There's flimsy evidence on the pill's ability to manage/prevent weight gain and the development of other disorders that are associated with PCOS.
While weight loss is often harder for women with PCOS, especially if you have associated conditions such as an under active thyroid, it's not impossible.
Your lifetime chances of developing Diabetes are significantly higher with PCOS, and this chance goes up again if you struggle with increased body weight. PCOS and appetite changes like binge eating have been associated with each other, too.
So you'll only know if managing your weight and eating habits make a difference with your PCOS, when you've actually tried them to the absolute best of your ability. If you are at an increased ideal weight, losing weight can be very effective to manage and reduce the symptoms of PCOS.
Of the many, many thousands of women I've looked after, I'm sorry to say that those with PCOS who are very pro-active with managing their weight, perhaps taking medications as advised by their doctor (the pill and Metformin are the most common ones I see), and exercising regularly, are those who have the highest chance of being 'healthy' (though I do not use the term 'healthy' lightly).
Ultimately, PCOS is one of those things that just happens and isn't your fault. I also have an endocrine disorder that makes it very easy for me to gain weight and very difficult for me to lose it, so I absolutely understand the situation yours in right now.
But, what do you do with this information? Do you say, "I am X, Y and Z because of my PCOS" and leave it at that? Or do you say "I suffer with X, Y and Z because of my PCOS, so I make life choices to reduce the impact of my PCOS by 1, 2 and 3".
So my advice is this: PCOS may be the hand you've been dealt, but your lifestyle choices can massively improve the chances of you reducing its impact on your long-term health. I'm not blaming you, or acting like healthy eating, exercise and medication decisions are easy; they are not. Please recall I'm in a similar boat, and I'm not one to blame women for their complex health conditions.
I could talk all day about PCOS but this is my best attempt to summarise it for you.
It's really hard making tough life choices to manage the hand you've been dealt. I fully understand. I've gotten better at it as I've gotten older. @mrhaitch makes similar big decisions, because he has two diabetic parents and one diabetic siblings, so he takes care of his health to a brilliant degree, to try to give himself the best chance of not developing diabetes himself.

☝️ me being your hype man
Love,
-- Haitch xxx
10 notes
·
View notes
Text
My Medical History: A Comedy of Errors
This is long as shit but since it's finally sort of resolved itself I figured it'd be worth documenting. Strap in, folks.
Me, age 12: I have Experiences
Doctor: You're schizoaffective you need many pills.
Me: Sure, I guess.
Me: Dad I experience these kinds of things being schizoaffective.
Dad, also schizoaffective: Huh I relate to none of that.
Me: Should we look into that discrepancy further?
Dad: Nah.
Me: Mom I forgot to take one of the seven medications I'm on for over a month and felt no effect from not taking it. Is there a chance I'm potentially on too much medication?
Mom: You need to take all the pills the doctors give you.
Me: I'm on more Seroquel than both you and Dad combined and have been since I was 13 is that bad?
Mom: No it's normal and good, actually.
Me: I have nothing to compare this too and if I disagree too hard with you I might be left to fend for myself in the wilderness like a newly-stray cat.
Different Doctor: I don't think you're schizoaffective because you were way too young to show signs when you were diagnosed.
Me, age 17: Oh? What do you think I am?
Different Doctor: No idea. Moving on!
Therapist: You aren't bipolar.
Me, age 18: What am I, then?
Therapist: Probably nothing. It really doesn't matter.
Me: I don't know what to do with that information.
An additional doctor: Yeah, I agree with that doctor you saw almost a decade ago. I don't think you're bipolar.
Me, 26, very tired: Okay.
Additional doctor: You're too traumatized for me to diagnose, though.
Me: Uh-huh. That's - fine. I guess.
Additional doctor: Here are some anti-psychotics though.
Me: These anti-psychotics make me throw up at least once a week can we switch to a different kind?
Additional doctor: Eh I don't know. They're not making you psychotic so it's probably fine.
Me: cool okay
Me: Hey I was on 900mgs of Seroquel from ages 13-21 do you think that could be a bad thing for me health-wise?
A doctor, at some point: It is a medical improbability that taking that much of that medication for that long didn't give you diabetes.
Me: Great. Love that for me.
Me: Therapist I need a diagnostic I'm losing my mind.
Therapist: I'm reading your diagnosis and you actually don't meet the basic clinical criteria for really any mental illness.
Me: ??????? cool
Therapist: You might have ADHD though.
Wife: You absolutely have ADHD.
Me: Can I get treated for ADHD please?
New psych: I can't treat you for ADHD if you're diagnosed as bipolar.
Me: I have had multiple doctors say I'm not bipolar. I have a diagnostic that says I'm not bipolar.
New psych: Someone at some point said you were bipolar.
Me: I was 12.
New psych: Either way. Also this diagnostic you took says you have BPD.
Me in my next therapy session: Hey uh Therapist when were you going to tell me I have BPD?
Therapist: You...don't? You don't have that.
Me: My psych said the diagnostic you sent her shows I do.
Therapist: She apparently doesn't know how to read the diagnostic then because that's - um. Incorrect.
Wife: You need to stop telling new psychs you were ever diagnosed bipolar it's clearly making them biased.
Me: That feels like denying medical people medical information they need for medicine.
Therapist: I agree with Wife actually.
Me: You - really? Fuck. I mean, okay.
Me, in an intake appointment: I was never diagnosed bipolar.
Current psych: Uh okay.
Me: I'm lying.
Current psych: Oh. Oh?
Me (Sobbing): I'm so sorry I'm lying I just lied.
Current psych: It's okay. You're - um -
Me (Weeping, shame spiraling): You seem so nice -
Current psych: Wow. Wow you are struggling.
Few Sessions Later
Current psych: Yeah you could have ADHD. Probably wanna be careful though because ADHD meds can cause mania in bipolar people, so even though you haven't really shown any signs of bipolar or schizophrenic symptoms we should still air on the side of caution.
Few More Sessions
Current psych: Ah yeah you're super ADHD. That makes sense and surprises nobody.
Me, 27, lying face-down on the floor: rad hooray for medicine.
#life stuff#neurodivergent#stuff will potentially get better soon#tw medical abuse#tw parental neglect#my bones are tired haha
8 notes
·
View notes
Text
My doctor’s gonna be disappointed I didn’t get the imaging yet they wanted me to get for diagnostic criteria but the last imaging was $1200 out of pocket and frankly I spent the months in between the imaging they ordered and this appointment I have soon going on trips and I wanted to spend my money on that instead.
I’ve already spent so much money and time off work to get 2 endoscopies, get a gastric emptying study done (it was like 2 hours and I was fighting nausea the entire time) and go to these doctor appointments. I’m getting bloodwork done tomorrow.
Idk man we know my stomach won’t empty but we have no idea why, everything looked good, they took cultures while in my tummy and djdnt find anything, I have no family history of diabetes or gastroparesis or celiac or IBS like my dad (literally a gastroenterologist, just not MY gastroenterologist) says it’s extremely likely my stomach is not functioning correctly after one of the GI viruses I’ve had before. But idk how you prove that.
Currently the only direction I was given was “eat 5-6 small low fat meals a day” which is super impractical unless I work from home or never go on vacation, so, thanks.
Idk man. My mom got mad at me for admitting I put the testing off but she of all people should understand when you have a chronic illness with no discernible cause sometimes you just wanna stop with all the tests and shit cause it’s useless. Again, I’d rather spent that $1200 on concert tickets (which I did, plus I’m paying that off each month in installments which I don’t think the hospital would let me do easily)
#personal shit#anyway any one else with a shitty stomach hit me up#what’s your DX#kinda funny to me people spent so much money to get gastric me whatever#or get ozempic to kill their appetite#just get gastroparesis it’s free
2 notes
·
View notes
Text
What are the 3 main symptoms of Autism
Autism is a complex neurodevelopmental disorder that affects a person’s ability to communicate and interact socially with other people. It is estimated that around 1 in 54 children in the US are diagnosed with autism, making it more common than diabetes, cancer, and AIDS combined.
When it comes to autism, there are three main symptoms that are generally seen in those who are affected. These are difficulties with social interaction, repetitive behaviors, and communication challenges. This article will provide an overview of these three main symptoms of autism, as well as detailing some of the specific issues associated with them.
Social interaction difficulties are a hallmark symptom of autism. People with autism often have difficulty recognizing or identifying facial expressions and identifying emotions from others. This difficulty in understanding the emotions of others can make it difficult for people with autism to connect with people and build relationships.

Finally, people with autism often have communication challenges. This can include difficulty understanding language, speaking in a proper manner, having difficulty understanding the meaning of words, and having difficulty making sense of conversations. People with autism may also have difficulties with pragmatic languages, such as understanding sarcasm or making jokes.
These are the three main symptoms of autism, and they can often be identified through diagnostic criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). In order to diagnose autism, medical professionals use a variety of assessments to evaluate the severity of the symptoms and help develop an appropriate treatment plan.
In this article, we will take a closer look at each of these three main symptoms of autism, as well as provide some tips for recognizing them and seeking treatment for those affected.
Read more
2 notes
·
View notes
Text
Patient is a [ ] yo male/female presenting to the clinic for a preoperative evaluation.
Procedure [ ]
Scheduled date of procedure [ ]
Surgeon performing procedure requesting consultation for preop is [ ] and can be contacted at [ ]
This patient is/is not medically optimized for the planned surgery, see below for details.
EKG collected in office, interpreted personally and under the direct supervision of attending physician as follows- sinus rate and rhythm, no evidence of ischemia or ST abnormalities, no blocks, normal QTc interval.
The following labs are to be completed prior to surgery, and will be evaluated upon completion. Procedure is to be performed as scheduled barring any extraordinary laboratory derangements of concern.
Current medication list has been thoroughly reviewed and should not interfere with surgery as written.
Patient has no prior history of adverse reactions to anesthesia, problems with airway management, difficult IV access, prolonged emergence, or postoperative nausea/vomiting.
Airway Mallampati score: This patient is a Grade based on the criteria listed below
-Grade I Tonsillar pillars, soft palate, entire uvula
-Grade II Tonsillar pillars, soft palate, part of uvula
-Grade III Soft palate, base of uvula
-Grade IV Hard palate only, no uvula visualized
Patient is a low/medium/high risk for this low/medium/high risk surgical procedure.
Will send documentation of this preoperative visit to surgeon [ ].
**** ADDITIONAL INFORMATION****
Patient Risk for Elective Surgical Procedure as Determined with the Criteria Below:
1- Very Low Risk
No known medical problems
2- Low Risk
Hypertension
Hyperlipidemia
Asthma
Other chronic, stable medical condition without significant functional impairment
3- Intermediate Risk
Age 70 or older
Non-insulin dependent diabetes
History of treated, stable CAD
Morbid obesity (BMI > 30)
Anemia (hemoglobin < 10)
Mild renal insufficiency
4- High Risk
-Chronic CHF
-Insulin-dependent diabetes mellitus
-Renal insufficiency: creatinine > 2
-Moderate COPD: FEV1 50% to 70%
-Obstructive sleep apnea
-History of stroke or TIA
-Known diagnosis of dementia
-Chronic pain syndrome
5- Very High Risk
-Unstable or severe cardiac disease
-Severe COPD: FEV1 < 50% predicted
-Use of home oxygen
-Pulmonary hypertension
-Severe liver disease
-Severe frailty; physical incapacitation
Surgical Risk Score Determined as Below:
1- Very Low Risk
Procedures that usually require only minimal or moderate sedation and have few physiologic effects
-Eye surgery
-GI endoscopy (without stents)
-Dental procedures
2- Low Risk
Procedures associated with minimal physiologic effect
-Hernia repair
-ENT procedures without planned flap or neck dissection
-Diagnostic cardiac catheterization
-Interventional radiology
-GI endoscopy with stent placement
-Cystoscopy
3- Intermediate Risk
Procedures associated with moderate changes in hemodynamics, risk of blood loss
-Intracranial and spine surgery
-Gynecologic and urologic surgery
-Intra-abdominal surgery without bowel resection
-Intra-thoracic surgery without lung resection
-Cardiac catheterization procedures including electrophysiology studies, ablations, AICD, pacemaker
4- High Risk
Procedures with possible significant effect on hemodynamics, blood loss
-Colorectal surgery with bowel resection
-Kidney transplant
-Major joint replacement (shoulder, knee, and hip)
-Open radical prostatectomy, cystectomy
-Major oncologic general surgery or gynecologic surgery
-Major oncologic head and neck surgery
5- Very High Risk
Procedures with major impact on hemodynamics, fluid shifts, possible major blood loss:
-Aortic surgery
-Cardiac surgery
-Intra-thoracic procedures with lung resection
-Major transplant surgery (heart, lung, liver)
High risk surgery: yes/no
Hx of ischemic heart disease: y/n
Hx of CHF: y/n
Hx of CVA/TIA: y/n
Pre-op tx with insulin: y/n
DM/how are blood sugars?
Pre-op Cr >2mg: y/n
OTHER EVALUATIONS BASED OFF PATIENT HISTORY SEE BELOW:
1. CARDIAC EVALUATION
A. Ischemic Cardiac Risk- Describe any history of cardiovascular disease and list the cardiologist/electrophysiologist. For CAD, report the results of the most recent stress test or cardiac cath, type of procedures or type of stents, date of MI, and recommendations for perioperative management. Include antiplatelet management. Continue baby aspirin for patients with cardiac stents - unless having neurosurgery, then coordinate with surgeon.
B. Ventricular function - include most recent echocardiogram evaluation ideally performed within the past 2 years
C. Valvular heart disease- include most recent echocardiogram, type of prosthetic valve
D. Arrhythmias - include any implanted devices and recent interrogation report, contact electrophysiology about device management during the surgery and include recommendations provided. For A-Fib, include CHA2DS2-VASc score
E. Beta blockade - All patients on chronic beta blockers should have these medications continue throughout the perioperative period unless there is a specifically documented contraindication.
F. Hypertension - Other than for cataract surgery, ACEI inhibitors and ARBs should be held for 24hours prior to surgery and diuretics should be held the morning of surgery
G. Vascular disease - include antiplatelet management and dates of strokes
2. PULMONARY EVALUATION
A. COPD/Asthma - include any recent exacerbations, intubations, chronic O2 use, amount of rescue inhaler use
B. OSA risk - STOPBANG score - address severity of sleep apnea and CPAP use
3. HEMATOLOGIC EVALUATION
A. Bleeding Risk - assess the bleeding risk and history for every patient
B. VTE Prophylaxis/Thrombotic risk - estimate risk and provide recommendations
C. Anticoagulation management - include pre-op and post-op medication instructions
D. Anemia - pre-op treatment plan
D. Oncology - history and treatments
4. ENDOCRINE EVALUATION
A. Diabetes mellitus - include type, medication use, recent A1c, pre-op and post-op management instructions
B. Adrenal insufficiency risk - assess for prolonged steroid use in the last year
5. RENAL EVALUATION
A. CKD - include stage, baseline labs
B. ESRD - include dialysis schedule, type, access, dry weight, location of dialysis. Generally, surgery should not be scheduled on a dialysis day.
C. Electrolyte abnormalities
6. GI EVALUATION
A. Liver disease - including MELD score and Child-Pugh classification
7. OTHER relevant comorbidities or anesthesia considerations
[substance abuse, chronic pain, delirium risk, PONV (post-operative nausea and vomiting) risk, psych disorders, neurologic disorders, infectious disease, etc.]
5 notes
·
View notes
Text
>It will never not baffle me how hard society tries to insist that fatness is an abnormality.
It is abnormal. The human body was never meant to be obese. It was never meant to carry massive amounts of excess weight, much less upwards of a hundred extra pounds of it. It’s not insisting on something completely outlandish, it is a simple observation. No one was meant to be 300+ lbs. No one.
>The average western woman wears plus size clothing. One of the smallest garments on the scale is called a medium.
Just because the average person is overweight or obese does not mean that being overweight or obese is normal. The fact that people are considerably larger on average than they were only fourty years ago should tell you something. The general population has gotten more obese since the 1980s. Pointing to clothing sizes does not actually refute the argument that the growing number of obese people is a concern. Especially with the rise of vanity sizing, where clothing sizes today are equal in measure to much larger labeled sizes in past decades.
>Most people with anorexia are in the overweight bmi category, yet somehow that's known as "atypical anorexia".
Most people with anorexia are not overweight. One of the literal criteria for anorexia is a low body weight and a fear of gaining weight. Because when you are starving you lose weight. Shocking. Atypical anorexia is called atypical because while it lacks the underweight requirement, the patient still has experienced rapid weight loss as a result of severe food restriction.
This is really such an insane thing to lie about that is easily disproven by common knowledge or simple google search of the conditions diagnostic criteria.
If you really gave a fuck about people with EDs you would stop trying to coopt the struggles of people with anorexia and destigmatize getting help for people with BED, NES, and EDNOS which are far more common and far more likely to effect overweight and obese individuals than AN or BN.
>Fatness is often labeled the cause of a number of diseases, but there are literally no diseases exclusive to fat bodies.
Because it is. Being obese can cause motor issues in the joints as a direct result of the excess weight. It can cause fatty heart and fatty liver. It can causes hormonal problems because visceral fat is hormonally active. It results in an increased risk of heart disease and diabetes. It increases one’s risk of multiple types of cancers, including reproductive cancers.
This is literally like saying that people should just continue to smoke cigarettes because people who don’t smoke also get lung cancer. We know people who don’t smoke get lung cancer, but the risk is much higher and people who otherwise would not have gotten lung cancer are 15 to 30 times more likely to get it if they are smokers.
>Looking at movies and television, you'd think the world was 98% thin people. It's not.
I hate the use of obfuscated terms like thin and fat in these conversations because it’s entirely subjective. This is why fat activists hate terms like obese and morbidity obese, because they can actually be measured and defined. What is considered fat or thin in one culture, community, group, etc could easily be vastly different from another. Like someone could be considered hugely fat while they live in LA but move to Georgia and be considered very thin. The same for western vs Asian countries.
According to the WHO, adult overweight and obesity has risen from 25% in 1990 to 43% in 2022. Nearly doubled. Meaning, no, the “thin” population is not 98%, but 57%. But that’s not a diversity win, that is a huge cause for concern.
It will never not baffle me how hard society tries to insist that fatness is an abnormality. The average western woman wears plus size clothing. One of the smallest garments on the scale is called a medium. Most people with anorexia are in the overweight bmi category, yet somehow that's known as "atypical anorexia". Fatness is often labeled the cause of a number of diseases, but there are literally no diseases exclusive to fat bodies. Looking at movies and television, you'd think the world was 98% thin people. It's not.
My point isn't that if it was pretty rare to be fat, fatphobia would be okay. Of course not.
My point is that we're surrounded by all these artificial indicators that fatness is unnatural and uncommon and it's just not true?? Humans are not always thin and we've never all been thin and we're not all meant to be thin. Fat humans are a normal type of human. Fatness is a feature, not a bug.
33K notes
·
View notes
Text
Is All-on-X Right for You? Eligibility and Benefits of Full Arch Implants

Are you struggling with tooth loss or frustrated by uncomfortable dentures?
Full arch dental implants, particularly the All-on-X system, could be the perfect solution for you. Imagine having a natural-looking smile with a permanent and secure alternative to traditional dentures.
The All-on-X system replaces an entire arch of teeth using just four to six implants, offering exceptional stability, comfort, and durability.
If you’re considering this option, it’s essential to understand the eligibility criteria, the procedure, and the many benefits it offers. While this treatment may not be suitable for everyone, it can be a transformative solution for those seeking a long-term fix for their smile.
Let’s explore why All-on-X has become a preferred choice for so many people today.
Who Is Eligible for All-on-X?
All-on-X provides a life-changing solution for individuals looking for a permanent remedy for missing teeth. However, not everyone is a candidate for this advanced procedure. Several factors determine eligibility, including:
Bone Density: Sufficient jawbone density is required to support the implants.
Overall Health: Good general health is crucial for successful healing and implant integration.
Medical Conditions: While age is not a major factor, conditions such as uncontrolled diabetes can affect the healing process.
Consultation and Diagnostics: A detailed evaluation, including diagnostic imaging, will determine if you qualify for the procedure. If you're considering All-on-X implants in Hugo, schedule a consultation to assess your suitability for this life-enhancing treatment.
Benefits of All-on-X Full Arch Implants
Full arch implants like the All-on-X system offer a durable, long-term solution for tooth loss. Here’s why many patients choose this option:
Permanent Solution: Unlike dentures that may shift or wear out, All-on-X implants provide a secure and lasting fit.
Improved Functionality: These implants restore natural speech, chewing ability, and confidence.
Aesthetic Appeal: All-on-X delivers a natural-looking smile that closely resembles real teeth.
Enhanced Comfort: The stable, secure fit eliminates the discomfort often associated with traditional dentures.
Reduced Treatment Time: Compared to individual implants, the All-on-X procedure is quicker and requires fewer surgeries.
Long-Term Cost-Effectiveness: Although the initial investment is higher, the durability of All-on-X implants makes them a more cost-effective option in the long run.
The All-on-X Procedure: What to Expect
The All-on-X procedure is efficient and carefully planned. Here’s what you can anticipate:
Consultation: Your dentist will assess your oral health, jawbone density, and overall suitability for the procedure.
Implant Placement: Four to six titanium implants are strategically placed in your jaw to serve as the foundation for your new teeth. The procedure is performed under local anesthesia or sedation.
Temporary Teeth: After implant placement, temporary teeth are attached, allowing you to adjust while the implants integrate with the bone.
Recovery: Healing takes time, with most patients resuming normal activities within 1-2 weeks. Full integration typically occurs over 3-6 months, with follow-up visits to monitor progress.
Comparing All-on-X to Other Tooth Replacement Options
When choosing a tooth replacement method, it’s important to compare alternatives. Here’s how All-on-X stands out:
Dentures: Unlike removable dentures that may slip or require adhesives, All-on-X implants provide a stable, permanent solution.
Bridges: Traditional bridges involve altering adjacent healthy teeth, whereas All-on-X preserves them.
Individual Implants: While single implants are effective for isolated tooth loss, All-on-X is a more efficient option for full arch replacement, requiring fewer implants and reducing recovery time.
Cost: Although All-on-X implants have a higher initial cost, their durability makes them a cost-effective choice over time. Studies show a survival rate of 99.0% over a 36-month period.
Is All-on-X Right for You?
Wondering if All-on-X is the best choice for your dental needs? Consider the following:
Consult a Specialist: A consultation with an experienced All-on-X provider will help determine if this treatment suits your oral health, bone structure, and lifestyle.
Assess Your Needs: If you’re frustrated with traditional dentures or seeking a lasting solution for missing teeth, All-on-X may be the right option.
Consider the Long-Term Benefits: If you value comfort, convenience, and a permanent solution for your smile, All-on-X implants offer significant advantages.
All-on-X implants provide an effective, long-lasting solution for those dealing with tooth loss. If you’re considering this treatment, consulting a qualified dental professional can help you make an informed decision. With a faster recovery, enhanced comfort, and permanent results, All-on-X could be the life-changing dental solution you’ve been searching for.
0 notes
Text
So uhhhhh someone's trying to argue that psychiatric disorders can exist on an entirely non-physical level
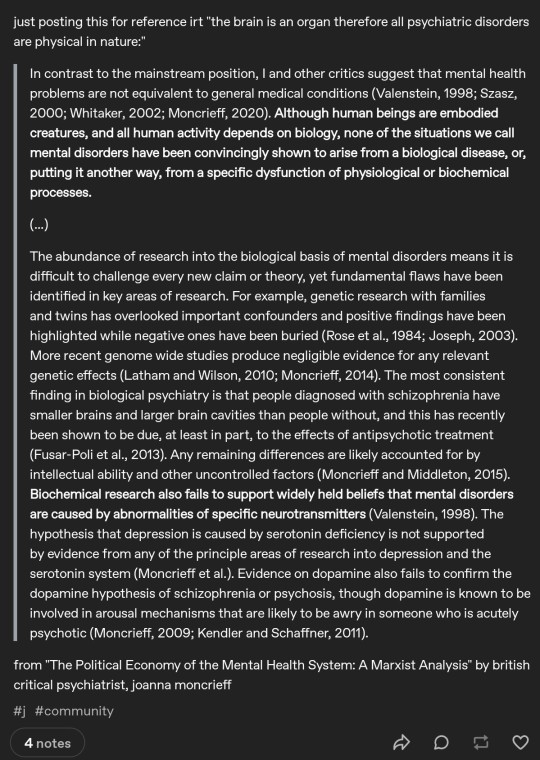
1. This is from a sociopolitical analysis of the institution of psychiatry, and I suspect is therefore taken wildly out of context at best and is irrelevant to actual neurology at worst.
2. It claims that psychiatric conditions have not (yet) been convincingly SHOWN to arise from physical conditions, directly contradicting the claim that humans are embodied and therefore all human activity is biology-dependent.
3. Unless the claims of genetics being largely unrelated to mental health is about a very specific topic, that's just science denial. The MTHFR gene has been heavily implicated in multiple commonly comorbid conditions that are also suspected to be post-viral in a large percentage of cases, such as chronic fatigue syndrome, POTS, and mast cell diseases. Multiple conditions, from diabetes to bipolar to autism to again, mast cell diseases, are known to be highly genetic, despite the exact genetic cause often still being unclear.
4. The sources used to back up the prior point are: an article in "Independent Science News for food and agriculture", which also platformed multiple articles and even a Twitter thread about the conspiracy theory of covid being leaked from a chinese lab; and an article about how the diagnostic criteria of bipolar was changed and is now overdiagnosed to sell more drugs.
5. The supposedly "suppressed" "negative" articles are potentially out of date (I've had a harder time accessing them). From what I can find, though, the former is a book largely considered more political than scientific, which was criticizing overly reductionist perspectives on genes as related to systemic social inequality. The latter appears to be about personality and "neuroticism" primarily, with little said about genetic roles in psychiatric health. It seems that they do not actually contradict the possibility of even some genetic influence on psychiatric health, let alone physical influence.
6. The whole argument is a logical fallacy, arguing that because we've ruled out some of the few biochemical and structural/physiological characteristics that could cause mental illness, we've ruled physical causes out entirely. It uses two highly specific discrete claims about two disorders in the vast spectrum of mental health, claiming that brain sizes affected in part by antipsychotic use do not seem to cause schizophrenia and that all other differences in neurobiology are likely due to "intellectual ability" and the conveniently vague "other uncontrolled factors". They further use depression and schizophrenia again to talk about how two specific neurotransmitters had not been proven to cause the illnesses - specifically, ones which have evidence supporting their role in other disorders, such as ADHD. While some of the theories of chemical imbalances causing mental illnesses have since been more conclusively disproven, others have had more evidence emerge supporting them having some role in multiple psychiatric diagnoses.
7. That whole paragraph actually only focuses on whether or not there are neurobiological causes for mental illness. Even purely sociogenic mental illnesses, such as certain cases of PTSD, still have been shown to have effects on the brain at a physiological level, while others show up in studies as changes in patterns of bioelectrical brain activity or changes in chemical production or reuptake efficiency. Proving or disproving origin does not actually provide evidence for mechanism. However, in case I am misinterpreting the word "cause" here and it is actually meant as "mechanism", disproving mechanisms is quite literally part of the process to find the true mechanism, and does not actually support that psychiatric conditions occur entirely separately from the physical brain.
Essentially, even aside from the irreputable and irrelevant sources cited, the lack of scientific consistency and sociopolitical focus of the excerpt; the author's repeated self-citations; the failure of insufficient, unreliable, and outdated evidence to support the claims they make; the fact that their actual argument that mental health problems are not "equivalent" to other health issues; amd that psychiatric conditions have not yet been observed as arising from a direct proven neurological source, while actively admitting that humanity is stored in the body, so to speak...
None of this proves that there is not a biochemical or physiological mechanism and/or origin for psychiatric illnesses that, in our search closed eyes in the dark for understanding of the human brain, we are fumbling for. Neurology is a science in its infancy compared to most other medical fields, still stumbling its way through "four humours" levels of rudimentary understanding of the highly complex processing and control unit that is the 86 billion neurons of the human brain. This is even more true when we soften the science of neurology into neuropsychiatry, practically poking experiences of the conscious mind with a caveman-stick. This is not to disparage the sciences, but rather, to point out that we understand so little that we can't even recognize the full scope of our ignorance, that 600 years from now may earn us the same ridicule as blood-letting leeches and cocaine soda for head colds.
More to the point, anything we process - sensory input, emotion, thought, pain, dissociation even, oppression, poverty, trauma - it all goes through the brain. Our entire understanding, self-conception, and consciousness arise from biochemical, physiological, and bioelectric actions and reactions. The "self" is essentially a simulation run by a fleshy machine as it responds to stimuli and generates aspects of identity from desires to beliefs.
While the point that the excerpt is likely building to in a larger context, that many mental illnesses may originate in part of in whole from factors like systemic injustice and external conditions to the body, that doesn't make the illness itself occur outside of the physical human bodymind. Even experiences like religion and "communing" with a higher power, astral projecting, and so on, require your brain to perceive them as occurring, which means that extremely complex series of chemical production and absorption and electrical signals and activity traversing specific paths in specific regions of the brain are occurring.
The same is true of mental-illness-as-reaction-to-conditions.
To argue otherwise is to argue that some metaphysical conscious separate from the physical human body exists. This is just cartesian dualism, and falls entirely outside the realm of science and well into philosophy. If a "soul" of the self exists that can suffer an "illness" or other "corruption" causing severe distress and dysfunction within the physical world, it is outside of the realm of science to even examine, let alone make claims about. Furthermore, even then in order to be perceived within our physical reality, the brain must process and/or create that perception of said "soul" and "illness".
This is far more into the realm of philosophy than is comfortable, considering that philosophy claiming to be science is just pseudoscience in a stick-on mustache. (I respect philosophy in its own right - love it, actually - but when it plays at being a rational and empirical science, I draw the line. It has its own internal logic systems and reasoning which has little overlap with or application to scientific methodology.)
But, returning firmly to science, the irony is that it's entirely possible that some psychiatric conditions may not be entirely or even primarily neurological. The gastrointestinal, endocrine, lymphatic, and immune system have all been implicated to some degree in having varying degrees of impact on mental health. Some conditions we call mental health may originate in dysfunction of other systems, which may also in turn be driven by external factors. The brain is the control center of the body, and the body processed all consumed materials into needed resources for the brain and body alike.
Some primarily physical disabilities even have significant neurocognitive symptoms, such as brain fog/cognitive impairment and strong mood swings. Some symptoms themselves may straddle the line, such as seizures and sleep disorders/disturbances. Some physical symptoms, such as dysautonomia, have been reported to cause symptom sets highly similar to neuropsychiatric conditions like ADHD, traumatic brain injuries have been observed to sometimes replicate symptoms of dissociative disorders, and Chiari malformations have been noted to sometimes cause anxiety.
Mast cell disorders have overactive release of neurotransmitters as part of the process which drives symptoms, and those neurotransmitters can affect the brain strongly, to the point of causing an array of mental symptoms - some of which even drive further degranulation in a vicious cycle.
In any case, mental illnesses may not all be neurogenic or even primarily neurological. But they are still, in fact, physical. Everything we perceive or imagine must be processed by the brain. Only the imperceptible does not cause any sort of brain action or reaction, and if we are not aware of it or affected by it on any level, it's outside of the realm of science, let alone medicine.
Now, if you wanna talk philosophy, we can argue whether something must be perceived to exist. That's a really fun philosophical topic, one which I contradict myself on, even.
But from a medical perspective? Medicine, including psychiatry and the classification and treatment of mental illness, does require a perceived experience which affects you, which results squarely into some kind of physical process in the brain. That's science, babeyyyyy!
#yes I know I put a couple of memes into my logic#let me have this I went to search their blog after seeing an absolutely bizarre tag#that left me wondering if they don't think chemical processes are physical or something#but honestly this is worse#I don't know how much more I can break down 'perception requires neurological processing on a physical level'#just absolutely beyond the pale take#'psychiatric disorders are not physical' ex-ca-fucking-SCUSE me?!?! 'not PHYSICAL'?!?!?!#and why? because we don't yet UNDERSTAND the mechanisms which drive them?!?!?!!?#like I don't know how to tell you that they thought some physical illnesses were also nonphysical and just demons at some point either#(I know that's not most historical medicine since like. y'know they were splinting broken bones tens of thousands of years ago)#but like that's the level of illogic we're dealing with!!!#not physical my ass#as in if psychiatric conditions aren't physical than neither is my copious empirically experiential butt#which they can eat for subjecting me to this take#I'm being half facetious I'm more in awe than angry#I'm not sure if this is just a result of the severe drop in societal critical analysis and reasoning skills#or if there's something beyond that going on#I'm leaning the former given someone trying to use a marxist political commentary to prove a neuroscientific negative#but just. wow.#if someone commits a logical fallacy on tumblr and no one reads it does it still cause annoyance#lmao that last tag is utter nonsense I'm calling myself out now XD
0 notes
Text
Online Fellowship in Diabetes Mellitus in India for MBBS Doctors

Diabetes Mellitus (DM) is one of the most common chronic diseases globally, with India witnessing an alarming increase in the number of cases over the past few decades. The nation is now considered the “Diabetes Capital of the World,” with millions suffering from this condition. Given the prevalence of the disease and its potential complications, medical practitioners in India are increasingly seeking specialized training in diabetes management. For MBBS doctors, this growing demand for diabetes expertise presents an opportunity to advance their careers and contribute more effectively to healthcare. One of the most popular and flexible ways for doctors to pursue specialized training in diabetes mellitus is through online fellowship programs.
Importance of Specialization in Diabetes Mellitus
The impact of diabetes extends beyond high blood sugar levels, often leading to complications such as cardiovascular disease, kidney failure, vision problems, and neuropathy. Given the long-term nature of the disease, patients require continual monitoring and tailored treatment plans. General practitioners, though equipped with a broad medical background, may lack in-depth knowledge of managing complex diabetic cases. This gap in expertise can affect the quality of care and the ability to mitigate complications effectively.
For MBBS doctors, obtaining a fellowship in diabetes mellitus enables them to acquire the latest knowledge on diabetes care, develop practical skills in patient management, and stay updated with evolving treatment guidelines. Specializing in diabetes also opens new career pathways, from setting up a dedicated diabetes clinic to working in specialty hospitals and healthcare centers focusing on endocrinology and metabolic diseases.
Why Choose an Online Fellowship?
With the increasing demands of clinical practice, many doctors find it challenging to enroll in full-time courses or take extended time off to pursue additional qualifications. This is where online fellowship programs serve as an ideal solution. They offer flexible learning schedules that allow doctors to continue their practice while pursuing higher education.
The key benefits of enrolling in an online fellowship in diabetes mellitus include:
Flexibility: Doctors can complete the course at their own pace, balancing their clinical duties with study time. This flexibility is crucial for professionals who cannot take extended breaks from their practice.
Accessibility: These online programs are accessible from any location, meaning that doctors practicing in remote areas or smaller cities can gain access to the same high-quality education as their peers in urban centers.
Cost-effectiveness: Online courses tend to be more affordable than traditional on-campus programs, reducing the financial burden on doctors.
Quality Learning: Many of these programs are designed and led by leading endocrinologists, diabetologists, and healthcare institutions. They often include multimedia resources, case studies, webinars, and interactive sessions, ensuring a comprehensive learning experience.
Certification and Recognition: Most fellowship programs culminate in a recognized certification, adding significant value to a doctor’s professional credentials and enhancing their career prospects.
Structure of Online Fellowship Programs in Diabetes Mellitus
Though the exact structure may vary depending on the institution offering the fellowship, most online programs for diabetes mellitus specialization include the following components:
Core Curriculum: The syllabus usually covers various aspects of diabetes mellitus, including its pathophysiology, diagnostic criteria, classification (type 1, type 2, and gestational diabetes), and prevention strategies. It also explores complications of diabetes, such as diabetic neuropathy, nephropathy, retinopathy, and cardiovascular complications.
Diabetes Management: A significant portion of the course focuses on clinical management, including pharmacotherapy (insulin, oral hypoglycemics, etc.), lifestyle modifications (diet, exercise), and modern therapies such as continuous glucose monitoring and insulin pumps.
Research and Evidence-Based Practice: The program often emphasizes evidence-based practices in diabetes care, encouraging doctors to stay updated on recent studies, treatment guidelines, and clinical trials.
Case Studies and Practical Application: Many online fellowship programs incorporate real-life case discussions, allowing doctors to analyze, interpret, and apply knowledge to complex diabetes cases. This practical component equips participants with the clinical acumen needed to manage diabetes patients effectively.
Assignments and Examinations: Periodic assessments, including assignments and online examinations, help in tracking progress and ensure that participants are grasping key concepts.
Clinical Attachments (Optional): Some fellowship programs may offer optional clinical attachments or observerships in diabetes centers, where participants can gain hands-on experience in a clinical setting.
Duration: The duration of most online fellowship programs ranges from 6 to 12 months, depending on the intensity of the course and the time commitment of the participants.
Eligibility Criteria and Enrollment Process
Typically, the eligibility criteria for enrolling in an online fellowship in diabetes mellitus in India include:
A MBBS degree from a recognized institution.
Medical Council of India (MCI) registration or its equivalent.
Some programs may require a minimum number of years of clinical experience.
The enrollment process is generally straightforward and involves:
Filling out an online application form through the institution's official website.
Providing academic and professional documents, including MBBS certificates and MCI registration.
Some programs may require candidates to submit a statement of purpose or attend a brief interview.
Career Prospects After Fellowship
Completing an online fellowship in diabetes mellitus opens several career opportunities for MBBS doctors. Some potential career pathways include:
Specialized Diabetes Clinics: Doctors can establish their own diabetes care centers, providing dedicated and personalized care to diabetic patients.
Consulting Diabetologist: Graduates can work as diabetologists in hospitals, clinics, and specialty diabetes centers.
Public Health: Doctors with an interest in public health can work on diabetes prevention programs, policy development, and community outreach initiatives.
Research and Academia: Those inclined towards research can contribute to clinical trials, diabetes research, or take on teaching roles in medical colleges and institutions.
Endocrinology Training: The fellowship can also serve as a stepping stone for further specialization in endocrinology.
Conclusion
An online fellowship in diabetes mellitus offers a valuable opportunity for MBBS doctors in India to enhance their knowledge, skills, and career prospects in the field of diabetes care. With flexible learning options, accessible programs, and recognized certification, this form of higher education is ideally suited for medical professionals who want to make a significant impact on diabetes management while continuing their clinical practice. As diabetes continues to rise across India, specialized training in its management is not only a career advancement opportunity but also a step toward improving healthcare outcomes in the country.
#online fellowship programs#Fellowship in Diabetes Mellitus#fellowship in Diabetes Mellitus global med academy
0 notes
Text
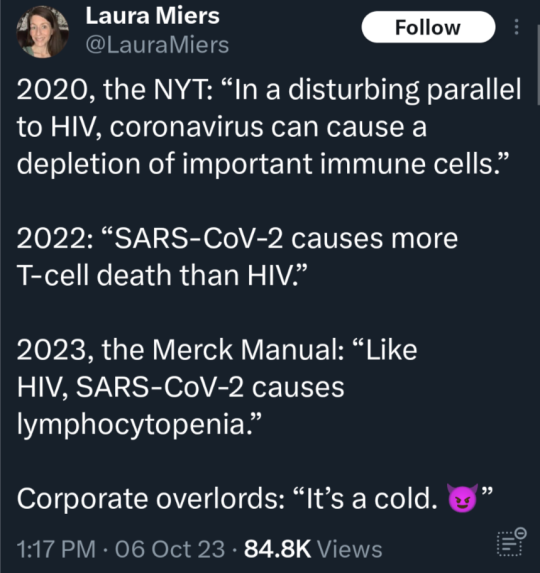
sup. so i was diagnosed with chronic fatigue syndrome after having covid multiple times. at the moment something like half of all long covid sufferers also fit the diagnostic criteria for CFS. They're extremely similar, if not the same thing.
No one talks about CFS who doesn't have it or a loved one with it, and certainly the average person doesn't know what it actually looks like. What the quality of life is actually like. So let me tell you.
According to multiple studies, the quality of life of people with CFS is significantly lower than many of the well known and dreaded conditions like: MS, Parkinsons, diabetes, late stage cancer, you name it. According to these studies, people with CFS generally have a similar quality of life to someone with a late stage cancer during chemo treatment. Feelings of unwellness, sickness, fatigue, pain, sleep disturbances, neurological and cognitive deficits, etc. etc. but that's the baseline. It's been 3 years of this for me.
Another way I've seen it described in one of these studies based on self reported surveys across many chronic illnesses - people's numbers with CFS show we've got a similar quality of life to someone with untreated AIDS might expect around 4 months before death. This, based on thousands of surveys from thousands of people. These are ugly comparisons, meant to describe an ugly reality that is otherwise completely unknown by using comparison with what is known. We know AIDS entails terrible suffering. We know late stage cancer and the chemotherapy treatments for it entails terrible suffering. My mum went through her third cancer diagnosis and chemo treatment just over two years ago and in the end passed away from complications. I know and am not making light.
So, why use this horrible yardstick to measure?
I've had to teach my doctors about CFS. I've had to teach them the symptoms, send them research and current medication recogmmendations to symptoalleviatems even if we can't cure them because we don't know what CFS is. What's causing it, what's gone wrong, where to look - we don't fucking know. Most meds we've tried out haven't improved anything.
I have CFS as a diagnosis on file, but my doctor and I are working on the understanding that I only developed this after having COVID twice. By technicality, I could also have long covid on file, or have been given a long COVID diagnosis rather than CFS. Which one you get is based more on chance than anything - whichever one your doctor knows more about and thinks of first, that's usually what you get. But we don't know shit about fuck, babes. Not us, not 99% of doctors, not any of the health authorities who have been ignoring cfs as 'hysterical women' for decades whilst so many people had to live with it and the isolation and hopelessness it brings.
There are now millions of people with long covid in the USA alone. You DO NOT want this. Wash your hands, wear a mask, get boosters, avoid giant indoor or even outdoor crowds when you can.
if i got any of this information wrong - inevitable, pls link your data, me n my cog issues are laying down now ✌



(source)
51K notes
·
View notes
Text
Fellowship in Pediatric Endocrinology: Complete Guide

What is Pediatric Endocrinology?
Definition and ScopePediatric endocrinology focuses on diagnosing and treating hormonal disorders in children. These conditions can range from growth issues to metabolic and thyroid disorders.
Importance of Pediatric Endocrinology in Modern MedicineWith advancements in medicine, understanding pediatric endocrine health is vital for managing diseases that could affect a child’s growth and development long-term.
What is a Fellowship in Pediatric Endocrinology?
Overview of the Fellowship ProgramA pediatric endocrinology fellowship is an advanced training program designed to provide in-depth knowledge and clinical expertise in managing complex endocrine disorders in children.
Purpose of Specialized TrainingThis fellowship equips physicians with the skills needed to address specific hormonal challenges in pediatric populations, ensuring quality care and fostering innovation in treatment.
Eligibility Criteria for Pediatric Endocrinology Fellowships
Academic Qualifications RequiredApplicants typically need to complete a residency in pediatrics or internal medicine-pediatrics before applying.
Additional Prerequisites and CertificationsMany programs require certification from relevant boards, such as the American Board of Pediatrics.
Core Curriculum and Training Focus
Clinical TrainingFellows gain hands-on experience diagnosing and treating a variety of endocrine disorders, including diabetes and adrenal diseases.
Research OpportunitiesFellowships often include research components, enabling participants to contribute to advancements in pediatric endocrinology.
Hands-on Experience with Endocrine DisordersTrainees work directly with patients under the supervision of experienced endocrinologists, enhancing their clinical decision-making skills.
Duration and Structure of the Fellowship
Typical TimelineMost fellowships span three years, with a blend of clinical and research responsibilities.
Division of Clinical and Research ResponsibilitiesTime is divided between patient care, laboratory work, and academic learning, ensuring comprehensive training.
Benefits of Pursuing a Pediatric Endocrinology Fellowship
Enhanced Clinical ExpertiseThis program refines your ability to handle complex cases and improves diagnostic accuracy.
Career Advancement OpportunitiesGraduates often secure prestigious roles in hospitals, research institutions, and private practices.
Top Institutions Offering Pediatric Endocrinology Fellowships
Prestigious Programs in the USInstitutions like Harvard, Stanford, and Johns Hopkins offer renowned fellowships.
Internationally Recognized FellowshipsPrograms in countries like the UK and Canada also provide excellent training opportunities.
Steps to Apply for a Fellowship in Pediatric Endocrinology
Researching ProgramsExplore institutions that align with your career goals and interests.
Preparing Your ApplicationCraft a compelling personal statement and gather strong recommendation letters.
Interview ProcessEngage confidently during interviews, showcasing your passion and qualifications.
Challenges During the Fellowship
Balancing Clinical and Research DutiesMaintaining equilibrium between patient care and academic pursuits can be challenging.
Managing Stress and Time EffectivelyEffective time management and stress-relief strategies are key to success.
Financial Aspects of the Fellowship
Fellowship Stipends and BenefitsWhile stipends vary, many programs provide financial support and healthcare benefits.
Additional Financial Support OptionsGrants and scholarships can help supplement income during training.
Career Pathways Post-Fellowship
Working in Academic MedicineMany fellows transition to roles in teaching and research at medical schools.
Opportunities in Private PracticeOthers opt for private practice, offering specialized care to children with endocrine disorders.
Importance of Continuing Medical Education
Staying Updated on Medical AdvancesOngoing education ensures you remain knowledgeable about the latest treatments and technologies.
Networking and CollaborationAttending conferences and joining professional societies enhances your career and fosters professional connections.
Must Read:
Fellowship in clinical hematology complete guide
FAQs
What Makes a Program Stand Out?Programs with a strong balance of clinical and research opportunities tend to be highly regarded.
Can International Medical Graduates Apply?Yes, many institutions welcome international candidates, provided they meet the necessary criteria.
Are Research Opportunities Mandatory?While not always mandatory, research experience is highly valued.
What is the Scope of Practice Post-Fellowship?Fellows can work in academic settings, hospitals, or private practices, with opportunities to specialize further.How Can I Improve My Chances of Selection?Focus on strong academic performance, relevant research experience, and a well-crafted application.
1 note
·
View note
Text
Diabetes: Diagnosis and Treatment
Diagnostic Methods Blood Tests Glycated Hemoglobin (A1C) Test Measures average blood sugar over 2-3 months Diagnosis criteria: Below 5.7%: Normal 5.7% to 6.4%: Prediabetes 6.5% or higher: Diabetes Not reliable for pregnancy or certain blood disorders Fasting Blood Sugar Test Taken after overnight fast Results interpretation: Less than 100 mg/dL: Normal 100-125 mg/dL: Prediabetes 126 mg/dL…
0 notes
Text
Exploring the MD in General Medicine Program at GS Medical College & Hospital
Choosing a postgraduate specialization in medicine is one of the most significant decisions for aspiring doctors. Among the many options available, pursuing an MD in General Medicine stands out as a foundation for diverse career opportunities, clinical expertise, and advanced medical practice. When selecting the right institution for this journey, GS Medical College & Hospital, a top-ranked private medical college in Ghaziabad, Uttar Pradesh, emerges as an excellent choice.
In this article, we will delve into the scope of the MD in General Medicine program, its benefits, career opportunities, and why GS Medical College & Hospital should be your preferred destination for postgraduate medical education.

MD in General Medicine: A Comprehensive Overview:
An MD in General Medicine is a highly sought-after postgraduate medical degree that focuses on the diagnosis, treatment, and prevention of a wide range of adult health conditions. This program provides a solid foundation in internal medicine, enabling doctors to manage everything from common illnesses to complex and chronic diseases. It emphasizes clinical expertise, patient care, and the development of advanced diagnostic and therapeutic skills.
Key Features of the Program:
Program Duration: 3 years of intensive training.
Eligibility Criteria:
MBBS degree from a recognized institution.
Qualifying marks in NEET-PG or equivalent entrance examinations.
Core Areas of Study:
Chronic disease management.
Acute care and emergency medicine.
Preventive healthcare strategies.
Multidisciplinary approach to complex cases.
Benefits of Pursuing an MD in General Medicine:
Diverse Career Opportunities:
Clinical Practice: Work as a general physician, providing primary care and specialized consultations.
Academic Roles: Pursue teaching positions in medical colleges and institutions.
Research Opportunities: Engage in groundbreaking medical research to advance healthcare.
Healthcare Administration: Leadership roles in hospitals or health organizations.
Pathway to Super-Specializations:
Opens doors to advanced fields like:
Cardiology
Nephrology
Endocrinology
Gastroenterology
High Demand for Physicians:
The growing prevalence of chronic diseases such as diabetes, hypertension, and cardiovascular disorders has created a steady demand for skilled internal medicine specialists.
Ability to serve in diverse settings, including hospitals, private clinics, and rural healthcare facilities.
Why Choose GS Medical College & Hospital for MD in General Medicine?:
GS Medical College & Hospital is a premier destination for postgraduate medical education, offering a perfect blend of academic rigor, clinical exposure, and state-of-the-art infrastructure. Its MD in General Medicine program stands out for its emphasis on holistic learning, hands-on training, and fostering excellence in internal medicine.
Key Features of GS Medical College & Hospital:
State-of-the-Art Facilities:
Equipped with advanced diagnostic laboratories for in-depth clinical investigations.
Features cutting-edge technology, including imaging systems, ICU units, and simulation labs for practical training.
Modern medical wards designed to support efficient patient care and learning opportunities.
Highly Qualified Faculty:
A team of experienced professors and clinicians with expertise in diverse medical specialties.
Faculty members dedicated to mentoring students in academics, research, and clinical practice.
Regular guest lectures and workshops conducted by renowned medical professionals to broaden learning horizons.
Comprehensive Clinical Exposure:
Located in Ghaziabad, a densely populated area with a diverse patient demographic.
High patient inflow ensures exposure to various medical conditions, from common illnesses to rare disorders.
Opportunities to work in multidisciplinary teams, enhancing decision-making and collaboration skills.
Robust Research Opportunities:
A strong focus on medical research with access to institutional resources and funding.
Encouragement to present papers at national and international conferences.
Publication support for research findings in reputed medical journals.
Holistic Learning Environment:
A curriculum that combines theoretical knowledge, clinical skills, and ethical medical practice.
Supportive campus environment with a focus on personal and professional development.
Regular seminars, case studies, and community outreach programs to instill well-rounded medical expertise.
Opportunities for Networking and Growth:
Active participation in medical forums, workshops, and collaborative projects.
Alumni network providing career guidance and opportunities for specialization.
Why GS Medical College is an Ideal Choice:
By choosing GS Medical College & Hospital, students gain unparalleled exposure to advanced medical training, research-driven learning, and an inspiring academic atmosphere. The institution’s focus on fostering excellence ensures that graduates are well-prepared to lead in the field of internal medicine, making a meaningful difference in patient care and healthcare innovation.
How GS Medical College Stands Out Among Other Private Medical Colleges in Uttar Pradesh:
GS Medical College & Hospital is a Private Medical Colleges in UP for PG that excels in providing a unique blend of practical exposure, academic excellence, and holistic development. It stands apart from other private medical colleges in Uttar Pradesh for several reasons, offering an enriched educational experience that prepares students to excel in the medical field.
Comprehensive Clinical Exposure:
One of the key advantages of studying at GS Medical College is the hands-on experience provided to students through its multi-specialty hospital:
High Patient Inflow: The hospital serves a diverse population, offering students exposure to a wide variety of medical cases across different specialties.
Advanced Medical Technology: Students get to work with state-of-the-art medical equipment and cutting-edge diagnostic tools, enhancing their clinical skills.
Real-Time Experience: Students gain valuable exposure to managing both acute and chronic medical conditions, fostering critical thinking and decision-making.
Multi-Departmental Rotations: Clinical training spans various specialties, including cardiology, pulmonology, orthopedics, and more, ensuring a well-rounded medical education.
Emergency Care Experience: The college offers training in medical emergencies, preparing students to handle high-pressure situations effectively.
Affordable Fees with Quality Education:
GS Medical College is committed to making high-quality education accessible to aspiring medical professionals:
Competitive Fee Structure: The college offers affordable tuition fees without compromising on the quality of education, making it an attractive option for students from diverse backgrounds.
Quality Education: Despite being cost-effective, GS Medical College maintains a high standard of education, equipping students with the knowledge and skills needed to excel in the medical field.
Financial Aid Options: The institution also offers financial support to eligible students, making education even more accessible.
Affordable PG Medical Education: Among the best PG medical colleges in Ghaziabad, GS Medical College provides postgraduate education at rates comparable to other institutions, ensuring an excellent return on investment for students.
Collaborative Learning Environment:
GS Medical College promotes a dynamic, student-centric learning environment that fosters academic growth and personal development:
Regular Seminars and Workshops: The college organizes frequent seminars, workshops, and symposia, where students can engage with experts and learn about the latest advancements in medical science.
Inter-Departmental Discussions: Cross-departmental collaboration encourages interdisciplinary learning, allowing students to gain insights into diverse fields of medicine and develop a more holistic understanding.
Research Opportunities: Students are encouraged to engage in research projects, presenting their findings in academic forums, and contributing to the scientific community.
Peer-to-Peer Learning: A culture of collaborative learning allows students to share knowledge, discuss case studies, and learn from one another’s experiences, fostering a supportive academic environment.
Holistic Development and Student Support:
There are List of PG Medical Colleges in Uttar Pradesh 2025 particularly GS Medical College focuses on the overall development of its students:
Personalized Mentorship: Faculty members provide continuous guidance and mentorship, ensuring students stay on track with their academic and professional goals.
Extracurricular Activities: The college offers a range of sports, cultural events, and leadership opportunities to ensure students develop essential life skills outside the classroom.
Well-Being and Support: Counseling services and wellness programs are available to support the mental and emotional well-being of students, ensuring a balanced lifestyle.
With its unmatched clinical exposure, affordable fees, and collaborative learning environment, GS Medical College offers a comprehensive and enriching educational experience that sets it apart from other private medical colleges in Uttar Pradesh.
The curriculum of MD in General Medicine:
The MD in General Medicine program is meticulously designed to provide a deep understanding of internal medicine while equipping students with clinical, research, and diagnostic expertise. The curriculum is a blend of core subjects, hands-on clinical training, and research-oriented learning, ensuring a holistic approach to postgraduate medical education.
Core Subjects:
Students gain an in-depth understanding of various medical specialties, including:
Cardiology: Diagnosis and management of heart-related conditions.
Gastroenterology: Study of digestive system disorders and their treatments.
Pulmonology: Understanding respiratory diseases and advanced interventions.
Nephrology: Management of kidney-related conditions, including dialysis.
Endocrinology: Exploration of hormonal disorders and metabolic issues.
Rheumatology: Treatment of autoimmune and joint diseases.
Clinical Training:
Practical exposure is a cornerstone of the program, focusing on:
Hands-on patient care in outpatient and inpatient settings.
Comprehensive training in diagnosing and managing medical emergencies.
Proficiency in diagnostic and therapeutic procedures, such as ECG interpretation, lumbar punctures, and more.
Rotations across specialties to ensure exposure to diverse clinical scenarios.
Research and Thesis Work:
The program emphasizes research and academic contributions through:
Encouragement to undertake innovative research projects addressing contemporary medical challenges.
Development of a thesis under expert faculty guidance, contributing to medical literature.
Opportunities to present research at national and international conferences.
Career Opportunities after MD in General Medicine:
The versatility and comprehensive training provided by an MD in General Medicine open doors to numerous rewarding career paths across clinical, academic, and administrative fields. Graduates are well-equipped to excel in diverse roles, contributing significantly to healthcare delivery and advancements.
Clinical Practice:
Graduates can establish themselves as expert physicians, managing a variety of medical conditions in different healthcare settings:
Serve as a consultant physician in hospitals, clinics, or private practices.
Provide long-term management for chronic diseases like diabetes, hypertension, and cardiovascular disorders.
Work in multidisciplinary teams, addressing acute and complex medical cases.
Deliver patient-centric care, emphasizing preventive medicine and lifestyle management.
Super-Specialization:
An MD in General Medicine provides a strong foundation for pursuing further specialization:
Enroll in a DM (Doctorate of Medicine) program in fields like cardiology, nephrology, oncology, or critical care medicine.
Super-specialize to address specific medical challenges and advance expertise in focused areas.
Enhance career prospects with high-demand sub-specialties, contributing to cutting-edge healthcare innovations.
Academic Roles:
For those passionate about teaching and mentorship:
Join medical colleges as a professor, lecturer, or mentor to train future doctors.
Contribute to academic excellence by designing curricula and delivering impactful lectures.
Participate in research collaborations, promoting evidence-based medicine.
Research:
Graduates interested in scientific exploration can:
Work with research institutions or pharmaceutical companies to develop innovative therapies and medications.
Participate in clinical trials, contributing to the advancement of medical science.
Publish research findings in reputable journals, gaining global recognition.
Healthcare Administration:
For leadership-oriented individuals:
Take up roles in hospital management, optimizing healthcare delivery.
Contribute to public health programs, addressing healthcare disparities at the community or national level.
Lead initiatives for healthcare policy reforms and quality improvement.
With its broad scope and high demand, an MD in General Medicine ensures a fulfilling career with endless possibilities for growth and impact.
Advantages of Studying at GS Medical College:
The Best Medical PG Institutes in UP India like GS Medical College & Hospital is renowned for its exceptional academic standards, state-of-the-art infrastructure, and a holistic approach to medical education. Situated in the heart of Uttar Pradesh, the institution provides an enriching environment for aspiring postgraduates to excel in their careers and contribute meaningfully to the field of medicine.
Recognized Institution:
GS Medical College stands as a beacon of quality medical education:
Ranked among the top private medical colleges in Uttar Pradesh, attracting students from across the country.
Known for its high academic standards, producing skilled healthcare professionals.
Offers a strong reputation, enhancing graduates’ career prospects globally.
Affiliations and Accreditations:
The institution’s affiliations ensure credibility and recognition:
Affiliated with prestigious medical councils and universities, guaranteeing compliance with global standards of medical education.
Holds accreditations that provide international recognition for degrees awarded.
Regularly updated curriculum aligned with national medical education frameworks ensures relevance and quality.
State-of-the-Art Infrastructure:
The Top PG Medical Colleges in Uttar Pradesh like GS Medical College boasts modern facilities for advanced learning:
Well-equipped laboratories and cutting-edge medical equipment facilitate hands-on training.
A comprehensive library with digital and physical resources supports research and academic growth.
Advanced simulation labs and diagnostic centers enable practical exposure in a controlled environment.
Expert Faculty and Mentorship:
Students benefit from the guidance of a dedicated faculty team:
Experienced professors and clinicians with extensive expertise in their respective fields.
A focus on personalized mentorship, helping students navigate academic challenges.
Regular guest lectures and workshops by national and international experts, enriching the learning experience.
Comprehensive Clinical Exposure:
GS Medical College is attached to a fully functional hospital offering diverse clinical opportunities:
High patient inflow provides exposure to a wide variety of medical cases and emergencies.
Opportunities to participate in multidisciplinary care, preparing students for real-world healthcare settings.
Structured clinical rotations in various departments ensure well-rounded training.
Research and Innovation Opportunities:
The institution actively encourages academic exploration:
Support for student-led research projects, fostering innovation.
Opportunities to present findings at conferences and seminars, both nationally and internationally.
Access to resources for publication in reputable medical journals, enhancing professional credibility.
Supportive Community and Holistic Development:
GS Medical College ensures students thrive both academically and personally:
A student-centric approach fosters a sense of belonging and collaboration.
Extracurricular activities, including sports and cultural events, promote work-life balance.
Counseling services and wellness programs support students’ mental health and overall well-being.
By combining academic excellence with practical training and a nurturing environment, GS Medical College provides an ideal platform for medical aspirants to achieve their goals and contribute meaningfully to the healthcare sector.
Conclusion:
Pursuing an MD in General Medicine from GS Medical College & Hospital is not just about earning a degree; it’s about embarking on a journey of excellence, growth, and service. With its state-of-the-art facilities, expert faculty, and a commitment to holistic education, GS Medical College stands out as a top choice for postgraduate medical education in Uttar Pradesh.
Whether you aspire to excel in clinical practice, academia, or research, GS Medical College equips you with the knowledge, skills, and confidence to succeed in your chosen path. Take the first step towards a fulfilling medical career by choosing GS Medical College & Hospital, and let your journey of excellence begin.
#GeneralMedicine#BestMedicalCollegeForPG#TopMedicalCollege#Ghaziabad#GSMedicalCollege#Hapur#UttarPradesh#List of PG Medical Colleges in Uttar Pradesh 2024#Private Medical Colleges in UP for PG#Best Medical PG Institutes in UP India#Top PG Medical Colleges in Uttar Pradesh#Best PG Medical Colleges in Ghaziabad Uttar Pradesh#UP Private Medical College
0 notes