#cranial nerve disorder
Explore tagged Tumblr posts
Text
does anyone else with tongue weakness have issues biting your tongue? when my neurological issues "flare up" my tongue tends to stick to the side and gets really sore from constantly catching under my teeth. not really a full on bite just irritation from always being under my teeth. I have such a hard time keeping it in the center of my mouth
#cranial nerve disorder#cranial nerve palsy#facial paralysis#physical disability#physically disabled#neurological disability#cripple punk#cripplepunk#chronic illness#chronically ill#systemic lupus erythematosus
17 notes
·
View notes
Note
Hope this isn't offensive (feel free to ignore if it is) but what illnesses do you have? I always see very detailed posts from you about different types of hyperspecific injuries or illnesses and I was wondering if you're just super well informed or have all of them.
Which is very helpful and cool for people who need the info, and I'm sorry if you are experiencing all those.
Oh, Christ. Right this is going to be a lot 😅
Conditions I have been diagnosed with as of 2024:
Ehlers Danlos Syndrome
Mast Cell Activation Syndrome
Dysautonomia/POTS/autonomic failure (they all mean a similar thing. I just have them all listed in my file because no one can decide what I actually have beyond “nervous system broke”)
Chronic Migraines
Hemiplegic Migraines
Cluster Headaches
Cranial Instability (caused by my EDS + neck injuries)
Trigeminal neuralgia
Occipital Neuralgia (caused by the cranial instability)
Binocular Vision Disorder
PMDD (likely linked to the MCAS)
Probably endometriosis but it’s unconfirmed.
Interstitial cystitis (definitely caused by the MCAS)
GERD (a symptom of my MCAS)
Pernicious Anemia (likely linked to the EDS and MCAS. I don’t absorb nutrients from my food as well as I should which is common when MCAS damages the GI tract.) which lead to hemolytic anemia in 2019 aka the “Almost Died For Real” year.
ADHD.
cPTSD
Dysthymia or “double depression”
“Probable ME/CFS” is in my file, but with everything else going on chronic and debilitating fatigue is pretty much unavoidable so my doctors are like 🤷🤷♀️
I had an intestinal perforation a few years ago that lead to severe diverticulitis that took about a year and a half to heal, but that’s healed now save for the occasional bout of nerve pain.
Uuuh… I think that’s it… (wait and see my spouse/friends chiming in with “you forgot about x”)
So yeah.
Chances are if you see me talking about it, I have it. I do sometimes talk about other conditions that I’ve learned about over the years of navigating my own stuff, but I will always defer to the lived experiences of others when it comes to their own conditions.
It’s a lot to deal with. Most of it links back to the MCAS/EDS/Autonomic failure.
Or as we like to call it: the generic trifecta of bullshit.
2K notes
·
View notes
Text
Facial Differences that You Should Consider Representing in Your Writing More
[large text: Facial Differences that You Should Consider Representing in Your Writing More]
As it has been said many times on this blog before, facial differences are a very wide spectrum - there’s thousands of conditions that cause it, and they’re often extremely different from each other. It’s an incredibly diverse category almost by definition. But…
In books, movies, and our inbox, it seems that a traumatic battle scar is the only facial difference that exists. I find this rather frustrating because I would like to see the real life diversity to be actually considered by writers when creating characters - and that’s exactly what this post is for. I hope that by making people just aware of the myriad of options they have, I can help a bit.
This isn’t to say that you shouldn’t write characters with scars, it’s to say that there’s more for you to consider. Just like not every physically disabled person has hip dysplasia and not every neurodivergent person has epilepsy, not every person with a facial difference has scars.
Of course, this list isn’t exhaustive - no such list exists, it would be like “list of every disability ever”, it simply can’t be done. This is just a dozen random facial differences that I would like to see incorporated into characters more often.
Facial paralysis Exactly what the name implies. There are many types of facial paralysis - complete, partial, bilateral, unilateral, chronic, acute, and it can affect the whole face, or only part of it. Sometimes it can cause problems with speech or dry eyes (mostly the latter), but it’s frequently just primarily a visual difference. A person with facial paralysis might be completely unable to make facial expressions at all if it’s severe, or have a lop-sided smile and inability to raise an eyebrow or control an eyelid like me. Causes include cranial nerve damage (especially the 7th nerve, which is called facial palsy), Bell’s palsy, Möbius syndrome, or multiple sclerosis! It can be congenital, like in my case, or acquired, like in most cases - mostly due to stroke. Here I would write something about the current media representation being good, bad, or what tropes to look out for but I don’t know a single character with it. So :-)
Anotia/microtia Microtia is a congenital facial difference that affects the outer ear(s) - as the name implies, they’re smaller than average; anotia means a complete lack of them. This usually will also result in being d/Deaf or hard of hearing in that ear, as the ear canal can be smaller or closed (depending on the “grade”). People with microtia who decide on using hearing aids will usually wear a bone-anchored hearing aid, which looks very differently from the “regular” HA; it’s worn with a headband. Microtia can be the only facial difference that a person has, but it can also be a part of Goldenhar syndrome, Treacher Collins syndrome (mentioned below), or hemifacial microsomia.
Congenital Trochlear Nerve palsy I have a subtype of this, and because it happens to have the most boring name in existence I have never seen anyone talk about it, certainly not see a character with it. So; CNIV palsy (again, an incredibly catchy name) is a disorder of one of the very easy to damage nerves that allow eyes to move. It causes constant double vision, severe strabismus, and progressive facial asymmetry. A person with CNIV palsy will have a 24/7 head tilt to the side and will have their chin tucked in, which causes said asymmetry - facial features on the side of the tilt will sag down, the eye will “sunk” in, and because it’s congenital, the jaw can grow to be misaligned (like mine). Over time, it causes neck pain and kyphosis, so add chronic pain to that. Trochlear nerve palsy can be congenital, acquired, traumatic, and even extremely rarely genetic (that’s me, allegedly <1 in a million). However, most acquired cases are only temporary, and “fix themselves” with the passage of time. Again, I would love to write something about CNIV palsy representation, but I’m confident it literally doesn’t exist : )
Sturge-Weber syndrome The most visible part of SWS - that you might be familiar with - are port wine stains. In this syndrome, they tend to be large and generally cover the forehead-eye area. Around 15% of people with any kind of port wine stain on their face have Sturge-Weber syndrome, and even more when it comes to larger ones. Most people with SWS will have epilepsy since childhood, and many will develop glaucoma (which causes blindness) if the PWS is around that eye. Hemiparesis (one-sided weakness) can also sometimes happen on the opposite side of the PWS. Here is a short article about media representation from a person with SWS.
Cystic Hygroma Also known as lymphangioma, it is a bump that mostly happens on a person’s lower face and/or neck. It’s almost always congenital and a result of a blockage in the lymphatic system (thus lymphangioma). Sometimes, if it affects the mouth or jaw, it may cause a speech disability where the person’s speech might not be fully understandable, or cause an airway obstruction; this generally means that the person has to have a trach tube in their neck to breathe. Here is a short article about living and growing up with cystic hygroma by Atholl Mills.
Congenital melanocytic nevus A complicated name for a specific kind of birthmark. Melanocytic means related to melanin, so it’s a black or brown birthmark that can show up on any part of the body and be of almost any size. Sometimes it can be hairy as well. While CMN doesn’t usually cause any problems, people who have it can have a higher risk of skin cancer, epilepsy, and brain tumors (if it's on the head). Here is a short article on representation - among other things - by a person with CMN.
Ptosis Ptosis is actually really common - I can almost guarantee that you have seen someone with it - but for some reason it never shows up in media, unless it’s to show that a character is under the influence or vaguely creepy. Ptosis is simply a drooped eyelid. It’s caused by damage to the third cranial nerve, which can be congenital, acquired, traumatic, etc. It’s very common in myasthenia gravis and CHARGE syndrome. In most cases ptosis is a visual thing, but it can sometimes cause problems - for me, it partially obstructs my vision and for some people who acquired it later in life that can cause pain (due to having to constantly lift the eyebrow). Ptosis is often misunderstood, and people tend to make bizarre assumptions about those of us who have it - even Wikipedia cites “looking sinister” as a symptom (not that I particularly trust Wikipedia as a source, but it shows the general public’s view quite well). In real life, we are normal people and all these “drunk/high/rude/evil” associations aren’t true at all.
Treacher Collins syndrome You have probably seen a person with TCS at some point, as it’s not that rare. This is a genetic, congenital disability that affects the development of the face. The bones of the jaw and cheeks are underdeveloped, eyes have a downturned shape, and microtia/anotia is often present as well. A lot of people with Treacher Collins are d/Deaf or hard of hearing. Sometimes, the small jaw might cause problems with breathing, which is why a lot of people with TCS will have a permanent tracheostomy tube in their neck. Similar to ptosis, eyes in TCS are often seen as “looking sad”, but that’s an incorrect assumption - that’s just how they look like. The main and only big representation of TCS in media is that one awful movie from a few years ago, that was literally just inspiration porn featuring an able-bodied actor based on a shitty book, made by an author with some sort of abled-person guilt. Very cool, don’t do that.
Crouzon syndrome Crouzon syndrome is a type of craniosynostosis; a congenital condition where a person’s skull fuses too early. There are other disabilities that can look somewhat similar, like Pfeiffer or Apert syndrome, but they are different!. CS will affect the person's skull - it will be taller than usual, eyes - they will be large and bulging, midface - it's often smaller than average and can look sunk in comparison to the jaw and forehead, and more. Sometimes people with Crouzon syndrome are d/Deaf or hard of hearing (very common with craniofacial differences), or experience long term effects of hydrocephalus, which happens fairly often. Here is a short article by Mikaela Moody about movie representation - and her piece on how it to be trans while having a facial difference, which I relate to a lot and wanted to share.
Phthisis bulbi Phthisis bulbi is something that I have mentioned on this blog before, as it logistically should be represented way more often in fiction than it currently is. It's also known as the “end-stage eye” which is a metal name. This is an ocular difference that can result after trauma to the eye. It can also result from a million other things, but trauma is apparently the most common thing to happen to an eye in fiction. With phthisis bulbi, the eye shrinks, sinks, and everything inside becomes stiff; this is permanent, and the eye isn't functional anymore - it's blind and unable to move. The only treatment is to have the eye removed, especially if it causes pain. If you're writing a character who got a Hot Sexy Scar over their eye and still has that eye, they probably should have this (and yes, the “shrunk and sunk” part is mandatory, you can't just make the eye lighter and call it a day).
Frontonasal dysplasia Frontonasal dysplasia is a congenital facial difference that affects the structure of the face. While it's a spectrum with a lot of variety, most people with FND will have hypertelorism (eyes spread widely apart), a flat and broad nose, and a cleft going through the middle of the nose. Other facial clefts (not necessarily just cleft lip) are also common. Sometimes, someone with it can also have cranium bifidum (meaning a brain/meninges that protrude through the skull, similar to how spina bifida works), or intellectual disability related to the potential absence of corpus callosum. Rarely, limb differences can also be a part of it; absent tibia, extra toes, or clubfoot. Again, I’m unaware of any representation of FND outside of “scary birth deformity” on medical shows =)
Parry–Romberg syndrome PRS is also known as progressive hemifacial atrophy, which is a much more descriptive name. It’s an acquired facial difference that people just get for unknown reasons, mostly before the age of 20 and usually between 5 and 15. Generally, PRS is considered to be slowly-progressing, but this can vary pretty widely between different people. As the name implies, it causes atrophy in the face, which affects everything from skin to fat and muscles to sometimes even bones. Some people will also experience skin darkening, alopecia (hair loss), or trigeminal neuralgia (very severe nerve pain) on the atrophied side. The difference between the two sides can be very pronounced, with a visible line between the halves showing up on the forehead. Again, no existing rep that I know of =)
And as always, I recommend this short PDF that in my opinion any writer who wants to include a character with an FD has to read. Additionally, you can also check our #face difference tag, this primer on facial difference, or this piece on making sure you’re not contributing to disfiguremisia.
Also apologies for the amount of “idk what to say about already existing rep because it literally doesn’t exist” but I hope it illustrates the problem =)
Happy Face Equality Week,
mod Sasza
#mod sasza#face difference#disabled character ideas#writing guide#writing resources#writing advice#writing help#face equality week#long post
899 notes
·
View notes
Note
what do you think the babys thoughts on asmr are? like those cranial nerve exams, or better yet, cat asmr, where its like, its just asmr with a cat. people groom the cats and theyre purring with asmr sounds, etc. just in general!!
i think hed love it, and chuuya would be over the moon because its a perfect way to get the baby to calm down for the night and settle down before bed :D
also i saw this one video of a mom doing asmr on her baby, like lightly brushing her face and tracing her fingers and tapping gently and whispering, im totally imagining chuuya doing that to babyzai and him eating it all up like a plate of canned crab 🌚
i think babyzai would also love it because of autism/sensory processing disorder (ik some of the things youve written about him with his sensory issues are autism coded- idk if that was your intention but just in general even in canon i headcanon dazai to be autistic!) because soft and gentle sounds are the perfect stimulation to get dazais nervous system to calm down (also now that i think of it, it would probably would help with his ptsd/trauma symptoms with calming his nervous system!)
i ended up ranting my thoughts hahaha, but what do you think the babys (and subsequently chuuya) would think of it :3
Perhaps this is a biased answer because I’m an asmr lover, but I do think he would be calmed and relaxed by the visuals or the sounds! (I have too many projects I want to tackle and not enough time but I would love to try making asmr one day 😭🩷 sorry tangent but my favorite ASMRtist is ASMR Rebecca, she does a lot of focus games and asmr for adhd, and I think because she actually has adhd she really understands how the brain works. I’ve seen some ‘asmr for adhd’ vids where the clips of the triggers are just cut together weirdly and it’s very jarring, Rebecca does continuous shots and just lets her own adhd go crazy playing with objects, I absolutely recommend her if you haven’t seen her vids)
Holy shit the cat asmr vids, Dazai would especially like those!! I also think he would enjoy the kinds of asmr vids where people make different wax seals or play focus games, he wants something to entertain him he’s not as much of a fan of just slow scratching on the mic for slow scratching sake
As far as CHUUYA doing the relaxing motions, I’m absolutely a fan! I’ve actually got some scenes written in upcoming chapters with Chuuya just trying to help lull the baby to sleep with relaxing touches or little things to focus on. Absolutely the kind of attention and affection that Babyzai would love, he’d feel so safe and relaxed. He really likes one on one attention like that, I’ve never thought about it as doing asmr on someone but it describes it perfectly 🥺🩷
I can totally see then snuggling into bed together and watching some nice relaxing videos on Chuuya’s phone, or even late at night when Dazai can’t sleep (literally I was watching asmr at 330 am last night because I couldn’t fall back asleep 😭)
The fact that Dazai reads as autistic in the au really makes me happy 🩷 I’m not necessarily trying to make him autistic coded, I’m just trying to do what I feel is right for the story while also being ‘in character’ (which is such an oxymoron with agere fics, in canon Dazai would never cry and hold a stuffed animal so I’m already working at a disadvantage haha), but i am also a personal believer in autistic Dazai so 🩷🩷🩷🩷🩷🩷🩷
Thank you for the wonderful ask 🩷🩷🥺
22 notes
·
View notes
Text
PATIENT NAME: [Redacted] DOB: [Redacted] AGE: 12 years DATE OF ADMISSION: [Redacted] REFERRING PHYSICIAN: Dr. [Redacted] ATTENDING PHYSICIAN: Dr. [Redacted] REASON FOR CONSULTATION: Traumatic Brain Injury (TBI), Memory Impairment
HISTORY OF PRESENT ILLNESS (HPI):
The patient is a 12-year-old male presenting with symptoms secondary to blunt force head trauma sustained approximately [X] days ago. According to reports, the patient was struck on the left temporoparietal region, causing rapid deceleration against a hard surface (counter edge). There was a brief loss of consciousness (~30 seconds) followed by initial confusion and disorientation upon awakening.
Since the injury, the patient has exhibited the following symptoms:
Cognitive impairment: Inconsistent recall of events, with some memories accessible at certain times but absent at others.
Disorientation: Occasionally misidentifies time and place, particularly under stress or fatigue.
Episodic dissociative states: Rare occurrences where the patient temporarily reverts to earlier behavioral and cognitive states, suggesting a memory retrieval issue rather than psychogenic dissociation.
The patient has no known history of prior neurological conditions, learning disabilities, or psychiatric disorders. No current medication use.
EXAMINATION FINDINGS:
Neurological Examination:
Mental status: Alert but intermittently confused. Inconsistent recall of recent events.
Cranial nerves: No deficits noted.
Motor function: Normal tone and reflexes. No paresis.
Gait & Coordination: Mild postural instability noted.
Speech & Language: Intact, though slightly slowed when recalling specific information.
Neuropsychological Screening:
Impaired episodic memory and executive function.
Fluctuating orientation.
Increased reliance on procedural memory over declarative recall.
Neuroimaging (CT/MRI): Findings consistent with diffuse axonal injury (DAI) localized predominantly in the left temporoparietal region, with evidence of microhemorrages in the subcortical white matter. Minor hippocampal atrophy observed, which may contribute to episodic memory dysfunction and fragmented recall.
IMPRESSION:
The patient sustained a moderate traumatic brain injury (TBI) with clinical findings suggestive of:
Post-Traumatic Amnesia (PTA): Resulting in episodic memory deficits and inconsistent recall.
Post-Concussive Syndrome (PCS): Persistent cognitive disturbances, particularly affecting memory retrieval and orientation.
Possible Retrograde Memory Fragmentation: Periodic retrieval of older memories without full contextual awareness, leading to brief reversions to earlier cognitive states.
RECOMMENDATIONS:
Neurological follow-up: Repeat MRI in 6 months to assess for structural changes.
Cognitive rehabilitation therapy: To improve memory recall and adaptive strategies.
Behavioral assessment: To monitor potential cognitive shifts or further dissociative-like episodes.
Caregiver education: Close observation for worsening cognitive deficits, confusion, or personality changes.
PROGNOSIS & EXPECTED OUTCOME:
The patient’s neurological prognosis is cautiously optimistic. While some memory inconsistencies may improve over time, the presence of hippocampal involvement suggests that episodic memory deficits and occasional cognitive reversion may persist. Memory retrieval may remain context-dependent, with certain recollections accessible only under specific circumstances. Long-term cognitive adaptation is expected, but periodic assessments are recommended to monitor progression.
18 notes
·
View notes
Text
How Does The Brain Work?
The brain stands as a marvel of biological engineering, Composing of a multitude of bodily functions ranging from cognition and memory to emotions and sensory perception. Together with the spinal cord, it constitutes the central nervous system (CNS), the command center of the human body.
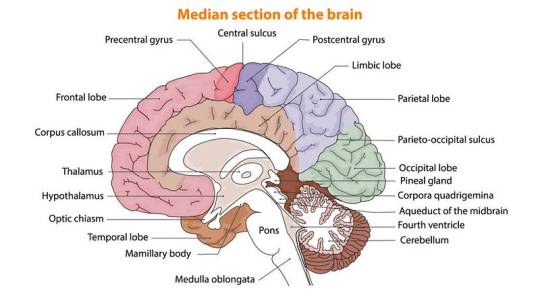
Composition of the Brain
Weighing approximately 3 pounds in adults, the brain’s main structure comprises about 60% fat, interspersed with water, protein, carbohydrates, and salts. Unlike muscles, it houses a complex network of blood vessels and nerves, including neurons and glial cells.
a) Gray and White Matter
Within the central nervous system, gray matter and white matter occupies distinct regions. In the brain, gray matter forms the outer layer, rich in neuron somas, while white matter constitutes the inner section, primarily composed of axons unsheathed in myelin. Conversely, in the spinal cord, this arrangement is reversed.
b) Brain Functionality
The brain operates by transmitting and receiving chemical and electrical signals throughout the body. These signals regulate a myriad of processes, with the brain disseminating each input. Some signals remain confined within the brain, while others traverse the spinal cord and nerves, disseminating information across the body’s expanse. This composes neural network relies on billions of interconnected neurons.
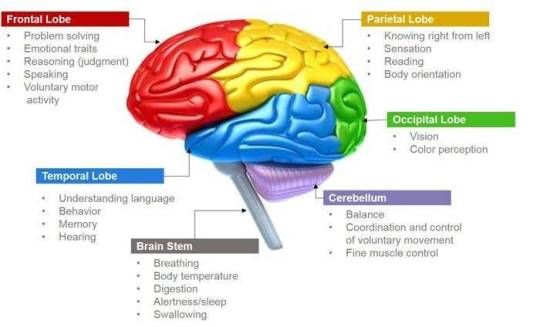
Major Brain Regions and Their Functions
1.Cerebrum
Dominating the brain’s landscape, the cerebrum encompasses the cerebral cortex and underlying white matter. It governs a spectrum of functions, including motor coordination, temperature regulation, language processing, emotional regulation, and sensory perception.
2. Brainstem
Serving as the bridge between the cerebrum and spinal cord, the brainstem comprises the midbrain, pons, and medulla. It regulates vital autonomic functions such as heart rate, breathing, and reflexive responses.
3. Cerebellum
Nestled at the posterior aspect of the brain, the cerebellum coordinates voluntary muscle movements, posture, balance, and motor learning.
Brain Coverings
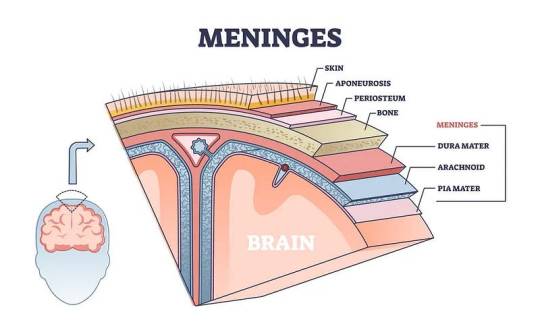
a) Meninges
Three layers of protective membranes, collectively known as meninges, enshroud the brain and spinal cord. These layers — dura mater, arachnoid mater, and pia mater — shield the delicate neural tissue from physical trauma and infection.
b) Lobes of the Brain
Each hemisphere of the brain comprises four lobes, each harboring distinct functional domains:
Frontal Lobe: Governing executive functions, motor control, and higher cognitive processes.
Parietal Lobe: Integrating sensory information, spatial awareness, and perception of pain and touch.
Occipital Lobe: Specialized for visual processing and perception.
Temporal Lobe: Involved in auditory processing, language comprehension, and memory consolidation.
Deeper Brain Structures
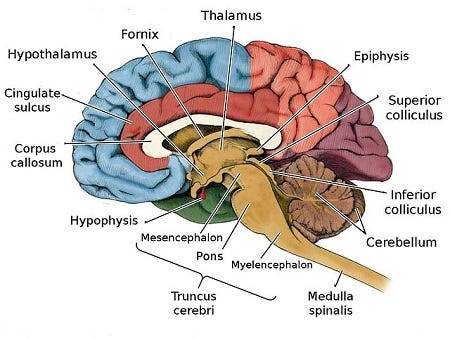
These encompass important structures such as the pituitary gland, hypothalamus, amygdala, hippocampus, and pineal gland, orchestrating hormone secretion, emotional regulation, memory consolidation, and circadian rhythms.
Blood Supply
The brain receives its oxygenated blood supply through the vertebral and carotid arteries, ensuring adequate perfusion of neural tissue. The main network of blood vessels, including the Circle of Willis, safeguards against ischemic insults and facilitates intraarterial communication.
Cranial Nerves
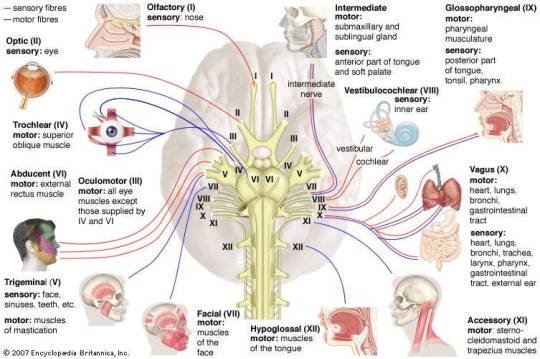
The twelve pairs of cranial nerves, originating from the brainstem, mediate a diverse array of sensory and motor functions, encompassing olfaction, vision, facial expression, and auditory perception.
Comprehending the anatomy and functionality of the brain fosters a deeper appreciation of its complexity and facilitates advances in neuroscientific research and therapeutic interventions aimed at diminishing neurological disorders.
Understanding the detailed anatomy and functionality of the brain is crucial for medical students embarking on their journey of study. Expert Academic Assignment Help offers invaluable assistance in navigating the complexities of neuroscience and related subjects. By leveraging expert guidance and support, students can excel in their medical education and contribute to advancements in the field of Medicine. Email us at [email protected] to embark on your path to scholarly excellence and professional competency.
#studying#studyblr#study blog#study aesthetic#student life#student#medical student#medical school#medicine#university student#university#university life#assignment help#medical students#nursing student#nursing school#healthcare#health and wellness#mental health#psychology#phd life#phd thesis writing service#online writing#do my online class#academic writing#essay writing#academic assignments#academia
15 notes
·
View notes
Text
The Causes of Facial Pain are Numerous by Siniša Franjić in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
One of the most difficult problems in modern medicine is facial pain. Sometimes an experienced doctor does not immediately recognize the symptoms and makes a misdiagnosis. The causes of facial pain are numerous. Therefore, the patient should be examined by physicians of several specializations.
Keywords
Facial Pain, Injuries, TN, TMD, CRS
Introduction
Facial pain occurring in the absence of trauma may be caused by a variety of disorders, many of which may be associated with referred pain, thereby making accurate localization of the source difficult [1]. For this reason, a careful examination of the face, orbits, eyes, oral and nasal cavities, auditory canals, and temporomandibular joints is an essential aspect of the evaluation of these patients.
Pain can result from many different disease processes [2]. The most common causes of facial pain are trauma, sinusitis, and dental disease. The history suggests the diagnosis, which is usually confirmed with the physical findings. With appropriate treatment and resolution of the disease, the pain also abates. Sometimes the cause of the pain is not apparent or the pain does not resolve with the other symptoms.
The trigeminal nerve (cranial nerve V) supplies sensation to the face. The first division (ophthalmic) supplies the forehead, eyebrows, and eyes. The second division (infraorbital) supplies the cheek, nose, and upper lip and gums. The third division (mandibular) supplies the ear, mouth, jaw, tongue, lower lip, and submandibular region. When pain is located in a very specific nerve distribution area, lesions involving that nerve must be considered. Tumors involving the nerve usually cause other symptoms, but pain may be the only complaint, and presence of a tumor at the base of the skull or in the face must be ruled out. When the work-up is negative, the diagnosis may be one of many types of neuralgia, which is a pain originating within the sensory nerve itself. Treatment is medical or, in some cases, surgical.
After immobilization, patients who are unconscious without respiratory effort require intubation to establish a functional airway, and this must be a first priority [3]. Laryngoscopically guided oral intubation is the technique of choice and must be undertaken without movement of the cervical spine; an assistant is essential in this regard and should remain at the patient’s head providing constant, in-line stabilization. Patients with inspiratory effort may be nasotracheally intubated provided that significant maxillofacial, perinasal, or basilar skull injuries are not present; when present or suspected, nasotracheal intubation is relatively contraindicated.
Facial pain remains a diagnostic and therapeutic challenge for both clinicians and patients [4]. In clinical practice, patients suffering from facial pain generally undergo multiple repeated consultations with different specialists and receive various treatments, including surgery. Many patients, as well as their primary care physicians, mistakenly attribute their pain as being due to rhinosinusitis when this is not the case. It is important to exclude non-sinus-related causes of facial pain before considering sinus surgery to avoid inappropriate treatment. Unfortunately, a significant proportion of patients have persistent facial pain after endoscopic sinus surgery (ESS) due to erroneous considerations on aetiology of facial pain by physicians. It should be taken into account that neurological and sinus diseases may share overlapping symptoms, but they frequently co-exist as comorbidities. The aim of this review was to clarify the diagnostic criteria of facial pain in order to improve discrimination between sinogenic and non-sinogenic facial pain and provide some clinical and diagnostic criteria that may help clinicians in addressing differential diagnosis.
History
Facial pain is pain localised to the face, and the diagnosis of facial pains has puzzled clinicians for centuries [5]. Some of the confusion is related to the delimitation of the facial structure and how pain is classified. The face is here defined as the part of the head that is limited by the hairline, by the front attachment of the ear and by the lower jaw, both the rear edge and the lower horizontal part of the jaw. The face also includes the oral and nasal cavity, the sinuses, the orbital cavity and the temporomandibular joint. Pain in the facial region can be classified in multiple ways, for example according to underlying pathology (malignant vs. non-malignant), the temporal course (acute vs. chronic), underlying pathophysiology (neuropathic, inflammatory or idiopathic), localisation (superficial vs. deep), the specific structure involved (the sinus joint, skin etc), and underlying etiology (infection, tumour etc). In some instances, the diagnosis of facial pain focuses on the involved structure, for example temporomandibular joint disorder, in other cases it is the underlying pathology (sinusitis), and in others it is the specific character of the pain that will dictate the diagnosis (e.g. trigeminal neuralgia).
A history of carious dentition in association with a gnawing, intolerable pain in the jaw or infraorbital region is seen in patients with gingival or dental abscesses [1]. Pressurelike pain or aching in the area of the frontal sinuses, supraorbital ridge, or infraorbital area in association with fever, nasal congestion, postnasal discharge, or a recent upper respiratory tract infection suggests acute or chronic sinusitis. Redness, swelling, and pain around the eye are suggestive of periorbital cellulitis. The rapid onset of parotid or submandibular area swelling and pain, often occurring in association with meals, is characteristic of obstruction of the salivary duct as a result of stone. Trigeminal neuralgia produces excruciating, lancinating facial pain that occurs in unexpected paroxysms, is initiated by the tactile stimulation of a “trigger point” or simply by chewing or smiling. Temporomandibular joint dysfunction produces pain related to chewing or jaw movement and is most commonly seen in women between the ages of 20 and 40 years; patients may have a history of recent injury to the jaw, recent dental work, or long-standing malocclusion. Facial paralysis associated with facial pain may be noted in patients with malignant parotid tumors. Dislocation of the temporomandibular joint causes sudden local pain and spasm and inability to close the mouth. Acute dystonic reactions to the phenothiazines and antipsychotic medications may closely simulate a number of otherwise perplexing facial and ocular presentations and must be considered. Acute suppurative parotitis usually occurs in the elderly or chronically debilitated patient and causes the rapid onset of fever, chills, and parotid swelling and pain, often involving the entire lateral face.
Injuries
Facial injuries are among the most common emergencies seen in an acute care setting [6]. They range from simple soft tissue lacerations to complex facial fractures with associated significant craniomaxillofacial injuries and soft tissue loss. The management of these injuries generally follows standard surgical management priorities but is rendered more complex by the nature of the numerous areas of overlap in management areas, such as airway, neurologic, ophthalmologic, and dental. Also, the significant psychological nature of injuries affecting the face and the resultant aftermath of scarring can have devastating and long-lasting consequences. Despite the fact that these injuries are exceedingly common, they are cared for by a large group of different specialists and as such have a remarkably heterogeneous presentation and diverse treatment schema. Nonetheless, guiding principles in the care of these injuries will provide the basis for the best possible outcomes. The following questions will guide general management and provide a framework for understanding the principles in the acute care of patients with facial injuries and trauma.
Despite the extremely common presentation of such injuries, there remains little standardization on repairing and then caring for the wounds or lacerations. There is great variation in the repair of lacerations as well as the different materials used to repair them. This is again because of the numerous different specialties involved in the care of the injuries and their desires to provide the best possible outcome with regard to scarring. Pediatricians, emergency department personnel, and surgeons may not all agree on the best modalities for repair. Placement as well as type of dressing are also controversial.
The timing of facial skin laceration closure is the same as that of any open wound. The presence of contaminating factors in the management of wound would generally not allow closure after six hours and would favor delayed closure. However, clinical practice is slightly more variable with facial lacerations because of the uniquely sensitive nature of facial scarring. Although we generally ascribe to experimental data regarding timing of closure, in practice the six-hour rule is often overlooked with an attempt to be vigorous in cleaning the wound. The presence of exceptionally rich blood supply in the face is also deemed of benefit in extending the six-hour rule.
TN
Facial pain, for all its rarity, can be a significant cause of morbidity when present [7]. The two types of non-odontological causes of facial pain that appear to be the most likely to be mistaken one for the other are trigeminal neuralgia (TN) and what used to be called atypical facial pain, but that is now called persistent idiopathic facial pain (PIFP). Confusion between causes of facial pain persists despite the fact that the diagnosis of classical TN should be rather straightforward and not present diagnostic difficulties to the trained clinician. (The term classical TN is generally restricted to TN caused by neurovascular compression.) The caveat is that secondary causes of TN need to be considered, and the cause of classical TN needs to be established for reasons that will be discussed later. A common mistake that should not be made is to treat TN medically without establishing the cause. PIFP, on the other hand, is a diagnostic problem that confronts us head on. Clearly stated guidelines are in fact ambiguous. Descriptive terms include dull, poorly defined, non-localized.
Individuals in whom attacks of pain last minutes to hours, or are persistent or chronic, waxing and waning over the course of the day, or in whom pain extends beyond one division of the trigeminal nerve, may still be mistakenly diagnosed as having trigeminal neuralgia. Such individuals may point to one side of the face as the site of their pain or may indicate that pain is bilateral. Their pain may be further atypical in lacking the usual triggers of pain such as brushing teeth or touching a trigger area. Such pain that is atypical for TN is a different kind of facial pain than classical TN. However, even in cases that are not characteristic trigeminal neuralgia, chewing, and even speaking, for example, may be triggers. Chewing and speaking activate orofacial and neck muscles, and are accompanied by small movements at the cervical–cranial junction. Nociceptive sites in these muscles may be activated by chewing or speaking. Patients with atypical facial pain are unlikely to have trigeminal neuralgia, and more likely to have what is now called persistent idiopathic facial pain (PIFP).
The diagnosis of classical TN is made on the basis of a characteristic history of lightning-like sharp, electrical pain that is felt in one division of the trigeminal nerve, leaving a dull after pain that lasts for a variable, usually short, period of time. There is often a trigger, but there does not need to be one. The attacks are typically infrequent at first, but become more frequent with the passage of time, and may increase in frequency to occur hundreds of times a day. Remissions occur, but relapses become more frequent with aging. There is no dullness or loss of feeling reported. Some patients tell atypical stories in which pain crosses divisions of the trigeminal nerve, or paroxysms of pain last longer than lightning attacks of pain. The neurological examination is normal in classical TN. Motor and sensory examination of the face in particular is normal in classical TN, but is useful in identifying secondary trigeminal nerve dysfunction that could lead to a diagnosis of secondary TN or trigeminal neuropathy. The same is true of the blink and other trigeminal reflex tests, as the presence or absence of an abnormal result does not affect the diagnosis of TN, but may indicate a need to examine for causes of secondary TN.
TMD
Painful temporomandibular disorder (TMD) is the most frequent form of chronic orofacial pain, affecting an estimated 11.5 million US adults with annual incidence of 3.5%. As with several other types of chronic, musculoskeletal pain, the symptoms are not sufficiently explained by clinical findings such as injury, inflammation, or other proximate cause [8]. Moreover, studies consistently report that TMD symptoms exhibit significant statistical overlap with other chronic pain conditions, suggesting the existence of common etiologic pathways. Most studies of overlap with orofacial pain have focused on selected pain conditions, classified according to clinical criteria (eg, headaches, cervical spine dysfunction, and fibromyalgia), location of self-reported pain (eg, back, chest, stomach, and head), or the number of comorbid pain conditions. Although there is a long tradition of depicting overlap between pain conditions qualitatively using Venn diagrams, we know of few studies that have quantified the degree of overlap between TMD and pain at multiple locations throughout the body.
Overlap of pain symptoms can occur when there are common etiologic factors contributing to each of the overlapping pain conditions. One example is diabetes that contributes, etiologically, to neuropathy in the feet and retinopathy in the eye, thereby creating overlap, statistically, of diseases at opposite ends of the body. The etiologic factor most widely cited to account for overlap of pain conditions is central sensitization, defined as “amplification of neural signaling within the central nervous system (CNS) that elicits pain hypersensitivity.” The amplification means that otherwise innocuous sensations are perceived as painful (ie, allodynia) and that formerly mildly painful stimuli now evoke severe pain (ie, hyperalgesia). However, somatosensory afferent inputs into the CNS are segmentally organized, making it plausible that sensitization is not uniform throughout the neuraxis.
Regardless of pain location, overlap creates serious problems for patients, adding to the suffering and disability caused by a single pain condition, and potentially complicating diagnosis and treatment for one or all of the overlapping conditions. This has broader implications for patients with multiple chronic illnesses who have poorer health outcomes and generate significantly greater health care costs than patients with a single illness. Thus, the aim of this epidemiological study was to quantify the degree of overlap between facial pain and pain reported elsewhere in the body.
CRS
Unfortunately, little is known of the underlying mechanisms that produce pain associated with CRS (chronic rhinosinusitis), but several mechanisms that may all contribute to some degree to the manifestation of facial pain in CRS have been postulated [9]. It has been hypothesized that occlusion of the osteomeatal complex may lead to gas resorption of the sinuses with painful negative pressures, yet most subjects with CRS have an open osteomeatal complex. Patients’ observations that pain and pressure is postural may reflect painful dilatation of vessels; however, postural pain is also observed in subjects with simply tension type headache. Local inflammatory mediators can excite nerves locally within the sinonasal mucosa directly illiciting pain. For example, maxillary rhinosinusitis can cause dental pain through the stimulation of the trigeminal nerve. In addition, local tissue destruction and inflammatory mediators may influence the central mechanism of pain via immune-to-brain communication through afferent autonomic neuronal transmission, transport across the blood brain barrier through the circumventricular organs and/or direct passage across the blood brain barrier.
The impact of inflammatory cytokines on the central nervous system have been associated with both pain as well as other health-related factors associated with chronic inflammation and sickness behavior such as disruption of sleep and mood. Interleukin-1[Beta] (IL-1[Beta]) and tumor necrosis factor-[alpha] (TNF-[alpha]) are two key pro-inflammatory cytokines with a pivotal role in the immune-to-brain pathway of communication. They are both upregulated in subjects with CRS and are two potential pro-inflammatory cytokines that have been implicated in fatigue, sleep dysfunction, depression, and pain. Characterizing the differential cytokine profiles of CRS subtypes and identifying associated symptom profiles may be an important step in understanding why some subjects experience greater health-related burden of disease, which is an important predictor of electing surgical intervention over continued medical therapy.
Examination
Carious dentition, gingivitis, and gingival abscesses may be diagnosed by inspection of the oral cavity and face [1]. Percussion tenderness over the involved tooth, swelling and erythema of the involved side of the face, and fever may be noted in patients with deep abscesses. Percussion tenderness to palpation or pain over the frontal or maxillary sinuses with decreased transillumination of these structures suggests sinusitis. Redness, tenderness, and swelling around the eye may suggest periorbital cellulitis. Pain with eye movement or exophthalmos may suggest an orbital cellulitis or abscess. Malocclusion may be noted in patients with temporomandibular joint dysfunction; tenderness on palpation of the temporomandibular joint, often best demonstrated anteriorly in the external auditory canal with the mouth open, is noted as well. Patients with temporomandibular joint dislocation present with anxiety, local pain, and inability to close the mouth. Unusual ocular, lingual, pharyngeal, or neck symptoms should suggest possible acute dystonic reactions. A swollen, tender parotid gland may be seen in patients with acute parotitis, in parotid duct obstruction secondary to stone or stricture, and in patients with malignant parotid tumors; evidence of facial paralysis should be sought in these latter patients. Palpation of the parotid duct along the inner midwall of the cheek will occasionally reveal a nodular structure consistent with a salivary duct stone. In patients with herpes zoster, typical lesions may be noted in a characteristic dermatomal pattern along the first, second, or third division of the trigeminal nerve or in the external auditory canal. It is important to remember that patients with herpes zoster may have severe pain before the development of any cutaneous signs. This diagnosis should always be considered when vague or otherwise undefinable facial pain syndromes are described. Simple erythema may be the first cutaneous manifestation of herpetic illness. Patients with trigeminal neuralgia have an essentially normal examination.
Ventilation
In patients with inspiratory effort but without adequate ventilation, mechanical obstruction of the upper airway should be suspected and must be quickly reversed [3]. The pharynx and upper airway must be immediately examined and any foreign material removed either manually or by suction. Such material may include blood, other secretions, dental fragments, and foreign body or gastric contents, and a rigid suction device or forceps is most effective for its removal. Obstruction of the airway related to massive swelling, hematoma, or gross distortion of the anatomy should be noted as well, because a surgical procedure may then be required to establish an airway. In addition, airway obstruction related to posterior movement of the tongue is extremely common in lethargic or obtunded patients and is again easily reversible. In this setting, insertion of an oral or a nasopharyngeal airway, simple manual chin elevation, or the so-called jaw thrust, singly or in combination, may result in complete opening of the airway and may obviate the need for more aggressive means of upper airway management. Chin elevation and jaw thrust simply involve the manual upward or anterior displacement of the mandible in such a way that airway patency is enhanced. Not uncommonly, insertion of the oral airway or laryngeal mask airway may cause vomiting or gagging in semialert patients; when noted, the oral airway should be removed and chin elevation, the jaw thrust, or the placement of a nasopharyngeal airway undertaken. If unsuccessful, patients with inadequate oxygenation require rapid sequence oral, or nasotracheal, intubation immediately.
If an airway has not been obtained by one of these techniques, Ambu-bag–assisted ventilation using 100% oxygen should proceed while cricothyrotomy, by needle or incision, is undertaken rapidly. In children younger than 12 years, surgical cricothyrotomy is relatively contraindicated and needle cricothyrotomy (using a 14-gauge needle placed through the cricothyroid membrane), followed by positive pressure insufflation, is indicated. During the procedure, or should the procedure be unsuccessful, Ambu-bag–assisted ventilation with 100% oxygen and an oral or a nasal airway may provide adequate oxygenation.
In addition, rapidly correctable medical disorders that may cause central nervous system and respiratory depression must be immediately considered in all patients and may, in fact, have precipitated the injury by interfering with consciousness. In all patients with abnormalities of mental status, but particularly in those with ventilatory insufficiency requiring emergent intervention, blood should immediately be obtained for glucose and toxic screening, and the physician should then prophylactically treat hypoglycemia with 50 mL of 50% D/W, opiate overdose with naloxone (0.4–2.0 mg), and Wernicke encephalopathy with thiamine (100 mg). All medications should be administered sequentially and rapidly by intravenous injection and any improvement in mental status or respiratory function carefully noted. Should sufficient improvement occur, other more aggressive means of airway management might be unnecessary.
Conclusion
Facial pain can be painful and frightening. Facial pain can be caused by a cold, sinusitis, muscle tension in the jaw or neck, dental problems, nerve irritation or trauma. One of the most common causes is sinusitis, but another common cause is jaw dysfunction which often occurs after trauma and can lead to jaw injury or meniscus irritation. In the case of major trauma, fractures of the jawbone or fractures of the face may also occur.
#Facial Pain#Injuries#TN#TMD#CRS#jcrmhs#Journal of Clinical Case Reports Medical Images and Health Sciences impact factor
3 notes
·
View notes
Text
Cranial Nerve Conditions and Diagnosis

The cranial nerves are 12 pairs of nerves that emerge from the brain and are responsible for providing motor and sensory functions. They are among the most delicate nerves in the human nervous system and require experts who specialize in their normal and abnormal presentations.
Cranial nerve issues can affect a motor nerve, called cranial nerve palsy, or affect a sensory nerve, causing pain or diminished sensation. Individuals with a cranial nerve disorder may suffer from symptoms that include intense pain, vertigo, hearing loss, weakness or paralysis. These disorders can also affect smell, taste, facial expression, speech, swallowing, and muscles of the neck.
3 notes
·
View notes
Text
Day 60/100
📚 studied at a coffee shop, took notes on cranial nerves, pain disorders, and opioids, took quiz on skull landmarks
☀️ leg day at gym
💕 went to a market with my husband, called my grandma and my childhood friend on the phone
🫧 scrubbed bathroom
#self improvement#growth#self healing#mindset#journal#self love#studyblr#that girl#100 days of productivity#med student
5 notes
·
View notes
Text
Traumatic Brain Injury in Children Traumatic brain injury (TBI) has been one of the primary public health problems under health concerns over several decades. Health statistics reveal that this problem has been common among the male adolescents, as well as the young adults under the age bracket of 15 to 24 years. Similarly, this disorder is common among the elderly people of both sexes under the age of 75 and above. However, this paper is of high concern about children of ages 5 and below, or 5 to 18 years, who are at high risk of traumatic brain injuries. TBI is among the leading causes of death and acquired disabilities among infants and children. Traumatic brain injury is an acquired injury to an individual's brain resulting from an external physical force exerted on the head, leading to partial or total disability and/or psychological impairment. This scenario may adversely impact on a child's educational performance. This term TBI does not apply to degenerative or congenital brain injuries, or any induced brain injuries during birth trauma. It applies to any closed or open head injury that results to impairments on any body part (Fenwick, Manly, Anderson & Robertson, 2012). Such impairments may relate to language, cognition, memory, reasoning, attention, judgment, abstract thinking, speech, problem solving, sensory and motor abilities, physical performance, and psycho-social behavior of a child. TBI can thereby change how a child acts, moves, thinks and performs in the course of learning. Motor vehicle accidents, falls, and playing with risky objects are the common contributing factors for unintentional causes while child abuse and assaults during infancy, young age, and adolescence ages are the ill-fated causes of TBI. Many research and health institutions thereby focus on limiting the primary brain injuries and minimizing the secondary brain injuries (Lazar & Menaldino, 2009). Today, many health institutions, understand the importance of a healthy brain and its traumatic responses. However, health research institutions still have much to do in order to understand the treatment and how to reverse the damage that results from head injuries (Porr, 2012). Whereas the symptoms of brain injuries among the children may be similar to those experienced by the adults, the impact may be very different in terms of functionality (Povlishock & Christman, 2003). This is because the brains of children continuously develop as opposed to those of adults. In the past, people had an assumption that children with brain injuries would recover quicker and better than the adults due to the "plasticity" in younger brains. This cliche is no longer functional. The most recent health researches on brain injuries reveal that brain injuries in children has more devastating effects than brain injuries of similar severity within the mature adults. The perceptive impairment symptoms on children may take longer to appear, but may be apparent as the child grows into adult age. Lazar and Menaldino (2009) affirmed that such delayed impacts may lead to lifetime challenges on physical performance, learning, as well as the social life. The greatest challenge facing lots of children with brain injuries involve changes in formal social behaviors, and the ability to think and learn. Mutual deficits upon brain injury may include impaired judgment, difficulty in reasoning and processing information. In adults, these deficits may become apparent just in months after the brain injury. On the contrary, the injury deficits may take years to become apparent, after which the impact advances to be so treacherous. At the time of damage incidence, the child may only show cranial fractures, contusions, cranial nerve injuries, intracranial or extra-parenchymal hematomas, and edema (Povlishock & Christman, 2003). Hematoma is damage to the blood vessel in the head region. After the head injury, cerebral damage may become secondary to the injury complications or primary to the trauma. The secondary damages encompass the subsequent insults after the impact or insults during the process of emergency medical interventions. The primary cerebral damage commonly becomes permanent; however, both of the damage types may result into limitations of body functional outcomes (Lazar & Menaldino, 2009). Most of the primary focal injuries are temporary and frontal amongst children. A clinician may use a computer tomography scan after an injury in order to predict the degree and types of the subsequent functional limitations. Using the magnetic resonance imaging of the corpus callosum and brainstem, the clinician can identify the diffuse axonal injuries (DAI). These injuries are as a result of shearing forces during the time of impact and may also result into augmented intracranial pressure, edema and denervation hypersensitivity (Povlishock & Christman, 2003). A child's brain tissues develop differently as compared developments within adults' brain hence; young children and infants are always vulnerable damages caused by the secondary trauma. The complications involved in secondary trauma include cerebral edema, cerebral swelling, hematomas and vasospasm, which subsequently result into increased hypoxia, hypotension, ischemia, and increased intracranial pressure. Immediately after the traumatic period, pressure necrosis, infarction, and herniation may occur. According to Hall and Cope (2007), damages from such secondary complications are more diffuse in children than in adults and may resolve during the rehabilitation and recovery period of a child. According to Lehmkuhl, High and Boake (2008), it is commonly advisable for parents of children recovering from traumatic brain injury to refer their children to rehabilitation services of any kind. In adolescent children with TBI, the most commonly observed, functional limitations are in the areas of speech, vision, self-feeding, hearing, dressing, bathing, walking, behavior, and cognition (Hall & Cope, 2007). During childhood, traumatic brain injury may have long-term effects on psychosocial and cognitive functioning; including unsatisfactory academic achievements resulting from significant deficits in the child's working memory. TBI may exhibit a wide range of both physical and psychological symptoms. As in adults, the signs and symptoms among children may be moderate, mild, or severe, depending on the magnitude of the brain damage. Some of these symptoms may be apparent immediately upon the traumatic event, whereas other signs and symptoms may become apparent days, weeks, months, or years later. A child with a mild traumatic brain injury may experience loss of consciousness or remain conscious over a given duration. In both children and adults, the mild traumatic brain injury may exhibit symptoms such as confusion, headache, dizziness, tired eyes, blurred vision, loss of appetite, fatigue, mood swings, change in sleeping patterns, and troubles with thinking, attention, memory and concentration. Nonetheless, young children and infants may lack appropriate communication skills to report some of these feelings, such as sensory problems, headaches, and confusion. Most of the TBI's signs and symptoms will thereby be apparent through observations and visualization (Lehmkuhl et. al., 2008). Some of these observable symptoms include change in nursing and eating habits, easy or unusual irritability, persistent crying, inability to pay attention, depressed moods, change in sleeping habits, and loss of interest in activities or favorite toys. These signs and symptoms may vary depending on the injured part of the brain and the level of severity. Children who are capable of communicating and expressing their feelings and ideas are at a higher position of exposing the signs and symptoms of the TBI. According to Jennings and Blaskey (2013), they can show their physical disabilities hearing, speaking, seeing, and using other senses. They can communicate their feelings of headache and fatigue. When walking, parents, health doctors, or any other person can be able to see their difficulties in movement due to a paralyzed body or body part. Following the brain injuries, it is general that the child's ability to utilize their brain will change drastically (Kinsella, Prior & Sawyer, 2006). The child may have problems with the short-term memory (the ability to remember from one minute to another). Similarly, the child may suffer from trouble of long-term memory (the ability to recollect information from a while ago). Kinsella et al. (2006) assert that these memory troubles may lead to forgetfulness of what the teacher just taught in class or the facts learnt from the previous lessons. The child will always be able to focus attention just within a short time or completely losses concentration, either at home or in class. Children with TBI will always experience social troubles when interacting with fellow children since they commonly undergo sudden changes in anxiety, moods, and depression. They may laugh or cry a lot, lack control over their emotions, and sometimes become restless. It is thereby essential to understand that during growth and development of a child, both teachers and parents may be able to notice the child's problems. This is because they both have high expectations on these children to use their brains in developing new skills and useful knowledge. However, it may be challenging for parents and educators to notice some of the problems related to TBI at earlier stages. The problems can then develop gradually to affect the child in learning and to develop such new skills (Fenwick, et al., 2012). One of the most common but minor type of traumatic brain injury is the concussion. Technically, concussion is short-term loss of consciousness as a result of head injury. After an injury, a child may lose consciousness, seem dazed, or have a seizure. The symptoms occur immediately after the concussion and even some few days or weeks later. Concussion symptoms may be hard to notice since some children may act to be fine even if they are in traumatic brain troubles. During diagnosis of concussion, a child's caregiver may check the child's eyes, memory, strength of the child's arms, and legs. Jennings and Blaskey (2013) elicit that this check (neurologic exam) may be sufficient to tell the caregiver how well the child's brain works. Similarly, an X-ray of the child's neck and the head may help in checking extra injuries. Porr (2012) affirms that upon complete examination, TBI doctors commonly issue instructions on a child's medications on the traumatic brain injury. Ibuprofen and/or acetaminophen are the commonly recommended medicines given to reduce a child's pain from TBI. Use of ice on the child's head for 15 to 20 minutes; two hours a day may help in reducing pain and swelling of the child's head, as well as preventing further tissue damages (Fenwick, et al., 2012). After concussion, a child may take a rest on the bed or play quietly if one has to do so. Activity restriction is another method for managing a child's TBI conditions and symptoms (Jennings & Blaskey, 2013). The child may be restricted from playing or involving in activities that may lead to a blow on the head. In conclusion, traumatic brain injury is one of the leading causes of acquired disability during childhood. Therefore, parents, clinician, educators should be aware of the potential damages to a child's brain; both immediate and late symptoms on a child. It is thereby recommended that the government, in compliance with the health sectors should encourage education for families and specialists about the impending challenges of TBI on children. This should cut across from moderate to mild injuries on a child's brain. Through this education, both parents and educators will be able to acquire knowledge on how to tackle the traumatic brain injuries on children; its preventions, treatment, and symptom management. References Fenwick, T., Manly, T., Anderson, V. & Robertson, I. (2012). Attentional skills following traumatic brain injury in childhood: A componential analysis. Journal of Brain Injuries, 57(12), 237 -- 249. Hall, K., & Cope, D. (2007). The benefit of rehabilitation in traumatic brain injury: A literature review. Journal of Head Trauma Rehabilitation, 26 (10), 1 -- 13. Jennings, M. & Blaskey, J.(2013). Traumatic brain injury: Decision making in pediatric neurologic physical therapy. New York, NY: Churchill Livingstone. Kinsella, G., Prior, M. & Sawyer, M. (2006). Indicators and predictors of academic outcomes in children two years following traumatic brain injury. Journal of the International Neuropsychological Society, 8(3), 108 -- 116. Lazar, M.R., & Menaldino, S. (2009). Cognitive outcome and behavioral adjustment in children following traumatic brain injury: A developmental perspective. Journal of Head Trauma Rehabilitation, 14(10), 55 -- 63. Lehmkuhl, L.D., High, W.M. & Boake, C. (2008). Critical analysis of studies evaluating the effectiveness of rehabilitation after traumatic brain injury. Journal of Head Trauma Rehabilitation, 103(10), 14 -- 26. Porr, S. (2012). Children with traumatic brain injury; pediatric therapy: A systems approach. Philadelphia F.A. Davis. Povlishock, J. & Christman, C. (2003). The pathobiology of traumaticallyinduced axonal injury in animals and humans: A review of currentthoughts. Journal of Neurotrauma, 74(12) https://www.paperdue.com/customer/paper/traumatic-brain-injury-in-children-125641#:~:text=Logout-,TraumaticBrainInjuryinChildren,-Length6pages, Read the full article
0 notes
Text
The Era of Precision Medicine in Minimally Invasive Maxillofacial Surgery
The Collision of Minimally Invasive Techniques with Maxillofacial Surgery
The so-called minimally invasive surgery refers to the advanced surgical mode in which modern photoelectric imaging system, micro-surgical device and energy generation equipment, replace traditional open operation with endoscopic technology, and precision controlled surgical instruments with traditional scalpel to complete the diagnosis and treatment of lesions through tiny wounds.
Maxillofacial surgery is an important branch of oral medicine for the surgical treatment of cranial and maxillofacial facial bones, soft tissues and temporomandibular joints.
According to the surgical symptoms and treatment purpose can be divided into the following categories:
1. Trauma Repair Surgery
Treatment range: facial fracture
Typical surgery: open reduction and internal fixation of the fracture
2. Orthognathic Surgery
Treatment range: jaw development deformity
Typical surgical method: type Le Fort I osteotomy, lost split osteotomy
3. Tumor Resection and Reconstructive Surgery
Treatment range: jaw bone cystic lesions, benign and malignant tumors
Typical surgical method: lesion enlargement resection combined with vascularized free tissue flap grafting
4. Temporomandibular Joint Surgery
Treatment scope: joint ankylosis, structural disorder
Typical surgical methods: joint disc reduction, joint molding
Important structures such as trigeminal nerve branches, facial nerve and external carotid artery are centrally distributed in the maxillofacial area. Traditional surgery is easy to cause nerve damage and vascular bleeding. At the same time, the incision scar formed after the traditional surgery is more obvious, while the minimally invasive technology can realize the incision concealment and non-trace healing. Therefore, the application of minimally invasive techniques is important for maxillofacial surgery.

Application of Micro Power Tools in Minimally Invasive Maxillofacial Surgery
1. Bone Cutting and Plastic Surgery:
Zygomatic and Mandibular Plastic Surgery: Micro bone drills and bone saws can be used to precisely cut bones and reshape bone contours through oral or small skin incisions, avoiding scars and nerve damage caused by traditional large incisions
Fracture Reduction and Fixation: In complex fractures such as zygomatic arch and mandible, micro power tools can finely polish the bone surface, assist in reduction, and cooperate with micro titanium plate fixation to reduce intraoperative bleeding
2. Neurodecompression Technique: For facial nerve compression (such as Bell's palsy), micro drills can be used with endoscopic assistance to remove bone (such as temporal bone) that compresses the nerve, avoiding damage to surrounding soft tissues
3. Dental Implantation and Bone Augmentation:
Preparation of Implant Cavity: Micro implant drill bit (diameter can be less than 2mm) reduces bone thermal damage and improves initial stability of the implant by accurately controlling the speed and torque
Bone Augmentation Surgery: used in bone splitting or bone compression surgery to increase bone mass while preserving autogenous bone activity, promoting bone regeneration
4. Endoscopic Assisted Surgery:
Temporomandibular Joint (TMJ) Surgery: Through endoscopic channels, micro power tools can clean joint cavity adhesions, repair joint discs, or grind bone spurs to improve joint function
Salivary Gland Stone Extraction: Micro drills are used to crush stones in the submandibular gland or parotid duct, avoiding gland resection
5. Tumor Resection and Biopsy:
Removal of Jaw Cysts and Small Tumors: Through minimally invasive approaches, precise removal of lesions and preservation of surrounding healthy bone tissue are achieved, reducing the risk of postoperative deformities

Advantage of Minimally Invasive Techniques
1. Clinical Advantage of Functional Recovery
2. Multi-dimensional Improvement in Patient Benefit
Physiological Level: the blood loss was <50ml (traditional surgery> 200ml), and the hospital stay was reduced to 1-3 days (traditional 5-7 days)
Psychological Level: the wound is invisible, and the recovery time of social activities is 2-3 times earlier
Economic Benefits: reduced cost of comprehensive treatment
3. Innovation at the Operational Level
Improved visualization ability
Operation accuracy breakthrough
Contrast Dimensions
Traditional Surgery
Minimally Invasive Surgery
Bone Healing Time
Six to eight weeks after surgery
4-5 weeks after surgery (Piezosurgery promotes osteocyte activity)
The Occlusal Function Restore
Six weeks after surgery
2-3 weeks after surgery (Precise reduction reduces error)
Opening Training Starts
Four weeks after surgery
1 week after surgery (Arthroscopic techniquereduces adhesions)
Complex surgery simplified
With the continuous innovation of technology, minimally invasive maxillofacial surgery will continue to develop in the direction of precision, personalization and intelligence, to provide safer and more effective treatment plans for patients.
0 notes
Note
hey how do u feel about the cranial nerve exam asmr trend, i had no idea cranial nerve issues were even a real thing until recently, thought it was a fake thing asmrtists made up 🤦🤦
I'll be honest I did not know this was a thing before this ask
cranial nerve exams are a real thing done by neurologists to look for cranial nerve disorders. they're not very well known so I don't blame you for not being aware of them. you've probably heard of a couple, you just probably didn't know they were cranial nerve disorders (Bell's palsy and trigeminal neuralgia being the most known cranial nerve disorders)
7 notes
·
View notes
Text
MCQ on Cranial Nerves Test your knowledge of the cranial nerves with this multiple-choice question. Understand their functions, anatomical pathways, and clinical relevance in diagnosing neurological disorders. How well do you know the key cranial nerves and their roles in sensory and motor control?
0 notes
Note
Hi, do you have any good resources explaining common types of facial differences (preferably with pictures)? I already have a character with a port wine birthmark, but I want to incorporate a variety of facial differences in my body of work.
Hey! I'm glad you're interested in learning more about facial differences :) (smile) Especially with having more than one character.
My main recommendation would be "Types Of Visible Difference" by ChangingFaces. You can read it here. There are other pages linked there (the "see our page on X") that break specific types of facial differences further with pictures and/or descriptions, either way giving you basic information on what to google search for further research. A big category that this page is missing are facial differences caused by chromosomal conditions, which are extremely common (for example Down Syndrome).
There is also "Defining Facial Differences" by AboutFace that has way more entries, but there are no photos and it has a lot of medical language. If you're just looking for ideas it can be great to just read the little blurb written about the condition and then search for actual pictures if that's something you're looking for. It also allows you to filter for congenital and acquired conditions which is pretty cool (and also see that a huge portion of facial differences is congenital).
The third (worst) option is just going through Wikipedia pages in the "skin-related conditions" or "craniofacial syndromes" categories, but a lot of these are very rare/obscure and a lot of them don't have images attached. The first two options are much better in my opinion, but it's still something.
My personal recommendations for common but unrepresented facial differences to incorporate would be craniofacial conditions (e.g., Treacher Collins or Apert Syndromes), chromosomal disorders (e.g., Wolf–Hirschhorn or Down Syndromes), cranial nerve diseases (they're mostly just differentiated by numbers unfortunately, but there's a couple of them), and cancers of the head and/or neck. It would be nice to see them shown more, especially in a positive light.
I hope this helps,
mod Sasza
#capripian#mod Sasza#face difference#writeblr#writing resources#writing advice#writing disabled characters#art reference#disabled character ideas
591 notes
·
View notes
Text
Neuro-Ophthalmology Explained: When Eye Problems Are Linked to the Brain
Did you know that not all vision problems originate in the eyes? Some eye conditions are actually linked to the brain and nervous system, requiring specialized care from a neuro-ophthalmologist.
At Dr. Dudhabhate Netralaya & Retina Centre (DNRC), Pune, our Neuro-Ophthalmology Department specializes in diagnosing and treating complex vision issues related to the brain, optic nerve, and nervous system.

🔹 What Is Neuro-Ophthalmology?
Neuro-ophthalmology is a super-specialty of ophthalmology and neurology that deals with visual disorders caused by brain and nerve conditions. These include problems with the optic nerve, eye movements, and brain processing of vision.
🔍 Common Neuro-Ophthalmic Disorders Treated at DNRC
1️⃣ Optic Nerve Disorders
🔹 Optic Neuritis — Inflammation of the optic nerve, often linked to multiple sclerosis (MS). 🔹 Ischemic Optic Neuropathy — Reduced blood flow to the optic nerve, leading to vision loss. 🔹 Optic Disc Swelling (Papilledema) — Swelling due to increased pressure inside the skull.
2️⃣ Double Vision (Diplopia) & Eye Movement Disorders
🔹 Cranial Nerve Palsies — Nerve damage affecting eye movement. 🔹 Myasthenia Gravis — A neuromuscular disorder causing droopy eyelids & double vision. 🔹 Nystagmus — Uncontrolled, repetitive eye movements affecting vision stability.
3️⃣ Visual Field Defects & Brain-Related Vision Issues
🔹 Stroke-Related Vision Loss — Partial vision loss due to a stroke. 🔹 Brain Tumors Affecting Vision — Tumors pressing on the optic pathways, leading to vision problems. 🔹 Migraine-Associated Vision Disturbances — Temporary vision loss or flashes of light due to migraines.
🩺 How DNRC Diagnoses Neuro-Ophthalmic Conditions
At DNRC, Pune, we use advanced diagnostic tools to identify and treat neuro-ophthalmic conditions early.
✔ Optical Coherence Tomography (OCT) — High-resolution imaging of the optic nerve. ✔ Visual Field Testing — Detects blind spots caused by optic nerve or brain issues. ✔ MRI & CT Scans — Brain imaging to identify neurological causes of vision loss. ✔ Electrophysiology Tests (VEP, ERG) — Measures how the optic nerve & brain respond to visual stimuli.
✅ Treatment Options for Neuro-Ophthalmic Disorders at DNRC
🔹 Medications & Injections — For conditions like optic neuritis & myasthenia gravis. 🔹 Vision Therapy & Rehabilitation — To improve eye coordination & visual processing. 🔹 Surgical Treatments — For droopy eyelids (ptosis), eye misalignment, and tumor-related vision issues. 🔹 Multidisciplinary Approach — Coordination with neurologists, neurosurgeons, and endocrinologists for holistic treatment.
🔹 When Should You See a Neuro-Ophthalmologist?
👁 Sudden Vision Loss or Blurry Vision 👁 Double Vision or Difficulty Moving the Eyes 👁 Drooping Eyelids (Ptosis) 👁 Frequent Headaches with Visual Symptoms 👁 Unexplained Blind Spots or Tunnel Vision
If you experience any of these symptoms, consult a neuro-ophthalmologist immediately.
📍 Get Expert Neuro-Ophthalmic Care at DNRC, Pune
🔹 State-of-the-Art Diagnostics & Treatments 🔹 Expert Team of Neuro-Ophthalmologists & Neurologists 🔹 Comprehensive Care for Complex Eye-Brain Conditions
0 notes
Text
What Are Some Ways to Fix Squint?
Squint, medically known as strabismus, is a condition in which the eyes do not align properly. One eye may look straight ahead while the other eye turns inward, outward, upward, or downward. This condition can affect people of all ages, but it is most common in children. While squint may seem like a cosmetic issue, it can lead to vision problems if not treated early.
At GS Hospital, recognized as one of the Top Eye Hospitals in UP, patients receive comprehensive care for squint and other eye conditions. With a team of the Top Eye Hospitals in Hapur, the hospital provides advanced treatment options to help patients achieve proper eye alignment and improve their quality of life.

Understanding Squint:
What is Squint (Strabismus)?:
Squinting occurs when the muscles controlling eye movement do not work properly. This misalignment can affect depth perception and lead to double vision, lazy eye (amblyopia), or other visual challenges.
1. Esotropia – Inward Turning of the Eye:
Description: In esotropia, one or both eyes turn inward toward the nose, creating a "cross-eyed" appearance.
Common in: Children, often congenital or developing in early childhood.
Subtypes:
Congenital Esotropia: Appears in infants before six months of age.
Accommodative Esotropia: Caused by severe farsightedness (hyperopia) and excessive focusing effort.
Non-Accommodative Esotropia: Occurs independently of focusing issues and may be linked to neurological conditions.
Symptoms:
Double vision (diplopia).
Eye strain or fatigue.
Decreased depth perception.
2. Exotropia – Outward Turning of the Eye:
Description: In exotropia, one or both eyes drift outward, often noticed when focusing on distant objects or during moments of fatigue.
Common in: Both children and adults, with symptoms often becoming more noticeable over time.
Subtypes:
Intermittent Exotropia: Misalignment occurs occasionally, often triggered by stress or tiredness.
Constant Exotropia: Persistent outward turning of the eye.
Symptoms:
Squinting or closing one eye in bright sunlight.
Blurred or double vision.
Difficulty maintaining focus on close objects.
3. Hypertropia – Upward Turning of One Eye:
Description: Hypertropia occurs when one eye is misaligned upward while the other remains properly aligned.
Causes:
Congenital muscle imbalances.
Paralysis of the muscles controlling vertical movement.
Trauma or neurological disorders.
Symptoms:
Vertical double vision.
Tilting of the head to compensate for the misalignment.
Headaches due to strain on the neck and eye muscles.
4. Hypotropia – Downward Turning of One Eye:
Description: In hypotropia, one eye is positioned lower than the other, disrupting alignment and binocular vision.
Causes:
Congenital factors.
Nerve palsy, especially involving the fourth cranial nerve.
Trauma or injury to the eye muscles.
Symptoms:
Vertical misalignment of vision.
Difficulty in perceiving three-dimensional images.
Tilting the head upward to improve vision.
5. Intermittent Squint – Occasional Misalignment:
Description: In this type, the misalignment of the eyes occurs sporadically, often under specific conditions like stress, fatigue, or illness.
Characteristics:
The alignment of the eyes appears normal most of the time.
Episodes of misalignment may increase in frequency if untreated.
Triggers:
Illness or physical exhaustion.
Emotional stress or anxiety.
Exposure to bright light or focusing on distant objects.
Symptoms:
Squinting or closing one eye during episodes.
Difficulty maintaining focus during tasks.
Headaches or eye strain.
Comprehensive Analysis: Causes of Squint (Strabismus):
1. Congenital Causes – Present at Birth:
Some squint cases are congenital, meaning they are present from birth or develop in infancy. These cases are often linked to improper development of the eye muscles or related structures.
Key Features:
Occurs in infants under six months of age.
Often linked to genetic factors or developmental anomalies in utero.
Associated with conditions like congenital esotropia, where one or both eyes turn inward.
Contributing Factors:
Premature birth, which may lead to incomplete eye muscle development.
Low birth weight, increasing the risk of developmental complications.
Congenital syndromes such as Down syndrome or Goldenhar syndrome.
Signs:
Noticeable misalignment of the eyes soon after birth.
Poor tracking of objects or difficulty focusing.
2. Refractive Errors – Vision Problems:
Uncorrected vision issues, such as nearsightedness (myopia), farsightedness (hyperopia), or astigmatism, can strain the eye muscles, leading to squint.
How Refractive Errors Cause Squint:
In children with severe farsightedness, the eyes must work harder to focus, causing one or both eyes to turn inward (accommodative esotropia).
Persistent eye strain from uncorrected vision issues disrupts muscle coordination.
Common Symptoms:
Blurred vision or difficulty reading or focusing on distant objects.
Complaints of headaches or eye strain after visual tasks.
Prevention:
Early vision screening and corrective lenses can prevent squint associated with refractive errors.
3. Neurological Conditions – Brain or Nerve Dysfunction:
The brain and cranial nerves play a vital role in coordinating eye movements. Disorders affecting these systems can result in squint.
Examples of Neurological Causes:
Cerebral Palsy: Impaired muscle coordination affects the eyes, causing misalignment.
Stroke: Damage to the brain can weaken the muscles controlling the eyes.
Cranial Nerve Palsies: Paralysis of the third, fourth, or sixth cranial nerves disrupts normal eye movement.
Brain Tumors: Growths pressing on the nerves or muscles controlling eye movement can lead to squint.
Symptoms to Watch For:
Sudden onset of squint in adults.
Accompanying symptoms like dizziness, headaches, or difficulty walking.
Double vision or loss of peripheral vision.
4. Eye Injuries or Surgery – Trauma-Induced Squint:
Trauma to the eye or surrounding muscles can cause squint by damaging the structures responsible for eye alignment.
Types of Trauma:
Blunt Injuries: Physical impacts can displace or weaken eye muscles.
Penetrating Injuries: Damage to nerves or muscles inside the eye socket can cause permanent misalignment.
Surgical Complications: Procedures involving the eyes or brain may unintentionally affect eye muscle function.
Common Scenarios:
Sports-related injuries.
Car accidents or falls leading to head trauma.
Post-surgical complications following cataract or retinal surgery.
Prevention:
Wearing protective eyewear during high-risk activities.
Prompt medical attention for any eye injury.
5. Hereditary Factors – Genetic Predisposition:
A family history of squint significantly increases the likelihood of developing the condition.
Genetic Links:
Squint often runs in families, suggesting a hereditary component.
Genetic disorders like Marfan syndrome or Ehlers-Danlos syndrome may contribute to squint by affecting connective tissues and muscles.
How It Manifests:
Children with a parent or sibling with squint are more likely to develop the condition.
May combine with other risk factors like refractive errors or congenital abnormalities.
Symptoms of Squint (Strabismus):
1. Visible Eye Misalignment:
The most apparent symptom of squint is when one or both eyes are not aligned properly. This misalignment can occur in various forms:
Esotropia: One or both eyes turn inward.
Exotropia: One or both eyes turn outward.
Hypertropia: One eye turns upward.
Hypotropia: One eye turns downward.
Intermittent Squint: Misalignment occurs only at specific times, such as when tired or stressed.
2. Double Vision (Diplopia):
Patients may experience seeing two images of a single object. This occurs when the brain receives conflicting signals from the misaligned eyes. Common in adults with sudden-onset squint. Children may not report double vision because their brain suppresses input from the misaligned eye, leading to lazy eye (amblyopia).
3. Difficulty Focusing:
Squint can interfere with the ability to maintain clear vision. This may manifest as:
Difficulty focusing on objects, especially at close range.
Trouble maintaining concentration during reading or visual tasks.
Challenges in school performance for children.
4. Head Tilting or Turning:
Many individuals with squint tilt or turn their head to compensate for the misalignment. This adjustment helps to:
Improve vision clarity.
Reduce double vision.
Align the eyes temporarily for specific tasks.
5. Eye Strain or Fatigue:
The extra effort required to correct or compensate for misaligned eyes often leads to discomfort, particularly after prolonged use of the eyes.
Symptoms include aching or tired eyes.
Increased strain during activities requiring focus, like reading or watching screens.
6. Blurred Vision:
Squint can cause blurry vision, resulting from:
Improper focus due to eye misalignment.
Suppression of the visual input from the weaker or misaligned eye.
7. Additional Symptoms in Children:
Poor Depth Perception: Difficulty judging distances or recognizing three-dimensional objects.
Clumsiness: Frequently bumping into objects due to impaired spatial awareness.
Frequent Eye Rubbing: Indicative of discomfort or visual strain.
Diagnosis of Squint (Strabismus):
Diagnostic Methods:
· Visual Acuity Test: Determines how well each eye can see.
· Cover Test: Checks for eye movement and alignment issues.
· Refraction Test: Identifies refractive errors contributing to the squint.
· Eye Muscle Test: Evaluates the function and coordination of eye muscles.
· Imaging Tests: MRI or CT scans may be used to rule out underlying neurological causes.
Effective Ways to Fix Squint (Strabismus):
Non-Surgical Treatment Options:
1. Glasses or Contact Lenses:
Correcting refractive errors is one of the most common and effective treatments for squint, particularly in children.
How It Works: Properly prescribed lenses reduce strain on the eye muscles, allowing them to align better.
When It’s Effective: Ideal for cases where squint is caused by farsightedness or other refractive errors.
Additional Benefits: Regular use can prevent the development of amblyopia (lazy eye).
2. Eye Patches:
Eye patch therapy is a tried-and-true method for strengthening the weaker eye, especially in children.
How It Works: The stronger eye is covered, forcing the weaker eye to work harder.
Duration of Use: Worn for a few hours daily over weeks or months, depending on the severity.
When It’s Effective: Primarily for children with amblyopia caused by squint.
3. Vision Therapy:
Vision therapy involves structured exercises aimed at improving the coordination and strength of eye muscles.
How It Works: Conducted under the guidance of an eye specialist using specialized equipment or exercises.
Key Exercises: Pencil push-ups, focusing activities, and stereoscopic vision tasks.
When It’s Effective: Best for intermittent squints or minor misalignments.
4. Prism Lenses:
Prism lenses are an advanced optical solution for correcting eye alignment.
How It Works: These lenses bend light entering the eye, compensating for misalignment.
When It’s Effective: Ideal for individuals with double vision or mild squints.
Additional Benefits: Reduces eye strain and improves visual comfort.
Surgical Treatment Options
5. Strabismus Surgery:
Surgery is a widely used option for moderate to severe squint cases.
How It Works: Involves adjusting the length or position of the eye muscles to achieve proper alignment.
Types of Surgery:
Muscle Tightening (Resection): Strengthens a weak muscle by shortening it.
Muscle Loosening (Recession): Relaxes a tight muscle by repositioning it further back on the eye.
Post-Surgery Care: Includes eye drops, medications, and follow-up visits to monitor recovery.
6. Adjustable Sutures:
A modern surgical technique that allows fine-tuning of muscle adjustments after the operation.
How It Works: Surgeons use adjustable sutures to achieve precise alignment based on postoperative results.
When It’s Effective: Particularly beneficial for adult patients.
Advanced Treatment Options:
7. Botox Injections:
Botulinum toxin injections can temporarily weaken overactive eye muscles.
How It Works: Reduces muscle pull, allowing the eyes to align.
Duration of Effectiveness: Results last for 3–6 months, making it suitable for short-term correction.
When It’s Effective: Used for adults or as a trial before surgery.
8. Orthoptic Exercises:
A tailored program focusing on strengthening eye muscles and improving coordination.
Key Techniques:
Focusing on moving objects.
Alternating focus between near and far objects.
Synchronization exercises for binocular vision.
When It’s Effective: Ideal for treating intermittent squints or as part of postoperative rehabilitation.
Lifestyle and Supportive Measures:
9. Regular Eye Checkups:
Routine eye exams are crucial for tracking progress and making necessary adjustments to the treatment plan.
Frequency: Recommended every 6–12 months, depending on the severity and type of squint.
Key Benefits: Ensures early detection of complications and timely intervention.
10. Parental Guidance for Children:
For children with squint, consistent parental involvement is essential.
Tips for Parents:
Ensure compliance with glasses or patching therapy.
Encourage participation in vision exercises.
Monitor for signs of discomfort or vision changes.
11. Nutritional Support:
Maintaining a balanced diet supports overall eye health.
Essential Nutrients:
Vitamin A: Found in carrots, sweet potatoes, and leafy greens.
Omega-3 Fatty Acids: Found in fish, walnuts, and flaxseeds.
Antioxidants: Found in berries, citrus fruits, and green tea.
Conclusion:
Though often perceived as a minor issue, squint can significantly impact vision and quality of life if left untreated. Understanding its causes, symptoms, and treatment options is essential for making informed decisions. The Best Eye Hospital in Ghaziabad like GS Hospital, patients receive a tailored treatment plan designed to restore normal vision, improve eye alignment, and enhance their overall quality of life. At GS Hospital, recognized as the Best Eye Care Centre in Ghaziabad UP, patients receive world-class care from diagnosis to recovery. Whether it’s glasses, vision therapy, or surgery, the hospital’s expert team ensures optimal outcomes for every patient.
#Top Eye Hospitals in UP#Best Eye Care Centre in Ghaziabad UP#Best Eye Hospital in Ghaziabad UP#Best Ophthalmologist in Ghaziabad#Top Eye Hospitals in Hapur
0 notes