#causes Hypospadias
Text
Intersex Support FAQ
1. What is intersex?
Intersex is an umbrella term that describes people who have variations in sex characteristics that fall outside of the sex binary. This includes variations in genitals, internal reproductive organs like testes and ovaries, chromosomes, secondary sex characteristics, and/or the way that your body produces or responds to hormones. Some examples of intersex variations include AIS, CAH, PCOS, Klinefelters, hypospadias, and more.
The three main factors that define intersex variations are:
Variation in sex characteristics
The variation falls outside of the sex binary and is different from what is considered typical “male” or “female” development. These variations in traits might often be stigmatized and discriminated against for being outside of the sex binary.
This variation is either present from birth or develops spontaneously later in life. It is not caused by transitioning or by something temporary like a medication side effect, tumor, or other medical diagnosis.
(This definition is inspired by InterACT).
2. Does ____ count as intersex?
There are around 40 different intersex variations that are currently known. InterACT”s intersex variation glossary lists out those intersex variations and gives a brief description of each one.
However, we know that isn’t a complete list. People have intersex variations that haven’t been medically researched yet, or might have a rare variation that the intersex community isn’t aware of yet.
There are also some variations that might seem on the border between perisex and intersex. Some types of hormonal or reproductive diagnoses might not have a clear answer on whether they’re intersex or not.
Ultimately, intersex is a social/political identity rather than a strictly medical one. Increased research and changing social attitudes can cause the definition of intersex to expand over time. Regardless of whether someone has a confirmed intersex variation or an “intersex adjacent” diagnosis, if intersex resources are helpful to you, we hope that you continue to use them and act in solidarity with the intersex community.
On this blog, we do include PCOS with hyperandrogenism as part of the intersex community. Check out our PCOS tag for more posts about our reasoning, and PCOS specific resources.
3. Am I intersex?
We cannot diagnose you with an intersex variation over the internet. We can share resources such as the intersex variations glossary, share tips for navigating the medical system, and share information on other non-clinical signs of being intersex.
Some questions to ask yourself that can help you start the process of intersex discovery:
What do my sex traits (genitalia, secondary sex characteristics, hormone levels, etc) look like? Does this seem like it lines up with the “typical” descriptions of those sex traits?
Do I have any information about my birth? Were there any complications? Did doctors do extra testing at birth? Did doctors take me away from my parents for long periods of time? Did it take me longer to have my sex assigned at birth?
What was puberty like for me? Did I have early or late puberty? Did I have to go on hormones to start puberty? Did I have any variations in puberty, such as unexpected breast growth, irregular periods, or other changes? Did I go through puberty at all?
If you’ve tried to have children, are you infertile or struggling with fertility?
Did I have any unexplained surgeries or medical procedures as a child? Was I ever told I had to have organs removed and was told it was because of a cancer risk? Did I have to be on specific medications or hormones throughout my childhood? Did I have to go see a doctor more frequently? Did I go to an endocrinologist or pediatric urologist as a child?
Do I have surgery scars or scar tissue? Do I have more frequent UTIs than typical?
Do I have access to my medical records? Is there records of hormone panels, ultrasounds, physical exams, surgeries, or other medical procedures?
This kind of information can help you start to piece together if you think you might have an intersex variation, or if you think your intersex variation was hidden from you.
If you’re sending in an ask trying to figure out if your symptoms line up with a specific intersex variation, please share as much information as you’re comfortable with so that we can answer with the most helpful resources.
4. Can I self diagnose as intersex?
It’s complicated! Intersex is different from other LGBTQIA identities, in that it’s not only about self determination, but also about our embodied experience in a very specific way. In order to be intersex, you have to have an intersex variation. And there are many intersex variations that can only be confirmed through medical testing, so it’s not something that is easy to self-diagnose.
However, we recognize that the medical system is expensive, discriminatory, and often actively hides information about people’s intersex variations from them. (it wasn’t even until 2006 that the AAP stopped recommending that doctors lie to their patients about intersex status, so many intersex adults were born before that policy change!) Considering all that we know about intersex oppression, curative violence, and medical abuse, it feels incredibly cruel to tell people that they have to force themself through that system in order to seek answers.
So, we understand that there are ways of finding out that you are intersex without having a specific, confirmed, medical diagnosis. Many of us might find out that we’re intersex because we realize that our genitalia visibly looks different, and we can tell that we are intersex, even if we don’t know our specific diagnosis. Others might find out that we’re intersex because of strange discrepancies in our medical record. We might find out through discovering surgery scars on our body. We might go through puberty and realize that we’re developing in an atypical way to our peers. We might do a lot of research into intersex variations and have a pretty good guess into what variation lines up with our experiences. We might have some test results that help us understand we have intersex traits, even if we don’t know our specific diagnosis.
Before self diagnosing, we think it’s important to do thorough research into intersex variations, so that you truly understand what intersex means, what intersex variations exist, and understand how that information applies to yourself. It’s also important to be considerate of how we interact in community spaces, and respect other intersex people's boundaries as you engage in a questioning or diagnosis process.
5. Are intersex people trans?
Some intersex people are trans, and some aren’t. Most intersex people are still assigned a gender at birth, and many intersex people who are raised as one gender and then later identify as another gender identify with the label trans. Intersex people can be cis or trans just like any other group of people.
Many intersex people have complicated relationships with gender, and don’t feel like labels like cis or trans really fit their experiences. For this reason, terms like intergender and ipsogender were coined.
6. Are intersex people LGBTQIA?
It’s complicated! The “I” in LGBTQIA stands for intersex. Intersex history is intertwined with other parts of queer history. For example, the very first protest for intersex people in the United States was organized by Hermaphrodites with Attitude and Transexual Menace. There are intersex inclusive versions of community pride flags. Many intersex people view their intersex identity as a queer identity. Intersex oppression overlaps in many ways with homophobia and transphobia.
However, not all intersex people think that intersex should be included in the LGBTQIA community. Sometimes this is for bigoted reasons, with intersex radfems who use this stance as a way to be transphobic. But there are also intersex people who think that the “I” should only be included in the acronym when intersex people are actually meaningfully being included in queer spaces and resources. Many of us feel frustrated when people put “LGBTQIA” on a resource but then don’t actually have any intersex specific information in those resources.
In general, this is an ongoing intracommunity discussion where we don’t have a consensus.
7. Are intersex people disabled?
It’s complicated! Intersex is an umbrella term for many different experiences, and there is not one universal intersex experience. Some intersex people identify as disabled. Some intersex people do not.
Many intersex variations do cause disabling impacts in our bodies and lives. Some intersex variations are comorbid with other health conditions. Other intersex people become disabled because of violent normalizing interventions we’ve survived, such as forced surgery or other types of medical abuse.
Intersex people are also impacted by many of the same structures of oppression that harm disabled people. Both intersex people and disabled people are harmed by ableism. Both intersex people and disabled people are harmed by pathologization. Both intersex people and disabled people are harmed by curative violence.
In the book Cripping Intersex, Celeste Orr explores all these concepts and creates something called “intersex is/and/as/with disability,” which is a model to think about all these different and sometimes conflicting relationships with disability. Some intersex people might identify directly as disabled. Others might sometimes think about the way that intersex is treated as a disability. Other intersex people might think about intersex and disability as a way to have solidarity. All of these relationships with disability are meaningful parts of the intersex community.
8. What is intersex oppression/intersexism/interphobia/compulsory dyadism?
Intersex people face a lot of oppression in many ways in society. At the core, intersex oppression relies on the idea that the only acceptable sex traits are sex traits that fit into the sex binary. Intersex oppression relies on mythical ideas of the “ideal male or female” body, where someone's chromosomes perfectly line up with their genitalia and internal reproductive organs, with perfectly normal hormone levels and perfect secondary sex characteristics that don’t have any variation. When people don’t fit into that “perfect” sex binary, they are seen as less valuable, abnormal, and threatening. There is then a societal pressure to eradicate any traits and people that fall outside of the sex binary, which causes a lot of targeted discrimination of intersex people. This form of oppression is called “compulsory dyadism,” and was coined by Celeste Orr.
Compulsory dyadism is also rooted in, overlaps with, and is the foundation for many other types of oppression. For example, ableism is another form of oppression that creates ways of harming people whose bodies and minds are labeled as less valuable for societally constructed reasons. Check out Talila Lewis’s definition of ableism for more information. Another example is how racialized people are targeted by sex testing policies in sports--both intersex and perisex women of color are consistently targeted by sex testing policies designed to exclude intersex people from sports. Another example is that homophobia and transphobia contribute to why intersex bodies are seen as threats that need to be eradicated--society views existing with intersex sex traits as a slippery slope to growing up as a gay or trans adult. Compulsory dyadism is also at the root of a lot of transphobic rhetoric about how transitioning “ruins” people’s bodies. All these forms of oppression are connected.
There are a lot of ways that compulsory dyadism causes intersex people to be targeted and discriminated against. A huge issue is nonconsensual surgeries at birth, that attempt to “normalize” ambiguous genitalia, remove intersex people’s gonads, and otherwise alter genitalia or internal structures. These surgeries are often referred to as intersex genital mutilation, or IGM. These surgeries do not have any medical necessity, but doctors lobby to continue to be allowed to perform them anyway. These surgeries can sterilize intersex people, cause lifelong trauma, and also cause many disabling medical complications. Alongside IGM, intersex people also face a lot of different types of medical abuse.
Besides curative violence and medical abuse, intersex people also face discrimination in our schools, jobs, and public places. We face legal discrimination in changing our names and sex markers. We face discrimination from institutions like CPS, which often target parents, especially people of color, that refuse to put their children through intersex genital mutilation. Many intersex people survive targeted sexual violence. We have a widespread lack of resources, visibility, and representation. Many people still have prejudiced ideas about intersex people and call us slurs. These are just a few examples of the many way that interphobia/intersexism show up in our lives.
9. What is intersex justice?
Intersex justice is a framework created by intersex activists through the Intersex Justice Project as a way to fight for intersex liberation.
“Intersex justice is a decolonizing framework that affirms the labor of intersex people of color fighting for change across social justice movements. By definition, intersex justice affirms bodily integrity and bodily autonomy as the practice of liberation. Intersex justice is intrinsically tied to justice movements that center race, ability, gender identity & expression, migrant status, and access to sexual & reproductive healthcare. Intersex justice articulates a commitment to these movements as central to its intersectional analysis and praxis. Intersex justice acknowledges the trauma caused by medically unnecessary and nonconsensual cosmetic genital surgeries and addresses the culture of shame, silence and stigma surrounding intersex variations that perpetuate further harm.
The marginalization of intersex people is rooted in colonization and white supremacy. Colonization created a taxonomy of human bodies that privileged typical white male and female bodies, prescribing a gender binary that would ultimately harm atypical black and indigenous bodies. As part of a liberation movement, intersex activists challenge not only the medical establishment, which is often the initial site of harm, but also governments, institutions, legal structures, and sociocultural norms that exclude intersex people. Intersex people should be allowed complete and uninhibited access to obtaining identity documents, exercising their birth and adoption rights, receiving unbiased healthcare, and securing education and employment opportunities that are free from harm and harassment.” (Source: Dr. Mel Michelle Lewis through the Intersex Justice Project.)
There are seven principles to intersex justice:
Informed consent
Reparations
Legal protections
Accountability
Language
Children's rights
Patient-centered healthcare
10. What is intergender?
Intergender is a gender identity for use by intersex people only. It doesn’t have one specific definition-it is used by intersex people to mean a whole variety of things. It’s used to describe the unique ways our intersex experience intersects with and influences our gender. Some people use it as a modifying term, such as calling themselves an intergender man or woman, as a way to explain the way being intersex affects their identity. Other people identify solely as intergender, and have that be their whole gender.
11. What is dyadic/perisex/endosex?
All are words that mean “not intersex.” Different groups will have different preferences on which one they like to use.
12. Is hermaphrodite an offensive term?
Yes. It is an incredibly offensive slur that perisex people should never say. Many intersex people have a very painful history with the slur. Some of us reclaim the term, which can be an important act of healing and celebration for us.
12. Can perisex people follow?
Feel free, but understand that questions by intersex people are prioritized! Anyone is welcome to follow.
13. I’m writing a character who’s intersex…
Check out this post: https://trans-axolotl.tumblr.com/post/188153640308/intersex-representation. If you’re writing about intersex people for a paid project, you should pay an intersex person to act as a sensitivity reader before publishing.
Check out our Resources and Intersex Organizations pages as well!
#faq#intersex#actually intersex#actuallyintersex#lgbtqia#intersexism#disability#intersex resources#you can also find this post as one of our pages at intersex.support.tumblr.com/faq
135 notes
·
View notes
Text
How Does Hypospadias Affect the Penis?
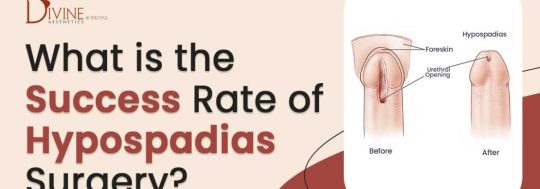
During the early development of a baby, the urethra starts as an open channel. The tube closes as the baby develops before birth. The opening of the urethra is known as the meatus and it is typically at the tip of the penis.
If a baby is suffering from hypospadias, then the meatus forms in a different location. It might be on the shaft of the penis, the scrotum, or inside the tip of the penis. Depending on the position of the meatus, hypospadias can be classified into different types, including:
Subcoronal: In this condition, the meatus is located near the head of the penis
Midshaft: In this condition, the meatus is located along the penis shaft
Penoscrotal: In this condition, the meatus is located where the penis and the scrotum meet
Know more about cause and symptoms of hypospadias
2 notes
·
View notes
Text

If you’re experiencing recurrent UTIs after what was considered a successful hypospadias repair, it’s crucial to consult a urologist. The long-term success of the surgery is often evaluated based on the absence of fertility issues and UTIs in adulthood. Depending on the findings, your urologist may suggest a treatment plan that could include redoing the surgery.
However, if the UTIs aren’t due to surgery failure but rather antibiotic resistance, here’s what you can do:
Antibiotic Resistance: Recurring UTIs may be caused by bacteria resistant to the antibiotics you’ve been prescribed. In such cases, your doctor may need to change the antibiotics to find one that is more effective.
Pelvic Floor Exercises: Strengthening the pelvic floor through exercises can help reduce the frequency of UTIs.
Dietary Adjustments: Avoid foods and drinks that irritate the bladder, and increase your intake of immunity-boosting foods like cranberry juice to help your body fight off bacteria.
Lifestyle Changes: Adopting a healthier lifestyle and routine can help prevent long-term complications.
Hygiene Practices: Maintain good local hygiene, empty your bladder frequently, and avoid using unclean public restrooms to reduce the risk of infection.
Taking these steps can help manage and reduce the occurrence of UTIs, whether they’re related to hypospadias surgery or not.
0 notes
Text
*DR. SMITA GOEL HOMEOPATHY CLINIC*
www.thehomeopathyclinic.co.in
Infertility case is increasing in all over world. The main causes of this is change our life style, foods, hight stress level etc. Around 10% - 15% is facing to infertility problems.
*Causes in Men:*
• Low sperm count: The man ejaculates a low number of sperm. A sperm count of under 15 million is considered low. Around one third of couples have difficulty conceiving due to a low sperm count.
• Low sperm mobility (motility): The sperm cannot “swim” as well as they should to reach the egg.
• Abnormal sperm: The sperm may have an unusual shape, making it harder to move and fertilize an egg.
• Genetic factors: A man should have an X and Y chromosome. If he has two X chromosomes and one Y chromosome, as in Klinefelter’s syndrome, the testicles will develop abnormally and there will be low testosterone and a low sperm count or no sperm.
• Mumps: If this occurs after puberty, inflammation of the testicles may affect sperm production.
• Hypospadias: The urethral opening is under the penis, instead of its tip. This abnormality is usually surgically corrected in infancy. If the correction is not done, it may be harder for the sperm to get to the female’s cervix. Hypospadias affects about 1 in every 500 newborn boys.
• Cystic fibrosis: This is a chronic disease that results in the creation of a sticky mucus. This mucus mainly affects the lungs, but males may also have a missing or obstructed vas deferens. The vas deferens carries sperm from the epididymis to the ejaculatory duct and the urethra.
• Radiation therapy: This can impair sperm production. The severity usually depends on how near to the testicles the radiation was aimed.
• Some diseases: Conditions that are sometimes linked to lower fertility in males are anemia, Cushing’s syndrome, diabetes, and thyroid disease.
*Causes in Women:*
• Age: The ability to conceive starts to fall around the age of 32 years.
• Smoking: Smoking significantly increases the risk of infertility in both men and women, and it may undermine the effects of fertility treatment. Smoking during pregnancy increases the chance of pregnancy loss. Passive smoking has also been linked to lower fertility.
• Alcohol:

0 notes
Text
What kind of diseases do urologists treat
Urologists are medical specialists who diagnose, treat, and manage diseases of the urinary tract in both men and women, as well as the male reproductive system. The scope of conditions they handle is extensive, covering a range of common to complex diseases and disorders.
One of the primary areas urologists focus on is urinary tract infections (UTIs). These infections can occur in any part of the urinary system, including the kidneys, bladder and urethra. UTIs are more common in women but can affect men and children as well. Urologists evaluate symptoms such as painful urination, frequent urination, and lower abdominal pain, and they prescribe antibiotics or other treatments to manage the infection and prevent recurrence.
Kidney stones are another significant condition treated by urologists. These hard deposits of minerals and salts form in the kidneys and can cause severe pain when passing through the urinary tract. Urologists use imaging tests to diagnose kidney stones and may recommend treatments ranging from medication to manage pain and facilitate stone passage to more invasive procedures like shock wave lithotripsy, which uses sound waves to break the stones into smaller pieces, where a scope is used to remove the stones directly.
Urologists also specialize in treating prostate diseases, including benign prostatic hyperplasia. BPH is a non-cancerous enlargement of the prostate gland that can cause urinary problems such as difficulty starting urination, weak urine flow, and frequent urination, especially at night. Treatments may include medications to shrink the prostate or relax the muscles around it, minimally invasive procedures, or surgery. Prostate cancer, a leading cause of cancer in men, involves more complex management, often requiring a combination of surgery, radiation therapy, hormone therapy, and chemotherapy, depending on the stage and aggressiveness of the cancer.
Bladder conditions are also within the purview of urology. Bladder infections, interstitial cystitis, and bladder cancer are common issues. Bladder cancer symptoms include blood in the urine, frequent urination, and pain during urination. Treatment strategies can include surgical removal of the tumor, chemotherapy, immunotherapy, or radiation therapy, tailored to the cancer’s stage and severity.
Male reproductive health is another critical aspect of urology. Urologists treat erectile dysfunction (ED), a condition where a man cannot achieve or maintain an erection sufficient for sexual intercourse. Causes of ED can be psychological, physical, or a combination of both. Urologists provide various treatment options, including oral medications, vacuum erection devices, penile injections, or implants. They also address male infertility issues, conducting tests to identify causes such as low sperm count or poor sperm motility and offering treatments ranging from medication to surgical interventions.
Incontinence, or the inability to control urination, is another area of expertise for urologists. This condition can result from various factors, including weakened pelvic floor muscles, nerve damage, or an overactive bladder. Urologists assess the underlying cause and recommend treatments such as pelvic floor exercises, medications, nerve stimulation, or surgery.
Urologists also manage congenital abnormalities of the urinary tract in children, such as vesicoureteral reflux (where urine flows backward from the bladder to the kidneys), hypospadias (a birth defect in boys where the opening of the urethra is on the underside of the penis). Early diagnosis and treatment are crucial to prevent complications and ensure normal development.
Another critical aspect of urology is the treatment of urologic cancers, including cancers of the kidney, bladder, prostate, and testicles. Kidney cancer symptoms may include blood in the urine, persistent back pain, or a lump in the abdomen. Treatment often involves surgery to remove part or all of the kidney, sometimes combined with targeted therapies or immunotherapy. Testicular cancer, though less common, typically affects younger men and is highly treatable, especially when detected early. Treatment may include surgery, radiation, and chemotherapy.
In addition to treating these diseases, urologists are involved in preventive care and education. They help patients manage chronic conditions such as diabetes and hypertension that can impact urinary and reproductive health. They also provide guidance on lifestyle changes to improve overall urological health, such as diet modifications, fluid management, and smoking cessation.
Best Urologist in Gurgaon often collaborate with other specialists, such as oncologists, radiologists, nephrologists, and gynecologists, to provide comprehensive care. This multidisciplinary approach ensures that patients receive well-rounded treatment plans tailored to their specific needs and conditions.
In conclusion, urologists treat a wide array of diseases and conditions related to the urinary tract and male reproductive system. Their expertise spans from common issues like UTIs and kidney stones to complex conditions like cancers and congenital abnormalities. If you live in Gurgaon and are looking for best Andrologist in gurgaon and best Kidney Transplant Surgeon in gurgaon, then Dr. Sumit Sharma can prove to be your best option. Through a combination of diagnostic evaluations, medical treatments, surgical interventions, and preventive care, urologists play a crucial role in maintaining and improving patients' urological health and overall well-being. Their work not only addresses immediate health concerns but also contributes to long-term health and quality of life.
0 notes
Note
I think I might be intersex? I'd kill for your opinion. I was born with a penis but had surgery as a baby (I'm to understand it was falling into my body) and it's always resided internally in its own cavity. I've heard of intersex folks that have an identical situation, any adivce/thoughts? I've been at a loss with this (and doctors don't take you seriously when you're overweight so they've been no help).
Hi anon! Sorry it took so long to answer.
I'm sorry you've been having to deal with discrimination from doctors--that's so messed up and you deserve better.
The first thing that comes to mind for me is that might have been a sign of hypospadias or epispadias, and that the surgery you had as a child might have been hypospadias or epispadias repair. Hypospadias is a condition where the urethra is located on the underside of the penis, and epispadias is when the urethra doesn't develop into a full tube and is located in a different place on the penis. A lot of times, hypospadias and epispadias also come along with congenital chordee, which means that the penis is curved and bent in a different direction due to bands of fibrous tissue. Undescended testicles (cryptorchidism) are also often associated with them. Hypospadias and epispadias are both considered intersex variations. I'm not too sure what that aftermath of that surgery looks like or potential complications as an adult, but that's something that really comes to mind to me as a possibility for you.
Another possibility might be Penoscrotal Transposition, which is a variation where people's penis is located below or in the middle of the scrotum. I'm less familiar with what surgery looks like for that, or what the possible after effects might be.
There are also several different intersex variations that could cause different genital configuration, but those would be probably less likely unless you also had more symptoms like growing breasts during puberty, micropenis, infertility, or other signs of estrogen based puberty.
I hope some of that might be relevant, and if any followers have any other suggestions please add on! (As always, disclaimer that we can't diagnose or provide medical advice.)
9 notes
·
View notes
Text



Hypospadias is a clinical group of best Hypospadias Surgeon in Hyderabad and as a surgical issue has enchanted the surgeons and the patients since time immemorial. In the past, hypospadias operations have had very poor success rates. Then after some time, the fact was accepted that the Hypospadias surgery needs to be done by a Surgeon who specializes in Hypospadias Surgery, namely a Hypospadiologist. One of the best Hypospadias Surgery Doctor in Hyderabad are available at Ankura hospital.
Hypospadias is a congenital (birth) defect found in a male child. In this condition, the opening of urethra is not placed at the penis's tip. The urethra originates abnormally during 8-14 weeks of pregnancy. This abnormal opening is usually anywhere, beginning from just below the end of the penis to the scrotum. The condition can only be treated by the best Hypospadias Surgery in hyderabad.
Types of Hypospadias: There are three types of hypospadias:
Subcoronal: The urethral opening is placed somewhere close to the penis head.
Midshaft: The urethral opening is placed along the penis’s shaft.
Penoscrotal: The urethral opening is placed where the penis meets scrotum.
Symptoms of Hypospadias: The common signs and symptoms of hypospadias are: Beneath curved penis (chordee).
The opening of the urethra is placed in other sites than the penis's head.
The hooded appearance of the penis when its upper half is covered by the foreskin.
Unnatural spraying while urinating. These conditions can only be treated with the help of hypospadias surgery by the best Hypospadias Treatment Doctors in Hyderabad.
Cause of Hypospadias: For many pediatric urologists, it's difficult to find the main cause of Hypospadias. Our Best Hypospadias Surgery Doctor in Hyderabad at Ankura Hospital have recognized some of its main causes:
Being obese or Overweight in pregnancy.
Family history of Hypospadias
Pregnancy after the age of 35.
Undergoing IVF fertility treatment
Errors or mutations in Genetic sequencing.
Best Treatment for Hypospadias in Children
In the case of mild hypospadias, when the urethral opening is just a little down from regular and there is no bending of the penis, treatment may not be required. However, in most cases, operation is needed to fix the hypospadias. It can be done in one operation. But, if the condition is more complicated, there may be a requirement of two operations. The best Treatment for Hypospadias in Children is majorly done when the child is about 6-18 months old.
Book an Appointment Now!
Ankura Hospital Hyderabad is the best hypospadias surgeon nearby Best Hypospadias Surgeon in Hyderabad, Best Hypospadias Surgeon near me, Best Hypospadias Surgery Doctor in Hyderabad, Best Hypospadias Surgery in Hyderabad, Best Hypospadias Treatment Doctors in Hyderabad, Best Treatment for Hypospadias in Children, Best Surgery for Hypospadias Treatment, Hypospadias Surgery Cost in Hyderabad, Best Hypospadias Surgery cost near me. For more information contact +91 9053 108 108.
youtube
#Best Hypospadias Surgeon in Hyderabad#Best Hypospadias Surgeon near me#Best Hypospadias Surgery Doctor in Hyderabad#Best Hypospadias Surgery in Hyderabad#Best Hypospadias Treatment Doctors in Hyderabad#Best Treatment for Hypospadias in Children#Best Surgery for Hypospadias Treatment#Hypospadias Surgery Cost in Hyderabad#Best Hypospadias Surgery cost near me#Youtube
0 notes
Text

Hypospadias is a congenital condition that affects boys, where the urethral opening is not positioned at the tip of the penis. This occurs due to abnormal formation of the urethra during the 8-14 weeks of pregnancy. The urethral opening can appear anywhere along the underside of the penis, including at the scrotum. Depending on the location of the opening, the condition can be classified as either distal.
Types of Hypospadias:
The types of hypospadias a boys has depends on location of the opening of the urethra:
Subcoronal: The opening of the urethra is located somewhere near the head of the penis.
Midshaft: The opening of the urethra is located along the shaft of the penis.
Penoscrotal: The opening of the urethra is located where the penis and scrotum meet.
Understanding the normal penis and urethra
The normal urethra is a tube through which that urine flows out of the bladder. It passes through the penis. The opening of the urethra (meatus) is normally at the end of the penis, partly covered by the foreskin.
What is the penis like in hypospadias?
The main problem is that the urethra opens on the underside of the penis instead of at the end of the penis. The opening can be anywhere from just below the normal position (mild) to as far back as the base of the scrotum (severe).
Hypospadias may also include the following:
A hooded appearance of the foreskin. This is because the foreskin does not develop on the underside of the penis.
Tightening of the tissues on the underside of the penis (called ‘chordee’). This pulls the penis down and it cannot fully straighten. This is commanly seen in severe hypospedias
What problems can hypospadias cause?
Problems are likely to occur if hypospadias is left untreated. The further back the opening of the urethra is, the more severe the problems are likely to be.
Passing urine is different to normal. A baby in nappies will have no problem. However, when older, the urine stream may not be able to be directed forward into a urinal. When going to the toilet the urine is likely to ‘spray’ backwards. Sitting on a toilet may be needed to pass urine without mess.
Chordee causes bending of the penis. This is more noticeable when the penis is erect. Sexual intercourse may be difficult or impossible in severe cases.
Psychological problems about being ‘different’ to normal are common.
How common is hypospadias and what causes it?
About 1 in 300 boys are born with some degree of hypospadias. It seems to be getting more common. The reason why the penis does not develop properly is still not clear. The development of the penis while the baby is growing in the womb (uterus) is partly dependent on the male sex hormones such as testosterone.
youtube
What is the treatment for hypospadias?
If the hypospadias is mild, with the opening of the urethra just a little down from normal and with no bending of the penis, no treatment may be needed. However, in most cases an operation is required to correct the hypospadias. This can usually be done in one operation. However, if the hypospadias is more complicated, two operations may be necessary. The operation is usually done when the child is around 6-18 months old. The goals of treatment are:
For urine to be passed in a forward way.
For the penis to be straight when erect.
For the penis to look as normal as possible.
The position of the opening of the urethra is altered. Also, if chordee is present then this is corrected to allow the penis to straighten. The foreskin is usually used during the operation to make the new urethra so it is important that a circumcision is not done before the corrective surgery is performed and depending on the hypospedias surgery in delhi
The success of the operation and the ‘normality’ that can be achieved depends on the severity of the hypospadias done in single as two stage.
#best pediatric urologist in delhi#hypospedias surgery in delhi#pediatric surgeon in delhi#pediatric urologist in india#Youtube
0 notes
Text

Urology, a branch of medicine focusing on the urinary tract system and male reproductive organs, encompasses a wide range of conditions that affect both men and women of all ages. From kidney stones to urinary tract infections, understanding common urological issues and their treatments is crucial for maintaining optimal health and well-being.
Understanding General Urology
General urology addresses a myriad of conditions affecting the urinary system. These conditions may include urinary tract infections (UTIs), kidney stones, benign prostatic hyperplasia (BPH), urinary incontinence, and erectile dysfunction, among others. While some conditions are more prevalent in specific demographics, such as BPH in older men or UTIs in women, many urological issues can affect anyone regardless of age or gender.
Common Urological Conditions and Treatments
Urinary Tract Infections (UTIs): UTIs are bacterial infections that can occur anywhere in the urinary system. Symptoms may include a frequent urge to urinate, burning sensation during urination, and cloudy or foul-smelling urine. Treatment typically involves antibiotics and increased fluid intake to flush out bacteria.
Kidney Stones: These are solid mineral deposits that form in the kidneys and can cause severe pain when they pass through the urinary tract. Treatment options range from pain management and increased fluid intake to surgical procedures such as lithotripsy or ureteroscopy.
Benign Prostatic Hyperplasia (BPH): BPH is a common condition in aging men where the prostate gland enlarges, causing urinary symptoms such as frequent urination, difficulty starting or maintaining urination, and weak urine flow. Treatment may include medications to relax the prostate or surgical procedures like transurethral resection of the prostate (TURP).
Urinary Incontinence: This refers to the involuntary loss of urine, which can significantly impact quality of life. Treatment options vary depending on the underlying cause and severity of the condition, ranging from lifestyle modifications and pelvic floor exercises to medications or surgical interventions.
Erectile Dysfunction (ED): ED is the inability to achieve or maintain an erection sufficient for sexual intercourse. Treatment options may include oral medications, injections, vacuum devices, or surgical implants, depending on individual needs and preferences.
Seeking Specialized Urological Care
When faced with urological issues, seeking prompt and specialized care is essential for accurate diagnosis and effective treatment. Whether it's finding the best endo-urology care in Sector B, Lucknow, or locating the nearest urological hospital, access to expert healthcare providers is crucial.
Expert Care for Specific Needs
Endo-Urology: Specializing in minimally invasive procedures for treating kidney stones and other urinary tract conditions, endo-urologists offer advanced techniques such as laser lithotripsy and ureteroscopy for optimal outcomes.
Uro-Oncology: For individuals facing urological cancers such as prostate, bladder, or kidney cancer, comprehensive uro-oncology care provides personalized treatment plans, including surgery, chemotherapy, and radiation therapy.
Kidney Transplants: Renal transplantation offers a life-saving treatment option for individuals with end-stage kidney disease. Accessing reputable centers with experienced transplant surgeons ensures the best possible outcomes for patients in need of kidney transplants.
Female Urology: Dedicated to addressing the unique urological needs of women, female urologists specialize in conditions such as urinary incontinence, pelvic organ prolapse, and recurrent UTIs, providing compassionate and effective care.
Pediatric Urology: Children with congenital or acquired urological conditions require specialized care from pediatric urologists trained to manage conditions such as hypospadias, vesicoureteral reflux, and undescended testicles with expertise and sensitivity.
Male Infertility: Urologists specializing in male infertility offer comprehensive evaluations and treatments for issues affecting sperm production, transport, or erectile function, helping couples achieve their reproductive goals through assisted reproductive techniques.
Conclusion
General urology encompasses a wide array of conditions affecting the urinary system and male reproductive organs, requiring specialized care tailored to individual needs. Whether it's managing common urological issues or addressing specific concerns like kidney transplants or male infertility, seeking timely and expert care ensures optimal outcomes and improved quality of life. With access to the best urological care providers and treatments, individuals can confidently navigate their urological health journey towards lasting wellness and vitality.
#best pediatric urology care#best general urology care near me#best female urology care dr. aditya sharma#best endo urology care in sector b lucknow#best uro oncology care near me#kidney transplant near me#male infertility care near me
0 notes
Link
#market research future#urethral stricture market#urethral stricture market size#urethral stricture market shar#urethral stricture growth
0 notes
Text
Hypospadias
Hypospadias is a common variation in fetal development of the penis in which the urethra does not open from its usual location on the head of the penis. It is the second-most common birth defect of the male reproductive system, affecting about one of every 250 males at birth. Roughly 90% of cases are the less serious distal hypospadias, in which the urethral opening (the meatus) is on or near the head of the penis (glans). The remainder have proximal hypospadias, in which the meatus is all the way back on the shaft of the penis, near or within the scrotum. Shiny tissue that typically forms the urethra instead extends from the meatus to the tip of the glans; this tissue is called the urethral plate.
In most cases, the foreskin is less developed and does not wrap completely around the penis, leaving the underside of the glans uncovered. Also, a downward bending of the penis, commonly referred to as chordee, may occur. Chordee is found in 10% of distal hypospadias and 50% of proximal hypospadias cases at the time of surgery. Also, the scrotum may be higher than usual on either side of the penis (called penoscrotal transposition).
The cause of hypospadias is unknown; however, there is likely to be a genetic component. It most often occurs by itself, without other variations, although in about 10% of cases it may be part of an intersex condition or a medical syndrome with multiple abnormalities
Hypospadias can be a symptom or indication of a difference in sex development or an intersex condition, but some consider that the presence of hypospadias alone is not enough to classify someone as a person with a difference/variation in sex development or as intersex. In most cases, hypospadias is not associated with any other condition. Hypospadias is itself recognized as an intersex condition by several intersex rights activist groups, who consider the repositioning of a working urethra on a child too young to consent to be a human rights violation.
Source: Wikipedia, the free content online encyclopedia
1 note
·
View note
Text

Fistula formation is a common complication following hypospadias repair surgery. In this condition, a small hole may develop anywhere along the bladder, causing urine to leak. Hypospadias itself is a congenital abnormality in boys, where the urethral opening is not located at the tip of the penis.
So, does the formation of a fistula lead to fertility problems? It depends on several factors:
Fistula Repair: A fistula can typically be corrected with a follow-up surgery, which is generally straightforward and has a high success rate. When repaired successfully, the chances of fertility issues are nearly zero.
Untreated Fistula: If a fistula is left untreated, it may affect the structure of the penis, potentially leading to secondary fertility issues. The longer the condition persists without treatment, the greater the risk of complications.
Severity of Hypospadias: The severity and type of hypospadias play a significant role in fertility. For example, in cases where chordee (a downward curvature of the penis) is present, penetration can be painful or uncomfortable, and ejaculation might be problematic. In severe cases, gender determination can also be challenging.
Other Complications: When a fistula occurs in combination with a narrow bladder or a small penis size, the likelihood of fertility issues increases.
In summary, while a fistula after hypospadias surgery can be concerning, it is usually treatable with minimal impact on fertility, especially if addressed promptly. However, the underlying severity of hypospadias and any associated complications should also be considered when evaluating potential fertility concerns.
0 notes
Text

Is Your Child Facing Urological Challenges? Unveiling Causes, Types, and Risk Factors
Introduction:
As parents, we always strive to ensure the well-being of our children, addressing their needs and concerns with utmost care. However, when it comes to urological issues in children, many parents might feel uncertain or unaware of what signs to watch for and when to seek help. Understanding the causes, types, and risk factors associated with pediatric urological problems is crucial for early detection and effective management. In this article, we'll delve into these aspects, shedding light on the importance of awareness and the expertise of pediatric urologists like Dr. Abhijit Benare in Pune.
Understanding Pediatric Urological Issues:
Urological issues encompass a range of conditions affecting the urinary tract and genital organs in children. These conditions can manifest at any age, from infancy to adolescence, and may vary in severity. While some problems resolve on their own, others require medical intervention. It's essential for parents to be vigilant and proactive in recognizing potential signs of urological issues in their children.
Causes of Pediatric Urological Issues:
Congenital Anomalies: Many urological issues in children stem from congenital anomalies, meaning they are present at birth. These anomalies can affect various parts of the urinary tract, such as the kidneys, ureters, bladder, or urethra. Common congenital anomalies include vesicoureteral reflux (VUR), posterior urethral valves (PUV), and hydronephrosis.
Infections: Urinary tract infections (UTIs) are prevalent in children and can sometimes indicate an underlying urological problem. Recurrent or persistent UTIs may necessitate further evaluation by a pediatric urologist to rule out structural abnormalities or other underlying issues.
Functional Disorders: Some children may experience functional disorders of the urinary system, such as bladder dysfunction or voiding dysfunction. These disorders can lead to symptoms like urinary incontinence, urgency, or frequency, impacting a child's quality of life and requiring specialized management.
Types of Pediatric Urological Issues:
Hydronephrosis: This condition involves the swelling of one or both kidneys due to the backup of urine. It can occur as a result of blockages, reflux, or other structural abnormalities within the urinary tract.
Hypospadias: Hypospadias is a congenital condition where the opening of the urethra is located on the underside of the penis instead of the tip. Surgical correction may be necessary to restore normal urinary function and appearance.
Undescended Testicles: In some male infants, one or both testicles fail to descend into the scrotum from the abdomen. If left untreated, undescended testicles can lead to complications such as infertility and an increased risk of testicular cancer later in life.
Bladder Exstrophy: Bladder exstrophy is a rare congenital anomaly where the bladder protrudes through the abdominal wall. Surgical reconstruction is typically required to correct this condition and restore normal bladder function.
Ureteropelvic Junction (UPJ) Obstruction: UPJ obstruction occurs when there is a blockage at the point where the ureter connects to the kidney pelvis. This obstruction can lead to urinary stasis and potentially damage the kidney if not addressed promptly.
Risk Factors for Pediatric Urological Issues:
Family History: Children with a family history of urological issues may have a higher risk of developing similar conditions. Genetic factors can play a significant role in certain congenital anomalies and inherited disorders affecting the urinary tract.
Maternal Factors: Certain maternal factors, such as maternal age, smoking during pregnancy, or exposure to certain medications or toxins, may increase the risk of urological problems in offspring. Prenatal care and maternal health optimization are essential for reducing these risks.
Prematurity: Premature infants are more susceptible to urological issues due to the incomplete development of their organs and systems. Close monitoring and early intervention are crucial for addressing any urological concerns in preterm infants.
Previous Surgeries or Medical Conditions: Children who have undergone previous surgeries or have underlying medical conditions such as neurogenic bladder or spina bifida may be at higher risk for urological complications. Comprehensive medical history assessment is essential for identifying potential risk factors.
Conclusion:
Ensuring the optimal urological health of our children requires vigilance, awareness, and access to specialized care when needed. Dr. Abhijit Benare, a renowned pediatric urologist in Pune, possesses the expertise and dedication to address a wide range of pediatric urological issues with compassion and precision. By understanding the causes, types, and risk factors associated with these conditions, parents can play an active role in promoting their child's urological well-being and overall quality of life.
By prioritizing regular check-ups, prompt intervention when symptoms arise, and adherence to recommended treatment plans, parents can empower their children to lead healthy, fulfilling lives free from the burden of urological challenges.
Remember, early detection and intervention are key to ensuring the best possible outcomes for children with urological issues. Let's work together to safeguard our children's urological health and support them in reaching their full potential.
0 notes
Text
Introduction
Hypospadias is a congenital condition in males where the opening of the urethra is not at the tip of the penis, but on the underside. It is a relatively common condition, affecting approximately 1 in every 200-300 male births. The aim o...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Note
I found out about 10 years back that I had some kind of I surgery on my genitals as a child (when I was 1), but I didn't really think much about it at the time. I've since become more curious about what the surgery might have been for. It was listed as a 'labia separation', but as far as I can tell they don't normally perform that kind of surgery unless there is an urgent medical need (usually if the child isn't able to pee properly). I asked my mum for some more details (1/?)
(cont) She told me that the doctors said it was because they "didn't think my hole was big enough" and that my grandma (on my father's side) had a similar problem as a child also. I'm trying to find out more information as to why they would do this to a 1 year old, especially as this doesn't sound like a labia separation at all. Does this sound like the kind of surgery that might be performed on an intersex individual? 2/2
TW: detailed surgery talk
Hi anon,
It is definitely possible that this is a surgery that might be performed on an intersex person. Generally, surgeries that happen on intersex children at birth/early childhood include surgeries like vaginoplasty, clitoral reduction, gonadectomy, hypospadias repair, labiaplasty and some other outdated surgical techniques. This can actually include labia separation-some intersex variations like Congenital Adrenal Hyperplasia sometimes cause labial fusion, although they don't always and aren't the only cause of labial fusion.
The fact that the doctor said the reason was that the vagina wasn't big enough makes me think it's even more likely that it could have been some sort of procedure like vaginoplasty. In intersex kids who get vaginoplasty but still have a uterus, cervix and upper vagina, the procedure usually involves separating the fused labia and then creating a wider vagina. (source-tw for photos and explicit medical language). Of course, we can't confirm anything 100% over the internet-but a lot of the things you're describing, as well as the vague way that doctors talked about it, are things that are really common in a lot of intersex people's experiences with surgery. It's possible it could have just been labial fusion surgery to allow for urination, but the doctor's comment is really sticking out to me as something that a lot of doctors say in intersex surgeries.
If you ever had follow up surgeries, felt like you visited an OB/GYN or endocrinologist a lot more than average growing up, had frequent UTIs, pain during sex, or had other unexplained things in your medical record, those could all also be signs that would point towards intersex being more likely.
I know that thinking about the possibility of being intersex and learning that you might have undergone intersex surgery as a child can be a really overwhelming experience, so please feel to reach back out for as much support as you need. Whatever emotions you might be feeling about the possibility are valid. It can be a really big shock to think about being intersex, even if you've known about the surgery for years, and you don't need to go through that alone. We have a resources page and I can also direct you towards support groups if you're interested.
Sending love and solidarity your way anon, and please feel free to reach back out with any follow up questions.
💜💜💜
-Mod E
11 notes
·
View notes
Text



Hypospadias is a clinical group of best Hypospadias Surgeon in India and as a surgical issue has enchanted the surgeons and the patients since time immemorial. In the past, hypospadias operations have had very poor success rates. Then after some time, the fact was accepted that the Hypospadias surgery needs to be done by a Surgeon who specializes in Hypospadias Surgery, namely a Hypospadiologist. One of the best Hypospadias Surgery Doctor in India are available at Ankura hospital.
Hypospadias is a congenital (birth) defect found in a male child. In this condition, the opening of urethra is not placed at the penis's tip. The urethra originates abnormally during 8-14 weeks of pregnancy. This abnormal opening is usually anywhere, beginning from just below the end of the penis to the scrotum. The condition can only be treated by the best Hypospadias Surgery in India.
Types of Hypospadias: There are three types of hypospadias:
Subcoronal: The urethral opening is placed somewhere close to the penis head.
Midshaft: The urethral opening is placed along the penis’s shaft.
Penoscrotal: The urethral opening is placed where the penis meets scrotum.
Symptoms of Hypospadias: The common signs and symptoms of hypospadias are: Beneath curved penis (chordee).
The opening of the urethra is placed in other sites than the penis's head.
The hooded appearance of the penis when its upper half is covered by the foreskin.
Unnatural spraying while urinating. These conditions can only be treated with the help of hypospadias surgery by the best Hypospadias Treatment Doctors in India.
Cause of Hypospadias: For many pediatric urologists, it's difficult to find the main cause of Hypospadias. Our Best Hypospadias Surgery Doctor in India at Ankura Hospital have recognized some of its main causes:
Being obese or Overweight in pregnancy.
Family history of Hypospadias
Pregnancy after the age of 35.
Undergoing IVF fertility treatment
Errors or mutations in Genetic sequencing.
Best Treatment for Hypospadias in Children
In the case of mild hypospadias, when the urethral opening is just a little down from regular and there is no bending of the penis, treatment may not be required. However, in most cases, operation is needed to fix the hypospadias. It can be done in one operation. But, if the condition is more complicated, there may be a requirement of two operations. The best Treatment for Hypospadias in Children is majorly done when the child is about 6-18 months old.
Book an Appointment Now!
Ankura Hospital India is the best hypospadias surgeon nearby Best Hypospadias Surgeon in India, Best Hypospadias Surgeon near me, Best Hypospadias Surgery Doctor in India, Best Hypospadias Surgery in India, Best Hypospadias Treatment Doctors in India, Best Treatment for Hypospadias in Children, Best Surgery for Hypospadias Treatment, Hypospadias Surgery Cost in India, Best Hypospadias Surgery cost near me. For more information contact +91 9053 108 108.
youtube
#Best Hypospadias Surgeon in India#Best Hypospadias Surgeon near me#Best Hypospadias Surgery Doctor in India#Best Hypospadias Surgery in India#Best Hypospadias Treatment Doctors in India#Best Treatment for Hypospadias in Children#Best Surgery for Hypospadias Treatment#Hypospadias Surgery Cost in India#Best Hypospadias Surgery cost near me#Youtube
0 notes