#bipap mask vented
Explore tagged Tumblr posts
Text

Buy the Best Quality Synocare BIPAP Vented Full Face Mask
The Synocare BIPAP Vented Full Face Mask is a top-of-the-line solution designed for individuals who rely on BIPAP therapy for effective sleep apnea management. This mask ensures a secure and comfortable fit, providing optimal air circulation and reducing the risk of air leakage during use. Equipped with advanced venting technology, the Bi-pap masks vented design facilitates quiet and efficient exhalation, ensuring a peaceful night’s sleep for users.
Whether you are new to BIPAP therapy or looking to upgrade your current equipment, the Synocare BIPAP Vented Full Face Mask offers an ideal balance of comfort, durability, and performance. The soft, skin-friendly material minimizes pressure points, making it suitable for prolonged wear, while the adjustable straps provide a custom fit for a wide range of face shapes and sizes.
#Synocare BIPAP Vented Full Face Mask#bipap mask vented#medical equipment#surgical supplies#surgical#online surgical store#surgical products
1 note
·
View note
Text
So I don’t understand this one doctor at my dad’s rehabilitation place. He wants my dad to go 14 days without the ventilator and if he can, then he can have his tracheotomy removed. However, 3 other doctors from other hospitals said he should have it for life. He’s been intubated too many times and when my dad gets sick, it goes from 0 to 100 quick. The more you’re intubated the more scar tissue you gain to the point you may not be able to swallow. We all accepted the vent was the best route long term.
So it’s day 5 of this test. My dad sounded really tired last night. Then today I called him to ask if he wanted me to bring him food or something for Fathers Day since he didn’t want gifts. He was slurring his words on the phone saying he just woke up but I’ve been apart of every major medical emergency to know that’s a red flag. So I drove there, came in the room, he was sleeping but having a hard time waking up. He kinda gets up, slurs his words. It’s just oh no…this is how he acts when we have to call the EMT for him. So I ask where is your call light? He picks up his cell phone to call who knows who. I find it buried behind him.
Meanwhile Georgette was highly concerned. She kept nudging his hand aggressively. It wasn’t for food, it wasn’t pets. She started whimpering. A nurse aid comes in and I say he has to be back on the vent now. This ain’t him. So she runs and gets respiratory, his nurse and another nurse come running in. I told them I know the doctor doesn’t want it but he needs it. He’s literally dying.
So they place him back on the vent and within 2 minutes, he starts to wake up and suddenly his glassy eyes are gone and he’s looking around asking “what??” The nurses were going off by what he was telling them. They noticed he was off, he hadn’t eaten in days which is unlike him but he’d always say he was ok. I told them he masks his anxiety well and even if he’s dying he’ll say he’s fine because he doesn’t want to be a burden. So you have to really override his ok and look at his symptoms. Then no one apparently knew he was on a bipap machine at home when he slept so they were like fuck! He needs to be on the vent nightly anyway. My dad is a medical anomaly and should be dead if you look at his chart alone and one of his biggest issues is his body does not expel CO2. So if he doesn’t have a bipap or ventilator pulling the air out, it becomes trapped in his lungs and blood and his body basically poisons itself.
By the end, he was much better. I was like “dad!! I didn’t want to have to save your life on Father’s Day of all days! Tell people when you feel off!” Georgette wouldn’t leave his side until she knew he was ok. Then she went around the room thanking each nurse one by one. Dogs know. I just was confused why no one said this isn’t normal, let’s call the doctor and tell him he’s going back on the vent. I’m a little irritated by that, or even a simple phone call home asking what’s normal for him. Nothing. It took me being there in person saying fuck the doctor’s orders, place him back on.
But it was a happy ending. Just scary.
My pretty girl who protects her papa. ❤️


6 notes
·
View notes
Text
i think if we hadn't read Alice Wong, met our friend who uses a vent full time, & seen other vent users, we just would not have been able to see a future for ourselves where we can breathe. we arent at a point where we need invasive ventilation, but now that we're relying on the bipap for filtered air & our hypoventilation episodes during the day, we really rely on those images of bipap and vent users to see a future for ourselves. its really hard to see selfies with and without a bipap mask side by side and see both as recognizable, handsome/pretty, and social.
i havent figured out bipap bangs enough to feel confident sharing a selfie anywhere, but i did do a video appointment today and last week with it on and it was weird. like i could think clearer but i also had that hurdle of "will they recognize me as me? as an adult? as a person?" i needed to crawl over. im still crawling over it. i dont think id be able to do so if i didnt have those examples of ventilation users living, writing, learning, teaching, speaking, signing, breathing.
im still missing some of that access intimacy of like. feeling/being seen but i think ill get there. i know there's futures for people like us.
n e weigh. chag chanukah sameach and a freylikhn khanikeh to all my handsome/pretty crips. we'll make it. i know we will.
#alice also became nonspeaking recently n her piece on that experience was nice n i think similar#like in terms of recognizing ways of living and communicating that are often suppressed
1 note
·
View note
Text
SSI healthcare Medisafe CPAP/BIPAP Full Face Mask (Vented, Medium Size)
Price: (as of – Details) Full face mask gel uses cushion to give a good seal and comfortable fit. Excellent advancement for cpap users who need a full-face mask. A comfortable forehead cushion and enhanced stability selector combine with our popular blue gel replaceable cushion to create a high level of comfort and stability. Date First Available : 5 June 2019 Manufacturer : SSI…

View On WordPress
0 notes
Note
as a fellow cripple I 100% agree with you on the fact that Musk is going to likely try to trick desperate newly disabled people into signing up for neuralink and we should be kind to and offer support to those people. I developed moderate-severe CFS in Jan 2020 (thank covid /s) and that first year after you transition from "able bodied or mostly able bodied" to "barely able or unable to function independently" sucks ass. I literally spent the whole year swinging between deeply depressed/suicidal and feeling like I needed to fix it right now. You really feel like you have nothing to lose, it would be easy to get roped into doing something unsafe for yourself if it was framed as being for the greater good. I think one of the most important things we can emphasize now is peer and professional counseling for newly physically disabled people to help them process the initial grief and depression that a lot of us feel.
Thank you
That first while before life settles in and you learn how to live with your disability is the fucking WORST and I just started having to do that with the ventilator (I got it friday!) so I'm feeling the "what odds would you take?" feeling really keenly.
Im handling it really well but every once in a while the "this is your life now, the only time you won't need that mask strapped to your face is when they punch a hole directly in your neck" panic starts creeping in. I can't imagine having to go from fully abled to full time ventilator use. I even had a wall unit bipap to ease me into noninvasive ventilation for like 5 months before I finally had to have the vent.
19 notes
·
View notes
Note
Hi there! I want to ask if a patient who got overdosed with multiple types of sleeping pills, struggling against the tubes and wires that were keeping them alive in the ICU and so they were restrained but still were as restless and anxious in their semi-conscious stage, would the doctor sedate the patient to keep them calm? Given that they were overdosed with drugs i was wondering if that is advisable. Thank you a lot in advance.
Any time someone is on a ventilator, the goal is to get them safely off the ventilator.
Typically when thinking of sedating a patient who is on a ventilator, we're using something called a RASS score. RASS stands for Richmond Agitation-Sedation Scale:
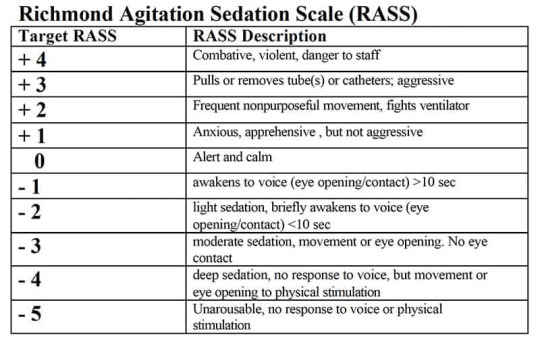
Typically, a nurse will have orders for a continuous infusion of a sedating medication (usually propofol, a benzodiazepine, or a barbiturate). They can increase or decrease this dose a set amount on a set schedule (say, one titration every hour) to keep the person between -1 and +1.
Since it sounds like your patient is somewhere +2 and +3, assuming this patient still needed the ventilator, the nurse would likely increase the infusion rate to decrease the patient's agitation. The presence of other medication in their system would be something they would know about, watch and monitor closely, but would not necessarily stop them from using a sedating medication. The patient is already on a ventilator and a ton of monitoring, so the likelihood that additional medication would kill them without a fight is very low.
HOWEVER:
Ventilators, like almost everything in healthcare, are not without risks- so you have to weigh the risk of things like ventilator associated pneumonia, diaphragm deconditioning, sores in the respiratory tract, and other vent-associated problems with the perk of the patient continuing to breathe.
So one big question here is: assuming this patient was put on the vent because they didn't have a respiratory drive due to overdose, but are now fighting the vent- has this patient regained enough of their own respiratory drive that they no longer need the vent?
There are many other options for supporting breathing. Is this person awake enough to use a CPAP or BiPAP? Could we get away with a mask or high flow nasal cannula?
To answer this, the nurse would probably call over a respiratory therapist and the intensivist (the doc that works in the ICU). They'd chat and decide if it was appropriate to do something called a breathing trial (a test to determine if the patient still needs a ventilator, or at least to see if the patient can tolerate a lower level of ventilatory support). Breathing trials are typically done on most patients every morning, but for something like a drug overdose where the inability to breathe would be expected to be really temporary, they might do one off schedule.
If they decided that was appropriate, the nurse would reduce or withdraw the sedation, and the respiratory therapist would adjust the vent settings so the patient was doing all the work of breathing (with the exception of a small amount of pressure support to compensate for the fact that they still have a tube down their throat). Then they'd wait and see if the patient started breathing on their own. If they did, they'd extubate the patient and monitor their oxygen and CO2 levels to make sure the person was breathing on their own well enough without the vent.
If so, yay! No more vent!
- Ross ( @macgyvermedical )
81 notes
·
View notes
Text
@ancatmom
I have read your reply and wanted to give it a better response than this, but this is the best I can do right now. This is because I am exhausted and need to sleep before I exert any brain power toward anything. This is also because, after the night I've had dealing with my census of entirely unvaccinated dying COVID-19 patients, your reply filled me with a level of frustration I haven't felt in a long time, and I am going to need to pace myself here so as to ensure what I say is actually helpful. It is easy to talk about these things theoretically, but when you are in my situation and dealing with the real-life consequences of anti-vaccine rhetoric, it gets harder to stay calm when faced with the not-so-subtle insinuation that you, a physician who spends most of your waking hours treating very ill COVID-19 patients and following all research to stay up to date on its trends, are either lying as part of a conspiracy or are, despite years of both performing biomedical research and learning how to interpret it, are somehow failing to do so adequately now, and thus failing your patients. I am trying to go slowly and play nice, but I can't promise I'll stay that way.
The short answer is that I can't reply to you because you have cited no sources. You refer to the many studies that contradict the CDC's position on vaccines (as if I only cited the CDC in my original post, when they were only one of many different sources I used...), but failed to provide them. I've looked over a lot of literature on this topic and while you will always have a few outlier studies that find something different, the overwhelming trend is consistent and reproducible data supporting vaccine use. The value of vaccines in protecting against severe disease, particularly ICU-worthy illness, intubation, and death, is what matters the most to me right now because frankly that is what is killing people and the health system. I have yet to see any research at all from a reputable source calling into question the use of vaccination in protecting against severe disease. If you have any studies you want me to look over that contradict any of this, please send them my way so I can fully review them. That way I could at least give you a response that means something. I like to believe that 11 years of higher education and employment in both medicine and medical research says at least something for my ability to interpret a research paper.
I really love that I cited a number of studies, but somehow everything gets dismissed by you because I also cited the CDC. Still, I defend my use of the CDC as a source. The CDC data (which I referenced most heavily while talking about adverse events) is pulled from VAERS data. It is the biggest national data set we have and I'd be an idiot not to refer to it when trying to get statistics for widespread trends. Just because the CDC is a big organization doesn't mean every scrap of data it produces is bullshit. I have used their data in the past and will continue to do so, especially when the trends they report are matching up consistently with what we are seeing anecdotally and what we are told to expect based on RCTs. The reason I cited their page directly for some things rather than link straight to the VAERs data or a research paper is because the VAERS raw data is a massive spreadsheet that is time consuming and difficult to parse through, and most casual Tumblr users probably do not know how to read and interpret a scientific article as that does require training. I still cited plenty of RCTs and other studies, but wanted to make sure I had those mixed with some more easily accessible sources.
This is not a fake pandemic. The vaccine is not a conspiracy to make you sick. Debate about vaccine and mask mandates if you want, but recognize the reality of the virus and the utility of vaccination. People are dying because they are failing to get vaccinated. Adverse side effects from the vaccine are very rare and almost always minor. ICUs are filled with the unvaccinated. Vents and CPAPs and BiPAPs are taken up by the unvaccinated, and they are still dying. Non-COVID patients are dying because COVID patients are using up all our resources. You say the CDC has an agenda as if you do not. Perhaps they do, but it is the agenda of the anti-vax crowd that has the highest body count right now, and I'm damn tired of being the one who has to pronounce your all's victims dead.
22 notes
·
View notes
Text
Liver Care Tablets in India
Syno Care
Medical Equipment Manufacturers in Mohali, India
We are a Manufacturer of Bipap And Cpap Masks - Face Bipap Mask, Bipap Cpap Mask Strap delivered by Syno Care Private Limited Mohali, India.
Explore Synergy Synocare Pvt Ltd, Established in the year 2019, is a fast growing company in manufacturing, importing and exporting of revolutionary Lithium Ion Battery, Solar Battery, Electric Vehicle Batteries, Medical Batteries etc. Lithium batteries are the future of emerging technology as it is more efficient, has a longer life span and provides reliable, stable, long lasting power.
Synocare Full Face Mask for Bipap Machine with Cushion Pads and Adjustable Headgear for Men and Women.
Nasal mask is designed to provide comfort and stability. The comfortable headrest is round stitched headgear for long use, Easy clip-on headgear clips.
360-degree swivel rotation of the elbow. More venting holes to reduce noise and effectively disperse airflow.
The soft cushion and different height forehead pad with pressure distribution technology for comfort.
Size – 154.93mm x 78.38mm x 60.51mm (L x W x H). Indigenous product completely made in IndiaHow to use – Fix the upper ends of the strap to the mask, attached the mask to the face, fix the lower strap to the mask, and then tighten the lower end of the strap. Install the main air hose for circulation.
Syno Care Pvt Ltd
09780313311
0 notes
Note
Hi! Can you please explain life support more than the basics, specifically someone coming off of it alive and the effects it would have on him/her physically and cognitively?
Hey there nonny! Thanks for this question. Let’s dive in!
��Life support” is an extremely nebulous term. For example, the term “basic life support” is a fancy way of saying CPR and rescue breathing, while “advanced cardiac life support” is a nice way of saying “extreme cardiac event resuscitation with tubes, IVs, and drugs.”
Both of those are real-life American Heart Association classes.

But I have a sneaking suspicion that what you mean by “life support” is closer to “life-saving care in the ICU.”
That still comes in a great many different forms. “Life support” is the term for the whole care package, the sum totality of all things that are directly assisting to keep the person alive. That might include --
feeding systems via nasogastric (NG) tubes
IV drips of life-saving medications, including sedatives if they’re intubated, and those that increase blood pressure such as norepinephrine
a breathing tube and a ventilator
a cardiac assistive device, such as a balloon pump (which is a pump connected to a balloon in the aorta), an LVAD (Left Ventricular Assist Device) or BiVAD (BiVentricular VAD) which are pumps in one or both ventricles, an Impella device (similar to a VAD but different technology), Berlin heart (a type of VAD)
ECMO (Extracorporeal membrane oxygenation), aka “pulmonary bypass”; this is a set of enormous IV tubing that hooks up to a big external filter where the blood is allowed to exchange carbon dioxide for oxygen
The character’s “life support” is entirely dependent on what’s wrong and what they need.
I would say the most common thing people mean when they say “life support” is a ventilator, because it’s extremely common and it takes over a natural and basic function -- breathing.
As for a character coming off the ventilator, this is also an extremely common occurrence! The point of a ventilator is, in most cases, a temporary way to help the lungs oxygenate (with pressure support), and a way to reduce the workload of breathing (which can help other parts of the body). Characters may also be intubated for “airway protection,” meaning that they have a high risk of vomiting and not being able to clear it on their own.
Coming off the ventilator is a decision made by the doctors about the character’s health. They’ve decided that the character can breathe effectively on their own, or that they at least want to see whether or not they can.
So they disconnect the vent, deflate the balloon at the end of the tube, have the character take a deep breath, and, as they exhale, they’ll pull the tube out of the throat. They may suggest that the character cough while it’s being removed as well.
If all goes well the character won’t need any kind of respiratory support, but if they need something, there are a lot of ways to help. Oxygen via a cannula (the little plastic bits you see in noses on TV all the time) helps a little bit, but if they need some pressure support without a vent, a face mask known as CPAP or BiPAP can get the job done. (More recently, high-flow nasal cannula, or HFNC, is coming into style as a way to give pressure support without obstructing the character’s mouth, so that they can eat and speak effectively. HFNC is usually very well tolerated.
After Effects
You asked about physical and cognitive effects of coming off of “life support.”
This is kind of hard to say. That’s because a large number of ICU patients wind up with delirium in the ICU and may develop post-traumatic stress even after leaving. ICUs are hard places to be: medications mess with your energy levels and sedation can really cause disorientation and possibly even hallucinations, physically, the character can’t move much; there are constant alarms everywhere to the point that I don’t know how ICU nurses survive without going bonkers.
Then there’s the fact that sometimes characters in the ICU are restrained, particularly if they have a breathing tube in and they try to pull it out. Imagine being in pain, unable to speak, and unable to move or request help. That’s a big deal from a psychological perspective.
Physically, intubation can be traumatic. Vocal cords can be damaged by the tube, leading to difficulty speaking, a raspy voice, etc. Also, artificial ventilation can cause some damage to the lungs, which can cause decreased ability to breathe after the fact, and may require pulmonary rehab. (This is less common than it used to be.)
IVs can cause bruising and pain. Norepinephrine in particular can cause necrosis of tissue further down the limb, which is why it’s usually given through a central line, a big IV in the groin, clavicle, or neck. Cardiac assist devices, like LVAD/BiVAD, are almost always permanent. Devices like balloon pumps, which are temporary, still leave whopping big holes in the groin and can cause toes down the leg to die due to obstructed blood flow.
And none of this even talks about why the person was in the ICU to begin with.
Some characters will get better, leave the ICU, and lead healthy normal lives again. Some will have permanent reminders of what it was that brought them there and how they felt in the unit. And some -- too many -- will die on the unit.
I hope this helped!
xoxo, Aunt Scripty
[disclaimer]
313 notes
·
View notes
Text
i think if we hadn't read Alice Wong, met our friend who uses a vent full time, & seen other vent users, we just would not have been able to see a future for ourselves where we can breathe. we arent at a point where we need invasive ventilation, but now that we're relying on the bipap for filtered air & our hypoventilation episodes during the day, we really rely on those images of bipap and vent users to see a future for ourselves. its really hard to see selfies with and without a bipap mask side by side and see both as recognizable, handsome/pretty, and social.
i havent figured out bipap bangs enough to feel confident sharing a selfie anywhere, but i did do a video appointment today and last week with it on and it was weird. like i could think clearer but i also had that hurdle of "will they recognize me as me? as an adult? as a person?" i needed to crawl over. im still crawling over it. i dont think id be able to do so if i didnt have those examples of ventilation users living, writing, learning, teaching, speaking, signing, breathing.
im still missing some of that access intimacy of like. feeling/being seen but i think ill get there. i know there's futures for people like us.
n e weigh. chag chanukah sameach and a freylikhn khanikeh to all my handsome/pretty crips. we'll make it. i know we will.
#alice also became nonspeaking recently n her piece on that experience was nice n i think similar#like in terms of recognizing ways of living and communicating that are often suppressed
1 note
·
View note
Text
Pneumo Care Health Private Limited Easy 2 Neb (E2N) Mask with Head Gear Vented - Large
Pneumo Care Health Private Limited Easy 2 Neb (E2N) Mask with Head Gear Vented – Large
Price: (as of – Details) Easy2Neb Mask (Vented) is the world’s first NIV Full Face Mask with universal Nebulization ports for BiPAP/CPAP Users. Easy2Neb Mask provides Aerosol providing during Non-Invasive Ventilation The Nebulizer port is between the expiratory port and the mask leading to higher deposition rates The unique mask design comes with an Auto Adjustable Frame and a Fused Dual Wall…

View On WordPress
0 notes
Link
ResMed AirFit F20 Full Face CPAP&BiPAP Mask
InfinitySeal cushion technology
The AirFit F20 features an InfinitySeal™ cushion – the most adaptive we’ve ever designed – along with a soft and flexible frame that includes integrated padding. The result is the mask that comfortably moves with you and provides a reliable seal throughout the night, regardless of sleep position.
QuietAir vent technology
QuietAir™ is our innovative diffuser vent technology within the mask elbow that makes the AirFit F20 89% quieter1 and 70% gentler than before2. Featuring small multidirectional openings over a widespread area, QuietAir breaks up exhaled air so that it’s spread out lightly.
Designed for simplicity
The AirFit F20 is designed to fit your lifestyle – featuring magnetic clips, a quick-release elbow and a simple design that make it fast and easy to put on as well as clean and reassemble.
Plush Headgear
The headgear is designed for extra comfort and stability providing you with a better night's sleep no matter your sleep position.
Compatible with AirMini
The AirFit F20 is compatible with our travel CPAP, AirMini.
Specification
Manufacturer: ResMed In the package:
Frame system
One select size cushion
Headgear
SHOP NOW
#CPAP#cpap machine#cpap therapy#Cpap Mask#Cpap Accessories#cpap equipment#philips respironics#philips respirator#cpap machine travel bags#travel backpack#nasal interface#Cpap Pillow#nasal cushions
0 notes
Text
Respiratory Helmets Can Decrease Need for Intubation and Spread of COVID-19 Virus

MedicalResearch.com Interview with:

Aurika Savickaite Aurika Savickaite RN Adult Gerontology Acute Care Nurse Practitioner Bulletproof Coach University of Chicago Medicine MedicalResearch.com: Would you briefly explain what is meant by helmet-based ventilation? How does it work? Response: For patients in respiratory failure, noninvasive positive pressure ventilation (NIPPV) is usually delivered through a nasal mask or facemask. Many patients develop pain, discomfort – even claustrophobia -- from using NIPPV systems. The transparent helmet was developed to improve the tolerance of noninvasive ventilation. It allows the patient to see, read, speak and drink without interrupting noninvasive positive-pressure ventilation (NPPV). The helmet has a sealed connection and a soft collar that adheres to the neck which helps prevent the air leaks that are very common with nasal- or face masks. High positive end-expiratory pressure (PEEP) is vital in treating patients in respiratory failure and thanks to helmets “none to minimum air leak” system, PEEP can be set high (up to 25). NIPPV via a nasal- or full-face mask typically begins to show air leaks when the required pressure exceeds 15-20cm H2O. MedicalResearch.com: Is it expensive? Available? Easy to use?

The noninvasive ventilation helmet is a transparent hood that covers the entire head of the patient and has a rubber collar neck seal.The University of Chicago Medicine Response: Helmets cost about $150 to $165, and currently are available from two companies: Sea-Long and Amron. We are updating the list of manufacturers 24/7. Link here: https://www.helmetbasedventilation.com/post/where-to-get-a-helmet-for-helmet-based-ventilation The helmet is easy to use and can be applied by a respiratory therapist or a nurse (based on experience). As noted on our website, new companies making helmets, but who are not ready to sell yet. That means that they are testing helmets and will be selling them soon. We get at least one to two calls daily from the USA manufacturers who want to start production. We guide them and connect them with professionals who know the process well and can expedite the production. Other world countries, including Brazil, Argentina, Israel, and Greece have contacted us and have been advised to start making the helmets. We share all the information that can help and encourage transparency. MedicalResearch.com: For whom should it be used, ie as first line therapy? Response: Helmets have been used for acute respiratory distress syndrome (ARDS) patients for many years in Europe, especially Italy. Studies show that 54 percent of ARDS patients avoided the need for intubation. When helmet based NIPPV was used - the ICU mortality rate was only 6 percent vs 54 percent for intubated patients. Today, based on international guidelines from pulmonologists around the world, helmets are preferred NIPPV for COVID-19 patients. The closed-airflow helmet system with a filter will prevent aerosolization of the virus and minimize the risk to medical personnel. Based on feedback from Italian doctors, this therapy will prevent intubation for 20 to 30 percent of COVID-19 patients. In COVID19 intubated patients, the mortality rate is 70 to 86 percent.
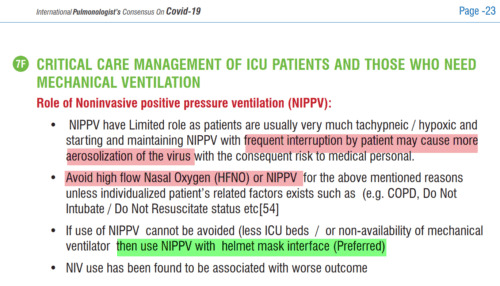
https://www.unah.edu.hn/dmsdocument/9674-consenso-internacional-de-neumologos-sobre-covid-19-version-ingles MedicalResearch.com: Is there anything else you would like to add? Response: With helmet NIPPV, the following issues can be resolved in the COVID19 pandemic: The shortage of ventilators: Helmets can be connected to oxygen with medical airflow or BiPAP machine. The shortage of medical staff and ICU rooms: Not all patients who are on NIPPV via helmet will need ICU rooms. Also, helmets are easy to manage and can be applied in a timely manner by respiratory therapists or nurses. Patients fail on prolonged NIPPV via nasal- or face mask and/or get intubated without trying NIPPV (guideline, vent shortages, etc): Helmets can be worn for a longer time and 20 to 30 percent of COVID-19 patients will avoid intubation. For many patients, symptoms will improve in the next one to two hours following helmet access and if no improvement is achieved, they will then get intubated. Any disclosures? HelmetBasedVentilation.com is a non-commercial private citizen initiative to organize information and help health care professionals learn the benefits of noninvasive ventilation (NIV) via the helmet. We publish information about the manufacturers, inventors and funding sources to help them connect so they can speed up the production of working helmets. The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website. Read the full article
0 notes
Text
The history of ventilators is a ‘remarkable journey’
From bed-sized iron lungs to portable, computer-controlled systems, the ventilators used to treat life-threatening respiratory diseases—and so much in demand today—have had a “remarkable journey.”
It was painful to watch. At the height of the epidemic, hundreds of patients arrived at hospitals, smothering or drowning in their own secretions. The demand for ventilators far exceeded their supply. Sound familiar?
In 1931, the epidemic was polio. The victims were mostly small children, many with lungs paralyzed by the disease. And the ventilator, invented just three years before at Harvard Medical School, was the “iron lung”—initially a rectangular metal box in which individual patients were placed with only their heads protruding.
Air pumps from two vacuum cleaners changed the pressure inside the box, pulling air in and out of the lungs.
Refined versions of iron lungs became the mainstay in treating polio victims during the next three decades. In 1939, the National Foundation for Infantile Paralysis began mass distribution of iron lungs, which cost about $1,500 each—then the average price of a home.
Eugene Farley neared completion of his medical degree at the University of Rochester during one of the last major polio outbreaks. Patients in iron lungs filled two wings of Strong Hospital. “Helping care for these patients paid for my senior year of medical school,” Farley says.
Even in the 1950s, however, the shortage of iron lungs was so acute that tubes had to be inserted in some patients through the mouth or by tracheotomy to force air into their lungs. This measure, previously used only in the operating room, also saved lives.
Back to normal breathing
Modern mechanical ventilators—whose short supply is now at the center of a national debate about the nation’s preparedness for the COVID-19 pandemic—bear little resemblance to the cumbersome iron lungs that saved thousands of lives before the development of a polio vaccine in the mid-1950s.
The modern devices—used to assist or actually substitute for a patient’s normal breathing in a wide range of clinical scenarios—are smaller, more portable, and are electronically controlled by microchips to exactly adapt air flow and pressure to an individual patient’s needs. They are the result of more than three centuries of experimentation and design.
And the Lord God formed man of the dust of the ground and breathed into his nostrils the breath of life. (Genesis 2:7)
And he [Elisha] went up, and lay upon the child, and put his mouth upon his mouth and the flesh of the child waxed warm. (II Kings 4:34)
As the two Old Testament passages above suggest, humans have known how to use mouth-to-mouth resuscitation to force air into stricken lungs—a form of “positive pressure” ventilation—at least as early as Biblical times.
However, Robert Hooke, the scientist who coined the word “cell,” may have been the first to experiment with mechanical ventilation. In the 17th century, he demonstrated that mechanical ventilation can help do the work of damaged lungs by using a bellows to blow air into the injured lungs of a dog.
During the 1800s and early 1900s, negative-pressure ventilators predominated, mimicking the normal breathing process. The systems worked because when we expand our rib cage and chest cavity, it decreases pressure in the cavity, causing the lungs to expand as well. That causes air inside the lungs to decrease—creating negative pressure relative to the atmosphere—which results in air flowing into the lungs through inhalation.
For example, in 1838 Scottish physician John Dalziel described a full-body type “tank ventilator.” It consisted of an airtight box in which a patient sat, with only the head protruding. Manually pumping air into and out of the box established negative pressure.
This led to the negative pressure “iron lungs” and eventually smaller, more portable devices used to treat polio victims.
For example, Rochester Review in June 1959 (page 26) reported that John H. McKeehan, a mechanical engineering alumnus living in Syracuse, had “taken it upon himself to see that the chest shell respirators, in which two neighbors who have been stricken with polio must live, are functioning properly night and day.”
McKeehan greased the devices and checked their batteries every month, and twice a year took the artificial lungs completely apart and rebuilt them. “‘This is a pretty tense job; it could be disastrous if I accidentally stripped a screw, for instance,'” he explained. To do this job he searched out and studied a service manual for the respirators “which are a compact version of the familiar iron lung.”
At the time, the devices were usually referred to as “respirators”—a term now used for protective face masks.
From past to present
In the 1960s there was a movement away from negative-pressure ventilators in favor of positive-pressure devices that force air into a patient’s lungs, either noninvasively with nose or face masks for less severe breathing problems or by invasively inserting tubes in a patient’s airway.
Robert Kacmarek, director of respiratory care at Massachusetts General Hospital and a professor of anesthesiology at Harvard Medical School, describes this “remarkable journey” in a 2011 paper.
“In just 50 short years we have gone from relatively crude, totally mechanical devices that could provide only machine-triggered volume ventilation to highly evolved microprocessor-controlled systems capable of any form of ventilatory support imaginable,” he writes.
These systems include:
CPAP (Continuous Positive Airway Pressure) machines, which deliver slightly pressurized air through a small nose mask. They are commonly used to treat sleep apnea but are also used for patients with pulmonary vascular disease and in Neonatal Intensive Care Units (NICU) for infants with breathing problems, such as respiratory distress syndrome. They have not been recommended for COVID-19 because of studies suggesting such devices can pump viruses into the air, potentially increasing the spread of a contagious disease.
BiPAP (Bilevel Positive Air Pressure) machines that raise the pressure to push air during inhalation, then lower it to allow exhalation. They are used to treat obstructive sleep apnea, chronic obstructive pulmonary disorder, pneumonia, asthma flare-up, poor breathing after an operation, and neurological disease that disturbs breathing. The settings on these machines may allow them to be adjusted to treat COVID-19 patients.
Invasive positive-pressure ventilator machines used for patients who cannot breathe on their own or suffer from severe respiratory disease. Air is delivered through tubes inserted in a patient’s airway. These machines, used in intensive care units and as anesthesia ventilators in operating rooms, are needed for treating severe cases of COVID-19.
Elizabeth Palermo, an assistant professor of clinical nursing and specialty director of the Adult-Gerontology Acute Care Nurse Practitioner Program at the School of Nursing, is grateful for the positive impact the machines have had.
For example, the microprocessors in modern ventilators “not only determine the pressure inside the lungs,” but also adjust the timing, flow, and delivery of pressure and air to the lungs so that they are “customized for the patient’s condition and help the patient work better with the vent,” she says.
“Ventilators used to take up a great deal of valuable space in a room. Now, they are smaller, something every nurse in a crowded patient room appreciates,” says Palermo. They also have more readable displays to easily attend to the patient’s performance on the vent.
“When transporting patients on ventilators from ICUs to diagnostic tests or the operating room, we used to have to manually breathe for them using a bag-like device,” she says. “Depending on how long the trip was, this could be exhausting for the nurse and not very comfortable for the patient. Now, ventilators are much more portable, so patients can stay on a ventilator as they are transported across the hospital.”
Ventilation technology takes a team
With the advances in technology have also come an increased recognition and understanding of the risks involved in mechanical ventilation, Palermo adds.
“We have learned that too much pressure delivered by the ventilator can further injure the lungs, above and beyond the damage done by the disease itself,” she says.
“Patients on ventilators are prone to pneumonia, skin ulcers, and weakness, among other problems. We have learned that heavily sedating patients on ventilators makes it harder for them to become free of the ventilator when their lungs have healed. Our recognition of these problems and the efforts made to prevent them are probably the most important advances I have seen.”
She cautions that “ventilators do not cure disease. They allow the health care team to provide supportive care and ensure adequate oxygen delivery while treatments, such as antibiotics for pneumonia, take effect, allowing lungs injured by something like coronavirus to rest and heal.”
Moreover, using a ventilator to manage a patient’s respiratory problem is not as simple as “let’s buy more ventilators,” Palermo says. It requires a team effort involving:
A knowledgeable physician, nurse practitioner, and/or physician assistant “to determine the need for ventilation and if it is consistent with the patient’s wishes or advance directives.”
A competent respiratory therapist who understands the technical aspects of the ventilator machine and can adjust the pressure, oxygen, and alarms to ensure the ventilator helps the patient without causing injury.
A competent nurse at the bedside, educated in caring for patients on ventilators, who can closely monitor a patient’s condition, respond to alarms, and use evidence-based practice to prevent injury or complications.
“The critically ill patient with respiratory failure due to COVID-19 needs a knowledgeable interdisciplinary team that communicates closely with each other to coordinate that patient’s care.”
Source: University of Rochester
The post The history of ventilators is a ‘remarkable journey’ appeared first on Futurity.
The history of ventilators is a ‘remarkable journey’ published first on https://triviaqaweb.weebly.com/
0 notes
Text
Rutgers Researcher Partners With NYU in Creating Sleep Apnea Machine Alternative to Ventilators and a Virus-Trapping Hood
The designs, using readily available components, will be free to medical personnel
A Rutgers researcher is testing modified sleep apnea machines intended to help relieve the shortage of mechanical ventilators for COVID-19 patients.
After testing for safety and efficacy, the design will be available free to medical professionals and can be created quickly using readily available components. It was created by a team led by Vikram Kapila, a professor at the New York University Tandon School of Engineering.
Patients using the modified breathing supports – called the NYU Tandon AirMOD – wear a nonvented mask with filters that trap the virus when they exhale and keep it from entering the environment. The machines also can be used as breathing support for critical care patients being eased off ventilators, thereby freeing those ventilators for other patients. Unlike other methods being used to convert these CPAP and BiPAP sleep apnea machines for COVID-19 use, these design modifications assemble in minutes and use FDA-approved off-the-shelf components in stock at most hospitals.
Rutgers is also testing a prototype for a second system called the NYU Tandon AirVENT. It is a portable, personal, negative pressure hood that sucks virus particles exhaled by the wearer into a filter and traps them. The hood was designed to allow health care workers easy access to the patient. It can be placed over possible COVID-19 patients in waiting rooms and be used in ICUs, while physicians intubate patients or during patient transfers.
Jorge Serrador, associate professor of pharmacology, physiology and neuroscience at Rutgers New Jersey Medical School, is testing both systems for safety and efficacy. “A normal CPAP or BiPAP machine would spread the virus widely because not only is the mask vented, but pressurized air from the system would amplify the dispersion of the virus. The AirMOD design cuts off that avenue of exhaust and uses a system that filters out the virus before it enters the environment,” he said.
To test the designs, Serrador measured how much carbon dioxide, which is expelled through breathing, is present outside the devices while they are being used. “When we turn on the fan inside the hood, we see the level of carbon dioxide outside the hood decrease to the level seen in normal room air, which indicates that expired air — and thus the virus — is not escaping,” he said. “Negative pressure rooms are already used safely for infectious disease patients. We have just created a personal negative pressure area around the patient’s head.”
The AirMOD design is less expensive than ventilators and has other benefits to health care workers, such as being portable and requiring minimal set-up. “There are also benefits to patients,” Serrador said. “It gives people the assistance they need in their natural breathing to maintain their oxygen levels while allowing their bodies to deal with the virus. Since they are not intubated, they do not need to be sedated and can talk, clear their throats and cough, which helps prevent pneumonia.”
0 notes
Text
Rutgers, NYU Create Sleep Apnea Machine Alternative to Ventilators and a Virus-Trapping Hood
The following article Rutgers, NYU Create Sleep Apnea Machine Alternative to Ventilators and a Virus-Trapping Hood is courtesy of Elly Mackay's Sleep Blog
A Rutgers researcher is testing modified sleep apnea machines intended to help relieve the shortage of mechanical ventilators for COVID-19 patients.
After testing for safety and efficacy, the design will be available free to medical professionals and can be created quickly using readily available components. It was created by a team led by Vikram Kapila, PhD, a professor at the New York University Tandon School of Engineering.
Patients using the modified breathing supports—called the NYU Tandon AirMOD—wear a non-vented mask with filters that trap the virus when they exhale and keep it from entering the environment. The machines also can be used as breathing support for critical care patients being eased off ventilators, thereby freeing those ventilators for other patients. These design modifications assemble in minutes and use FDA-approved off-the-shelf components in stock at most hospitals.
Rutgers is also testing a prototype for a second system called the NYU Tandon AirVENT. It is a portable, personal, negative pressure hood that sucks virus particles exhaled by the wearer into a filter and traps them. The hood was designed to allow health care workers easy access to the patient. It can be placed over possible COVID-19 patients in waiting rooms and be used in ICUs, while physicians intubate patients or during patient transfers.
Jorge Serrador, PhD, associate professor of pharmacology, physiology, and neuroscience at Rutgers New Jersey Medical School, is testing both systems for safety and efficacy. “A normal CPAP or BiPAP machine would spread the virus widely because not only is the mask vented, but pressurized air from the system would amplify the dispersion of the virus. The AirMOD design cuts off that avenue of exhaust and uses a system that filters out the virus before it enters the environment,” he says in a release.
To test the designs, Serrador measured how much carbon dioxide, which is expelled through breathing, is present outside the devices while they are being used. “When we turn on the fan inside the hood, we see the level of carbon dioxide outside the hood decrease to the level seen in normal room air, which indicates that expired air—and thus the virus—is not escaping,” he says. “Negative pressure rooms are already used safely for infectious disease patients. We have just created a personal negative pressure area around the patient’s head.”
The AirMOD design is less expensive than ventilators and has other benefits to health care workers, such as being portable and requiring minimal set-up. “There are also benefits to patients,” Serrador says. “It gives people the assistance they need in their natural breathing to maintain their oxygen levels while allowing their bodies to deal with the virus. Since they are not intubated, they do not need to be sedated and can talk, clear their throats and cough, which helps prevent pneumonia.”
The AirMOD modifications were also reviewed by pulmonologists and physicians at NYU Langone and other centers. The designs can be downloaded here.
from Sleep Review https://www.sleepreviewmag.com/sleep-treatments/therapy-devices/cpap-pap-devices/rutgers-nyu-sleep-apnea-machine-ventilators-virus-trapping-hood/
from Elly Mackay - Feed https://www.ellymackay.com/2020/04/10/rutgers-nyu-create-sleep-apnea-machine-alternative-to-ventilators-and-a-virus-trapping-hood/
0 notes