#bacterial pneumonia treatment
Explore tagged Tumblr posts
Text
Pneumonia & Your Lungs: Essential Facts for Better Breathing
Understand how pneumonia impacts your lungs, signs to look out for, and proactive steps to protect your respiratory health. Your guide to maintaining lung health.
To know more: https://lalithachestandskinhospital.com/blog/breathe-easy-understanding-the-impact-of-pneumonia-on-your-lungs/
chest hospital in karimnagar,top lung specialists,pulmonologist doctor near me,pneumonia treatment antibiotics,bacterial pneumonia treatment

#chest hospital in karimnagar#top lung specialists#pulmonologist doctor near me#pneumonia treatment antibiotics#bacterial pneumonia treatment
0 notes
Link
0 notes
Link
0 notes
Text
Treatment Options for Bacterial Pneumonia in Dogs and Cats
Bacterial pneumonia in dogs and cats is a serious respiratory condition that affects both dogs and cats. It can lead to severe health issues if not treated promptly. At Tri-County Animal Hospital, we prioritize your pet’s health and well-being, offering comprehensive treatment options for bacterial pneumonia in pets. Understanding the treatment options available can help pet owners make informed decisions and ensure their furry friends receive the best care possible.

Understanding Bacterial Pneumonia in Pets
Bacterial pneumonia is an infection of the lungs caused by bacteria, leading to inflammation and difficulty breathing. Common bacteria that cause pneumonia in pets include Bordetella bronchiseptica, Streptococcus, and Staphylococcus species. Pets with bacterial pneumonia often show symptoms such as coughing, difficulty breathing, lethargy, fever, and loss of appetite. If you notice any of these signs, it is crucial to seek veterinary attention immediately.
Diagnostic Process
Before starting treatment, a thorough diagnosis is essential. At Tri-County Animal Hospital, our veterinarians perform a series of diagnostic tests to confirm bacterial pneumonia and identify the causative bacteria. These tests may include:
Physical Examination: Listening to the lungs for abnormal sounds like crackles or wheezes.
Chest X-rays: To visualize the lungs and identify areas of infection and inflammation.
Blood Tests: To assess the overall health of the pet and identify any underlying conditions.
Tracheal Wash or Bronchoalveolar Lavage: Collecting samples from the lower airways to identify the specific bacteria causing the infection.
Treatment Options for Pet’s Bacterial Pneumonia
Once bacterial pneumonia in pets is diagnosed, prompt and effective treatment is necessary to ensure a full recovery. The treatment plan typically includes the following:
Antibiotic Therapy
The cornerstone of treating bacterial pneumonia in dogs and cats is antibiotic therapy. The choice of antibiotics depends on the type of bacteria identified and their sensitivity to specific drugs. Commonly used antibiotics include amoxicillin, doxycycline, and enrofloxacin. The treatment duration usually ranges from two to six weeks, depending on the severity of the infection and the pet's response to the medication. It is crucial to follow the veterinarian’s prescription and complete the entire course of antibiotics, even if the pet’s symptoms improve before the medication is finished.
Supportive Care
Supportive care is essential to help pets recover from bacterial pneumonia. This may include:
Hydration: Ensuring the pet remains well-hydrated to thin mucus and support lung function. In severe cases, intravenous fluids may be necessary.
Nutritional Support: Providing a high-quality, nutritious diet to support the immune system and overall health.
Oxygen Therapy: For pets with severe breathing difficulties, oxygen therapy may be administered to improve oxygen levels in the blood.
Nebulization and Coupage
Nebulization involves the administration of aerosolized medications to the lungs, helping to loosen mucus and improve breathing. Coupage, a technique that involves gently tapping the chest, can help loosen and clear mucus from the lungs. At Tri-County Animal Hospital, we demonstrate these techniques to pet owners for at-home care.
Anti-inflammatory Medications
In some cases, anti-inflammatory medications may be prescribed to reduce lung inflammation and alleviate symptoms. These medications should only be used under the guidance of a veterinarian, as improper use can have adverse effects.
Rest and Recovery
Ensuring that pets get plenty of rest is crucial for their recovery. Limiting physical activity and providing a calm, stress-free environment can help pets heal faster. It’s important to monitor your pet closely and follow any specific care instructions provided by the veterinarian.
Follow-up Care
Regular follow-up visits to Tri-County Animal Hospital are essential to monitor the pet’s progress and adjust the treatment plan as needed. Follow-up chest X-rays and physical examinations help ensure that the infection is resolving and that there are no complications. In some cases, additional diagnostic tests may be required to confirm the pet's recovery.
Preventing Bacterial Pneumonia in Pets
Prevention is always better than cure. Here are some tips to reduce the risk of bacterial pneumonia in pets:
Vaccination: Ensure your pets are up-to-date on their vaccinations, especially those protecting against respiratory infections.
Good Hygiene: Maintain a clean living environment for your pets, and avoid exposing them to other animals with respiratory infections.
Regular Veterinary Check-ups: Routine health check-ups at Tri-County Animal Hospital can help detect and manage underlying health issues that may predispose pets to pneumonia.
Healthy Diet: Provide a balanced diet to support your pet's immune system and overall health.
Conclusion
Bacterial pneumonia in dogs and cats is a serious condition that requires prompt and effective treatment. At Tri-County Animal Hospital, we are dedicated to providing comprehensive care to help your pets recover and thrive. By understanding the treatment options and following the veterinarian's guidance, pet owners can ensure their furry friends receive the best possible care and make a full recovery. If you suspect your pet has bacterial pneumonia, don’t hesitate to contact us for an evaluation and personalized treatment plan.
#Bacterial Pneumonia in Pets#Bacterial Pneumonia in Dogs#Bacterial Pneumonia in Cats#Dog and Cat Respiratory Health#Tri-County Animal Hospital#Pet Pneumonia Treatment#Comprehensive Pet Care#Veterinary Pneumonia Treatment#Respiratory Conditions in Dogs and Cats#Pet Health Information#Treating Pneumonia in Pets
0 notes
Text
"A new study evaluated a low-cost yet effective way to combat bacterial resistance using curcumin–the natural yellow plant compound in turmeric.
In 2017, a tragic death in a Nevada hospital was linked to a new strain of bacteria that had developed a resistance to 26 different antibiotics. Called ‘superbugs’, such antibiotic-resistant bacteria (including MRSA) remains a pressing public health threat.
Now researchers at Texas A&M University have shown that curcumin, the compound that gives turmeric its characteristic bright yellow color, can be used to reduce this antibiotic resistance.
They showed that when curcumin is intentionally given to bacteria as food, and then activated by light, it can trigger deleterious reactions within these microbes, eventually killing them. They demonstrated that this process reduces the number of antibiotic-resistant strains and renders conventional antibiotics effective again.
The results of the study were published this week in the journal Scientific Reports.
“We need alternative ways to either kill the superbugs or find a novel way to modify natural processes within the bacteria so that antibiotics start to act again,” said Dr. Vanderlei Bagnato, professor in the Department of Biomedical Engineering and senior author on the study.
Photodynamic inactivation, a technique that has shown promise in combating bacterial resistance, uses light and light-sensitive molecules, called photosensitizers, to produce reactive oxygen species that can kill microorganisms by disrupting their metabolic processes.
In the new experiments, the team used curcumin, which is also a natural food for bacteria. They tested this technique on strains of Staphylococcus aureus (MRSA) that are resistant to amoxicillin, erythromycin, and gentamicin.
The researchers exposed the bacteria to many cycles of light exposure and then compared the minimum concentration of antibiotics needed to kill the bacteria after light exposure versus those that did not get light exposure.
“When we have a mixed population of bacteria where some are resistant, we can use photodynamic inactivation to narrow the bacterial distribution, leaving behind strains that are more or less similar in their response to antibiotics,” Bagnato told Texas A&M News.
“It’s much easier now to predict the precise antibiotic dose needed to remove the infection.”
MORE PROGRESS ON SUPERBUGS: • The Humble Potato Could Hold Key to Beating Hospital Superbugs and Crop Diseases • Compounds in Amber Could Help Fight Drug-Resistant Bacteria Superbugs, Say Scientists • When Antibiotics Failed, She Found a Natural Enemy of the Superbug to Save Husband’s Life
The team noted that photodynamic inactivation using curcumin has tremendous potential as an adjuvant or additional therapy with antibiotics for diseases, like pneumonia, caused by antibiotic-resistant bacteria.
“Photodynamic inactivation offers a cost-effective treatment option, which is crucial for reducing medical expenses not only in developing countries but also in the United States,” said Dr. Vladislav Yakovlev, professor in the Department of Biomedical Engineering and author on the study..."
-via Good News Network, February 8, 2025
#superbugs#immunology#epidemiology#microbiology#turmeric#antibiotics#antibiotic resistance#public health#medical news#medical research#good news#hope
895 notes
·
View notes
Text
(Image descriptions are in alt text due to taking up most of the post and making people less likely to read and reblog, a fully screen reader friendly version can be found here: https://www.tumblr.com/nightmaretour/761524737363099648/this-is-the-fully-screen-reader-friendly-version)

With everything going on, it's easy to miss that September is sepsis awareness month. As a sepsis survivor myself, I feel a great responsibility to spread awareness of this greatly underestimated killer, in hopes that this information might help some of you to save a life in the future.

Sepsis is a disease that affects around 49 million people worldwide every year, and responsible for around 20% of all global deaths, claiming approximately 11 million lives per year. It's estimated that one person dies of sepsis every 2.8 seconds. Around half of those who survive sepsis are left with physical or cognitive disabilities for the rest of their lives. On top of that, it's the most vulnerable of us that are most likely to develop sepsis.

Despite being one of the global leading causes of death, very few people know much about sepsis or how to spot it, which is what makes it all the more deadly. Sepsis kills approximately 1 in 6 people who contract it, but spotted early, patients with sepsis are around half as likely to die as those who have been allowed to develop into the later stages.
Sepsis is always the result of an existing bacterial, viral, fungal or even parasitic infection, usually due to a serious infection such as pneumonia or meningitis, but it can also be caused by something as small as an infected papercut or bug bite. Almost half of all cases occur in children.

But most importantly, it's all about time. If you or someone you know is experiencing any symptoms that you suspect might be sepsis, get to a hospital. It's far better to be wrong and live than it is to be wrong and die. I sincerely hope that you will never have to use this information, but if you do, I hope that it will help you to save a life.

Sepsis is incredibly time sensitive, even a few hours could be the difference between life and death. If you spot any of the signs in yourself or someone else, do not delay. Seek emergency treatment immediately.
For more information, visit:
Worldsepsisday.org
Globalsepsisalliance.org
Sepsisresearch.org.uk
Sepsis.org
244 notes
·
View notes
Photo
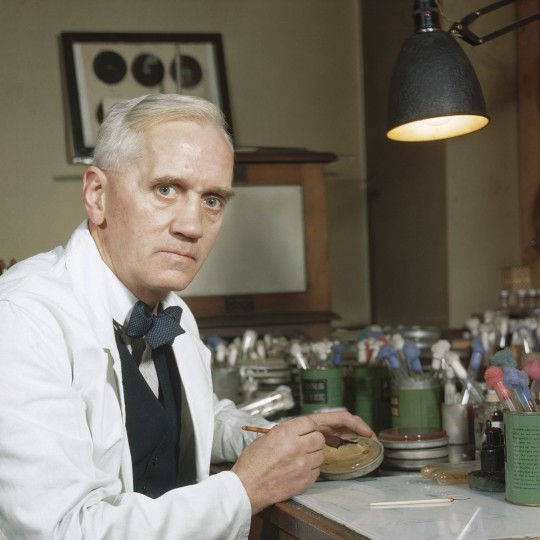
Discovery of Penicillin
The age of antibiotics began in September 1928, with the discovery of penicillin by Alexander Fleming (1881-1955), then a professor of bacteriology at St. Mary's Hospital in London. Previously there were no effective treatments against a range of bacterial infections from pneumonia to sepsis.
Penicillin became the basis for curing bacterial infections including smallpox, cholera, tuberculosis, scarlet fever, pneumonia, gonorrhea, meningitis, and diphtheria. Later antibiotics would form a class of medicines designed to combat, and cure, bacterial infections but also prevent the further growth of such infections.
Background
The use of fungi and molds, which contain antibacterial substances, to treat bacterial infections can be traced back to ancient cultures around the world, but these early attempts were unable to identify the component that provided the medicinal effect. Joseph Lister (1827-1912), an English surgeon and the "Father of antisepsis," recognized the antibacterial component of mold, but did not publish his findings. In the 1870s, Robert Koch (1843-1910), a German biologist, and Louis Pasteur (1825-1895) and Jules Francois Joubert (1834-1910), two French biologists, discovered the germ theory, which established that particular bacteria cause specific diseases. Additionally, they proved that the effects of introducing certain bacteria to various cultures inhibited the growth of more deadly bacteria.
The discovery of penicillin represented a turning point in medical history while Fleming would later be recognized by Time magazine as one of the most influential people of the 20th century:
When I woke up just after dawn on September 28, 1928 I certainly didn't plan to revolutionize all medicine by discovering the world's first antibiotic, or bacteria killer. But I suppose that is exactly what I did.
Continue reading...
172 notes
·
View notes
Text
Reference archived on our website
Abstract
Co-infection with diverse bacteria is commonly seen in patients infected with the novel coronavirus, SARS-CoV-2. This type of co-infection significantly impacts the occurrence and development of novel coronavirus infection. Bacterial co-pathogens are typically identified in the respiratory system and blood culture, which complicates the diagnosis, treatment, and prognosis of COVID-19, and even exacerbates the severity of disease symptoms and increases mortality rates. However, the status and impact of bacterial co-infections during the COVID-19 pandemic have not been properly studied. Recently, the amount of literature on the co-infection of SARS-CoV-2 and bacteria has gradually increased, enabling a comprehensive discussion on this type of co-infection. In this study, we focus on bacterial infections in the respiratory system and blood of patients with COVID-19 because these infection types significantly affect the severity and mortality of COVID-19. Furthermore, the progression of COVID-19 has markedly elevated the antimicrobial resistance among specific bacteria, such as Klebsiella pneumoniae, in clinical settings including intensive care units (ICUs). Grasping these resistance patterns is pivotal for the optimal utilization and stewardship of antibiotics, including fluoroquinolones. Our study offers insights into these aspects and serves as a fundamental basis for devising effective therapeutic strategies. We primarily sourced our articles from PubMed, ScienceDirect, Scopus, and Google Scholar. We queried these databases using specific search terms related to COVID-19 and its co-infections with bacteria or fungi, and selectively chose relevant articles for inclusion in our review.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
29 notes
·
View notes
Note
Pneumonia is no joke! I had it really bad as a kid and had to do these nebulozer treatment things (where you breath in the medicine through steam) and they were the only thing that helped. 🤧
I hope you feel better soon and the doctors give you stuff to help you breath better. 💜
((And if you’re not too dizzy, maybe try deep inhales over a steaming cup of coffee or tea. It might help some of the sharp crackles.))
thank you so much!!!!! ❤❤❤❤
my doc prescribed me with these huge fuckoff antibiotics on monday and I was back to 85% within the first two days (I just had to try not to overdo it immediately lmao)
but apparently it was something bacterial and nasty, and I'm so glad I went because I genuinely think I would still be sick right now otherwise. (I had a fever for 5 days before I went to see the doc which is probably not the best idea)
I lived off pills and tea during that time, and now I can finally taste again!!!!



thanks again and lots of love to you!!!! mwah mwah mwah!! <3
9 notes
·
View notes
Text
Update 3th April 2024
How are we into the 4th month of the year already? This year is slipping away so quickly. Anyway, my husband finished Radiotherapy mid Feb, had a few weeks off treatment, and is now on 6 cycles of strong chemotherapy. He has 5 days on tablet dose, then 23 days off, so its a 4 week cycle. We had an update meeting with his Neurologist. The tumour hasn't started to grow back, but we've got to add a 'yet' to that. The type of brain tumour (Glioblastoma) is an incredibly agressive form of brain cancer, spreading tendrils out into the crevices of the brain that there is never any way of scooping the whole thing out and getting every last bit with surgery. Thus the Radiotherapy and chemotherapy to try and blast - i cant think of a better word - as much remaining cancer as it can. He'll have regular MRI's to monitor any regrowth etc, and as he's mid 40's if he's strong enough he can have surgery again.
So now we're at the start of April and to be honest the last three months have been horrible. At the start of the year i caught a cough that developed into Bronchitis, and then by mid March i was so ill it was Pneumonia. When Hubby was on his 'rest' weeks post radiotherapy he was unable to rest as he had to help me care for our son. Sidenote; our Son's type 1 diabetes has been somewhat out of control during this time too. Two weeks ago i was admitted to the emergency dept at Hospital with chest pains. Hardly surprising with the amount of stress i'm under, but it turned out to be caused by bruising my internal chest muscles from coughing so much due to the pneumonia. Doctors told me i must rest. Well, the universe decided it didn't like that option and the day after Hubby went down with a cold/flu like virus, and because of his cancer treatment all but destroying his immune system, it's knocked him sideways. We're now 10 days later and its still in full force. I had to take him to the cancer hospital yesterday to have blood tests to ensure it hadn't turned bacterial (it hasn't) but we've been having awful nights sleep for the both of us which means neither of us are recovering at a rate we need.
So that's were we're at. Its just a massive cycle of illness followed by illness and it feels like we can't get out of it.
51 notes
·
View notes
Note
HI Miss Hill!!
Howlong does it take for a lung infection to go away?
🥇🐦
Hi! Thanks for sending an ask!!
The time it takes for a lung infection to go away depends on the type of infection, the severity of the infection, and your overall health. Acute lung infections typically clear up in a few days to weeks, while chronic lung infections can last for months or years.
Acute lung infections: Bacterial pneumonia: Most bacterial pneumonia can be cured in 1–2 weeks with treatment. Walking pneumonia and viral pneumonia: These types of pneumonia can take 4–6 weeks to go away. Viral infections: Most viral infections require your body to fight off the infection on its own.
Chronic lung infections: Chronic lung infections are more difficult to treat than acute lung infections. If your symptoms persist beyond a few weeks, you may have a chronic pulmonary infection.
#((I'm not a doctor and I use Google don't trust me for shit))#caroline hill rp#dc rp#tim drake rp#ask reply♡
6 notes
·
View notes
Text
Understanding Pneumonia: Symptoms, Causes & Treatment Insights
Explore the symptoms, causes, and treatment options for pneumonia. Get informed on how to effectively combat this respiratory illness and recover quickly.
To know more: https://lalithachestandskinhospital.com/blog/battling-pneumonia-understanding-symptoms-causes-and-treatment-options/

best pulmonologist in Karimnagar,md pulmonologist near me,best pediatric pulmonologist near me,bacterial pneumonia treatment,pneumonia treatment in hospital,respiratory infection treatment
#best pulmonologist in Karimnagar#md pulmonologist near me#best pediatric pulmonologist near me#bacterial pneumonia treatment#pneumonia treatment in hospital#respiratory infection treatment
0 notes
Text
New antibiotic kills pathogenic bacteria, spares healthy gut microbes
Article Date: May 29, 2024
Article Blurb:
Researchers have developed a new antibiotic that reduced or eliminated drug-resistant bacterial infections in mouse models of acute pneumonia and sepsis while sparing healthy microbes in the mouse gut. The drug, called lolamicin, also warded off secondary infections with Clostridioides difficile, a common and dangerous hospital-associated bacterial infection, and was effective against more than 130 multidrug-resistant bacterial strains in cell culture.
[...]
Numerous studies have found that antibiotic-related disturbances to the gut microbiome increase vulnerability to further infections and are associated with gastrointestinal, kidney, liver and other problems.
[...] In a series of experiments, Muñoz designed structural variations of the Lol inhibitors and evaluated their potential to fight gram-negative and gram-positive bacteria in cell culture. One of the new compounds, lolamicin, selectively targeted some “laboratory strains of gram-negative pathogens including Escherichia coli, Klebsiella pneumoniae and Enterobacter cloacae,” the researchers found. Lolamicin had no detectable effect on gram-positive bacteria in cell culture. At higher doses, lolamicin killed up to 90% of multidrug-resistant E. coli, K. pneumoniae and E. cloacae clinical isolates.
When given orally to mice with drug-resistant septicemia or pneumonia, lolamicin rescued 100% of the mice with septicemia and 70% of the mice with pneumonia, the team reported.
Extensive work was done to determine the effect of lolamicin on the gut microbiome.
“The mouse microbiome is a good tool for modeling human infections because human and mouse gut microbiomes are very similar,” Muñoz said. “Studies have shown that antibiotics that cause gut dysbiosis in mice have a similar effect in humans.”
Treatment with standard antibiotics amoxicillin and clindamycin caused dramatic shifts in the overall structure of bacterial populations in the mouse gut, diminishing the abundance several beneficial microbial groups, the team found.
“In contrast, lolamicin did not cause any drastic changes in taxonomic composition over the course of the three-day treatment or the following 28-day recovery,” the researchers wrote.
Many more years of research are needed to extend the findings, Hergenrother said.
[More in Article]
Note: The main scientific journal itself is paywalled (and not yet available in unpaywall nor sci-hub), Nature Journal Link
14 notes
·
View notes
Text
Healing Moments
Title: Healing Moments Fandom: TMNT 2003 Word Count: 3960 Author: aquietwritingcorner/realitybreakgirl Rating: K Characters: Raphael, Donatello, Leonardo, Michelangelo, Splinter, April O’Neil, Casey Jones Warning: NA Summary: Raph escaped Shredder’s ship with broken ribs. But broken ribs still have consequences. Notes: This was written for someone a bit back. I never published it outside of showing it to that individual, which was a shame. So I’m publishing it now! I hope you all enjoy it! ff.net || AO3
______________________________________
Healing Moments
Don sat next to Raph, wetting down a cloth and using his left hand to wring it out and lay it on Raph’s forehead. His brother turned his head slightly and murmured, but otherwise didn’t react to the cloth. Don frowned but didn’t leave his brother’s side. The rest of his family was sleeping, at least as much as any of them could with their injuries from Shredder’s Ship. It wasn’t unusual for any of them to be awake at odd hours because they just couldn’t get comfortable.
They should have been paying more attention to Raph being uncomfortable.
It had started with a cough. They hadn’t paid it much mind. As much as April and Casey cleaned, this farmhouse was old, and they were all sleeping in the attic. It wouldn’t be out of the realm of possibility that there was something up here or even just outside that Raph was mildly allergic to. Mike had even teased him a little bit about it.
But then the cough had gotten worse, and Raph had begun sleeping more. He had just brushed it off as healing, which also made sense. It took a lot of energy to heal, something that they, unfortunately, knew well. It was only when he had looked feverish, his eyes a bit glassy, his head a bit warm, that it had hit them that something else was going on. With April and Casey’s help—as they were the only ones uninjured and able to help the most effectively—Don gave Raph a look over.
Don didn’t have access to medical care. Here, at the farm, he didn’t even have access to his lab. He would have liked to confirm the illness that he was positive Raph had, but instead he had to make do with his observation and the very small lab he had set up in the barn. Still, he was certain that he knew what Raph had.
Pneumonia.
It made sense. Raph’s main injuries had been his ribs, which, of course, were near his lungs. With the pain of his broken ribs, Raph likely wasn’t breathing as deeply as he should have been. That would have set him up for an infection to settle in his lower lungs and turn into pneumonia. That was only confirmed by the way that Raph’s lungs sounded. That crackling was pretty distinctive, even in mutant turtles.
Don had immediately started on what treatments they could do at the farm. Making sure that Raph was sitting up instead of laying down, giving him over the counter pain killers, making sure he stayed hydrated, and having him sit in a steamy bathroom. Splinter had brought some of his teas with him, as well, and he made sure that Raph drank plenty of those. But it wasn’t enough. Raph continued to get worse, and Don had sent out April and Casey to see if they could get their hands on any antibiotics. He hadn’t questioned how they had managed to get what they did, he had just taken it.
Now they just had to hope that they were going to work on Raph and that he wouldn’t need something stronger.
“How is he?”
Don looked up at Leo’s voice, not terribly surprised to hear it. Leo hadn’t been sleeping much lately, and Don honestly wasn’t sure if it was emotional, or because of his injured shell. It was likely both.
Don looked back down at Raph. “He’s resting, at least. The fever is still up, though. I did manage to get him to drink some the last time he was awake.”
Leo nodded, standing over their brother. “That’s good at least. The medicine will help the fever, right?”
Don frowned. “The NSAID will help the fever. The antibiotics will help the infection, as long as it’s a bacterial infection.”
Leo paused. “What do you mean, ‘as long as it’s a bacterial infection’?”
Don looked back down at Raph, laying a hand on the back of his neck as a way to check his temperature. “Pneumonia in humans is most likely to be caused by a bacterial or viral infection. In turtles it can also be fungal. I highly doubt that it’s fungal, but it could be viral. If it is, the antibiotics won’t do him any good. We’ll have to rely on treating the symptoms and hope that his body can handle the rest. If it’s bacterial, then the anti-biotics will help.”
Leo was quiet for a moment. “How can you tell which kind it is?”
“Here?” Don said “I can’t. I’m making the best guess that I can. We’re just going to have to hope we’re lucky.”
Leo’s frowned deepened and he turned away. “Luck is not something I think we can rely on.”
Don sighed. “Well, it’s all we’ve got right now, Leo,” he replied, perhaps a little bit snippier than he needed to be. “So, we’ll have to make do.”
He turned his attention back to Raph as the other turtled started to cough. Don helped him sit up a bit more, and supported him as he coughed, none of his breaths as deep as Don had hoped they would be, but better than nothing. It sounded so very painful each time he did this, but coughing out the infection was a good thing, even if he knew it set Raph’s broken ribs aflame with pain.
With a sigh, Don helped to lean Raph back in his bed, making sure he was propped securely on the pillows and that he was as comfortable as he could be. Raph’s eyes cracked open, and he looked over at Don.
“Donnie?” he croaked out, his voice sounding rough and weak.
“Yeah, Raphie, it’s me,” Don said with a smile. “How are you feeling?”
“Awful.”
Don chuckled slightly. “Yeah, I’d imagine so. I’m guessing your ribs are pretty sore?”
“Yeah.”
“Do your lungs feel sore as well?” Don asked.
Raph paused a moment more before answering that one. “Yeah,” he said.
Don nodded. “I thought so. You just rest, alright? I’ll take care of things right now. We all will.”
Raph let out a bit of a grunt, winced, and then closed his eyes. It wasn’t long before he drifted off to sleep again. Don sighed, and moved the washcloth back to Raph’s head, keeping watch over his brother.
Leo watched the whole thing, not interfering with Don’s care, and then let out what sounded like an irritated sigh and walked away, going towards the window.
Don watched, and then turned back to Raphael, keeping his own sigh to himself, and replacing the cloth on Raph’s head.
~*~
Mikey wasn’t terrible surprised when he looked over and found Donnie asleep at Raph’s side. Mikey had come over to relieve Don, to give him a break from the constant watch he had been keeping on Raph. After all, even though Don was usually in charge of their care when they were sick, at this point Raph’s care really wasn’t anything that the rest of them couldn’t do. Helping Raph sit up to cough, trying to get him to drink water, putting cold cloths on his forehead to keep his fever down, those were all things that anyone could do. Don was just stubborn and didn’t want to leave Raph’s side.
So, Mike had come anyway, told Don that Master Splinter had sent him up to give Don a break, and not objected when Don wanted to stay nearby a little longer. He hadn’t been surprised when, within moments, Don had fallen asleep. Mike had draped a blanket over his purple-banded brother, made sure he wasn’t putting pressure on his arm, and then turned all of his attention to Raph.
His brother did not look good. Raph was always all strength and attitude, even when he was being soft and caring. Right now, he didn’t look like either of those things. He was propped up on a mound of pillows, cradling his shell to keep him almost upright. His mouth was open as he breathed, although his breaths were a bit gaspy. He was pale and didn’t look like he’d be able to hold up his head much less fight anything off.
Mikey didn’t like it.
“Heya, Raph, just me, come to check on you. Well, that and to give Donnie a break. You know how he gets when one of us is sick. He’s a worse mother hen than Leo!”
Leo… that was another brother to be worried about, although for a completely different reason. But Mike would come back to that later.
“He’s been with you most of the time, but, I mean, part of it makes sense. He does know the most, and he’s honestly the most mobile of us. Well, Leo might be too, but I think his shell hurts him more than he lets on, and Don fusses over it, too.”
Mikey was working as he was talking, taking the moment to check Raph’s temperature and make sure that the cloth on his head was nice and cool.
“Anyway, since I can’t do much more than sit on my butt and stare at the wall, I figured I might as well sit on my butt here, give Donnie a break, and grace you with my presence!”
Raph stirred under Mikey’s touch, and Mike leaned in as much as his broken legs would allow. “Raph?”
Raph’s eyes cracked open, and he blearily blinked at his brother. “Mike?” he mumbled, his voice weak. “S’you?”
Mike grinned at his brother. “Yep! The one and only! I decided to give Donnie a little break!”
Raph grunted a little, and his eyes traveled around until they landed on Don, who was asleep, hunched over the end of Raph’s bed. “Good.”
Raph started coughing again, shallow ones that sounded like they needed to be deeper. His face contorted in pain and his arms wrapped around his middle. Mikey reached over as best he could, supporting him. It was hard to see Raph in pain like this, and not be able to do anything about it. He rubbed Raph’s shell, trying to find a way to soothe him at least a little.
Coughing, he knew, was good with something like pneumonia. It brought up the junk in the lungs, and Mikey knew to use a little bowl to catch anything that Raph coughed up. As gross as it was, Donnie would want to examine it. But it also was hard to watch him be in pain from coughing with broken ribs.
As the coughing eased up, Mikey helped Raph lean back again, watching as his brother gasped for breath, pain still clear across his face. He picked up a glass of water with a straw and held it up to Raph. “Here, Raphie. Think you can drink some of this? You need to get some water in you.”
Raph gave a tired nod, still working on catching his breath back. But as soon as he could, he clamped his lips around the straw, drinking it slowly. Mikey held it up as long as Raph would drink it, and then sat it to the side. “Think you can swallow some pills? Don left a schedule for your medicine.”
Raph nodded, and Mikey fumbled around for the pills, doing the best to reach for the pills without hurting himself, too. He read the instructions, and then took out the correct dosages, helping Raph to take them and drink a bit more water.
“You think you can finish up this glass of water? It’d be good for you if you could.”
“Yeah…” The word was faint and tired, but it was there.
Mike held the glass up again, never once letting it drop and adjusting it so that Raph could get every last bit out if out.
“That’s good, Raph. I’ll see if we can get you a refill, okay? In the meantime, just lay back. I’ll get that cloth back on your head.”
“…thanks, Mikey.”
“No problem, bro,” Mike said with a smile. “Hey—why don’t I catch you up on what’s been going on!”
As Mike prattled on, talking for as long as he knew Raph was listening, and hoping that it brought him some comfort.
~*~
April looked over when she heard a small groan. She had been changing the water out, making sure that all of it was fresh after having sent all of the others either to rest or to go outside. They had all been taking turns looking after Raph and they all needed a break. She could take care of Raph for a while and let them have that break. They deserved it.
“Hey there, big guy,” she said when she noticed that Raph’s eyes were open. “About time you woke up. It’s nearly noon.”
Raph blinked around the room blearily. “…where’s…?”
“I sent them all out for some sunshine,” she said, finishing up with the water. “I’d send you out for it, too, but I don’t think you’re quite up for it yet.”
Raph leaned his head back and closed his eyes. “…sounds nice.”
April smiled at him. “Don’t worry, you’ll be out there soon enough.”
Raph merely let out a grunt and said nothing more. April went on about straightening up the attic—Despite the presence of Master Splinter, there were four teenaged boys living there—at least until she heard Raph start to cough. She turned around and frowned when she saw him starting to cough again, pain clear on his face. She immediately rushed to his side, putting an arm around him and taking some of his weight on herself.
The coughs were a little deeper than she had heard him have before, which was good, but the pain on his face wasn’t nearly as good and it tore at her heart. The guys were like little brothers to her, and she hated to see them all in this much pain. Still, she held him against her as he coughed and hacked, rubbing her hand on the rim of his shell, holding a cloth up to his face, and speaking soft, encouraging words to him.
When he finished, he was breathless, but he didn’t seem quite as breathless as she’d seen him before. Still, she helped to lay him back carefully, letting him catch his breath, and went to fetch him a glass of water.
“Here you go, Raph. Drink as much of it as you can, alright?” she said, carefully adjusting the glass at need. “Just take it at your own pace.”
April held the glass until Raph had finished it off, filling it up again and offering him more. Raph drank a little more until he finally stopped and laid his head back in the pillows that were piled up around him.
“…Thanks, Ape…” he said, his voice scratchy.
“It’s not a problem,” she said. April settled in beside him, taking care not to put stress on his lungs or ribs, and brought him to her, letting her little brother lean on her and relax. She gave the top of his head a peck. “What are big sisters for?”
~*~
“I think this commentator’s whack,” Casey said. “There ain’t no way they’re gonna win. They ain’t got the stats.”
Raph glanced over at Casey, from where both of them were watching the TV that he had managed to bring up the stairs and hook up enough to get the game. Raph still wasn’t up for much, but he had managed to stay awake through a couple of innings at least, which was more than last time.
Casey looked at him. “Don’t look at me like that, bro. They just pulled up three guys from the minor league after they traded off their top players. There ain’t no way they’re gonna do well after that.”
“…was stupid,” Raph agreed. “…but they got that guy… from Puerto Rico…”
“Yeah, he is really good,” Casey admitted. “But ya can’t rely on one guy to bring up the whole team! Besides, the other team managed to get four of the best players in the league!”
“…no others.”
“Yeah? Well, ya know what? Those three should be able to pull the team through!”
“YOU said—”
Raph’s rebuttal was cut off by a round of harsh coughing, which immediately brought the argument to an end. Casey abandoned his argumentative stance, instead moving to support Raph through the coughing, bringing up the small kidney bowl for him to spit anything out into. He kept a strong arm around Raph, making sure that he didn’t bend too far in his coughing, aggravating his ribs more.
As soon as Raph was finished, Casey helped him recline back on his mountain of pillows and sat the kidney bowl down.
“Hang on, Raph, lemme get ya some water.” Casey turned back to the water they were still keeping nearby and poured Raph some fresh into a cup. He helped Raph hold it, only letting go when it felt like Raph had a good hold on it, although he kept his hands hovering nearby. “Don’t drink it too fast, Raph. Ya don’t wanna throw up with broken ribs. Trust me on that one.”
Raph shot Casey a look, but he kept drinking the water anyway, draining it until the glass was empty. Casey poured him another one, and Raph started in on it too. Finally, he finished, and he let Casey take the glass, his arms dropping tiredly.
“…goofball.”
“Who me?” Casey said. “I ain’t the one that just tried to yell with pneumonia. Even I ain’t that stupid.”
Casey settled back down next to Raph and said nothing about the breadcrumb that Raph flicked at him, just flicking it back again. Raph flicked it back, and the two settled into a silent war as they watched the game.
~*~
“How are you feeling today, my son?”
Raph looked over at his father as Splinter carried a tray of tea towards him. “Better, Master Splinter,” he said, although his voice was still scratchy and weak.
“I am glad to hear it,” Splinter said with a smile. “I’ve brought you some food and tea, my son. Do you feel like eating?”
“I can try.”
“I would like that.”
Splinter sat the tray down and sat out the lap tray they had been using for Raphael’s meals. Taking his time, he sat some of the food on Raphael’s tray. Raph eyed the food that was left over. It was a lot of food, and Raph wasn’t sure he could eat all of that.
Splinter sat himself down next to Raphael’s bed. “I hope you do not mind if I take lunch with you, my son. Your brothers are otherwise occupied, and I believe that Mr. Jones and Ms. O’Neil would appreciate some time together.”
Raph smiled. So that’s why there was so much food on the tray. “Yer fine, Sensei.”
For a little bit, the two ate in relative silence, until Raph felt the urge to start coughing again. He tried to finish his bite and swallow before the urge hit, but he didn’t quite make it, some of the food coming out as he coughed.
Immediately, Splinter was at his side, a hand on his shell. “Keep coughing, Raphael, it is okay. Just keep coughing it up.”
Raph didn’t really have much of choice, but when he was finished, he sagged back on the pillows again, trying to catch his breath.
“S-sorry,” he started to apologize, mostly for the mess of food particles he had coughed out.
Splinter immediately dismissed it. “Do not apologize, my son. Believe me, this is far from the worst mess you and your brothers have left on me.” There was a trace of humor in his voice, even as he made sure that Raphael was settled and brushed the food away.
He reached for the tea, and held it to his son, helping Raphael to drink it. “Finish it all,” Splinter said. “And then, when you feel like it, finish what you can eat. I will be here with you.”
Raph couldn’t help the smile that touched his lips. Somehow, even at this age, knowing that his father was there was comforting.
~*~
Raph woke up, not sure what had woken him up until he looked over and saw the silhouette of Leo sitting beside him. Everyone else was asleep, and only the moonlight illuminated the attic room.
“…Leo?”
Leo shifted. “Did I wake you?” he asked.
Raph shook his head. “Dunno.”
Leo hummed.
For a moment, the two sat in silence, until Raph felt the urge to cough building again. He hated coughing at night, because it disturbed his whole family. Still, it couldn’t be denied, and it wasn’t long before Raph was coughing, holding his ribs as he did.
He felt Leo’s arm come around his shoulder, his other bracing Raph from the front, not letting him curl over on himself. Finally, the coughing fit finished, and Leo leaned Raph back.
“Here,” he said, bringing a glass up. “Drink some water.”
Raph took the glass, drinking the water slowly. Leo watched him closely, taking the glass when he was finished, and then sitting back at Raphael’s side. For a moment, neither of them said anything.
“…Do your ribs still hurt?”
“…yeah. But not as bad.”
More silence. Then…
“I’m sorry, Raphael.”
“Don’t be.”
They didn’t say anything else, but Leo sat by Raph’s side for the rest of the night, helping him anytime he needed it.
~*~
“Hey! Look who’s finally downstairs!” Casey said with a grin.
“Yeah, yeah,” Raph said, grinning, even if he was being supported by both Leo and Don on both sides.
“With his fever broken for a few days, and his ribs seeming to heal, it seemed a good time to bring him downstairs,” Don said.
“It’s good to see you down here,” April said with a smile.
Leo and Mikey helped Raph to the couch, where they carefully lowered him down.
“If you feel tired or if you need anything, make sure you tell us,” Don said, hovering over Raph.
“I will, Don, ya don’t have to hover,” Raph said.
“Dude, Don not hovering is like asking Master Splinter not to give us tea,” Mikey said.
“Which is exactly what I am bringing you now,” Splinter said. “And you will drink it.”
“I’m glad you’re feeling better, Raphael.” Leonardo said, giving his shoulder a squeeze before moving away.
“Thanks, bro,” Raph said, settling in on the couch and taking the tea that Master Splinter offered him. He let out a shallow sigh of contentment, glad to be out of the attic and among his family again.
“Hey—who wants to watch a movie?” Mikey asked.
“I’ll make the popcorn!” Don volunteered.
“I’ll come help you,” April said.
“What movie did you have mind?” Casey asked, leaning over to look at the collection they had brought with them.
Raph watched as Splinter settled down in a chair, and Leo moved closer to the family as they all gathered around. His ribs still hurt, he still had a cough, and he couldn’t breathe deeply, but he was glad to be here with his family. Maybe none of them were whole and healthy, but they were well on their way to healing at least—and with the way his family gathered around him, he could tell that they felt the same way.
Raph settled back, drank his tea, and listened to his family argue the finer points of the best Star Trek movie.
“Ya better just hope that Five ain’t the only one that still plays.”
He couldn’t help but grin at the cacophony of protests that rose at his words. Yeah. They’d all be fine in time.
9 notes
·
View notes
Text
Denis Rancourt Interview – The COVID-19 Illusion: Biological Stress-Induced Bacterial Pneumonia
Posted on December 27, 2024 Author Ryan Cristián
Joining me today once again is Denis Rancourt PhD, here to discuss his newest study breaking down the illusion that is COVID-19. We review his previous work on the topic highlighting how it is a clear mathematical possibility for a government to use preexisting illness numbers and conflate them with a current focus, combining that with false positives from PCR tests and deadly treatments (pre-COVID injection), all to create an illusion of a “novel” illness — whether a virus was ever there to begin with, or exists at all. We also discuss the (very well known) deleterious effects of lockdowns, masks, and of course the very deadly modRNA injections, and how all of these only added to this illusion when their effects were also conflated with the ever-shifting claims of the alleged “COVID-19” symptoms. We then discuss Denis’ recent research around the idea of what’s called “biological stress-induced transmission-less bacterial pneumonia” and the profound impact this has on the entire conversation, and to a degree, even bridges the gap between those who believe in terrain theory and those who believe in germ theory.
4 notes
·
View notes
Text
"An international research team has found almost a million potential sources of antibiotics in the natural world.
Research published in the journal Cell by a team including Queensland University of Technology (QUT) computational biologist Associate Professor Luis Pedro Coelho has used machine learning to identify 863,498 promising antimicrobial peptides -- small molecules that can kill or inhibit the growth of infectious microbes.
The findings of the study come with a renewed global focus on combatting antimicrobial resistance (AMR) as humanity contends with the growing number of superbugs resistant to current drugs.
"There is an urgent need for new methods for antibiotic discovery," Professor Coelho, a researcher at the QUT Centre for Microbiome Research, said. The centre studies the structure and function of microbial communities from around the globe.
"It is one of the top public health threats, killing 1.27 million people each year." ...
"Using artificial intelligence to understand and harness the power of the global microbiome will hopefully drive innovative research for better public health outcomes," he said.
The team verified the machine predictions by testing 100 laboratory-made peptides against clinically significant pathogens. They found 79 disrupted bacterial membranes and 63 specifically targeted antibiotic-resistant bacteria such as Staphylococcus aureus and Escherichia coli.
"Moreover, some peptides helped to eliminate infections in mice; two in particular reduced bacteria by up to four orders of magnitude," Professor Coelho said.
In a preclinical model, tested on infected mice, treatment with these peptides produced results similar to the effects of polymyxin B -- a commercially available antibiotic which is used to treat meningitis, pneumonia, sepsis and urinary tract infections.
More than 60,000 metagenomes (a collection of genomes within a specific environment), which together contained the genetic makeup of over one million organisms, were analysed to get these results. They came from sources across the globe including marine and soil environments, and human and animal guts.
The resulting AMPSphere -- a comprehensive database comprising these novel peptides -- has been published as a publicly available, open-access resource for new antibiotic discovery.
[Note: !!! Love it. Open access research databases my beloved.]"
-via Science Daily, June 5, 2024
#superbugs#bacteria#viruses#microbiology#antibiotics#medicines#public health#peptides#medical news#antibiotic resistance#good news#hope#ai#artificial intelligence#pro ai#machine learning
184 notes
·
View notes