#athetoid
Explore tagged Tumblr posts
Text
Cerebral palsy (CP) is a group of disorders that affect a child’s ability to move and maintain balance and posture, often due to brain damage that occurs during pregnancy, childbirth, or shortly after birth. The condition manifests in various forms, including spastic, dyskinetic, ataxic, and mixed types, each impacting movement control in distinct ways. Early diagnosis and intervention are crucial for managing CP, and kids neuro clinics in Dubai offer specialized care for children with this condition. Pediatric neurologists in Dubai are experts in evaluating the type and extent of cerebral palsy, providing personalized treatment plans to help manage symptoms. With advancements in cerebral palsy treatment in Dubai, therapies like physical therapy, occupational therapy, and speech therapy are commonly used to enhance motor skills and communication abilities, enabling children to achieve greater independence and improve their quality of life.
#types of cerebral palsy#hypotonic cerebral palsy#athetoid cerebral palsy#spastic cerebral palsy#ataxic cerebral palsy
0 notes
Text
Get Best Cerebral Palsy Occupational Therapy in India | Trishla Foundation
Trishla Foundation provides leading cerebral palsy occupational therapy in India, focusing on enhancing daily living skills and promoting independence. Their expert therapists use customized interventions to help individuals achieve their fullest potential in personal and social functioning.
#Athetoid Cerebral Palsy Symptoms#Athetoid Cerebral#Athetoid Definition#Athetoid Meaning#Athetoid Movement#Athetoid Movements#Cerebral Palsy Athetoid
0 notes
Text
Commission One Shot:Foxy Fucking

Now never it be said that Hinata Hyuuga wasn’t afraid to stand uo for herself, especially and particularly when it came to men who assumed she was a whore who’d be pretty much ready to bend over and cheat on her man. Really just because she was a kunoichi and happened to luck oint big time on puberty didn’t mean she was an easy lay but some guys just got the wrong idea. Which really put a damper on her good mood coming to this hot springs resort with Naruto and wouldn’t you know it, the Raikage happened to be in attendance along with Samui escorting him as is bodyguard. And the arrogant bastard sent her an invite to a private coed springs to discuss what he called “diplomatic relations”.
Which much to her annoyance and shock as well as the shock and confusion of Samui, consisted of the arrogant bastard flashing his naked body and demanding they service him like the bitches they were born to be. Or to put it bluntly, he liked them and he wanted them and they could do this the easy way or the hard way, the choice was theirs but really who was he kidding? It was going to be the hard way either way but Just so happened date had other ideas for this attempted cuckolding. You see this particular resort’s hot springs, especially this private one had a little secret in its waters, due to only having special properties for healing and relaxation…but a rather unusual affect on the bodies of women as the two kunoichi were about to find out first hand.
Neither of them was sure how or why it happened, was it their chakra mixing with the water or just some kinky, bizarre twist of fate but before the raikage knew it, Somethjng began to happen to the two Kunoichi’s bodies. Their thick curvy frames first beginning to grow in height and their Super model toned proceeding to grow slightly in muscle mass. And by slightly, I mean they began to bulk up and hulk out, going from fitness model athetoid tone into veritable woman mountains of muscle who did a lot more than lift, bruh!! Firm pecs ideal for supporting their juicy milk tank tits, tree trunk thighs capable of popping melons into juicy pulps, arms that needed a vet because they were some sick pythons and a set of washboard abs so cut that you could grate cheese off of them!!
They weren’t sure how or how it happened but they knew for sure just the sensations in their core alone made them orgasm so intensely that their thighs were soaked with sticky nectar. The lewd and cloud kunoichi recovering from their spontaneous sensual muscle growth to find they now towered over the stunned speechless raikage…and remembered just what the arrogant bastard had intended mere moments before. What followed was a sequence of violence so severe that this beatdown can’t be described in detail for the faint of heart but he was alive at the end. Albeit he’d be in traction for a while in the intensive care unit to say the very least, as he laid behind a clutch of rocks looking like a bruised and battered human pretzel.
As Hinata and Samui dusted off their hands, they couldn’t help but finally take notice of one another’s bodies and suddenly found themselves performing a showdown of pose offs. Crunching those six pack abs, flexing those biceps to make them pump and swell and clenching those firm powerful thighs while making those well toned bubbly booties clap. Only to pause when they were interrupted by the door to the private spring opening, revealing none other than Hinata’s husband, the whisker faced orange fox boy Naruto Uzumaki himself, standing in the frame slack jawed and bug eyed at the sight before him. The muscular amazonian beauties feeling no shame or embarrassment being caught in the nude, rather their gazes were drawn more to the raging hard tent being pitched under Naruto’s towel, sensually licking their lips as if some switch in their brain had been flipped.
Before the hyperactive knucklehead could ask what was going on and what had all that commotion had been that drew his attention to here moments ago, he suddenly found Hinata and Samui strutting over his way. For some reason he was hearing some heavy techno beat and the words by “Death! By Snusnu!!” over and over in his head like a mantra, as the amazonian kunoichi’s glorious titanic tires bounce and jiggled. The statuesque stunners making those delicious muscles ripple and flex with their silky movements as they squatted down to kneel before him and grabbed that towel. Pulling it off to expose the prize they sought, shuddering erotically as their pushes quivered with growing wanton need and desire at the length and girth that stood rigid before them and pulsed with a promise to fuck them so hard that no other man would ever suffice.
The next thing the knuckle headed hokage knew, he found himself laying on the cool marble floor as he was experiencing heaven on earth in the form his wife and the busty ice queen kunoichi performing a tandem fellatio on his cock. His length becoming soaked with a heavy coating of drool as they licked and kissed it, taking turns sucking and blowing on it as they deepthroated him with abandon. Their eyes burning with lust as they massaged and squeezed his balls, as if coaxing the baby batter contained within to come forth and give their thirst for his potent protein. Their pussies quivering as sticky juices flowed forth, making their intent to have that dick come fill them snd rut them deep and hard, wondering which of them woild be the first horny bitch to get some first.

Naruto of course made his answer clear as this lewd, slutty tag team blowjob caused the fox within him to take the helm, making his libido kick in as if primal instincts recognised the presence of bitches in heat who desired a virile alpha male to mate and breed with. Finding his arms moving on stint as they made a familiar hand sign, as in a massive burst of smoke, seven shadow clones stood around the muscular ninja girls. Looking around them in awe as they beheld those firm, stiff cocks just ready, waiting and able to grant their desire to destroy them. If Jiraiaya was watching from the afterlife, he’d likely be inspired with so much material for his icha icha books, that is after recovering from drowning in a puddle of his own blood from the nosebleed he’d be having.
Hinata and Samui of course wasted no time in seizing this wonderful opportunity presented to them by the former’s ever obliging husband, each having themselves four Naruto’s to service and pleasure. Starting things off with a little blowbang as as they shifted between stroking off a pair each while moving their heads back and forth to suck and blow them off, their mouths and throats becoming glorified oral pocket pussies for those bitchbreakers. Those lengths and girths pulsing in their silky palms and fingers as they deepthroated so intensely that those heavy balls were smacking their chins. But of course Naruto was never one to leave a lady to do all the work so it was omly right he begs to return the favour and bring a little of his foreplay A game to these muscular female works of art.
So to Hinata’s delight, she found her foursome working over her amazonian frame which had its quite gifted flexibility still available to her being put to its limits. One Naruto having her sit in his face as he ate her out, tongue probing her slit while another stood in front of her to hold her juicy tits between his shaft, pumping and thrusting into her cleavage like a man possessed as her naughty mouth and licked and sucked what came her way. The third knelt beside her as rubbed snd ground his cock along and against her abs, shuddering as those muscles ran along his length with massaging strokes. While the fourth squatted behind her, holding her glorious muscle booty as he thrust between those meaty cheeks to stroke his own cock off with them, pre flying and spraying her sculpted backside and painting her porcelain like skim.
Samui meanwhile was moaning with sensual delight and abandon as a pair of Narutos squeezed her tits as they licked and sucked on them, as if wanting to drain them of rich, delicious milk. The third had her sitting in his lap as his shaft pumped and thrust between her powerful thighs, her slit costing it in her sloppy flow of nectar. While her fourth stood beside her and her her curling and flexing her arm with his cock trapped by her bicep and forearm to stroke him off. To say he was clearly aroused by their newfound musculature was clearly an understatement.
Now if you’re wondering, not that you should really give a fuck but yes the raikage was still a human pretzel, unconscious behind some rocks and right about now eben in his comatose state? Had a feeling he was getting shown up and majorly, rightfully cuckolded because hey that’s karma baby!! But back to the real reason you’re all here right now which was seeing two hot buff ninja girls get the best lays in their entire lives by a one man gangbang. Rutted and fucked to such a degree thst quite frankly it’d be surprising if they didn’t wind up pregnant after this, the duo aroused at the idea of their washboard abs becoming round and full with the growing life of Uzumaki babies. Speaking of which, naturally the 8 deviant knuckleheads’ foreplay soon lesd to them getting some intense, hard and deep dicking as Hinata felt the rush and thrill akin to her first time and her honeymoon while Samui found any and every prior man she’d ever been with out to shame. Starting off with taking it from behind doggy style, their asses clapping every impact as those balls smacked their clits. While a pair of Narutos each knelt down in front of them holding their hair in firm grips as they performed powerful facefucking piston motions, the horny ninja muscle sluts taking it to their oral pussies like champs as those seed loaded balls smacked their chins. That of course was just the opening sequence to what was followed by an intense pornographic montage.
One moment Hinata would be held up in the air, the muscular filling of a Naruto sandwich as one hammered into her tight, naughty ass as the other hammered away into her sloppy, slutty pussy. While Samui rode one cowgirl style as she bounced and rode that Uzumaki dick with nymphomanic desire as another pounded her juicy ass, slapping those twin buns like besting a bongo drum. The next, the hokage wife was riding a Naruto in reverse cowgirl, stroking and sucking of a pair while Samui was on her back, taking it in a missionary position as she was getting fucked hard and fast, another Naruto straddling her shoulders as he pounded into her naughty mouth with vigorous lust. Her big tits bouncing and smacking his backside as the momentum of this particular spitroast was working her over hard.

The muscular Kunoichi Amazon duo relished each and every orgasm of course, especially the raw undiluted thrill of Naruto cumming on and inside of them. The rush of his white seed flowing and pumping into their wombs, intent to ensure there would be sum buns in those ovens. A constant tangle of limbs and bodies as they shifted between taint one on one to two or more, relishing being the centrepiece of their own combined orgy and gangbang. A new clone made whenever one poofed out or they wanted more Naruto cock to satisfy their erotic thirst. The hyperactive, unpredictable knucklehead truly making the most of that boundless stamina of his, was it all due to the newfound physical upgrade the kunoichi duo got or something that really motivated him today?
All he knew was eventually even after a constant round the clock stream of clones, Hinata and Samui were still ready and willing to go eben as the sun was starting to set. Now able to focus solely on the original himself and relishing his attention, coaxing him to keep mounting them like the bitches in heat they were and mark his claim and territory, whatever these springs had done to him also seemed to make their stamina a match for his. Not that he minded of course, his libido was still pretty much at the helm, telling him to keep at it as he had the muscular babes lay atop each other, watching them make out as he thrust his raging cock between their slits before fucking them in turn. Even after all the orgasms he had given them, they still yearned for his seed, intent on being bred.
Stil they showed no signs what so ever of stopping, even long into the night as they took it back to the hotel room the Uzumaki couple were staying in. Now driven to see to it that the bed would be destroyed and to keep at it until sunrise and perhaps even the rest of their stay. Meantime of course one of the staff had finally found the raikage, confused and shocked at the state he was in as he was doing in bandages and casts from head to toe. They’d never know what hit him, not even he could recall the how and why of it all, Hinata and Samui had beat the 7 shades of shit out of him so bad he suffered amnesia in regards to the before and after.
Not long after this vacation, Samui had herself transferred from Cloud to Leaf village as a live in ambassador , but unofficially she was the Hokage’s second wife. Her and Hinata turning heads with their newfound statuesque stunning muscles which they showed off with all manner of new outfits, only the more naughty or revealing stuff for their foxy man behind closed doors of course. As their bellies began to grow with new life, promising sweet little Himawari a few new brother or sister in the months to come. But of course they wouldn’t be the only kunoichi’s to get some from their whiskered baby daddy.
You see, Hinata and Samui maybe might have spread and shared details to certain fellow kunoichi friends of theirs about the private hot spring and it’s secret upgrade trick. Friends who happened to share equal parts admiring lust and love or their Uzumaki alpha male, having had many a sleepless night of intense wet dreams, being his personal bitches and baby factories. And who began to waste little to no time booking themselves some sessions in that spring as hey made p,and to give their favourite fox boy, or man rather, a little Amazonian surprise. When bitches wanted their Uzumaki, ooh you bet your ass they’d get their Uzumaki….
#sketchfan#sketchfanda#sketchfan85#naruto#naruto uzumaki#uzumaki naruto#hinata hyuuga#hyuuga hinata#samui#female muscle growth
26 notes
·
View notes
Text
What is Cerebral Palsy?
Cerebral palsy is a neurological disorder that affects movement, muscle control, and coordination. It is caused by damage to the developing brain, typically before or during birth. This condition can have a significant impact on individuals and their families, requiring specialized care and support.
According to the Centers for Disease Control and Prevention (CDC), cerebral palsy affects approximately 1 in 323 children in the United States. Despite its prevalence, there is often a lack of understanding and awareness about this condition and its different types.
In this article, we will discuss the four main types of cerebral palsy, the causes and risk factors, the process of diagnosis, treatment options, and resources available for individuals and families affected by this condition.

Types of Cerebral Palsy
Cerebral palsy is a neurological disorder that affects movement and muscle coordination. It is the most common childhood motor disability, with about 17 million people worldwide living with this condition. While the cause of cerebral palsy is not fully understood, it is important to understand its different types in order to provide appropriate treatment and support.
Four Main Types of Cerebral Palsy
· Spastic: This is the most common type of cerebral palsy, accounting for 70-80% of cases. It is characterized by stiff and jerky muscle movements, making it difficult to control the limbs.
· Dyskinetic: Also known as athetoid cerebral palsy, this type is characterized by uncontrolled and involuntary movements of the face, trunk, and limbs.
Read more
2 notes
·
View notes
Text
Cerebral Palsy Pain: Understanding and Managing Pain
For example, spastic cerebral palsy and athetoid cerebral palsy patients may experience permanently tightened muscles and suffer from pain in the legs, arms, shoulders, hips, neck, and back.
Ataxic cerebral palsy patients may develop pain in similar areas due to their poor posture and balance.
5 notes
·
View notes
Text
Cerebral Palsy Lawyer: Fighting for Justice and Fair Compensation
Introduction
Cerebral palsy is a neurological disorder caused by brain damage that leads to impaired movement and coordination. It often occurs as a result of complications during childbirth, making the role of a cerebral palsy lawyer crucial in ensuring justice and fair compensation for affected families. A specialized birth injury lawyer can help parents navigate the complex legal landscape surrounding birth injury cases, holding negligent parties accountable and providing support during a challenging time.
Understanding Cerebral Palsy
Cerebral palsy is a recommended birth injury lawyer near me term used to describe a group of disorders affecting movement and muscle tone or posture. It is often associated with brain injury or abnormal brain development that occurs while a child’s brain is still developing—especially during pregnancy, birth, or shortly after birth. Understanding cerebral palsy is vital in addressing the legal aspects of birth injuries.
Types of Cerebral Palsy
Cerebral palsy can be categorized into several types based on the symptoms and affected areas of the body:
Spastic Cerebral Palsy: Characterized by stiff muscles and awkward movements, this is the most common form of cerebral palsy. Athetoid Cerebral Palsy: This type involves uncontrolled movements, making it difficult to maintain a steady posture. Ataxic Cerebral Palsy: Affecting balance and coordination, ataxic CP can make walking and controlling body movements a challenge. Mixed Cerebral Palsy: Some individuals may experience a combination of symptoms from the different types.
The Role of a Cerebral Palsy Lawyer
A cerebral palsy lawyer specializes in handling cases where brain injuries during or before birth lead to cerebral palsy. Their main objective is to provide families with the legal representation they need to secure Best birth injury lawyer near me fair compensation for medical expenses, therapy, and other related costs incurred due to negligence.
When to Consult a Birth Injury Lawyer
Families affected by cerebral palsy should consider consulting a birth injury attorney if:
They suspect that medical negligence contributed to the injury. They wish to seek compensation for past and future medical expenses. They want to hold healthcare providers accountable for their actions.

Identifying Medical Negligence in Birth Injury Cases
In cases involving cerebral palsy, it is crucial to prove that medical negligence occurred. Some common examples include:
youtube
Failure to Monitor Fetal Distress: If healthcare providers do not recognize signs of fetal distress leading to cerebral palsy. Delayed Delivery: Failing to deliver the baby in a timely manner can result in oxygen deprivation, potentially causing cerebral palsy. Errors in Forceps or Vacuum Delivery: Misuse of these instruments can lead to physical trauma to the baby’s brain. Improper Management of Prenatal Complications: Neglecting to address issues such as maternal infections or diabetes can affect the fetus.
Choosing the Right Birth Injury Law Firm
Selecting a reputable birth injury law firm
1 note
·
View note
Text
¶ … cerebral palsy affects motor development. A brief introduction to cerebral palsy will be given, and then a more detailed look at exactly how motor development is affected will be entered into. Cerebral palsy is a general term for a variety of disorders caused by damage to the brain (Schuelein, 2002). The damage occurs before or during birth or in the first few years of life, and may cause severe crippling, or the symptoms may be so mild that they hardly interfere with the patient's activities (Schuelein, 2002). There are several types of cerebral palsy, and all involve lack of muscle control: common effects of the disorder include a clumsy walk, lack of balance, shaking, jerky movements, and unclear speech (Schuelein, 2002). In many patients, the brain damage also causes mental retardation, learning disability, seizures, and problems in sight and hearing (Schuelein, 2002). In most cases of cerebral palsy, the causes of faulty growth of the brain that result in cerebral palsy cannot be determined (Schuelein, 2002). In some cases, however, brain damage may result from illness in the mother during pregnancy; rubella can severely harm an unborn child, even though the mother may have had only mild symptoms or none at all during pregnancy (Schuelein, 2002). Brain damage can also occur during the birth process, especially in premature births (Schuelein, 2002). In babies born after a normal term of pregnancy, brain damage may occur if there is a significant period of hypoxia (lack of oxygen), which can cause brain cells to die (Schuelein, 2002). After birth, a baby may develop cerebral palsy if disease or injury damages the brain; during the first year of life, infections and accidental head injuries are the most frequent causes of the condition (Schuelein, 2002). There are four chief types of cerebral palsy: these are (1) ataxic, (2) athetoid, (3) hypotonic, and (4) spastic (Schuelein, 2002). In the ataxic form, the patient's voluntary movements are jerky, and a loss of balance is suffered (Schuelein, 2002). In the athetoid type, the person's muscles move continually; these movements prevent or interfere greatly with voluntary actions (Schuelein, 2002). A person with hypotonic cerebral palsy appears limp, and the person can only move a little or not at all because the muscles cannot contract (Schuelein, 2002). Spastic cerebral palsy patients have stiff muscles and cannot move some body parts (Schuelein, 2002). A person with cerebral palsy may have more than one muscle disorder, and the person may be only slightly disabled or completely paralyzed (Schuelein, 2002). Now we have seen what cerebral palsy is, how it can be classified (in borad terms) and how cerebral palsy can be caused, and, further, have looked at the various types of cerebral palsy, we will look in more detail at the specific effects of cerebral palsy on motor development, through a review of the measures used by clinicians to assess cerebral palsy. Cerebral palsy can be caused by a static lesion to the cerebral motor cortex that is acquired before, at, or within 5 years of birth (Dabney et al., 1997). Multiple causes for the condition exist and include cerebral anoxia, cerebral hemorrhage, infection, and genetic syndromes (Dabney et al., 1997). Cerebral palsy is commonly classified according to the type of movement problem that is present (spastic or athetoid) or according to the body parts involved (hemiplegia, diplegia, or quadriplegia) (Dabney et al., 1997). To care for children with cerebral palsy, a team approach is most effective; the team should include pediatrician and orthopedist, among others (Dabney et al., 1997). In the non-ambulatory patient, good sitting posture, the prevention of hip dislocation (spastic hip disease), and the maintenance of proper custodial care are prime concerns (Dabney et al., 1997). Careful monitoring and treatment of spastic hip disease and the correction of scoliotic spinal deformity are also important (Dabney et al., 1997). In the ambulatory patient, the main goal is to maximize function; computerized gait analysis in patients with complex gait patterns helps to show whether orthotic or surgical treatment is indicated (Dabney et al., 1997). Damanio and Abel (1996) showed that certain gait parameters, that are used to measure the degree of the lack of muscular control, are related to the computerised gait analysis, confirming that gait is representative of general motor status in cerebral palsy patients, and that the Gross Motor Function Measure and gait analysis are therefore complementary measures for the functional assessment of cerebral palsy patients (Damanio and Abel, 1996). The use of gait to assess motor function can therefore be a useful tool with which to assess the severity of cerebral palsy within the patient, and also to design the most effective treatment. Further to Damanio and Abel's (1996) paper, and Dabney et al.'s (1997) report, Barbosa et al. (2003) argued that understanding the natural history of development in children with cerebral palsy is important for studying the consequences of early intervention, and as part of this hypothesis looked at the Test of Infant Motor Performance and the Alberta Infant Motor Scale for a variety of infant ages, and found that the Alberta Infant Motor Scale is most effective in clinical settings, due to the greater ease of use of this scale for clinicians (Barbosa et al., 2003). In terms of the effects on motor development of cerebral palsy, as opposed to the diagnostic uses of deviances from 'normal' motor function, Hanna et al. (2003) have studied the development of hand function amongst children with cerebral palsy. As part of the study, assessments of hand function and the quality of upper-extremity movement were conducted on 29 males and 22 females and on four other occasions over 10 months (Hanna et al., 2003). Linear mixed effects modeling was used to estimate average developmental curves and the degree of individual differences in the patterns of development which were conditional on the body-site distribution of CP and severity of impairments (Hanna et al., 2003). The results indicate that hand function in this population of children with cerebral palsy develops differently from overall upper-extremity skills with declines in function in upper-extremity skills being more common and pronounced among older children (Hanna et al., 2003). Substantial inter-individual variation was, however, found, and it was found that the distribution of cerebral palsy and the severity of impairments in motor function were significant predictors of development (Hanna et al., 2003). In 2002, Rosenbaum et al. published a landmark paper on the subject of motor function in cerebral palsy and its application for prognoses (Rosenbaum et al., 2002). The paper stemmed from a lack of a valid classification method for the degree of severity of cerebral palsy, and its objective was to describe the gross pattern of motor development in children with cerebral palsy by severity, suing longitudinal observations (Rosenbaum et al., 2002). The study developed five distinct motor development curves, with which important differences in the rates and severity of cerebral palsy can be predicted, giving a method for evidence-based prognostication of gross motor progress in children with cerebral palsy (Rosenbaum et al., 2002). Yokochi has been an important contributor to the literature concerning motor function in cerebral palsy patients. His 1993 paper looked at motor function in infants with athetoid cerebral palsy, through the analysis of the motor function of 35 children with athetoid cerebral palsy using videotape recordings made at five to eight months of age (Yokochi et al., 1993). Many infants showed asymmetric tonic neck, Moro and Galant reflexes, and the movements which proved to be difficult included: keeping a symmetric supine posture, isolated movements of the hips and knees, forward extension of the upper extremity, extension of neck and trunk in the prone position and in ventral suspension, flexion of the neck in the traction response, and weight support by the upper extremities (Yokochi et al., 1993). Asymmetric or excessive opening of the mouth was also present in all infants, indicating a defect in motor function in all patients tested; it was hypothesised that the grade of difficulty for each posture and movement might reflect subsequent motor disability at three years of age (Yokochi et al., 1993). An earlier paper, Yokochi et al. (1990) looked at the gross motor patterns in children with cerebral palsy, by analysing rolling, sitting, and crawling patterns in 72 children with cerebral palsy and spastic diplegia; the relation between these patterns and the severity of the locomotive disability was studied (Yokochi et al., 1990). In rolling, trunk rotation and elbow support were difficult for the most severely diplegic children (Yokochi et al., 1990). When sitting, most patients had a between-heel sitting pattern in which the thighs were adducted and the knees were flexed (Yokochi et al., 1990). When crawling, the reciprocal thigh movements were insufficient and accompanied by lateral bending of the trunk in many patients (Yokochi et al., 1990). In the more impaired patients, the thighs supported the weight in flexion and did not move reciprocally (Yokochi et al., 1990). Creeping on the elbows without reciprocal leg movements was demonstrated in the most severely affected children after 2 years of age (Yokochi et al., 1990). A study by Kanda et al. (2004) has built upon the work of the Yokochi group, and has attempted to determine the clinical effectiveness of early onset long-term intensive physiotherapy on motor development in children with spastic diplegic cerebral palsy (Kanda et al., 2004). The study found that a consistently applied physiotherapy program resulted in better motor outcomes as compared to taking no physiotherapy, or inconsistently applied physiotherapy (Kanda et al., 2004). A further study (Sterba et al., 2002) looked at the effect of horseback riding on gross motor function in children with cerebral palsy, and found that this may help children with cerebral palsy in terms of improving gross motor function, which may reduce the degree of motor disability (Sterba et al., 2002). Treatment of cerebral palsy is aimed at preventing the condition from worsening and also helping the child use his or her abilities to the best possible advantage (Schuelein, 2002). Each type of cerebral palsy requires different therapy, and each patient needs individual care (Schuelein, 2002). The impact of cerebral palsy on people's lives obviously depends on the extent of their disabilities (Schuelein, 2002). As we have seen, most people with cerebral palsy can be helped by physical therapy. (Schuelein, 2002) If possible, the patient learns to maintain balance and to move about unaided, and in even the worst cases of cerebral palsy, it is found that through physiotherapy, the patient may develop such self-help skills as dressing, eating, and toilet care (Schuelein, 2002). Physicians may prescribe drugs for cerebral palsy patients to relax muscles and to control their convulsions (Schuelein, 2002). Braces and other mechanical devices provide support and help the victim walk, and in some cases, a surgical operation called selective posterior rhizotomy can reduce the rigidity of spastic muscles, although this is an extreme measure, in terms of the procedure, recovery times and the likely benefit to be gained (Schuelein, 2002). In summary, therefore, we have seen that cerebral palsy can have various effects on motor development and motor function in cerebral palsy patients: this manifests itself in varying degrees of immobility, and lack of motor control, which can be measured most easily by assessments of gait. Several tests have been developed with which to assess the trajectory of the cerebral palsy in the patient from a young age, and methods of 'controlling' the effects of this dis-abled motor function have been suggested, including prolonged, consistent physiotherapy and horseback riding, which have both been shown to be extremely beneficial to cerebral palsy patients, in terms of improving motor control. It is only in extreme cases that surgery is considered, and only then in patients that have the discipline to begin and to continue a challenging and prolonged physiotherapy program following surgery. Bibliography Barbosa, V.M. et al. (2003). Longtitudinal performance of infants with cerebral palsy on the Test of Infant Motor Performance and on the Alberta Infant Motor Scale. Phys. Occup. Ther. Pediatr. 23(3): 7-29. Dabney, KW et al. (1997). Cerebral palsy. Curr. Opin. Pediatr. 9(1): 81-8. Damanio, D.L. And Abel, M.F. (1996). Relation of gait analysis to gross motor function in cerebral palsy. Dev. Med. Child. Neurol. 3(5): 389-396. https://www.paperdue.com/customer/paper/cerebral-palsy-and-the-effects-it-has-on-167057#:~:text=Logout-,CerebralPalsyandtheEffectsitHasonMotorDevelopment,-Length8pages Hanna, S.E. et al. (2003). Development of hand function among children with cerebral palsy: growth curve analysis for ages 16 to 70 months. Dev. Med. Child. Neurol. 45(7): 448-455. Kanda et al. (2004). Motor outcome differences between two groups of children with spastic diplegia who received different intensities of early onset physiotherapy followed for 5 years. Brain Dev. 26(2): 118-126. Rosenbaum, P.L. et al. (2002). Prognosis for Gross Motor Function in Cerebral Palsy. JAMA 288: 1357-1363. Schuelein, M. (2002). Cerebral Palsy. World Book Encyclopedia for Macintosh. Version 7.1.1. Sterba, J.A. et al. (2002). Horseback riding in children with cerebral palsy. Dev. Med. Child Neurol. 44(5): 301-308. Yokochi, K. et al. (1990). Gross motor patterns in children with cerebral palsy and spastic diplegia. Pediatr. Neurol. 6(4): 245-250. Yokochi, K. et al. (1993). Motor function in infants with athetoid cerebral palsy. Dev. Med. Child. Neurol. 35(10): 909-916. Read the full article
0 notes
Text
Cerebral Palsy - Athetoid
Cerebral Palsy – Athetoid What is Athetoid Cerebral Palsy? Athetoid cerebral palsy (also known as “dyskinetic cerebral palsy”) is a movement disorder caused by damage to the developing brain. Children with athetoid CP fluctuate between hypertonia and hypotonia. Hypertonia is used to describe unusually high muscle tone, which creates stiffness and tension in the muscles. Hypotonia is used to…
View On WordPress
0 notes
Text
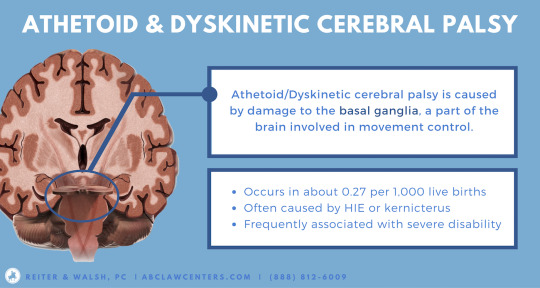
Dyskinetic Cerebral Palsy: An Overview
Dyskinetic Cerebral Palsy is one of the four subtypes of Cerebral Palsy and occurs due to damage sustained by the cerebellum or basal ganglia. It causes involuntary contractures and gait abnormalities that can be highly painful to navigate, which is why it is vital for children to start receiving treatment as early as possible. It is natural to feel overwhelmed if you hear that your child has Dyskinetic Cerebral Palsy, which is why having a thorough understanding of what to expect is critical. Here, we provide a brief guide to the same.
Understanding Dyskinetic Cerebral Palsy
Dyskinetic Cerebral Palsy is a subtype of Cerebral Palsy, which refers to a group of neurological disorders that affect movement, muscle tone, coordination, and motor skills caused by damage or abnormalities in the developing brain. It typically occurs due to injury or infection before, during, or shortly after birth. Dyskinetic Cerebral Palsy is a subtype characterized by abrupt involuntary movements that can be fast and jerky or slow and writhing. Often, children exhibit a range of symptoms on the basis of which doctors further subdivide the diagnosis. The two main Dyskinetic Cerebral Palsy types include:
Athetoid Dyskinetic Cerebral Palsy: This subtype leads to sudden movements in the limbs, hands, and feet, and sometimes the face and tongue. The movements may be jerky or slow and can be repetitive at times, or may be continuous and writhing and get worse as the child tries to move. Stress may exacerbate the movements.
Dystonic Dyskinetic Cerebral Palsy: This leads to random and twisting involuntary movements when the child tries to move on their own, which can be painful. Here too, the movements may be either fast or slow. Dystonia may occur all over the body or just in certain limbs.
However, these terms are often used interchangeably, and the causes and treatments are the same for both. As a non-progressive disease, Dyskinetic Cerebral Palsy will not worsen with time, although the patient’s needs may evolve as they grow older. Treatment helps to manage the symptoms and improve the patient’s overall functionality.
Symptoms of Dyskinetic Cerebral Palsy
Patients with Dyskinetic Cerebral Palsy have difficulty moving their muscles the way they want them to. The symptoms will vary based on the location and extent of the brain damage. There is considerable overlap between the symptoms of the Athetoid and Dystonic subtypes, which is why we can list them together. The commonly observed Dyskinetic Cerebral Palsy symptoms include:
Developmental delays in crawling, sitting up, standing, walking, or reaching for objects
Abnormal involuntary movements, either fast or slow
Twisting of the torso
Writhing movements in the hands or limbs
Pain during involuntary movements
Uncontrollable eye movements and/or squinting
Involuntary facial movements like grimacing or drooling
Muscle spasms from hypertonia or hypotonia and fluctuations between the two
Difficulty holding onto objects
Difficulties with balance and posture
Problems with speaking and swallowing
Comorbidities like epilepsy
The initial symptoms of Dyskinetic Cerebral Palsy, including jerky movements and poor balance, may be noticeable as early as nine months of age. However, some children may have irregular movement patterns simply because of a developmental delay and not Cerebral Palsy. Parents should thus avoid panicking and rely on the child’s doctor to provide a diagnosis.
Causes and risk factors of Dyskinetic Cerebral Palsy
Cerebral Palsy occurs due to damage to the brain before, during, or shortly after birth. Specifically, Dyskinetic Cerebral Palsy occurs due to damage sustained by either the cerebellum or the basal ganglia.
Basal ganglia damage: The basal ganglia are a group of nuclei located in the cerebral cortex, the part of the brain that controls voluntary movement. The basal ganglia also regulate learning and thinking. When the basal ganglia are damaged, motor function is disrupted, which leads to involuntary movements.
Cerebellum damage: The cerebellum regulates precision of movement, coordination, and balance, along with cognitive functions like attention and communication. When the cerebellum is damaged, it affects fine motor skills and general coordination, and may also lead to co-occurring conditions like epilepsy or autism.
The risk factors for Dyskinetic Cerebral Palsy include:
Infections during pregnancy
Complications during birth or negligence on the part of the physician
Premature birth
Blood clots in the placenta
Fetal strokes
Genetic conditions
Lack of oxygen during pregnancy or at birth
Jaundice, meningitis, or other infections shortly after birth
Head trauma sustained at or after birth
Diagnosing Dyskinetic Cerebral Palsy
There is no specific diagnostic test for Dyskinetic Cerebral Palsy. If you observe symptoms in your child, it is important to get an appointment with a doctor who will observe your child’s movements and reflexes in a clinic setting. As a parent, you will need to provide a full medical history for the child, including any conditions that run in the family, along with detailed information on your child’s symptoms.
If the doctor suspects Dyskinetic Cerebral Palsy, they may then recommend you to a specialist who will closely examine your child’s movement, speech, hearing, reflexes, posture, and coordination. Some of the tests they might order include an MRI, a CT scan, an electroencephalography (EEG), and an electromyography (EMG). These serve to identify brain damage and also rule out any other conditions that may be causing the symptoms. In addition, they may recommend specialists who will assess the child’s speech, hearing, vision, and intellectual capabilities. Getting a final diagnosis might take thus some time, up to several months in some cases. It is important to be patient and not panic unduly.
Treatment for Dyskinetic Cerebral Palsy
A treatment plan tailored to your child’s symptoms and abilities will help to expand their range of functional movement. The earlier the intervention, the better your child’s chances at gaining motor control and functionality. Typically, Dyskinetic Cerebral Palsy treatment will feature the following:
Physical Therapy: This is perhaps the most essential component of Dyskinetic Cerebral Palsy treatment. It includes a variety of exercises to improve muscle strength, coordination, and control over gross and fine motor skills. There will typically be daily sessions with a therapist, which may even be incorporated into the school day to make sure that the child is making consistent progress.
Occupational Therapy: This involves teaching the child how to perform daily activities of living on their own, such as getting dressed, having a bath, or feeding themselves. The therapist will teach them useful exercises that help them improve coordination and control, and may recommend special gadgets to make it easier.
Speech Therapy: Children who have trouble speaking and swallowing can benefit from Speech Therapy, as the therapist will teach them articulation techniques, safe swallowing techniques, and exercises to improve strength in the mouth and jaws. This not only helps them communicate better but also ensures that they are ingesting proper nutrition.
Stem Cell Therapy: This revolutionary form of treatment involves using the patient’s own healthy cells to treat the ones damaged by cerebellar degeneration. The process is safe, easy, and allows patients to go home the very same day.
Assistive devices: Thera[ists may recommend mobility devices like leg braces, walkers, or wheelchairs to help children get around more easily.
Medication/surgery: There are special medicines that doctors may prescribe to ease muscle stiffness and pain. In addition, surgery can correct significant deformities in the limbs and joints, thus helping children move more comfortably.
Yoga: Activities like yoga or stretching, when performed with a trained therapist, can help to alleviate the pain of muscle contractions.
Diet: The doctor may recommend special nutrition for your child to help their muscles grow properly.
Some parents may wish to sign their child up for alternative treatments like herbal medicine or acupuncture. However, always consult your doctor before doing so, as some of these treatments may interfere with the doctor-prescribed therapies.
0 notes
Text
What is Cerebral Palsy?
Cerebral palsy is a neurological disorder that affects movement, muscle control, and coordination. It is caused by damage to the developing brain, typically before or during birth. This condition can have a significant impact on individuals and their families, requiring specialized care and support.
According to the Centers for Disease Control and Prevention (CDC), cerebral palsy affects approximately 1 in 323 children in the United States. Despite its prevalence, there is often a lack of understanding and awareness about this condition and its different types.
Types of Cerebral Palsy
Four Main Types of Cerebral Palsy
· Spastic: This is the most common type of cerebral palsy, accounting for 70-80% of cases. It is characterized by stiff and jerky muscle movements, making it difficult to control the limbs.
· Dyskinetic: Also known as athetoid cerebral palsy, this type is characterized by uncontrolled and involuntary movements of the face, trunk, and limbs.
· Ataxic: This type of cerebral palsy affects balance and coordination, making it difficult to perform precise movements.
· Mixed: Some individuals may have a combination of two or more types of cerebral palsy, resulting in a mix of symptoms and challenges.
Causes and Risk Factors
Cerebral palsy is a neurological disorder that affects muscle coordination and movement. While the exact cause of cerebral palsy is unknown, there are several factors that can contribute to its development. These factors include brain injuries, infections, and genetic factors. read more about Cerebral palsy

1 note
·
View note
Link
#cerebralpalsy#cerebralpalsyresources#cerebralpalsysuccessstories#cerebralpalsysupport#inclusivesociety#managingcerebralpalsy#neurologicalconditions#raisingawareness#understandingcerebralpalsy
0 notes
Text
Understanding Cerebral Palsy: A Guide to Classification and Treatment Options
Cerebral Palsy (CP) is a group of neurological disorders that affect movement, muscle tone, and coordination. It can be caused by damage to the developing brain before, during, or after birth. Although cerebral palsy is a non-progressive disorder, it can affect a person’s mobility, communication, and daily living activities .
According to Northern Territory Government information and services, Cerebral Palsy in Australia is the most common physical disability in children, with an estimated 34,000 people affected. Early intervention and therapy can improve outcomes and quality of life for those with CP.
Classification of CP
There are five main types of cerebral palsy and each type of CP is characterised by specific symptoms and affects different areas of the body.
Ataxic Cerebral Palsy
Ataxic CP is less common, affecting around 5–10% of people with CP. It is caused by damage to the cerebellum, which is responsible for coordinating movement and balance. People with ataxic CP have poor balance and coordination, and they may have difficulty with fine motor skills, such as writing or buttoning clothes. They may also have a wide-based gait and may sway or stumble when walking.
Athetoid Cerebral Palsy
Athetoid CP, also known as dyskinetic CP, affects around 10–20% of people with CP. It is caused by damage to the basal ganglia, which is responsible for controlling movement. People with athetoid CP have involuntary movements that can be slow and writhing or fast and jerky. They may also have difficulty controlling their posture and may have trouble sitting upright or holding their head steady.
Hypotonic Cerebral Palsy
Hypotonic CP is a rare form of CP, affecting less than 5% of people with CP. It is caused by damage to the cerebellum or the brainstem, which can affect muscle tone and coordination. People with hypotonic CP have low muscle tone, which means their muscles are floppy and weak. They may also have difficulty with posture and may have trouble sitting upright or holding their head steady.
Spastic Cerebral Palsy
Spastic CP is th e most common type, affecting around 70–80% of people with CP. It is caused by damage to the motor cortex of the brain, which controls voluntary movement. People with spastic CP have increased muscle tone, which means their muscles are constantly contracted and can be stiff and difficult to move. They may also experience muscle spasms, especially when trying to move quickly. Spastic CP can affect one or both sides of the body, and it can also affect the legs, arms, or both.
Mixed Cerebral Palsy
Mixed type CP is a combination of two or more types of CP. For example, a person may have spastic and athetoid CP, or ataxic and hypotonic CP. The symptoms and severity of mixed type CP can vary depending on the types of CP involved.
Explore the comprehensive article for deeper insights into Understanding Cerebral Palsy Treatments
0 notes
Text
Different Treatment Options for Children with Dyskinetic Cerebral Palsy

Dyskinetic cerebral palsy is a type of disorder caused by involuntary movements. However, they are not as common as spastic cerebral palsy or not as rare as ataxic CP.
Athetoid cerebral palsy is a result of basal ganglia damage in the brain. As the basal ganglia are responsible for transferring messages to the body parts to coordinate and control movements, damage to it can cause abnormal and involuntary movements.
However, there are various treatment options one can opt for. Let's check them out here.
Treatment Options for Athetoid Cerebral Palsy
The first type of treatment highly advisable for athetoid cerebral palsy is physical therapy. In fact, physical therapy should be started as soon as the child reaches school age. The treatment can be included in his daily schedule at school, along with a weekend treatment session with a designated physical therapy center or at home with a licensed therapist. Traditional physical therapy don’t help so much for these children. They need relaxation, tome reducing posture and therapy to improve control and balance so that child can do they functional activity in smooth manner.
As children with dyskinetic cerebral palsy generally face communication problems, speech therapy must be provided along with physical therapy. Speech therapy can help the child learn to communicate efficiently. Moreover, it will assist them with chewing and breathing problems and learn the techniques with regular practice.
Further, various medications can be prescribed to a dyskinetic cerebral palsy patient. Since the primary symptoms of the issue are involuntary muscle movements, the medicines mostly prescribed are anticholinergics to help control muscle spasms and pain. While the other medications can include a muscle relaxant, gastric reflux, and medicines for sleep problems.
In case none of the oral medications work, other treatment plans include a baclofen pump in which a small pump is implanted in the abdominal wall of the child. The pump then disperses baclofen to the nervous system in regular increments.
In some cases, orthopedic surgery or is advised to correct limb deformities like contractures. However, surgery is limited for children with marked deformities who continue to experience pain while moving or walking.
Connect with the Right Medical Center
For dyskinetic cerebral palsy children, the treatment depends upon the severity of the brain damage. Children with minor symptoms can respond well to the treatments and live an independent life, while those with severe cases will need in-depth, long-term medical care. Trishla Foundation is the right medical care you should connect with to provide your child the treatment and care he deserves. Your child will indeed receive comprehensive care here from the industry-leading experts.
0 notes
Text
What is Cerebral Palsy?
Cerebral palsy is a neurological disorder that affects movement, muscle control, and coordination. It is caused by damage to the developing brain, typically before or during birth. This condition can have a significant impact on individuals and their families, requiring specialized care and support.
According to the Centers for Disease Control and Prevention (CDC), cerebral palsy affects approximately 1 in 323 children in the United States. Despite its prevalence, there is often a lack of understanding and awareness about this condition and its different types.
In this article, we will discuss the four main types of cerebral palsy, the causes and risk factors, the process of diagnosis, treatment options, and resources available for individuals and families affected by this condition.

Types of Cerebral Palsy
Cerebral palsy is a neurological disorder that affects movement and muscle coordination. It is the most common childhood motor disability, with about 17 million people worldwide living with this condition. While the cause of cerebral palsy is not fully understood, it is important to understand its different types in order to provide appropriate treatment and support.
Four Main Types of Cerebral Palsy
· Spastic: This is the most common type of cerebral palsy, accounting for 70-80% of cases. It is characterized by stiff and jerky muscle movements, making it difficult to control the limbs.
· Dyskinetic: Also known as athetoid cerebral palsy, this type is characterized by uncontrolled and involuntary movements of the face, trunk, and limbs.
Read more
1 note
·
View note
Photo

This is my daughter Talitha Grace The decision makers at PIP/DLA have decided that she does not qualify for any assistance. Talitha has Down's Syndrome, Athetoid Cerebral Palsy, Spastic Quadriplegia, a right sided Hemiparesis, a cardiac condition, is awaiting major spinal surgery for Scoliosis and has a feeding tube.
#a cardiac condition#a right sided Hemiparesis#At that time#Athetoid Cerebral Palsy#is awaiting major spinal surgery for Scoliosis and has a feeding tube#it was awarded for life#Please share#Spastic Quadriplegia#Talitha has Down&039;s Syndrome#The decision makers at PIP/DLA have decided that she does not qualify for any assistance#they stopped her DLA and we had to fight to get it reinstated#This is my daughter Talitha Grace#When Talitha was small#With many thanks to: Deborah McClenahan for the original posting
0 notes
Text
¶ … cerebral palsy affects motor development. A brief introduction to cerebral palsy will be given, and then a more detailed look at exactly how motor development is affected will be entered into. Cerebral palsy is a general term for a variety of disorders caused by damage to the brain (Schuelein, 2002). The damage occurs before or during birth or in the first few years of life, and may cause severe crippling, or the symptoms may be so mild that they hardly interfere with the patient's activities (Schuelein, 2002). There are several types of cerebral palsy, and all involve lack of muscle control: common effects of the disorder include a clumsy walk, lack of balance, shaking, jerky movements, and unclear speech (Schuelein, 2002). In many patients, the brain damage also causes mental retardation, learning disability, seizures, and problems in sight and hearing (Schuelein, 2002). In most cases of cerebral palsy, the causes of faulty growth of the brain that result in cerebral palsy cannot be determined (Schuelein, 2002). In some cases, however, brain damage may result from illness in the mother during pregnancy; rubella can severely harm an unborn child, even though the mother may have had only mild symptoms or none at all during pregnancy (Schuelein, 2002). Brain damage can also occur during the birth process, especially in premature births (Schuelein, 2002). In babies born after a normal term of pregnancy, brain damage may occur if there is a significant period of hypoxia (lack of oxygen), which can cause brain cells to die (Schuelein, 2002). After birth, a baby may develop cerebral palsy if disease or injury damages the brain; during the first year of life, infections and accidental head injuries are the most frequent causes of the condition (Schuelein, 2002). There are four chief types of cerebral palsy: these are (1) ataxic, (2) athetoid, (3) hypotonic, and (4) spastic (Schuelein, 2002). In the ataxic form, the patient's voluntary movements are jerky, and a loss of balance is suffered (Schuelein, 2002). In the athetoid type, the person's muscles move continually; these movements prevent or interfere greatly with voluntary actions (Schuelein, 2002). A person with hypotonic cerebral palsy appears limp, and the person can only move a little or not at all because the muscles cannot contract (Schuelein, 2002). Spastic cerebral palsy patients have stiff muscles and cannot move some body parts (Schuelein, 2002). A person with cerebral palsy may have more than one muscle disorder, and the person may be only slightly disabled or completely paralyzed (Schuelein, 2002). Now we have seen what cerebral palsy is, how it can be classified (in borad terms) and how cerebral palsy can be caused, and, further, have looked at the various types of cerebral palsy, we will look in more detail at the specific effects of cerebral palsy on motor development, through a review of the measures used by clinicians to assess cerebral palsy. Cerebral palsy can be caused by a static lesion to the cerebral motor cortex that is acquired before, at, or within 5 years of birth (Dabney et al., 1997). Multiple causes for the condition exist and include cerebral anoxia, cerebral hemorrhage, infection, and genetic syndromes (Dabney et al., 1997). Cerebral palsy is commonly classified according to the type of movement problem that is present (spastic or athetoid) or according to the body parts involved (hemiplegia, diplegia, or quadriplegia) (Dabney et al., 1997). To care for children with cerebral palsy, a team approach is most effective; the team should include pediatrician and orthopedist, among others (Dabney et al., 1997). In the non-ambulatory patient, good sitting posture, the prevention of hip dislocation (spastic hip disease), and the maintenance of proper custodial care are prime concerns (Dabney et al., 1997). Careful monitoring and treatment of spastic hip disease and the correction of scoliotic spinal deformity are also important (Dabney et al., 1997). In the ambulatory patient, the main goal is to maximize function; computerized gait analysis in patients with complex gait patterns helps to show whether orthotic or surgical treatment is indicated (Dabney et al., 1997). Damanio and Abel (1996) showed that certain gait parameters, that are used to measure the degree of the lack of muscular control, are related to the computerised gait analysis, confirming that gait is representative of general motor status in cerebral palsy patients, and that the Gross Motor Function Measure and gait analysis are therefore complementary measures for the functional assessment of cerebral palsy patients (Damanio and Abel, 1996). The use of gait to assess motor function can therefore be a useful tool with which to assess the severity of cerebral palsy within the patient, and also to design the most effective treatment. Further to Damanio and Abel's (1996) paper, and Dabney et al.'s (1997) report, Barbosa et al. (2003) argued that understanding the natural history of development in children with cerebral palsy is important for studying the consequences of early intervention, and as part of this hypothesis looked at the Test of Infant Motor Performance and the Alberta Infant Motor Scale for a variety of infant ages, and found that the Alberta Infant Motor Scale is most effective in clinical settings, due to the greater ease of use of this scale for clinicians (Barbosa et al., 2003). In terms of the effects on motor development of cerebral palsy, as opposed to the diagnostic uses of deviances from 'normal' motor function, Hanna et al. (2003) have studied the development of hand function amongst children with cerebral palsy. As part of the study, assessments of hand function and the quality of upper-extremity movement were conducted on 29 males and 22 females and on four other occasions over 10 months (Hanna et al., 2003). Linear mixed effects modeling was used to estimate average developmental curves and the degree of individual differences in the patterns of development which were conditional on the body-site distribution of CP and severity of impairments (Hanna et al., 2003). The results indicate that hand function in this population of children with cerebral palsy develops differently from overall upper-extremity skills with declines in function in upper-extremity skills being more common and pronounced among older children (Hanna et al., 2003). Substantial inter-individual variation was, however, found, and it was found that the distribution of cerebral palsy and the severity of impairments in motor function were significant predictors of development (Hanna et al., 2003). In 2002, Rosenbaum et al. published a landmark paper on the subject of motor function in cerebral palsy and its application for prognoses (Rosenbaum et al., 2002). The paper stemmed from a lack of a valid classification method for the degree of severity of cerebral palsy, and its objective was to describe the gross pattern of motor development in children with cerebral palsy by severity, suing longitudinal observations (Rosenbaum et al., 2002). The study developed five distinct motor development curves, with which important differences in the rates and severity of cerebral palsy can be predicted, giving a method for evidence-based prognostication of gross motor progress in children with cerebral palsy (Rosenbaum et al., 2002). Yokochi has been an important contributor to the literature concerning motor function in cerebral palsy patients. His 1993 paper looked at motor function in infants with athetoid cerebral palsy, through the analysis of the motor function of 35 children with athetoid cerebral palsy using videotape recordings made at five to eight months of age (Yokochi et al., 1993). Many infants showed asymmetric tonic neck, Moro and Galant reflexes, and the movements which proved to be difficult included: keeping a symmetric supine posture, isolated movements of the hips and knees, forward extension of the upper extremity, extension of neck and trunk in the prone position and in ventral suspension, flexion of the neck in the traction response, and weight support by the upper extremities (Yokochi et al., 1993). Asymmetric or excessive opening of the mouth was also present in all infants, indicating a defect in motor function in all patients tested; it was hypothesised that the grade of difficulty for each posture and movement might reflect subsequent motor disability at three years of age (Yokochi et al., 1993). An earlier paper, Yokochi et al. (1990) looked at the gross motor patterns in children with cerebral palsy, by analysing rolling, sitting, and crawling patterns in 72 children with cerebral palsy and spastic diplegia; the relation between these patterns and the severity of the locomotive disability was studied (Yokochi et al., 1990). In rolling, trunk rotation and elbow support were difficult for the most severely diplegic children (Yokochi et al., 1990). When sitting, most patients had a between-heel sitting pattern in which the thighs were adducted and the knees were flexed (Yokochi et al., 1990). When crawling, the reciprocal thigh movements were insufficient and accompanied by lateral bending of the trunk in many patients (Yokochi et al., 1990). In the more impaired patients, the thighs supported the weight in flexion and did not move reciprocally (Yokochi et al., 1990). Creeping on the elbows without reciprocal leg movements was demonstrated in the most severely affected children after 2 years of age (Yokochi et al., 1990). A study by Kanda et al. (2004) has built upon the work of the Yokochi group, and has attempted to determine the clinical effectiveness of early onset long-term intensive physiotherapy on motor development in children with spastic diplegic cerebral palsy (Kanda et al., 2004). The study found that a consistently applied physiotherapy program resulted in better motor outcomes as compared to taking no physiotherapy, or inconsistently applied physiotherapy (Kanda et al., 2004). A further study (Sterba et al., 2002) looked at the effect of horseback riding on gross motor function in children with cerebral palsy, and found that this may help children with cerebral palsy in terms of improving gross motor function, which may reduce the degree of motor disability (Sterba et al., 2002). Treatment of cerebral palsy is aimed at preventing the condition from worsening and also helping the child use his or her abilities to the best possible advantage (Schuelein, 2002). Each type of cerebral palsy requires different therapy, and each patient needs individual care (Schuelein, 2002). The impact of cerebral palsy on people's lives obviously depends on the extent of their disabilities (Schuelein, 2002). As we have seen, most people with cerebral palsy can be helped by physical therapy. (Schuelein, 2002) If possible, the patient learns to maintain balance and to move about unaided, and in even the worst cases of cerebral palsy, it is found that through physiotherapy, the patient may develop such self-help skills as dressing, eating, and toilet care (Schuelein, 2002). Physicians may prescribe drugs for cerebral palsy patients to relax muscles and to control their convulsions (Schuelein, 2002). Braces and other mechanical devices provide support and help the victim walk, and in some cases, a surgical operation called selective posterior rhizotomy can reduce the rigidity of spastic muscles, although this is an extreme measure, in terms of the procedure, recovery times and the likely benefit to be gained (Schuelein, 2002). In summary, therefore, we have seen that cerebral palsy can have various effects on motor development and motor function in cerebral palsy patients: this manifests itself in varying degrees of immobility, and lack of motor control, which can be measured most easily by assessments of gait. Several tests have been developed with which to assess the trajectory of the cerebral palsy in the patient from a young age, and methods of 'controlling' the effects of this dis-abled motor function have been suggested, including prolonged, consistent physiotherapy and horseback riding, which have both been shown to be extremely beneficial to cerebral palsy patients, in terms of improving motor control. It is only in extreme cases that surgery is considered, and only then in patients that have the discipline to begin and to continue a challenging and prolonged physiotherapy program following surgery. Bibliography Barbosa, V.M. et al. (2003). Longtitudinal performance of infants with cerebral palsy on the Test of Infant Motor Performance and on the Alberta Infant Motor Scale. Phys. Occup. Ther. Pediatr. 23(3): 7-29. Dabney, KW et al. (1997). Cerebral palsy. Curr. Opin. Pediatr. 9(1): 81-8. Damanio, D.L. And Abel, M.F. (1996). Relation of gait analysis to gross motor function in cerebral palsy. Dev. Med. Child. Neurol. 3(5): 389-396. Hanna, S.E. et al. (2003). Development of hand function among children with cerebral palsy: growth curve analysis for ages 16 to 70 months. Dev. Med. Child. Neurol. 45(7): 448-455. Kanda et al. (2004). Motor outcome differences between two groups of children with spastic diplegia who received different intensities of early onset physiotherapy followed for 5 years. Brain Dev. 26(2): 118-126. Rosenbaum, P.L. et al. (2002). Prognosis for Gross Motor Function in Cerebral Palsy. JAMA 288: 1357-1363. Schuelein, M. (2002). Cerebral Palsy. World Book Encyclopedia for Macintosh. Version 7.1.1. Sterba, J.A. et al. (2002). Horseback riding in children with cerebral palsy. Dev. Med. Child Neurol. 44(5): 301-308. Yokochi, K. et al. (1990). Gross motor patterns in children with cerebral palsy and spastic diplegia. Pediatr. Neurol. 6(4): 245-250. Yokochi, K. et al. (1993). Motor function in infants with athetoid cerebral palsy. Dev. Med. Child. Neurol. 35(10): 909-916. https://www.paperdue.com/customer/paper/cerebral-palsy-and-the-effects-it-has-on-167057#:~:text=Logout-,CerebralPalsyandtheEffectsitHasonMotorDevelopment,-Length8pages Read the full article
0 notes