#antifungal treatment size
Explore tagged Tumblr posts
Link
#market research future#antifungal treatment market#antifungal treatment industry#antifungal treatment analysis#antifungal treatment size
0 notes
Link
#market research future#antifungal treatment market#antifungal treatment industry#antifungal treatment analysis#antifungal treatment size
0 notes
Link
#market research future#antifungal treatment market#antifungal treatment industry#antifungal treatment analysis#antifungal treatment size
0 notes
Text
In February, a dermatologist in New York City contacted the state’s health department about two female patients, ages 28 and 47, who were not related but suffered from the same troubling problem. They had ringworm, a scaly, crusty, disfiguring rash covering large portions of their bodies. Ringworm sounds like a parasite, but it is caused by a fungus—and in both cases, the fungus was a species that had never been recorded in the US. It was also severely drug-resistant, requiring treatment with several types of antifungals for weeks. There was no indication where the patients might have acquired the infections; the older woman had visited Bangladesh the previous summer, but the younger one, who was pregnant and hadn’t traveled, must have picked it up in the city.
That seemed alarming—but in one of the largest and most mobile cities on the planet, weird medical things happen. The state reported the cases to the Centers for Disease Control and Prevention, and the New York doctors and some CDC staff wrote up an account for the CDC’s weekly journal.
Then, in March, some of those same CDC investigators reported that a fungus they had been tracking—Candida auris, an extremely drug-resistant yeast that invades health care facilities and kills two-thirds of the people infected with it—had risen to more than 10,000 cases since it was identified in the US in 2016, tripling in just two years. In April, the Michigan Department of Health and Human Services rushed to investigate cases of a fungal infection called blastomycosis centered on a paper mill, an outbreak that would grow to 118 people, the largest ever recorded. And in May, US and Mexican health authorities jointly rang an alarm over cases of meningitis, caused by the fungus Fusarium solani, which seemed to have spread to more than 150 clinic patients via contaminated anesthesia products. By mid-August, 12 people had died.
All of those outbreaks are different: in size, in pathogen, in location, and the people they affected. But what links them is that they were all caused by fungi—and to the small cadre of researchers who keep track of such things, that is worrisome. The experts share a sense, supported by incomplete data but also backed by hunch, that serious fungal infections are occurring more frequently, affecting more people, and also are becoming harder to treat.
“We don’t have good surveillance for fungal infections,” admits Tom Chiller, an infectious disease physician and chief of the CDC’s mycotic diseases branch. “So it’s hard to give a fully data-driven answer. But the feeling is definitely that there is an increase.”
The question is: Why? There may be multiple answers. More people are living longer with chronic illnesses, and their impaired immune systems make them vulnerable. But the problem isn’t only that fungal illnesses are more frequent; it is also that new pathogens are emerging and existing ones are claiming new territory. When experts try to imagine what could exert such widespread influence, they land on the possibility that the problem is climate change.
Fungi live in the environment; they affect us when they encounter us, but for many, their original homes are vegetation, decaying plant matter, and dirt. “Speculative as it is, it's entirely possible that if you have an environmental organism with a very specific ecological niche, out there in the world, you only need a very small change in the surface temperature or the air temperature to alter its niche and allow it to proliferate,” says Neil Stone, a physician and fungal infections lead at University College London Hospitals. “And it's that plausibility, and the lack of any alternative explanation, which makes it believable as a hypothesis.”
For this argument, C. auris is the leading piece of evidence. The rogue yeast was first identified in 2009 in a single patient in Japan, but within just a few years, it bloomed on several continents. Genetic analyses showed the organism had not spread from one continent to others, but emerged simultaneously on each. It also behaved strikingly differently from most yeasts, gaining the abilities to pass from person to person and to thrive on cool inorganic surfaces such as plastic and metal—while collecting an array of resistance factors that protect it from almost all antifungal drugs.
Arturo Casadevall, a physician and chair of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health, proposed more than a decade ago that the rise of mammals over dinosaurs was propelled by an inherent protection: Internally, we’re too hot. Most fungi flourish at 30 degrees Celsius or less, while our body temperature hovers between 36 and 37 degrees Celsius. (That’s from 96.8 to the familiar 98.6 degrees Fahrenheit.) So when an asteroid smashed into the Earth 65 million years ago, throwing up a cloud of pulverized vegetation and soil and the fungi those would have contained, the Earth’s dominant reptiles were vulnerable, but early mammals were not.
But Casadevall warned of a corollary possibility: If fungi increased their thermotolerance, learning to live at higher temperatures as the climate warms, mammals could lose that built-in protection—and he proposed that the weird success of C. auris might indicate it is the first fungal pathogen whose adaptation to warmth allowed it to find a new niche.
In the 14 years since it was first spotted, C. auris has invaded health care in dozens of countries. But in that time, other fungal infections have also surged. At the height of the Covid pandemic, India experienced tens of thousands of cases of mucormycosis, commonly called “black fungus,” which ate away at the faces and airways of people made vulnerable by having diabetes or taking steroids. In California, diagnosis of coccidioidomycosis (also called Valley fever) rose 800 percent between 2000 and 2018. And new species are affecting humans for the first time. In 2018, a team of researchers from the US and Canada identified four people, two from each country, who had been infected by a newly identified genus, Emergomyces. Two of the four died. (The fungus got its name because it is “emerging” into the human world.) Subsequently, a multinational team identified five species in that newly-named genus that are causing infections all over the world, most severely in Africa.
Fungi are on the move. Last April, a research group from the Washington University School of Medicine in St. Louis examined the expected geographic range in the US of what are usually called the “endemic fungi,” ones that flourish only within specific areas. Those are Valley fever in the dry Southwestern US; histoplasmosis in the damp Ohio River valley; and blastomycosis, with a range that stretched from the Great Lakes down the Mississippi to New Orleans, and as far east as the Virginia coast. Using Medicare data from more than 45 million seniors who sought health care between 2007 and 2016, the group discovered that the historically documented range of these fungi is wildly out of step with where they are actually causing infections now. Histoplasmosis, they found, had been diagnosed in at least one county in 94 percent of US states; blastomycosis, in 78 percent; and Valley fever in 69 percent.
That represents an extension of range so vast that it challenges the meaning of endemic—to the point that Patrick Mazi, an assistant professor of medicine and first author on the paper, urges clinicians to cease thinking of fungal infections as geographically determined, and focus on symptoms instead. “Let’s acknowledge that everything is dynamic and changing,” he says. “We should recognize that for the sake of our patients.”
Without taking detailed histories from those millions of patients, it can’t be proven where their infections originated. They could have been exposed within the fungi’s historic home ranges and then traveled; one analysis has correlated the occurrence of Valley fever in the upper Midwest with “snowbird” winter migration to the Southwest. But there is plenty of evidence for fungal pathogens moving to new areas, via animals and bats, and on winds and wildfire smoke as well.
However fungi are relocating, they appear to be adapting to their new homes, and changes in temperature and precipitation patterns may be part of that. Ten years ago, CDC and state investigators found people in eastern Washington state infected with Valley fever, and proved they had acquired it not while traveling, but locally—in a place long considered too cold and dry for that fungus to survive. A group based primarily at UC Berkeley has demonstrated that transmission of Valley fever in California is intimately linked to weather there—and that the growing pattern of extreme drought interrupted by erratic precipitation is increasing the disease’s spread. And other researchers have identified cases of a novel blastomycosis in Saskatchewan and Alberta, pushing the map of where that infection occurs further north and west.
The impact of climate change on complex phenomena is notoriously hard to prove—but researchers can now add some evidence to back up their intuition that fungi are adapting. In January, researchers at Duke University reported that when they raised the lab temperatures in which they were growing the pathogenic fungus Cryptococcus deneoformans—the cause of a quarter-million cases of meningitis each year—the fungus’s rate of mutation revved into overdrive. That activated mobile elements in the fungus’s genome, known as transposons, allowing them to move around within its DNA and affect how its genes are regulated. The rate of mutation was five times higher in fungi raised at human body temperature than at an incubator temperature of 30 degrees Celsius—and when the investigators infected mice with the transformed fungi, the rate of mutation sped up even more.
Researchers who are paying attention to rising fungal problems make a final point about them: We’re not seeing more cases because we’ve gotten better at finding them. Tests and devices to detect fungi, especially within patients, haven’t undergone a sudden improvement. In fact, achieving better diagnostics was top of a list published by the World Health Organization last fall when it drew up its first ranking of “priority fungal pathogens” in hopes of guiding research.
Multiple studies have shown that patients can wait two to seven weeks to get an accurate diagnosis, even when they are infected with fungi endemic to where they live, which ought to be familiar to local physicians. So understanding that fungi are changing their behavior is really an opportunity to identify how many more people might be in danger than previously thought—and to get out in front of that risk. “Patients are being diagnosed out of traditional areas, and we are missing them,” Mazi says. “All of these are opportunities to achieve better outcomes.”
33 notes
·
View notes
Note
hi! obligatory ‘I’m sorry if this sounds weird’ since it Feels weird at all to ask these questions, but. I’m AFAB and have an E cup size. For I think around half a year now I’ve been getting a really weird red area right under my breasts sometimes. It’s slimy and smells weird (weird as in something wrong weird, not as in Normal Body Odor And I Haven’t Showered In A While weird) and is extremely sensitive to touch. Not itchy though. It usually dies down or goes away after I shower, or if it persists, I’ve literally just gone to putting a heaping of baby powder under my breasts before I sleep. I don’t know if it actually helps at all but it at least makes it more bearable to put a bra on since it’s not slimy. It looks a lot like a yeast infection, but I’m not sure since I only get it under my breasts. and don’t have any other symptoms. I just don’t know if it’s a hygiene thing or if it’s something I should actually be worried about?
I’m also on a few medications (including contraceptives) if it sounds like a common side effect to something! I just have no idea ;o;
Hi Anon,
Obligatory "not weird at all!"
A rash under the breasts (or between any skin folds!) is called intertrigo, and is very common, especially with larger breasts and with more body fat. There are a variety of potential causes ("differential diagnoses"), including irritation of the tissues, allergic reaction, psoriasis, and bacterial and yeast infections. The most common culprit is just irritation of the tissues rubbing together.

Whatever the cause, the first step is making sure the area is being cared for properly. This includes:
regular cleaning with mild soap
ensuring the area is dry before putting on a bra (pat dry or cool setting on blow-drying)
use a cotton bra with good support (separates bottom of breast from chest wall, if possible)
try using an antiperspirant containing 20% aluminum chloride (often called "Clinical strength") on the area
If these steps don't work on their own within a couple of weeks, then you are more likely to have a bacterial or yeast infection. A health provider will be able to tell you which and prescribe proper treatment, as these require different things. You could also try a topical (cream) antifungal (Lotrimin or Monistat) on the area for 2 weeks. If that also doesn't work, definitely make an appointment with a provider because it's more likely to be a bacterial infection at that point, which may require antibiotics (either oral or topical), or a topical steroid.
Hope this helps, Anon!
PS I generally advise against baby powder. You can use cornstarch instead, if the antiperspirant is not adequate.
14 notes
·
View notes
Text
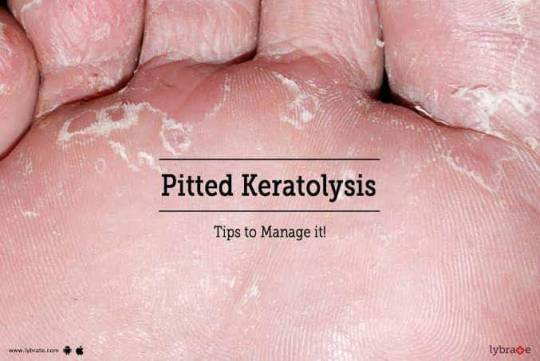
Pitted keratolysis is a bacterial infection of the skin. It can affect the palms of the hands and, more commonly, the soles of the feet, particularly the weight-bearing areas.
This infection causes small depressions, or pits, in the top layer of the skin. It can also lead to a bad smell.
Pitted keratolysis usually affects people who wear enclosed warm footwear for long periods, including soldiers, sailors, and athletes. It also tends to be common in tropical areas where people usually go barefoot.
The bacteria species Kytococcus sedentarius, Dermatophilus congolensis, Corynebacterium, or Actinomyces usually cause the infection.
These bacteria thrive in moist environments. According to the American Osteopathic College of Dermatology, pitted keratolysis has an association with excessive sweating, but this is not its only cause.
Perspiration, along with tight fitting socks or shoes, creates the perfect conditions for the bacteria to multiply.
Other risk factors for pitted keratolysis include:
• not drying the feet thoroughly after bathing
• not wearing absorbent socks
• sharing towels with others
People whose occupation may increase their risk of pitted keratolysis include:
• athletes
• farmers
• sailors and fishing workers
• industrial workers
• people who work in the military
Other risk factors that can make someone more likely to develop pitted keratolysis include:
• hot, humid weather
• sweating a lot on the hands or feet
• having thickened skin on the palms or soles
• having diabetes
• being older
• having a compromised immune system
The main symptom of the infection is clusters of small pits in the top layer of the skin on the soles of the feet. Each pit is usually 1–3 millimeters in size. The skin may also look white or wrinkly.
The pits usually cluster around the balls of the feet, the heels, or both. They tend to appear more pronounced when the feet are wet. Without treatment, the pits can join together to form a large crater-like lesion.
Pitted keratolysis can also cause an unpleasant smell, but people do not usually experience any redness or swelling because this condition is not an inflammatory skin condition.
Less commonly, the infection can affect the hands. When this happens, the characteristic pits usually occur on the palms.
Rarely, the doctor may also recommend oral antibiotics, such as erythromycin or clindamycin. Effective treatment will usually clear the lesions and the smell in 3–4 weeks.
The doctor may also treat excessive sweating if it is contributing to the disorder. Aluminum chloride 20% solution or the off-label use of botulinum toxin injections are options that can decrease sweating.
People need prescription medications to treat pitted keratolysis. However, they can take some preventive measures to help stop the infection from coming back. These include:
• wearing boots for as short a time as possible
• wearing absorbent cotton or wool socks
• washing the feet with soap or antiseptic cleanser twice a day
• applying antiperspirant to the feet
• avoiding wearing the same shoes 2 days in a row
• avoiding sharing footwear or towels with other people
• keeping the feet as dry as possible
People who experience foot odor often try to treat the problem with over-the-counter products. Doing this can make the infection worse because these treatments tend to contain antifungal and antiperspirant ingredients that moisten, rather than dry, the foot.
Pitted keratolysis can affect anyone, but people who wear warm, closed footwear for long periods are particularly at risk.
Prescription antibacterial and antiseptic medicines can treat the infection. With the right treatment, the infection and the smell will usually clear up within a few weeks.
It is important to note that the infection can come back. People can help prevent this by ensuring that they keep their feet dry and by avoiding wearing enclosed footwear whenever possible.
www.thehomeopathyclinic.co.in
#greater noida#best homeo clinic in indirapuram#ghaziabad#homeopathy clinics#homeopathy doctor#homeopathy for ibs#best skin doctor in ghaziabad#homeopathy#homeopathy cold treatment in indirapuram#homeopathy medicine#best homeopathy clinic in indirapuram#best homeopathy doctor#homeopathy skin allergies treatment in indirapuram#homeopathy skin allergies treatment in noida#homeopathy specialist in indirapuram#homeopathy treatment#laser treatment in indirapuram#skin specialist in indirapuram#indirapuram#ghaziabad latest news#ghaziabadnews#ayurvedic doctor in ghaziabad#wave city ghaziabad#child doctor in noida#child specialist in noida#noida news#noida#skin treatment#skincare#skintight
2 notes
·
View notes
Text
A-Z Cheaters Guide to Facial Oils
Image Credit: Kelly Sikkema on Unsplash
I put together this quick guide with some basic information on single-source oils used in skincare. This is not a comprehensive list of all oils used in skincare, just a list of those commonly used as single-source oils. Some oils have more abundant information than others.
As a review, single-source facial oils are used to add moisture and restore skin's natural barrier. To use, you can add a few drops to your favorite moisturizer and mix in your hands prior to application or you can use oils on their own. Simply put a few drops in your palm to warm, then apply a thin layer to skin.
Some of these oils are quite common and can be found in your average grocery store. Others might only be available from specialty retailers, health food stores, and the like. Remember to check and make sure whatever you're buying is organic and has no additives.
CLICK BELOW FOR A-Z FACIAL OILS AND THEIR PROPERTIES.
Acai
Loaded with vitamins and antioxidants
Good for aging skin
Almond
High in Vitamin E, Zinc, proteins, and potassium
Lighter than olive oil and shea butter
Absorbs easily
Can cause allergic reaction
Soothes dry, irritated skin
Good for regenerating damaged skin cells
Good for dry, acne-prone, and sensitive skin
Apricot
High in Vitamin E and fatty acids
Absorbed easily
May help soften and calm irritated, itchy skin; good for acne prone skin
Anti-inflammatory, antioxidant, anti-aging, antiseptic, and antibacterial
Argan
Good for dry, dehydrated skin
High in Vitamin A and E, monounsaturated fatty acids
May help with the appearance of wrinkles, fading scars, skin texture, and treating acne
Doesn't clog pores
Avocado
High in oleic acid, a monounsaturated fatty acid, and other essential and trace minerals
Good for dry, damaged skin
May increase sebum production
Not recommended for acne-prone skin
Can reduce pore size and remove impurities
Reverse signs of aging
Improve conditions like psoriasis and eczema
Carrot Seed
Antifungal, antibacterial, and anticancer qualities due to flavonoid content
Improves elasticity, tone, and overall appearance
Calms irritated skin; may help with eczema and psoriasis
Slows signs of aging
Castor
Strong purging and detoxing properties
May help with acne; increases cell turnover
Can be drying for some skin types due to ricinoleic acid content
Chia Seed
Works well for all skin types including oily and irritated skin; especially beneficial for sensitive, inflamed, dehydrated skin
Rich with omega-3s and -6s and antioxidants
Patients suffering from xerotic eczema who used a simple cream with 4% chia seed oil for eight weeks found significant relief
Decreases transepidermal water loss
Do not use if allergic to chia seeds
Coconut
Available in two forms: solid or liquid
Do not use refined coconut oil on skin
Absorbs easily
High in Vitamin E and K, fatty acids, and polyphenols
Antifungal, anti-inflammatory, and antibacterial properties
Not good for those with acne
Stimulates collagen production
Evening Primrose
Good for aging skin
Promotes elasticity, anti-inflammatory, enhances skin's cellular structure
Helps lighten skin and reduce hyperpigmentation
May help with acne and balancing hormones when taken orally; often used in menopausal women
Grapeseed
High in Vitamin E, fatty acids
Antioxidant, antimicrobial, anti-inflammatory properties
Good for oily skin
Reduces redness
Helps heal acne scarring
Tones and tightens skin
Protects against sun damage
Reduces the appearance of wrinkles, stretch marks, and blemishes
Hemp Seed
Good for oily skin
Great for dry, itchy skin, psoriasis, and eczema
Tolerated by both oily and sensitive skin
Can help balance oil production
Reduces redness and inflammation caused by acne
Jojoba
Good for dry, dehydrated skin
Technically a wax, not an oil
Mimics skin's sebum (natural oils)
May help reduce oil-production in oily skin, basically by tricking it into thinking it's produced enough; can make a good acne treatment
Absorbed easily
Doesn't clog pores
Marula
Good for dry, dehydrated skin
High in antioxidants
Protects from environmental toxins
Reduces signs of aging and sun damage
Soothing for all skin types
Olive
Slightly heavier moisturizer
Typically doesn't trigger allergic reactions
Can cause/worsen atopic dermatitis for some
High in Vitamins A (natural retinoid), D, E, and K; fatty acids and plant sterols
Antioxidant-rich
Smooths skin texture
Reduces signs of aging, inflammation, and redness
Heals dry skin
Pumpkin Seed
Good for oily skin
Has DHT-blocking properties
Rich in zinc and selenium
Great for fighting acne-causing bacteria
Low chance of clogging pores
Increases firmness
Rosehip
High in Vitamin A (natural retinoid) and C, fatty acids, and other antioxidants
Recommended for sensitive skin, anti-aging
Possible use for eczema
Good for oily, dry, damaged, mature, and irritated skin
May help reverse the effects of sun damage
Improves skin texture
Helps with signs of aging, stretch marks, scars, and hyperpigmentation
Safflower
High in linoleic acid
Great at treating blackheads and other skin impurities
Sesame Seed
Promotes wound healing
Kills acne-causing bacteria
Has great antibacterial properties
Protects against sun damage
Helps skin texture and overall appearance
Allergen risk
Shea Oil/Butter
Available in two forms: solid or liquid
Excellent moisturizer; highly protective against rough skin during dry, cold months
Reduces inflammation; soothes distressed skin
Sunflower Seed
Absorbed easily
High in Vitamin E
Protects skin barrier
Antimicrobial properties
Doesn't cause/worsen atopic dermatitis
Good for irritated skin
Good for most skin types
Balances, moisturizes, and fights signs of aging
Squalane
Lightweight
Derived from sugarcane
Good for sensitive skin
Absorbs easily
Tamanu
Comes from a tree in the pine/evergreen family; strong, pine-like scent
Amazing healing properties
Great for acne spot treatment, healing and fading acne scars
Can be used to fade other types of scarring as well
Good for delicate skin
2 notes
·
View notes
Text
Clinically Validated Liposomes: Revolutionizing Drug Delivery and Nutrition
What Are Clinically Validated Liposomes?
Liposomes are microscopic, spherical vesicles made of lipid bilayers that can encapsulate active compounds such as vitamins, drugs, and supplements. Clinically Validated Liposomes refer to liposomal formulations that have undergone rigorous scientific testing to ensure their safety, stability, and bioavailability. These advanced delivery systems are widely used in pharmaceuticals, skincare, and nutraceuticals to enhance the effectiveness of active ingredients.

How Does Liposomal Encapsulation Technology Work?
Liposomal Encapsulation Technology (LET) involves enclosing active ingredients within lipid-based carriers to protect them from degradation and improve their absorption in the body. The process works by:
Encapsulation: Active compounds are surrounded by lipid bilayers, mimicking cell membranes.
Protection: The liposomal shell shields sensitive ingredients from stomach acids and enzymes.
Enhanced Absorption: The lipid structure allows for better absorption in the intestines and direct delivery to cells.
Sustained Release: Some liposomal formulations offer controlled, prolonged release of nutrients or drugs, improving efficacy.
Why Are Clinically Validated Liposomes Superior to Traditional Delivery Methods?
Traditional oral supplements and medications often suffer from low bioavailability due to breakdown in the digestive system. Clinically Validated Liposomes solve this problem by:
Increasing absorption rates up to 10 times compared to conventional forms.
Bypassing first-pass metabolism in the liver, allowing more of the active ingredient to enter the bloodstream.
Reducing gastrointestinal discomfort associated with some supplements.
Enhancing the stability and potency of sensitive compounds like vitamin C, glutathione, and curcumin.
What Are the Key Applications of Liposomal Technology?
Clinically Validated Liposomes are transforming multiple industries, including:
1. Pharmaceuticals
Liposomal drug formulations improve targeted drug delivery and reduce side effects.
Used in chemotherapy, vaccines, and antifungal treatments.
2. Nutraceuticals & Dietary Supplements
Liposomal vitamins (e.g., C, D, B12) enhance nutrient absorption.
Effective in delivering antioxidants like glutathione and resveratrol.
3. Skincare & Cosmetics
Helps active ingredients penetrate deeper layers of the skin.
Common in anti-aging serums and moisturizers.
4. Gene Therapy & Biotechnology
Used in RNA and DNA delivery, playing a crucial role in personalized medicine and vaccine development.
Are Liposomal Supplements Safe?
Yes, when formulated correctly, Clinically Validated Liposomes are safe and well-tolerated. Studies confirm that high-quality liposomal products:
Use phospholipids derived from natural sources (e.g., sunflower lecithin).
Are free from harmful additives like synthetic emulsifiers and preservatives.
Undergo rigorous testing to confirm purity, stability, and efficacy.
However, not all liposomal products are created equal. It’s essential to choose brands that prioritize clinical validation and transparency in ingredient sourcing.
What to Look for in a Clinically Validated Liposomal Product?
When selecting a liposomal supplement or drug, consider the following factors:
Clinical Studies: Has the product been tested in human trials?
Ingredient Quality: Are non-GMO, organic, and natural phospholipids used?
Particle Size: Nano-sized liposomes (<200 nm) enhance absorption.
Manufacturing Standards: Does the company follow Good Manufacturing Practices (GMP)?
Third-Party Testing: Are purity and potency verified by independent labs?
How Are Companies Like Lipsobio Advancing Liposomal Technology?
Leading companies like Lipsobio are pushing the boundaries of liposomal technology through:
Research-Backed Formulations: Ensuring that each product is scientifically validated for maximum efficacy.
Advanced Encapsulation Methods: Using cutting-edge techniques to enhance stability and bioavailability.
Commitment to Purity: Utilizing clean, high-quality ingredients without unnecessary fillers or synthetic chemicals.
By focusing on innovation and quality, Lipsobio is setting new standards in the industry, making liposomal supplementation more effective and accessible.
Conclusion: Are Clinically Validated Liposomes the Future of Nutrient and Drug Delivery?
The science behind Clinically Validated Liposomes and Liposomal Encapsulation Technology is transforming the way we absorb and utilize essential nutrients and medications. With superior bioavailability, targeted delivery, and enhanced efficacy, liposomes are paving the way for a new era in pharmaceuticals and nutrition.
If you’re looking for high-quality, research-driven liposomal products, consider brands like Lipsobio that are dedicated to delivering cutting-edge solutions backed by science.
0 notes
Link
0 notes
Text
0 notes
Text

Global Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) Market Report 2032
According to the Markets and Data Research report, “Global Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) Market Assessment, Opportunities and Forecast, 2017-2031F”, the market for chronic rhinosinusitis with nasal polyps (CRSwNP) is expected to grow at a CAGR of 6.95% from 2024 to 2031. The market size shall increase from USD 3,540.00 million in 2023 to USD 6,246.16 million by 2031. The global market for CRSwNP is expected to grow due to the increasing demand for CRSwNP therapeutics. This demand will continue to rise as the prevalence of chronic rhinosinusitis is significantly increasing. The market growth can also be largely attributed to the advent of targeted therapies that involve biological treatments against selected pathways of inflammation, which have subsequently gained regulatory approval. Raising awareness and ensuring the availability of new drugs in pipelines are other factors that would further boost the market.
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a recurring inflammatory chronic disease involving the sinuses, which causes obstructive nasal symptoms. The CRSwNP market is growing steadily, and it is mainly boosted by the increasing prevalence of demographic as well as environmental factors, such as aging, air pollution, and smoking. The growth of this market has been propelled by the successful approval of biologic drugs that target specific inflammatory pathways. The market expansion remains underpinned by new drugs, high awareness of the disease, and the entry of other advanced therapy modalities. The last few quarters have seen the introduction of several notable medicines near launch, including XHANCE and GSK’s Depemokimab, which emphasized the new ways of treating the disease.
Click: https://www.marketsandata.com/industry-reports/chronic-rhinosinusitis-with-nasal-polyps-market
The “Global Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) Market” report is 287 pages long and includes an in-depth TOC, over 155 market data figures, latest market developments, key drivers and opportunities, and a thorough study of major company profiles. Moreover, the report offers strategic recommendations, pricing analysis, market share analysis, and value chain analysis in detail.
Key Takeaways:
The demand for CRSwNP therapeutics increases with rising prevalence fueled by an aging population, air pollution, and high smoking rates. Chronic rhinosinusitis puts more pressure on effective treatments for the disorder.
Increasing regulatory approvals for CRSwNP biologics are driving growth by providing new, effective treatment options.
Some new promising product offerings in the pipeline will be able to fill the clinical gap, like GSK’s depemokimab and Upstream Bio’s verekitug. All these developments unveil promising activities that will help develop better therapy for CRSwNP.
The market is experiencing increased sales through hospital pharmacies apart from traditional retail pharmacies. However, online pharmacies are rapidly growing as they offer enhanced accessibility and convenience to consumers.
Global chronic rhinosinusitis with nasal polyps (CRSwNP) market is segmented in the following categories:
By Treatment Type: Biologics, Corticosteroids, Antibiotics, Antifungal Drugs, Others
By Route of Administration:Parenteral, Oral, Nasal
By Distribution Channel: Hospital Pharmacies, Retail Pharmacies, Online Pharmacies
By Region: North America, Europe, South America, Asia-Pacific, Middle East and Africa
Based on treatment, the use of biologics is increased in the treatment of chronic rhinosinusitis with nasal polyps (CRSwNP) due to their specific mechanism of action targeted at type 2 inflammation, which is an important element in the pathology of the condition. The approved biologics include dupilumab, omalizumab, and mepolizumab, all of which have been shown to potently block specific cytokines such as IL-4, IL-5, and IL-13, which are all major mediators of the inflammatory pathway associated with CRSwNP. Clinical trial evidence has shown considerable improvements in polyp sizes, reduction of symptoms, and overall quality of life for patients who respond poorly to conventional treatment options. This shift toward biologics illustrates a greater trend toward personalized medicine that aims to address complex inflammatory disorders.
Based on the route of administration, the parenteral route is most preferred as it is an effective drug delivery system that can deliver medications to the site of action with rapid action and high bioavailability. Two biologics, dupilumab and mepolizumab, work specifically on pathways involved in the inflammatory pathways of CRSwNP and require the precise dosing provided by parenteral administration. This approach avoids GI absorption issues; hence, the drug will quickly and effectively reach systemic circulation, which is necessary for treating acute symptoms and inflammation in patients. Furthermore, many patients with CRSwNP would tolerate gastrointestinal adverse effects; therefore, oral delivery is less appropriate in many circumstances.
Based on distribution channels, hospital pharmacies have dominated the market because of their capability to offer specialized medicines and therapies, often by medical professionals. The services the pharmacies present are far better than those of the retail dispensaries due to their competency in dealing with complex cases, which ensures that patients are provided with tailored treatments and have access to treatments such as biologics and corticosteroids that may not be available at the standard retail outlets. Meanwhile, there is rapid growth in online pharmacies due to the increasing demand among consumers for convenience and ease at one end. It has enabled patients to order from home, which helps them stick to their regimens, avoid long trips, and wait in line.
North America, particularly the United States, plays a crucial role in the global chronic rhinosinusitis with nasal polyps market due to its advanced healthcare infrastructure and regulatory frameworks. The United States Food and Drug Administration significantly influences this market by approving innovative treatments, such as Dupixent and Nucala, which target specific inflammatory pathways associated with CRSwNP. These approvals enhance treatment options and set regulatory precedents that can affect global drug development strategies. The FDA’s rigorous evaluation ensures that new therapies meet high safety and efficacy standards, fostering trust and adoption in other markets. The Asia-Pacific region is expected to grow fastest due to the high population and adoption of biologics.
Download Free Sample Report
Major Companies Operating in Global Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) Market Include:
Sanofi-Aventis US LLC
GlaxoSmithKline plc
Genentech, Inc.
Novartis Pharmaceuticals Corporation
Regeneron Pharmaceuticals Inc.
AstraZeneca plc
Intersect ENT Inc.
Keymed Biosciences Inc.
Optinose US Inc.
Chongqing Genrix Biopharmaceutical Co., Ltd.
Major companies in the global chronic rhinosinusitis with nasal polyps (CRSwNP) market are strategically involved in mergers and acquisitions to strengthen their research and development (R&D) to enhance their product portfolio, expand capacity, and launch new products.
In February 2024, GSK plc acquired Aiolos Bio, Inc. This biopharmaceutical company specializes in innovative treatments for respiratory and inflammatory conditions. By doing this, GSK enhances its portfolio in respiratory biologics to address unmet medical needs in patients afflicted with these debilitating diseases. GSK reinforces its capabilities in accelerating research and development (R&D) to improve patient care and access to advanced therapies significantly.
“Global Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) Market Assessment, 2017-2031F”, evaluates the future growth potential of global chronic rhinosinusitis with nasal polyps (CRSwNP) market and provides statistics and information on market size, structure, and future market growth. The report intends to provide innovative market intelligence and help decision-makers make strategic investment decisions for their organizations. Moreover, the report identifies and examines the emerging trends along with key drivers, challenges, and opportunities in the global chronic rhinosinusitis with nasal polyps (CRSwNP) market.
Contact
Mr. Vivek Gupta
5741 Cleveland street,
Suite 120, VA beach, VA, USA 23462
Tel: +1 (757) 343-3258
Email: [email protected]
Website: https://www.marketsandata.com
0 notes
Link
#market research future#antifungal treatment market#antifungal treatment industry#antifungal treatment analysis#antifungal treatment size
0 notes
Link
#market research future#antifungal treatment market#antifungal treatment industry#antifungal treatment analysis#antifungal treatment size
0 notes
Text
Propolis Extract Market Size, Trends, and Growth Forecast to 2025
The Propolis Extract Market is experiencing steady growth, driven by increasing consumer awareness of its health benefits and expanding applications across various industries.
Get free sample copy @ https://www.statsandresearch.com/request-sample/31614-propolis-extract-market
Market Overview:
Market Size and Growth: In 2023, the global propolis extract market was valued at approximately USD 700 million and is projected to reach USD 905.3 million by 2030, growing at a compound annual growth rate (CAGR) of 5.8% during the forecasted period from 2024 to 2030.
Key Market Drivers:
Health Benefits: Propolis extract is renowned for its antibacterial, antifungal, antiviral, antioxidant, and anti-inflammatory properties, making it a sought-after ingredient in the pharmaceutical and cosmetic industries.
Cosmetic Industry Demand: The skincare sector is increasingly incorporating propolis extract into products like moisturizers, serums, and tonics due to its healing and protective properties.
Pharmaceutical Applications: Propolis extract is utilized in various medicinal formulations, including throat lozenges and topical treatments, owing to its therapeutic benefits.
Market Segmentation:
By Product Type:
Liquids
Creams
Other Product Types
By Distribution Channel:
Retail Stores
Online Retailers
Get full report @ https://www.statsandresearch.com/report/31614-propolis-extract-market/
Regional Insights:
North America: The region holds a significant share of the market, driven by a strong demand for natural health products and a well-established cosmetic industry.
Europe: Europe is a key market for propolis extract, with increasing consumer preference for natural and organic skincare products.
Asia-Pacific: The Asia-Pacific region is witnessing rapid growth in the propolis extract market, fueled by rising health consciousness and expanding cosmetic industries.
Key Players:
Comvita Limited
Bee Health Limited
Apis Flora
Propolia
Herbal Hills
Challenges:
Quality Control: Ensuring the purity and potency of propolis extract can be challenging due to variations in raw material quality.
Regulatory Compliance: Navigating the complex regulatory landscape for natural health products requires adherence to stringent standards.
Get enquiry before buying @ https://www.statsandresearch.com/enquire-before/31614-propolis-extract-market
0 notes
Text
0 notes
Text
A Deep Dive into the Antifungal Drugs Market: Insights and Analysis
The global antifungal drugs market size is expected to reach USD 20.52 billion by 2030, according to a new report by Grand View Research, Inc. The market is expected to expand at a CAGR of 3.8% from 2024 to 2030. The increasing incidence of fungal infections worldwide is the key factor stoking the growth of the market. In addition, the rise in the adoption of immunosuppressive and antineoplastic agents, prosthetic devices and grafts, and broad-spectrum antibiotics has resulted in an increased incidence of fungal infections in recent years.
According to statistics published by the Centers for Disease Control and Prevention in 2017, it has been estimated that every year, nearly 220,000 new individuals are affected by cryptococcal meningitis, which is a brain infection and has resulted in 181,000 deaths per year around the world. Most of the deaths were reported in sub-Saharan Africa, due to the high prevalence of HIV/AIDS. This indicates the potential demand for antifungal drugs due to the high prevalence of mycological infections around the globe.
The government authorities in many countries had ordered nationwide lockdowns in order to contain the spread of COVID-19. Similarly, health systems in a number of countries around the world were having trouble maintaining their supply chains. The slowness of the supply chain has also impacted the demand for antifungal medications. As aged people are more prone to infectious diseases and chronic conditions, including HIV and cancer, the rise in the geriatric population worldwide is likely to stir up the demand for antifungals to treat opportunistic fungal infections. The demand for fungistatic agents is estimated to remain strong through 2030 due to mounting cases of fungal infections that are difficult to diagnose, yielding high mortality and morbidity rates.
Gather more insights about the market drivers, restrains and growth of the Antifungal Drugs Market
Antifungal Drugs Market Report Highlights
• The Azoles drug class segment dominated the market and accounted for a revenue share of 47.6% in 2023. This dominance is attributed to the influence of key therapeutic agents, including noxafil, vfend, diflucan, and cresemba.
• The Candidiasis segment held the largest market share in 2023 due to rising incidence of the disease in immunocompromised patients and high rate of recurrent infections.
• Aspergillosis is expected to register significant CAGR during the forecast period. Aspergillosis is an infection caused by mold called aspergillosis, which usually affects the respiratory system.
• Oral drugs dosage form led the market in 2023. This is attributed to the fact that certain antifungal medications are designed for oral administration to ensure proper ingestion.
• Hospital pharmacies led the market in 2023. Hospital pharmacies play a key role in ensuring immediate access to crucial medications. They serve both out-patient and in-patient services, facilitating the seamless treatment of fungal infections.
• North America dominated the market and accounted for 40.9% share in 2023. This region dominance is attributed to the highly developed healthcare infrastructure, better affordability, and increasing awareness.
• Asia Pacific is anticipated to witness significant growth during the forecast period. This is owing to the presence of large target population, developing healthcare facilities, and increase in investments by leading market players.
Antifungal Drugs Market Segmentation
Grand View Research has segmented the global antifungal drugs market report based on drug class, indication, dosage form, distribution channel, and region:
Antifungal Drug Class Outlook (Revenue, USD Million, 2018 - 2030)
• Azoles
• Echinocandins
• Polyenes
• Allylamines
• Others
Antifungal Drugs Indication Outlook (Revenue, USD Million, 2018 - 2030)
• Dermatophytosis
• Aspergillosis
• Candidiasis
• Others
Antifungal Drugs Dosage Form Outlook (Revenue, USD Million, 2018 - 2030)
• Oral Drugs
• Ointments
• Powders
• Others
Antifungal Drugs Distribution Channel Outlook (Revenue, USD Million, 2018 - 2030)
• Hospital Pharmacies
• Retails Pharmacies
• Others
Antifungal Drugs Regional Outlook (Revenue, USD Million, 2018 - 2030)
• North America
o U.S.
o Canada
• Europe
o Germany
o UK
o France
o Italy
o Spain
o Denmark
o Norway
o Sweden
• Asia Pacific
o China
o Japan
o India
o South Korea
o Australia
• Latin America
o Brazil
o Mexico
o Argentina
• Middle East and Africa (MEA)
o Saudi Arabia
o UAE
o South Africa
o Kuwait
Order a free sample PDF of the Antifungal Drugs Market Intelligence Study, published by Grand View Research.
#Antifungal Drugs Market#Antifungal Drugs Market Size#Antifungal Drugs Market Share#Antifungal Drugs Market Analysis#Antifungal Drugs Market Growth
0 notes