#amenorrhea and pcos
Explore tagged Tumblr posts
Text
Can I Get Pregnant If I Have PCOS?
Polycystic ovary syndrome (PCOS) is a relatively common disorder that affects about 10 percent of women during their childbearing years. This condition can cause many unique symptoms and issues. One of the most worrying is low fertility. PCOS is one of the most widespread causes of infertility in women.
But contrary to popular belief, pregnancy with PCOS is possible.
What is PCOS?
PCOS is a condition that causes an imbalance of reproductive hormones. That imbalance causes issues within the ovaries. Women can develop fluid-filled sacs in the ovaries, and hormonal changes can affect how the ovaries produce eggs. With PCOS, eggs might not develop. If they do, they may not be released during ovulation.
Experts don't know the exact cause of PCOS. However, several factors may play a role in the condition's development. One common theory is high levels of androgens, male sex hormones. Another potential cause is high insulin levels.
There are many PCOS symptoms. Many women find out they have PCOS when they're trying to get pregnant and encounter fertility issues. However, symptoms can point to this condition much earlier. The most common symptoms include irregular menstrual cycles. In many cases, periods will stop for several months or years.
Many women also experience weight gain, excessive hair growth throughout the body, acne and thinning hair.
Pregnancy with PCOS
PCOS makes it difficult to get pregnant because it interferes with ovulation. The condition impacts how eggs develop and move from the ovaries. In some cases, it stops eggs from growing properly due to the hormonal imbalances. Then, PCOS can prevent ovulation. When the eggs don't release, it's impossible to get pregnant.
There's still a chance, but infertility is common in women with PCOS. For those who do get pregnant, many risks exist. Women with PCOS have a higher risk of miscarriage and stillbirth. Babies born to women with PCOS also often need newborn intensive care.
Fortunately, there are options available if you have PCOS and want to get pregnant. This condition is manageable, and many fertility treatments can substantially increase your chances of conceiving.
Read a similar article about polycystic ovary syndrome specialists here at this page.
0 notes
Text
Mantra of the week...
I allow my body to fully heal. I am finding complete balance within myself. I am on the right path and everything is working out.
4 notes
·
View notes
Text
I get such bad night sweats every single time i take any form of progesterone, and I hate it so much. My body is supposed to make this shit naturally why does it fuck me up so much every time I use it?
#if you can't afford natural hormones store bought are fine#except its not it makes it hard for my to sleep!#also the depo shot made me fucking lose my shit and apparently can give you brain cancer so#but at the time they refused to give me combo pills that I'd been taking for 4 years at that point because of my weight which hadn't changed#god forbid i have a body that works right#pcos#amenorrhea#obviously I'm gonna keep taking it because what other choice do i have if my body won't work properly#and yes i take supplemental and metformin to control other symptoms but that doesn't make your period come back instantly
1 note
·
View note
Text
Understanding Amenorrhea: Causes, Symptoms, and Treatment Options
Amenorrhea refers to the absence of menstruation, and it can be a sign of an underlying health issue. While missing a period occasionally may not be a cause for concern, consistently not having a period for several months can indicate a more significant problem. Understanding the causes, symptoms, and treatment options for amenorrhea is important for maintaining overall health.
What is Amenorrhea?
Amenorrhea is the medical term for the absence of menstruation. There are two types:
Primary Amenorrhea: When a young woman has not started her periods by the age of 16.
Secondary Amenorrhea: When a woman who has had regular periods stops menstruating for three months or more.
Menstruation is essential to women’s health, as it indicates a normal functioning reproductive system. The absence of periods may disrupt hormonal balance and fertility.
Causes of Amenorrhea
Several factors can contribute to amenorrhea:
Hormonal Imbalances: Issues with hormones like estrogen and progesterone can stop periods. Conditions like polycystic ovary syndrome (PCOS) or problems with the pituitary gland may lead to this imbalance. Similarly, the causes of oligomenorrhea and how they affect your health can be linked to these hormonal changes, where women experience infrequent periods instead of the complete absence.
Thyroid Disorders: Both hypothyroidism (low thyroid hormone levels) and hyperthyroidism (high thyroid hormone levels) can interfere with the menstrual cycle.
Pregnancy: The most common cause of secondary amenorrhea is pregnancy. If you’ve missed a period and suspect pregnancy, a test or a visit to your healthcare provider will confirm this.
Stress and Lifestyle Factors: Excessive stress, extreme weight loss, or excessive exercise can all disrupt your menstrual cycle. These factors affect hormone production and can prevent ovulation.
Other Medical Conditions: Conditions like diabetes, obesity, and eating disorders can also cause amenorrhea.
Symptoms of Amenorrhea
The primary symptom of amenorrhea is the absence of periods for three months or longer. Additional symptoms may include:
Weight changes (gain or loss)
Excessive hair growth (hirsutism)
Acne or oily skin
Headaches or vision changes
Breast discharge or pain
If you experience any of these symptoms along with missed periods, it’s important to consult a doctor.
Diagnosing Amenorrhea
To diagnose amenorrhea, a healthcare provider will first take a medical history and conduct a physical exam. Tests such as blood work, ultrasounds, or MRIs may be done to check hormone levels or identify any reproductive system abnormalities.
Treatment Options for Amenorrhea
Treatment will depend on the underlying cause of amenorrhea:
Lifestyle Changes: Improving nutrition, reducing stress, and maintaining a healthy weight can often restore menstrual cycles.
Medications: Hormonal treatments such as birth control pills or hormone therapy may help regulate periods.
Surgical Options: If structural issues like ovarian cysts or uterine problems are found, surgery may be needed.
Fertility Treatments: If amenorrhea is affecting fertility, treatments like ovulation induction may be considered.
Preventing Amenorrhea
Maintaining a balanced diet, exercising regularly but not excessively, and managing stress are important steps in preventing amenorrhea. Staying healthy helps regulate hormone production and supports the menstrual cycle.
When to Seek Medical Help
If you’ve missed several periods or are experiencing unusual symptoms like excessive hair growth or weight changes, it’s time to seek medical advice. Early diagnosis and treatment are crucial to prevent long-term health issues.
Conclusion
Amenorrhea can be a sign of various health problems, but with early intervention, many women can restore their menstrual cycles and maintain good health. If you notice symptoms of amenorrhea, don’t hesitate to consult a healthcare professional to find the right treatment for you.
Tags: #Amenorrhea #MenstrualHealth #HormonalImbalances #PCOS #ThyroidDisorders #HealthyLifestyle #FemaleHealth #ReproductiveHealth #MissedPeriods #Oligomenorrhea
0 notes
Link
#Amenorrhea#Dysmenorrhea#PCOS#PelvicDiseases#PelvicPain#PelvicScan#PelvicUltrasound#TransvaginalScan
0 notes
Link
0 notes
Text
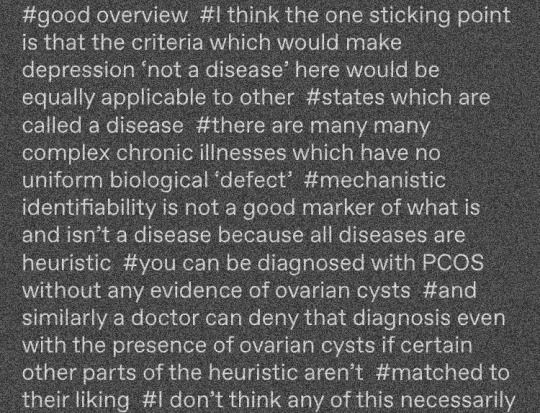
these tags annoyed me to be honest
1. PCOS is a bad point of comparison because despite the name, diagnosis is not *supposed to be* done on the primary basis of finding cysts in the ovaries; these are common and not inherently of concern. instead, the more indicative biomarker is the hormone test (high levels of testosterone *throughout the menstrual period*, with corresponding disruption to the expected/typical fluctuations in estrogen/progesterone) but often diagnosis is done more on the basis of a physical exam ('exam') confirming characteristics such as hairiness or adiposity. this absolutely DOES result in PCOS overdiagnosis for some demographics; while a real biological condition, PCOS is also a load-bearing diagnostic term in the enforcement of very specific standards of (white) femininity and its use also frequently masks, for example, the frequency of hypothalamic amenorrhea (HA) secondary to chronic energy deficiency (as in anorexia), which doctors are loathe to diagnose because they view weight loss as prima facie good
2. the reason it matters that psychiatric diagnoses do not have a 'biology' is not because every disease must have a single specific biomarker; it is correct that some do not. however, the way patient complaints are sifted into categories labelled 'psychiatric' versus '(otherwise) medical' begins essentially with determining whether the distress is 'physical' or 'mental'. in other words, in the case of, say, the chronic fatigue syndrome (famously, lacking a known specific biomarker), the symptoms being investigated by the non-psychiatrist physician are still physical (PEM; mast cell dysregulation; pain; etc) whereas a diagnosis of depression may be accompanied by, but requires no, physical symptoms or presentation. the psychiatric claim that its diagnoses have biological causes and correlates is specifically a claim about the role of neurobiology in the causation of affective states; thus, the comparison to physical complaints is meaningless here
3. this person goes on to claim that depressives do in fact share, though not universally, certain biomarkers such as mitochondrial dysregulations. such claims typically come from various imaging studies plagued with systemic problems in the selection and definition of patient populations as well as the subjectivity of result interpretation and analysis. these claims are not well supported and typically rely on circular selection and definition of patient populations
4. speaking philosophically, it is in fact often correct to challenge the notion that a physical 'disease' chronically lacking a specific biomarker is indeed a disease, in any sense besides the colloquial one. that is, diseases that cannot be correlated with one cause or presentation are often better understood as 'syndromes', which is to say, as a taxonomical heuristic that is likely grouping together multiple disparate physical (anatomical, physiological, functional, &c) problems with multiple disparate causes. this is almost certainly the case for chronic fatigue syndrome, for example. this is a philosophical distinction that matters for research and understanding, and does not mean or imply anything to minimise or contradict the patient experience of the syndrome or symptoms. it matters because, for instance, CFS triggered by the epstein-barr virus may indeed turn out to have different disease mechanisms to CFS triggered by, say, covid-19, or may have different specific mechanisms when running in certain families, and so on. distinguishing these much more specific presentations, and possibly distinct diseases, from the current discursive schema of the overlying syndrome is potentially very good for patients, who likely have different needs and treatments to one another despite currently all sharing the same label in their charts
5. which goes back to an overlying point, which is that (despite frequent defensiveness to the contrary), whether or not something is a disease does not inherently tell us anything about its reality, its severity, its cause, the moral status of its sufferers, &c
67 notes
·
View notes
Text
I have almost all the symptoms except hair loss on my head. The weight gain around isn't too bad, but it was bad enough for ME to notice.
I started my period at 14, which is really late for the woman in my family as we tend to start as young as 11. For months before I turned 14, I had massive headaches that would sometimes leave me unable to stand without blinding pain.
This continued until I was about 17 years old, when I finally started falling over because of really bad stomach aches that had started hitting me in the gut over the past couple of months. My mom had me checked out, and the nurse almost flipped when she saw how low my blood pressure was. After seeing a doctor, I was diagnosed with PCOS and started treatment.
But something wasn't adding up. While all this was happening, my mom and one of my sisters were seeing a doctor that specialized in woman's health to help lose weight. (Their issues were unrelated to PCOS) I heard about all the good things this woman was doing for my family, so I asked to see her. After she checked me over, she determined that I had Amenorrhea, a condition very similar to PCOS, but curable, I just had all the same symptoms.
I'm still struggling with it even years later, but I'm almost better. I know that Amenorrhea is different to PCOS, but I still wanted to share my story.
This has been on my mind for a while so I have a question:
If you’ve never heard of it, Polycystic Ovarian Syndrome is pretty much just what it sounds like. It is when a woman develops cysts on her ovaries, or has the potential to. These cysts often throw hormonal balance out of whack throughout the entire body. Pregnancy-like symptoms can occur, as well as heightened testosterone levels.
Common symptoms of PCOS are:
Excessive body or facial hair
Insulin resistance that causes rapid weight gain and weight that can’t be shed even with proper diet and exercise
Excessive weight around the gut, a beer belly or inner tube
Hair loss on head
Irregular or entirely missing periods
Intense sugar cravings
Depression
And of course, painful ovarian cysts
There is no cure for PCOS yet, but there are treatments. If you suspect PCOS, get your hormones checked. Talk to a doctor. Estrogen-progesterone birth control may help, as well as Metformin (an insulin resistance drug for diabetics)
It is not considered genetic, but I disagree.
I am not a doctor, but I have PCOS and I’ve been doing a lot of research to help clear up my issues. I hadn’t been able to lose weight even with a healthy diet and regular 20 minute bike rides. It’s frustrating and debilitating. I thought that I was just stuck, but talking to my doctor gave me hope.
I know several other girls with PCOS (every woman on my dad’s side of the family) with all different struggles.
What’s your story?
35 notes
·
View notes
Text
so i've been thinking about my genderfluid/bigender identity and my upcoming appointment for gender affirming care, and something occurred to me that i felt like is worth sharing
i have PCOS. my body produces naturally high levels of testosterone. i never knew i was intersex until i was 23, but it made a lot of stuff make sense from my adolescence. the irregular periods, the deep voice, the way my body developed during puberty. when i was 18 i went on hormonal birth control, so i never had to confront this reality as an adult until i went off it.
it was amazing at first. i didn't tell anyone until i had to, because i liked what it was doing to my body. but, after 6 months of amenorrhea i started getting really bad daily ovarian cramps. at this point, i knew before they told me that i had PCOS. i had to do something, i just didn't know what.
i went back on hormonal birth control after getting my PCOS diagnosis. i never wanted to, but the gynecologist framed it as the only option for treatment. the only way to lessen those pesky "androgenizing effects" and the cramps i was getting. i was trying yet another new type, an extended cycle estrogen based pill, in a desperate attempt to lessen the pain of almost every stage of my menstrual cycle, but hormonal birth control was always a necessary evil for me.
every day since then i have gotten more and more tired and unsettled in my own body. i've always been a man, but i have never felt so uncomfortable as a woman as i have been since realizing what my body is capable of, and yet still making the choice to "feminize" myself with hormones.
then, it hit me. getting my testosterone levels sorted out to a level that makes me comfortable and not dysphoric isn't just about my identity as a trans man. it's about my identity as an intersex woman.
i want to be a woman with natural testosterone. the kind that my body produces. and that's okay!
it's complicated. all identity is. but putting a name to this feeling has really helped me, and if you're intersex/nonbinary and struggling with your feelings about hormones, i hope it helps you too
131 notes
·
View notes
Text
Understanding Menstrual Disorders: Causes, Symptoms, and Solutions

Menstrual disorders are a group of conditions that interfere with the normal menstrual cycle, affecting millions of women worldwide, including in the Democratic Republic of Congo. These disorders can significantly impact daily life and overall well-being, yet many women suffer in silence due to stigma or lack of access to adequate healthcare.
If you are experiencing irregularities in your menstrual cycle or unusual symptoms, know that help is available. Let’s dive into the causes, symptoms, and solutions for menstrual disorders, and how online consultations through platforms like CongoRx can provide timely and effective support.
What Are Menstrual Disorders?
Menstrual disorders refer to a range of issues that deviate from a regular menstrual cycle. Common conditions include:
Dysmenorrhea: Painful periods with cramping.
Amenorrhea: Absence of menstruation for three months or longer.
Menorrhagia: Heavy or prolonged menstrual bleeding.
Premenstrual Syndrome (PMS): Physical and emotional symptoms occurring before menstruation.
Polycystic Ovary Syndrome (PCOS): A hormonal disorder affecting ovulation and menstrual cycles.
Irregular Periods: Unpredictable cycle lengths.
These disorders often stem from underlying health issues, hormonal imbalances, or external factors like stress and lifestyle.
Causes of Menstrual Disorders
Several factors contribute to menstrual disorders, such as:
Hormonal Imbalances: Fluctuations in estrogen and progesterone levels can disrupt the cycle.
Medical Conditions: PCOS, thyroid disorders, and uterine fibroids.
Stress and Lifestyle: High stress levels, poor diet, and lack of exercise.
Infections: Untreated pelvic infections are a leading cause in regions like Congo, where access to timely healthcare is sometimes limited.
Addressing these causes often requires a multidisciplinary approach, including lifestyle changes and medical interventions.

Symptoms to Watch For
While menstrual symptoms vary widely, it’s essential to recognize warning signs that may require medical attention:
Excessively heavy bleeding or passing large clots.
Severe pelvic pain or cramping.
Irregular cycles lasting less than 21 days or more than 35 days.
Spotting or bleeding between periods.
Chronic fatigue, dizziness, or anemia.
If you or someone you know in Congo is experiencing these symptoms, seeking professional guidance is crucial.
Managing Menstrual Disorders
Lifestyle Adjustments:
Maintain a balanced diet rich in iron and vitamins.
Engage in regular physical activity to regulate hormones.
Practice stress management techniques, like yoga or meditation.
Medical Treatments:
Hormonal therapies such as birth control pills or IUDs.
Medications for pain relief and symptom control.
Surgical interventions for conditions like fibroids or endometriosis.
Online Consultation Services: Access to healthcare is a challenge in many parts of Congo. Platforms like CongoRx offer online consultations with gynecologists and specialists, ensuring timely diagnosis and treatment from the comfort of your home.
Why Addressing Menstrual Disorders Matters
In countries like Congo, cultural stigmas around menstruation often deter women from seeking help. Education and accessible healthcare can transform this narrative. With services like CongoRx, women can connect with trusted doctors for compassionate and confidential care, ensuring they don't face these challenges alone.
Take the First Step with CongoRx
Living with menstrual disorders can be challenging, but you don’t have to face it alone. Whether you’re dealing with painful cramps, irregular cycles, or suspect an underlying condition, timely consultation with a healthcare professional can make a difference.
Visit CongoRx today to book an online consultation and start your journey toward better health. Empower yourself to take charge of your menstrual health—because every woman deserves care and understanding.
2 notes
·
View notes
Text

BMI: body mass index; E2: estradiol; FSH: follicle-stimulating hormone; hCG: human chorionic gonadotropin; MRI: magnetic resonance imaging; PCOS: polycystic ovary syndrome; PRL: prolactin; T: testosterone; TSH: thyroid-stimulating hormone.
* Many clinicians also measure serum 17-hydroxyprogesterone at the initial visit to rule out nonclassic 21-hydroxylase deficiency. Some also measure serum dehydroepiandrosterone sulfate (DHEAS).
¶ Mild hyperprolactinemia can sometimes be seen with hypothyroidism. Euthyroidism should be confirmed before performing MRI.Δ Pituitary MRI not required in those with clear explanation for their hypogonadotropic amenorrhea, eg, eating disorder, excessive exercise, celiac disease, or type 1 diabetes mellitus.
4 notes
·
View notes
Text
Amenorrhea Recovery Diaries - Back into the woods
Getting my period back felt like a new beginning. A new start.
but now it seems to have disappeared, and I feel lost again. I don’t know why it stopped. And I seem to be questioning everything again. Do I have PCOS? Is there something else wrong? Is this why my back pain is getting worse?
0 notes
Note
How do I go about finding out if I am intersex? I have a unilateral labia (only one), pcos (high testosterone and secondary amenorrhea), and pelvic floor dysfunction. I also believe there may have been something done to me as a child , but Idk. I feel like I'm going crazy. I've never felt completely like a girl and I use she/they pronouns, I currently identify as nonbinary.
Any advice would be appreciated, I feel really lost.
Hey, it might be helpful for you to search up hyperandrogenism and/or PCOS on our blog. If that doesn't work then resend the ask and I can try to find some posts, but everything you've said (hyperandrogenic PCOS especially, the other traits can be connected to that as well), if intersex feels like a term that would help you, then you should! No mod on this blog would tell you not to, or that your feelings about your experience aren't valid.
I suggest reading stories from other intersex people, it can be hard to connect to other intersex people right away, but there are a lot of intersex people online who share their stories that I think would be great to explore + you might find comforting.
17 notes
·
View notes
Text
It is wild to me that even in this long thoughtful article about how eating disorders can affect people of all sizes, the writer notes that, well, a 15-yr-old who had amenorrhea, malnutrition, and a "dangerously low heart rate" because she wasn't eating was hospitalized and treated. But then she got fat again and her periods stopped because of PCOS which is more common in fat people so 🤷🏻 maybe the eating disorder was better than being fat, it's complicated! /sarcasm
I don't wish PCOS on you but it's fuck tons less fatal than anorexia.
Diet companies won’t tell you this but starving yourself is a lot worse for your health than overeating
100K notes
·
View notes
Link
#Amenorrhea#Dysmenorrhea#PCOS#PelvicDiseases#PelvicFibroid#PelvicScan#PelvicUltrasound#TransvaginalScan
0 notes
Text
Empowering Women's Health: The Role of Modern Gynecology

Gynecology, a critical branch of medicine, focuses on the health and well-being of the female reproductive system. Its scope encompasses the diagnosis, treatment, and prevention of conditions affecting the uterus, ovaries, fallopian tubes, and breasts. In addition, gynecology often intersects with obstetrics, which deals with pregnancy and childbirth, forming the combined field known as obstetrics and gynecology (OB-GYN). This article delves into the history, scope, common conditions, diagnostic tools, treatments, and future directions of gynecology.Discover trusted Gynecologists Dallas,TX.Offering advanced care for all your women’s health needs.Contact leading specialists near you now.Historical Background
The roots of gynecology trace back to ancient civilizations. The ancient Egyptians documented medical practices for women’s health in the Ebers Papyrus, dating to around 1550 BCE. Similarly, Hippocrates, often regarded as the "Father of Medicine," wrote extensively about women's health in ancient Greece. In the 19th century, gynecology emerged as a distinct medical specialty. Dr. James Marion Sims, despite his controversial methods, is recognized as one of the pioneers in gynecological surgery. The evolution of gynecology has since been marked by advancements in surgical techniques, diagnostic tools, and patient care.
Scope of Gynecology
Gynecology addresses a wide range of medical issues:
Preventive Care: Routine screenings such as Pap smears, mammograms, and pelvic exams are essential for early detection of conditions like cervical cancer and breast abnormalities.
Menstrual Disorders: Conditions such as dysmenorrhea (painful periods), amenorrhea (absence of menstruation), and menorrhagia (heavy menstrual bleeding) fall under the gynecologist’s purview.
Reproductive Health: Gynecologists manage fertility issues, contraceptive counseling, and family planning.
Pelvic and Uterine Health: Conditions like fibroids, endometriosis, and pelvic inflammatory disease (PID) are commonly treated.
Menopause Management: Guidance on hormone replacement therapy and symptom management is a critical aspect of gynecological care.
Gynecological Oncology: The diagnosis and treatment of cancers of the reproductive organs, including ovarian, uterine, and cervical cancer.
Common Gynecological Conditions
Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, causing pain and potentially affecting fertility.
Polycystic Ovary Syndrome (PCOS): Characterized by hormonal imbalances, irregular periods, and cysts on the ovaries, PCOS is a leading cause of infertility.
Uterine Fibroids: Non-cancerous growths in the uterus that can cause heavy bleeding, pain, and pressure symptoms.
Vaginal Infections: Conditions like bacterial vaginosis, yeast infections, and sexually transmitted infections (STIs) are common complaints.
Cervical Dysplasia: Abnormal changes in cervical cells, often detected via Pap smears, which can progress to cancer if untreated.
Diagnostic Tools and Techniques
Modern gynecology employs advanced diagnostic methods:
Ultrasound: Transabdominal or transvaginal ultrasounds are commonly used to visualize reproductive organs.
Hysteroscopy: This procedure allows direct visualization of the uterine cavity using a thin, lighted tube.
Colposcopy: A colposcope magnifies the cervix to identify abnormalities after abnormal Pap smear results.
Laparoscopy: A minimally invasive surgical technique for diagnosing and treating conditions like endometriosis and ovarian cysts.
Treatment Approaches
Treatment in gynecology ranges from lifestyle interventions to advanced surgical procedures:
Medications: Hormonal therapies, antibiotics, and pain relievers are commonly prescribed.
Minimally Invasive Surgery: Techniques such as laparoscopic and robotic surgeries reduce recovery time and complications.
Traditional Surgery: For conditions like advanced cancer, traditional open surgeries may be necessary.
Lifestyle Changes: Diet, exercise, and stress management play roles in managing conditions like PCOS and menopause symptoms.
Physical Therapy: Pelvic floor therapy helps with conditions such as pelvic pain and incontinence.
The Role of Preventive Care
Preventive care is a cornerstone of gynecology. Regular visits to a gynecologist allow for early detection and management of potential health issues. Vaccinations, such as the HPV vaccine, significantly reduce the risk of cervical cancer. Education on sexual health, hygiene, and safe practices also empowers women to take control of their reproductive health.
Challenges in Gynecology
Despite advancements, gynecology faces several challenges. Social stigma and cultural taboos can deter women from seeking care. Disparities in access to healthcare, especially in low-income and rural areas, result in untreated conditions. Additionally, the ethical dilemmas surrounding reproductive rights and technologies continue to spark debate worldwide.
Conclusion
Gynecology is a vital field that addresses the complex and dynamic needs of women’s health. Through preventive care, early detection, and innovative treatments, gynecology continues to improve quality of life for countless women worldwide. However, addressing disparities in healthcare access and breaking societal barriers remain critical to ensuring that all women receive the care they deserve. The continued evolution of this field promises a healthier future for women globally.Find trusted Gynecology in Dallas for personalized care and support.Comprehensive services for every stage of women’s health.Connect with experienced specialists near you now.
0 notes