#ameloblastoma recovery
Explore tagged Tumblr posts
Text
Update!
My apologies for being away from this blog for so long! I ended up getting pregnant, then having complications with the pregnancy (pre-eclampsia and HELLP syndrome) that resulted in a month-long hospital stay and a very premature birth (29 weeks and 5 days, born December 25th), which led to 68 days in the NICU. Since then, it's been a whirlwind of moving into our basement suite, adjusting to parenthood, and getting to all of my and my daughter's appointments. I've developed chronic fatigue and pain since the birth, as well as had continued liver and blood pressure issues, so I'm getting all sorts of tests for autoimmune disorders, liver function, etc.
Now, on to my teeth!
I finally have my final prosthetic! It was a bit of a journey, we started with a fixed appliance for a few months but found that it was simply too difficult for me to clean underneath the bridge and around the screws. Now I have a removable appliance that looks like a metal retainer with teeth attached, see below for photos:




^ Here it is from a number of different angles, including underneath where the attachment points are visible.
It definitely feels weird to have in, as I've gone nearly half a decade without my three lower left molars, and the metal bar feels strange to speak with, but I'm adjusting to it well. I'm still quite tentative about chewing on that side, but this is a functional appliance and I know that I need to use it or risk losing density in the bone graft.
I've had this appliance for nearly a month now, and it's quite comfortable to have in. I take it out at night and let it soak in its case with water and a denture tablet, then in the morning I rinse it off and stick it back in.
What really gets me about this appliance is how natural it looks once it's in. I can feel with my tongue that it isn't my teeth or gums, but the colour and shape and everything matches my other teeth so well that it looks like it's really my teeth!
I have a follow-up appointment regarding this appliance later this month that I look forward to.
It really seems like this is finally wrapping up! I will be sad to leave this blog, and I may continue updating sporadically if checkups or developments occur, but it seems like this journey is nearing its end.
I started this blog as a way to document my journey and store images and progress notes for others who may be undergoing the same or a similar experience. When my ameloblastoma was diagnosed, I could only find a handful of personal accounts about the lesion, none of which continued into the recovery process. It became my goal to to continue my account through my recovery and reconstruction, whatever came up.
I hope that this blog can be a valuable resource for those studying dentistry and/or oral pathology, but most especially for those that feel as I did - scared, overwhelmed, hopeless, and alone.
This side account is linked to my main account, so I should receive notifications if messages are sent with any questions, etc. You may also feel free to follow me on Instagram at pocketwatchesandtea, it is currently set to "private" as I have photos of my daughter on there, but send me a message here with your account when you request to follow and I'll accept and give you access, as my x-ray photos and specimen photos are hosted there.
0 notes
Text
Orbital Ameloblastic Carcinoma – Unusual Presentation in A Non-Odontogenic Location

Abstract
Ameloblastic carcinoma has been described as an ameloblastoma in which there is histological evidence of carcinoma in a primary or recurrent ameloblastoma. The frequency of the lesion is estimated to be less than 1% of all ameloblastomas occurring in the mandible and maxilla.1 We present a case of a 30-year-old woman who presented with painless swelling of left upper face and recurrent upper respiratory tract infections. She was evaluated with CECT, MRI and PET-CT which showed 3.6 x 3.5 x 3.3 cm mass arising from the inferomedial wall of left orbit with sunburst periosteal reaction and cloudy osteoid matrix which was thought to be an osteosarcoma. She underwent a transorbital and trans nasal endoscopic wide local excision of the lesion which was then diagnosed as ameloblastic carcinoma on histopathology. Imaging features and pathological findings of the tumor along with novel treatment strategies and differential diagnosis are discussed in this case report.
Keywords: MRI; orbital tumor; ameloblastic carcinoma; osteosarcoma; CECT; PET
Abbreviations: 18F-FDG-PET: 18F-fluorodeoxyglucose–Positron Emission Tomography; CECT: Contrast Enhanced Computed Tomography; FLAIR: Fluid Attenuated Inversion Recovery; MRI: Magnetic Resonance Imaging; WHO: World Health Organization
Read More About This Article Click on Below Link: https://lupinepublishers.com/otolaryngology-journal/fulltext/orbital-ameloblastic-carcinoma-unusual-presentation-in-a-non-odontogenic-location.ID.000260.php Read More about Lupine Publishers Google Scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=dMOUw-wAAAAJ&cstart=100&pagesize=100&citation_for_view=dMOUw-wAAAAJ:v_xunPV0uK0C
#lupine publishers#lupine publishers group#scholarly journal of otolaryngology#journal of otolaryngology#sjo
0 notes
Text
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery

Parapharyngeal Space Tumors - "A Surgical Challenge"
Authored by Gauri Kokane
Abstract
Parapharyngeal space tumors are rare entity. Overall incidence is less than 0.5%. These tumors are divided into prestyloid and post styloid tumors. Salivary gland neoplasma are common in prestyloid compartment whereas Neurogenic tumors in post styloid compartment. As these tumors are painless and does not express signs and symptoms at early stage, diagnosis of such tumors needs critical evaluation. Anatomic complexity of PPS makes surgical excision more challenging. We have reported 4 cases of parapharyngeal space tumors over a period of 10 years.
Keywords: Parapharyngeal; Schwannoma; Paraganglioma; Neurogenic; Transcervical
Background
Parapharyngeal space is an inverted pyramid from base of the skull to hyoid bone. It is bounded medially by pharynx, anteriorly pterygomandibular raphe, posterolaterally carotid sheath, posteromedially retropharyngeal space, laterally above the level of mandible it is bounded by ramus of mandible, deep lobe of parotid and medial pterygoid muscle, below the level of mandible; it is bounded by posterior belly of diagastric muscle. It is divided into prestyloid and poststyloid compartment by aponeurosis of zuckercandle and testus [1]. 80% of the PPS tumours are benign while 20% are malignant [2]. Incidence of parapharyngeal space tumors is less than 0.5% [3]. Majority of the tumours are slow growing, painless and progressive in nature. If untreated might result in severe life threatening complications like airway obstruction and cranial nerve deficit resulting in significant morbidity. Systematic diagnostic evaluation plays an important role in diagnosis. Surgical excision has Pivotal significance in PPS tumors. We have identified and reported four cases of parapharyngeal space tumors at our centre over a period of 10 years.
Case Description
Case 1
29 year old male presented with complain of painless lateral neck swelling since 3 months. There was no history of dysphagia, Hoarseness of voice. There was no cranial nerve involvement. FNAC showed spindle cell tumor. On MRI there was 50x 37mm well circumscribed lesion over left side of neck suggestive of schwannoma. Surgical Excision of the tumor was done using transcervical approach (Figure 1). There was no intra-operative complication. ICA, ECA, Vagus nerve and IJV were identified and preserved. Tumor was excised completely (Figure 2). Post operatively there was reduction in high pitch sounds. Origin of tumor from vagus nerve was confirmed intra-operatively. Microscopic picture revealed presence of mixed Antoni A and Antoni B cells concluding to the microscopic features of schwannoma.
Case 2
34 year old female presented with painless swelling over right side of neck. CT neck showed 64x46x35mm lesion in the carotid space compressing right IJV and displacing it anterolaterally (Figure 3). Superiorly it was extended up to carotid canal. Differential diagnosis includes paraganglioma in view of intense enhancement of lesion and vagal schwannoma in view of displacement pattern of vessel. FNAC was suggestive of spindle cell tumor. Intraoperatively there was rupture of internal carotid artery which was repaired with 6-0 ethilon, vagus nerve was also sacrificed due to the severe adherence of the tumor to the nerve.
Case 3
24 year old female complains of painless progressive swelling with dysphagia to solids and liquids since 4yrs. CT scan showed heterogeneously enhancing lesion 85x31mm with retrosternal extension displacing major vessels laterally. Intraoperatively transcervical incision was taken and tumor was dissected to free it from the major vessels and nerves and it was removed in to (Figure 4).
Case 4
40 year female patient presented with swelling of left submandibular region since 1 month (Figure 5). FNAC showed spindle cell tumor, USG showed 41x39mm Heterogenous mass and left submandibular gland. CT Scan Showed 4.5cm enhancing well circumscribed lesion, left submandibular gland and another 1.3x1cm lesion adjacent to it. No dysphagia or hoarseness of voice, intra-operatively Hypoglossal nerve was sacrificed. Lingual nerve was identified and preserved. Histopathology report showed neurogenic tumour i.e. schwannoma.
Discussion
Para-pharyngeal space (PPS) tumors are very rare. We have identified 4 patients after reviewing 10 years retrospective data of all head and neck tumors presented at Manavata curie cancer centre Nashik. Incidence of parapharyngeal space tumors at our institute was 0.004%. Overall incidence of these tumors is less than 0.5%. These tumors are slow growing, painless and patients express at later stage when the size become considerably large. Usually patients are asymptomatic but may exhibit dysphagia or hoarseness of voice. In our 4 patients only one patient had dysphagia to solids and liquids rest of the patients were asymptomatic [4,5]. 80% of the tumors arising in this region are benign [2]. Pleomorphic adenoma is the most common tumor of prestyloid compartment where poststyloid tumors are mostly neurogenic like shwannoma, paraganglioma, neurofibroma, hemangiomas etc. Chordomas, lypomas, lymphomas, chemodectomas, rhabdomyomas, chondrosarcomas, desmoid tumours, ameloblastomas, amyloid tumours, ectomesenchymomas, fibrosarcomas and plasmocytomas have also been reported [2].
Diagnosis of these tumors is difficult as they are asymptomatic. Diagnostic evaluation constitutes CT scan and MRI to clearly define the extent of the tumor mass. Arteriography also plays a significant role to assess vascular compression. In our identified cases CT scan was performed in 3 cases and MRI in one case. MRI has been shown to gives better dimensions of the parapharyngeal space tumors. Advantage of MRI is, it distinguishes tumor from Muscular structures and give better dimentions of the tumor [6].
Arteriography was not performed in any of our cases. Once the nonvascular nature of tumor is confirmed by radio-imaging, FNAC can be performed for definitive diagnosis. FNAC is accurate in 90-95% of the cases and helps in surgical planning [7]. Limited role is explained in post styloid compartment. We performed FNAC in all our patients and it was conclusive [8,9].
Schwannoma may arise at any age but in our institute patient's age ranged from 3rd to 4th decades of life. There is no gender predilection. Schwannoma may be of two types histologically consisting of either Antoni A cells or Antoni B cells. We had two patients with Antoni A cells and other one was of mixed variety [10]. Paragangliomas are tumors of autonomic nervous system. Head and neck paragangliomas are unique in its variety as they don't release catecholamines. Incidence of paraganglioma is 1 in 30,000 cases [11]. Histopathological picture shows two types of cells; Chief cells and sustantecular cells. One of our patient's histological features were identical to it.
Surgical management of parapharyngeal space tumors is very challenging owing to anatomic complexity ofthe space and vicinity of the tumor with major neurovascular structures. There are 7 different approaches described for PFS tumors. Transcervical, Transcervical- transparotid, Transoral-transcervical approach, Extended approach, Transcervical-mandibulotomy aaproach, Transcervical-transmastoid approach have been explained [12]. 4cm is the limit for radical tumour excision with the transcervical approach without mandibulotomy. For a safe and radical resection of tumours > 4cm the “swing” approach or the transmandibular with a double osteotomy is required [2]. We used transcervical approach without mandibulotomy in all cases. Accesiblity was compromised in larger tumors but we could enucleate entire tumor without much difficulty. ICA was ruptured in one case but it was managed. Minimal accessibility may be a compromise but there is less surgical morbidity and post op recovery is faster in our experience.
Complications after surgical management are unavoidable. Expected complications are due to sacrifice of cranial nerves. There may be unexpected neurological complications in spite of preservation of nerves like first bite syndrome, Trismus, facial nerve weakness, orocutaneous fistula, Seroma. We experienced loss of high pitched sounds in two of our patients and there was hypoglossal nerve palsy as hypoglossal nerve was sacrificed in one case.
Conclusion
CT scan or MRI should always be performed in order to distinguish prestyloid from poststyloid lesions and assessment of the extension of the tumour and its relationship with adjacent structures. Trans-cervical approach is safe and should be the first choice for large tumors; other approaches are reserved for selected cases.
Clinical Significance
These are painless slow growing non malignant tumors with very less incidence of recurrance. Management of PPS tumors is challenging for surgeons. Neurological and Surgical complications should always be explained to patients preoperatively. Preoperative assessment and careful surgical manipulation are of utmost importance.
For more articles in Open access Journal of Head Neck & Spine Surgery | Juniper Publishers please click on: https://juniperpublishers.com/jhnss/index.php
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Simple Bone Cyst of the Anterior Mandible: A Case Report
Authored by Rattana-arpha Pornpop
Abstract
Simple bone cyst is a benign pseudo cystic cavity in the bone that is either empty or contains fluid. It is an uncommon disorder of the jaw bones as well as the other skeletal bones, particularly the long bones. The body of the mandible is the most common site of the jaw bones. Its onset occurs mainly during the first two decades of life. This article will describe the case of a SBC located in the anterior mandible of a 15 years old female patient including clinical, radiographic, histopathologic features and its treatment.
Keywords: Simple bone cyst; Anterior mandible; Differential diagnosis
Introduction
Simple bone cyst (SBC) was first recognized by Lucas & Blum in 1929 [1]. Blum reported the first three cases in dentistry in 1932 [2]. It has been identified with many names such as solitary bone cyst, traumatic bone cyst, hemorrhagic bone cyst, unicameral bone cyst, progressive bone cavity, extravasation cyst, primary bone cyst and idiopathic bone cavity [3]. Trauma is the most frequently discussed about its etiologic factor in the formation of SBC. Most of SBC are diagnosed incidentally in panoramic radiograph and most of the individuals affected are in teens [4]. Radiographically, it manifests as a well-defined unilocular, radiolucency which occasionally presents a typical festooned pattern around the apices of the adjacent teeth [5,6]. Definite diagnosis of SBC is inevitably reached during surgery when a cavity lacing epithelial lining is either empty or with content or filled with serous or sanguineous fluids [6]. This report describes a rare SBC case of anterior mandible with incidental finding from panoramic radiograph.
Case Report
A 15 years old female was referred to the clinic by a general dentist for evaluation of an asymptomatic radiolucent lesion located in the anterior mandible. The medical history was not contributed and she could not recall a history of trauma. Extra-and intraoral examinations revealed no abnormal findings. The lower anterior teeth were not mobile and positive for the vitality tests. No palpable lymph node was presence.
Panoramic radiograph revealed a well-defined unilocular radiolucent area of size 2×3.5cm extending from inferior aspect of the roots of lower right canine to lower left canine (Figure 1 & 2). The inferior border of the mandible was not affected. The lateral cephalometric radiograph revealed a mild labial expansion with a thin labial cortex. The radiographic differential diagnosis comprised odontogenic keratocyst, unicystic ameloblastoma, central giant cell granuloma and SBC.
Under local anesthesia, a biopsy was performed before the determination of the definitive treatment. On surgical exploration, the lesion was found to be an empty cavity, with no evidence of epithelial lining or tumoral tissue, and contained small amount of fluid mixed with blood. The operative findings were suggestive of SBC; therefore, curettage of the cavity was performed. The removed pieces of bone with minimal amount of soft tissue were sent for histopathological examination. Histopathologically, the section revealed thin strips of osseous wall and overlying fibrous connective tissue with no epithelial lining (Figure 3 & 4). Extravasated erythrocytes and congested blood vessels were also seen. On the basis of clinical, radiological and histopathological findings, thus, a final diagnosis of SBC was made. The postoperative recovery was uneventful and the complete healing was observed one year later.
Discussion
The SBC is an uncommon non epithelial-lined cavity of the jaws, found mainly in young patients [7]. Most of them are found in the posterior mandible between the canine and the third molar followed by the mandibular symphysis [7]. Clinically, the lesion is generally asymptomatic and is often incidentally discovered during routine radiological examination [4]. Pain is infrequent and presents in 10% to 30% of patients [8]. Radiographically, the SBC generally shows up as unilocular radiolucency, which its margins are characteristically scalloped among dental roots [4,7,9,10]. Definitive diagnosis of SBC is done with surgery when an empty space without epithelial lining is observed, with very little amount of fluid [8,10]. Associated conditions such as cement-osseous dysplasia and fibrous dysplasia were reported and it seemed to be occur in the older patients [11,12].
In this present case, the patient was a young female without any symptoms. The age, the clinical finding and the site of the lesion led the clinician to suspect benign lesion. Radiographic features of this case can be confused with a wide variety of odontogenic and non-odontogenic radiolucent lesions of the anterior lower jaw such as the unicystic ameloblastoma, odontogenic keratocyst, glandular odontogenic cyst and central giant cell granuloma. Therefore, a surgical exploration is needed to establish the correct diagnosis. The diagnosis of this SBC case is achieved in conjunction with the clinical, radiographic and histological features.
The pathogenesis of SBC remains unclear. The most accepted version of the SBC is the traumatic-hemorrhagic theory, which suggests that lesions develop if intramedullary clots due to trauma do not undergo lysis or resolution [4]. In this case, the patient could not experience of previous trauma or interventions in the interested area. However, micro trauma could not be excluded.
The most commonly recommended treatment for SBC is surgical exploration of the lesion followed by curettage of the bony walls. This surgical exploration serves both as diagnostic maneuver and definitive therapy by producing bleeding in the cavity. This bleeding helps to form a clot which is eventually replaced by the bone [3]. The recurrence rate of SBC is between 20% and 30%. Cases of multiple cysts or associated with florid cemento-osseous dysplasia have high recurrence ratesrespectively about 71% and 75% [13,14].
Conclusion
SBC is a rare pseudocyst of the jaw bone with an unclear etiology. Diagnosing SBC is a challenging since it can be achieved in conjunction with the clinical, radiographic and histological features. The most commonly recommended treatment for SBC is curettage after surgical exploration of the lesion. It is generally associated to a good prognosis with a low recurrent rate.
For more Open Access Journals in JuniperPublishers please click on: https://www.linkedin.com/company/juniper-publishers
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555626.php
#Juniper Publishers Review#Juniper Publishers Journals#Geriatric Medicine#Medical Genetics#Pulmonology#Surgical Oncology#Vascular surgery
0 notes
Text
Surgery went well yesterday, I'll be putting a post up on my sideblog @ameloblastomadiary to talk about it :)
0 notes
Text
Big Things
Today, I received the contact information for our province's Minister of Health.
For those of you who don't know, based on my province's health coverage, only my initial big surgery was covered.
My followup procedures, braces, metal screws, and upcoming prosthetic are not covered by the province. I still live at home, so I am able to take advantage of my parents' extended health and dental coverage.
The way that our provincial healthcare works is that it covers things to do with the body, and things in hospital. Inside of my mouth is considered "dental" and is thereby not covered.
The extended coverage considers dental implants and prostheses to be "cosmetic," and so that is not covered either.
Our province will cover prostheses for limbs, partial hands and feet, breasts, eyes, noses and ears. The province will also cover maintenance of the aforementioned prostheses.
I do not believe that it is right or fair that my reconstructive prosthetic should be considered "cosmetic" and not be covered simply because it is not two to three inches higher.
Because my reconstruction is inside of my mouth, I will be having to pay tens, if not hundreds of thousands of dollars out of my own pocket for the rest of my life to purchase and maintain my prosthetic.
I lost a ~5cm section of my jawbone and three teeth due to a (luckily benign) aggressive cancer. I hate referring to it as "cancer" because I feel as if I am not deserving of the title of "cancer survivor," due to my not having had to go through chemotherapy and the typical journey that we think of cancer survivors having gone through. That said, the reason I did not go through chemotherapy is because ameloblastomas do not respond at all to radiation.
Please wish me luck as I go to my provincial government to lobby for change! I hope that I am able to create positive change that will support myself and other survivors of oral cancers.
4 notes
·
View notes
Text
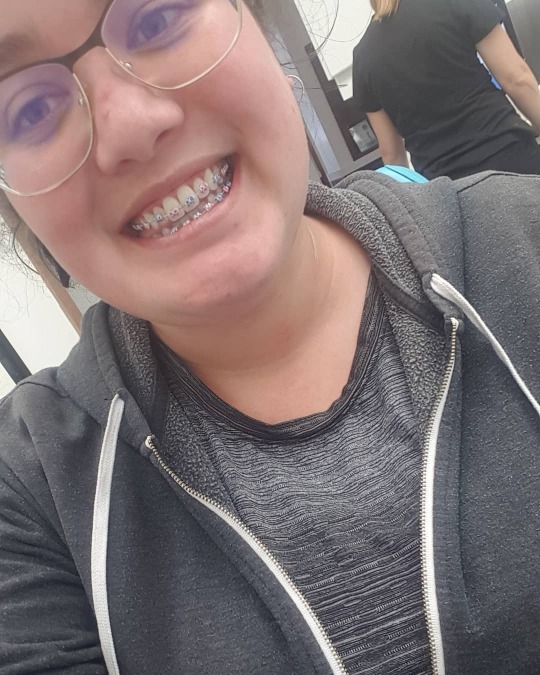
My braces went on yesterday! I like them aesthetically, but they are super sore and uncomfortable and bumpy inside my mouth. I'll post a more in-depth post later on them!
17 notes
·
View notes
Text
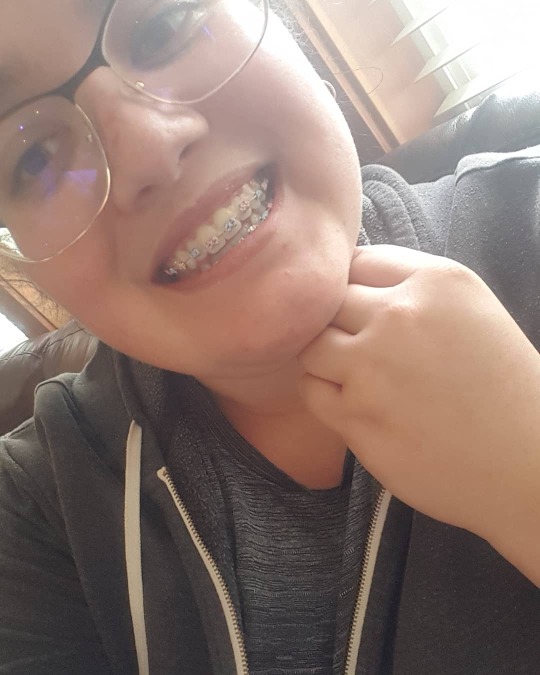
Had my first braces tightening today!
My top teeth are all in position, so we are just straightening out my bottom teeth before widening my bite. Top teeth have been chained, bottom teeth are still individual ties, and I now have elastics to wear at night.
In terms of adjusting this past month, this hasn't been too horrible. The first few days sucked, and I wanted to rip my teeth out of my head, but I've adjusted to them. The inside of my mouth has also gotten accustomed to them and I don't feel like I've got a cheese grater in my mouth all the time anymore.
But comapred to losing a chunk of bone and 3 molars and some hip bone, this is a cakewalk.


Excuse my shitty selfies, haha.
Also, I got my elastics on the first try so I'm quite proud of myself.
#my face#news#ameloblastoma recovery#braces#adult braces#the top chain is a pearlescent purple but it looks blue stretched out and the bottom ties are pearlescent green
16 notes
·
View notes
Text
A Huge Milestone
Today marks the first time I've played clarinet in nearly two years.
I haven't played since my surgery back in 2018, initially because I needed the jaw to heal, and then because I was afraid of how much of my muscle tone I had lost. I was so scared that I would be starting from zero and need to re-learn how to make the sounds happen. I was also concerned that the numbmess on my lower left quadrant of my lips would affect my ability.
Fortunately, I didn't lose as much as I thought I had! I picked it up and played a basic scale a couple of times. Then I played a higher scale, and higher, until I realized I was able to play all the notes that I used to be able to. I played a few of my favourite songs from my very dog-eared Hal Leonard Pirates of the Caribbean sheet music book, as well as some Andrew Lloyd Webber favourites.
I only played for half an hour, because my braces started to bother me, but I'll adjust to that in time.
I really feel like myself again, and playing this instrument really feels like I'm coming home to myself.
5 notes
·
View notes
Text


Just wrapped up my talk at the Pacific Dental Conference!
I feel like it went very well.
Unfortunately, my camera stopped recording after about 11 minutes, which is really too bad. I had wanted to record it and post it on youtube, but I guess that can't happen. Next time I do a talk, I'll try to record it.
4 notes
·
View notes
Text
Another update!
I saw my specialist this past Wednesday and things are going well! I am healing well, and I got the OK to start braces. I called the orthodontist's office and they've scheduled me in for July 8th, so from that point I'll be braceface for a while!
1 note
·
View note
Text
Surgery Update!
I just had my most recent surgery this past Wednesday, the 26th of February, 2020. It went surprisingly well, despite a few complications.
The bone in the back of my jaw was not stable, as per usual, and some bone was contaminated again, so my surgeon had to scrape out the contaminated bone and repack the graft.
I also woke up once or twice, which has always been my biggest fear with surgery, but it wasn’t scary, and I was so frozen that I couldn’t feel anything. I remember opening my eyes and seeing them working and being told they weren’t done yet, so I went back to sleep. The other time, I remember hearing the drill, but it didn’t scare me because that’s a normal jaw surgery sound. If I had woken up and they were doing something else I would’ve been scared, but it was all as expected, so I was fine.
Despite this, we were able to get the three screws in for my implants! I’m still tender today, but every day gets monumentally easier to deal with the pain. I’m not even especially swollen as evidenced by this photo:

(Look how cute my bangs are!)
I have a followup appointment next Wednesday, March 4th, then my talk on the 7th at Pacific Dental Conference! If I can get someone to record the talk, I will post it to YouTube and link it here, as well as on other social media.
I am back to liquids/blenderized food only again, for at least a week. Hopefully, it won’t be 7 months like last time! I don’t expect to be able to eat hard crunchy stuff, but I’m hoping to be able to have bread, pasta, rice, oatmeal, etc, since that’s all more filling than just smoothies, yogurt, soup, etc. I can do the all-liquid thing, but I don’t like to.
Once the bone is more integrated with the screws, I probably will be able to eat normally.
And at some point, maybe in a month or so, I’ll get those braces on, get my teeth in the right position, and then we can pop on the prosthetic and be done with this all!
This was yet another surgery, but it’s finally moving forward. I feel like this is actually moving towards living normally again, as opposed to just going back in to clean out bad bone because I just didn’t heal properly last time.
Here’s to starting to see the light at the end of this long, long tunnel!
1 note
·
View note
Text
So apparently, I can't post images right now, and that's what's been keeping me from being able to post that I've been braces-free since June 14, 2022!
I now have bonded retainers on the top and bottom, as well as tray style retainers for night which I fill with MI Paste for remineralization, or Cresr Whitening Emulsions for stain removal.
Next Wednesday, I'll be seeing my specialist to figure out a timeline for getting my prosthetic in!
Today also marks exactly 4 years since that initial dentist appointment where my tumour was discovered, so that's interesting. I've gotten some other worrying health news today, so it's been difficult to cope with that as it feels quite close to when my tumor was found. Fingers crossed that it all turns out well, I'll be seeing my family doctor on Tuesday to discuss that.
1 note
·
View note
Text
Finally an update!
I recently saw my orthodontist and my specialist. They have agreed that the best course of action for my prosthesis will me a hybrid appliance, which means my braces are probably good to come off soon.
I'll need a procedure to expose the implant screws and attach healing abutments, and then once that's healed the prosthetic can go in!
I'm so ready, it's been 3 and a half years without those molars for me.
0 notes
Text
Long time, no update!
I've been wicked busy with school, so I haven't been able to dedicate as much time as I would like to this.
So, in the past little while, I've had my braces adjusted here and there, and a fresh new X-ray from the other day.
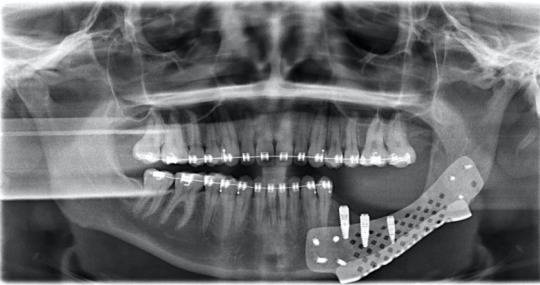
It's definitely interesting so see how my teeth have shifted, and to see the braces in the radiograph!
I also gave another talk about this whole process last night via Zoom to a class at UBC. I feel very confident with how it went, possibly being the best lecture I've delivered to date! I was able to invite some family and friends to watch, and I felt very good about the whole thing.
0 notes
Text
Liquid
So, I'm still on liquid/puree since my most recent surgery in February. We are being super careful this time so that I dont split my gums open or anything again this time.
In some ways, it's nice because I can just stick with one or two menus for my day, but I definitely miss solid food.
A nice side effect is that I'm losing weight like crazy. I get bored cooped up at home so I try to get some exercise in most days (as intense as I'm allowed, which is Not Intense At All), and that coupled with only having liquids/pureed foods means I'm very close to being down 30lbs since the morning of my first surgery in November.
So I'm hanging onto that as a positive for this situation. May as well make the most of it.
And as of like Friday or Saturday, all of my mouth stitches are out. I'm hoping that the tissues are strong enough to hold together on their own. I'll be seeing my specialist tomorrow, so hopefully it's all good.
0 notes